Introduction
Coronary artery disease (CAD)-induced myocardial
ischemia (MI), including acute myocardial infarction (AMI), is a
disease entity with the highest mortality rate in the world.
Approximately 800,000 US residents experience AMI annually and 27%
of these patients do not survive (1,2).
Coronary angiography (CAG) is the gold standard for diagnosing CAD
and MI, whereas invasive operations are high-risk treatment methods
that are not easily accepted by patients, such as lack of expensive
devices and experienced operators (3,4). Prior
to the development of CAG, electrocardiography (ECG) was the best
noninvasive technique for CAD/MI diagnosis (5). In 1979, stress echocardiography (SE)
was classified as an invaluable technique that combines
echocardiography and ECG with stress testing (6). Treadmill or bicycle exercise is the
most frequently used type of workload stressor and dobutamine or
dipyridamole may be administered as pharmacological agents
(6,7). For instance, the 2015 European Society
of Cardiology guidelines and the 2014 American Heart Association
consensus statement recommend the use of noninvasive stress imaging
for the diagnosis of stable CAD and female ischemic heart disease
due to the significantly higher diagnostic accuracy of this
technique (8). Douglas et al
(9) reported that exercise ECG
testing and SE may improve the diagnostic sensitivity and
specificity in females with obstructive CAD. However, only a
limited number of studies have combined exercise ECG testing
(EET)/SE with CAG/coronary CT angiography (CCTA) in order to
confirm the diagnosis of CAD (10).
SE is frequently used in i) risk stratification of
patients with suspected CAD, ii) pre-operative risk assessment,
iii) revascularization evaluation, iv) assessment of indications
for percutaneous coronary intervention (PCI) and v) CAD/MI of
unclear significance as determined by CAG or CT (6,11). A
high number of studies have reported on the use of myocardial
contrast echocardiography (MCE) perfusion imaging to improve the
wall motion sensitivity of SE (12,13).
MCE allows for simultaneous evaluation of myocardial perfusion and
regional function and has a potential role in viability assessment
(6,7). Furthermore, excessive elevation of
systolic blood pressure during physical exercise is associated with
an increased left ventricular mass in pre-hypertensive individuals
(14). This result suggests that
exercise blood pressure and EET are not only useful tools for
screening indications and contraindications but also assistant
diagnostic techniques for CAD/MI. An arterial segment that is
dysfunctional or exhibits recession at the resting or loading state
reflects the contracting wall response of
ischemia/necrosis/viability (6).
In the present study, analysis of EET ST-segments
combined with SE wall motion abnormalities (WMA) was used to
predict MI in adults with unknown MI status and was subsequently
compared with CAG/CCTA results to assess the
sensitivity/specificity/positive-predictive value (PPV) and
negative-predictive value (NPV) in detecting CAD/MI. Therefore, the
present study was performed to address the aforementioned issues
and assess a possible association of the diagnostic accuracy
between invasive and noninvasive CAD/MI. The present study provided
an improved strategy for the noninvasive imaging diagnosis of
CAD/MI.
Materials and methods
Study population
The Ethics Committee of The First Affiliated
Hospital of Nanjing Medical University (Nanjing, China) approved
the present study and all patients provided written informed
consent (approval no. SRFA-048). A total of 278 patients were
enrolled between August 2018 and August 2019 at The First
Affiliated Hospital of Nanjing Medical University (Nanjing, China).
Certain patients had undergone PCI at least 6 months previously,
whereas others did not undergo PCI. None of the patients had a
previous history of heart failure or severe symptoms of atypical
chest pain, severe dyspnea or an echocardiograph indicative of
ischemic WMA. Prior to EET/SE, all patients underwent resting
ECG/echocardiography, which was independently interpreted as
negative for MI by three cardiologists. The patients who were
diagnosed with pulmonary disease, including chronic obstructive
pulmonary disease and asthma, as well as severe bundle-branch
blocking/cardiac insufficiency, which may affect the safety of
exercise testing, were excluded. In addition, patients with more
than moderate valvular dysfunction, permanent pacemaker
implantation with post-PCI were not included. The patients' medical
information was recorded and subsequently analyzed. Following
EET/SE, all patients underwent CAG/CCTA. A total of 66 patients
were diagnosed with MI (CAG vessel stenosis ≥50%) and 212 patients
were diagnosed with non-MI (CAG vessel stenosis <50%).
Diagnostic criteria
All diagnoses based on SE were divided into 4
categories according to wall motion function: i) Normal response,
ii) ischemic response, iii) necrotic response and iv) viability
response. Categories ii, iii and iv were reported in a recent
study, whereas category i was not found to be present (6). A total of three experienced
cardiologists assessed the results, which were classified as
positive or negative.
EET was performed and independently interpreted by
three cardiologists. Resting/exercise ECG, heart rate (HR) and
blood pressure (BP) were recorded during the process. In the
present study, the treadmill exercise and Bruce protocol were used
to evaluate the method. Severe ischemia (severe chest pain, ST
segment elevated ≥2 mm horizontal or downsloping ST depression),
severe hypertension [HTN; systolic blood pressure (SBP) ≥220 mmHg
or diastolic blood pressure (DBP) ≥120 mmHg], hypotension (SBP ≤90
mmHg or DBP ≤60 mmHg), presyncope, or significant arrhythmia and
fatigue were defined as the end-points of the test. For those
patients who achieved a workload of ≥9 metabolic
equivalent/dobutamine load or achieved target heart pace without
any symptoms, hemodynamic compromise or ECG changes, the test was
considered negative. The following symptoms were considered to
indicate a positive test: Hypotension, significant chest pain,
related arrhythmias, two or more leads exhibiting ST segment
elevation ≥1 mm and planar or downsloping ST depression during
exercise or in recovery (6,13).
Stress test/SE
All patients were treated using a treadmill protocol
(GE T2100) or dobutamine infusion. Short axis and apical 4-chamber,
2-chamber and 3-chamber images were obtained (iE33 Philips Medical
Systems B.V.). Imaging of rest, peak-exercise, post-exercise and
recovery were evaluated as described above. Information on exercise
capacity, BP, HR and rhythm changes was collected and analyzed
(15). WMA analysis was also
performed (15). Sonovue (Bracco),
an ultrasound contrast agent, was administered by intravenous bolus
injection (0.3-0.5 ml) and was flushed with saline (16). The final results were independently
interpreted by three cardiologists. A 17-segment left-ventricle
model was evaluated by a four-point score (1, normal; 2,
hypokinetic; 3, akinetic; 4, dyskinetic motion), which was used to
analyze WMA and wall thickening (6). A negative judgment was defined as
normal ST segments at baseline, exercise and recovery stages.
Peak-exercise was defined as patients achieving the age-predicted
target HR at a workload of at least 7 METS Regional WMA at rest or
randomized exercise stages were deemed as a positive SE result
(6,13).
A standard dobutamine stress protocol was offered to
those who were less suitable for high workload. Continuous
intravenous infusion of dobutamine was performed in 3 min
increments with a 5 µg/kg/min onset, which was increased to 10, 20,
30 and 40 µg/kg/min (6).
Exercise EET test
The EET results were interpreted by three expert
cardiologists. The treadmill and Bruce protocols were used for
evaluation (17). The parameter
estimation and assessment were performed as described above.
CAG/CCTA
Standard techniques were used for performing
CAG/CCTA. A visual quantitative scoring system was used to evaluate
stenosis, which was defined as luminal diameter narrowing in one or
more epicardial coronary arteries or major branches by ≥50%. A
cutoff value of 50% was used, as this amount was previously
indicated to be prognostic of stenosis (18).
Statistical analysis
SPSS 22.0 (IBM Corp.) and GraphPad Prism 5 (GraphPad
Software, Inc.) were used for the statistical analyses. Values are
expressed as percentages and frequencies or as the mean ± standard
error of the mean. Student's unpaired two-tailed t-test and the
χ2 test were used to analyze differences between groups.
A two-tailed P<0.05 was considered to indicate a statistically
significant difference.
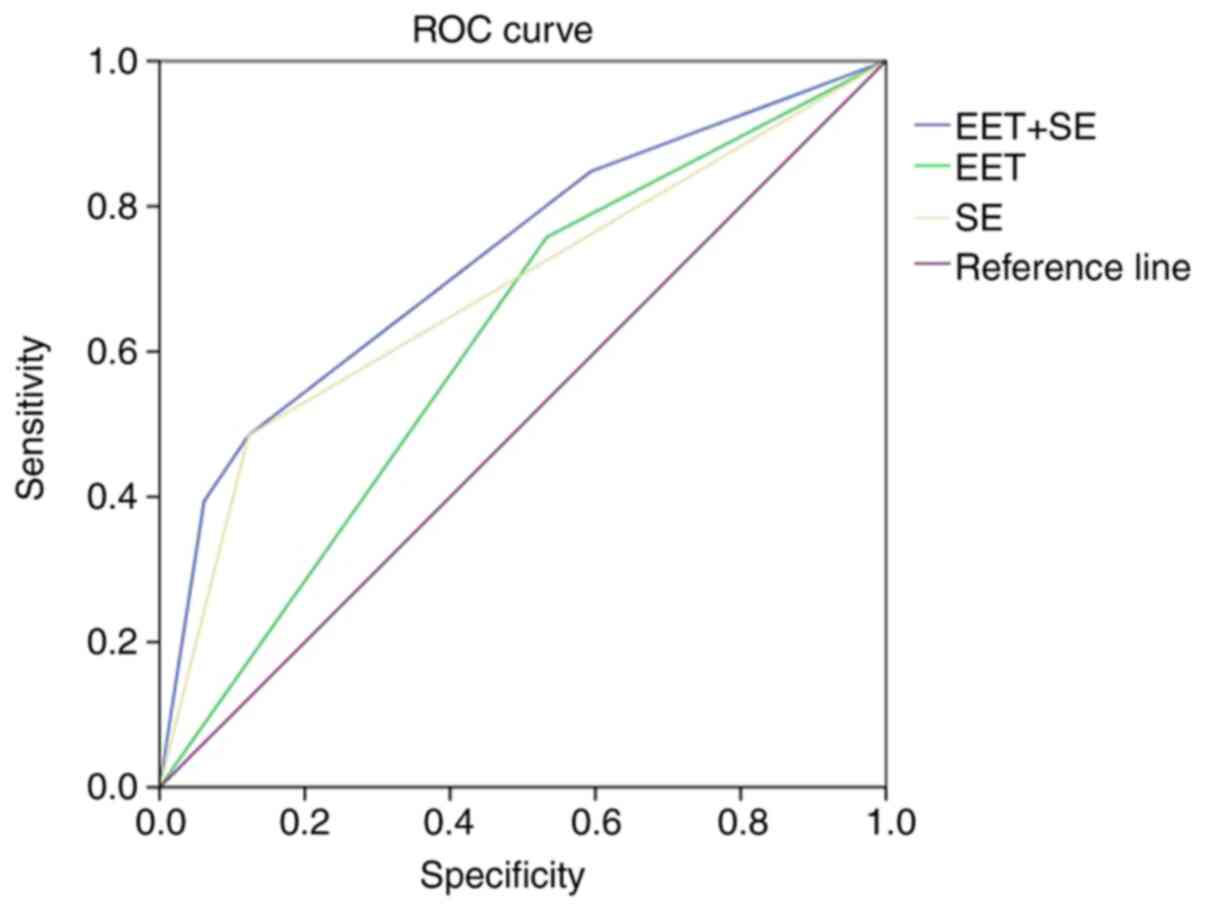
Receiver operating characteristic curve (ROC)
analysis was used to calculate the specificity and sensitivity in
the combined diagnosis of the SE+EET group or of the EET/SE groups
following binary logistic regression analysis and combined factor
calculation. The following equations were used: PPV=(true
positives)/(true positives + false positives); NPV=(true
negatives)/(true negatives + false negatives).
Results
Study population
Between August 2018 and August 2019, 278 inpatients
or outpatients were enrolled from the Cardiology Department of The
First Affiliated Hospital of Nanjing Medical University (Nanjing,
China). All of them were suspected to have MI. CAG or CCTA was used
for the diagnosis of MI according to the assessment criteria
described above. All patients underwent EET and SE and the baseline
characteristics were not significantly different. In the MI and the
non-MI groups, the mean age was 61.6±1.05 and 60.5±0.62 years,
respectively. Other baseline comparison analyses included the HR,
SBP, DBP, HTN, diabetes, syncope, dyspnea, chest pain, ejection
fraction (EF) and fractional shortening (FS). The demographic and
clinicopathological characteristics of the patients are provided in
Table I.
 | Table IClinical characteristics of the study
subjects. |
Table I
Clinical characteristics of the study
subjects.
| Parameter | MI (n=66) | Non-MI (n=121) | P-value |
|---|
| Age (years) | 61.6±1.05 | 60.5±0.62 | 0.21 |
| Sex
(male/female) | 39/27 | 96/116 | 0.05 |
| HR (bpm) | 73.6±0.64 | 75.1±1.29 | 0.29 |
| SBP (mmHg) | 130.8±0.79 | 132.1±1.39 | 0.42 |
| DBP (mmHg) | 75.0±0.77 | 72.3±1.24 | 0.08 |
| SaO2
(%) | 97.8±0.12 | 98.0±0.15 | 0.19 |
| Diabetes | 18(27) | 36(17) | 0.07 |
| HTN | 52(79) | 101(48) | <0.001 |
| Syncope | 2(3) | 8(4) | 0.78 |
| Dyspnea | 12(18) | 20(9) | 0.05 |
| Chest pain | 10(15) | 19(9) | 0.15 |
| EF (%) | 62.3±0.41 | 64.3±0.18 | <0.001 |
| FS (%) | 29.4±0.31 | 30.6±0.16 | <0.001 |
Diagnostic efficiency
Following EET, SE and SE+EET, positive patients and
patients with typical cardiovascular symptoms underwent CAG
according to the diagnostic guidelines of CAD. In this group,
patients who underwent CCTA were also included. The PPV and NPV for
initial EET were 30.7 and 46.9%, respectively (P<0.001). These
values were used for the prediction of flow-limiting disease by
angiography. The PPV and NPV values for the initial SE were 55.2
and 82.2%, respectively (P<0.001). Significant improvements were
observed in the PPV and NPV values using the combination of EET and
SE for diagnosis (66.7 and 89.6%, respectively; P<0.001;
Table II). The sensitivity and
specificity (95% CI) were also evaluated in each group (Table II). In summary, the combination of
EET and SE for diagnosis had particularly good sensitivity and/or
specificity. ROC curves were used to further assess the diagnostic
accuracy of the EET/SE and EET+SE combination (Fig. 1). The areas under the ROC curves
(AUCs) are presented in Table
III. The results indicated an excellent AUC for differentiating
between EET, SE and their combination (EET+SE). The AUC values for
EET/SE and EET+SE were 0.612/0.681 (0.5-0.7, low prediction effect)
and 0.728 (0.70-0.85, standard prediction effect), respectively.
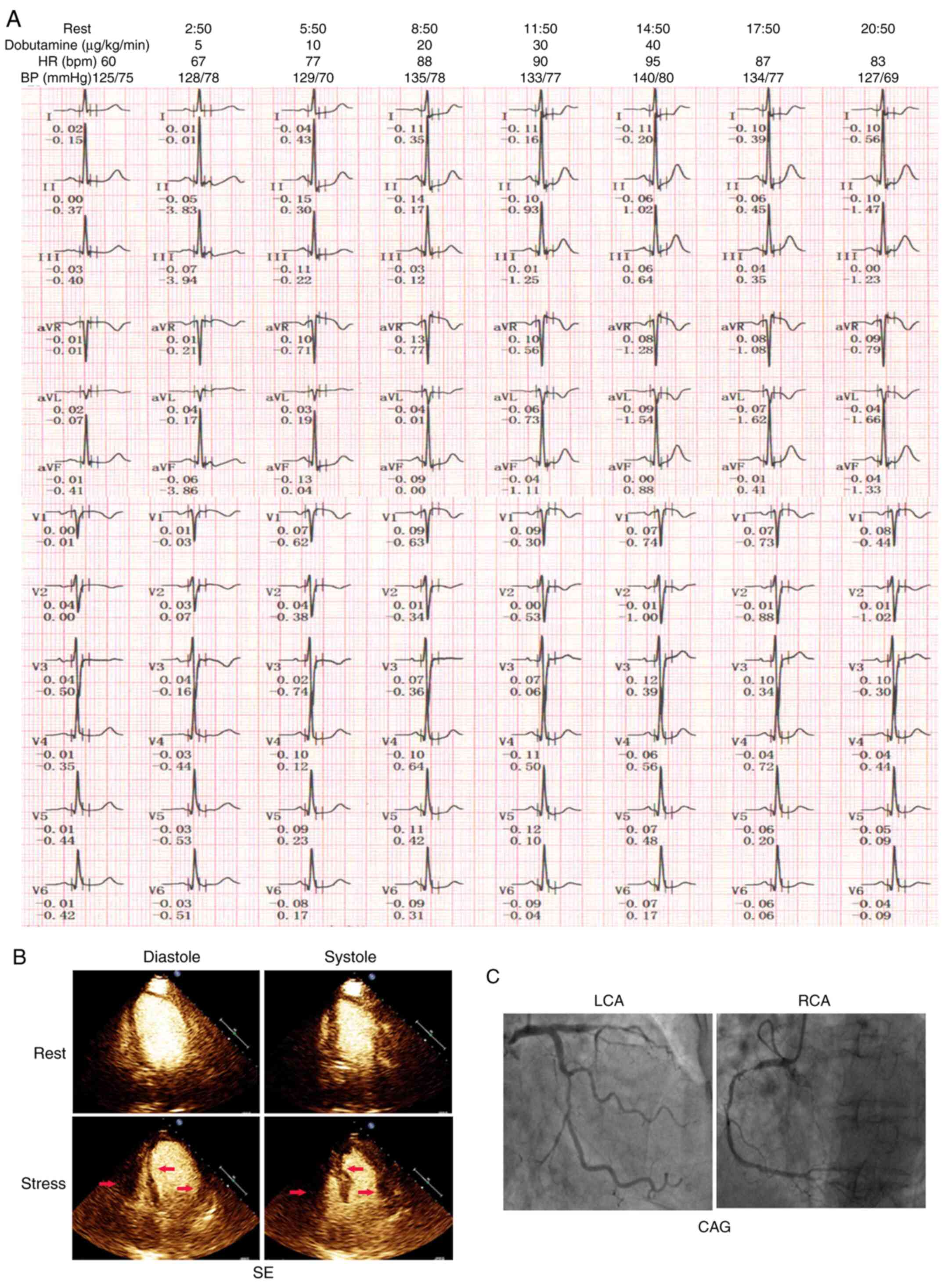
Images for a representative case with the application of the
diagnostic combination are presented in Fig. 2. A markedly positive EET and
dobutamine-induced SE were observed in a 77-year-old female
patient. Positive ST-segment changes were observed in the ECG and
were reflected in the apical 4-chamber frame of the WMA of the
ventricular septum, as well as in the lateral wall of the left and
right ventricles.
 | Table IIPatient number and diagnostic value of
EET/SE/EET+SE in the MI/non-MI groups. |
Table II
Patient number and diagnostic value of
EET/SE/EET+SE in the MI/non-MI groups.
| A, Patients
stratified (n) |
|---|
| Group | EET(+) | EET(-) | SE(+) | SE(-) | EET+SE(+) | EET+SE(-) |
|---|
| MI | 50 | 16 | 32 | 34 | 26 | 10 |
| Non-MI | 113 | 99 | 26 | 186 | 13 | 86 |
| B, Diagnostic
value |
| Modality | Sensitivity, % (95%
CI) | Specificity, % (95%
CI) | PPV (%) | NPV (%) |
| EET | 75.758 (65-86) | 46.919 (40-54) | 30.675 | 46.919 |
| SE | 48.485 (36-61) | 87.736 (83-92) | 55.172 | 82.199 |
| EET+SE | 72.222 (57-88) | 86.869 (80-94) | 66.667 | 89.583 |
 | Table IIIParameters from the ROC curve
analysis. |
Table III
Parameters from the ROC curve
analysis.
| Modality | AUC (95% CI) | P-value |
|---|
| EET | 0.612
(0.54-0.69) | <0.001 |
| SE | 0.681
(0.60-0.76) | <0.001 |
| EET+SE | 0.728
(0.65-0.80) | <0.001 |
Discussion
Interventional technology has provided a novel
perspective on CAD diagnosis and therapy. In the last 30 years, a
high number of patients with CAD or MI have been successfully
treated due to the progress made in CAG and PCI (1,2).
However, the difficulty encountered during the operation and the
patients' unwillingness to accept the procedure have limited the
prevalence of these methods in primary medical care and in general
hospitals. Several studies confirmed that noninvasive tests, such
as electrocardiography, echocardiography, myocardial perfusion
imaging (MPI), cardiac magnetic resonance imaging (CMR), EET, SE
and CCTA provide additional diagnostic value for CAD (19). A review from the Mayo Clinic
reported that SE provided an excellent NPV in diagnosing CAD in
females without a prior history of ischemic heart disease (7). Various studies illustrated that EET
was a useful test for excluding CAD in suspicious patients
(20). The stress test provided a
physiological mimic both in male and female patients and an easy
dynamic monitoring process (21).
To the best of our knowledge, the present study was the first to
describe the combined use of EET+SE in the diagnosis of MI and
compared it with that of EET or SE.
In the present study, the treadmill test and Bruce
protocol or dobutamine infusion were used to mimic the stress
status in the patients (6). EET or
SE is a common method used to exclude MI and a high NPV is
particularly valuable for screening patients with a low
cardiovascular risk (19). To
analyze the predicted sensitivity and specificity of EET and SE,
the results were verified by CAG/CCTA. The baseline parameters were
compared to eliminate marked bias. Previous studies demonstrated
that the predicted data of the SE were superior to those of EET and
several follow-up studies provided optimal diagnostic accuracy and
prognostic value in the SE group (22). Accordingly, the present study
provided novel insight into the diagnosis of MI by EET+SE combined.
These results may open new avenues of research into the improvement
of the diagnostic efficiency of noninvasive MI diagnosis. The
present results indicated that the PPV and NPV were 30.675 and
46.919%, respectively (P<0.001) for EET and 55.172 and 82.199%,
respectively (P<0.001) for SE. However, a significant
improvement in the diagnostic accuracy of MI was obtained when
using EET+SE combined with a PPV and NPV of 66.667 and 89.583%,
respectively (P<0.001). Similar to the NPV/PPV, the sensitivity
and specificity were superior with the EET+SE method compared to
those of either EET or SE alone. Furthermore, superior statistical
power was provided by the ROC curve for the EET+SE method. This
initial observation suggested the usefulness of combined EET+SE for
the diagnosis of patients with suspected MI, and the sex
differences would not influence the results. Therefore, the
traditional stress test analysis using the EET or SE requires
further development, which may enhance its diagnostic value. In the
clinic, the original stress test such as the treadmill or bicycle
protocol has been used to exclude MI in potential cases (7,22). The
first step was to perform a differential diagnosis of ischemia in
patients with a low risk of CAD or those with ischemic symptoms. In
both outpatients and inpatients, the total or average costs were
significantly reduced and the hospitalization time was reduced
(13). Previous studies have
reported that compared with CCTA/MPI/CAG, the lack of radiation
exposure is an important consideration for pregnant females or
those at a high risk of breast cancer (23). Due to its excellent NPV, the
combination of the EET and SE represents an efficient and low-cost
choice for cardiologists to exclude MI.
In previous studies, EET or SE was proven beneficial
for predicting coronary artery stenosis in the heart (6,17).
Accordingly, CAG is considered a hallmark for MI diagnosis and
prediction of artery stenosis (18). Subsequently, intravascular
ultrasound/optical coherence tomography/CMR (coronary flow reserve)
and other invasive examinations were used to accurately analyze
stenosis of arteries based on CAG (24). These highly accurate examinations
focused on microangiopathy or mesangiopathy, respectively. However,
the 2020 European Society of Cardiology guidelines have pointed out
that non-invasive coronary heart disease examinations are
particularly valuable in low-risk patients, whereas SE and EET are
particularly recommended as common examination methods (2). The unbalanced allocation of medical
resources, resistance to invasive surgery, avoidance of radiation
exposure and the reliability of results have led to the wide
acceptance and use of CCTA for coronary ischemia examination. The
study assessed SE/SEET by using CAG/CCTA or CAG as the gold
standard, which is more in line with the ratio of detection methods
used in the clinic. Structural or functional disorders result in
flow limitations that reflect cardiovascular symptoms. However,
coronary slow flow (CSF) without coronary artery stenosis was
detected in patients with partial typical angina presenting at
emergency departments (25). These
patients exhibited vascular endothelial dysfunction or vasospasm
(26). In a previous study, EET or
SE was also used as a functional test to predict MI and CSF
(27). However, it was indicated
that the comparatively lower diagnostic efficiency in EET or SE
limited its application in the detection of these diseases.
The present study demonstrated that the combination
of EET+SE produced outstanding PPV and ROC values in the diagnosis
of MI. It may provide MI detection with improved sensitivity in
medical facilities that lack intravascular imaging devices. In a
large meta-analysis evaluating the diagnostic accuracy of
dobutamine-induced SE, the sensitivity for stenosis detection in
the left circumflex coronary artery (55%) was lower than that in
the left anterior descending (72%) and right coronary arteries
(76%) (28). Of note, the study
further indicated higher sensitivity values in detecting
three-artery disease (92%) in comparison with one-artery disease
(74%) and two-artery disease (86%) (28). These results suggested that the
combined EET-associated ST-segment changes and the SE-associated
WMA analysis provided an improvement in the detection of artery
diseases thanks to the dual-localized detection method. The
combined SE/EET test may improve the accuracy of diagnosis, notably
in terms of the NPV. It may effectively improve the detection
ability of ECG ischemic abnormality examinations in pregnant
females, tumor patients and low-risk CAD groups and reduce
complications, the duration of hospital stay and medical
expenses.
In brief, the present study demonstrated that SE or
EET were useful for diagnosing MI in potential patients. The
results of the present study confirmed that the combined analysis
improved the accuracy of the prediction and diagnosis of MI. This
high diagnostic efficiency may provide cardiologists with novel
insight into the differential diagnosis/prediction of MI.
The present study has certain limitations. First, it
was a single-center study. In addition, the sample size was limited
and 3 cardiologists performed EET and SE. Both workload and
dobutamine infusion were used as stress protocols. The present
study also lacked prognostic factor analysis for post-PCI patients.
Subsequently, CCTA/CAG examinations were selected based on the
cardiologist's experience and the EET/SE results.
In conclusion, EET and SE are important noninvasive
examination methods that may be used for MI diagnosis. According to
the present results, superior diagnostic efficiency for MI was
noted when the combined EET+SE method was used; however, it may
still be inferior to the gold standard. This methodological
improvement may provide novel insight for cardiologists to develop
strategies for MI exclusion and prediction. Therefore, the
prevalence of combined EET+SE analysis may be used to optimize MI
diagnosis and reduce the financial costs used for cardiac exams
either in primary medical care or in general hospitals.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81670328, 81441011
and 81570328).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
NZ, XF and DL designed the study. NZ, QH, JW, JZ and
DL performed the experiments. Data were collated by NZ and QH and
the results were discussed by all authors. NZ, QH and JW prepared
the figures. NZ, XF and QH wrote the first draft of the manuscript.
All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
This research was approved by the Committee of
Ethics in Human Research at The First Affiliated Hospital of
Nanjing Medical University (Nanjing, China; no. SRFA-048). All of
the volunteers were aware of the risks and provided written
informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Boateng S and Sanborn T: Acute myocardial
infarction. Dis Mon. 59:83–96. 2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Collet JP, Thiele H, Barbato E, Barthélémy
O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T,
Folliguet T, et al: 2020 ESC Guidelines for the management of acute
coronary syndromes in patients presenting without persistent
ST-segment elevation. Eur Heart J: ehaa575, 2020 doi:
10.1093/eurheartj/ehaa575 (Epub ahead of print).
|
|
3
|
Lu L, Liu M, Sun R, Zheng Y and Zhang P:
Myocardial infarction: Symptoms and treatments. Cell Biochem
Biophys. 72:865–867. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Engstrøm T, Kelbæk H, Helqvist S, Høfsten
DE, Kløvgaard L, Clemmensen P, Holmvang L, Jørgensen E, Pedersen F,
Saunamaki K, et al: Effect of ischemic postconditioning during
primary percutaneous coronary intervention for patients with
ST-Segment elevation myocardial infarction: A randomized clinical
trial. JAMA Cardiol. 2:490–497. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Chai SC, Teo HK, Lee PS, Kam CJW and Tong
KL: Prognostic impact of stress echocardiography with discordant
stress electrocardiography in patients with suspected coronary
artery disease. Singapore Med J. 61:142–148. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sicari R and Cortigiani L: The clinical
use of stress echocardiography in ischemic heart disease.
Cardiovasc Ultrasound. 15(7)2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Padang R and Pellikka PA: The role of
stress echocardiography in the evaluation of coronary artery
disease and myocardial ischemia in women. J Nucl Cardiol.
23:1023–1035. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Prejean SP, Din M, Reyes E and Hage FG:
Guidelines in review: Comparison of the 2014 AHA/ACC guideline for
the management of patients with non-ST-elevation acute coronary
syndromes and the 2015 ESC guidelines for the management of acute
coronary syndromes in patients presenting without persistent
ST-segment elevation. J Nucl Cardiol. 25:769–776. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Douglas PS, Hoffmann U, Patel MR, Mark DB,
Al-Khalidi HR, Cavanaugh B, Cole J, Dolor RJ, Fordyce CB, Huang M,
et al: Outcomes of anatomical versus functional testing for
coronary artery disease. N Engl J Med. 372:1291–1300.
2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Radulescu D, Pripon S, Parv A, Duncea C
and Gulei I: Electrocardiography and conventional radiology
accuracy compared to echocardiography in evaluating left
ventricular remodelling patterns in hypertensive patients.
Panminerva Med. 50:97–103. 2008.PubMed/NCBI
|
|
11
|
Pellikka PA, Nagueh SF, Elhendy AA, Kuehl
CA and Sawada SG: American Society of Echocardiography. American
Society of Echocardiography recommendations for performance,
interpretation, and application of stress echocardiography. J Am
Soc Echocardiogr. 20:1021–1041. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Calvino-Santos R, Estevez-Loureiro R,
Peteiro-Vazquez J, Salgado-Fernandez J, Rodriguez-Vilela A,
Franco-Gutierrez R, Bouzas-Mosquera A, Rodríguez-Fernández JÁ,
Mesías-Prego A, González-Juanatey C, et al: Angiographically Guided
Complete Revascularization versus selective stress
echocardiography-guided revascularization in patients with
ST-Segment-elevation myocardial infarction and multivessel disease:
The CROSS-AMI randomized clinical trial. Circ Cardiovasc Interv.
12(e007924)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Gurunathan S, Zacharias K, Akhtar M, Ahmed
A, Mehta V, Karogiannis N, Vamvakidou A, Khattar R and Senior R:
Cost-effectiveness of a management strategy based on exercise
echocardiography versus exercise electrocardiography in patients
presenting with suspected angina during long term follow up: A
randomized study. Int J Cardiol. 259:1–7. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Demola P, Crocamo A, Ceriello L, Botti A,
Cremonini I, Pattoneri P, Corradi D, Visioli F, Goldoni M and Pelà
G: Hemodynamic and ECG responses to stress test in early adolescent
athletes explain ethnicity-related cardiac differences. Int J
Cardiol. 289:125–130. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Recommendations for cardiac chamber
quantification by echocardiography in adults: An update from the
american society of echocardiography and the European Association
of, Cardiovascular imaging. Eur Heart J Cardiovasc Imaging.
17(412)2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Brown AS, Calachanis M, Evdoridis C,
Hancock J, Wild S, Prasan A, Nihoyannopoulos P and Monaghan MJ:
Sonovue improves endocardial border detection and variability in
assessing wall motion score and ejection fraction during stress
echocardiography. Ir J Med Sci. 173:13–17. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Glancy DL and Patterson CM: Exercise
electrocardiography. J La State Med Soc. 155:26–35. 2003.PubMed/NCBI
|
|
18
|
Fihn SD, Blankenship JC, Alexander KP,
Bittl JA, Byrne JG, Fletcher BJ, Fonarow GC, Lange RA, Levine GN,
Maddox TM, et al: 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of
the guideline for the diagnosis and management of patients with
stable ischemic heart disease: A report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines, and the American Association for Thoracic Surgery,
Preventive Cardiovascular Nurses Association, Society for
Cardiovascular Angiography and Interventions, and Society of
Thoracic Surgeons. J Am Coll Cardiol. 64:1929–1949. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mordi IR, Badar AA, Irving RJ, Weir-McCall
JR, Houston JG and Lang CC: Efficacy of noninvasive cardiac imaging
tests in diagnosis and management of stable coronary artery
disease. Vasc Health Risk Manag. 13:427–437. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Beri N, Dang P, Bhat A, Venugopal S and
Amsterdam EA: Usefulness of excellent functional capacity in men
and women with ischemic exercise electrocardiography to predict a
negative stress imaging test and very low late mortality. Am J
Cardiol. 124:661–665. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ermolao A, Gasperetti A, Rigon A, Patti A,
Battista F, Frigo AC, Duregon F, Zaccaria M, Bergamin M and
Neunhaeuserer D: Comparison of cardiovascular screening guidelines
for middle-aged/older adults. Scand J Med Sci Sports. 29:1375–1382.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rachwan RJ, Mshelbwala FS, Dardari Z and
Batal O: False-positive stress echocardiograms: Predictors and
prognostic relevance. Int J Cardiol. 296:157–163. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Little MP, Schaeffer ML, Reulen RC,
Abramson DH, Stovall M, Weathers R, de Vathaire F, Diallo I, Seddon
JM, Hawkins MM, et al: Breast cancer risk after radiotherapy for
heritable and non-heritable retinoblastoma: A US-UK study. Br J
Cancer. 110:2623–2632. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Eshtehardi P, McDaniel MC, Dhawan SS,
Binongo JN, Krishnan SK, Golub L, Corban MT, Raggi P, Quyyumi AA
and Samady H: Effect of intensive atorvastatin therapy on coronary
atherosclerosis progression, composition, arterial remodeling, and
microvascular function. J Invasive Cardiol. 24:522–529.
2012.PubMed/NCBI
|
|
25
|
Watanabe Y, Sakakura K, Taniguchi Y,
Yamamoto K, Wada H, Momomura SI and Fujita H: Determinants of slow
flow in percutaneous coronary intervention to the culprit lesion of
Non-ST elevation myocardial infarction. Int Heart J. 59:1237–1245.
2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mehta HH, Morris M, Fischman DL, Finley JJ
IV, Ruggiero N, Walinsky P, McCarey M and Savage MP: The
spontaneous coronary slow-flow phenomenon: Reversal by
intracoronary nicardipine. J Invasive Cardiol. 31:42–45.
2019.PubMed/NCBI
|
|
27
|
Tsetskhladze E and Khintibidze I:
Retrospective study of evaluation of patients with st elevation
myocardial infarction and intact coronary arteries. Evaluation of
treatment approaches; outcome and prognosis. Georgian Med News.
48–52. 2017.PubMed/NCBI
|
|
28
|
Geleijnse ML, Fioretti PM and Roelandt JR:
Methodology, feasibility, safety and diagnostic accuracy of
dobutamine stress echocardiography. J Am Coll Cardiol. 30:595–606.
1997.PubMed/NCBI View Article : Google Scholar
|