Introduction
Cervical cancer is one of the most common cancers in
developing countries, second only to breast cancer, with more than
450,000 new cases every year (1).
Romania has the highest incidence of cervical cancer in Europe with
28.6 cases/100,000, more than four times the incidence found in
Western Europe (1,2). This is in part explained by the lack
of an effective nationwide screening program that would allow the
detection and treatment of premalignant cervical/precancerous
lesions. In addition, due to the ineffective screening program,
many cases are diagnosed at a later stage than in developed
countries (3-11).
As a consequence, treatment response is generally poorer, with a
death rate of 0.38 per new case in Romania, compared to just for
0.21 per new case in developed countries such as Germany (2,12).
Given these particularities found in developing
countries, where the number of patients diagnosed at a later stage
is considerable, we aimed to ascertain the role of surgery in the
multimodal treatment of locally advanced cervical cancer. Most
studies and guidelines recommend radiotherapy with or without
chemotherapy as the gold standard for locally advanced cervical
cancer (13). Furthermore, some
studies suggest that performing surgery after radiotherapy does not
improve therapeutic outcome and moreover it increases patient
morbidity (14). However, the great
majority of locally advanced cases diagnosed in Romania are treated
with radiotherapy and if there is a good response and downstaging
occurs, usually adjuvant surgery is performed. The most important
argument for this therapeutic plan is that in many cases,
radiotherapy in association or not with chemotherapy is not able to
completely destroy the malignant cells and up to 40-50% of patients
have histopathological evidence of residual tumor (15). Additionally, by performing surgery,
better local control of the disease is achieved (16). Thus, we consider surgery as having
an essential role in treating locally advanced cervical cancer.
The most common histologic variant of cervical
cancer is squamous cell carcinoma (SCC) with an incidence of up to
80-95% (17,18), but due to the wide implementation of
screening programs in developed countries and detection of
premalignant disease, its incidence showed a marked decline over
the past 40 years (18,19). Unfortunately, the same is not true
for other histologic variants. There has been a constant rise in
the incidence of endocervical adenocarcinomas over the last 40,
especially in young women. The incidence of endocervical
adenocarcinomas has doubled in the last decades, representing
~20-25% of cases of cervical cancer (18,20,21).
Studies suggest that hematoxylin and eosin staining is sufficient
for establishing the histology of primary endocervical
adenocarcinoma and its variants, and that more expensive
immunohistochemistry is not always mandatory (21). From the wide spectrum of cervical
adenocarcinoma subtypes we will focus on two of most common
variants: Adenocarcinoma usual endocervical subtype (AC) and
adenosquamous carcinoma (ASC) (16,20).
The most common variant is the AC subtype, that account for 75-80%
of all cases of invasive cervical adenocarcinomas (21,22). A
high density of medium sized round or oval glands and loss of
lobular arrangement characterize these tumors. A wide variety of
architectural patterns can be encountered ranging from papillary
growth, tubular glands, and cribriform glands to solid areas of
undifferentiated cells, depending on how well the tumor is
differentiated. Cells typically show intracytoplasmic mucin that is
usually abundant and mitotic activity; also apoptotic bodies are
quite common (21,23). ASC of the cervix is less common than
AC, but still accounts for up to 5-10% of cervical carcinomas and
is composed of a malignant glandular component and a malignant
squamous component (24,25). Both components are clearly visible
on hematoxylin and eosin staining, without the need for
histochemical stains. The glandular component is usually of
endocervical subtype but it may also be mucinous or mixed
endocervical and mucinous, endometrioid or clear cell. The squamous
component may be glycogenated (21,26).
Although not mandatory, immunohistochemistry (IHC)
can offer greater information regarding the exact diagnosis and
tumor characteristics and it should be performed when possible. For
example, to distinguish between endocervical AC and endometrioid
AC, IHC is usually warranted. The presence of carcinoembryonic
antigen (CEA) and p16 expression combined with the absence of
progesterone receptors (PRs) and estrogen receptors (ERs) favor a
cervical origin (27).
Studies have shown that patients with AC/ASC
histology have worse survival outcome than those with SCC (19,28).
However, the tumor response to chemoradiotherapy of AC/ASC compared
to SCC has been rarely studied. The present study was designed to
investigate the rate of residual cancer in patients with locally
advanced cervical cancer who underwent surgery after concurrent
chemoradiotherapy and to find out the impact of tumor histological
subtype on the chemoradiotherapy response.
Patients and methods
Patients
Data were obtained retrospectively for all patients
with locally advanced cervical cancer, treated between January 2005
and December 2014 at the Oncology Institute of Bucharest, Romania.
The patients were staged according to the International Federation
of Gynecology and Obstetrics (FIGO) staging criteria (29) and only patients with FIGO stages
IIB-IVA were selected. Depending on the histological classification
of the tumor, patients were divided into an SCC histology group or
an AC/ASC histology group. All patients were treated by the same
multidisciplinary team according to the same protocol.
The data collected retrospectively did not contain
personal information and only the agreement of the Ethics Committee
of the Oncology Institute ‘Prof. Dr. Alexandru Trestioreanu’
Bucharest was required and obtained without the need of informed
consent or the consent of the patient/legal representative in the
case of minors.
A comprehensive/rigorous staging protocol was used,
consisting of clinical examination, including vaginal and rectal
exam. The protocol also included computed tomography and/or
magnetic resonance imaging (chest-abdomen-pelvis). For cases in
which bladder or rectum involvement was suspected, the staging
protocol also included cystoscopy and colonoscopy. Patients with
evidence of distant metastasis were excluded from the study.
Treatment
The treatment plan first included chemoradiotherapy.
For radiotherapy the protocol was whole pelvic external beam
radiation with a total dose of 50.4 Gy and two high dose rate
brachytherapy with a total dose of 15 Gy to A point. Concurrent
chemotherapy was administered, consisting of cisplatin 40
mg/m2 weekly for a total of 5 weeks.
In all cases, adjuvant surgery was performed after
6-8 weeks from the completion of chemoradiotherapy. The type and
extent of the surgical intervention was determined according to
pre-treatment data, post-radiation observations and operative
findings. In the majority of cases, type II or III radical
hysterectomy (radical abdominal hysterectomy with bilateral pelvic
lymphadenectomy or Wertheim-Meigs procedure) was performed. In 10
cases where bladder or rectum involvement was confirmed, pelvic
exenteration (partial or complete) was performed.
All surgical specimens were sent for pathology
assessment. The tumor response rate to chemotherapy was assessed by
preoperative data and histopathological examination of the cervical
specimen. A complete response (CR) was defined as the absence of
residual tumor at pathology examination. A partial response (PR)
was defined as the presence of residual tumor at the pathology
examination.
Statistical analysis
For statistical analysis we used NCSS 2019
Statistical Software (2019) [NCSS, LLC. (ncss.com/software/ncss)] (two proportions comparison
test). The results were analyzed and interpreted according to the
obtained P-value; P<0.05 was considered to be statistically
significant.
Results
Between January 2005 and December 2014, a total of
461 women with locally advanced cervical cancer (stages IIB-IVA),
were treated at the Oncology Institute of Bucharest and were
included in this study. Of these, 385 patients had SCC histology,
being assigned to the SCC group, 49 patients had AC and 27 patients
had ASC, being assigned to the AC/ASC group.
The characteristics of the patients are summarized
in Table I. Tumor FIGO stage was
IIB in 393 cases, IIIA-IIIB in 58 cases and IVA in 10 cases. There
were no statistically significant differences between FIGO staging
in the SCC group and the AC/ASC group (P>0.05). The mean age for
the SCC group was 61.7 years, while for the AC/ASC it was 59.1
years.
 | Table ICharacteristics of the patients
included in the study. |
Table I
Characteristics of the patients
included in the study.
| | All patients | SCC group | AC/ASC group |
|---|
| No. of patients
(%) | 461(100) | 385(83) | 76(17) |
| Age (years) |
|
Range | 28-82 | 28-82 | 29-71 |
|
Mean | 61.7 | 62.9 | 59.1 |
| FIGO stage, n
(%) |
|
IIB | 393 | 329 (85.5) | 64 (84.2) |
|
IIIA,
IIIB | 58 | 47 (12.2) | 11 (14.5) |
|
IVA | 10 | 9 (2.3) | 1 (1.3) |
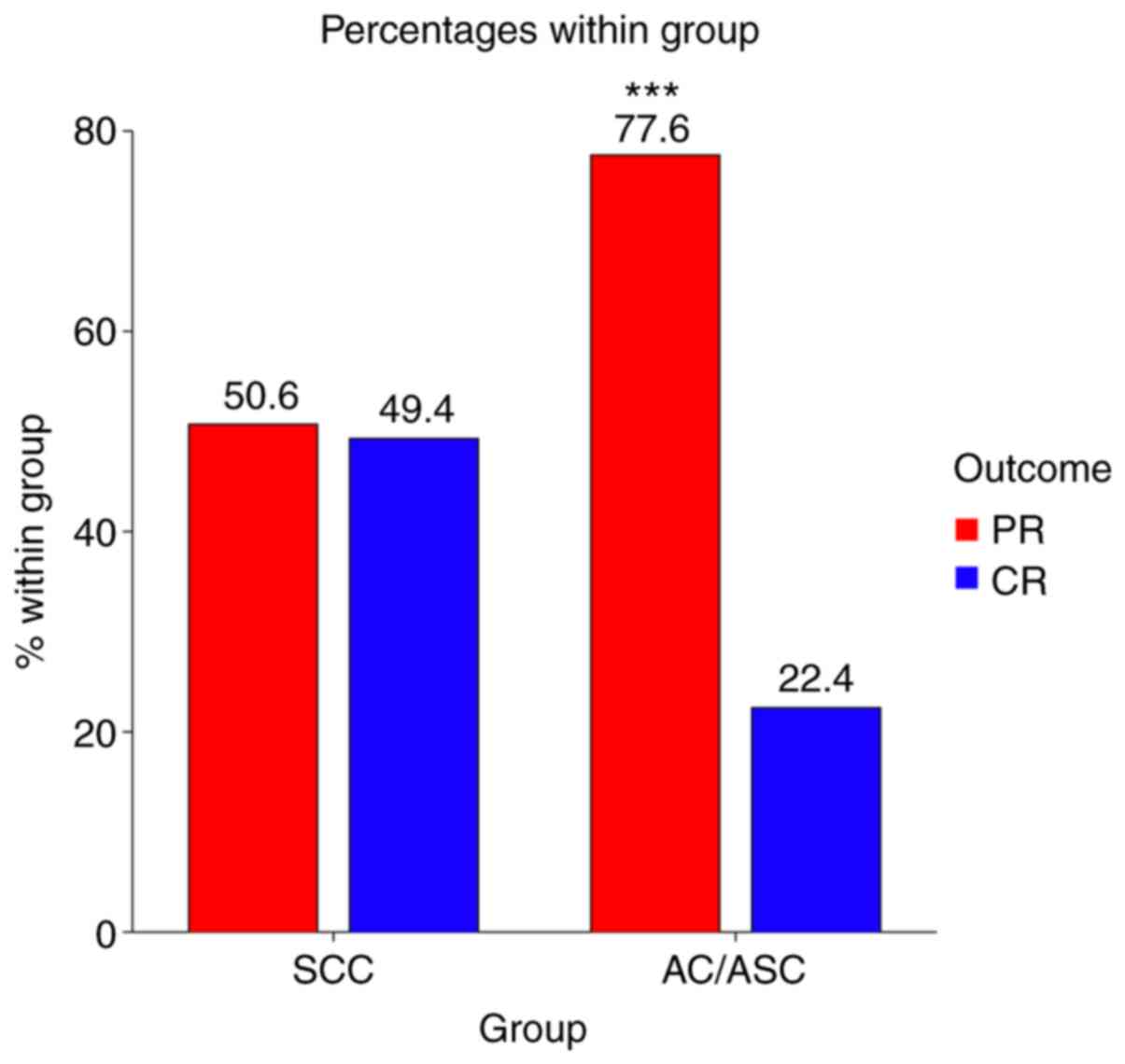
From the pathological reports of surgical specimens,
PR with residual tumor in the cervix was found in 254 patients
(55.1%). Histopathological distribution of the cases is presented
in Table II, with residual tumor
present in 195 (50.6%) of the 385 SCC cases, and in 59 (77.6) of
the 76 AC/ASC cases.
 | Table IIHistopathological distribution of the
cases with residual tumor. |
Table II
Histopathological distribution of the
cases with residual tumor.
| Histology
subtype | SCC | AC/ASC | AC | ASC | Total |
|---|
| Total no. of
patients | 385 | 76 | 49 | 27 | 461 |
| Patients with
residual tumor after chemoradiotherapy, n (%) | 195 (50.6) | 59 (77.6) | 36 (73.5) | 23 (85.1) | 254 (55.1) |
The PR rate for the SCC group was 50.6%, while for
the AC/ASC group the PR rate was 77.6%; significantly higher
(P<0.001) (Fig. 1). In the
AC/ASC group the PR rate was 73.5% for the AC histology and 85.1%
for the ASC histology. This finding comes to confirm the poorer
response of AC and ASC to chemoradiotherapy.
Discussion
Our results come to confirm that the histologic
subtype of the tumor in any malignancy must be taken into account
when deciding the therapeutic plan, since depending on the tumor
characteristics, the response to therapy can vary widely (30,31).
In addition, before establishing the therapeutic options, a
rigorous evaluation of the patient for distant metastasis must be
performed, since there have been reports of rare metastatic sites
such as the spleen from primary cervical cancers (32).
Numerous studies conducted over the last two decades
have found that the treatment response and overall survival of
patients with adenocarcinoma usual endocervical subtype (AC) or
adenosquamous carcinoma (ASC) is generally poorer compared with
that of patient with squamous cell carcinoma (SCC) (27,28,33,34).
Our study comes to confirm once more that tumor response to
chemoradiotherapy is worse for AC/ASC histology. The rate of
residual tumor was almost 50% higher for AC/ASC group (77.6%) in
comparison with the SSC group (50.6%). However, despite these
findings, the therapeutic recommendations of these patients did not
change over time; the treatment strategy being similar to that used
for SCC histology (35).
The results clearly show that there is a need for a
more effective treatment protocol for patients with locally
advanced cervical cancer who exhibit AC/ASC histology. Some studies
suggest that adjuvant surgery may play a crucial role in these
cases where residual tumor is still present after chemoradiotherapy
(36). The guidelines usually do
not recommend surgery for these advanced stages, but depending on
the geographic region and local protocols, surgery is often taken
into consideration, one such example being Romania (37).
According to the latest recommendations for women
with early-stage cervical cancer from IA2 up to IB2, modified
radical hysterectomy is preferred over primary radiation therapy
(38). Nonradical surgery is
recommended for women with microscopic disease with stromal
invasion <3 mm in depth in whom there is no evidence of
intermediate or high risk features (39). The preservation of fertility may be
targeted in carefully selected cases of patients who meet all of
the five criteria: Desire to preserve fertility; reproductive age
<40 years, at most stage IB1, lack of risk factors for
recurrence, only low-risk histology adenocarcinoma or squamous cell
carcinoma and mandatory the lack of lymph node metastasis (40).
Primary radiotherapy is reserved for women with
several important medical comorbidities and altered general status
(41). The cases with early
cervical cancer treated primary by surgical approach should
continue with adjuvant therapy in the presence of findings that
suggests an increased risk of recurrence. The benefit of surgery
compared with radiotherapy is the possibility of ovarian
conservation through surgery avoiding premature menopause and
offering possibilities for reproduction technologies (42).
Regarding the advanced stages of cervical cancer,
primary chemoradiation which has demonstrated superior positive
results compared to radiotherapy alone is recommended by the latest
studies. Radiotherapy in conjunction with chemotherapy, especially
brachytherapy results in significant higher rates of survival
(43-47).
Most centers do not perform hysterectomy after chemoradiation and
the results of research performed in this field until now show that
after a 3-year follow-up women who underwent hysterectomy exhibit
no difference in survival rate (48).
One limitation of our study is that it was conducted
at a single institution and that it included a relatively small
number of patients with AC/ASC subtypes/histology due to their low
incidence. Another limitation is that being a retrospective study,
we cannot exclude potential sources of biases, although the FIGO
staging was similar for both the SSC and AC/ASC group.
The prognostic significance and treatment response
of AC or ASC histologic subtypes in comparison with SCC should be
evaluated in further prospective large scale multi-center studies,
for a clear conclusion to be drawn and in order to develop a
treatment protocol for these subtypes of cervical cancer.
In conclusion, the present study demonstrated that
cervical cancer patients with AC/ASC histology have significant
poorer treatment response to chemoradiotherapy than those with SCC.
Current guidelines for cervical cancer do not take into account the
different histologyic subtypes and may not be adequate for all
patients, since studies show that response to chemoradiotherapy
varies significantly depending on the histologic subtype. We found
that in 55.1% of the cases included in the study, despite
chemoradiation, there was a partial response, with residual tumor
still present. The percentage was significantly higher for the
AC/ASC group (77.6%), compared to the SCC group (50.6%). We
consider that in such cases where a residual tumor is present,
adjuvant surgery is mandatory for improving the survival rates. In
literature, the differences regarding the therapeutic response to
chemoradiotherapy between AC/ASC and SCC have been rarely studied,
thus further research is warrant to draw a definite conclusion.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SV, REB and CGH collected, analyzed and interpreted
the patient data regarding the treatment strategies corresponding
to the patients with early stage cervical cancer. AS, RGI, LIC and
NB collected the data and made substantial contribution to the
conception of the research and statistical analysis. SV, FF, DCS
and AN substantially contributed to the conception of the study,
the interpretation of the data and the writing of the manuscript.
All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The data collected retrospectively did not contain
personal information and only the agreement of the Ethics Committee
of the Oncology Institute ‘Prof. Dr. Alexandru Trestioreanu’
Bucharest was required and obtained without the need of informed
consent or the consent of the patient/legal representative in the
case of minors.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Altobelli E and Lattanzi A: Cervical
Carcinoma in the European Union. Int J Gynecol Cancer. 25:474–483.
2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Solomon I, Voiculescu VM, Caruntu C, Lupu
M, Popa A, Ilie MA, Albulescu R, Caruntu A, Tanase C, Constantin C,
et al: Neuroendocrine factors and head and neck squamous cell
carcinoma: An affair to remember. Dis Markers.
2018(9787831)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Boda D, Docea AO, Calina D, Ilie MA,
Caruntu C, Zurac S, Neagu M, Constantin C, Branisteanu DE,
Voiculescu V, et al: Human papilloma virus: Apprehending the link
with carcinogenesis and unveiling new research avenues. Int J
Oncol. 52:637–655. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Boda D, Neagu M, Constantin C, Voinescu
RN, Caruntu C, Zurac S, Spandidos DA, Drakoulis N, Tsoukalas D and
Tsatsakis AM: HPV strain distribution in patients with genital
warts in a female population sample. Oncol Lett. 12:1779–1782.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Calenic B, Greabu M, Caruntu C, Nicolescu
MI, Moraru L, Surdu-Bob CC, Badulescu M, Anghel A, Logofatu C and
Boda D: Oral keratinocyte stem cells behavior on diamond like
carbon films. Rom Biotechnol Lett. 21:11914–11922. 2016.
|
|
7
|
Lupu M, Caruntu A, Caruntu C, Boda D,
Moraru L, Voiculescu V and Bastian A: Non-invasive imaging of
actinic Cheilitis and squamous cell carcinoma of the lip. Mol Clin
Oncol. 8:640–646. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Boda D: Cellomics as integrative Omics for
cancer. Curr Proteomics. 10:237–245. 2013.
|
|
9
|
Lupu M, Căruntu A, Moraru L, Voiculescu
VM, Boda D, Tanase C and Căruntu C: Non-invasive imaging techniques
for early diagnosis of radiation-induced squamous cell carcinoma of
the lip. Rom J Morphol Embryol. 59:949–953. 2018.PubMed/NCBI
|
|
10
|
Bohîlțea RE, Turcan G, Cîrstoiu MM,
Ionescu C, Nemescu D, Turcan N and Vladareanu R: Clinical
implementation of ultrasound gynecological examination report
(software REGU) based on international consensuses of tumor study
groups. 5th Romanian congress of the romanian society of ultrasound
in obstetrics and gynecology, bucharis, Romania. Filodiritto
Publisher, pp99-104, 2017.
|
|
11
|
Badea M, Baroş A, Bohîlţea RE, Julea IE,
Furtunescu FL, Istrate-Ofiţeru AM, Iovan L, Cîrstoiu MM, Burcin MR,
Turcan N, et al: Modern interdisciplinary monitoring of cervical
cancer risk. Rom J Morphol Embryol. 60:469–478. 2019.PubMed/NCBI
|
|
12
|
Teleanu C, Baili P, Berrino F, Micheli A,
Furtunescu F, Minca DG and Sant M: Recent trends of cancer
mortality in Romanian adults: Mortality is still increasing,
although young adults do better than the middle-aged and elderly
population. Eur J Cancer Prev. 22:199–209. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chereau E, De LA, Hosseraye C, Ballester
M, Monnier L, Rouzier R, Touboul E and Daraï E: The role of
completion surgery after concurrent radiochemotherapy in locally
advanced stages IB2-IIB cervical cancer. Anticancer Res.
33:1661–1666. 2013.PubMed/NCBI
|
|
14
|
Touboul C, Uzan C, Mauguen A, Gouy S, Rey
A, Pautier P, Lhomme C, Duvillard P, Haie-Meder C and Morice P:
Prognostic factors and morbidities after completion surgery in
patients undergoing initial chemoradiation therapy for locally
advanced cervical cancer. Oncologist. 15:405–415. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Carcopino X, Houvenaeghel G, Buttarelli M,
Esterni B, Tallet A, Goncalves A and Jacquemier J: Equivalent
survival in patients with advanced stage IB-II and III-IVA cervical
cancer treated by adjuvant surgery following chemoradiotherapy. Eur
J Surg Oncol. 34:569–575. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Blidaru A, Bordea C, Burcoș T, Duduș L,
Eniu D, Ioanid N, Kacso G, Minciuna C, Savu M, Scripcariu V, et al:
Mind the gap between scientific literature recommendations and
effective implementation. Is there still a role for surgery in the
treatment of locally advanced cervical carcinoma? Chirurgia
(Bucur). 114:18–28. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Yoshida T, Sano T, Oyama T, Kanuma T and
Fukuda T: Prevalence, viral load, and physical status of HPV 16 and
18 in cervical adenosquamous carcinoma. Virchows Arch. 455:253–259.
2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Smith HO, Tiffany MF, Qualls CR and Key
CR: The rising incidence of adenocarcinoma relative to squamous
cell carcinoma of the uterine cervix in the United States-A 24-year
population-based study. Gynecol Oncol. 78:97–105. 2000.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gien LT, Beauchemin MC and Thomas G:
Adenocarcinoma: A unique cervical cancer. Gynecol Oncol.
116:140–146. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sasieni P and Adams J: Changing rates of
adenocarcinoma and adenosquamous carcinoma of the cervix in
England. Lancet. 357:1490–1493. 2001.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Young RH and Clement PB: Endocervical
adenocarcinoma and its variants: Their morphology and differential
diagnosis. Histopathology. 41:185–207. 2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hodgson A and Park KJ: Cervical
adenocarcinomas: A heterogeneous group of tumors with variable
etiologies and clinical outcomes. Arch Pathol Lab Med. 143:34–46.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Pirog EC: Cervical adenocarcinoma:
Diagnosis of human Papillomavirus-positive and human
Papillomavirus-negative tumors. Arch Pathol Lab Med. 141:1653–1667.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yasuda S, Kojima A, Maeno Y, Oki N,
Miyahara Y, Sudo T, Takekida S, Yamaguchi S and Nishimura R: Poor
prognosis of patients with stage Ib1 adenosquamous cell carcinoma
of the uterine cervix with pelvic lymphnode metastasis. Kobe J Med
Sci. 52:9–15. 2006.PubMed/NCBI
|
|
25
|
Harrison TA, Sevin BU, Koechli O, Nguyen
HN, Averette HE, Penalver M, Donato DM and Nadji M: Adenosquamous
carcinoma of the cervix: Prognosis in early stage disease treated
by radical hysterectomy. Gynecol Oncol. 50:310–315. 1993.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lim C, Leecy T, McKenzie P, Pather S,
Carter J and Russell P: Two cases of adenosquamous carcinoma of the
cervix with extensive in situ and invasive endometrial extension.
Int J Gynecol Pathol. 30:193–197. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Fujiwara K, Monk B and
Devouassoux-Shisheboran M: Adenocarcinoma of the uterine cervix:
Why is it different? Curr Oncol Rep. 16(416)2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chen JLY, Huang CY, Huang YS, Chen RJ,
Wang CW, Chen YH, Cheng JC, Cheng AL and Kuo SH: Differential
clinical characteristics, treatment response and prognosis of
locally advanced adenocarcinoma/adenosquamous carcinoma and
squamous cell carcinoma of cervix treated with definitive
radiotherapy. Acta Obstet Gynecol Scand. 93:661–668.
2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bhatla N, Berek JS, Cuello Fredes M, Denny
LA, Grenman S, Karunaratne K, Kehoe ST, Konishi I, Olawaiye AB,
Prat J, et al: Revised FIGO staging for carcinoma of the cervix
uteri. Int J Gynecol Obstet. 145:129–135. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Herghelegiu CG, Neacşu A, Oprescu ND,
Cărbunaru AE, Brăila AD, Curea FG, Marcu ML, Ioan RG and Bohîlţea
RE: Difficulties of clinical and histopathological diagnosis in
advanced vulvar clear cell carcinoma. Rom J Morphol Embryol.
59:1233–1237. 2018.PubMed/NCBI
|
|
31
|
Anghel RM, Trifanescu OG, Mitrica RI,
Curea FG, Botnariuc I, Herghelegiu CG, Orlov CM and Ilie SM: Good
prognosis went badly: Fulminant evolution of a 29-Year-old patient
with verrucous carcinoma of the cervix. J Adolesc Young Adult
Oncol. 6:499–502. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Marcu ML, Neacşu A, Stoica C, Bacalbaşa N,
Contolenco A and Radu E: Clinical and pathological features of
splenic metastasis from cervical squamous cell carcinoma. Rom J
Morphol Embryol. 58:1157–1164. 2017.PubMed/NCBI
|
|
33
|
Kaidar-Person O, Yosefia S and
Abdah-Bortnyak R: Response of adenocarcinoma of the uterine cervix
to chemoradiotherapy. Oncol Lett. 9:2791–2794. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Aoki D: Annual report of gynecologic
oncology committee, Japan society of obstetrics and gynecology,
2013. J Obstet Gynaecol Res. 40:338–348. 2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Koh WJ, Abu-Rustum NR, Bean S, Bradley K,
Campos SM, Cho KR, Chon HS, Chu C, Clark R, Cohn D, et al: Cervical
cancer, NCCN clinical practice guidelines in oncology. J Natl Compr
Canc Netw. 17:64–84. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Yokoi E, Mabuchi S, Takahashi R, Matsumoto
Y, Kuroda H, Kozasa K and Kimura T: Impact of histological subtype
on survival in patients with locally advanced cervical cancer that
were treated with definitive radiotherapy:
Adenocarcinoma/adenosquamous carcinoma versus squamous cell
carcinoma. J Gynecol Oncol. 28(e19)2017.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Berceanu C, Mehedintu C, Berceanu S,
Paitici S, Ciortea R, Bratila E, Cirstoiu MM, Navolan D, Hainarosie
R and Bohîlțea RE: Acetic acid and lugol tests in colposcopic
assessment and surgical management of cervical intraepithelial
lesions. Rev Chim. 69:930–933. 2018.
|
|
38
|
Dimitriu MCT, Ionescu CA, Gheorghiu DC,
Socea LI, Bratu OG, Constantin VD, Ples L, Neacsu A, Bobic S and
Socea B: Mepivacaine hydrochloride-an efficient local anesthetic
solution for the electroresection of the benign and preneoplastic
lesions of the cervix and uterus. Rev Chim. 69:2391–2395. 2018.
|
|
39
|
Bacalbasa N, Balescu I, Vilcu M, Neacsu A,
Dima S, Croitoru A and Brezean I: Pelvic exenteration for locally
advanced and relapsed pelvic malignancies-an analysis of 100 cases.
In Vivo. 33:2205–2210. 2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Bohîlțea RE, Bacalbașa N, Turcan N,
Cîrstoiu M, Terzea DC, Simion G, Munteanu O, Berceanu C and Brătilă
E: Bilateral serous surface papillary borderline ovarian tumor in
19 years old patient: Ultrasound, immunohistochemical and
therapeutic particularities. Rom J Morphol Embriol. 58:989–995.
2017.PubMed/NCBI
|
|
41
|
Marcu RD, Spinu AD, Mischianu D, Oprea IS,
Diaconu C, Socea B and Bratu OG: The efficiency of hyaluronic acid
in the management of radiation induced cystitis. Farmacia.
67:50–55. 2019.
|
|
42
|
Iorga RA, Bratu OG, Marcu RD, Constantin
T, Mischianu DLD, Socea B, Gaman MA and Diaconu CC: Venous
thromboembolism in cancer patients: Still looking for answers. Exp
Ther Med. 18:5026–5032. 2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Nacer K, Bratu O, Berechet M, Bumbu G and
Bumbu A: Global surgical principles in the vaginal approach of
advanced pelvic organ prolapse. In: Proceedings of the 14th
National Congress of Urogynecology and the National Conference of
the Romanian Association for the Study of Pain. Filodiritto
Publisher, pp172-180, 2017.
|
|
44
|
Spinu AD, Bratu OG, Diaconu CC, Stanescu
AMA, Bundau S, Fratila O, Bohiltea R and Mischianu DLD: Botulinum
toxin in low urinary tract disorders-over 30 years of practice
(Review). Exp Ther Med. 20:117–120. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Ionescu CA, Matei A, Navolan D, Dimitriu
M, Bohîltea R, Neacsu A, Ilinca C and Ples L: Correlation of
ultrasound features and the risk of ovarian malignancy algorithm
score for different histopathological subtypes of benign adnexal
masses. Medicine (Baltimore). 97(e11762)2018.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Berceanu C, Cîrstoiu M, Mehedințu C,
Brătilă P, Berceanu S, Vlădăreanu S, Bohîlțea R and Brătilă E:
Hormone Deficiency and its Impact on the Lower Urinary Tract. In:
The 13th National Congress of Urogynecology (UROGYN 2016). Brătilă
E (ed). Filodiritto Publisher, pp29-38, 2016.
|
|
47
|
Brătilă E, Comandasu D, Coroleucă C,
Cirstoiu M, Bohîlțea R, Mehedințu C, Vlădăreanu S and Berceanu C:
Gastrointestinal symptoms in endometriosis correlated with the
disease stage. Filodiritto Editore-Proceedings, XXXVI National
Congress of Gastroenterology, Hepatology and Digestive Endoscopy,
66-70, 2016.
|
|
48
|
Bumbu A, Nacer K, Bratu O, Berechet M,
Bumbu G and Bumbu B: Ureteral Lesions in Gynecological Pathology.
Proceedings of the 14th National Congress of Urogynecology and the
National Conference of the Romanian Association for the Study of
Pain, Bucharest, Romania. Filodiritto Publisher, pp82-89, 2017.
|