Introduction
The most frequent cause of acromegaly is pituitary
hypersecretion of growth hormone (GH) (1). High levels of GH and insulin-like
growth factor-1 (IGF-1) result in systemic alterations such as
acral enlargement, skin thickening, soft tissue hyperplasia and
excessive sweating (1). Acromegaly
may also be associated with dyslipidemia, insulin resistance,
diabetes mellitus and cardiovascular events (1-3).
Previous reports have revealed increased overall mortality rates in
patients with acromegaly compared with the healthy control
population (4).
Acromegaly-associated physical alterations may not be detected by
the patients at the early stages of disease (5,6).
However, health professionals may also misdiagnose acromegaly in
patients exhibiting slow disease progression and limited symptoms
(1). As previously reported,
diagnostic error may notably impact therapeutic management,
prognosis and patient quality of life (7). Diagnostic error has also been the
cause of numerous lawsuits of medical malpractice (8). The present report outlines a case of
acromegaly that was undiagnosed for multiple years, which affected
the therapeutic management of the patient.
Case report
The case was a 44-year-old Japanese man referred to
the Department of Internal Medicine, Kuwana City Medical Center
(Kuwana, Mie, Japan) in October 2017 for severe hyperglycemia,
which was detected during a general workplace checkup. The patient
experienced mild hyperglycemia during a medical check-up five years
before admission, without subsequent medical follow-up. The
clinical findings during the examination were as follows: Height,
168 cm; body weight, 77 kg; body mass index, 27.3 kg/m2;
blood pressure, 110/64 mmHg; heart rate, 70 beats/min; and body
temperature, 36.9˚C. The laboratory data revealed a hemoglobin A1c
level of 15.8% and a random blood glucose level of 330 mg/dl
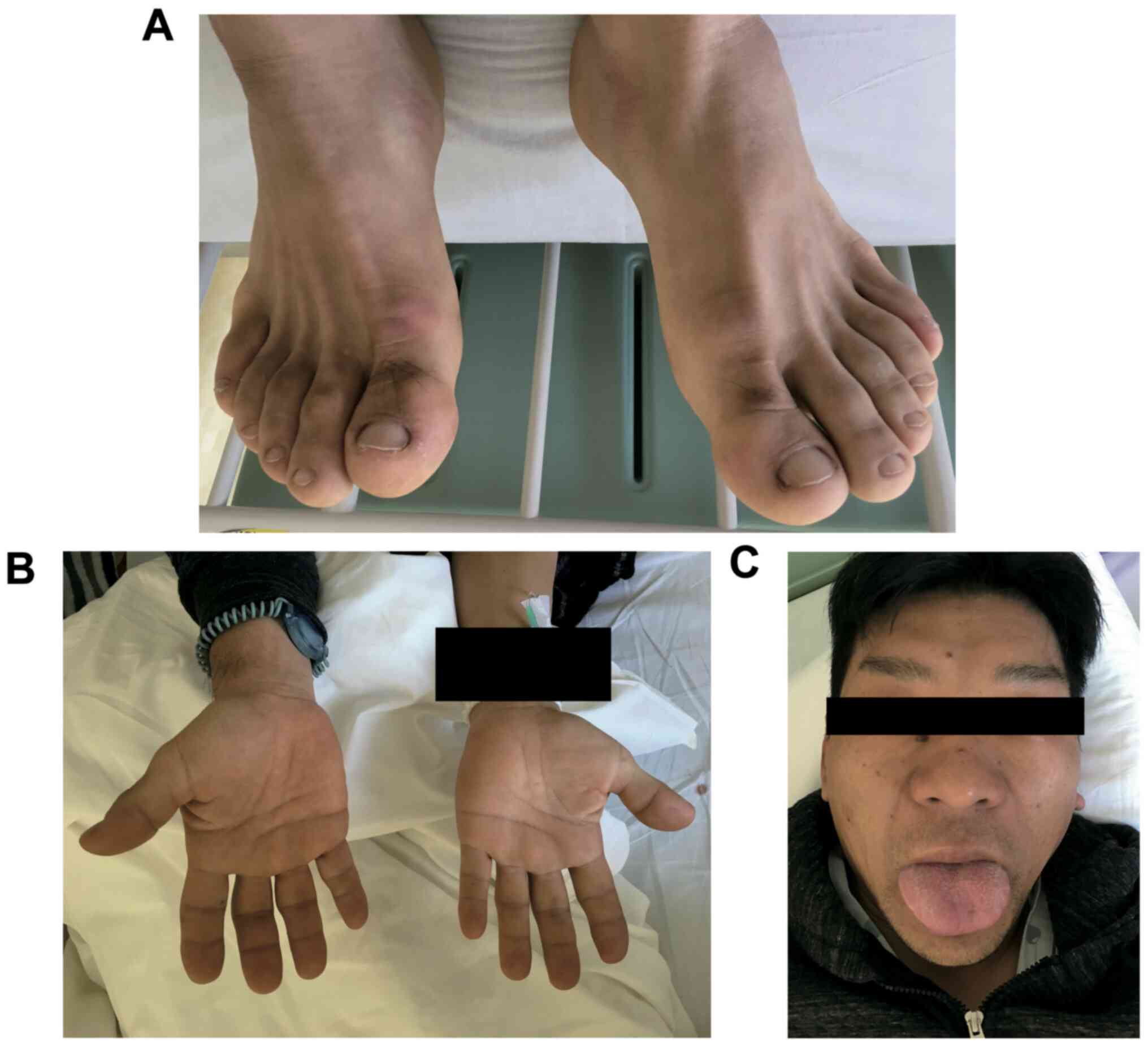
(Table I). A routine physical foot
examination for diabetic patients revealed enlargement of both feet
(Fig. 1A). The feet had no
pitting-edema and were not painful, red or warm. Additional
physical examination disclosed hyperhidrosis, jaw malocclusion,
prominent supraciliary arches and enlarged hands and tongue
(Fig. 1A-C). The patient was
transferred to the Department of Diabetes and Endocrinology of Mie
University Hospital (Tsu, Mie, Japan) as he was suspected of having
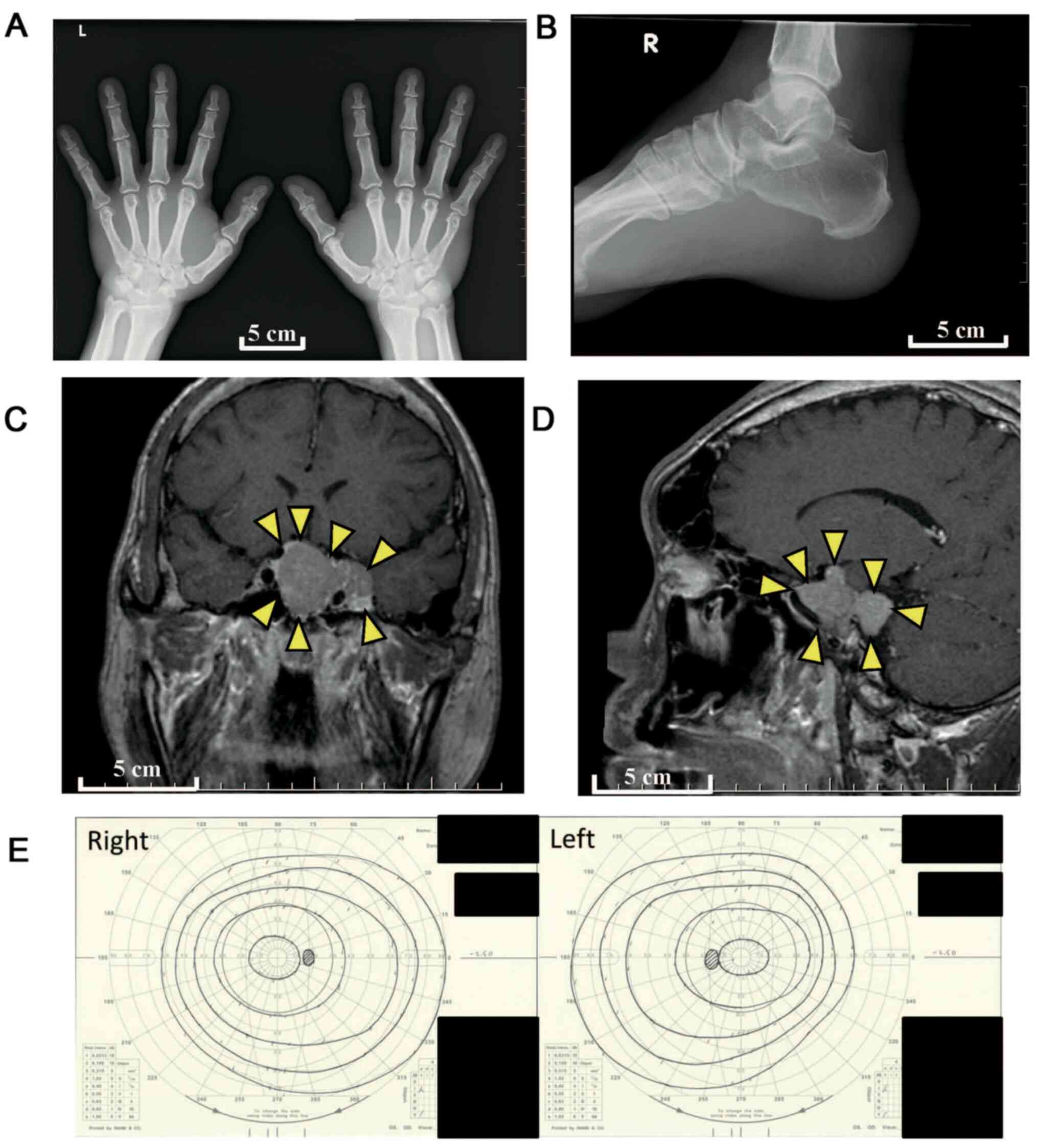
an endocrine disorder. A plain radiograph indicated hypertrophied
terminal phalangeal tufts and soft tissue hypertrophy (Fig. 2A) with heel pad thickness (Fig. 2B).
 | Table IEndocrine parameters. |
Table I
Endocrine parameters.
| Variable | Value | Reference range |
|---|
| GH, ng/ml | 870 | <1.0 |
| IGF-1, ng/ml | 582 | 92-255 |
| Random blood glucose,
mg/dl | 330 | <200 |
| HbA1c (%) | 15.8 | 4.9-6.0 |
| TSHa (µIU/ml) | 0.84 | 0.35-4.9 |
| Free T3a (pg/ml) | 1.80 | 1.7-3.7 |
| Free T4a (ng/dl) | 0.79 | 0.70-1.48 |
| LHa (mIU/ml) | 0.44 | 0.57-12.07 |
| FSHa (mIU/ml) | 2.11 | 0.95-11.95 |
| ACTHa (pg/ml) | 43.4 | 7.2-63.3 |
| Cortisola (µg/dl) | 8.3 | 4.5-21.1 |
| PRLa (ng/ml) | 5.9 | 3.6-12.8 |
| AVPa (pg/ml) | 1.7 | <2.8 |
| Serum
osmolalitya
(mOsm/kg/H2O) | 295 | 275-295 |
Table I describes
the results of endocrine parameter analysis. There was an increased
serum concentration of GH and IGF-I, and the serum level of
luteinizing hormone was low. However, the circulating levels of
adrenocorticotropic hormone, thyroid stimulation hormone,
follicle-stimulating hormone, free triiodothyronine, free thyroxine
and cortisol were within the normal range. The circulating levels
of prolactin and arginine vasopressin, as well as the serum
osmolality, were also within the normal range. As presented in
Table II, a luteinizing-hormone
releasing hormone test revealed that the levels of luteinizing
hormone and follicle-stimulating hormone were also normal (6). Magnetic resonance imaging (MRI)
revealed an enhanced pituitary tumor of 4.5 cm (Fig. 2C and D). Ophthalmic examinations revealed no
vision loss secondary to the pituitary tumor or diabetic
retinopathy (Fig. 2E). There were
no symptoms of Cushing's syndrome, and the overall results of the
corticotropin-releasing hormone stimulation test showed no
significant abnormality (Table II)
(9). A test for cortisol rhythm was
not performed.
 | Table IIResults of CRH and LHRH tests. |
Table II
Results of CRH and LHRH tests.
| | Time of
measurement |
|---|
| Variable | 0 min | 30 min | 60 min |
|---|
| CRH test |
|
ACTH,
pg/ml | 55.3 | 62.1 | 47.2 |
|
Cortisol,
µg/dl | 20.1 | 21.9 | 17.6 |
| LHRH test |
|
LH,
mIU/ml | 0.56 | 4.91 | 7.29 |
|
FSH,
mIU/ml | 2.65 | 4.37 | 5.48 |
The patient was diagnosed with acromegaly, type 2
diabetes mellitus and acromegaly-associated exacerbation of
diabetes mellitus. However, tumor removal will ultimately clarify
whether type 2 diabetes mellitus is only secondary to acromegaly.
Subsequent investigation disclosed the presence of sleep apnea,
colon polyps and thyroid enlargement; based on a previous report
(10). The summary of positive
clinical findings of acromegaly in the present case was as follows:
Pituitary gland tumor, acral enlargement, jaw malocclusion,
hyperhidrosis, colon polyps, left ventricular hypertrophy, sleep
apnea, diabetes mellitus, dyslipidemia and enlargement of tongue
and thyroid gland (10). In the
present case, the electrocardiogram demonstrated a first-degree
atrioventricular blockade (PR interval, 212 ms; reported normal
range, 120-200 ms) with no ST-segment changes (11). Echocardiography demonstrated a
left-ventricular ejection fraction of 55% (using the modified
Simpson method), diffuse mild left ventricular hypertrophy and mild
thickening of the mitral valve (12). The right and left ankle-brachial
indexes were 1.19 and 1.22 (reported normal range, 0.9-1.3),
respectively (13). Carotid
ultrasonography revealed no atherosclerotic changes. Based on
previous studies (11-13),
an expert (Dr K.S). from the Department of Cardiovascular Medicine
(Mie University), recommended no further therapy for these mild
cardiovascular changes.
The tumor was unresectable due to excessive
enlargement and cavernous sinus invasion. Treatment with
somatostatin receptor ligands (SRLs; lanreotide and pasireotide)
were recommended, as these compounds can potentially reduce tumor
size (14,15). As such, SRLs are the first treatment
choice for patients with acromegaly (16). Lanreotide has a high affinity for
both somatostatin receptor (SSTR) 2 and SSTR5, and a weak affinity
for SSTR3(16). Pasireotide is able
to bind multiple SSTRs (SSTR1, 3, 5 and 2) and with a greater
affinity than lanreotide (16).
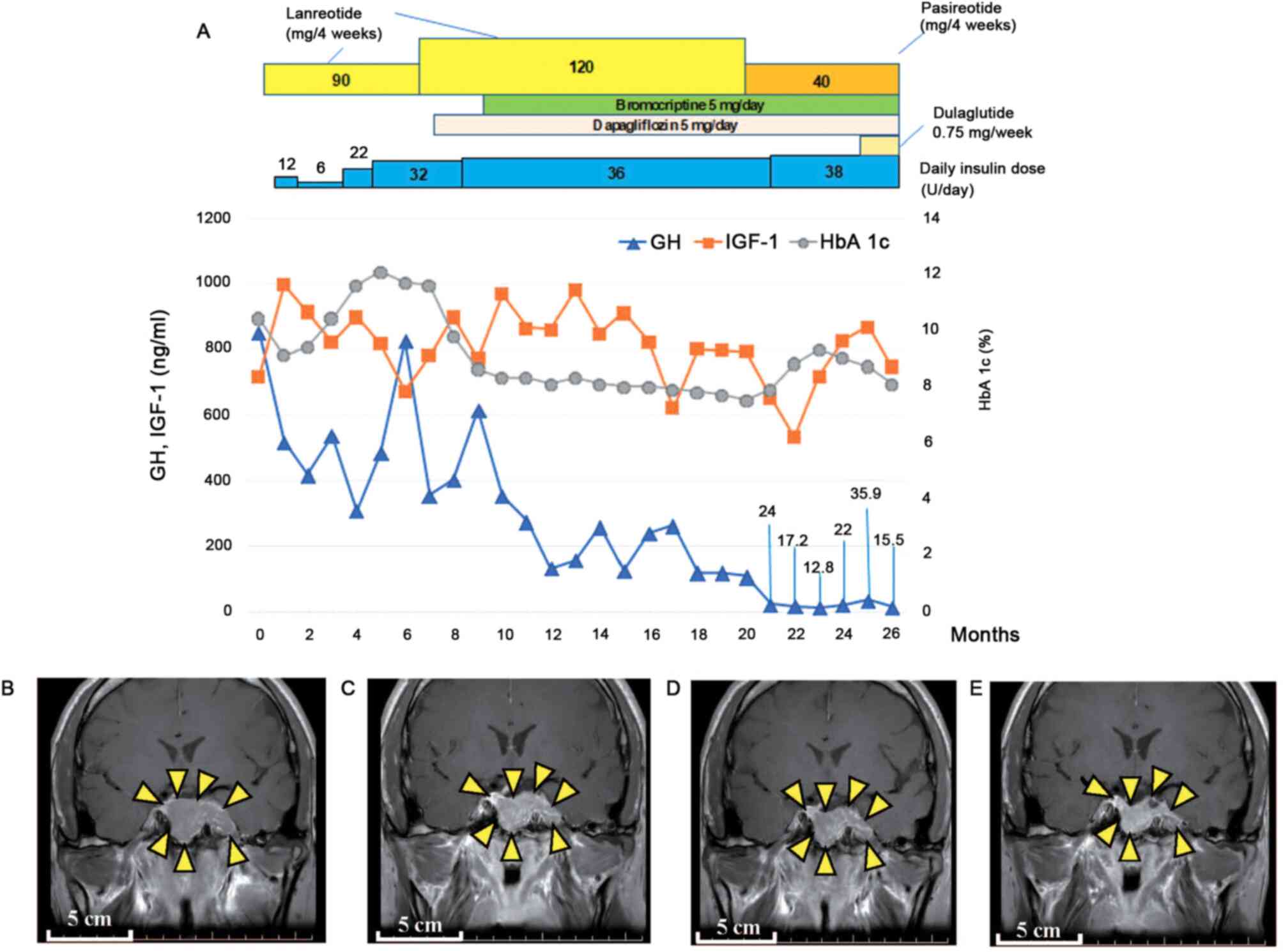
Initially, the use of lanreotide (90 or 120 mg) was indicated every
4 weeks. In addition to diet and exercise therapy, hypoglycemic
agents are the first treatment of choice for those with type 2
diabetes mellitus (17). However,
the blood glucose level of the current case was >300 mg/dl on
admission, and the patient was therefore treated with insulin
according to previous clinical guidelines (17). During follow-up and five months
after starting therapy with lanreotide, laboratory data revealed
decreased circulating levels of GH with increasing doses of
lanreotide (Fig. 3A), and a MRI
study demonstrated a reduction in tumor size (Fig. 3B-E). A previous study reported that
serum GH levels of >10 ng/ml were not correlated with serum
IGF-1 levels (18). This may
explain the persistently high levels of IGF-1, despite the
decreased levels of GH, observed in the present case (Fig. 3A). During follow-up, no therapeutic
response to lanreotide was observed. Therefore, the patient was
subsequently treated with pasireotide (40 mg every 4 weeks), in
additional to 5 mg bromocriptine per day. Bromocriptine is a
dopamine agonist that suppresses GH secretion by binding to the D2
receptor in the pituitary tumor (16). International consensus statement
also recommend the use of cabergoline, a dopamine agonist (14). However, the Japanese Health
Insurance System does not cover cabergoline, and therefore,
bromocriptine was indicated in the present case (19). A previous report demonstrated the
beneficial effects of bromocriptine in acromegaly-associated
glucose abnormalities (16). Due to
the large size of the tumor and the high levels of circulating of
IGF-1, no surgical procedures were indicated at the time of the
present report. Tumor debulking surgery will be indicated after
appropriate tumor shrinkage.
Discussion
Acromegaly may reduce the life expectancy of
individuals. Metabolic disorders associated with acromegaly
accelerate arteriosclerosis and increase the risk of cardiovascular
events (20). The first therapeutic
option for acromegaly is surgical resection of the pituitary
adenoma, although surgery is not feasible in patients with large
tumors (6). Patients with
unresectable tumors receive treatment with SRLs and GH receptor
antagonists (20). However, the
lack of an international consensus for the duration of therapy, the
high economic burden for the patient and the potential adverse
effects associated with the prolonged use of specific SRLs, make
the routine indication of these drugs difficult in clinical
practice (21). Therefore, the
early diagnosis of acromegaly is imperative to successful
treatment. However, subtle progressive physical alterations may go
unnoticed by patients and attending physicians, leading to delayed
or missed diagnoses with detrimental implications for patient care
(22). Current clinical guidelines
describe the importance of a thorough foot examination for the
diagnosis of acromegaly (23);
however, available guidelines lack a detailed description of the
clinical disease presentations in the presence of comorbidities
(such as diabetes mellitus) (23).
The present case indicated that, in addition to diabetic foot,
acral abnormalities (such as enlarged feet) should also be assessed
during the routine examination of patients with untreated diabetes
mellitus. The present report is an illustrative case of missed
diagnosis of acromegaly that negatively affected medical treatment.
Due to a missed diagnosis of acromegaly at the early stages (during
routine medical check-ups over numerous years), the patient could
not undergo debulking surgery of the pituitary tumor. Therefore,
this case also underscores the critical importance of early
diagnosis for the management of patients with acromegaly.
Another point that could have prevented a missed
diagnosis in the present case is the detection of hyperglycemia.
Diabetes mellitus is a metabolic disorder that may be associated
with acromegaly (20). A cohort
study in a Mexican population revealed that, among patients with
acromegaly, the incidence of diabetes mellitus appeared to be
higher in women than in men (16).
However, epidemiological data from other geographical areas
revealed no differences between the sexes (4,24-28).
Clinical suspicion of acromegaly is generally difficult during
anamnesis of patients with diabetes mellitus, particularly in the
absence of disease-related symptomatology. However, following
routine checkpoints may prevent patients and practitioners from
overlooking the signs of acromegaly. The American Diabetes
Association recommends a comprehensive and routine foot examination
during the initial visits of all diabetic patients (29,30).
In addition to evaluating the presence of diabetic foot, peripheral
artery disease or diabetic neuropathy, careful foot examination may
also provide hints for the early diagnosis of acromegaly. In the
present case, laboratory data during the medical check-up disclosed
hyperglycemia that was indicative of diabetes mellitus. Failure to
examine the foot of the patient, despite the suspicion of diabetes
mellitus, was another contributing factor for the missed diagnosis
of acromegaly. In the present case, improvement of glucose
metabolism after surgical treatment may demonstrate that acromegaly
was the cause of hyperglycemia (16). The patient is currently under
clinical follow-up, and will undergo surgery when the tumor becomes
operable.
Diagnostic error is a frequent cause of patient harm
and adverse events in hospital practice and outpatient care
(31,32). In 2015, the National Academy of
Medicine stated that most individuals ‘will experience at least one
diagnostic error in their lifetime, sometimes with devastating
consequences’ (33-35).
There are different types of diagnostic errors, such as the wrong
diagnosis (misdiagnosis), failure to diagnose (missed diagnosis)
and delayed diagnosis (32).
Diagnostic errors may be detrimental to patient health, resulting
in delayed or inappropriate therapy or diagnostic procedures
(32,33). The current report is a typical case
of acromegaly where, due to missed diagnosis over a number of
years, the most appropriate treatment was not received.
The present report outlines a case of missed
diagnosis of acromegaly associated with severe hyperglycemia. After
10 years of missed diagnosis, the associated pituitary tumor became
inoperable due to invasive growth into the adjacent tissue. This
case highlights the importance of hyperglycemia and abnormal feet
in acromegaly. In addition, the case underscores the requirement
for a careful examination of the feet of diabetic patients, and the
critical importance of early diagnosis of acromegaly to prevent
devastating consequences for patient care.
Acknowledgements
The authors would like to thank Dr Kei Sato from the
Department of Cardiology, Mie University Hospital, for his clinical
assistance in this case.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KN was responsible for clinical treatment, follow-up
in Kuwana City Medical Center and Mie University Hospital and
preparation of the first draft of the manuscript. YY, TY and ECG
contributed to the interpretation of the data and made intellectual
contributions for the preparation of the manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of clinical details and images.
Competing interests
The authors declare that they have no competing of
interests.
References
|
1
|
Colao A, Grasso LFS, Giustina A, Melmed S,
Chanson P, Pereira AM and Pivonello R: Acromegaly. Nat Rev Dis
Primers. 5(20)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Espinosa-de-los-Monteros AL, González B,
Vargas G, Sosa E and Mercado M: Clinical and biochemical
characteristics of acromegalic patients with different
abnormalities in glucose metabolism. Pituitary. 14:231–235.
2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
González B, Vargas G, de Los Monteros ALE,
Mendoza V and Mercado M: Persistence of diabetes and hypertension
after multimodal treatment of acromegaly. J Clin Endocrinol Metab.
103:2369–2375. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Dal J, Feldt-Rasmussen U, Andersen M,
Kristensen LØ, Laurberg P, Pedersen L, Dekkers OM, Sørensen HT and
Jørgensen JO: Acromegaly incidence, prevalence, complications and
long-term prognosis: A nationwide cohort study. Eur J Endocrinol.
175:181–190. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Caron P, Brue T, Raverot G, Tabarin A,
Cailleux A, Delemer B, Renoult PP, Houchard A, Elaraki F and
Chanson P: Signs and symptoms of acromegaly at diagnosis: The
physician's and the patient's perspectives in the ACRO-POLIS study.
Endocrine. 63:120–129. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Melmed S, Kleinberg D and Ho K: Pituitary
physiology and diagnostic evaluation. In: Williams Textbook of
Endocrinology. Melmed S (ed). Elsevier Saunders, Philadelphia, PA,
pp175-228, 2011.
|
|
7
|
Kalra J: Medical errors: An introduction
to concepts. Clin Biochem. 37:1043–1051. 2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Oyebode F: Clinical errors and medical
negligence. Med Princ Pract. 22:323–333. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kageyama K, Oki Y, Sakihara S, Nigawara T,
Terui K and Suda T: Evaluation of the diagnostic criteria for
Cushing's disease in Japan. Endocr J. 60:127–135. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Melmed S: Medical progress: Acromegaly. N
Engl J Med. 355:2558–2573. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kashou AH, Goyal A, Nguyen T and Chhabra
L: Atrioventricular Block. StatPearls, Treasure Island, FL,
2020.
|
|
12
|
Zemaitis MR, Boll JM and Dreyer MA:
Peripheral arterial disease. StatPearls, Treasure Island, FL,
2020.
|
|
13
|
Colao A, Auriemma RS, Galdiero M, Lombardi
G and Pivonello R: Effects of initial therapy for five years with
somatostatin analogs for acromegaly on growth hormone and
insulin-like growth factor-I levels, tumor shrinkage, and
cardiovascular disease: A prospective study. J Clin Endocrinol
Metab. 94:3746–3756. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Melmed S, Bronstein MD, Chanson P,
Klibanski A, Casanueva FF, Wass JAH, Strasburger CJ, Luger A,
Clemmons DR and Giustina A: A consensus statement on acromegaly
therapeutic outcomes. Nat Rev Endocrinol. 14:552–561.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zahr R and Fleseriu M: Updates in
diagnosis and treatment of acromegaly. Eur Endocrinol. 14:57–61.
2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ferrau F, Albani A, Ciresi A, Giordano C
and Cannavo S: Diabetes secondary to acromegaly: Physiopathology,
clinical features and effects of treatment. Front Endocrinol
(Lausanne). 9(358)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Haneda M, Noda M, Origasa H, Noto H, Yabe
D, Fujita Y, Goto A, Kondo T and Araki E: Japanese clinical
practice guideline for diabetes 2016. Diabetol Int. 9:1–45.
2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Oldfield EH, Jane JA Jr, Thorner MO,
Pledger CL, Sheehan JP and Vance ML: Correlation between GH and
IGF-1 during treatment for acromegaly. J Neurosurg. 126:1959–1966.
2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Matsubayashi K and Kawakami K: Prevalence,
incidence, comorbidities, and treatment patterns among Japanese
patients with acromegaly: A descriptive study using a nationwide
claims database. Endocr J: Jun 10, 2020 (Online ahead of
print).
|
|
20
|
Gadelha MR, Kasuki L, Lim DST and Fleseriu
M: Systemic complications of acromegaly and the impact of the
current treatment landscape: An update. Endocr Rev. 40:268–332.
2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kasuki L, Wildemberg LE and Gadelha MR:
MANAGEMENT OF ENDOCRINE DISEASE: Personalized medicine in the
treatment of acromegaly. Eur J Endocrinol. 178:R89–R100.
2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Graber ML: The incidence of diagnostic
error in medicine. BMJ Qual Saf. 22 (Suppl 2):ii21–ii27.
2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Katznelson L, Laws ER Jr, Melmed S,
Molitch ME, Murad MH, Utz A and Wass JA: Endocrine Society:
Acromegaly: An endocrine society clinical practice guideline. J
Clin Endocrinol Metab. 99:3933–3951. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Schöfl C, Franz H, Grussendorf M, Honegger
J, Jaursch-Hancke C, Mayr B and Schopohl J: participants of the
German Acromegaly Register: Long-term outcome in patients with
acromegaly: Analysis of 1344 patients from the German Acromegaly
Register. Eur J Endocrinol. 168:39–47. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mestron A, Webb SM, Astorga R, Benito P,
Catala M, Gaztambide S, Gomez JM, Halperin I, Lucas-Morante T,
Moreno B, et al: Epidemiology, clinical characteristics, outcome,
morbidity and mortality in acromegaly based on the Spanish
Acromegaly Registry (Registro Espanol de Acromegalia, REA). Eur J
Endocrinol. 151:439–446. 2004.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Fieffe S, Morange I, Petrossians P,
Chanson P, Rohmer V, Cortet C, Borson-Chazot F, Brue T and Delemer
B: French Acromegaly Registry: Diabetes in acromegaly, prevalence,
risk factors, and evolution: Data from the French Acromegaly
Registry. Eur J Endocrinol. 164:877–884. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Bex M, Abs R, T'Sjoen G, Mockel J,
Velkeniers B, Muermans K and Maiter D: AcroBel-the Belgian registry
on acromegaly: A survey of the ‘real-life’ outcome in 418
acromegalic subjects. Eur J Endocrinol. 157:399–409.
2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Arosio M, Reimondo G, Malchiodi E,
Berchialla P, Borraccino A, De Marinis L, Pivonello R, Grottoli S,
Losa M, Cannavò S, et al: Predictors of morbidity and mortality in
acromegaly: An Italian survey. Eur J Endocrinol. 167:189–198.
2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
American Diabetes Association: 4.
Comprehensive Medical Evaluation and Assessment of Comorbidities:
Standards of Medical Care in Diabetes-2019. Diabetes Care 42 (Suppl
1): S34-S45, 2019.
|
|
30
|
American Diabetes Association: 4.
Comprehensive Medical Evaluation and Assessment of Comorbidities:
Standards of Medical Care in Diabetes-2020. Diabetes Care 43 (Suppl
1): S37-S47, 2020.
|
|
31
|
Neale G, Hogan H and Sevdalis N:
Misdiagnosis: Analysis based on case record review with proposals
aimed to improve diagnostic processes. Clin Med (Lond). 11:317–321.
2011.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Singh H and Graber ML: Improving diagnosis
in health care-the next imperative for patient safety. N Engl J
Med. 373:2493–2495. 2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ball JR and Balogh E: Improving diagnosis
in health care: Highlights of a report from the National Academies
of Sciences, Engineering, and Medicine. Ann Intern Med. 164:59–61.
2016.PubMed/NCBI View
Article : Google Scholar
|
|
34
|
Committee on Diagnostic Error in Health
Care, Board on Health Care Services, Institute of Medicine, The
National Academies of Sciences, Engineering, and Medicine:
Improving diagnosis in health care. Balogh EP, Miller BT and Ball
JR (eds). National Academies Press (US), Washington, DC, 2015.
|
|
35
|
Mane KK, Rubenstein KB, Nassery N, Sharp
AL, Shamim EA, Sangha NS, Hassoon A, Fanai M, Wang Z and
Newman-Toker DE: Diagnostic performance dashboards: Tracking
diagnostic errors using big data. BMJ Qual Saf. 27:567–570.
2018.PubMed/NCBI View Article : Google Scholar
|