Introduction
Hair follicle stem cells may serve as seed cells, as
these are easy to obtain and abundantly available (1). Numerous studies have demonstrated the
potential of hair follicle stem cells to differentiate into skin
appendages such as epidermis, hair follicles, nerves and sebaceous
and sweat glands and their ability to regenerate and repair skin
and skin appendages (2-4).
The beneficial effects of hair follicle stem cells on wound healing
has been observed in a variety of reported clinical cases (5,6)
Clinical results indicate the rapid healing of the dermal graft is
due to the differential potential of hair follicle stem cells
(7). Martínez et al
(8) demonstrated that autologous
transplantation of terminal hair follicles induces wound healing in
chronic venous leg ulcers. Moreover, the outer root sheath cells
and dermal papilla (DP) cells of hair follicles may be induced to
differentiate into osteocytes (9),
bone marrow cells (10), adipocytes
(11), myocytes (12) and neurons (13) in vitro. However, it is
currently not possible to specifically isolate and obtain hair
follicle stem cells, due to their hybrid and dynamic cell
components during the growth cycle (14). Currently, micro-isolation, culture
methods and cell surface-specific markers are widely used to
isolate hair follicle stem cells (15). Alkaline phosphatase (ALP), α-smooth
muscle actin (α-SMA), SOX2 and neural cell adhesion molecule (NCAM)
are highly expressed in DP cells, which are used in the
identification of DP cells (16).
Ohyama (17) labelled and purified
hair follicle stem cells using laser-capture microdissection but
failed to obtain monoclonal cells. Furthermore, in a previous
study, these monoclonal cells were partially purified through
screening with surface markers, but their viability and number
decreased (18). Although
microscopic operation is suitable for the purification of cells,
this process is unpersuasive and time-consuming (19). In the present study, hair follicle
cells were cultured via the mouse embryonic fibroblast
(MEF)/keratinocyte serum-free medium (KSF) (MEF/KSF) culture system
in vitro to detect their three-directional induction
potentials. In addition, biological characteristic tests were
performed to demonstrate that the cells were derived from DP cells,
as well as to identify effective and convenient methods that could
be used to culture hair follicle DP cells in vitro.
Materials and methods
Configuration of MEF-conditioned
medium
The current study was approved by the animal
experimental ethical commission of Shanghai Ninth People's Hospital
Affiliated to Shanghai Jiaotong University, School of Medicine
[approval no. (2014)61]. Female mice (age, 12.5 weeks; weight,
30.0-35.0 g) were housed under a 12 h light/dark cycle, at
temperatures of 23˚C and a relative humidity of 40-60% humidity,
with ad libitum access to food and water. Mice with
confirmed pregnancy (Kunming mice; Institute of Laboratory Animal
Science, Chinese Academy of Medical Science of PLA, China) were
used. A total of 30 female mice and 25 fetal mice was used in the
present study. The food and water intake and of animals were
monitored once a day for their well-being. Animals will be
euthanized using an intraperitoneal injection of 200 mg/kg sodium
pentobarbital when they exhibited >20% loss of body weight or
obvious stress, such as grooming their head and forepaws more than
usual, exaggerated escape behaviors, or hiding more than usual. A
Buprenorphine HCl, S.C. injection (0.05 mg/kg) was used 30 mins
prior to surgery to reduce pain for the animals and one pregnant
mouse was housed per cage to prevent fighting between mice.
Anesthesia was performed using 80-100 mg/kg Ketamine and 10 mg/kg
Xylazine. Mouse epidermis was harvested from fetal mice (embryo
13.5-14.5 day) collected from the abdominal cavity of female mice,
and the pregnant mice were terminated. The samples were sheared
into pieces, digested with 0.2% collagenase at 37˚C for 4 h and
resuspended. After filtration with a 200-mesh filter, the samples
were centrifuged at 500 x g for 5 min at room temperature. The
supernatant was discarded and the isolated MEF cells were
resuspended in DMEM containing 10% FBS (Gibco; Thermo Fisher
Scientific, Inc.). The cells were plated in a 10-cm Petri dish to
obtain MEF cells. MEF cells (prior to P4 generation) that had
reached 50% fusion were cultured for an additional 48 h after
changing the DMEM containing 4.5 g/l D-glucose (Gibco; Thermo
Fisher Scientific, Inc.) culture medium. The cell culture medium
was subsequently centrifuged at 200 x g for 5 min and the obtained
supernatant was filtered through a 0.22-mm needle filter. MEF/KSF
medium (Gibco; Thermo Fisher Scientific, Inc.; 500 ml basal medium,
5 ml keratinocyte growth supplement and 5 ml
penicillin/streptomycin solution)-conditioned culture medium was
obtained after mixing MEF-conditioned medium with KSF culture
medium without serum at a ratio of 1:1.
Isolation and culture of mouse hair
follicle stem cells
Dorsal skin samples were obtained from sacrificed
C57 mice (20 female mice; 6 weeks old; 18-20 g; Kunming, China)
housed under a 12 h light/dark cycle, at a temperature of 23˚C and
a humidity 40-60%, with free access to water and food. Uunder
aseptic conditions, samples were cut into pieces. Samples were
subsequently soaked in chloramphenicol for 5 min and cultured
overnight with 0.2% dispase II at 4˚C. Following incubation, the
pieces were dehaired with tweezers and soaked in 0.05% trypsin for
digestion in a water bath on an oscillator at 40˚C for 10 min.
Trypsin was rapidly inactivated using DMEM containing FBS serum,
and a cell suspension was obtained via filtration. The suspension
was centrifuged at 500 x g for 5 min at room temperature and the
supernatant was discarded. Following resuspension and
re-centrifugation at 500 x g for 5 min at room temperature, the
cells were counted using a hemocytometer and randomly distributed
into the following four groups: KSF culture medium group (Group A),
KSF + 10% FBS culture medium group (Group B), DMEM + 10% FBS
culture medium group (Group C) and MEF/KSF-conditioned culture
medium group (Group D). In each group, cells were seeded at a
density of 1x104 cells/cm².
Identification of three-directional
induction conditions for mouse hair follicle stem cells in vitro
Identification of conditions for cell induction and differentiation
toward osteoblasts
Hair follicle stem cells were cultured at 37˚C in an
osteogenic induction medium (100 nmol/l dexamethasone, 50 µmol/l
levorotatory vitamin C and 10 nmol/l β-glycerophosphate; (Gibco;
Thermo Fisher Scientific, Inc.). P1-MEF/KSF-HFSC (hair follicle
stem cells) were subjected to Von Kossa. Cells were fixed using 4%
paraformaldehyde for 30 min at room temperature, washed twice with
PBS and dissolved using 100 mg of Silver nitrate in 2 ml water
(5%). Aliquots (500 µl) were added to each 6-well plate for 20-30
min under UV light and washed twice with water. Samples were then
dissolved in 100 mg sodium thiosulfate in 2 ml water (5%) and added
to each well for 5 min (500 µl). Samples were washed twice. Nuclear
Fast Red staining solution (500 µl) was added, and cells were
incubated for 5 min at room temperature. Samples were washed in
triplicate and then subjected to and alizarin red staining. For
this procedure, cells were fixed with 4% paraformaldehyde for 30
min at room temperature and incubated at room temperature for 15
min, rinsed cells three times with PBS and added to Alizarin red
staining solution (1X Alizarin Red Stain Solution; cat. no.
2003999; EMD Millipore). After incubation at room temperature for
at least 20 min, excess dye was removed, and samples were washed
three times with PBS. Finally, 1-5 ml PBS was added to each well to
prevent cells from drying. Procedures were performed on day 21 of
cell culture, then observed under a light microscope (Leica
Microsystems, Inc.; magnification, x40).
Identification of conditions for cell
induction and differentiation toward adipocytes
Cells were cultured at 37˚C in an adipogenic
induction medium (Gibco; Thermo Fisher Scientific, Inc.) 1 mmol/l
dexamethasone, 10 mg/l of recombinant human insulin, 0.5 mmol/l
IBMX (3-Isobutyl-1-Methylxanthine) and 100 mol/l indomethacin).
P1-MEF/KSF-HFSC were subjected to oil red staining on day 21 of
cell culture.
Identification of conditions for cell
induction and differentiation toward chondroblasts
Cells were cultured at 37˚C in a chondroblast
induction medium (Gibco; Thermo Fisher Scientific, Inc.; 1 mmol/l
sodium pyruvate, 0.1 mmol/l vitamin C, 0.1 nmol/l dexamethasone, 10
ng/ml transferrin growth factor (TGF)-β3, 6.25 µg/ml recombinant
human insulin, 6.25 µg/ml transferrin, 6.25 ng/ml selenious acid,
1.25 ng/ml BSA and 5.35 µg/ml linoleic acid). P0-MEF-HFSC cells
were washed twice with PBS (pH 7.4) for 1 min on day 21 and fixed
with 10% neutral formaldehyde after 30 min. The cells were observed
under a microscope and imaged after the immunohistochemical
detection of type II collagen. Samples were fixed with 4%
paraformaldehyde in PBS for 15 min at room temperature. Aspirated
fixative was rinsed twice in PBS for 5 min each, after which
samples were permeabilized with 0.1-0.5% triton x-100 in PBS for 10
min. Aspirated triton x-100 was rinsed twice in PBS for 5 min each
and incubated with 10% normal goat serum (cat. no. ab7481; Abcam)
in PBS for 30 min at room temperature. Aspirated goat serum was
incubated with sections and collagen type II primary antibodies
(1:200; cat. no. ab188570; Abcam) overnight at 4˚C or 1 h at 37˚C.
Samples were rinsed three times in PBS for 5 min each and incubated
with HRP-conjugated secondary antibodies (1:500; Goat Anti-Rabbit
IgG; cat. no. ab6721; Abcam) for 1 h at 37˚C in the dark. Samples
were subsequently rinsed three times in PBS for 5 min each in the
dark. Samples were incubated with 1 µg/ml DAPI at room temperature
for 5 min and mounted with a drop of mounting medium.
Identification of the biological
characteristics of hair follicle-derived cells from mice
Immunofluorescence staining
The culture medium from P1-MEF-HFSC cells was
discarded, the cells were washed with PBS and fixed with 4%
polyformaldehyde for 15 min at room temperature. Cells were washed
with PBS and treated with 0.3% Triton after 20 min. The samples
were washed in PBS and blocked with 10% goat serum (cat. no.
ab7481; Abcam) for 1 h at room temperature, followed by an
overnight incubation with 1:200 diluted K15, α-SMA primary antibody
(cat. no. ab5694; Abcam) and NCAM monoclonal antibody (cat. no.
ab204446; Abcam) at 4˚C. Cells were washed with PBS and treated
with secondary antibodies [1:500; Goat Anti-Rabbit IgG H&L
(Alexa Fluor® 488); cat. no. ab150077; 1:500; Goat Anti-Rabbit IgG
H&L (TRITC); cat. no. ab7087; Abcam] at 37˚C for 30 min. The
nucleus was stained with DAPI for 10 sec at 37˚C. Images were
acquired using a Leica immunofluorescences microscope (Leica
Microsystems, Inc.; magnification, x40).
Alkaline phosphatase (AKP)
staining
The culture medium was removed and P1-MEF-HFSC cells
were washed with PBS. Cells were embedded in 10% formaldehyde (4˚C)
for 10 min at room temperature. After washing with distilled water,
cells were incubated with a drop of a solution containing 20 mg
naphthol AS-BI phosphate, 0.5 ml DMSO, 50 ml 0.2 mol/l veronal
acetate buffer (pH 9.2) and 0.5 ml 1 mol/l 6-azo-pararosaniline (pH
9-10 adjusted with NaOH) at room temperature for 45 min. The glass
slide was washed with PBS, dried and mounted with glycerin gelatin
(GG1-10X15ML; Sigma-Aldrich; Merck KGaA). Images were obtained with
light microscope (Leica Microsystems, Inc.; magnification,
x40).
Flow cytometry
The cell suspension obtained from P1-MEF/KSF-HFC
cells following digestion was filtered through a 40-µm filter to
remove impurities, followed by centrifugation at 500 g or 5 min.
Flow cytometry staining was subsequently performed (on the ice).
Cell pellets were washed, resuspended in ice-cold
fluorescence-activated cell sorting (FACS) buffer (pH 7.4; 0.1 M
PBS; 1 mM EDTA and 1% BSA) and stained for markers with the
following antibodies: Pan-cytokeratin (CK; 1:1,000; anti-pan
Cytokeratin antibody; cat. no. ab234297; Abcam), α-SMA (1:1,000;
cat. no. ab5694; Abcam) and NCAM (1:1,000; cat. no. ab204446;
Abcam) were added for 30 min at 4˚C. PBS buffer was used for the
control group. The cells were washed twice with PBS and centrifuged
at 500 x g for 5 min at 4˚C. Subsequently, goat anti-rabbit
(1:1,000) antibodies including: (Alexa Fluor® 488; cat.
no. ab150077; Abcam), Goat Anti-Rabbit IgG H&L
(Cy5®; cat. no. ab6564; Abcam) and Goat Anti-Rabbit IgG
(FITC; cat. no. ab6717) were added and incubated for 30 min in the
dark at 4˚C. Samples were rinsed twice with PBS, centrifuged at 500
x g or 5 min at 4˚C, resuspended in PBS containing 2% FBS and
prepared for further analysis. The cells were analyzed using flow
cytometry analysis software Flow Jo7.6.5 (FlowJo LLC).
Reverse transcription PCR
(RT-PCR)
Cell culture media from P1-MEF/KSF-HFC cells and
primary cultures of neuronal cells obtained from mice via digestion
(control group) were discarded and cells were washed with PBS.
Brain samples from mice were used as control group. The samples
were treated with 1 ml TRIzol® (cat. no. 15596018;
Thermo Fisher Scientific, Inc.) reagent on ice, followed by
incubation for 5 min at 4˚C with RNAse for the inactivation of RNA
enzymes (all the materials used for RNA treatment were performed as
previously described (20). The
samples were transferred into 1.5-ml Eppendorf tubes, followed by
the addition of 400 µl chloroform. The mixtures were shaken well
for 15 sec and placed on ice for 15 min. The mixtures were
centrifuged at 12,000 x g at 4˚C for 15 min and 500 µl supernatants
were transferred into new Eppendorf tubes, followed by treatment
with 500 µl ice-cold isopropanol. The samples were mixed, placed on
ice for 10 min, centrifuged at 12,000 x g and 4˚C for 10 min. The
supernatants were discarded and the pellets were treated with 70%
alcohol. The mixtures were centrifuged at 7,500 x g and 4˚C for 10
min. The supernatants were discarded and the residual liquid was
absorbed with filter papers. The pellets were dried for 10 min and
suspended in 20 µl double-distilled water treated with Diethyl pyro
carbonate (cat. no. 4387937; Thermo Fisher Scientific, Inc). The
absorbance values at 260 nm were measured and the concentration of
RNA was adjusted to 1 µg/µl. These samples were stored at
-80˚C.
A total of 2 µg total RNA was used for the reverse
transcription reaction. The reaction conditions were: 2 µl reverse
transcription buffer (10X), 4 µl 25 mM MgCl2, 2 µl 10 mM dNTP, 1 µl
Oligo dT-adaptor primer, 0.5 µl RNA enzyme inhibitor (40 U/µl) and
0.5 µl AMV reverse transcriptase (5 U/µl). The final volume was
measured to 20 µl with water. The RT reaction was performed under
following conditions: 37˚C for 10 min, 42˚C for 1 h, 99˚C for 5 min
and 4˚C for 5 min.
The product (2 µg) was used for PCR amplification of
the target gene fragment. PCR reaction conditions were as follow: 2
µl PCR buffer (10X), 150 µl MgCl2 (25 mM), 0.5 µl 10 mM dNTP, 0.25
µl Taq enzyme (5 U/µl; cat. no. 9012-90-2; Sigma-Aldrich; Merck
KGaA) and 0.3 µl upstream and downstream primers (12.5 pmol/µl).
The primers used were as follows: SOX-2 forward,
5'-GCGGAGTGGAAACTTTTGTCC-3' and reverse,
3'-GGGAAGCGTGTACTTATCCTTCT5'; NCAM forward,
5'-AGAAATCAGCGTTGGAGAGTCC-3' and reverse,
3'-TCGTCATCATTCCACACCACT-5'; α-SMA forward,
5'-CCCAGACATCAGGGAGTAATGG-3' and reverse,
3'-TCTATCGGATACTTCAGCGTCA-5'; β-actin forward,
5'-GTGACGTTGACATCCGTAAAGA-3' and reverse,
3'-GCCGGACTCATCGTACTCC-5', The final volume was measured to 20 µl
with water. The PCR program was as follows: Initial denaturation at
94˚C for 4 min, followed by 35 cycles of degeneration at 94˚C for
30 sec, annealing temperature for 45 sec, 72˚C for 45 sec; followed
by final extension step at 72˚C for 10 min. Electrophoresis
identification was performed with 10 µl PCR products on 1.5%
agarose gel and the remaining PCR products were restored. DNA
marker (5 µl) was loaded in the same gel and used under a UV
transilluminator to visualize the PCR product in the agarose gel.
β-Actin was chosen as the reference gene for control. The results
of PCR were analyzed using FIJI image processing software (version,
-v2.0.0-rc-59/1.51n; National Institutes of Health)
Statistical analysis
All data are presented as the mean ± SD (n=3) and
the statistical analyses were analyzed using the statistical
software Statistical Package for the Social Sciences (SPSS version
19.0; IBM Corp.). An unpaired Student's t-test was applied to
analyze the difference between groups. P<0.05 was considered to
indicate a statistically significant difference.
Results
Growth conditions of adherent cells in
different cultured systems
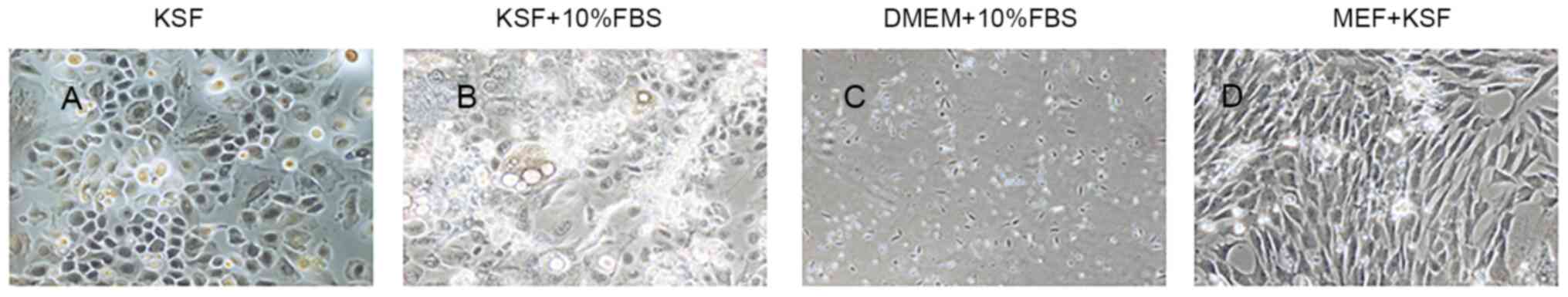
Hair follicle stem cells from the same batch were
distributed and cultured in four different systems. Of these, small
cell clones appeared after 3 days in Group B and Group D, but after
7 days in Group A. Moreover, no small cell clone formation was
observed after incubation of cells in Group C. Adherent cells in
Group A appeared to be typical epidermal-like cells characterized
by small size, close arrangement and a cobblestone-like shape.
(Fig. 1A).
The number of clones for cells from the Group B was
low; however, the growth condition of cells was excellent, as
indicated by the consistent morphology, fusiform and polygonal
appearance and longer cytoplasmic projections. (Fig. 1B).
Cell cloning in Group C was not notable and the cell
growth was decreased. A few cells adhered to the dish in group C
during planting. In addition, the cells died of aging without
obvious cell clone formation (Fig.
1C).
It was indicated that cells in Group D exhibited the
strongest proliferative ability. Adherent cells formed flat
polygons and exhibited aggregative growth. Cell morphologies were
similar to those of hair follicle DP cells and dermal sheath cells
(21). The majority of cell clones
formed from day 3 and these cells had proliferative abilities from
day 5. (Fig. 1D).
Growth and passage condition of hair
follicle-derived cells cultured in MEF-conditioned medium
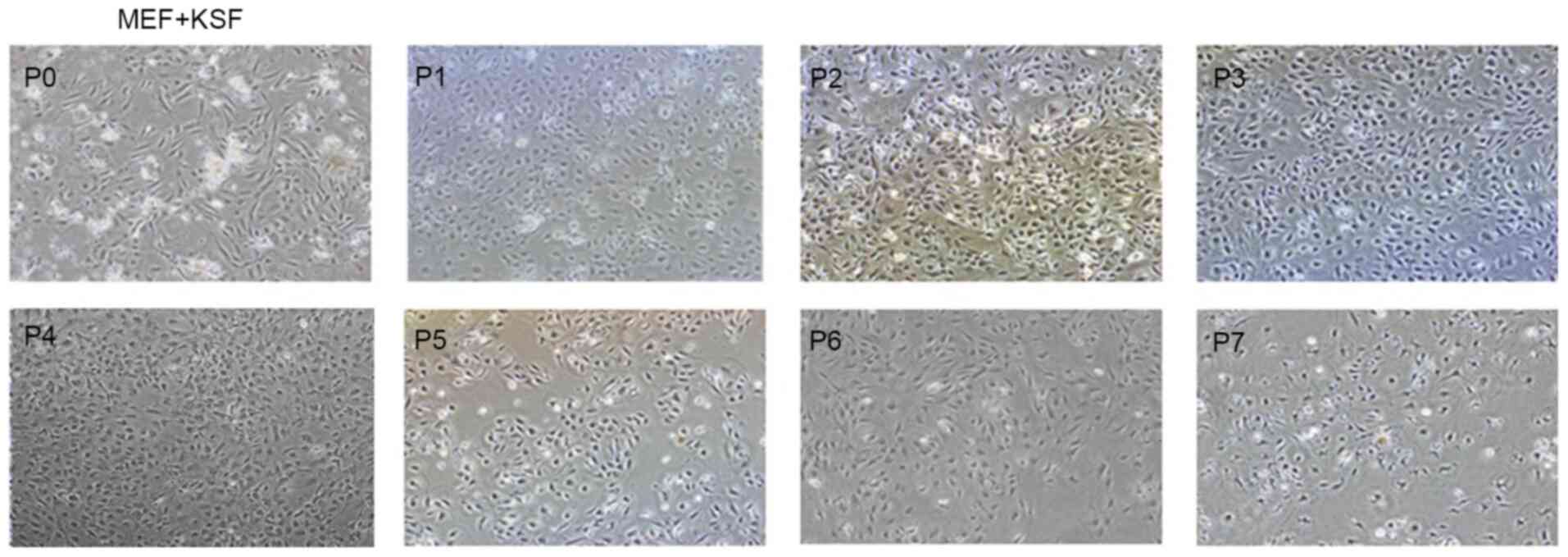
Group D cells exhibited strong proliferative and
formative abilities and the dish was confluent in 5-7 days. These
cells were sub-cultured, and it was indicated that the cells
retained their strong proliferative abilities and were able to
reach their next generation after 3 days. Moreover, cell
proliferation decreased from generation 6 and the cells stopped
proliferating at generation 7 (Fig.
2).
Identification of induction ability of
P1-MEF/KSF-HFSC cells in vitro Identification of the
differentiation potential of osteoblasts
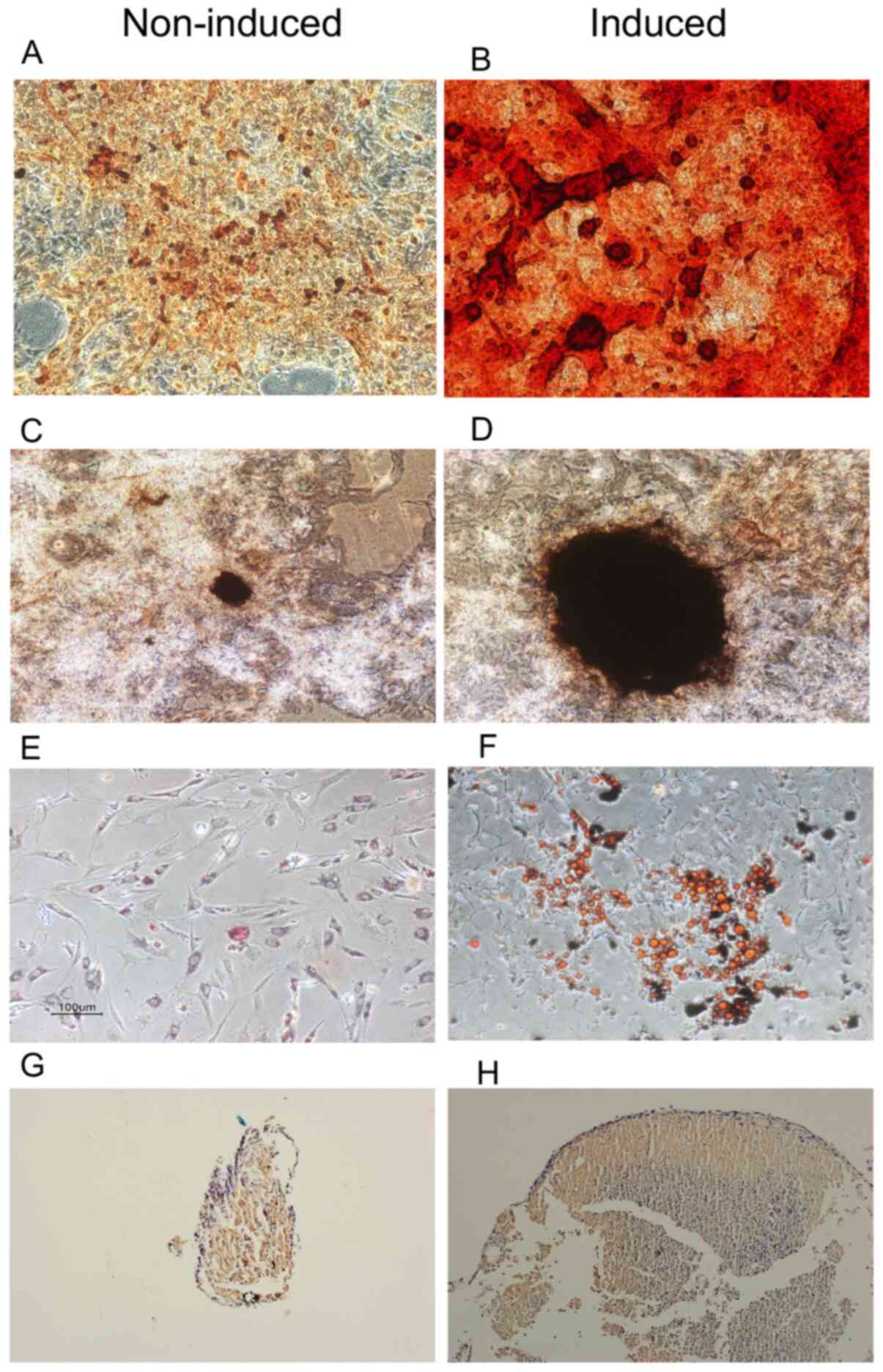
The results of alizarin red staining suggested that
both osteo-induced and non-induced groups exhibited diffused matrix
mineralization, but this was less obvious in the non-induced group.
Compared with the non-induced group, Alizarin red staining
indicated a larger and increased level of black calcium nodules in
the osteo-induced group (Figs. 3A
and B). In addition, von Kossa
staining granules of varying sizes were arranged in groups around
the nucleus in the majority of cells from the lipid-induced group
(Fig. 3C and D).
Identification of the differentiation
potential of lipoblasts
The results also indicated that only a few cells
from the non-induced group exhibited lipoblasts granules on day 21
following oil red O staining (Fig.
3E and F)
Identification of the differentiation
potential of chondroblasts
The non-induced group did not exhibit a stable
pallet structure, and a complicated structure was observed from the
slice. However, a pallet structure was observed in cells from the
chondro-induced group. The pallet slice subjected to
immunohistochemical collagen II staining was stained brown
(Fig. 3G and H).
Identification of MEF-HSFC surface
markers Identification of cell surface markers of primary (P1 and
P2 generation) cells
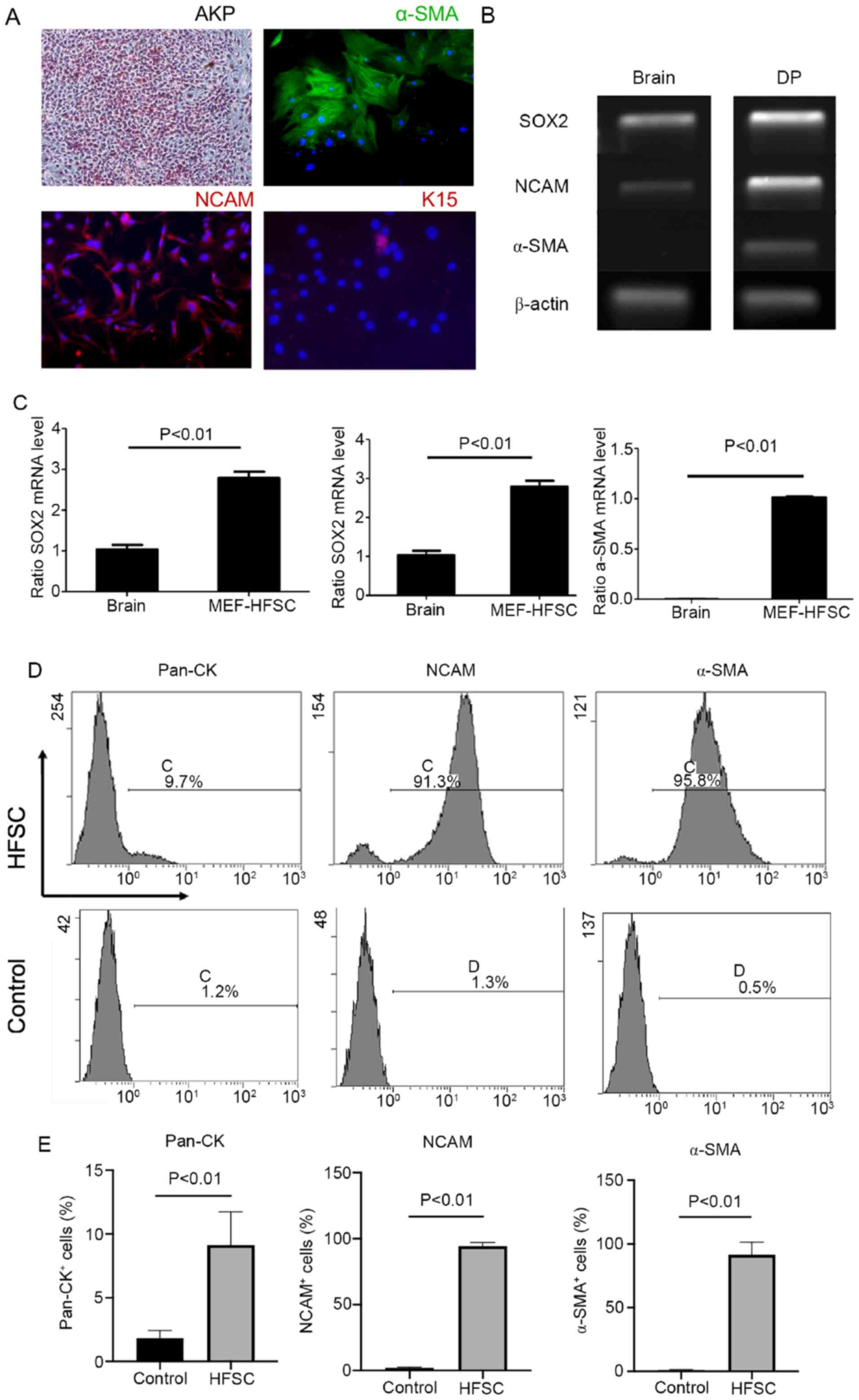
Results from the AKP staining were accurately
observed and imaged. All cells from each generation adhered and
exhibited the expression of AKP, SMA and NCAM (Fig. 4A) except for K15 expression as this
is not observed in cells cultured by MEF medium.
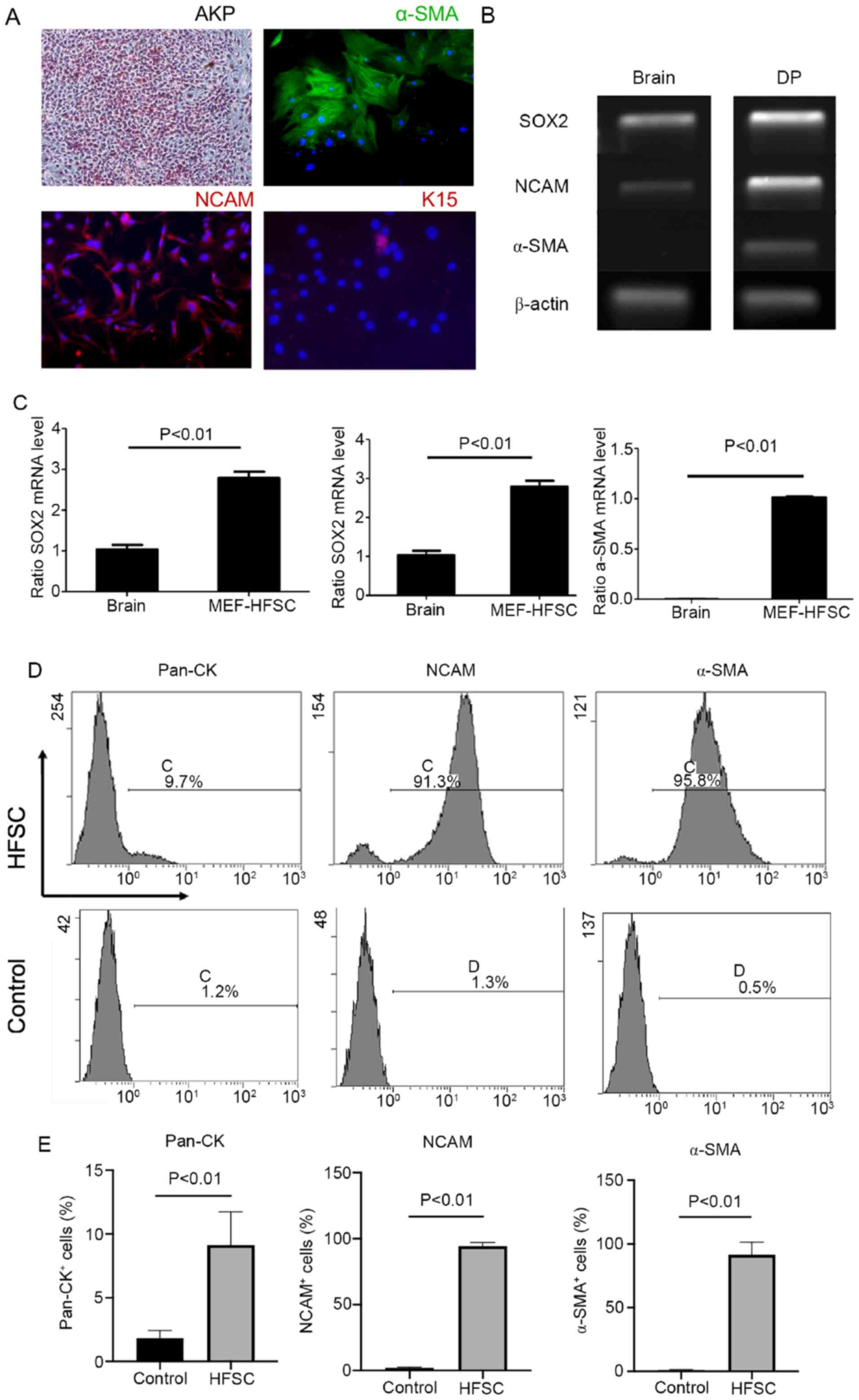 | Figure 4Identification of markers from
MEF-HFSC. Staining for (A) AKP (upper left; magnification, x40),
α-SMA (upper right; magnification, x100), NCAM (lower left;
magnification, x100) and K15 (lower right; magnification, x100).
Immunofluorescence staining. (B and C) reverse transcription-PCR of
SOX2, NCAM and α-SMA from MEF-HFSC. (D and E) Flow cytometry for
pan-CK, NCAM and α-SMA from MEF-HFSC. α-SMA, α-smooth muscle actin;
NCAM, neural cell adhesion molecule; MEF/KSF, mouse embryonic
fibroblast/keratinocyte serum-free medium; AKP, alkaline
phosphatase; pan-CK, pan-cytokeratin. |
Result of RT-PCR
The mRNA expression of SOX-2, NCAM and α-SMA were
significantly higher in cells from the P1 generation compared with
cells from the control group (Fig.
4B and C).
Result of flow cytometry
The flow cytometry results in the HFSC group
suggested that Pan-CK, α-SMA, and NCAM accounted for 9.7, 91.3 and
95.8% of all cells, respectively (Fig.
4D). Quantification of flow cytometry results are presented in
Fig. 4E. The expression of Pan-CK
was only 9.7%, but α-SMA and NCAM levels were significantly
increased.
Discussion
Bone defects are common and may be associated with
trauma, infection, tumor resection and congenital diseases
(22). Bone tissue engineering,
conceptualized in the 1980s, is an emerging method that is used to
repair bone defects (23) and
involves the application of cells, synthetic materials and
cytokines for in vivo tissue regeneration and in
vitro construction (24). Seed
cells have attracted increased attention and mesenchymal stem cells
derived from bone marrow (25),
amniotic fluid (26), umbilical
cord blood (27), adipose tissue
(28), muscles (29), dental pulp (30) and hair follicles are currently being
investigated as seed cells for bone tissue engineering.
Hair follicles containing epithelial and mesenchymal
stem cells, which are useful for cellular research (31,32).
Through a series of cell labelling experiments, Cotsarelis
(18) revealed that a hair follicle
stem cell population may be located in the hair bulb and in the
bulge region of the hair follicle outer root sheath cells. Hair
follicle stem cells were first isolated by extracting hair
follicles from the human scalp and digesting them with pancreatic
enzymes. Moreover, the outer root sheath cells were cultured
through the collagen-coating method used by Kurata et al
(33). However, the known methods
of amplification and purification of DP cells are associated with a
number of different limitations. To address this issue, the present
study aimed to enrich hair follicle-derived mesenchymal stem cell
populations and subject these cells to osteogenic differentiation
for applications in tissue engineering.
KSF follicular epithelium stem cell culture medium
and DMEM+100S mesenchymal stem cell culture medium was used to
culture embryonic stem cells that were used for the growth of hair
follicle-derived stem cells. Human embryonic stem cells have been
successfully cultured via feeder layer isolation and cultivation of
MEF by Thomson et al (34)
in 1998. MEF cells are normally grown as feeder layer cells to
preserve the multi-directional differentiation potential of primary
generation cells in long-term cultures, due to their high
availability, ease of preparation and remarkable effect (35). Furthermore, Chin et al
(36) used MEF cells and
MEF-conditioned medium in 2007 and suggested that pigment
epithelium-derived factor (PEDF), insulin-like growth factor
binding protein (IGFBP)-2, IGFBP-7, monocyte chemoattractant
protein-1 (MCP-1) and interleukin-6 (IL-6) served as growth factors
in MEF-conditioned medium, as well as facilitated the low
differentiation of embryonic stem cells. Based on these findings,
MEF/KSF conditioned medium was used to culture and amplify hair
follicle cells in the present study.
In the current study, cells lacking proliferative
and adherent abilities revealed that no adipocytes and fibroblasts
contained in hypodermis tissues were infiltrated in the cell
suspension obtained via the sampling and enzyme digestion process
in DMEM+10% FBS medium. In addition, the three types of phenotypes
obtained under three different culture conditions facilitated the
development of general conclusions based on the cellular
morphologies. For example, cells cultured in KSF-conditioned medium
may be hair follicle-derived epithelium stem cells and those
cultured in KSF+100S medium may be hair follicle mesenchymal cells
with stronger adipogenic potential. Furthermore, adherent cells
cultured in MEF/KSF-conditioned culture medium are analogous to
bone marrow-derived mesenchymal stem cells and hair papilla cells
obtained using the combination of microsurgery and enzyme
digestion. The adherent cell population was considered to be the
hair follicle-derived mesenchymal stem cells and exhibited stronger
proliferative and osteoblastic ability, as expected from the
findings of cell induction and identification studies. Therefore,
the results suggested that MSF/KSF-conditioned culture medium was
useful for screening hair follicle-derived mesenchymal stem cells
with osteoblastic capacity. However, the proliferation assay of
cells cultured in MSF/KSF-conditioned culture medium requires
further study, so follow-up experiments are required to verify
these results.
Hair follicle stem cells are derived from skin and
hair and are widely used in tissue engineering, due to their
abundant source and ease of isolation. Aside from their ability to
differentiate into skin and skin appendages, hair follicle stem
cells have the potential to differentiate into osteocytes,
adipocytes, myocytes, chondrocytes and neurons (37). Prior to the study on hair follicle
stem cells, in vitro osteo-induction of bone marrow-derived
mesenchymal stem cells from mice was performed with the osteogenic
induction system and the results of AKP staining (2 weeks later)
and alizarin red staining (3 weeks later) were positive for the
osteo-induced group, but negative for the non-induced group (Data
not shown). Therefore, the induction and detection system for
osteogenic differentiation containing vitamin C, sodium
β-glycerophosphate and dexamethasone was beneficial.
In the present study, no positive results for
osteo-induction were observed for cells from KSF and KSF+10% FBS
groups, suggesting that these groups lacked the osteogenic
potential. Therefore, these cells were considered to be
epithelium-derived stem cells that exhibited only the ability of
unidirectional differentiation in the hair follicle. Furthermore,
MEF/KSF-conditioned culture medium was used for the induction of
cells from primary (P1 and P2) generations, and strong and weak
positive results were identified for cells from the induced and
non-induced groups, respectively. Therefore, the components of
MEF/KSF-conditioned culture medium may exhibit effects on
osteo-induction but failed to produce positive results when used to
induce cells from subsequent generations; this finding may be
associated with the loss of stem cell potential during cell
passaging. It has been previously reported that DP and dermal
sheath cells from hair papilla of Wistar rats may exhibit
osteogenic and adipogenic abilities (3). Moreover, Bajpai et al (38) observed an increase in the
intracellular concentrations of Runx2, ALP and osteonectin
following osteo-induction of human hair follicle mesenchymal cells.
The osteogenic potential peaked in the eighth generation of
cultured cells and started to decline from generation 11.
Collectively, these results are in line with those reported in the
present study.
The current study detected the sources of cell
markers in cultures of hair follicle stem cells in vitro.
Hair follicle stem cells with osteogenic potential are located at
the bulge region of the epithelium of the hair follicle tissue and
hair papilla from the mesenchymal tissue (39). DP cells located in the basal region
of hair follicles are considered to be an effective source of adult
mesenchymal stem cells and used for the engineering of hair
follicles and skin (40), and also
bone (41), muscle (42) and nerve tissue (43). Therefore, it was hypothesized that
DP cells are mesenchymal cell-derived cells obtained from the DP
region of the hair follicle.
The markers of epithelium-derived cells from the
hair follicle and dermis-derived cells of mice were evaluated and
the results of the present study revealed that pan-CK and K15,
which are surface markers of epithelium-derived cells, were absent.
However, the cells exhibited positive results for AKP, α-SMA and
NCAM (44,45), which are surface markers of hair
follicle DP-derived cells. PEDF in MEF medium may enhance the
expression of AKP in DP cells, and it has been previously
demonstrated that pigment epithelium-derived factor enhances AKP
expression in human mesenchymal stem cells (46). NCAM expression was most likely
induced by insulin-like growth factor binding protein, which is
highly expressed in MEF. Lyles et al (47) identified changes in insulin like
growth factor II, which may regulate muscle NCAM expression during
embryonic development. SOX2 is a member of the SOX HMG box family
and is expressed in early stage in embryonic development to
maintain pluripotency and self-renewal in embryonic stem (ES) cells
(48). It has also been previously
demonstrated that the of AKP (AKP is a membrane bound enzyme)
activity and colony formation positively correlates with
self-renewal potential of human ES cells (49). These results may indicate how the
expression of this cell marker of DP cells was increased in MEF
medium. To avoid any false-positive results caused by nonspecific
antibody staining, typical epithelial and dermal cell markers were
selected for analysis using flow cytometry. The results indicated
that mesenchymal tissue-derived cells accounted for >90% of
cells obtained from MEF/KSF-conditioned medium.
The aforementioned results demonstrated that
MEF/KSF-HFSC may be sourced from DP of hair follicles. To identify
the multi-lineage differentiation capacity of DP cells, adipocytes
and chondroblasts originating from mesoderm differentiation were
used for induction. It was indicated that MEF-HFSC may be
spontaneously induced into osteoblasts, adipocytes, and
chondroblasts in the absence of specific conditions, as previously
reported by Jahoda et al (9). However, the speculation that
MEF/KSF-HFSC cells may be DP cells requires further
examination.
In conclusion, the present study suggested that
MEF/KSF-conditioned medium was an effective method for in
vitro culturing of mouse dermal papilla cells with osteogenic
differentiation potential.
Acknowledgements
Not applicable.
Funding
Funding: The National Natural Science Foundation of China (grant
no. 81401614) and Clinical Research Program of Ninth People's
Hospital affiliated to Shanghai Jiao Tong University School of
Medicine (grant no. JYLJ-10).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LX carried out the molecular genetic studies and
drafted the manuscript. WG conducted the literature search and cell
culture work. SB, XP and HD were involved in performing the
histology experiments. LX and WW supervised the experiments and
performed the analysis and interpretation of data. LX and WW are
responsible for confirming the authenticity of raw data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Amoh Y, Kanoh M, Niiyama S, Hamada Y,
Kawahara K, Sato Y, Hoffman RM and Katsuoka K: Human hair follicle
pluripotent stem (hfPS) cells promote regeneration of
peripheral-nerve injury: An advantageous alternative to ES and iPS
cells. J Cell Biochem. 107:1016–1020. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Carrasco E, Calvo MI, Blázquez-Castro A,
Vecchio D, Zamarrón A, de Almeida IJD, Stockert JC, Hamblin MR,
Juarranz Á and Espada J: Photoactivation of ROS production in situ
transiently activates cell proliferation in mouse skin and in the
hair follicle stem cell niche promoting hair growth and wound
healing. J Invest Dermatol. 135:2611–2622. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wang B, Liu XM, Liu ZN, Wang Y, Han X,
Lian AB, Mu Y, Jin MH and Liu JY: Human hair follicle-derived
mesenchymal stem cells: Isolation, expansion, and differentiation.
World J Stem Cells. 12:462–470. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Castro AR and Logarinho E: Tissue
engineering strategies for human hair follicle regeneration: How
far from a hairy goal. Stem Cells Transl Med. 9:342–350.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Li B, Hu W, Ma K, Zhang C and Fu X: Are
hair follicle stem cells promising candidates for wound healing?
Expert Opin Biol Ther. 19:119–128. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Brockmann I, Ehrenpfordt J, Sturmheit T,
Brandenburger M, Kruse C, Zille M, Rose D and Boltze J:
Skin-derived stem cells for wound treatment using cultured
epidermal autografts: Clinical applications and challenges. Stem
Cells Int. 2018(4623615)2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Bergeron L, Busuttil V and Botto JM:
Multipotentiality of skin-derived precursors: Application to the
regeneration of skin and other tissues. Int J Cosmet Sci. 42:5–15.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Martínez ML, Escario E, Poblet E, Sánchez
D, Buchón FF, Izeta A and Jimenez F: Hair follicle-containing punch
grafts accelerate chronic ulcer healing: A randomized controlled
trial. J Am Acad Dermatol. 75:1007–1014. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jahoda CA, Whitehouse J, Reynolds AJ and
Hole N: Hair follicle dermal cells differentiate into adipogenic
and osteogenic lineages. Exp Dermatol. 12:849–859. 2003.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Tögel F and Westenfelder C: Adult bone
marrow-derived stem cells for organ regeneration and repair. Dev
Dyn. 236:3321–3331. 2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Conejero JA, Lee JA, Parrett BM, Terry M,
Wear-Maggitti K, Grant RT and Breitbart AS: Repair of palatal bone
defects using osteogenically differentiated fat-derived stem cells.
Plast Reconstr Surg. 117:857–863. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Bueno DF, Kerkis I, Costa AM, Martins MT,
Kobayashi GS, Zucconi E, Fanganiello RD, Salles FT, Almeida AB, do
Amaral CE, et al: New source of muscle-derived stem cells with
potential for alveolar bone reconstruction in cleft lip and/or
palate patients. Tissue Eng Part A. 15:427–435. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hoogduijn MJ, Gorjup E and Genever PG:
Comparative characterization of hair follicle dermal stem cells and
bone marrow mesenchymal stem cells. Stem Cells Dev. 15:49–60.
2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Schneider MR, Schmidt-Ullrich R and Paus
R: The hair follicle as a dynamic miniorgan. Curr Biol.
19:R132–R142. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Rochat A, Kobayashi K and Barrandon Y:
Location of stem cells of human hair follicles by clonal analysis.
Cell. 76:1063–1073. 1994.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lin BJ, Lin GY, Zhu JY, Yin GQ, Huang D
and Yan YY: LncRNA-PCAT1 maintains characteristics of dermal
papilla cells and promotes hair follicle regeneration by regulating
miR-329/Wnt10b axis. Exp Cell Res. 24(112031)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ohyama M: Hair follicle bulge: A
fascinating reservoir of epithelial stem cells. J Dermatol Sci.
46:81–89. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cotsarelis G: Gene expression profiling
gets to the root of human hair follicle stem cells. J Clin Invest.
116:19–22. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
19
|
Moll I: Differential epithelial outgrowth
of plucked and microdissected human hair follicles in explant
culture. Arch Dermatol Res. 288:604–610. 1996.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chen L, Duan H, Xie F, Gao Z, Wu X, Chen F
and Wu W: Tetrahydroxystilbene glucoside effectively prevents
apoptosis induced hair loss. Biomed Res Int.
2018(1380146)2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chi W, Wu E and Morgan BA: Dermal papilla
cell number specifies hair size, shape and cycling and its
reduction causes follicular decline. Development. 140:1676–1683.
2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lammens J, Maréchal M, Delport H, Geris L,
Oppermann H, Vukicevic S and Luyten FP: A cell-based combination
product for the repair of large bone defects. Bone.
138(115511)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Vogler HW: Basic bioengineering concepts,
Concepts in bone performance, failure, and osteosynthesis. Clin
Podiatry. 2:161–189. 1985.PubMed/NCBI
|
|
24
|
Kneser U, Schaefer DJ, Polykandriotis E
and Horch RE: Tissue enginering of bone: The reconstructive
surgeon's point of view. J Cell Mol Med. 10:7–19.
2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Li X, Yuan Z, Wei X, Li H, Zhao G, Miao J,
Wu D, Liu B, Cao S, An D, et al: Application potential of bone
marrow mesenchymal stem cell (BMSCs) based tissue-engineering for
spinal cord defect repair in rat fetuses with spina bifida aperta.
J Mater Sci Mater Med. 27(77)2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Loukogeorgakis S and De Coppi P: Stem
cells form amniotic fluid-potential for regenerative medicine. Best
Pract Clin Obstet Gynaecol. 31:45–57. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Sypecka J and Sarnowska A: Mesenchymal
cells of umbilical cord and umbilical cord blood as a source of
human oligodendrocyte progenitors. Life Sci. 139:24–29.
2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Jin SE and Sung JH: Hair regeneration
using adipose-derived stem cells. Histol Histopathol. 31:249–256.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Cheng CS, Davis BN, Madden L, Bursac N and
Truskey GA: Physiology and metabolism of tissue-engineered skeletal
muscle. Exp Biol Med (Maywood). 239:1203–1214. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Tatullo M, Marrelli M, Shakesheff KM and
White LJ: Dental pulp stem cells: Function, isolation and
applications in regenerative medicine. J Tissue Eng Regen Med.
9:1205–1216. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Cotsarelis G, Sun TT and Lavker RM:
Label-retaining cells reside in the bulge area of pilosebaceous
unit: Implication for follicular stem cell, hair cycle, and skin
carcinogenesis. Cell. 61:1329–1337. 1990.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Taylor G, Lehrer MS, Jensen PJ, Sun TT and
Lavker RM: Involvement of follicular stem cell in forming not only
the follicle but also the epidermis. Cell. 102:451–461.
2000.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Kurata S, Itami S, Terashi H and Takayasu
S: Successful transplantation of cultured human outer root sheath
cells as epithelium. Ann Plast Surg. 33:290–294. 1994.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Thomson JA, Itskovitz-Eldor J, Shapiro SS,
Waknitz MA, Swiergiel JJ, Marshall VS and Jones JM: Embryonic stem
cell lines derived from human blastocysts. Science. 282:1145–1147.
1998.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Hu J, Hu S, Ma Q, Wang X, Zhou Z, Zhang W,
Sun X, Zhu W, Qian H and Xu W: Immortalized mouse fetal liver
stromal cells support growth and maintenance of human embryonic
stem cells. Oncol Rep. 28:1385–1391. 2012.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Chin AC, Fong WJ, Goh LT, Philp R, Oh SK
and Choo AB: Identification of proteins from feeder conditioned
medium that support human embryonic stem cells. J Biotechnol.
130:320–328. 2007.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Shwartz Y, Gonzalez-Celeiro M, Chen CL,
Pasolli HA, Sheu SH, Fan SMY, Shamsi F, Assaad S, Lin ETY, Zhang B,
et al: Cell types promoting goosebumps form a niche to regulate
hair follicle stem cells. Cell. 182:578–593. 2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Bajpai VK, Mistriotis P and Andreadis ST:
Clonal multipotency and effect of long-term in vitro expansion on
differentiation potential of human hair follicle derived
mesenchymal stem cells. Stem Cell Res. 8:74–84. 2012.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Morris RJ, Liu Y, Marles L, Yang Z,
Trempus C, Li S, Lin JS, Sawicki JA and Cotsarelis G: Capturing and
profiling adult hair follicle stem cells. Nat Biotechnol.
22:411–417. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
40
|
Morgan BA: The dermal papilla: An
instruction niche for epithelial stem and progenitor cells in
development and regeneration of the hair follicle. Cold Spring Harb
Perspect Med. 4(a015180)2014.PubMed/NCBI View Article : Google Scholar
|
|
41
|
McElwee KJ, Kissling S, Wenzel E, Huth A
and Hoffmann R: Cultured peribulbar dermal sheath cells can induce
hair follicle development and contribute to the dermal sheath and
dermal papilla. J Invest Dermatol. 121:1267–1275. 2003.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Liu JY, Peng HF, Gopinath S, Tian J and
Andreadis ST: Derivation of functional smooth muscle cells from
multipotent human hair follicle mesenchymal stem cells. Tissue Eng
Part A. 16:2553–2564. 2010.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Yu H, Kumar SM, Kossenkov AV, Showe L and
Xu X: Stem cells with neural crest characteristics derived from the
bulge region of cultured human hair follicles. J Invest Dermatol.
130:1227–1236. 2010.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Boden SD: The ABCs of BMPs. Orthop Nurs.
24:49–52; quiz53-54. 2005.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Lin CM, Yuan YP, Chen XC, Li HH, Cai BZ,
Liu Y, Zhang H, Li Y and Huang K: Expression of Wnt/β-catenin
signaling, stem-cell markers and proliferating cell markers in rat
whisker hair follicles. J Mol Histol. 46:233–240. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Li F, Song N, Tombran-Tink J and Niyibizi
C: Pigment epithelium-derived factor enhances differentiation and
mineral deposition of human mesenchymal stem cells. Stem Cells.
12:2714–2723. 2013.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Lyles JM, Amin W, Bock E and Weill CL:
Regulation of NCAM by growth factors in serum-free myotube
cultures. J Neurosci Res. 34:273–286. 1993.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Seo E, Basu-Roy U, Zavadil J, Basilico C
and Mansukhani A: Distinct functions of sox2 control self-renewal
and differentiation in the osteoblast lineage. Mol Cell Biol.
22:4593–4608. 2011.PubMed/NCBI View Article : Google Scholar
|
|
49
|
O'Connor MD, Kardel MD, Iosfina I, Youssef
D, Lu M, Li MM, Vercauteren S, Nagy A and Eaves CJ: Alkaline
phosphatase-positive colony formation is a sensitive, specific, and
quantitative indicator of undifferentiated human embryonic stem
cells. Stem Cells. 5:1109–1116. 2008.PubMed/NCBI View Article : Google Scholar
|