Introduction
Third molars have been described as different from
other teeth in the oral cavity. They have the highest rate of
developmental abnormalities and, most importantly, are last in the
eruption sequence (1). Often third
molars are subject to anomalies of eruption, such as inclusion,
retention, impaction, or inclusion decay, affecting the population
in 71% of cases (2).
One of the causes identified by several authors is
the lack of space for the eruption of lower third molar (3).
In 1979, the National Institute of Dental Research
of the USA sponsored a Consensus Development Conference about lower
third molars avulsion. It included workshops that focused on topics
such as the effects of the extraction of third molars on their
growth and development, the timing and technical considerations for
avulsions, prosthetic and periodontal considerations, postoperative
morbidity, and advantages and disadvantages of the extraction of
third molars (4). The indications
confirmed to date for the avulsion of third molars include the
increased frequency of local inflammation, tooth decay or
periodontal damage of the second molar, cystic degeneration of the
pericoronary (follicular) sac, and neuralgia associated with
involvement of the mandibular nerve (5-7).
Third molar extraction is the most frequent
procedure in oral surgery. A descriptive study made of 319 patients
subjected to surgical removal of a third molar in the context of
the Master of Oral Surgery and Implantology of the Barcelona
University Dental School, Barcelona, Spain between July 2004 and
March 2005 evaluated the following parameters: Sex, age, molar,
type of impaction, position according to the classifications of
Pell and Gregory and of Winter, and the reasons justifying
extraction. The study concluded that prophylaxis was the principal
indication of third molar extraction, followed by orthodontic
reasons. Regarding third molars with associated clinical symptoms
or signs, infectious disease, including pericoronitis, was the
pathology most often observed by the oral surgeon, followed by
caries (8). It is worth to note
that in some regions of the world, prophylactic surgical extraction
of third molars is not a common practice (1).
A study measuring the prevalence of disease of
mandibular third molars referred for removal found pericoronitis in
64% of cases, with odds ratio about 22 and 34 times higher for
molars partially covered by soft tissue than for molars completely
covered by soft or bone tissue (9).
Another study analyzed the occurrence of symptoms of unerupted
mandibular third molars, and investigated associated pathologies,
to determine indications for removal of unerupted mandibular third
molars in a Turkish population. The study found that 62.6% of all
unerupted third molars had no symptoms, while 37.4% were associated
with symptoms. The most frequent complaints of the patients were
pain and swelling, and pericoronitis was observed as the most
frequent pathology (10,11). A vertical position predominated
among the third molars with associated pathology (8).
Upon investigation of the relevant literature, to
the best of the authors' knowledge, no study or case presentation
has reported to date paresthesia as a dominant pre-operative
symptom of pericoronitis of third mandibular molars. The sole
article reported an odontogenic paresthesia was a case report from
1986, that describes selective anesthesia of peripheric branches of
the trigeminal nerve, due to an apical lesion on the second right
lower molar (12). On the other
hand, most of the literature on impacted third molars reports
exclusively on postsurgical sensory impairment following extraction
(13,14).
Case presentation
A 64-year old male Caucasian patient presented to
the ambulatory services of the Department of Oral Surgery,
University of Naples Federico II, Italy, complaining of periodic
inflammatory events in the retromolar region of the oral cavity. At
anamnesis, the patient reports about well compensated type II
diabetes mellitus and pharmacologically controlled hypertension
with valsartan/hydrochlorothiazide (Combisartan) 160/12.5 mg, and
amlodipine (Norvasc) 5 mg, 1 capsule daily. The frequency and the
intensity of the main clinical symptoms suggested the disodontiasis
of tooth 3.8 but included permanent paraesthesia of the left
hemi-lip, which was accentuated during inflammatory episodes. As a
result, the quality of life of the patient was severely
affected.
Upon clinical and radiological investigation, the
following diagnosis was established: Severe, generalized
periodontitis stage IV-grade C; Kennedy class II with one
modification in the mandible; subtotal maxillary edentation; severe
caries on lower left first premolar, lower right second premolar,
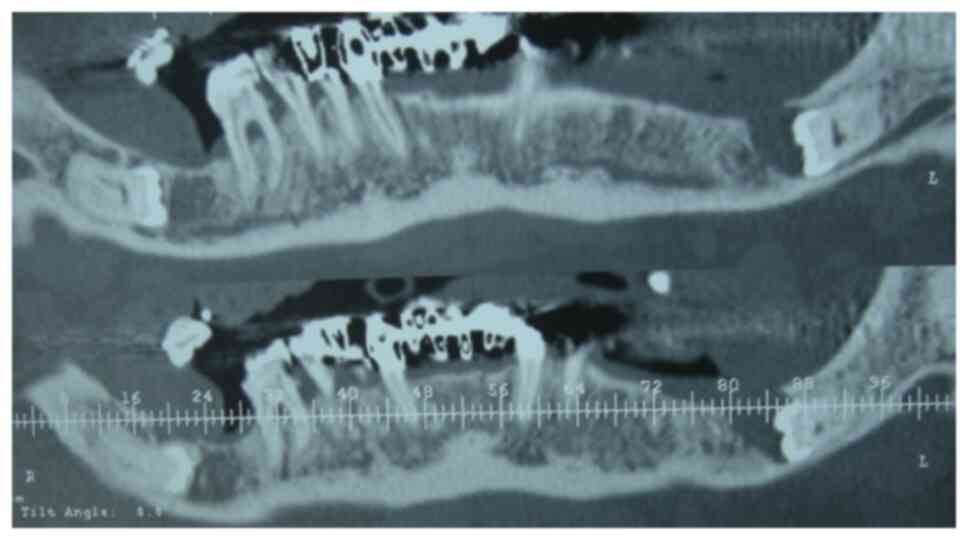
and first molar. The examination of the panoramic radiograph
revealed the inclusion of both third lower molars, both in the
horizontal position and in apparent contiguity with the mandibular
canal (Fig. 1). On the computed
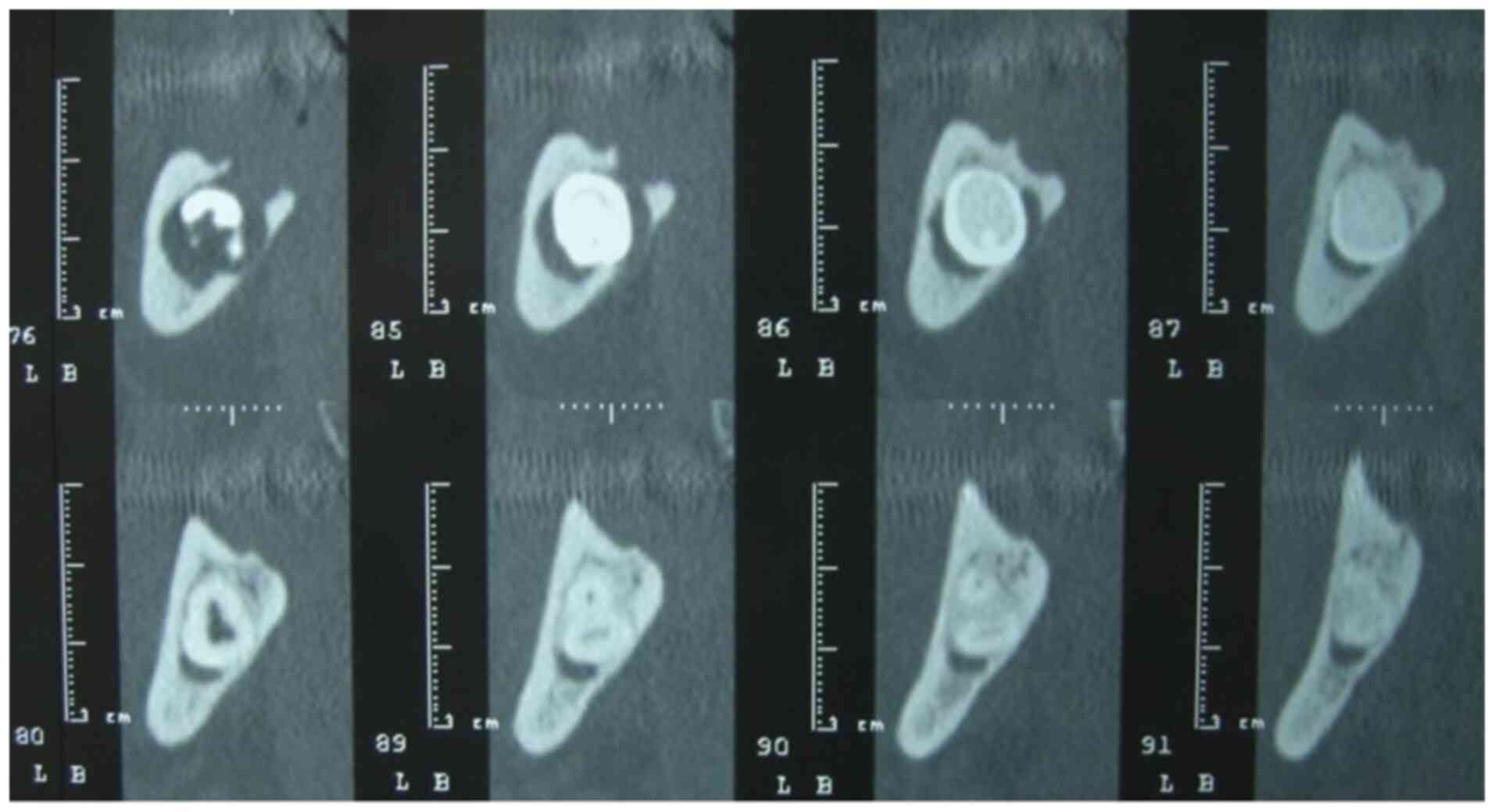
tomography (CT) sections pertaining to the molar's crown, the
interruption of the white lines and a compression of the mandibular
canal lumen by the impacted molar's crown was visible (Fig. 2). The CT examination confirmed that
the lower left third molar had two fused roots, which had
relationships of contiguity with the mandibular canal (Fig. 3). According to the classification of
Pell and Gregory, the lower left third molar was in class 3
position C (15). To assess the
tactile, pain and thermal sensitivity, three types of tests were
carried out to delineate and demarcate the area affected by
paraesthesia at baseline (Fig.
4).
The aim of the test for tactile sensitivity was
conducted to evaluate the large, myelinated fibers Aα, for fast and
slow adaptation. This sensitivity was evaluated by using nylon
sutures, slid in a direction perpendicular to the skin, by asking
the blind-folded patient whether the stimulus evoked or not a
specific sensation. Evaluation of the thermo-nociceptive
sensitivity tested the myelinated fibers Aδ and C. The sensation
was evoked using cotton pellets soaked in ethyl chloride or a
pencil of ice. The pain can be evoked more easily using thin
needles (16). These tests were
performed on those skin areas that already had been previously
outlined by a demographic pencil, as areas in which the patient
reported to have alterations in sensitivity; thus drawing an
initial mapping.
Because of the patient's medical history of diabetes
mellitus type II, antibiotic prophylaxis with amoxicillin 2 g
orally 1 h before surgery was administrated. The surgical procedure
was planned under regional anesthesia, using piezosurgery (Mectron
S.p.A.) to improve the intra-operative and post-operative
sensitivity and the surgical control in the vicinity of important
anatomical structures, such as neurovascular structures.
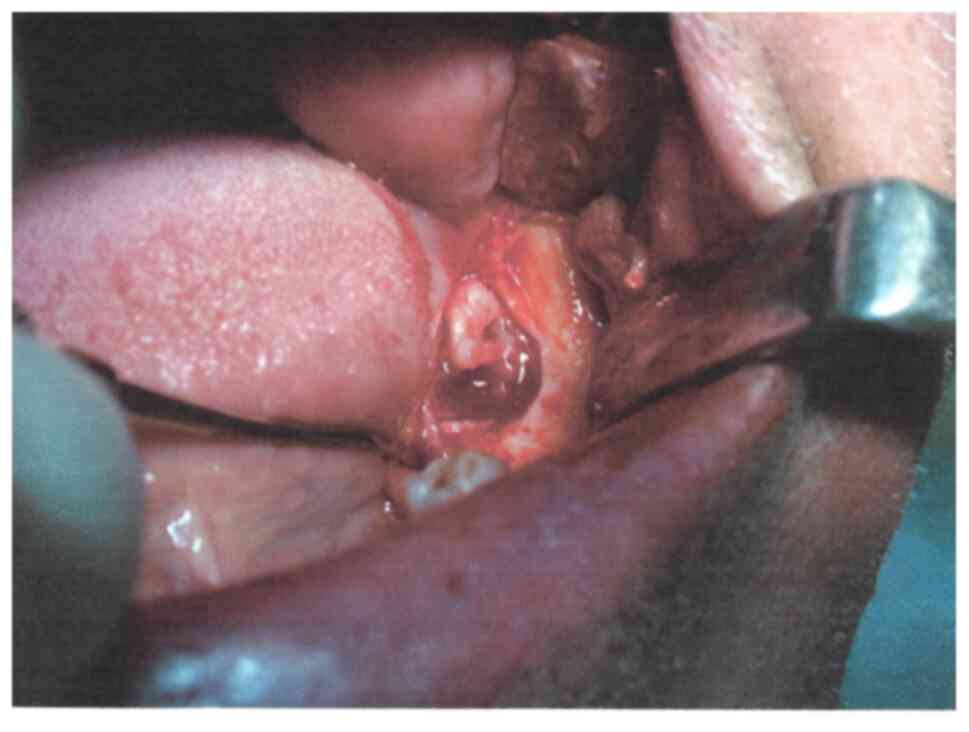
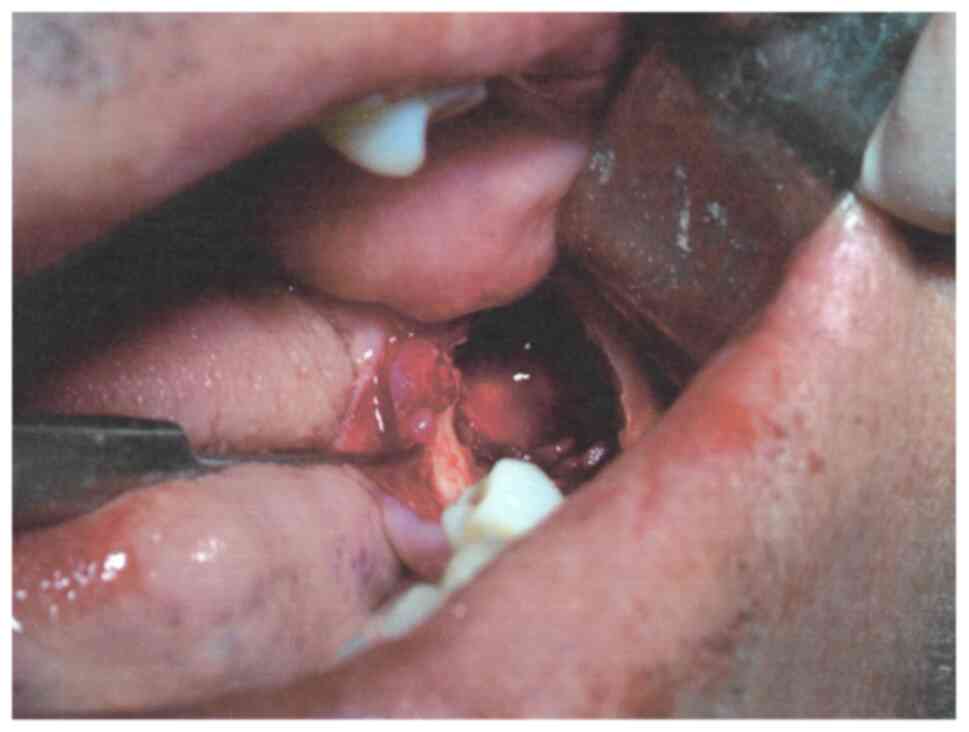
After rinsing for disinfection of the oral cavity
with Betadine (povidone iodine 10%), a mucoperiosteal flap was
created in the retro-molar trigone with release incisions distal to
the second premolar. Once the flap was raised and retracted, the
projection of the horizontally retained molar on the crestal
cortical was established, and an oblongated fenestration of the
bone right above the retained tooth was performed, thus
highlighting the distal aspect of the crown of the included third
molar. Once the fenestration was suitably enlarged, the
pericoronary sac became apparent and was partially removed
(Fig. 5), leaving the crown
exposed.
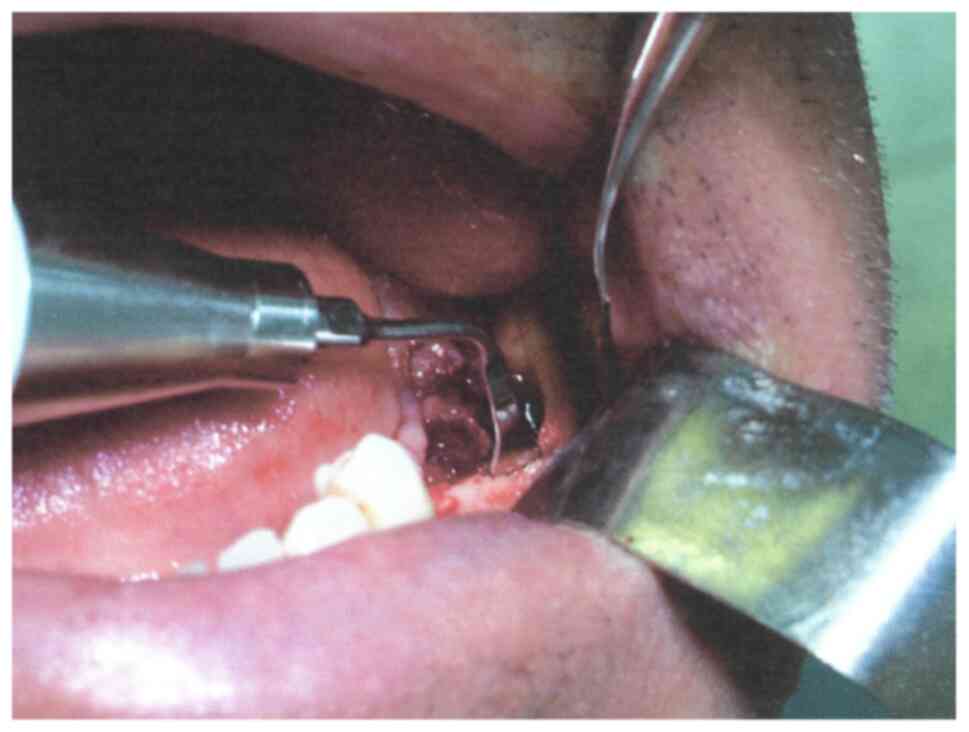
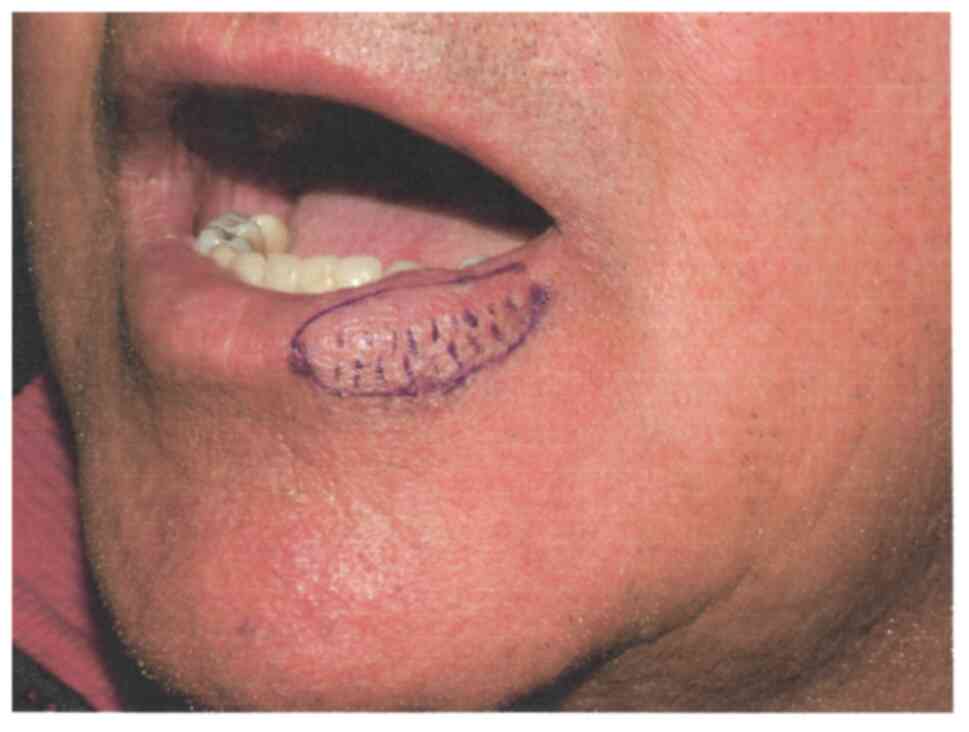
The coronal odontotomy was performed using the
piezoelectric handpiece (insert OT7-Ex1), completing the cut in the
vicinity of the lingual cortical (Fig.
6); a root elevator was used to mobilize and to remove the
coronal fragment. With the aid of two other root elevators (thin
straight and curved), once having established a slight mobility of
the remaining intra-osseous fragment, the latter was advanced along
the long axis of the root trunk, without the need for further
separation, and was removed (Fig.
7). The bone margins of the osseous crypt were regularized
(Fig. 8). The bone cavity was
irrigated with a combination of antibiotic solution 220 mg
ampicillin plus 147 mg sulbactam (Unasyn, Haupt Pharma Latina
S.R.L.), 1 g/3.2 ml solution, and prednisone (Deltacortenesol 25 mg
vials, Bruno Farmaceutici S.p.A). After hemostasis was achieved,
the flap was repositioned and sutured with 3/0 silk sutures
(Med-Silk, Med-Europe).
The healing occurred uneventful. After 7 days, the
stitches were removed. The area of hypoesthesia of the hemi-lip was
significantly reduced even at this early checkup, as evidenced by
the thermo-demographic test (baseline). Further improvement of
tactile and thermal pain was demonstrated in subsequent follow-up
at 1 and 3 months, postoperatively (Fig. 9).
Discussion
An early literature review analyzing the risks and
benefits associated with avulsion of third molars included four
possible different clinical situations: Risk of non-intervention,
risk of intervention, benefit of non-intervention and benefit of
intervention (17). According to
the authors, the risks in the case of non-intervention are crowded
teeth (when supported by the analysis of growth forecasts);
resorption of the adjacent tooth and periodontal problems;
development of infections, cysts, and tumors.
The risks in the case of intervention are minor
transient (paraesthesia, alveolitis, trismus, infection,
hemorrhage, dentoalveolar fracture and dislocation of the
neighboring teeth); less permanent (periodontal damage, damage to
adjacent teeth, temporomandibular joint damages). Other risks
include paresthesia, infection of vital organs, fracture of the jaw
and the maxillary tuberosity.
In our case, the indication for surgery was more
than evident, since the patient complained about periodic
inflammation associated with paraesthesia and a significant impact
on his quality of life. The literature indicates that symptomatic
pericoronitis can have adverse outcomes, compromising the quality
of life and inflicting pain on patients (18), while removal of the third molar
positively influences the quality of life outcomes in those with
minor symptoms of pericoronitis (19).
The surgical approach using the piezoelectric device
has provided more security to avoid further damage to the inferior
alveolar nerve. Not surprisingly, the use of piezosurgery for
removal of retained wisdom teeth has been promoted with the
objective to overcome the limits of the manual or rotary
instruments in bone surgery. The cutting action of the
piezoelectric element is the result of micro-linear ultrasonic
vibrations. The amplitude of only 20-60 µm in the longitudinal
direction enables the control of the surgical field in all
anatomical situations, cutting with extreme precision without
damaging the soft tissues accidentally touched, and without
generating an excess of temperature at the cutting edges.
The potential applications of piezosurgery as a
golden standard in maxillofacial surgery are diverse. The
versatility of the instrument (due to inserts specifically designed
for different purposes) is a further advantage that enables its use
both in extraction surgery and in implant surgery. The so-called
micrometric cutting allows the removal of internal bone lesions
with extreme precision, while avoiding excessive destruction of
bone tissue due to invasive approaches. Various manufacturers have
designed kit inserts for each specific application, that increase
the speed of piezosurgical procedures (20).
In addition, the cavitation effect of the
piezoelectric instruments helps in reducing the osseous bleeding
and maintains a clean bone surface, while promoting effective
cooling to avoid the risks of overheating the bone tissue, when
compared with conventional rotary instruments. Piezoelectric
surgery provides a precise, less aggressive osteotomy compared with
conventional rotatory techniques. However, it has not been found to
significantly reduce perioperative pain and anxiety (21).
The simple extraction of third mandibular molars can
sometimes result in neurological impairment of lingual and inferior
alveolar branches of the trigeminal nerve (22). The incidence varies, as reported in
the literature: The lingual nerve (0.6-8%) (23); the lower alveolar nerve (0.4-5%)
(24).
Several factors can increase the incidence of
complications that can increase the duration and difficulty of the
surgery: The age of the patient (because of the completed root
formation), the reduction of the periodontal space, the higher
density and bone mineralization; the depth of the inclusion; the
procedures that lead to exposure of the lower alveolar nerve.
Results of a study defining the incidence of operative and
postoperative morbidity associated with the removal of impacted
mandibular third molars in patients of various ages showed that
there is a significant increase in surgical morbidity as patients
become older (23). Another study
on 9,574 patients of a wide range of ages who had had 16,127 third
molars removed concluded that removal of mandibular third molar
teeth during the teenage years resulted in decreased operative and
postoperative morbidity (24).
Careful preoperative evaluation and proper planning
using cone beam computed tomography (CBCT) imaging are
indispensable to minimize the risks of intra-operative and
postoperative complications.
The difficulty of extraction (including both
osteotomy and odontotomy techniques) increases in the presence of
deep-situated anatomically elements with an unfavorable morphology,
and with the lack of experience of the operator (25,26).
In the present case, the contiguity with the dental element
represented the highest risk for nerve injury. In surgery of the
lower third molar, the possibility of nerve injuries appears more
frequently with paraesthesia (abnormal sensitivity) or dysesthesia
(abnormal sensitivity associated with burning pain). Similar to our
case, canal deviation and interruption of white lines were
associated with loss of canal cortication on CBCT in a very recent
study, indicating the sensory consequences of a direct contact
between the roots and the mandibular canal which required further
assessment prior to extraction (27). Contrary to another recent study
(28), our case report showed good
reliability of radiographic signs seen on OPG on predicting the
proximity of the third mandibular root with the mandibular canal,
when related to CBCT findings. These complications are considered
profoundly serious both because of the medical and psychological
sequalae, not to mention the possible legal consequences.
The post-operative evolution was characterized by
limited swelling of the cheek, the absence of immediate or delayed
bleeding, while the pain seemed well controlled with proper
medication. After one week, the quality of the wound healing
allowed for removal of the sutures, while the hypoaesthetic area
was already reduced when compared with the preoperative situation,
with considerable subjective benefits for the patient.
In conclusion, hemi-lip paraesthesia is a rare
symptom associated preoperatively with dysodontiasis, which
suggests the necessity of extraction of the retained causal tooth.
The surgical intervention performed with piezoelectric instruments
can be considered when there is a need to prevent damage to
important structures such as the lower mandibular nerve; a
procedure that, in turn, may support the regression of a contingent
paraesthesia.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used/analyzed in this study are
available from the corresponding author, upon reasonable
request.
Authors' contributions
MB, SIS, DR contributed substantially to the
protocol design. AEdL, FS and SP acquired the preoperatory and
intraoperatory clinical data. RG, AR, PS and SS participated in the
post-surgical data acquisition and interpretation and were involved
in drafting the manuscript and revising it critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This case report was approved by the Ethics
Committee of the Federico II University (no. 345/19/19.02.2020
available on request).
Patient consent for publication
A written informed consent was obtained from the
patient for publication of this case report and any accompanying
images. A copy of the written consent is available for review upon
request of the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Adeyemo WL, James O, Ogunlewe MO, Ladeinde
AL, Taiwo OA and Olojede ACO: Indications for extraction of third
molars: A review of 1763 cases. Niger Postgrad Med J. 15:42–46.
2008.PubMed/NCBI
|
|
2
|
Björk A, Jensen E and Palling M:
Mandibular growth and third molar impaction. Acta Odontol Scand.
14:231–272. 1956.
|
|
3
|
Valletta G, Bucci E and Matarasso S:
Odontostomatology (2 Vol.), (Italian). Piccin, Padova, 1997.
|
|
4
|
NIH consensus development conference for
removal of third molars. J Oral Surg. 38:235–236. 1980.PubMed/NCBI
|
|
5
|
Girod SC, Gerlach KI and Krueger G: Cysts
associated with long-standing impacted third molars. Int J Oral
Maxillofac Surg. 22:110–112. 1993.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Regezi JA, Kerr DA and Courtrex RM:
Odontogenic tumors: Analysis of 706 cases. J Oral Surg. 36:771–778.
1978.PubMed/NCBI
|
|
7
|
Guven O, Keskin A and Akal K: The
incidence of cysts and tumors around impacted third molars. Int J
Oral Maxillofac Surg. 29:131–135. 2000.PubMed/NCBI
|
|
8
|
Fuster Torres MA, Gargallo Albiol J,
Berini Aytés L and Gay Escoda C: Evaluation of the indication for
surgical extraction of third molars according to the oral surgeon
and the primary care dentist. Experience in the master of oral
surgery and implantology at barcelona university dental school. Med
Oral Patol Oral Cir Bucal. 13:E499–E504. 2008.PubMed/NCBI
|
|
9
|
Knutsson K, Brehmer B, Lysell L and Rohlin
M: Pathoses associated with mandibular third molars subjected to
removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
82:10–17. 1996.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Doğan N, Orhan K, Günaydin Y, Köymen R,
Okçu K and Uçok O: Unerupted mandibular third molars: Symptoms,
associated pathologies, and indications for removal in a Turkish
population. Quintessence Int. 38:e497–e505. 2007.PubMed/NCBI
|
|
11
|
Punwutikorn J, Waikakul A and Ochareon P:
Symptoms of unerupted mandibular third molars. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod. 87:305–310. 1999.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Barrett AP and Buckley DJ: Selective
anesthesias of peripheral branches of the trigeminal nerve due to
odontogenic infection. Oral Surg Oral Med Oral Pathol. 62:226–228.
1986.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Huang CK, Lui MT and Cheng DH: Use of
panoramic radiography to predict postsurgical sensory impairment
following extraction of impacted mandibular third molars. J Chin
Med Assoc. 78:617–622. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Su N, van Wijk A, Berkhout E, Sanderink G,
De Lange J, Wang H and van der Heijden GJMG: Predictive value of
panoramic radiography for injury of inferior alveolar nerve after
mandibular third molar surgery. J Oral Maxillofac Surg. 75:663–679.
2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pell GJ and Gregory B: Impacted mandibular
third molars: Classification and modified technique for removal.
Dent Dig. 39:330–338. 1933.
|
|
16
|
Maiorana C, Grossi GB, Borgonovo A and
Scarpelli M: Surgical extraction of mandibular third molars.
Edizioni Sinergie, Milano, pp1-137, 2006 (In Italian).
|
|
17
|
Mercier P and Precious D: Risks and
benefits of removal of impacted third molars. A critical review of
the literature. J Oral Maxillofac Surg. 21:17–27. 1992.PubMed/NCBI View Article : Google Scholar
|
|
18
|
McNutt M, Partrick M, Shugars DA, Phillips
C and White RP Jr: Impact of symptomatic pericoronitis on
health-related quality of life. J Oral Maxillofac Surg.
66:2482–2487. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Bradshaw S, Faulk J, Blakey GH, Phillips
C, Phero JA and White RP Jr: Quality of life outcomes after third
molar removal in subjects with minor symptoms of pericoronitis. J
Oral Maxillofac Surg. 70:2494–2500. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Vercellotti T: Piezosurgery: Essentials in
Piezosurgery. Clinical Advantages in Dentistry. Quintessece
Publishing, UK, 2009 (In Italian).
|
|
21
|
Topcu SIT, Palancioglu A, Yaltirik M and
Koray M: Piezoelectric surgery versus conventional osteotomy in
impacted lower third molar extraction: Evaluation of perioperative
anxiety, pain, and paresthesia. J Oral Maxillofac Surg. 77:471–477.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Montagna F, Baldoni M and Piras V: Atlas
of forensic dentistry. Elsevier Masson, 2005 (In Italian).
|
|
23
|
Bruce RA, Frederickson GC and Small GS:
Age of patients and morbidity associated with mandibular third
molar surgery. J Am Dent Assoc. 101:240–245. 1980.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Osborn TP, Frederickson G Jr, Small IA and
Torgerson TS: A prospective study of complications related to
mandibular third molar surgery. J Oral Maxillofac Surg. 43:767–769.
1985.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sedaghatfar M, August MA and Dodson TB:
Panoramic radiographic findings as predictors of inferior alveolar
nerve exposure following third molar extraction. J Oral Maxillofac
Surg. 63:3–7. 2005.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Susarla SM and Dodson TB: Risk factors for
third molar extraction difficulty. J Oral Maxillofac Surg.
62:1363–1371. 2004.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Al Ali S and Jaber M: Correlation of
panoramic high-risk markers with the cone beam CT findings in the
preoperative assessment of the mandibular third molars. J Dent Sci.
15:75–83. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Saha N, Kedarnath NS and Singh M:
Orthopantomography and Cone-beam computed tomography for the
relation of inferior alveolar nerve to the impacted mandibular
third molars. Ann Maxillofac Surg. 9:4–9. 2019.PubMed/NCBI View Article : Google Scholar
|