Introduction
Parapelvic renal cysts are renal cystic lesions that
most often occur adjacent to the renal collecting system (1). The majority of parapelvic renal cysts
are asymptomatic and found incidentally, but occasionally these
lesions are discovered because of pain, occult blood in the urine,
pyelonephritis, hypertension or renal dysfunction. It is generally
accepted that the treatment of parapelvic cysts is more difficult
than that of simple renal cysts (2). Traditional treatments of parapelvic
renal cysts include a period of observation, puncture, drainage of
the percutaneous renal cyst under ultrasonography and laparoscopic
renal cyst decortication (3). It
has been discovered that laparoscopic decortication of parapelvic
cysts requires advanced surgical skills because of the complexity
of the cysts and their proximity to the renal hilar structures and
the collecting system. The percutaneous approach is a safe and
effective method for treating peripherally located simple renal
cysts but carries a risk of damage to renal hilar structures and
the collecting system for parapelvic cysts (2). With the development of technology, the
advantages of flexible ureteroscopy have become more apparent in
the treatment of parapelvic cysts (4,5).
Parapelvic cysts are characterized by their complexity and
proximity to the renal hilar structures (2,6).
Endoscopic surgery avoids the risk of damage to the renal hilar
structures, and complicated surgical skills are not required to
perform laparoscopic approaches. Novel technology devices for laser
vaporization have been recently reported, and these devices have
been used in prostatectomy (7,8).
Technological development in laser vaporization has resulted in
higher-powered lasers, such as the 1470-nm diode laser. Water and
haemoglobin easily absorb the 1470-nm diode laser, and it is
thought to possess good haemostatic properties and high tissue
vaporization (7). The present study
applied laser devices at 1470-nm diode wavelengths to patients with
parapelvic renal cysts to evaluate the potential role of 1470-nm
diode laser vaporization of parapelvic renal cysts. The results
revealed that this may be used as a novel alternative choice for
the treatment of parapelvic renal cysts.
Materials and methods
Patients
A total of 65 patients charged into the First
Affiliated Hospital of Huzhou Teacher's University (Huzhou, China)
from June 2016 to December 2018 (37 males and 28 females; 55.6±13.6
years old) with parapelvic renal cysts were included in the current
retrospective study from January 2016 to June 2019. All patients
underwent renal enhanced CT and multi-planar reconstruction CT
urography before surgery to observe the relationship between renal
cysts and the renal pelvis. If the renal cysts were closely
adjacent to the renal pelvis in a horizontal position, the coronal
position and the sagittal position, and the adjacent width was
>10 mm in at least one position, the cyst was defined as a
parapelvic renal cyst. A total of 9 renal cysts were adjacent to
the renal collecting system and protruded from the surface of the
kidney. The inclusion criteria used for including patient data was
as follows: i) Recurrent or persistent pain without improvement
following conservative treatment; ii) repeated urinary tract
infection combined with or without renal calculi, without an
increase after conservative treatment; iii) renal cysts suggested
on CT imaging, with normal renal function or mild-to-moderate
lesions (preoperative blood pressure was controlled at <160/100
mmHg, Fasting blood glucose was controlled at <10 mmol/l and
postprandial blood glucose at <12 mmol/l); iv) renal cystic
diameter >4 cm; v) blood pressure and glucose controlled within
the normal range; and vi) Bosniak classification of CT imaging
grades I and II (9). The exclusion
criteria was as follows: i) History of the renal tumour and
nephrapostasis; ii severe cardiac, hepatic, pulmonary and brain
dysfunction, without tolerance to general anaesthesia; iii) Bosniak
classification of CT imaging grades III and IV (9); or iv) a polycystic kidney. All
clinical experiments and laboratory research were performed
according to protocols that were approved by the ethical committee
the First Affiliated Hospital of Huzhou Teacher's University, and
each patient participated after providing written informed
consent.
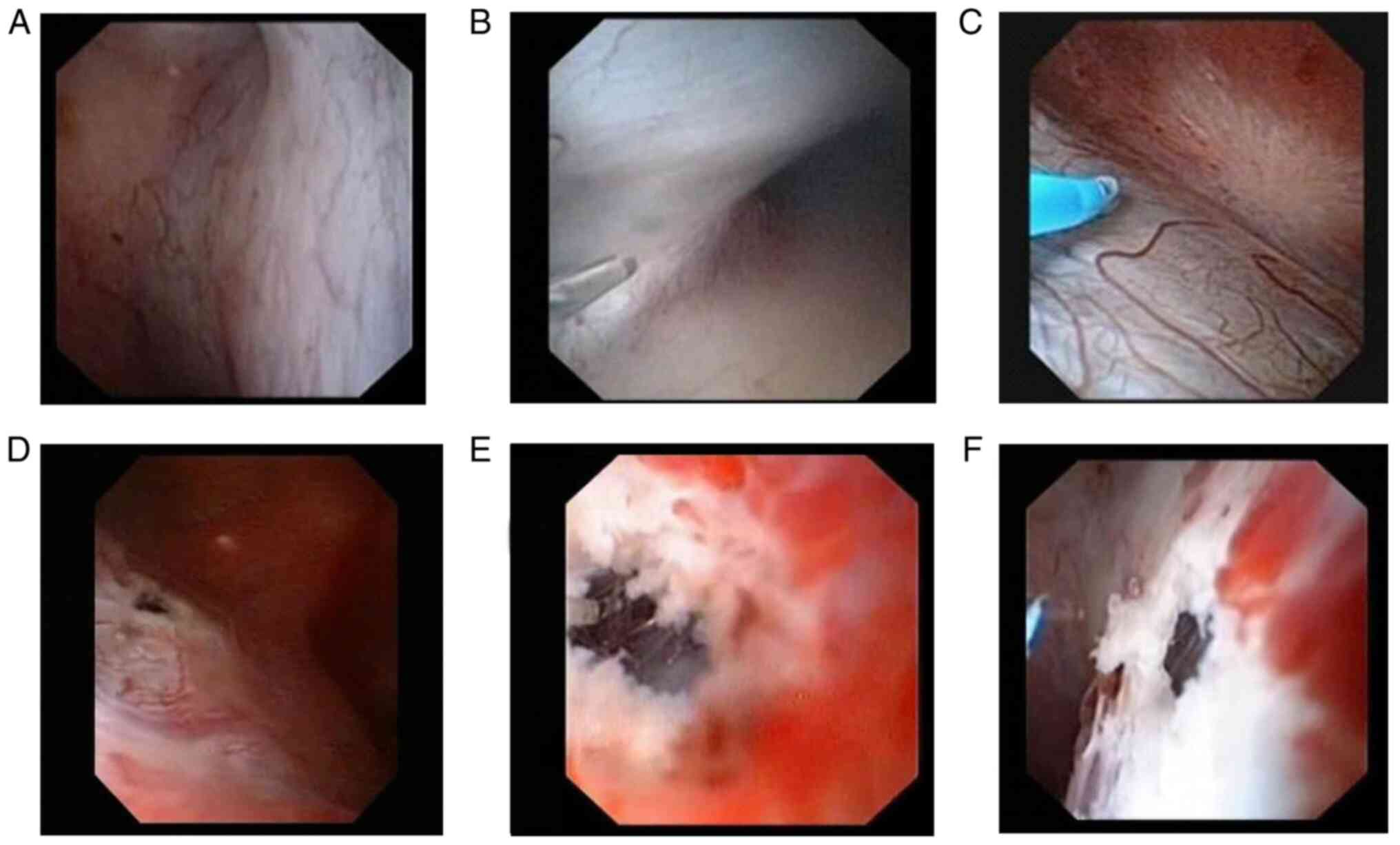
Definition of thin-walled and
thick-walled parapelvic renal cysts
Thin-walled parapelvic renal cysts were considered
when there was no obvious boundary between the renal cyst wall and
the mucosa of the renal pelvis and calyx. The mucosa of the renal
pelvis and calyx was commonly blue translucent or transparent, and
the diameter of the blue translucent or transparent area was >1
cm under the flexible ureteroscope (Fig. 1A-C). Thick-walled parapelvic renal
cysts were considered when a gap existed between the renal cyst
wall and the mucosa of the renal pelvis and calyx. The blue
translucent or transparent area on the mucosa of the renal pelvis
and calyx was commonly non-obvious under the flexible ureteroscope,
or the diameter of the blue translucent or transparent area was
<1 cm (Fig. 1D-F).
Treatment and therapy
A total of 65 patients underwent flexible
ureteroscopic surgery to incise the renal cyst using the holmium
laser or 1470-nm diode laser. The operation of 4 patients was
terminated because the parapelvic cyst could not be located. A
total of 3 patients undergoing holmium laser surgery were switched
to 1470-nm diode laser surgery due to excessive intraoperative
bleeding. The data from 90 renal cysts were collected from 61
patients (Table I), including 43
renal cysts that received holmium laser surgery (holmium laser
group) and 47 renal cysts that received 1470-nm diode laser surgery
(1470-nm diode laser group).
 | Table IPatient characteristics between the
1470-nm and holmium laser group. |
Table I
Patient characteristics between the
1470-nm and holmium laser group.
| Parameters | 1470-nm laser
(n=47) | Holmium laser
(n=43) | P-value |
|---|
| Sex | | | 0.718 |
|
Male | 28 | 24 | |
|
Female | 19 | 19 | |
| Age (years) | 60
(50,64)a | 59
(45,63)a | 0.531 |
| Unilateral/bilateral
cyst | | | 0.771 |
|
Unilateral | 27 | 26 | |
|
Bilateral | 20 | 17 | |
| Simple
cysts/polycystic | | | 0.324 |
|
Simple
cysts | 31 | 24 | |
|
Polycystic | 16 | 19 | |
| Kidney Cyst position,
n (%) | | | 0.997 |
|
Renal
pelvis | 22 | 20 | |
|
Superior
pole | 9 | 9 | |
|
Medium
pole | 9 | 8 | |
|
Inferior
pole | 7 | 6 | |
| Bosniak (I/II) | | | 0.313 |
|
I | 39 | 36 | |
|
II | 8 | 7 | |
| Cyst diameter
(cm) | 5.11±0.65 | 5.14±0.83 | 0.422 |
| Combined disease, n
(%) | | | 0.974 |
|
Kidney
stones | 13 | 11 | |
|
Localized
calyceal water | 8 | 9 | |
|
Hypertension | 16 | 13 | |
|
Diabetes | 7 | 7 | |
|
Coronary
heart disease | 7 | 5 | |
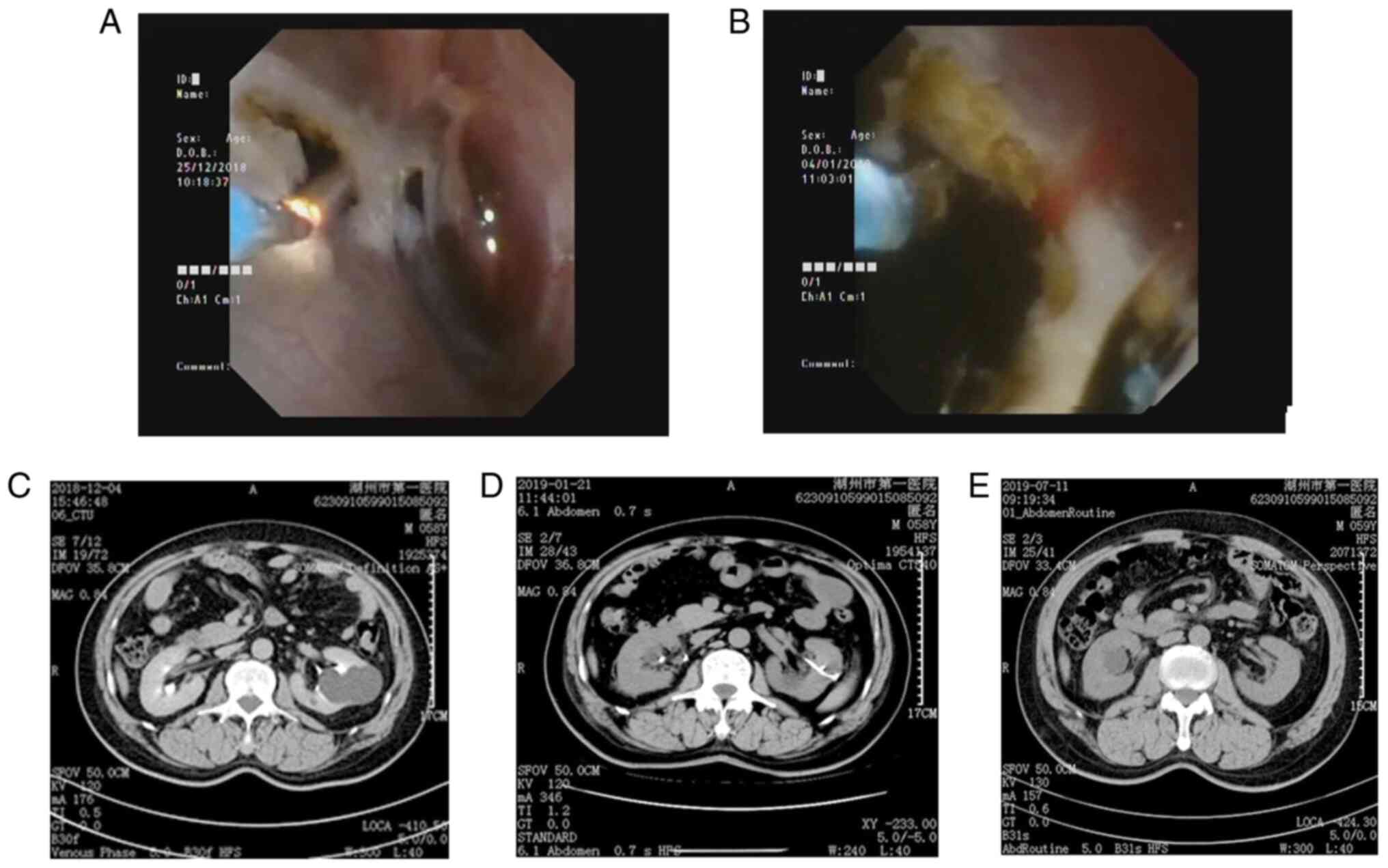
Surgical procedure
A double-J stent was placed in the ureter in the two
groups for 2 weeks preoperatively. After successful general
anaesthesia, the access sheath of a flexible ureteroscope was
advanced to the renal pelvis following the guidewire. A Flexible
Video Ureteroscope (Olympus URF-V, F8.5/9.9) was placed into the
renal pelvis through the access sheath. Preoperative CT with
intraoperative ultrasonography identified the suspicious location
of renal cysts. A translucent blue area was observed on the mucosa
of the renal pelvis and calyx, which was considered the area of
renal cysts adjacent to the renal pelvis and calyx. Ultrasound
images revealed a smoke-like image in the cyst during the laser
incision of the cyst wall. A 200-µm holmium laser fibre (1.0 J, 30
Hz) was used. The power of the laser was 30 W (1.0 J, 30 Hz), and
the incision width of the cyst wall was 1-3 cm in the holmium laser
group and 1470-nm diode laser group (Fig. 2A and B) to ensure that the cyst was completely
connected to the renal pelvis. The flexible ureteroscope was
advanced into the cyst to exclude tumour lesions. The proximal end
of an F6 double-J stent was placed in the cyst under ultrasound
guidance routinely following surgery. The catheter was removed 1-3
days post-surgery, and the F6 double-J stent was removed under a
cystoscope 14-28 days later.
Follow up and evaluation. The success rate of cyst
incision, operation time, intraoperative bleeding rate of the cyst
wall, postoperative infection rate and surgical efficacy were
compared between the two groups. Routine blood counts, renal
function, routine urinalysis and urine culture were re-examined
routinely after surgery. Plain CT scanning was used to evaluate the
change in renal cysts, perirenal effusion and the position of
double-J stenting 3-5 days after surgery. Renal CT was performed in
the preoperative period (Fig. 2C),
1 month after surgery (Fig. 2D) and
6 months after surgery (Fig.
2E).
The following variables were included in the current
study: Age, sex, side of cyst (unilateral or bilateral), cyst size,
location (upper pole, medium pole and inferior pole), simple
cyst/polycystic, Bosniak I/II score, blood loss, pre- and
postoperative cystic diameter, diameter of cyst incision and
complications (such as the presence of hematoma in renal cyst,
fever condition and Lumbago) during and after surgery. The primary
endpoint was efficacy of the treatment. Secondary endpoints were
safety, pain and the resolution of other complications (including
hematoma in renal cyst, fever condition and hematuria). All
patients underwent radiological imaging of the kidneys using
repeated CT 1 and 6 months after surgery.
A nurse in the Department of Urology evaluated pre-
and postoperative lumbar pain scores of the patients. The pain
score was assessed using a 10-point visual analogue scale ranging
from 0 (no pain) to 10 (severe pain). Pain intensity was graded on
a scale of 0 to 3 (slight), 4 to 6 (moderate) and >6 (severe)
(10-11). Patients with a flank pain score
>3, or with a residual pain rating, were categorized as
symptomatic lumbago. Patients with pain scores <3 were recorded
as being asymptomatic.
Statistical analysis
SPSS 19.0 software (IBM Corp.) was used for
statistical analyses. Measurement data are expressed as means ± SD.
Paired t-test was used to compare the pre- and post-operative
curative effects in the same group. Independent sample t-test and
Mann-Whitney U test was used to compare the pre- and post-operative
curative effects between the two groups. Quantitative data are
expressed as numbers (percentage), and the χ2 test or
Fisher's test was used for comparison between these groups.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Characteristics of patients at
baseline
A total of 65 patients underwent flexible
ureteroscopy to cut renal cysts and drain cyst fluid using a
holmium laser or 1470-nm diode laser. A total of 4 patients were
excluded as the parapelvic renal cyst wall was not able to be
located during surgery. Flexible ureteroscopic holmium laser
surgery was switched to flexible ureteroscopic 1470-nm diode laser
surgery in 3 patients due to intraoperative bleeding. Therefore,
the clinical data of 90 independent renal cysts were collected from
61 patients (35 males and 26 females; Table I), including 43 renal cysts that
received holmium laser surgery and 47 renal cysts that received
1470-nm diode laser surgery. There was no significant differences
in the general characteristics between the 2 groups prior to
surgery. A total of 24 cases of independent renal cysts with renal
calculi (0.5-1.5 cm) received holmium laser lithotripsy before
decortication and drainage of renal (data not shown).
Perioperative results
Flexible ureteroscopic decortication and drainage of
parapelvic renal cysts were completed under general anaesthesia in
the two groups. There was no statistical difference in the incision
diameter of the renal cyst during surgery (1.81±0.38 vs. 1.72±0.52
cm; P=0.194; Table II). Notably,
the incision diameter in the 1470-nm diode laser group
significantly exceeded the holmium laser group in the thick-walled
parapelvic renal cysts subgroup [1.70(1.50,1.90) vs.
1.30(1.25,1.70) cm, P=0.007; Table
III].
 | Table IIPerioperative results and
follow-up. |
Table II
Perioperative results and
follow-up.
| Parameters | 1470-nm laser (n
=47) | Holmium laser (n
=43) | P-value |
|---|
| Wall thickness | | | 0.413 |
|
Thin | 20 | 22 | |
|
Thick | 27 | 21 | |
|
Thin
wall+thick wall | 47 | 43 | |
| Diameter of cyst
incision (cm) | 1.81±0.38 | 1.72±0.52 | 0.194 |
| Cyst diameter | | | |
|
Preoperation
(cm) | 5.11±0.65 | 5.14±0.83 | 0.422 |
|
One month
(cm) | 1.59±0.64 | 1.61±0.68 | 0.417 |
|
Six months
(cm) | 1.1 (0.7,1.4) | 1.2 (0.9,1.9) | 0.110 |
| Hematoma in renal
cyst | 0 | 4 | 0.048 |
| Fever
condition | 5 | 5 | 1.000 |
|
Lumbagoa | 9 | 8 | 0.950 |
| Radiologic
failure | | | |
|
At 1
month | 0 | 0 | - |
|
At 6
months | 2 | 5 | 0.252 |
 | Table IIIThe perioperative results in
thin-walled cysts subgroups and thick-walled cysts subgroups of two
lasers and follow-up. |
Table III
The perioperative results in
thin-walled cysts subgroups and thick-walled cysts subgroups of two
lasers and follow-up.
| A, Thin wall |
|---|
| Parameters | 1470-nm laser
(n=47) | Holmium laser
(n=43) | P-value |
|---|
| Number of
cysts | 20 | 22 | |
| Diameter of cyst
incision (cm) | 1.95
(1.53,2.28) | 1.95
(1.5,2.28) | 0.859 |
| Cyst diameter | | | |
|
Preoperation
(cm) | 5.16±0.74 | 5.18±0.89 | 0.473 |
|
One month
(cm) | 1.43±0.67 | 1.46±0.73 | 0.447 |
|
Six months
(cm) | 1.01±0.38 | 1.03±0.53 | 0.454 |
| Hematoma in renal
cyst | 0 | 1 | 1.000 |
| Fever
condition | 0 | 1 | 1.000 |
| Lumbago | 4 | 4 | 1.000 |
| Radiologic
failure | | | |
|
At 1
month | 0 | 0 | - |
|
At 6
months | 0 | 1 | 1.000 |
| B, Thick wall |
| Parameters | 1470-nm laser
(n=47) | Holmium laser
(n=43) | P-value |
| Number of
cysts | 27 | 21 | |
| Diameter of cyst
incision (cm) | 1.70
(1.50,1.90) | 1.30
(1.25,1.70) | 0.007 |
| Cyst diameter | | | |
|
Preoperation
(cm) | 5.07±0.59 | 5.10±0.79 | 0.441 |
|
One month
(cm) | 1.70±0.60 | 1.78±0.59 | 0.332 |
|
Six months
(cm) | 1.21±0.57 | 1.88±0.94 | 0.002 |
| Hematoma in renal
cyst | 0 | 3 | 0.077 |
| Fever
condition | 5 | 4 | 1.000 |
| Lumbago | 5 | 4 | 1.000 |
| Radiologic
failure | | | |
|
At 1
month | 0 | 0 | - |
|
At 6
months | 2 | 5 | 0.252 |
The results at one and six months
after surgery
CT was re-examined, and the double-J stenting was
removed in the holmium laser group and the 1470-nm diode laser
group 1 and 6 months after surgery. It was observed that in
patients with renal cyst recurrence that required clinical
reoperation, the cysts drained were not completely blocked or
unstable at 1 month, and the cysts drained were blocked or stable
at 3 months. The renal cystic diameter of the two groups separately
was markedly reduced 1 and 6 months after surgery. However, there
was no significant difference in the renal cystic diameter between
the two groups 1 month after surgery (1.59±0.64 vs. 1.61±0.68 cm;
P=0.422), and the diameter of the renal cyst had a lower trend in
the 1470-nm diode laser group than the holmium laser group 6 months
after surgery [1.1(0.7,1.4) vs. 1.2(0.9,1.9) cm; P=0.110]. The
cystic diameter 1 month after surgery did not exhibit any
significant difference between thin and thick-walled cyst
subgroups, but a marked increase was noted in the holmium laser
group (1.46±0.73 vs. 1.78±0.59 cm; P=0.064; Table IV). In the thin-walled and
thick-walled cysts subgroups that received the holmium laser
(Table III), 1 case recurred in
the thin-walled cysts subgroup of holmium laser treatment, and 5
cases recurred in the thick-walled cysts subgroup of holmium laser
6 months after surgery. No cases recurred in the thin-walled cysts
subgroup of the 1470-nm diode laser, and only 2 cases recurred in
the thick-walled cysts subgroup of the 1470-nm diode laser 6 months
after surgery. The diameter of the renal cyst was significantly
lower in the thin-walled cysts subgroup that received the holmium
laser than the thick-walled cysts subgroup that received the
holmium laser at 6 months post-surgery (1.03±0.53 vs. 1.88±0.94 cm;
P=0.0004; Table IV).
 | Table IVThe perioperative cyst diameter in
thin-walled cysts subgroups and thick-walled cysts subgroups of two
lasers and follow-up. |
Table IV
The perioperative cyst diameter in
thin-walled cysts subgroups and thick-walled cysts subgroups of two
lasers and follow-up.
| Parameters | Treatment
groups | Thin wall subgroup
diameter (cm) | Thick wall subgroup
diameter (cm) | P-value |
|---|
| A, One month |
|---|
| Cyst
characteristics | 1470-nm laser (n
=20) | 1.43±0.67 | 1.70±0.60 | 0.095 |
| Cyst
characteristics | Holmium laser
(n=22) | 1.46±0.73 | 1.78±0.59 | 0.155 |
| B, Six months |
| Parameters | Treatment
groups | Thin wall subgroup
diameter (cm) | Thick wall subgroup
diameter (cm) | P-value |
| Cyst
characteristics | 1470-nm laser
(n=27) | 1.01±0.38 | 1.21±0.57 | 0.064 |
| Cyst
characteristics | Holmium laser
(n=21) | 1.03±0.53 | 1.88±0.94 | 0.0004 |
No difference in cystic diameter was indicated
between the two subgroups that received the 1470-nm diode laser at
the six-month check-up (thin-walled vs. thick-walled, 1.01±0.38 vs.
1.21±0.57 cm, respectively; P=0.155; Table IV).
The diameter of the renal cyst was decreased in the
1470-nm diode laser group compared with the holmium laser group 6
months after surgery [1.1(0.7,1.4) vs. 1.2(0.9,1.9) cm; P=0.110;
Table II], and no significant
difference in cyst diameter was observed between the thin-walled
cysts subgroups treated with the two lasers 6 months after surgery
(1.01±0.38 vs. 1.03±0.53 cm, P=0.454; Table III).
Discussion
Laparoscopic surgery for renal cysts was first
described in 1992, and this technique is now widely used for
treatment (12). Antegrade
percutaneous ureteroscopic unroofing has also examined in the
treatment of renal cysts in recent years (13). Compared with exogenous renal cysts,
parapelvic renal cysts are more likely to cause symptoms, such as
bleeding and obstruction of the renal collecting system, which
urgently require treatment by urologists (1). It is often difficult for urologists to
treat parapelvic cysts using laparoscopic surgery or percutaneous
ureteroscopic surgery since the cysts may have proximity to the
renal hilar structures and pelvis (14). The surgical path of flexible
ureteroscopic surgery runs closer to parapelvic renal cysts than
the laparoscopic surgery anatomically (14). As this technique is transluminal
naturally and leads to less bleeding, less risk and faster
recovery, it has been favoured by a considerable number of
urologists (2,14-22).
The key to the incision and drainage of parapelvic renal cysts via
flexible ureteroscopy is the accurate location of the cysts. The
present study suggested that the evaluation of cyst positioning
should include ultrasonography, intravenous urography, retrograde
pyelography, CT and an enhanced CT (2,14-20).
A recent Chinese randomized controlled trial confirmed that the
injection of methylene blue into the parapelvic renal cysts reduced
the identification time and operation time of the cysts under a
flexible ureteroscope (21). A
previous study revealed that MPR-CTU combined with a precise
intraoperative ultrasonography-guided flexible ureteroscope exerted
better therapeutic effects (increased the successful rate of
surgery and reduced complications) via easily locating the cystic
wall compared with the flexible ureteroscope technique (5).
Holmium lasers are commonly used for the incision
and drainage of parapelvic renal cysts under a flexible
ureteroscope (5,14,22).
Yu et al (14) used a
holmium laser to incise and drain endogenous symptomatic renal
cystic diseases under a flexible ureteroscope. During the 24-month
postoperative follow-up period, no cysts were detected in 26
patients with parapelvic cysts, and no serious perioperative
complications occurred. A study by Luo et al (16) used a 200-mm laser fibre to treat
renal parapelvic cysts using a flexible ureteroscope. Within the 14
cases used in the aforementioned study, cyst size was reduced by
50% of the previous size in only 1 case, cyst sizes were reduced to
<50% of the previous size in 4 cases and no cysts were detected
in the other 10 cases, after a mean follow-up of 44±17.24 months
(range 24-84). None of the patients exhibited intraoperative
complications. A number of previous studies have used the 200 nm
fiber setting (14,16,17,21,23).
Therefore, the 200 nm fiber was used at the hospital in the current
study. Future studies should compare the two different therapeutic
effects of different settings (365 vs. 200 nm). During the 6 months
of follow-up in the present study, it was revealed that the
recurrence rate was higher in the thick-walled cysts subgroup with
holmium laser incision, and the diameter of thin-walled renal cysts
was significantly lower than thick-walled renal cysts (1.03±0.53
vs. 1.88±0.94 cm; P=0.0004; Table
IV). The present study demonstrated that the holmium laser was
effective for haemostasis of thin-walled renal cysts, but it was
much less effective for the haemostasis of thick-walled renal cysts
under a flexible ureteroscope. Moreover, there was a significant
difference observed between thick/thin walled values combined and
the two treatment techniques (P=0.048; Table II), indicating that the 1470 nm
laser was more effective for haemostasis overall. The current study
also observed that the diameter of the holmium laser incision of
the thin-walled renal cyst was 1.95(1.5,2.28; quantile spacing for
non-normally distributed data) cm, and the diameter of thick-walled
renal cysts was 1.30(1.25,1.70; quantile spacing for non-normally
distributed data) cm. It may be suggested that the surgery is less
favourable due to intraoperative bleeding, which may decrease the
long-term curative effect due to the reduced incision diameter of
cysts.
The 1470-nm diode laser treatment apparatus was a
semiconductor laser, which possesses higher power and provides a
continuous infrared laser. The 1470-nm laser produces little
bleeding and exhibits a good curative effect (7,24). The
1470-nm diode laser is widely used in the treatment of benign
prostatic hyperplasia. To the best of our knowledge, the current
study was the first to use the 1470-nm diode laser in the treatment
of parapelvic renal cysts. According to biological and physical
principles, the higher cell and tissue absorption of the laser
reduces the penetration depth. Compared with the holmium laser, the
1470-nm diode laser is more easily absorbed by haemoglobin and
water, which allows heat to be concentrated in a small piece of
tissue with a penetration depth of 2-3 mm (7). This characteristic may reduce
intraoperative bleeding, which was conducive to expanding the
diameter of the cyst incision, draining of the cystic fluid and
improving the surgical effect.
The results of the present study indicated that the
incision diameter of thick-walled parapelvic renal cysts in the
1470-nm diode laser group was significantly higher compared with
the holmium laser group in the perioperative period. The current
study concluded that the 1470-nm diode laser was significantly
superior to the holmium laser in haemostasis, as the risk of
bleeding was reduced, and the incision diameter of parapelvic renal
cysts was expanded to facilitate the drainage of cystic fluid. The
1470-nm diode laser and the holmium laser exerted equivalent
effects on thick-walled and thin-walled renal cysts 1 month after
surgery. It may be suggested that the placement of double-J
stenting may serve an important role in draining cystic fluid and
preventing cystic atresia within 1 month following surgery. In the
current study, it was observed that in patients with renal cyst
recurrence that required clinical reoperation, the cysts drained
were not completely blocked or unstable at 1 month, and the cysts
drained were blocked or stable at 3 months. The surgical effect of
the 1470-nm diode laser was comparable to the holmium laser in the
thin-walled parapelvic renal cysts subgroup 6 months after surgery.
Therefore, the current study concluded that the thin-walled renal
cyst was not prone to atresia or relapse after the incision.
However, the surgical effect of 1470-nm diode laser was superior to
the holmium laser in the thick-walled parapelvic renal cysts
subgroup 6 months after surgery. Due to the excellent haemostatic
effect of the 1470-nm diode laser, the surgeon could enlarge the
incision diameter of thick-walled parapelvic renal cysts as much as
possible, which made the cyst less prone to atresia and facilitated
cystic fluid drainage. These results indicated that renal cysts
should be open-incised as extensively as possible (2). However, the results of the present
study also indicated that the haemostatic effect of the holmium
laser was poor on thick-walled parapelvic renal cysts in the
clinical procedure. The surgeon reduced the incision diameter of
thick-walled parapelvic renal cysts out of caution in the holmium
laser group, which made the cysts prone to atresia and poor
drainage of cystic fluid and may have led to cyst recurrence.
In the current study, the 1470-nm diode laser was
used to treat parapelvic renal cysts under a flexible ureteroscope.
Compared with the holmium laser, the 1470-nm diode laser exhibited
a number of advantages in the treatment of thick-walled parapelvic
renal cysts, and may be used as an alternative choice for the
treatment of thick-walled parapelvic renal cysts. However, the
1470-nm diode laser was not the optimal treatment in thin-walled
cysts since it is not significantly superior to holmium laser.
Acknowledgements
Not applicable.
Funding
This manuscript or document was supported by the
Natural Science Foundation of Zhejiang Province (grant nos.
LGF18H050001 and LY17H050004), National Natural Science Foundation
of China, (grant no. 81370799), Zhejiang Provincial Medical and
Health Science and Technology Plan Project (platform focus; grant
no. 2016 ZDB 012), and Huzhou Municipal Science and Technology
Bureau (grant no. 2016GY23).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YC contributed to experiment implementation, data
analysis, figure composing and manuscript writing. RW and XS
performed data analysis and manuscript editing. JT, JS, ZF and ZS
were involved with data collection. XJ was involved in project
design and manuscript writing. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
All clinical experiments and laboratory research
were performed according to protocols that were approved by the
ethical committee the First Affiliated Hospital of Huzhou Teacher's
University, and each patient participated after providing written
informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Umemoto Y, Okamura T, Akita H, Yasui T and
Kohri K: Clinical evaluation of parapelvic renal cysts: Do these
represent latent urological malignant disease? Asian Pac J Cancer
Prev. 10:1119–1120. 2009.PubMed/NCBI
|
|
2
|
Basiri A, Hosseini SR, Tousi VN and
Sichani MM: Ureteroscopic management of symptomatic, simple
parapelvic renal cyst. J Endourol. 24:537–540. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kutcher R, Amodio JB and Rosenblatt R:
Uremic renal cystic disease: Value of sonographic screening.
Radiology. 147:833–835. 1983.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Taguchi K, Harper JD, Stoller ML, Duty BD,
Sorensen MD, Sur RL, Usawachintachit M, Tzou DT, Wenzler DL,
Isaacson D, et al: Identifying factors associated with need for
flexible ureteroscope repair: A Western Endourology STone (WEST)
research consortium prospective cohort study. Urolithiasis.
46:559–566. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wang R, Wang N, Tang J, Chen Y and Gao J:
The safety and efficacy of MPR-CTU combined with precise
intraoperative ultrasonography guided flexible ureteroscope in the
treatment of renal cystic disease. Exp Ther Med. 15:283–287.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Camargo AHLA, Cooperberg MR, Ershoff BD,
Rubenstein JN, Meng MV and Stoller ML: Laparoscopic management of
peripelvic renal cysts: University of California, San Francisco,
experience and review of literature. Urology. 65:882–887.
2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhao Y, Liu C, Zhou G, Yu C, Zhang Y and
Ouyang Y: A retrospective evaluation of benign prostatic
hyperplasia treatment by transurethral vaporization using a 1470 nm
laser. Photomed Laser Surg. 31:626–629. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu Z, Zhao Y, Wang X, Song M and Shi B:
Critical reviews of 1470-nm laser vaporization on benign prostatic
hyperplasia. Lasers Med Sci. 33:323–327. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Silverman SG, Pedrosa I, Ellis JH, Hindman
NM, Schieda N, Smith AD, Remer EM, Shinagare AB, Curci NE, Raman
SS, et al: Bosniak classification of cystic renal masses, version
2019: An update proposal and needs assessment. Radiology.
292:475–488. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Breivik EK and Skoglund LA: Comparison of
present pain intensity assessments on horizontally and vertically
oriented visual analogue scales. Methods Find Exp Clin Pharmacol.
20:719–724. 1998.PubMed/NCBI View Article : Google Scholar
|
|
11
|
de Jong AE, Bremer M, Schouten M,
Tuinebreijer WE and Faber AW: Reliability and validity of the pain
observation scale for young children and the visual analogue scale
in children with burns. Burns. 31:198–204. 2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yoder BM and Wolf JS Jr: Long-term outcome
of laparoscopic decortication of peripheral and peripelvic renal
and adrenal cysts. J Urol. 171:583–587. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hu J, Dirie NI, Yang J, Xia D, Lu Y, Yu X
and Wang S: Percutaneous ureteroscopy laser unroofing-a minimally
invasive approach for renal cyst treatment. Sci Rep.
7(14445)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yu W, Zhang D, He X, Zhang Y, Liao G, Deng
G and Jin B: Flexible ureteroscopic management of symptomatic renal
cystic diseases. J Surg Res. 196:118–123. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Li EC, Hou JQ, Yang LB, Yuan HX, Hang LH,
Alagirisamy KK, Li DP and Wang XP: Pure natural orifice
translumenal endoscopic surgery management of simple renal cysts:
2-year follow-up results. J Endourol. 25:75–80. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Luo Q, Zhang X, Chen H, Liu Z, Chen X, Dai
Y and Zhao Z: Treatment of renal parapelvic cysts with a flexible
ureteroscope. Int Urol Nephrol. 46:1903–1908. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Mao X, Xu G, Wu H and Xiao J:
Ureteroscopic management of asymptomatic and symptomatic simple
parapelvic renal cysts. BMC Urol. 15(48)2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mancini V, Cormio L, d'Altilia N,
Benedetto G, Ferrarese P, Balzarro M, Defidio L and Carrieri G:
Retrograde intrarenal surgery for symptomatic renal sinus cysts:
Long-term results and literature review. Urol Int. 101:150–155.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Liaconis H, Pautler SE and Razvi HA:
Ureteroscopic decompression of an unusual uroepithelial cyst using
the holmium: YAG laser. J Endourol. 15:295–297. 2001.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zhao Q, Huang S, Li Q, Xu L, Wei X, Huang
S, Li S and Liu Z: Treatment of parapelvic cyst by internal
drainage technology using ureteroscope and holmium laser. West
Indian Med J. 64:230–235. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wang Z, Zeng X, Chen C, Wang T, Chen R and
Liu J: Methylene blue injection via percutaneous renal cyst
puncture used in flexible ureteroscope for treatment of parapelvic
cysts: A modified method for easily locating cystic wall. Urology.
125:243–247. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Shen J, Chen Y and Wang R: Efficacy and
complication of flexible ureteroscopic holmium laser incision for
simple renal cysts: A retrospective study. J Endourol. 33:881–886.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wen J, Xu G, He G, Wang B, Mao X and Zhang
S: The clinical efficacy and safety of flexible ureteroscopic
treatment for parapelvic renal cyst and secondary renal stone. Urol
J. 17:243–247. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Te AE, Malloy TR, Stein BS, Ulchaker JC,
Nseyo UO, Hai MA and Malek RS: Photoselective vaporization of the
prostate for the treatment of benign prostatic hyperplasia:
12-month results from the first United States multicenter
prospective trial. J Urol. 172:1404–1408. 2004.PubMed/NCBI View Article : Google Scholar
|