Introduction
Diabetes mellitus prevalence is increasing and
becoming a common health problem worldwide; according to the report
from The International Diabetes Federation, there were an estimated
382 million individuals with diabetes in 2013 and the number may
rise to 592 million by 2035 worldwide (1). Similarly, the prevalence of diabetes
mellitus in China was 5.5% in 2001 and increased to 10.9% in
2013(2). The early stages of type I
diabetes mellitus (T1DM) are characterized by local autoimmune
inflammation and progressive loss of insulin-producing pancreatic β
cells, and β cells can respond to a pro-inflammatory environment
and remodeling of the regulatory landscape in T1DM (3). As β cells fail to produce adequate
amounts of insulin for glucose homeostasis, patients develop
hyperglycemia (4). Thus, there is a
need to determine how to repair impaired β cells in order to
prevent diabetes progression.
Among all etiological factors that contribute to the
onset of diabetes, air pollution has received considerable
attention (5-7).
Airborne particulate matters (PM) consist of airborne solid
particles and liquid droplets (8).
PM with a diameter <10 µm can deposit in the tracheobronchial
tree (9). PM with a diameter
<2.5 µm, termed PM2.5, easily move down into the
alveoli and enter the circulatory system (8). Epidemiological evidence has
illustrated the positive association between ambient
PM2.5 and the extent of inflammation (10,11),
as well as the incidence of metabolic syndrome (12) and type 2 diabetes (13), in cross-sectional studies. In
separate cohort studies, long-term exposure of PM2.5
increased the risk of diabetes in cohorts after 5.1 or 16 years of
follow-up (12,14), indicating a link between
PM2.5 and incidence of diabetes.
When PM2.5 particles processed from the
atmosphere are added to cultivated macrophages, they activate
Toll-like receptor (TLR)2 and TLR4 signaling pathways, stimulating
NF-κB transcription, and leading to interleukin-1β (IL-1β) and
cyclooxygenase-2 production (15).
In vivo, PM2.5 exposure in combination with a
sustained high-fat diet enhances the infiltration of macrophages
into adipose tissues and promotes tumor necrosis factor-α (TNFα)
production in wild-type mice (16).
Exposure to PM2.5 alone does not alter fasting blood
glucose (FBG) levels despite increased macrophage infiltration into
adipose tissues in wild-type mice (17). Environmental factors are involved in
the development of T1DM, providing an opportunity to detect and
prevent further autoimmune destruction of β cells via therapeutic
intervention (18). As the role of
inflammation in glucose homeostasis and β cell destruction has been
established (19-21),
it was hypothesized that mice with pre-exposure to PM2.5
may be prone to greater impairments in glucose tolerance and β cell
function when challenged with diabetic triggers. Therefore, in the
present study, wild-type mice were pre-exposed to an ambient
PM2.5 environment for 12 weeks and then administered an
intraperitoneal streptozotocin (STZ) injection.
Materials and methods
Mice and treatment
All the animal experiments were approved by the
Animal Care and Use Committee of Luhe Hospital, Capital Medical
University (2020 LH-KS-020; Beijing, China) and conducted in
accordance with the Guide for the Care and Use of Laboratory
Animals of the National Institutes of Health (22). In the present study, 8-week-old male
C57BL/6 mice (n=51; weight, 25-30 g) were purchased from Beijing
Vital River Laboratory Animal Technology Co., Ltd.
Mice were randomly exposed to ambient
PM2.5 (n=27) or filtered air (FA; n=24) from November
2016 to February 2017. PM2.5 exposure (14-289 µg/m3) was
performed using a ‘real-world’ versatile aerosol concentration
enrichment system in Tongzhou District, Beijing, China as described
by Sioutas et al (23) and
further modified by Chen et al (24). During the exposure time, the dynamic
daily concentration of ambient PM2.5 was monitored using
an individual particle monitor (pDR1500; Thermo Fisher Scientific,
Inc.). The FA mice were exposed to an identical environment with
the exception of a highly efficient particulate air filter
positioned in the inlet valve to remove PM2.5 in the air
stream. The mice in the exposure chamber were fed regular chow and
distilled water ad libitum, and raised under suitable temperature
(22±2˚C) and relative humidity (40-60%) conditions with a 12:12-h
light/dark cycle.
At 12 weeks after exposure, 18 mice in the
PM2.5 group and 15 mice in the FA group were
intraperitoneally injected with STZ (40 mg/kg) in acetic buffer
daily for 5 consecutive days. The rest of mice received an
equivalent volume of the acetic buffer. At 4th week after the last
injection, mice were weighed and plasma samples were collected from
the tail and reading by Accu-check Performa glucometer (Roche
Diagnostics) followed fasting overnight. To further dissect the
impact of PM2.5 on the features of diabetic mice,
STZ-injected mice with FBG levels ≥7 mmol/l were investigated in
the following analysis (STZ-treated with FA, n=8; STZ-treated with
PM2.5, n=14; acetic-treated with FA, n=9; and
acetic-treated with PM2.5, n=9). All mice were
euthanized via an intraperitoneal injection of 150 mg/kg
pentobarbital, blood samples (1 ml) were collected from the
inferior vena cava after euthanasia, and then fat and liver tissues
were dissected and stored at -80˚C. Death was confirmed based on
the absence of heart beat, breathing and reflexes. Blood samples
were centrifuged at 1,000 x g at 4˚C for 10 min, and the plasma was
collected for further analysis.
PM2.5 particle
preparation
PM2.5 samples were collected regularly in
Tongzhou (Beijing, China) between November 2016 and February 2017.
As described previously by Imrich et al (25), PM2.5 samples were
collected on Teflon filters (diameter, 47 mm; Whatman plc; Cytiva),
then particles were isolated by putting the Teflon filters into
50-ml centrifuge tubes and probe-sonicating for 2 min at 40 kHz at
room temperature in ultra-pure water before drying the filters in a
drying oven. The final concentration of the PM2.5
particle extracts was 5 mg/ml. PM2.5 particles were
stored at -80˚C for cell experiments.
Lipid measurement
Liver samples were homogenized using lysis buffer
(cat. no. C1053; Applygen Technologies, Inc.) and quantified by BCA
(Thermo Fisher Scientific, Inc.). Liver and plasma levels of
triglyceride (cat. no. 0220) and cholesterol (cat. no. 0180) were
measured using reagent kits (Biosino Bio-Technology & Science
Inc.) by triglycerophosphate oxidase-peroxidase and cholesterol
oxidase-peroxidase according to the manufacturer's
instructions.
ELISA
The levels of IL-1β (cat. no. 432604) and TNFα (cat.
no. 430904) in plasma, protein extracts from adipose tissues and
cell media were determined via ELISA according to the
manufacturer's instructions (both BioLegend, Inc.) and calculated
as previously described (26). The
levels of insulin in plasma and cell supernatant were evaluated via
ELISA using a kit (cat. no. EZRMI-13K; EMD Millipore) according to
the manufacturer's instructions.
Assessment of β cell function
Homeostasis model assessment of β cell function
(Homa-β) was performed using fasting insulin and glucose levels
according to the formula: Homa-β = [(360 x insulin level)/(glucose
(mg/dl - 63)] (27).
Cell culture and treatment
The mouse macrophage cell line RAW264.7 was
purchased from American Type Culture Collection and cultured in
Dulbecco's modified Eagle's medium (DMEM; Gibco; Thermo Fisher
Scientific, Inc.) containing 10% fetal bovine serum (FBS; HyClone;
Cytiva) and 1% penicillin-streptomycin. The mouse pancreatic β cell
line MIN6 was a gift from Professor Yang (Peking University Health
Science Center, Beijing, China) and cultured in DMEM (cat. no.
C11995500BT; Gibco; Thermo Fisher Scientific, Inc.), supplemented
with 15% FBS, 1% penicillin-streptomycin and 5 µl/l
β-mercaptoethanol. Cells were maintained in an incubator at 37˚C
with 5% CO2.
After reaching 100% confluence, cells were treated
with PM2.5 particles (0, 0.5, 5 or 50 µg/ml) for 24 h.
After harvesting, the cell and the supernatant were collected at
10,000 x g at 4˚C for 3 min. For insulin secretion, the MIN6 cell
were treated with PM2.5 for 24 h at 37˚C with 5%
CO2, followed by one wash with prewarmed Krebs-Ringer
bicarbonate buffer (KRB; Coolaber) without glucose, and then
incubation in KRB without glucose at 37˚C with 5% CO2
for 1 h. Cells were then incubated in KRB with 0, 2.5 or 20 mmol/l
glucose for 1 h at 37˚C. After incubation, the supernatant was
collected for ELISA.
Protein extraction
Proteins were extracted from adipose tissues using
lysis buffer (cat. no. C1053; Applygen Technologies, Inc.) in a
ratio of 1:1:100 (protein inhibitor: PMSF: RIPA lysis buffer,
respectively) and then calibrated to a consistent concentration
using a BCA protein assay kit (Thermo Fisher Scientific, Inc.)
before being subjected to ELISA.
Statistical analysis
Data were expressed as the mean ± SEM. All cell
experiments were repeated three times. In PM2.5-treated
cell experiments, one-way ANOVA followed by Dunnett's post hoc test
was used for data with normal distribution. When there were more
than two experimental treatments, two-way ANOVA followed by Sidak's
was used by comparing treated groups with the control. Both
WHO1999 and ADA2003 recommend cut points for
IGT as 7.8-11.0 mmol/l measured at the 2 h time point of an OGTT
(28). Since the T1DM model was
used in the present study, FBG levels ≥7 mmol/l were used as the
criteria for impaired glucose level. The incidence of mice with
impaired glucose level was analyzed by Fisher's exact test, using
FBG levels ≥7 mmol/l as the criteria for impaired glucose level.
P<0.05 was considered to indicate a statistically significant
difference. Statistical analysis was performed using GraphPad Prism
version 7.00 (GraphPad Software, Inc.).
Results
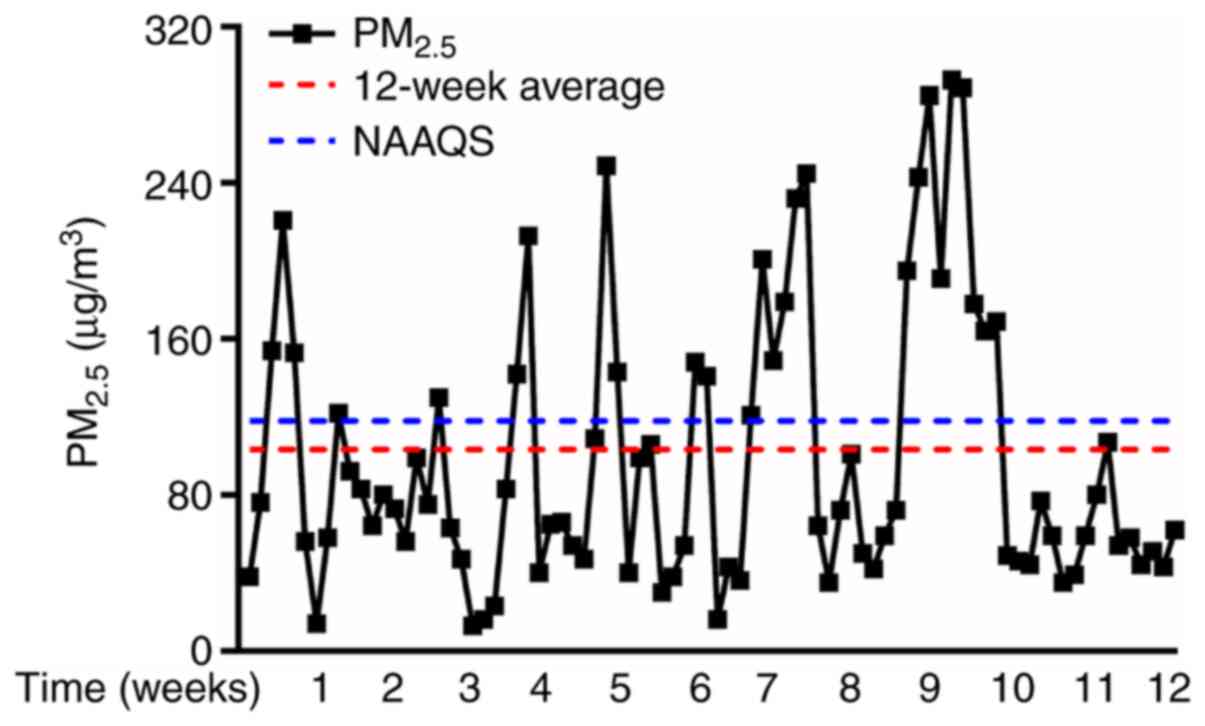
Ambient PM2.5 levels in the
exposure period
Throughout the study, mice were exposed to either FA
or PM2.5 in a ‘real-world’ ambient PM2.5
exposure system. During the exposure time, the dynamic daily
concentration of ambient PM2.5 was monitored using an
individual particle monitor. The average daily concentration of
ambient PM2.5 prior to STZ injection was presented in
Fig. 1. Across the study, the
average PM2.5 levels of the Beijing National Ambient Air
Quality Standard and in the exposure system were 118.08
µg/m3 and 103.27 µg/m3, respectively. This
result showed that it is ~1.1-fold lower than the average
PM2.5 National Ambient Air Quality Standard in China
(29).
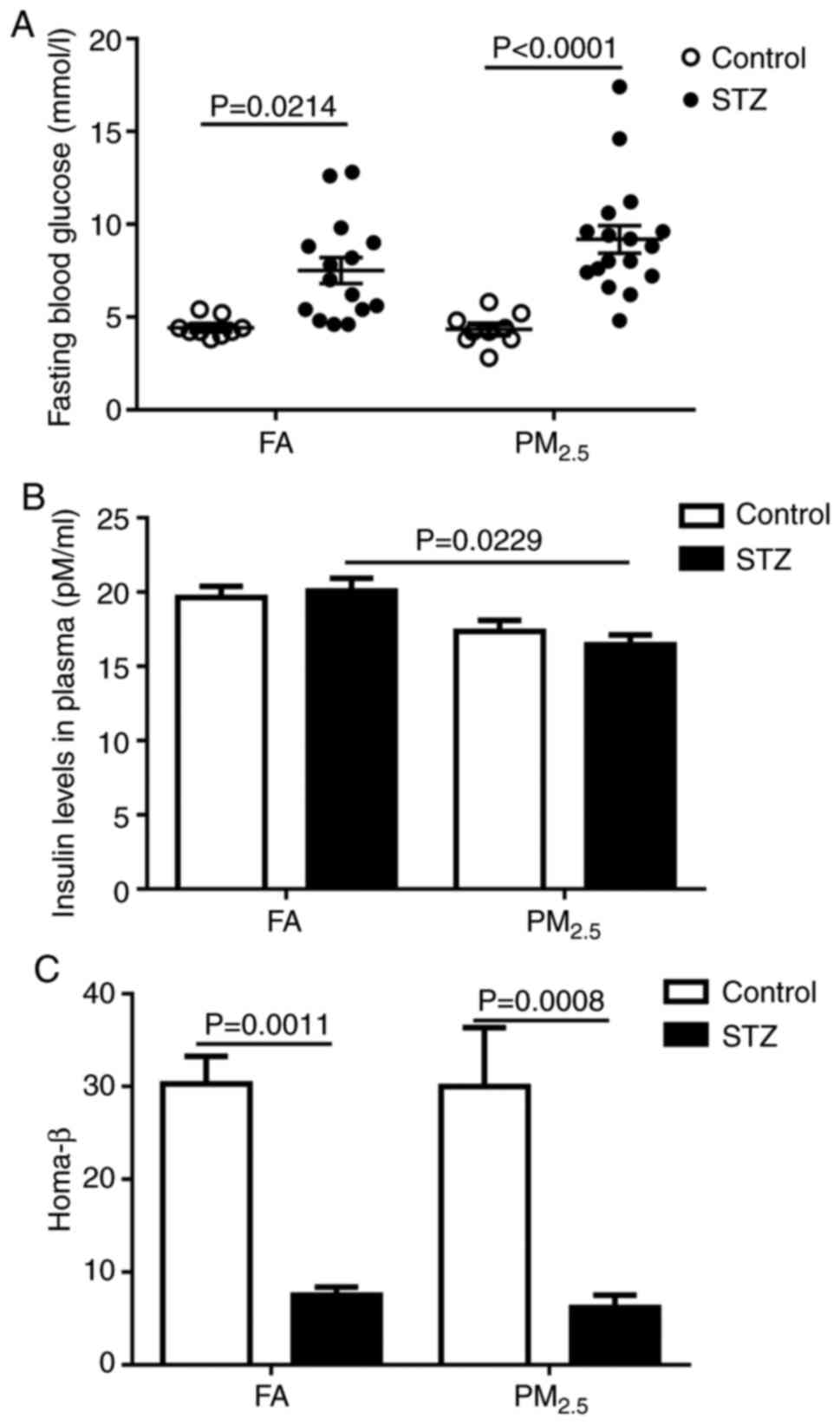
Effects of PM2.5
pre-exposure on FBG and insulin levels
PM2.5 exposure did not increase FBG
levels compared with the FA group. Additionally, at 4 weeks after
STZ injection, there was no significant difference in FBG levels
between mice pre-exposed to PM2.5 and those in the FA
group (Fig. 2A). Using FBG levels
≥7 mmol/l as the criteria for impaired glucose level, the incidence
of impaired glucose level upon STZ injection was 53.3% (8/15) in
the FA group and 77.8% (14/18) in the PM2.5 group,
although this was not significant (data not shown). The data
suggested that mice pre-exposed to PM2.5 may be prone to
developing impaired glucose metabolism; however, no significant
difference was observed. To further dissect the impact of
PM2.5 on the features of diabetic mice, STZ-injected
mice with FBG levels ≥7 mmol/l were investigated in the following
analysis (STZ-treated with FA, n=8; STZ-treated with
PM2.5, n=14). ELISA revealed that pre-exposure to
PM2.5 significantly reduced fasting insulin levels in
mice after STZ injection; meanwhile, pre-exposure to
PM2.5 also downregulated the insulin level; however,
there was no significant difference in acetic buffer groups
(Fig. 2B). Homa-β revealed that STZ
injection similarly reduced β cell function in FA and
PM2.5 mice (Fig. 2C).
These data suggested that PM2.5 exposure may contribute
to the impairments in glucose metabolism and insulin levels after
STZ injection.
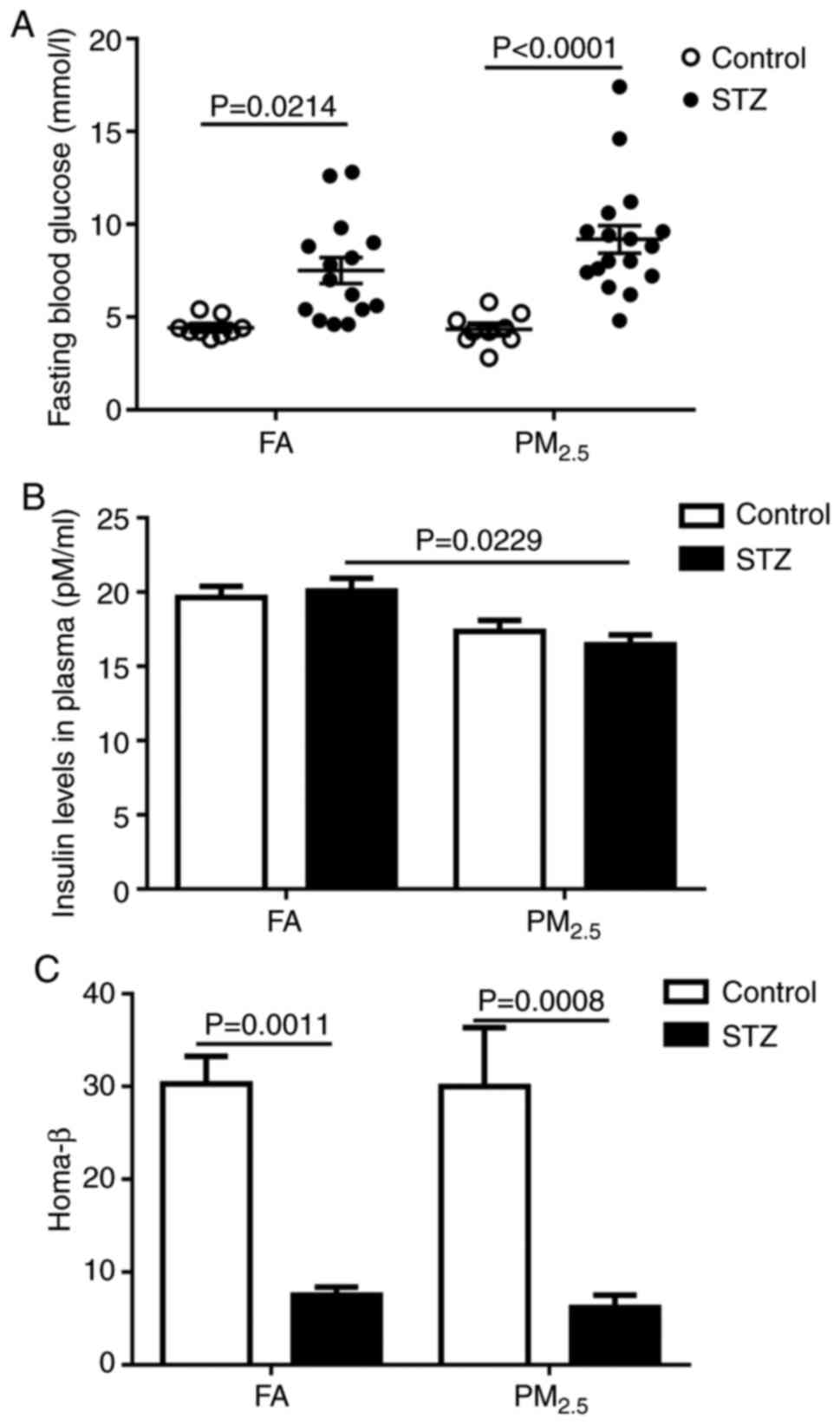 | Figure 2Effects of PM2.5 exposure
on glucose metabolism. After 12 weeks of FA or PM2.5
exposure, mice were injected with STZ (40 mg/kg) or an equivalent
dose of acetic buffer for 5 consecutive days. (A) At 4 weeks after
the last injection, mice were fasted overnight for the fasting
blood glucose test. (B) Insulin levels in the plasma were
quantified via ELISA. (C) Homa-β. Data are presented as the mean ±
SEM (control with FA, n=8; control with PM2.5, n=8;
STZ-treated with FA, n=8; STZ-treated with PM2.5, n=14).
FA, filtered air; PM2.5, particulate matters, diameter
<2.5 µm; STZ, streptozotocin; Homa-β, homeostasis model
assessment of β cell function. |
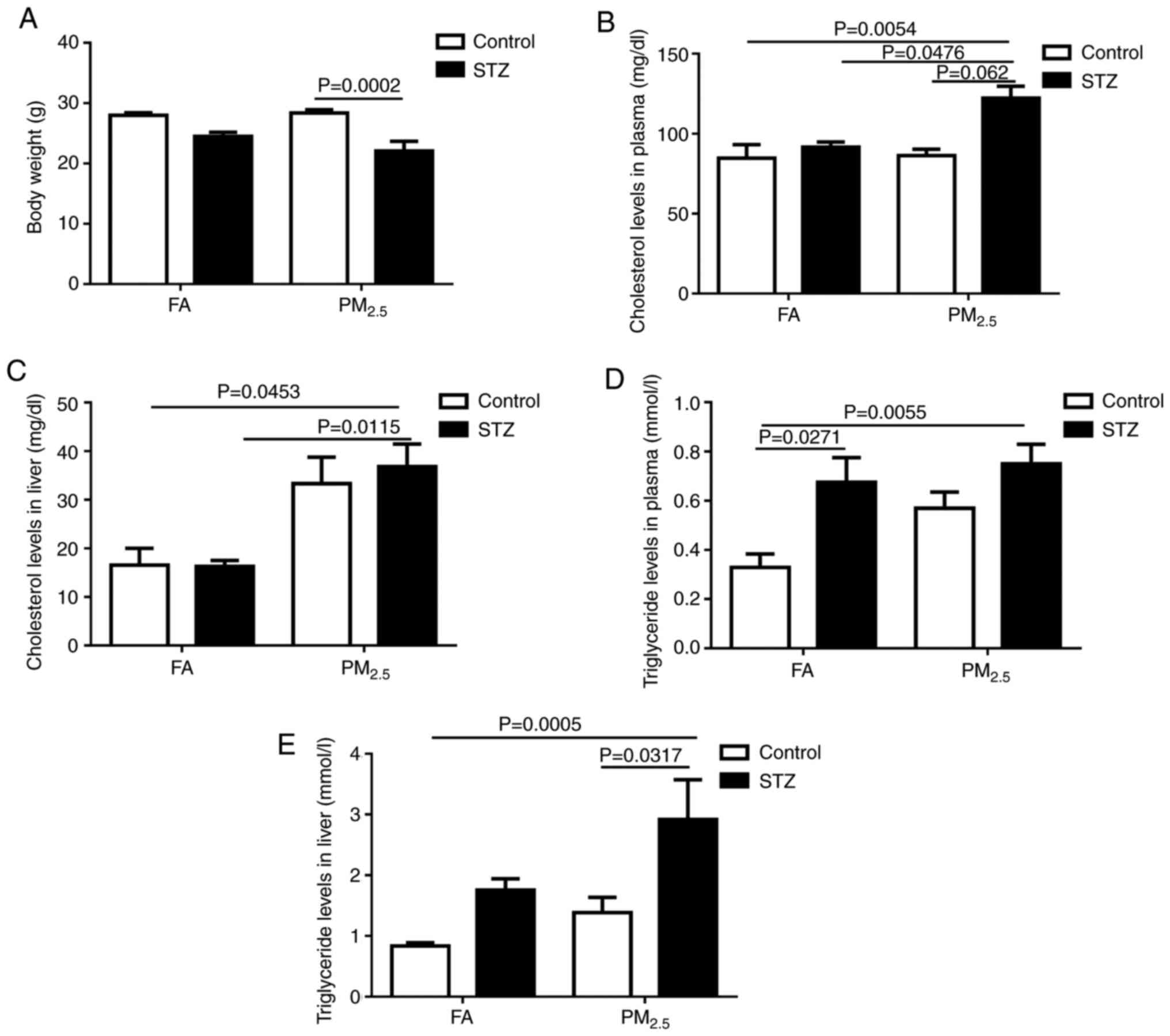
Effects of PM2.5
pre-exposure on body weight and lipid profile
Compared with mice injected with acetic buffer, mice
receiving STZ treatment exhibited significantly reduced body
weights in the PM2.5 group (Fig. 3A). Compared with the FA group
injected with acetic buffer, mice exposed to PM2.5 and
STZ injection exhibited significantly elevated cholesterol levels
in the plasma and liver (Fig. 3B
and C). In the plasma, STZ
injection significantly increased cholesterol levels in mice when
exposed to PM2.5 (Fig.
3B). Furthermore, pre-exposure to PM2.5 increased
both the plasma and liver cholesterol levels compared with FA and
STZ injection (Fig. 3B and C).
For triglyceride profiles, compared with the FA
injected with acetic buffer group, mice exposed to PM2.5
and STZ injection exhibited significantly elevated triglyceride
levels in the plasma and liver (Fig.
3D and E). In plasma, STZ
injection increased triglyceride levels in the FA group (Fig. 3D); and in the liver, STZ injection
increased triglyceride levels in the PM2.5 group
(Fig. 3E). These findings indicated
that PM2.5 exposure combined with STZ may affect lipid
metabolism.
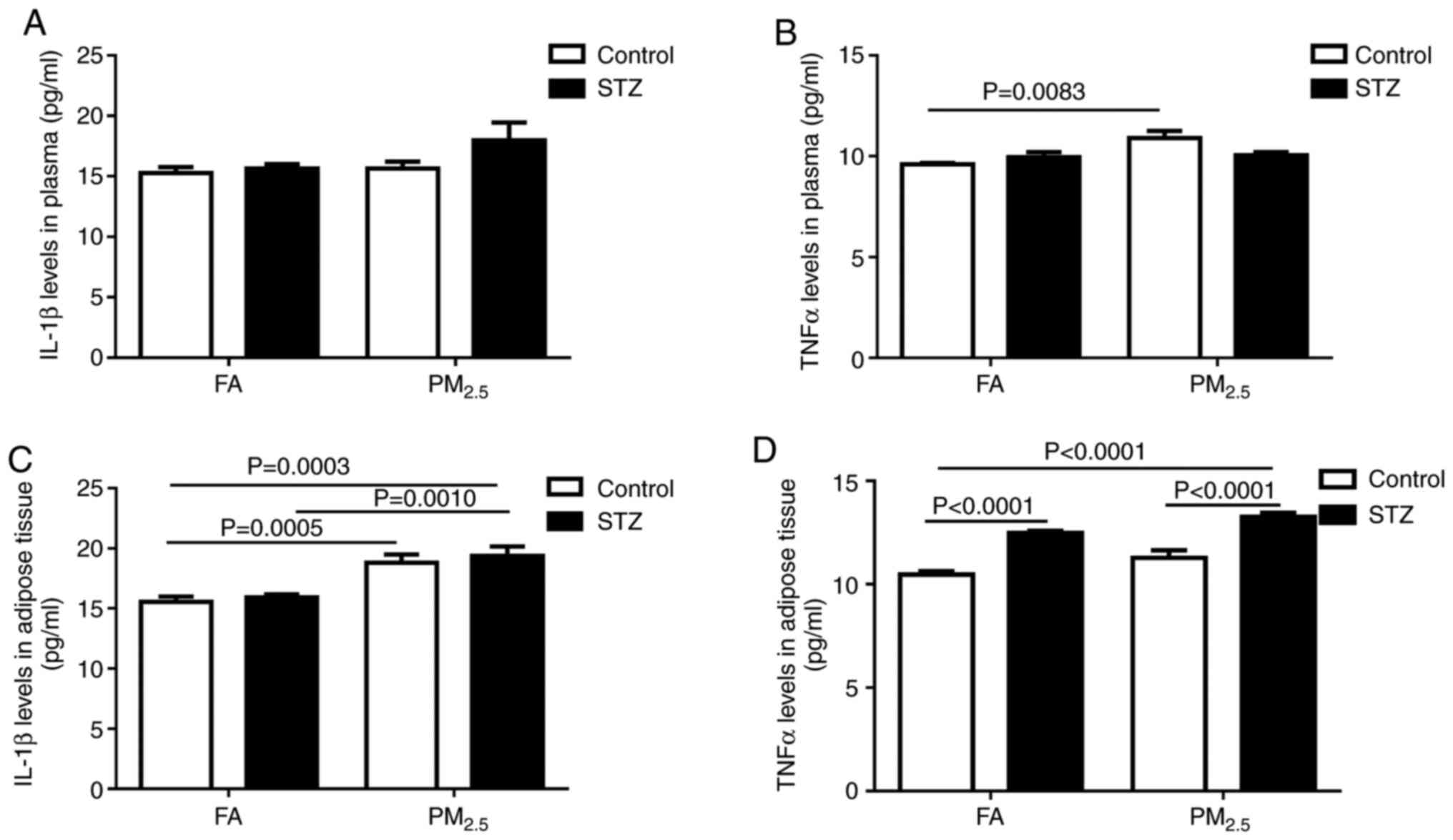
Effects of PM2.5
pre-exposure on inflammation
Accumulating evidence suggests that IL-1β and TNFα
are involved in the incidence and progression of diabetes (30). ELISA revealed that PM2.5
exposure may increase IL-1β levels compared with FA exposure in the
plasma of STZ-treated mice, whilst STZ exposure also elevated IL-1β
levels compared with the control; however, there was no
statistically significant difference (Fig. 4A). TNFα levels in plasma were
elevated in mice in the PM2.5 group compared with the FA
group (Fig. 4B). As adipose tissues
are the main source of IL-1β and TNFα (31), the adipose tissues of mice were
dissected for protein extraction. Compared with the FA group,
PM2.5 exposure significantly increased IL-1β production
in both acetic buffer- and STZ-treated adipose tissues (Fig. 4C); however, STZ significantly
upregulated TNFα production in adipose tissues compared with the
control independent of FA or PM2.5 exposure (Fig. 4D). These data suggested that
PM2.5 pre-exposure increased inflammation in mice
treated with STZ in adipose tissue.
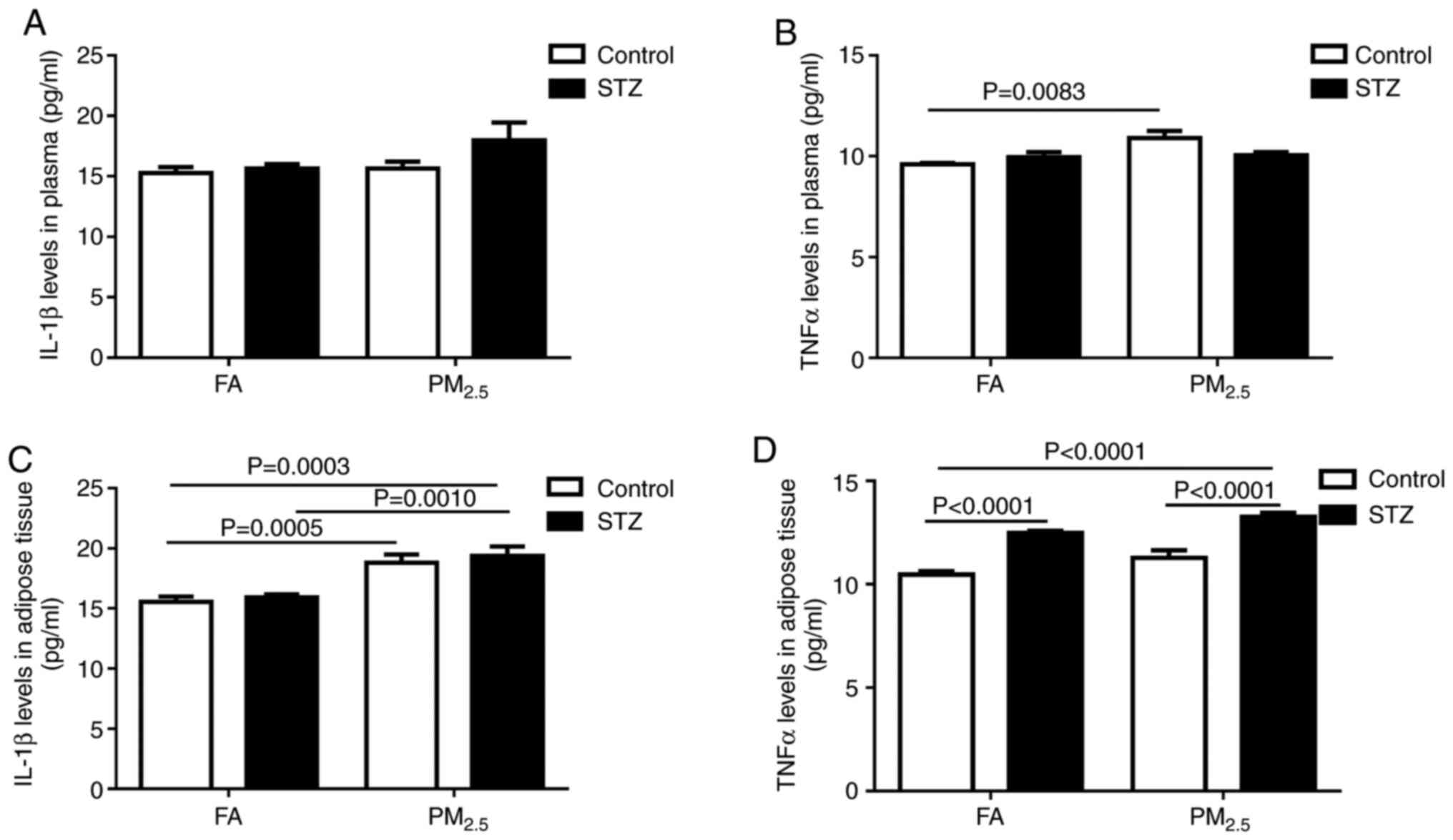 | Figure 4PM2.5 exposure affects
inflammatory responses in plasma and adipose tissues. After 12
weeks of FA or PM2.5 exposure, mice were injected with
STZ (40 mg/kg) or an equivalent dose of acetic buffer for 5
consecutive days. Plasma levels of (A) IL-1β and (B) TNFα in mice
after STZ injection. Expression of (C) IL-1β and (D) TNFα in
adipose tissue protein homogenates after PM2.5 exposure
and STZ injection. Data are presented as the mean ± SEM (control
with FA, n=8; control with PM2.5, n=8; STZ-treated with
FA, n=8; STZ-treated with PM2.5, n=14). FA, filtered
air; PM2.5, particulate matters, diameter <2.5 µm;
STZ, streptozotocin; IL-1β, interleukin-1β; TNFα, tumor necrosis
factor-α. |
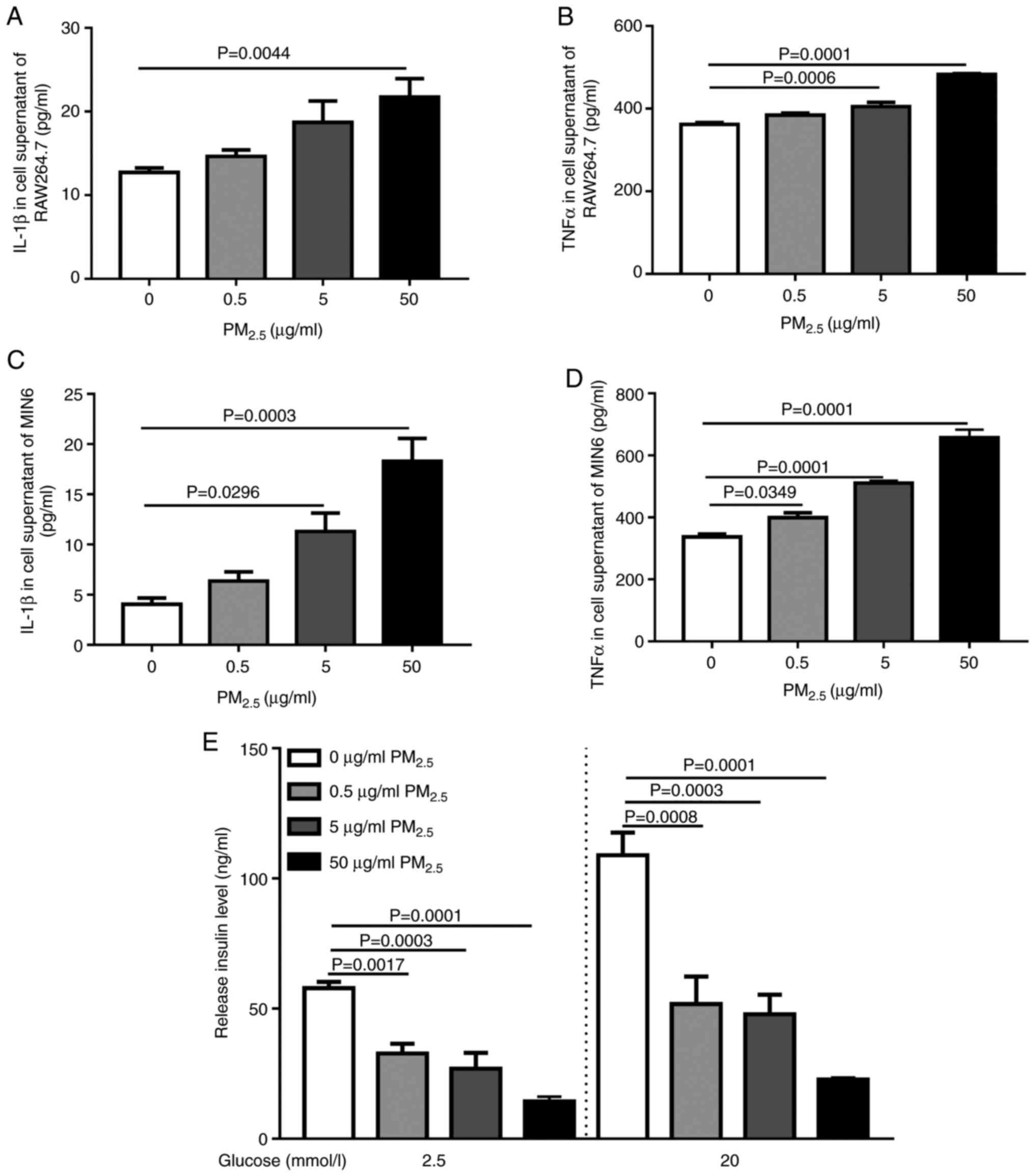
PM2.5 increases
inflammation and decreases glucose-induced insulin secretion
Cytokines appear to be major regulators of adipose
tissue metabolism, especially TNFα and IL-1β (32). The density of adipose tissue
macrophages is associated with adipose tissue inflammatory markers
and insulin resistance, and inflammation has been described as
causally related to decreased insulin secretion from β-cells
(33,34). Pancreatic β cells are the main
source of insulin. Therefore, the effects of PM2.5 on
IL-1β and TNFα production in macrophages and pancreatic β cells, as
well as pancreatic β cell insulin secretion, were evaluated. Mouse
RAW264.7 macrophage cells and mouse MIN6 pancreatic β cells were
treated with PM2.5 at different concentrations (0-50
µg/ml) for 24 h, and the supernatant was collected. ELISA revealed
that both RAW264.7 and MIN6 cells significantly increased release
of TNFα and IL-1β levels following PM2.5 exposure in a
dose-dependent manner (Fig. 5A-D).
Furthermore, PM2.5 exposure significantly decreased
insulin secretion in response to 2.5 and 20 mM glucose (Fig. 5E). These findings suggested that
PM2.5 exposure may aggravate β cell damage by increasing
inflammation and inhibiting insulin secretion.
Discussion
In the present study, the effect of pre-exposure to
PM2.5 on β cell function in mice challenged with a
diabetic trigger was investigated. The major findings are
summarized as follows: i) When pre-exposed to PM2.5,
there was a non-significant trend towards mice developing diabetes
following STZ injection based on increased numbers of animals with
IGT; ii) in STZ-injected mice, exposure to PM2.5
decreased the level of insulin, and elevated cholesterol levels in
the blood, and cholesterol and triglyceride contents in the liver;
iii) exposure to PM2.5 stimulated inflammation in the
present study by increasing TNFα and IL-1β levels in macrophages
and pancreatic β cells; and iv) exposure to PM2.5
decreased glucose-induced insulin secretory function. Collectively,
the present study indicated that pre-exposure to PM2.5
may accelerate impairments to β cells upon STZ injection, which may
be partially mediated via increased inflammation.
Studies have reported positive associations between
PM10 or PM2.5 exposure and cardiovascular injury
(35), atherosclerosis (36) and ischemic stroke (37). Consistent with these findings,
exposure to PM2.5 increased diabetic prevalence in
pregnant women (38), general
populations (12,39) or elderly individuals (40). Aside from increased diabetic
prevalence, long-term exposure to PM10 is associated
with hyperglycemia, as reflected by FBG and hemoglobin A1c levels,
and insulin resistance (IR), as determined by the Homa-IR index, in
patients with diabetes (41).
To explore the mechanism underlying the effects of
PM2.5 exposure on diabetes prevalence, mouse and rat
models have been frequently used; in these models, animals are
either exposed to PM2.5 alone or simultaneously in
combination with a high-fat diet (42,43).
Studies have found that PM2.5 is taken up by macrophages
via TLR2 and TLR4 (44,45). Downstream of TLR2 and TLR4, adaptor
protein myeloid differentiation primary response 88 mediates
inflammatory responses and activation of NF-κB transcription, both
of which contribute to inflammatory cytokine production in alveolar
and peripheral blood (46,47). Consistently, activation of
TLR4/JNK-induced inflammation has been reported to result in
impaired insulin secretion and apoptosis in MIN6 cells (48,49).
Following circulation, these inflammatory cytokines induce
endoplasmic reticulum stress and deteriorate brown adipocyte
activity by reducing uncoupling protein 1 expression in brown
adipose tissues (50), exaggerate
endothelial cell dysfunction (47)
and promote monocyte infiltration into fat tissues (16). Additionally, PM2.5
exposure stimulates the transition of M2 macrophages into M1
macrophages and increases Th1/Th17 cell number in peripheral
tissues (45,51), which further reinforces inflammation
and IR. However, whether long-term PM2.5 exposure prior
to a diabetic trigger such as STZ injection could enhance IGT and
IR has not been established. Therefore, the present study was
performed to investigate this, and the findings validated the
hypothesis that pre-exposure to PM2.5 promoted the onset
of impaired glucose level in mice challenged with STZ. However, the
observed reduction in insulin levels was comparable between
STZ-injected mice pre-exposed to FA or PM2.5, whereas
Homa-β was comparable between acetic buffer and STZ groups.
Therefore, it appears that the adverse effect of PM2.5
was primarily in relation to insulin levels rather than insulin
sufficiency.
The present study subsequently investigated how
PM2.5 may participate in the progression of impaired β
cell function. Despite functioning via different mechanisms, IL-1β
and TNFα signaling interferes with insulin signaling pathways, thus
serving as fundamental pathogenic factors underlying IR (52). IL-1β downregulates insulin substrate
receptor-1 (IRS-1) expression in adipocytes and hepatocytes
(19,20), whereas TNFα induces JNK
phosphorylation that phosphorylates IRS-1 at Ser307 (53,54).
Decreased IRS-1 protein expression and phosphorylation abrogate
insulin signal transduction in peripheral cells (55). In addition, TNFα inhibits glucose
transport in adipocytes (55). In
the present study, increased IL-1β and TNFα production was observed
in adipose tissues of mice exposed to PM2.5 and STZ
injection. Macrophages and β cells were hypothesized to be the
sources of increased IL-1β and TNFα production, as release of both
factors was increased in both cell types when treated with
PM2.5 particles. Following STZ injection, insulin levels
were significantly decreased in PM2.5-exposed mice, but
the levels of IL-1β in the peripheral blood did not increase
further in PM2.5-exposed mice compared with FA-exposed
ones. By contrast, IL-1β and TNFα expression were increased in
adipose tissues from PM2.5-exposed mice compared with
mice in the FA group following STZ injection, indicating enhanced
inflammation by PM2.5-exposure and STZ in vivo.
Subsequently, RAW264.7 and MIN6 cells were treated with
PM2.5 particles, and the levels of IL-1β and TNFα were
significantly upregulated in a dose-dependent manner. The secretion
of insulin from MIN6 cells was similarly decreased following
PM2.5-exposure.
The present study must be interpreted in the context
of some potential limitations. First, macrophages are critical
mediators in adipose tissues (56).
The kinetics of IL-1β and TNFα production in macrophages residing
in adipose tissues could not be evaluated in vivo. Instead,
the release of inflammatory cytokines was studied at only one
timepoint (24 h) in RAW264.7 and MIN6 mouse cell lines. Second,
when compared with FA injected with acetic buffer, liver
cholesterol and triglyceride levels demonstrated no significant
change in FA injected with STZ. However, whether and how increased
cholesterol and triglyceride in mice could facilitate impairment of
glucose levels was not studied, as it was not the main goal of the
present study. Further experimental verification and in-depth
exploration will be conducted in our subsequent research, including
investigation of the TLR4/JNK signaling pathway in
PM2.5-induced β cell injury.
In conclusion, the present study indicated that
pre-exposure of PM2.5 impaired pancreatic β cells in
mice upon STZ injection, which may be partially mediated via
increased IL-1β and TNFα production in macrophages and adipose
tissues.
Acknowledgements
The authors would like to thank Professor Ji Chun
Yang (Department of Physiology and Pathophysiology, School of Basic
Medical Sciences, Peking University Health Science Center, Beijing
100191, P.R. China) for the donation of the MIN6 cells. The
abstract was presented at the 80 Scientific Session of the American
Diabetes Association June 12-16, 2020 in Chicago, and published as
abstract no. 2322-PUB in Diabetes 69 (Suppl 1): 2020.
Funding
Funding: This study was funded by the Science and Technology
Committee of Tongzhou District (grant no. KJ2019CX014-25), the
Natural Science Foundation of Beijing (grant no. 7194282) and the
Natural Cultivation Fund of Capital Medical University (grant no.
pYZ2017051).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YM conceived the study. BZ analyzed the data. RY and
JL acquired and interpreted the data. LY was a major contributor in
writing the manuscript, revised it critically for important
intellectual content and analyzed the data from cell experiments.
DZ acquired the cell data and gave approval of the final version to
be published. LY, RY and DZ confirm the authenticity of all the raw
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All the animal experiments were approved by the
Animal Care and Use Committee of Luhe Hospital, Capital Medical
University (Beijing, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
International Diabetes Federation: IDF
Diabetes Atlas. 6th edition, 2013.
|
|
2
|
Hu C and Jia W: Diabetes in China:
Epidemiology and genetic risk factors and their clinical utility in
personalized medication. Diabetes. 67:3–11. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ramos-Rodríguez M, Raurell-Vila H, Colli
ML, Alvelos MI, Subirana-Granés M, Juan-Mateu J, Norris R,
Turatsinze JV, Nakayasu ES, Webb-Robertson BM, et al: The impact of
proinflammatory cytokines on the β-cell regulatory landscape
provides insights into the genetics of type 1 diabetes. Nat Genet.
51:1588–1595. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rorsman P and Ashcroft FM: Pancreatic
β-cell electrical activity and insulin secretion: Of mice and men.
Physiol Rev. 98:117–214. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yang BY, Fan S, Thiering E, Seissler J,
Nowak D, Dong GH and Heinrich J: Ambient air pollution and
diabetes: A systematic review and meta-analysis. Environ Res.
180(108817)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhang H, Dong H, Ren M, Liang Q, Shen X,
Wang Q, Yu L, Lin H, Luo Q, Chen W, et al: Ambient air pollution
exposure and gestational diabetes mellitus in Guangzhou, China: A
prospective cohort study. Sci Total Environ.
699(134390)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Renzi M, Cerza F, Gariazzo C, Agabiti N,
Cascini S, Di Domenicantonio R, Davoli M, Forastiere F and Cesaroni
G: Air pollution and occurrence of type 2 diabetes in a large
cohort study. Environ Int. 112:68–76. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nogueira JB: Air pollution and
cardiovascular disease. Rev Port Cardiol. 28:715–733.
2009.PubMed/NCBI
|
|
9
|
Kodros JK, Volckens J, Jathar SH and
Pierce JR: Ambient particulate matter size distributions drive
regional and global variability in particle deposition in the
respiratory tract. Geohealth. 2:298–312. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Li Y, Sun B, Shi Y, Jiang J, Du Z, Chen R,
Duan J and Sun Z: Subacute exposure of PM2.5 induces airway
inflammation through inflammatory cell infiltration and cytokine
expression in rats. Chemosphere. 251(126423)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Abramson MJ, Wigmann C, Altug H and
Schikowski T: Ambient air pollution is associated with airway
inflammation in older women: A nested cross-sectional analysis. BMJ
Open Respir Res. 7(7)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Coogan PF, White LF, Yu J, Burnett RT,
Seto E, Brook RD, Palmer JR, Rosenberg L and Jerrett M: PM2.5 and
diabetes and hypertension incidence in the Black Women's Health
Study. Epidemiology. 27:202–210. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Liu C, Yang C, Zhao Y, Ma Z, Bi J, Liu Y,
Meng X, Wang Y, Cai J, Chen R, et al: Associations between
long-term exposure to ambient particulate air pollution and type 2
diabetes prevalence, blood glucose and glycosylated hemoglobin
levels in China. Environ Int. 92-93:416–421. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Weinmayr G, Hennig F, Fuks K, Nonnemacher
M, Jakobs H, Möhlenkamp S, Erbel R, Jöckel KH, Hoffmann B and
Moebus S: Heinz Nixdorf Recall Investigator Group. Long-term
exposure to fine particulate matter and incidence of type 2
diabetes mellitus in a cohort study: Effects of total and
traffic-specific air pollution. Environ Health.
14(53)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bekki K, Ito T, Yoshida Y, He C,
Arashidani K, He M, Sun G, Zeng Y, Sone H, Kunugita N, et al: PM2.5
collected in China causes inflammatory and oxidative stress
responses in macrophages through the multiple pathways. Environ
Toxicol Pharmacol. 45:362–369. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sun Q, Yue P, Deiuliis JA, Lumeng CN,
Kampfrath T, Mikolaj MB, Cai Y, Ostrowski MC, Lu B, Parthasarathy
S, et al: Ambient air pollution exaggerates adipose inflammation
and insulin resistance in a mouse model of diet-induced obesity.
Circulation. 119:538–546. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Liu C, Xu X, Bai Y, Zhong J, Wang A, Sun
L, Kong L, Ying Z, Sun Q and Rajagopalan S: Particulate Air
pollution mediated effects on insulin resistance in mice are
independent of CCR2. Part Fibre Toxicol. 14(6)2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tomita T: Apoptosis of pancreatic β-cells
in Type 1 diabetes. Bosn J Basic Med Sci. 17:183–193.
2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Fantuzzi G: Adipose tissue, adipokines,
and inflammation. J Allergy Clin Immunol. 115:911–919; quiz 920.
2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jager J, Grémeaux T, Cormont M, Le
Marchand-Brustel Y and Tanti JF: Interleukin-1beta-induced insulin
resistance in adipocytes through down-regulation of insulin
receptor substrate-1 expression. Endocrinology. 148:241–251.
2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wasserman DH, Wang TJ and Brown NJ: The
vasculature in prediabetes. Circ Res. 122:1135–1150.
2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
National Research Council (US) Institute
for Laboratory Animal Research: Guide for the Care and Use of
Laboratory Animals. National Academies Press, Washington, DC, USA,
1996.
|
|
23
|
Sioutas C, Koutrakis P and Burton RM: A
technique to expose animals to concentrated fine ambient aerosols.
Environ Health Perspect. 103:172–177. 1995.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chen LC and Nadziejko C: Effects of
subchronic exposures to concentrated ambient particles (CAPs) in
mice. V. CAPs exacerbate aortic plaque development in
hyperlipidemic mice. Inhal Toxicol. 17:217–224. 2005.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Imrich A, Ning Y and Kobzik L: Insoluble
components of concentrated air particles mediate alveolar
macrophage responses in vitro. Toxicol Appl Pharmacol. 167:140–150.
2000.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Arhi CS, Bottle A, Burns EM, Clarke JM,
Aylin P, Ziprin P and Darzi A: Comparison of cancer diagnosis
recording between the Clinical Practice Research Datalink, Cancer
Registry and Hospital Episodes Statistics. Cancer Epidemiol.
57:148–157. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wallace TM, Levy JC and Matthews DR: Use
and abuse of HOMA modeling. Diabetes Care. 27:1487–1495.
2004.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yip WCY, Sequeira IR, Plank LD and Poppitt
SD: Prevalence of Pre-Diabetes across Ethnicities: A review of
impaired fasting glucose (IFG) and impaired glucose tolerance (IGT)
for classification of dysglycaemia. Nutrients. 9(9)2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ma X, Jia H, Sha T, An J and Tian R:
Spatial and seasonal characteristics of particulate matter and
gaseous pollution in China: Implications for control policy.
Environ Pollut. 248:421–428. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Carrero JA, McCarthy DP, Ferris ST, Wan X,
Hu H, Zinselmeyer BH, Vomund AN and Unanue ER: Resident macrophages
of pancreatic islets have a seminal role in the initiation of
autoimmune diabetes of NOD mice. Proc Natl Acad Sci USA.
114:E10418–E10427. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Rakotoarivelo V, Lacraz G, Mayhue M, Brown
C, Rottembourg D, Fradette J, Ilangumaran S, Menendez A, Langlois
MF and Ramanathan S: Inflammatory cytokine profiles in visceral and
subcutaneous adipose tissues of obese patients undergoing bariatric
surgery reveal lack of correlation with obesity or diabetes.
EBioMedicine. 30:237–247. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Coppack SW: Pro-inflammatory cytokines and
adipose tissue. Proc Nutr Soc. 60:349–356. 2001.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wentworth JM, Naselli G, Brown WA, Doyle
L, Phipson B, Smyth GK, Wabitsch M, O'Brien PE and Harrison LC:
Pro-inflammatory CD11c+CD206+ adipose tissue
macrophages are associated with insulin resistance in human
obesity. Diabetes. 59:1648–1656. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Biden TJ, Boslem E, Chu KY and Sue N:
Lipotoxic endoplasmic reticulum stress, β cell failure, and type 2
diabetes mellitus. Trends Endocrinol Metab. 25:389–398.
2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Pope CA III, Bhatnagar A, McCracken JP,
Abplanalp W, Conklin DJ and O'Toole T: Exposure to fine particulate
air pollution is associated with endothelial injury and systemic
inflammation. Circ Res. 119:1204–1214. 2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Bai Y and Sun Q: Fine particulate matter
air pollution and atherosclerosis: Mechanistic insights. Biochim
Biophys Acta. 1860:2863–2868. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Tian Y, Xiang X, Wu Y, Cao Y, Song J, Sun
K, Liu H and Hu Y: Fine particulate air pollution and first
hospital admissions for ischemic stroke in Beijing, China. Sci Rep.
7(3897)2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Fleisch AF, Gold DR, Rifas-Shiman SL,
Koutrakis P, Schwartz JD, Kloog I, Melly S, Coull BA, Zanobetti A,
Gillman MW, et al: Air pollution exposure and abnormal glucose
tolerance during pregnancy: The project Viva cohort. Environ Health
Perspect. 122:378–383. 2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Pearson JF, Bachireddy C, Shyamprasad S,
Goldfine AB and Brownstein JS: Association between fine particulate
matter and diabetes prevalence in the U.S. Diabetes Care.
33:2196–2201. 2010.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Chuang KJ, Yan YH, Chiu SY and Cheng TJ:
Long-term air pollution exposure and risk factors for
cardiovascular diseases among the elderly in Taiwan. Occup Environ
Med. 68:64–68. 2011.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Khafaie MA, Salvi SS, Ojha A, Khafaie B,
Gore SD and Yajnik CS: Particulate matter and markers of glycemic
control and insulin resistance in type 2 diabetic patients: Result
from Wellcome Trust Genetic study. J Expo Sci Environ Epidemiol.
28:328–336. 2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Ding S, Yuan C, Si B, Wang M, Da S, Bai L
and Wu W: Combined effects of ambient particulate matter exposure
and a high-fat diet on oxidative stress and steatohepatitis in
mice. PLoS One. 14(e0214680)2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Rajagopalan S, Park B, Palanivel R,
Vinayachandran V, Deiuliis JA, Gangwar RS, Das L, Yin J, Choi Y,
Al-Kindi S, et al: Metabolic effects of air pollution exposure and
reversibility. J Clin Invest. 130:6034–6040. 2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Shoenfelt J, Mitkus RJ, Zeisler R, Spatz
RO, Powell J, Fenton MJ, Squibb KA and Medvedev AE: Involvement of
TLR2 and TLR4 in inflammatory immune responses induced by fine and
coarse ambient air particulate matter. J Leukoc Biol. 86:303–312.
2009.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Zhao C, Liao J, Chu W, Wang S, Yang T, Tao
Y and Wang G: Involvement of TLR2 and TLR4 and Th1/Th2 shift in
inflammatory responses induced by fine ambient particulate matter
in mice. Inhal Toxicol. 24:918–927. 2012.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Jin Y, Wu W, Zhang W, Zhao Y, Wu Y, Ge G,
Ba Y, Guo Q, Gao T, Chi X, et al: Involvement of EGF receptor
signaling and NLRP12 inflammasome in fine particulate
matter-induced lung inflammation in mice. Environ Toxicol.
32:1121–1134. 2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Li Z, Wu Y, Chen HP, Zhu C, Dong L, Wang
Y, Liu H, Xu X, Zhou J, Wu Y, et al: MTOR suppresses environmental
particle-induced inflammatory response in macrophages. J Immunol.
200:2826–2834. 2018.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Schulthess FT, Paroni F, Sauter NS, Shu L,
Ribaux P, Haataja L, Strieter RM, Oberholzer J, King CC and Maedler
K: CXCL10 impairs beta cell function and viability in diabetes
through TLR4 signaling. Cell Metab. 9:125–139. 2009.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Lee T, Yun S, Jeong JH and Jung TW:
Asprosin impairs insulin secretion in response to glucose and
viability through TLR4/JNK-mediated inflammation. Mol Cell
Endocrinol. 486:96–104. 2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Liu C, Ying Z, Harkema J, Sun Q and
Rajagopalan S: Epidemiological and experimental links between air
pollution and type 2 diabetes. Toxicol Pathol. 41:361–373.
2013.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Ma QY, Huang DY, Zhang HJ, Wang S and Chen
XF: Exposure to particulate matter 2.5 (PM2.5) induced
macrophage-dependent inflammation, characterized by increased
Th1/Th17 cytokine secretion and cytotoxicity. Int Immunopharmacol.
50:139–145. 2017.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Mancini SJ, White AD, Bijland S,
Rutherford C, Graham D, Richter EA, Viollet B, Touyz RM, Palmer TM
and Salt IP: Activation of AMP-activated protein kinase rapidly
suppresses multiple pro-inflammatory pathways in adipocytes
including IL-1 receptor-associated kinase-4 phosphorylation. Mol
Cell Endocrinol. 440:44–56. 2017.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Aguirre V, Werner ED, Giraud J, Lee YH,
Shoelson SE and White MF: Phosphorylation of Ser307 in insulin
receptor substrate-1 blocks interactions with the insulin receptor
and inhibits insulin action. J Biol Chem. 277:1531–1537.
2002.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Dou L, Wang S, Sun L, Huang X, Zhang Y,
Shen T, Guo J, Man Y, Tang W and Li J: Mir-338-3p mediates
Tnf-A-induced hepatic insulin resistance by targeting PP4r1 to
regulate PP4 expression. Cell Physiol Biochem. 41:2419–2431.
2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Löfgren P, van Harmelen V, Reynisdottir S,
Näslund E, Rydén M, Rössner S and Arner P: Secretion of tumor
necrosis factor-alpha shows a strong relationship to
insulin-stimulated glucose transport in human adipose tissue.
Diabetes. 49:688–692. 2000.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Russo L and Lumeng CN: Properties and
functions of adipose tissue macrophages in obesity. Immunology.
155:407–417. 2018.PubMed/NCBI View Article : Google Scholar
|