Introduction
Pseudoaneurysms are caused by some forms of arterial
injury, which include perivascular inflammatory reactions or
infections, direct vascular trauma or iatrogenic factors (1,2). With
the advancement of complex surgical operations, iatrogenic
pseudoaneurysms are relatively commonly encountered in clinical
practice. Patients may present with sentinel bleeding or delayed
hemorrhage, which may be easily overlooked (3). These pseudoaneurysms, with the lack of
complete vascular wall structure, gradually increase in size and
are under a growing strain with the continuous impact of blood
flow, eventually resulting in burst and sudden bleeding.
The overall incidence of pseudoaneurysms following
abdominal and pelvic surgery or radiological intervention is
relatively low (4,5). If appropriate treatment is not
undertaken in a timely fashion, pseudoaneurysm may be associated
with high morbidity and mortality. Visceral artery pseudoaneurysms
(VAPA) refer to pseudoaneurysms occurring in the celiac artery,
superior mesenteric artery, or inferior mesenteric artery and their
branches. VAPA may manifest as gastrointestinal hemorrhage
(hematemesis, hematochezia) or abdominal hemorrhage (hematoma,
abdominal hematoma), which is frequently evident as continuous
hemorrhagic fluid from the abdominal drainage tube. A
pseudoaneurysm from the pelvic internal iliac artery may also
manifest as abdominal and pelvic hemorrhage or hematoma. A
pseudoaneurysm may be particularly life-threatening among patients
with thrombocytopenia or consumptive coagulopathy and therefore,
these patients require rapid clinical evaluation and treatment
(6,7).
Ultrasound with doppler and contrast-enhanced
techniques are commonly used as an initial screening tool for
pseudoaneurysm (8). However, CT
angiography (CTA) and digital subtraction angiography (DSA), are
the formal diagnostic tools for pseudoaneurysm (9). On CTA, a pseudoaneurysm may be seen as
a bubble-shaped (saccular), irregular nodule budding from the
lateral wall of the artery. DSA may not only clearly show the
location, size and shape of the pseudoaneurysm but also its
relationship with the parent artery (10,11).
Pseudoaneurysms are conventionally managed by surgery, including
surgical ligation, aneurysm resection and even the removal of
affected organs. More recently, endovascular embolization has
gradually become the preferred option of treatment instead of
surgery, given that it may be rapidly applied to hemodynamically
unstable patients while avoiding major surgical trauma,
particularly among patients with extensive comorbidities. Several
studies have also indicated high success and low recurrence rates
of pseudoaneurysm treated by endovascular embolization, justifying
the expansion of its applications in clinical practice (12-14).
The present study provided a retrospective review,
reporting on the practice and experience of endovascular
embolization at the Affiliated Hospital of North Sichuan Medical
College (Nanchong, China). The clinical effectiveness and safety of
this treatment for secondary pseudoaneurysm following abdominal and
pelvic surgery or radiological percutaneous abdominal procedure
were investigated.
Materials and methods
Patients
All patients with pseudoaneurysm secondary to
radiological intervention or abdominal or pelvic surgery, who were
then treated with endovascular embolization from January 2014 to
May 2019 at the Affiliated Hospital of North Sichuan Medical
College were included in the present study for a retrospective
review. The present study was approved by the Ethics Committee of
the Affiliated Hospital of North Sichuan Medical College (Nanchong,
China). Written informed consent was obtained from all
patients.
Inclusion and exclusion criteria
The inclusion criteria were as follows: i) patients
presented with symptoms of bleeding after abdominal or pelvic
surgery; and ii) patients without contraindications that underwent
emergency arteriography or embolization therapy. The following
exclusion criteria were applied: i) patients who are allergic to
iodinated contrast media; ii) patients who refused interventional
therapy; and iii) patients who underwent angiography without
embolization.
Angiography and endovascular
embolization technique
The Seldinger technique was used to puncture the
femoral artery percutaneously, followed by the insertion of a 5F
catheter sheath, as described in the previous study (15). Subsequently, a 5F Pig catheter, RH
catheter, Yashiro catheter and Simon 1 catheter (Terumo or Cordis
Co.) were inserted. Angiography of the abdominal aorta, celiac
artery, common hepatic artery, splenic artery, gastroduodenal
artery (GDA), superior mesenteric artery, inferior phrenic artery,
inferior mesenteric artery, and the internal and external iliac
artery, respectively, was performed to determine the location of
bleeding and pseudoaneurysm, the size of the parent artery and the
condition of collateral vessels.
A coil was routinely used for embolization at the
Affiliated Hospital of North Sichuan Medical College. Various
techniques for coil applications, including sac packing, isolation
and sandwich, were applied using the Tower or Diamond coils (Boston
VortX™-18 platinum coil or VortX™-18 Diamond platinum coil; 0.018
inches; Boston Scientific) and/or detachable coil embolization
system (Interlock Fibered IDC occlusion system; 0.018 inches;
Boston Scientific). The sac packing technique referred to the
filling the pseudoaneurysm sac with microcoils using coaxial
technology to push the distal end tip of a microcatheter (Renegade™
STC18; Boston Scientific) into the lumen and neck of the
pseudoaneurysm. The isolation technique involved occluding the
inflow and outflow embolization of the parent artery (exclusion
embolization), while sandwich embolization involved embolizing the
efferent artery, aneurysm cavity and afferent artery of the parent
artery, respectively. When a pseudoaneurysm had been located on the
lateral wall of the artery, the microcatheter was super-selectively
placed to the sac, for which the sac packing technique was applied
to maintain the patency of parent artery. If the pseudoaneurysm
lumen was small and microcatheter insertion was difficult,
isolation embolization was used instead of sac packing. The
sandwich technique was performed for large pseudoaneurysms, or with
collateral inflow and outflow arteries.
Post-embolization outcome
assessment
When technical and clinical embolization therapy
success was achieved, the study was stopped. The definitions and
criteria for the effectiveness, technical success and clinical
success of embolization were according to the Guidelines of the
Society of Interventional Radiology (SIR) (16). Technical success was defined as the
arrest of bleeding, disappearance of the pseudoaneurysm or
occlusion of the parent artery. Clinical success referred to the
absence of acute bleeding symptoms, stable hemodynamics, decrease
in hemoglobin no more than 15 g/l compared with the baseline level
of hemoglobin prior to embolization, no requirement for blood
transfusion, no evidence of ongoing loss of blood in the abdominal
drainage tube and no requirement for re-angiography or surgical
intervention (17). The short-term
clinical outcomes and the long-term clinical outcomes were
evaluated, including abdominal pain, fever and other clinical
parameters, including hemoglobin levels, signs of hemorrhage and
vital signs. Follow-up CTAs or enhanced CTs were also reviewed
within 6 months after embolization to evaluate the recurrence rate
of the pseudoaneurysm or any evidence of ectopic embolism. The SIR
criteria were also used for the classification of complications
after embolization.
Results
Clinical features and angiographic
findings
A total of 31 eligible patients were identified and
included in the present study. Of these, 17 patients developed
abdominal pseudoaneurysm following pancreaticoduodenectomy (PD), 5
after subtotal gastrectomy, 3 after a biliary operation, 5 after
resection of hilar tumors and 1 patient after the radiological
percutaneous drainage of an intra-abdominal collection (Table I). There were 5 females and 26
males, with the age of 58.24±8.35 years. All patients presented
clinically with either symptoms and signs of gastrointestinal
bleeding, abdominal hemorrhage, drainage of hemorrhagic fluid
through a drainage tube or local hematoma at varying degrees.
 | Table IClinical data of patients with
iatrogenic pseudoaneurysms. |
Table I
Clinical data of patients with
iatrogenic pseudoaneurysms.
| Pathogeny | Case, n (%) | Sex ratio,
male/female | Location and number
of aneurysms (n) |
|---|
| Post
pancreaticoduodenectomy | 17 (54.8) | 13/4 | Main GDA (8) |
| | | | Superior
pancreaticoduodenal artery (5) |
| | | | Right gastroepiploic
artery (3) |
| | | | Splenic artery
(2) |
| Postoperative gastric
cancer | 5 (16.1) | 3/2 | Main GDA (2) |
| | | | Splenic artery
(3) |
| Postoperative
biliary surgery | 3 (9.8) | 2/1 | Main GDA (1) |
| | | | Right
gastroepiploic artery (1) |
| | | | Right hepatic
artery (1) |
| Postoperative
treatment of hilar tumors | 5 (16.1) | 3/2 | Main GDA (3) |
| | | | Common hepatic
artery (2) |
| Postoperative
puncture drainage | 1 (3.2) | 0/1 | Branches of right
internal iliac artery (1) |
A total of 32 pseudoaneurysms were detected among
these patients, of which 23 were located at the main trunk and
branches of GDA, 5 were located at the splenic artery, 2 were
located at the common hepatic artery, 1 was located at the right
hepatic artery and 1 was located at the right internal iliac
artery. Of note, one patient was determined to have developed 2
pseudoaneurysms at the right gastroepiploic artery following
PD.
On angiography, the pseudoaneurysm displayed as a
cystic shadow that protruded out of the artery. It appeared as a
round or irregular-shaped nodule with sharp angles on the sac and
clear edges. The parent arteries were mostly spasmodic, narrowed
and stiffened.
All patients had progressive deterioration in the
level of hemoglobin at varying degrees. In one patient with a
continuous decrease in the hemoglobin level, the initial CTA did
not reveal any evidence of pseudoaneurysm but the subsequent DSA
was performed given the evidence of ongoing blood loss, which
revealed a pseudoaneurysm of the right hepatic artery.
Embolization techniques and
outcomes
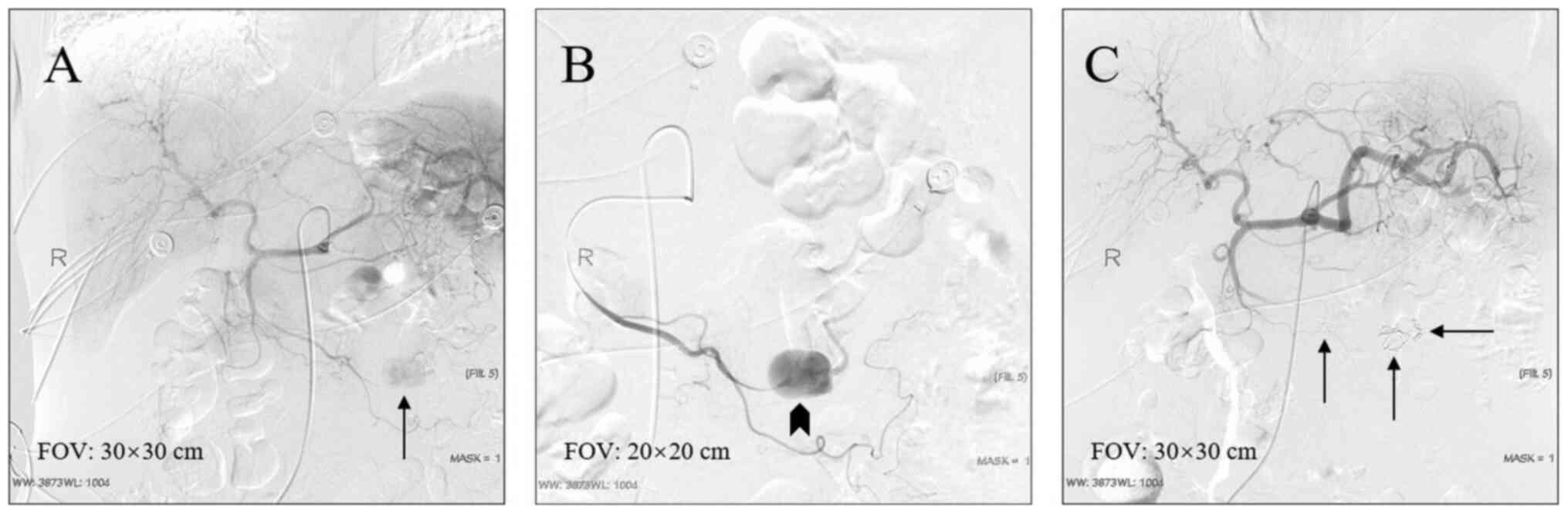
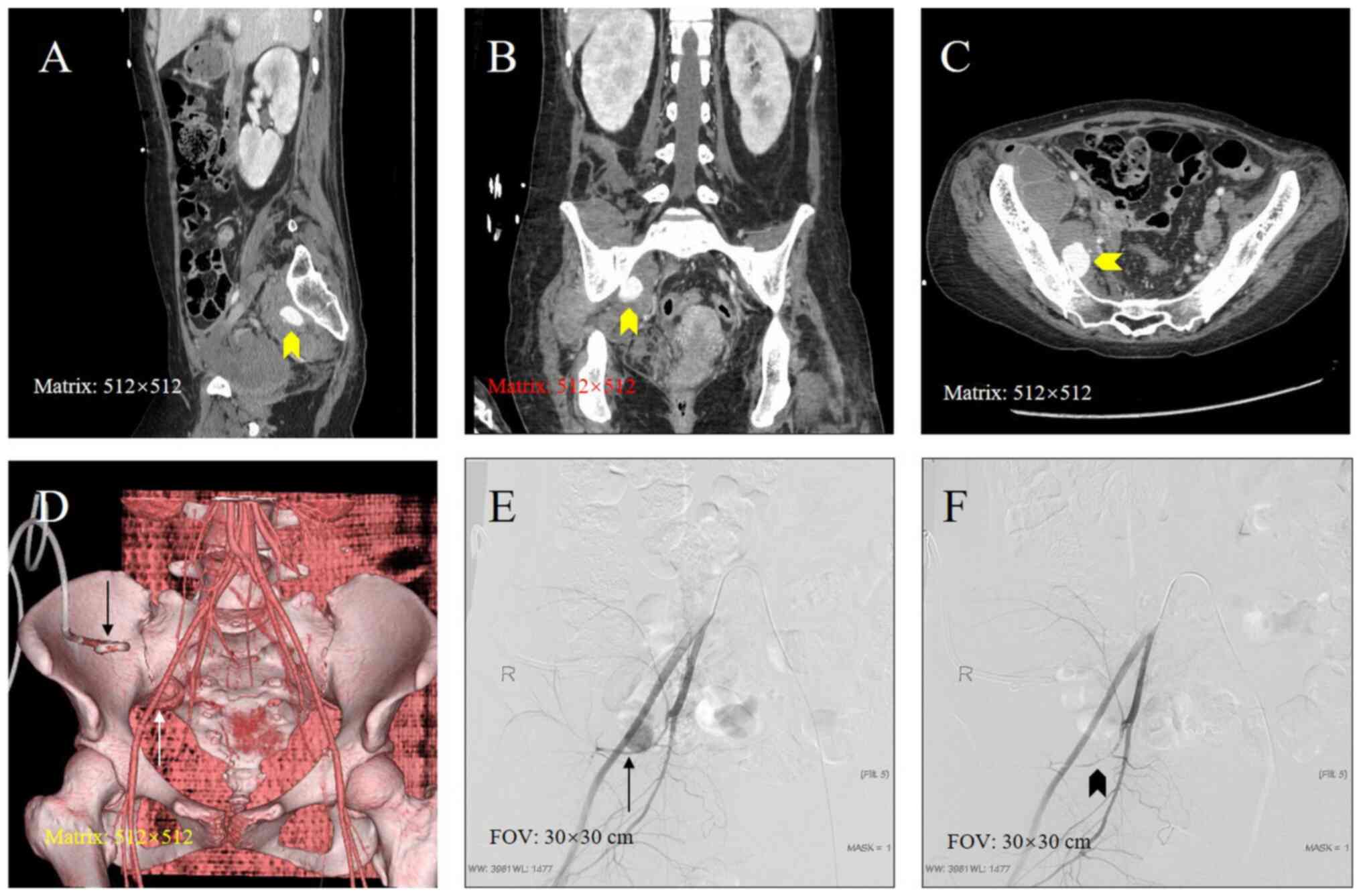
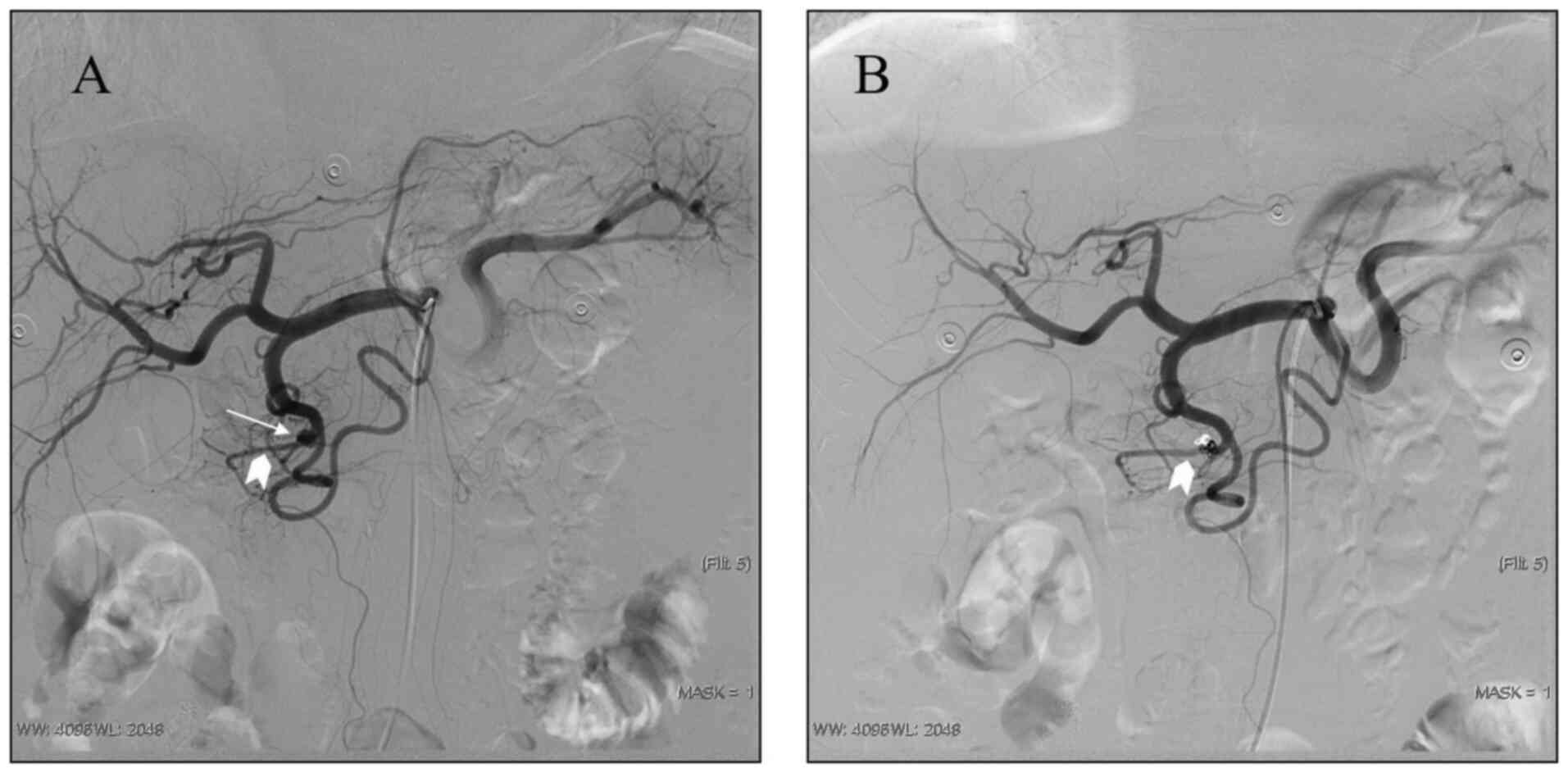
The isolation technique was most commonly performed
(19/32, 59%) for embolization, followed by the sandwich technique
(8/32, 25%; representative cases in Figs. 1 and 2), the sac packing technique (3/32, 9%;
representative case in Fig. 3) and
the proximal embolization technique (2/32, 6%). Pseudoaneurysms
located at the main trunk of the GDA and pancreatoduodenal artery
with no obvious communication with the superior mesenteric artery
and the splenic artery, were embolized with the sac packing
technique. The proximal embolization technique was used to embolize
the pseudoaneurysms that were located at the distal end of the
artery without collateral arteries. Of the 32 embolization
procedures performed, distal migration of the coil was observed in
1 patient only (Fig. 4).
Among 5 patients with splenic artery pseudoaneurysm
undergoing sandwich embolization, the subsequent imaging did not
indicate any large area of splenic necrosis and these patients did
not develop any significant splenic infection. However, one patient
with right hepatic artery pseudoaneurysm embolized by using the
sandwich embolization technique had developed transient hepatocyte
damage, as evidenced by the derangement of alanine transferase and
aspartate aminotransferase in the blood liver function test. All
embolization procedures had a technical and clinical success rate
of 100% (32/32); none of the patients required repetition of the
procedure and all patients achieved complete hemostasis following
embolization with no episode of re-bleeding. A total of 2 patients
with pancreatic head carcinoma died of multiorgan failure secondary
to severe infection 2 weeks after PD, but their deaths were not
directly associated with pseudoaneurysm or endovascular
embolization. There were no severe complications such as
gastrointestinal ischemia and necrosis.
Discussion
Pseudoaneurysm is usually caused by the disruption
of arterial wall continuity. Such a disruption may be secondary to
direct injury during an abdominal procedure or surgery or various
endovascular treatments, or an indirect injury from post-operative
peri-vascular inflammation or infections (18-20),
resulting in the formation of pseudoaneurysm. The majority of
patients in the present study had received hepatobiliary/gastric
surgery. Such predilection may have been due to corrosion of the
arteries around the pancreas by the pancreatic juice, causing
pseudoaneurysm formation and delayed bleeding (11,21).
The use of electrocautery and ultrasonic scalpel in the process of
clearing the lymph nodes around the artery and removing its
adventitia in addition to clamping of vessels during surgery may
also lead to vascular injury and subsequent pseudoaneurysm
formation (22). Therefore, it is
not surprising that in radical hepatobiliary/gastric surgery, the
elevated incidence of surgical complications was correlated with an
increase in mortality rate associated with bleeding and
pseudoaneurysm (22-25).
The risk of spontaneous rupture of a pseudoaneurysm
is high and sentinel bleeding is generally regarded as a precursor
of massive hemorrhage (3).
Therefore, rapid and accurate diagnosis is crucial, with CTA having
a sensitivity and accuracy rate of 95% (26,27).
CTA is able to indicate the size and location of the aneurysm and
its relationship between the parent artery and neck. One of the
patients of the present study had a false-negative result on CTA,
and DSA was used in this instance as a diagnostic adjunct to CTA.
It also offers the possibility of therapeutic interventional
therapy at the same time. During DSA, attention should be paid to
the observation angle, flow rate and injection pressure of contrast
agents to avoid missing small aneurysms. When necessary,
magnification and multi-angle angiography should be performed
(26-28).
Acute torrential hemorrhage from pseudoaneurysm may
be treated by open surgical exploration/ligation or endovascular
embolization (29). The following
factors may affect the clinician's choice of different treatment
methods: i) the time of bleeding and pseudoaneurysm; ii)
comorbidities and complications, such as inflammation and
infection; and iii) hemodynamics. Ligation, aneurysm resection and
removal of an involved organ are the major methods of surgical
treatment. Compared with the open surgical approach, endovascular
therapy prevents any potential risk of serious complications caused
by re-operation while minimizing further stress to impair the
patient's organ function (13,17).
Furthermore, the present study suggested that endovascular
embolization was highly effective, that there was no further
bleeding following the single intervention and no recurrence of
pseudoaneurysm was observed in any of the patients.
The endovascular approach to pseudoaneurysm consists
of either covered stent implantation or embolization. Endovascular
graft exclusion with a covered stent may completely isolate the
pseudoaneurysm immediately, prevent the rupture and bleeding of the
pseudoaneurysm and reconstruct the parent artery without affecting
the anatomical blood flow (30).
This is suitable for pseudoaneurysm that has sentinel hemorrhage
without rupture. However, a covered stent is usually not the first
choice due to the risk involved and the technical difficulty of
stenting in a visceral artery, in addition to the contraction of
the parent artery caused by the use of vasoconstrictive drugs.
Furthermore, economic and medical insurance factors are also
reasons for its limited application. Therefore, endovascular
embolization is widely used in clinical practice, including the
Affiliated Hospital of North Sichuan Medical College, as reported
in the present and previous studies (31-34).
For VAPA, due to the anastomosis of digestive arteries and abundant
collateral circulation, liquid embolic materials should be
carefully selected to prevent the occurrence of missed
embolization, and solid embolic agents generally do not cause
serious ischemia and necrosis (5).
The present study demonstrated that coil embolization is a safe
therapy for pseudoaneurysm and no serious complications were
encountered.
The selection of embolization techniques is mainly
based on the location, size and the neck of the pseudoaneurysm
(35). At the Affiliated Hospital
of North Sichuan Medical College, if the pseudoaneurysm occurs at
the main visceral artery and has a high risk of rupture, two-end
embolization (isolation technique) is used, which entails
embolization of the proximal and distal parent artery. In general,
this technique is associated with less serious complications such
as large-area organ necrosis and infection (31), and this was not observed among the
patients included in the present study. According to our
experience, if the GDA stump has a beak-like shape and the hepatic
artery is not damaged, no further treatment is required. However,
if the stump exhibits sac-like or bag-like structure, intervention
is required to prevent rupture regardless, of its length. If the
stump is long, the microcatheter may be inserted into the neck of
the sac. In this way, embolization with microcoils does not affect
the blood flow of the liver. If the stump is short or irregular,
isolation embolization or stent-assisted coil embolization should
be performed.
Embolization of VAPA may be technically challenging,
as the visceral artery is frequently small in caliber due to the
bleeding, decreased systemic blood pressure and the use of
vasoconstrictive drugs. This may be improved by hemodynamic
stabilization with volume replacement and discontinuation of
vasoconstrictive drugs. A large-diameter coil may then be selected
for embolization, as small-diameter coils used for embolization may
migrate to the efferent artery to cause rebleeding. In the present
study, distal coil migration occurred in one case. The present
experience conforms to the principle of 120-150, according to which
the ratio of the coil diameter to the diameter of the parent artery
or pseudoaneurysm should be at least 1.2-1.5, which is similar to
the ‘spaghetti technique’ (36).
For technical considerations of VAPA embolization,
it may be recommended to construct the coil with a low packing
density while ensuring it is stably located in the neck of the
pseudoaneurysm. According to certain scholars, a solid embolic
agent such as coils may increase the risk of aneurysmal rupture due
to the weak sac and damaged arterial wall, so that the sac packing
technique should be selected with caution (37), while other studies recommend the
sandwich technique or covered stent implantation for pseudoaneurysm
secondary to mechanically injured visceral arteries to avoid the
potential risk of massive bleeding during the procedure (38,39),
particularly among patients with pancreatic fistula after PD. In
recent years liquid embolic materials have been used for
pseudoaneurysms, but the risk of undesired ectopic embolization is
higher than that of a coil. The combined use of the two materials
may, however, bring a higher benefit (40,41).
There were certain limitations to the present study.
First, it was a retrospective, observational study with no
case-control cohort for comparative analysis to determine the true
effectiveness and safety of endovascular embolization over the
conventional surgical approach. In addition, the sample size was
relatively small due to the rarity of VAPA. Of note, the nature of
the patient's medical insurance, economical status and the
preference of family members are important factors that influence
the choice of treatment. Additionally, the majority of patients
prefer the conventional approach in China (19,31).
In conclusion, the present study indicated that
endovascular embolization is a safe and effective treatment for
pseudoaneurysm in the abdomen and pelvis. Several techniques of
embolization were presented and discussed. The endovascular
approach to VAPA should be considered as a preferred treatment
option in most cases.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed for the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HX and CJ made substantial contributions to the
conception and design of the present study and wrote the original
draft of the manuscript. JieZ, XM, JinZ, LY and YR were responsible
for the data acquisition, the analysis and the interpretation. HX
revised the manuscript critically for important intellectual
content. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethical
Committee of the Affiliated Hospital of North Sichuan Medical
College (Nanchong, China). Written informed consent was obtained
from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Luo J, Fu X, Zhou Y, Tang H, Song G, Tang
T, Liao X and Zhou X: Aortic remodeling following Sun's procedure
for acute Type A aortic dissection. Med Sci Monit. 23:2143–2150.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Nosher JL, Chung J, Brevetti LS, Graham AM
and Siegel RL: Visceral and renal artery aneurysms: A pictorial
essay on endovascular therapy. Radiographics. 26:1687–1704.
2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yekebas EF, Wolfram L, Cataldegirmen G,
Habermann CR, Bogoevski D, Koenig AM, Kaifi J, Schurr PG, Bubenheim
M, Nolte-Ernsting C, et al: Postpancreatectomy hemorrhage:
Diagnosis and treatment: An analysis in 1669 consecutive pancreatic
resections. Ann Surg. 246:269–280. 2007.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chen X, Yuan D, Zhao J, Huang B and Yang
Y: Hybrid repair for a complex infection aortic pseudoaneurysm with
continued antibiotic therapy: A case report and literature review.
Medicine (Baltimore). 98(e14330)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Madhusudhan KS, Venkatesh HA, Gamanagatti
S, Garg P and Srivastava DN: Interventional radiology in the
management of visceral artery pseudoaneurysms: A review of
techniques and embolic materials. Korean J Radiol. 17:351–363.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Martins A, Goncalves A, Passos P, Cardoso
M, Torres R, Almeida T and Midões A: Splenic artery pseudoaneurysm.
J Gastrointest Surg. 22:1297–1298. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rottoli M, Sabharwal T, Schizas AM and
George ML: Bleeding pseudoaneurysm of the internal iliac artery
after extended resection for advanced rectal cancer: Report of two
cases. Int J Colorectal Dis. 29:1585–1586. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Corvino A, Catalano O, de Magistris G,
Corvino F, Giurazza F, Raffaella N and Vallone G: Usefulness of
doppler techniques in the diagnosis of peripheral iatrogenic
pseudoaneurysms secondary to minimally invasive interventional and
surgical procedures: Imaging findings and diagnostic performance
study. J Ultrasound: May 20, 2020 doi: 10.1007/s40477-020-00475-6
(Epub ahead of print).
|
|
9
|
Li Y, Liang W, Zhang J and Peng R:
Association of difference in coronary sinus diameter by computed
tomographic angiography between patients in and not in stable
atherosclerotic plaque(S). Med Sci Monit. 24:3265–3273.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Keeling AN, McGrath FP and Lee MJ:
Interventional radiology in the diagnosis, management, and
follow-up of pseudoaneurysms. Cardiovasc Intervent Radiol. 32:2–18.
2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Saad NE, Saad WE, Davies MG, Waldman DL,
Fultz PJ and Rubens DJ: Pseudoaneurysms and the role of minimally
invasive techniques in their management. Radiographics. 25 (Suppl
1):S173–S189. 2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pitton MB, Dappa E, Jungmann F, Kloeckner
R, Schotten S, Wirth GM, Mittler J, Lang H, Mildenberger P,
Kreitner KF, et al: Visceral artery aneurysms: Incidence,
management, and outcome analysis in a tertiary care center over one
decade. Eur Radiol. 25:2004–2014. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Dohan A, Eveno C, Dautry R, Guerrache Y,
Camus M, Boudiaf M, Gayat E, Le Dref O, Sirol M and Soyer P: Role
and effectiveness of percutaneous arterial embolization in
hemodynamically unstable patients with ruptured splanchnic artery
pseudoaneurysms. Cardiovasc Intervent Radiol. 38:862–870.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Reiter DA, Fischman AM and Shy BD: Hepatic
artery pseudoaneurysm rupture: A case report and review of the
literature. J Emerg Med. 44:100–103. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Thaut L, Weymouth W, Hunsaker B and
Reschke D: Evluation of central venous access with accelerated
seldinger technique versus modified seldinger technique. J Emerg
Med. 56:23–28. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Angle JF, Siddiqi NH, Wallace MJ, Kundu S,
Stokes L, Wojak JC and Cardella JF: Society of Interventional
Radiology Standards of Practice Committee: Quality improvement
guidelines for percutaneous transcatheter embolization: Society of
Interventional Radiology Standards of Practice Committee. J Vasc
Interv Radiol. 21:1479–1486. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hassold N, Wolfschmidt F, Dierks A, Klein
I, Bley T and Kickuth R: Effectiveness and outcome of endovascular
therapy for late-onset postpancreatectomy hemorrhage using covered
stents and embolization. J Vas Surg. 64:1373–1383. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jabbour G, Al-Hassani A, El-Menyar A,
Abdelrahman H, Peralta R, Ellabib M, Al-Jogol H, Asim M and
Al-Thani H: Clinical and radiological presentations and management
of blunt splenic trauma: A single tertiary hospital experience. Med
Sci Monit. 23:3383–3392. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pan Z, Zhang H, Li L, Jia Y and Tian R:
Surgical treatment of traumatic lower limb pseudoaneurysm. Chin J
Traumatol. 17:285–288. 2014.PubMed/NCBI
|
|
20
|
Branchi V, Meyer C, Verrel F, Kania A,
Bölke E, Semaan A, Koscielny A, Kalff JC and Matthaei H: Visceral
artery aneurysms: Evolving interdisciplinary management and future
role of the abdominal surgeon. Eur J Med Res.
241(17)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gabelmann A, Gorich J and Merkle EM:
Endovascular treatment of visceral artery aneurysms. J Endovasc
Ther. 9:38–47. 2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Feng J, Chen YL, Dong JH, Chen MY, Cai SW
and Huang ZQ: Post-pancreaticoduodenectomy hemorrhage: Risk
factors, managements and outcomes. Hepatobiliary Pancreat Dis Int.
13:513–522. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dumitru R, Carbunaru A, Grasu M, Toma M,
Ionescu M and Dumitrascu T: Pseudoaneurysm of the splenic artery-an
uncommon cause of delayed hemorrhage after pancreaticoduodenectomy.
Ann Hepatobiliary Pancreat Surg. 20:204–210. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gao F, Li J, Quan S, Li F, Ma D, Yao L and
Zhang P: Risk factors and treatment for hemorrhage after
pancreaticoduodenectomy: A case series of 423 patients. Biomed Res
Int. 2016(2815693)2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Schafer M, Heinrich S, Pfammatter T and
Clavien PA: Management of delayed major visceral arterial bleeding
after pancreatic surgery. HPB (Oxford). 13:132–138. 2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jesinger RA, Thoreson AA and Lamba R:
Abdominal and pelvic aneurysms and pseudoaneurysms: Imaging review
with clinical, radiologic, and treatment correlation.
Radiographics. 33:E71–E96. 2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dohan A, Dautry R, Guerrache Y, Fargeaudou
Y, Boudiaf M, Le Dref O, Sirol M and Soyer P: Three-dimensional
MDCT angiography of splanchnic arteries: Pearls and pitfalls. Diagn
Interv Imaging. 96:187–200. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Balderi A, Antonietti A, Ferro L, Peano E,
Pedrazzini F, Fonio P and Grosso M: Endovascular treatment of
visceral artery aneurysms and pseudoaneurysms: Our experience.
Radiol Med. 117:815–830. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Vander Mijnsbrugge W, Laleman W, Van
Steenbergen W, Heye S, Verslype C and Maleux G: Long-term clinical
and radiological outcoome of endovascular embolization of
pancreatitis-related pseudoaneurysms. Acta Radiol. 58:316–322.
2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
You Y, Choi SH, Choi DW, Heo JS, Han IW,
Han S, Shin SW, Park KB, Park HS, Cho SK and Han SH: Long-term
clinical outcomes after endovascular management of ruptured
pseudoaneurysm in patients undergoing pancreaticoduodenectomy. Ann
Surg Treat Res. 96:237–249. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Xu H, Jing C, Zhou J, Min X, Zhao J, Yang
L and Ren Y: Clinical efficacy of coil embolization in treating
pseudoaneurysm post-Whipple operation. Exp Ther Med.
20(37)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhao Q, Xu H, Min X, Yang L and Ren Y:
Imaging features of vertebral aneurysmal bone cyst and the clinical
value of interventional embolization. Exp Ther Med. 20:3832–3836.
2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Liao X, Xu H, Liu F, Min X, Li Y, Yang L
and Ren Y: Value of angioembolization in the treatment of
iatrogenic renal vascular injury assisted by 3-dimensional digital
subtraction angiography. Med Sci Monit. 26(e927208)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Xu H, Min X, Li Y, Yang L and Ren Y: A
comparative study of conservation, endovascular embolization
therapy, and surgery for blunt renal trauma. Med Sci Monit.
26(e922802)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wang D, Su L, Han Y and Fan X:
Embolization treatment of pseudoaneurysms originating from the
external carotid artery. J Vasc Surg. 61:920–926. 2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Giurazza F, Corvino F, Cavaglià E,
Silvestre M, Cangiano G, Amodio F, De Magistris G and Niola R:
Emborrhoid in patients with portal hypertension and chronic
hemorrhoidal bleeding: Preliminary results in five cases with a new
coiling release fashion ‘Spaghetti technique’. Radiol Med.
125:1008–1011. 2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Sueyoshi E, Sakamoto I, Nakashima K,
Minami K and Hayashi K: Visceral and peripheral arterial
pseudoaneurysms. AJR Am J Roentgenol. 185:741–749. 2005.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Lwin TM, Leigh N, Iskandar ME, Steele JG,
Wayne MG and Cooperman AM: Rare, uncommon, and unusual
complications after pancreaticoduodenal resection. Surg Clin North
Am. 98:87–94. 2018.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Jesinger RA, Thoreson AA and Lamba R:
Abdominal and pelvic aneurysms and pseudoaneurysms: Imaging review
with clinical, radiologic, and treatment correlation.
Radiographics. 33:E71–E96. 2013.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Madhusudhan KS, Gamanagatti S, Garg P,
Shalimar Dash NR, Pal S, Peush S and Gupta AK: Endovascular
embolization of visceral artery pseudoaneurysms using modified
injection technique with N-Butyl cyanoacrylate glue. J Vasc Interv
Radiol. 26:1718–1725. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Leyon JJ, Littlehales T, Rangarajan B,
Hoey ET and Ganeshan A: Endovascular embolization: Review of
currently available embolization agents. Curr Probl Diagn Radiol.
43:35–53. 2014.PubMed/NCBI View Article : Google Scholar
|