Introduction
Total knee arthroplasty (TKA), a strategy used to
treat multiple advanced knee diseases, has been widely reported to
significantly improve knee function and patient quality of life
(1). Valgus knee is the condition
which leads to the requirement for TKA (2) and is often associated with lateral
condylar hypoplasia, lateral tibial plateau defect, contracture of
the lateral ligament complex of the knee joint and patellar locus
defects, all of which cause severe dysfunction and seriously affect
patients' quality of life (3). The
main goal of TKA in the treatment of valgus knee is to correct
valgus deformity, restore the balance of the flexion and extension
gap and ultimately restore joint function (1-3).
Surgical field exposure and soft tissue release play
crucial roles in the treatment of valgus knee. The choice of
operative approach determines the exposure of the surgical field,
and the main approaches to valgus knee surgery include the medial
parapatellar approach and the lateral parapatellar approach
(4). Soft tissue release mainly
refers to the release of lateral tense structures, including the
iliotibial band (ITB), lateral collateral ligament (LCL), popliteus
tendon (POP), posterolateral capsule (PLC) and lateral patellar
retinaculum (5). However, the best
choice of surgical approach and the best mode and order of soft
tissue release remains unknown (6).
Therefore, the aim of the present study was to investigate the
clinical efficacy of a lateral parapatellar approach with ITB
dissection from the Gerdy tubercle for TKA in the valgus knee.
Materials and methods
Clinical data
The present study is a retrospective analysis of all
patients that underwent TKA via a lateral parapatellar approach
with ITB dissection from the Gerdy tubercle for valgus knee between
January 2014 and May 2018 at the Second Affiliated Hospital of
Anhui Medical University and the Lu'an Affiliated Hospital of Anhui
Medical University. The inclusion criteria were: i) Patients
primarily underwent TKA; and ii) patients were followed up for more
than one year. The exclusion criteria were: i) Patients with
additional diseases (e.g. spinal or hip diseases) that may affect
the clinical efficacy of TKA; and ii) patients lost to
follow-up.
In total 56 patients (25 males and 31 females) were
included in the present study, and all patients signed written
informed consent for the surgery and use of their data at the time
of the study. The patients ranged in age from 55 to 72 years, with
a mean age of 62 years. There were 23 cases of rheumatoid
arthritis, 22 cases of osteoarthritis and 11 cases of traumatic
arthritis. The clinical valgus deformity ranged from 10˚ to 35˚
(mean 21.4˚) and the deformity was mild (<15˚) in 23 knees,
moderate (16˚-30˚) in 28 knees and severe (>30˚) in five knees
based on Keblish grade (6). The
following indicators were reviewed and analyzed: i) Operation
duration; ii) straight leg raising time (The time the leg was
raised after the operation); iii) correction angle of valgus
deformity; iv) the hip-knee-ankle angle (HKA angle); v) the frontal
femoral component angle (FFC angle); vi) the frontal tibial
component angle (FTC angle); vii) visual analogue score for pain
(VAS) (7); viii) range of movement
(ROM) (8) and ix) Knee Society
Score (KSS) (9). The HKA angle was
used to assess the lower limb force line and the FFC and FTC angles
were used to assess the prosthetic position. The ideal values of
the HKA, FFC, and FTC were 180˚, 96˚ and 90˚, respectively
(8). In addition, prosthetic
position deviation and limb alignment deviation within 5˚ were
considered to be within an acceptable range (8).
Main procedures of the lateral
parapatellar approach with ITB dissection from the Gerdy tubercle
for TKA
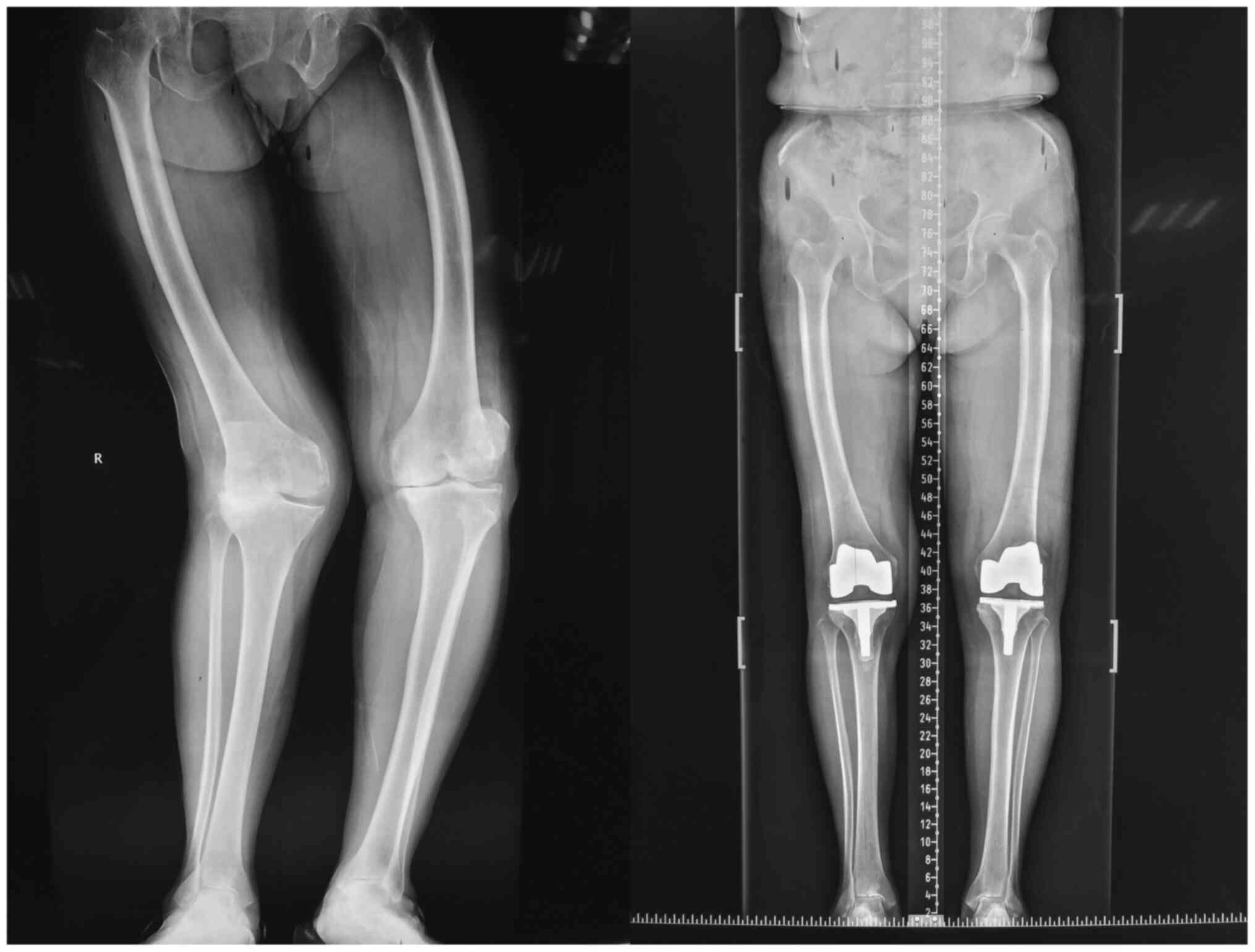
To ensure the successful completion of the
operation, all patients underwent full-length X-ray of their lower
limbs, anteroposterior and lateral X-ray of the knee and other
routine preoperative examinations of the circulatory system, heart
function, lung function and nervous system. All patients received
general anesthesia and femoral nerve block anesthesia, and a
tourniquet was used for every patient. All the operations were
performed by a skilled joint surgeon. An anterior midline
longitudinal incision approximately 12-14 cm across the knee was
performed from the proximal side of the patella to the lateral side
of the tibial tubercle. Skin, subcutaneous tissue and aponeurotic
fascia were cut in turn and then were sharply separated in an
outward direction. The lateral joint capsule and lateral
retinaculum were cut along the lateral margin of the rectus femoris
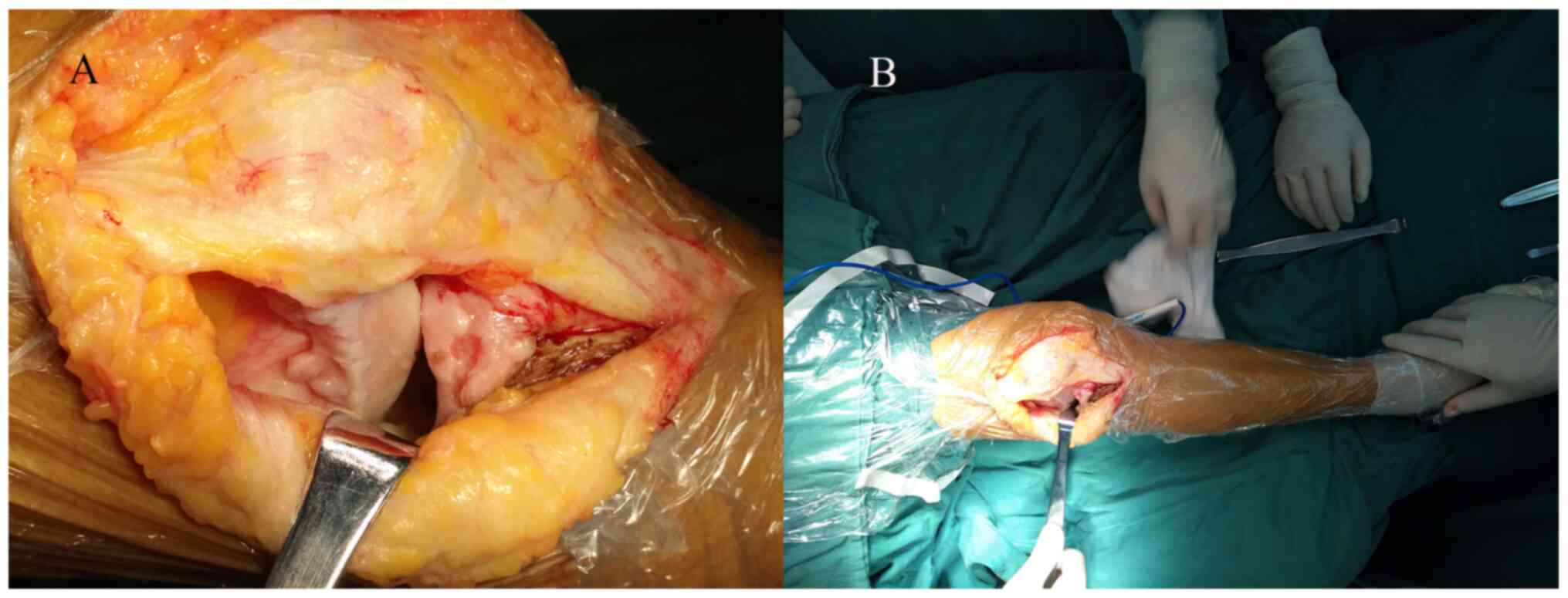
and the lateral margin of the patella to the Gerdy tubercle. The
ITB was completely dissected from the Gerdy tubercle and the knee
joint was fully exposed through patellar varus and partial removal
of the fat pad. After complete dissection of the ITB from the Gerdy
tubercle and removal of lateral osteophytes, it was indicated that
the majority of patients with straight valgus deformity are
corrected and the lower limb force line returns to normal. For most
patients, the valgus deformity could be corrected without further
release of additional lateral structures (Fig. 1).
After further release of the lateral collateral
ligament and posterior lateral articular capsule, soft tissue
balancing was performed and it was determined that the medial
structure was still relaxed, indicating that severe medial
structural relaxation was present. Therefore, simply releasing the
lateral structure is insufficient to obtain a good soft tissue
balance. Additional tightening reinforcement of the medial
collateral ligament and the use of a semi-restricted gasket (Smith
& Nephew plc) are required (5,6).
Therefore, reinforced sutures and semi-restricted gasket were used
for patients with severe medial collateral ligament relaxation,
while for other patients, PS (Posterior-stabilized) prostheses
(Smith & Nephew plc) were used. For patients with poor patellar
locus, the lateral joint capsule and lateral retinaculum were cut
along the lateral margin of the patella in a ‘Z’ shape, which
enabled final suture and closure of the articular capsule using a
staggered suture (Fig. 2). Then,
the stability, flexion and extension, and the force line of the
lower limb were checked. In addition, the patella locus and
internal and external stress were checked. Finally, the knee was
sutured layer by layer. Postoperative X-ray examination showed a
satisfactory lower limb force line and prosthesis position
(Fig. 3).
No patient received blood transfusion. All patients
received cefotiam to prevent infection and rivaroxaban to prevent
thrombosis. All patients underwent the same rehabilitation exercise
program including passive and active flexion and extension of the
knee, leg raising training, and walking with walking aids.
Statistical analysis
All data are shown as the mean ± standard deviation
followed by the median (in parentheses). Statistical analysis was
performed using SPSS 23.0 (IBM Corp.). One-way ANOVA followed by
Student-Newman-Keuls post hoc test was used for the comparison of
multiple groups.
Results
All patients were followed up for a minimum of one
year. The mean operation duration was 110.6±19.7 min and the mean
straight leg raising time was 3.1±1.0 days. The valgus deformity
was corrected from a mean of 21.4˚ before surgery to a mean of 2.6˚
after surgery. The mean VAS at 6 and 12 months after operation were
1.2 and 0.6, respectively, which was a significant improvement
compared with 4.8 preoperatively (both *P<0.05 vs.
pre-operatively; Table I). The mean
ROMs at 6 and 12 months after operation were 114 and 129,
respectively, which was significantly improved compared with 102
preoperatively (both *P<0.05 vs. pre-operatively;
Table I). The mean KSS knee scores
at 6 and 12 months after the operation were 82.5 and 92.3,
respectively, which was significantly improved compared with 52.0
preoperatively (both *P<0.05 vs. pre-operatively;
Table I). The mean KSS functional
scores at 6 and 12 months after operation were 78.4 and 84.3,
respectively, which was significantly improved compared with 41.1
preoperatively (both *P<0.05 vs. pre-operatively;
Table I). The mean HKA, FFC and FTC
angles after operation were 177.4˚, 95.4˚ and 89.7˚, respectively,
with no HKA, FFC or FTC angle deviation over 5˚ (Table II).
 | Table IPre-operative and postoperative
clinical results. |
Table I
Pre-operative and postoperative
clinical results.
| Measurement | Pre-operation | 6 months | 12 months |
|---|
| VAS | 4.8±0.72 (5.0) | 1.2±0.33a (1.0) | 0.6±0.28a (0.5) |
| ROM | 102±10.25(105) | 114±4.85a (115) | 129±4.37a (130) |
| KSS | | | |
|
Knee
score | 52.0±3.12 (52.0) |
82.5±2.89a
(83.0) |
92.3±4.13a
(95.0) |
|
Functional
score | 41.1±4.85 (40.0) |
78.4±8.12a
(80.0) |
84.3±5.13a
(85.0) |
 | Table IIProsthetic position deviation and limb
alignment results. |
Table II
Prosthetic position deviation and limb
alignment results.
| | Post-operation | Deviation over 5˚
(n) |
|---|
| HKA angle (˚) | 177.4±2.01
(178.2) | 0 |
| FFC angle (˚) | 95.4±1.40 (96.1) | 0 |
| FTC angle (˚) | 89.7±1.15 (88.9) | 0 |
In total, 5 patients with severe valgus deformity
underwent further release of the lateral collateral ligament and
posterior lateral articular capsule. An additional 2 patients with
severe medial collateral ligament relaxation were treated with
reinforced sutures and semi-restricted gasket. A single patient
with avulsion of the patellar ligament during the operation
recovered well after drilling and suture fixation, and no obvious
complications ensued. No patient underwent tibial nodule osteotomy,
which is used to fully expose the knee joint. There were no
instances of common peroneal nerve injury, patellar necrosis, or
poor patellar locus. All patients had good knee stability. Until
the last follow-up, no other complications were found in any of the
patients. In addition, 20 of the patients were followed up for more
than two years, but there was no significant difference in the
indicators in these patients at two years after operation compared
with at one year after operation (data not shown).
Discussion
The main finding of this study is that the lateral
parapatellar approach with ITB dissection from the Gerdy tubercle
for TKA can be used as an effective technique to treat valgus knee,
significantly improving pain and function without deviation of the
lower limb mechanical axis or prosthesis position. The factors
causing knee joint valgus deformity can be divided into bone tissue
factors and soft tissue factors (10). Bone tissue factors include lateral
cartilage erosion, lateral condylar hypoplasia, and metaphyseal
femoral and tibial plateau remodeling, while soft tissue factors
mainly refer to the lateral tense structures including the ITB,
LCL, PLC, POP, and hamstring tendons. Therefore, soft tissue
release and osteotomy are the top priority in total valgus knee
arthroplasty, especially soft tissue release. In addition, the
choice of operative approach and the method of soft tissue release
are still controversial and challenging (5,6). The
purpose of the present study was to explore the operative approach
and the release of soft tissue for TKA of the valgus knee.
At present, the operative approaches to valgus knee
are largely divided into the medial parapatellar approach and the
lateral parapatellar approach (4).
The medial parapatellar approach, as a widely used approach for
TKA, can provide sufficient surgical field exposure and is
convenient when performing surgical procedures because of the
outside location of the lower tubercles of the tibia, rendering
patella eversion easier (11).
Additionally, Ranawat et al (12) reported that the medial parapatellar
approach can reduce the incidence of postoperative skin infection,
necrosis and other complications and avoid lateral structural
spasms caused by sutures during lateral approach suturing. However,
the medial parapatellar approach also has its drawbacks. It is
difficult to release lateral tension structures directly,
especially in the posterolateral region, and the medial approach
may result in injury to the common peroneal nerve without direct
protection (12-14).
In addition, the medial parapatellar approach can also result in
damage to the blood supply inside the patella and thus increase the
risk of patellar necrosis because of the better blood supply of the
medial patellar flap compared with the lateral side (13,14).
Especially for patients with external patellar dislocation, in
order to obtain a good patellar locus, it is necessary to further
release the lateral patellar retinaculum, which can cause
additional damage to the blood supply of the patella and lead to
ischemic necrosis of the patella (13,14).
The greatest advantage of the lateral parapatellar approach in the
treatment of valgus knee is the ability to reach and release the
tense lateral soft tissues directly, with little damage to the
medial femoral muscle. Other advantages include a quick recovery
after operation (15) and the
avoidance of damage to the blood vessels around the patella
(16). Because the lateral patellar
retinaculum is cut directly during the surgery, the patellar locus
remains good after operation (13,14).
It has been reported that the main disadvantages of the lateral
patellar approach are the difficulty of patellar varus and the
difficulty of incision closure (17). However, the difficulty of incision
closure can be solved by using a ‘Z’ shape incision and dislocation
suture and the difficulty of patellar varus can be solved by tibial
tubercle osteotomy (17). In the
present study, only two patients had difficulty with patellar varus
due to complete exfoliation of the ITB, but the operation was not
affected. In addition, in the present study, there were no
incision-related complications and no tibial tubercle osteotomy was
required during operation. Avulsion of the patellar ligament
occurred in one patient during the operation, which may have been
caused by osteoporosis, but intraoperative traction cannot be
excluded. After drilling and suture fixation, the patient recovered
well and no obvious complications ensued. In summary, the present
data suggest that the lateral parapatellar approach can be used to
treat valgus knee and that the difficulties of incision closure and
patellar varus can be overcome by employing a ‘Z’ shaped incision
and dislocation suture.
Soft tissue release is not only an important step in
treatment of the valgus knee, but also a technical problem.
Controversies remain concerning the best method and sequence of
release of the lateral tense structures. The lateral tense
structures mainly include the ITB, LCL, PLC, and POP. The valgus
knee is generally divided into two types: Extension deformity
without concurrent flexion deformity, and extension deformity
complicated by flexion deformity. Most valgus deformities occur
during knee extension and there is no valgus deformity during
flexion. In addition, the ITB mainly affects valgus deformity in
knee extension, while the LCL, PLC and POP can affect valgus
deformity in both knee extension and knee flexion (5,6).
Krackow and Mihalko (18) suggested
that the ITB and LCL were the tensest lateral structures in the
valgus knee, such that the LCL should be considered first for
release and that the POP and ITB should be used to grade the
release when there is severe valgus deformity. Additionally, the
PLC is occasionally released and the lateral head of the
gastrocnemius is released only during flexion contracture. Aglietti
et al (19) carefully
performed the release of lateral tense structures using the
‘pie-crusting’ technique with small, multiple inside-out incisions
using a small knife blade (with a size of 15#). The POP was first
released, and then the LCL and ITB were released. In the present
study, all valgus deformities occurred during knee extension, which
was mainly caused by contracture of the ITB, and no valgus
deformity was observed in knee flexion. Therefore, the data suggest
that release of the ITB was the key to correcting the valgus
deformity. After dissection of the ITB from the Gerdy tubercle and
removal of lateral hyperplastic osteophytes from the knee, the
valgus deformity was corrected and soft tissue was well balanced.
The exposure of the surgical field and the release of lateral
contracture tissues were combined into one. When the knee joint
field was exposed, a satisfactory balance of force line could be
obtained, and the complex soft tissue balance technique of the
valgus deformity was simplified. In the present study, only 5
patients with severe valgus deformity needed further release, which
involved releasing the LCL and PLC using syringe needles through
repeated poking, which enabled avoidance of the excessive release
caused by the ‘pie-crusting’ technique (19). Additionally, the dissection of the
ITB facilitated exposure of the knee joint and reduced the pressure
of the ITB on the common peroneal nerve after valgus correction.
What needs to be emphasized is that after dissection of the ITB,
adaptive contracture of the ITB was produced according to the
corrected joint space, which meant that effects on the stability of
the knee could be avoided. In addition, because the lateral
structures of the valgus knee, except the ITB, were also
contracted, complete dissection of the ITB did not affect the
stability of the knee. All patients in the present study were
followed up and showed good knee joint stability. Therefore, it can
be suggested that simple ITB dissection can correct most valgus
deformities, especially mild and moderate knee valgus deformity.
The lateral parapatellar approach may minimize the operation time
and avoid further damage caused by long-term patella varus.
The present results demonstrated that the lateral
parapatellar approach with ITB dissection from the Gerdy tubercle
for TKA in valgus knees significantly improved pain and function at
different time points postoperatively compared with preoperative
values. No instances of common peroneal nerve injury, patellar
necrosis, or poor patellar locus occurred. All patients had good
knee stability. In addition, lower limb force line and prosthesis
position were within acceptable ranges.
This study is a preliminary observation of the
clinical efficacy of a new surgical approach and traditional
methods of surgery, such as simple lateral and medial approach,
were not compared to the new surgical method, which is a limitation
of the present study. Additionally, the small sample size is a
further limitation. A large sample study to compare the clinical
efficacy between this new surgical method and the traditional
surgical method is necessary to further confirm the findings.
In conclusion, the lateral parapatellar approach
with ITB dissection from the Gerdy tubercle for TKA can be used as
an effective technique to treat valgus knees, significantly
improving pain and function without deviation of the lower limb
mechanical axis or prosthesis position. The exposure of the
surgical field and the release of the lateral contracture tissue
were combined into one. When the knee joint field was exposed, a
satisfactory balance of force line could be obtained, and the
complex soft tissue balance technique of the valgus deformity was
simplified.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
WC, ZL, JZ, and JJ contributed to the conception of
the study. QC, HY, LQ and FY provided substantial contributions to
the acquisition, analysis and interpretation of data. WC and JJ
critically revised the work for important intellectual content. All
authors read and gave their final approval of the version to be
published.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were in accordance with the ethical standards of the
institutional and/or national research committee and with the 1964
Helsinki declaration and its later amendment. This study was
approved by the Ethics Committee of The Second Affiliated Hospital
of Anhui Medical University. The patients agreed to the use of
their follow-up data in scientific research and signed an informed
consent form.
Patient consent for publication
The patients signed consent forms agreeing to the
use of their data in scientific research.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Puliero B, Favreau H, Eichler D, Adam P,
Bonnomet F and Ehlinger M: Total knee arthroplasty in patients with
varus deformities greater than ten degrees: Survival analysis at a
mean ten years follow-up. Int Orthop. 43:333–341. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Saku S, Madanat R and Mäkinen T: Reasons
and risk factors for ninety days re-admission following primary
total knee arthroplasty in a high-volume Centre. Int Orthop.
42:95–99. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ohmori T, Kabata T, Kajino Y, Taga T,
Hasegawa K, Inoue D, Yamamoto T, Takagi T, Yoshitani J, Ueno T, et
al: The accuracy of the ‘projected surgical transepicondylar axis’
relative to the ‘true surgical transepicondylar axis’ in total knee
arthroplasty. Knee. 24:1428–1434. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Schiapparelli F, Amsler F and Hirschmann
M: Medial parapatellar approach leads to internal rotation of
tibial component in total knee arthroplasty. Knee Surg Sports
Traumatol Arthrosc. 26:1564–1570. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gunst S, Villa V, Magnussen R, Servien E,
Lustig S and Neyret P: Equivalent results of medial and lateral
parapatellar approach for total knee arthroplasty in mild valgus
deformities. Int Orthop. 40:945–951. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Guo CJ, Liu J, Niu DS, Ma J, Kou B, Zhang
HJ, Xu SW, Mu XD, Yang LL and Zhang H: Clinical application of
different operative approach of total knee replacement in knee
valgus patients. Retrospective cohort study. Int J Surg. 49:80–83.
2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Luo ZY, Li LL, Wang D, Wang HY, Pei FX and
Zhou ZK: Preoperative sleep quality affects postoperative pain and
function after total joint arthroplasty: A prospective cohort
study. J Orthop Surg Res. 14(378)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Li Z, Cheng W, Sun L, Yao Y, Cao Q, Ye S,
Qi L, Xu S, Wu X and Jing J: Mini-subvastus versus medial
parapatellar approach for total knee arthroplasty: A prospective
randomized controlled study. Int Orthop. 42:543–549.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Darrith B, Bohl DD, Karadsheh MS, Sporer
SM, Berger RA and Levine BR: Periprosthetic fractures of the distal
femur: Is open reduction and internal fixation or distal femoral
replacement superior? J Arthroplasty. 35:1402–1406. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rossi R, Rosso F, Cottino U, Dettoni F,
Bonasia D and Bruzzone M: Total knee arthroplasty in the valgus
knee. Int Orthop. 38:273–283. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
McAuley J, Collier M, Hamilton W, Tabaraee
E and Engh G: Posterior cruciate-retaining total knee arthroplasty
for valgus osteoarthritis. Clin Orthop Relat Res. 466:2644–2649.
2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ranawat A, Ranawat C, Elkus M, Rasquinha
V, Rossi R and Babhulkar S: Total knee arthroplasty for severe
valgus deformity. J Bone Joint Surg Am. 87 (Suppl 1):S271–S284.
2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Buechel F: A sequential three-step lateral
release for correcting fixed valgus knee deformities during total
knee arthroplasty. Clin Orthop Relat Res. 170–175. 1990.PubMed/NCBI
|
|
14
|
Chun K, Lee S, Baik J, Kook S, Han J and
Chun C: Clinical and radiological results of cruciate-retaining
total knee arthroplasty with the NexGen®-CR system:
Comparison of patellar resurfacing versus retention with more than
14 years of follow-up. J Orthop Surg Res. 12(144)2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fiddian NJ, Blakeway C and Kumar A:
Replacement arthroplasty of the valgus knee. A modified lateral
capsular approach with repositioning of vastus lateralis. J Bone
Joint Surg Br. 80:859–861. 1998.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sekiya H, Takatoku K, Takada H, Sugimoto N
and Hoshino Y: Lateral approach is advantageous in total knee
arthroplasty for valgus deformed knee. Eur J Orthop Surg Traumatol.
24:111–115. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chalidis B, Ye K, Sachinis N, Hawdon G and
McMahon S: Lateral parapatellar approach with tibial tubercle
osteotomy for the treatment of non-correctable valgus knee
osteoarthritis: A retrospective clinical study. Knee. 21:204–208.
2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Krackow K and Mihalko W: Flexion-extension
joint gap changes after lateral structure release for valgus
deformity correction in total knee arthroplasty: A cadaveric study.
J Arthroplasty. 14:994–1004. 1999.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Aglietti P, Lup D, Cuomo P, Baldini A and
De Luca L: Total knee arthroplasty using a pie-crusting technique
for valgus deformity. Clin Orthop Relat Res. 464:73–77.
2007.PubMed/NCBI View Article : Google Scholar
|