Introduction
Uterine fibroid is a common tumor in women with a
relatively high prevalence rate in infertile patients (1). The tumor has smooth muscle and
fibroblast components besides a large amount of extracellular
matrix, which has an important influence on this disease. This is
considered as a type of common clonal tumor and is also known as
liomyoma or leiomyoma (2). Prior
studies have shown that estrogen and progesterone can increase the
growth rate of the tumor (3), while
causing a series of grave and chronic symptoms. Excessive
menstruation is the most common symptom, which can lead to anemia,
fatigue and pain. In some cases, it may cause aperiodic pain,
abdominal protrusion or pelvic pressure, which affects intestinal
function and causes constipation (4). In addition, uterine fibroids have a
great influence on the pregnancy rate of women (5,6).
Traditionally, surgery for uterine fibroids, such as
hysterectomy (7), requires open
surgery. Although these treatments are of great benefit in the
treatment of patients with uterine fibroids, these operations can
easily lead to a series of complications such as urinary tract
infection and pain (8). In recent
years, more laparoscopic therapies, such as laparoscopic
myomectomy, have been widely used for the treatment of these
patients. Laparoscopic myomectomy technique has surpassed
laparotomy and become the treatment option for many medical
institutions worldwide. Compared with traditional laparotomy,
laparoscopic myomectomy has several advantages. Some studies showed
that laparoscopic myomectomy reduced morbidity and hospital stays
compared with traditional surgical methods (9-12).
In this study, we compared the safety and efficacy
of the two methods of surgeries and their influence on the
pregnancy rate after surgery.
Materials and methods
General information
This is a retrospective study. In total, 86 cases
with uterine fibroids were selected among patients who were
admitted in Zhangqiu District Maternal and Child Health Care
Hospital during the period of April, 2016 to April, 2017. Patients
who underwent laparoscopic myomectomy were enrolled in group A
(n=42), and those that underwent traditional laparotomy were
included in group B (n=44). Patients in group A were 26-46 years of
age, with an average age of (35.59±4.02) years, and patients in
group B were 28-44 years, with an average age of (36.01±3.97).
Inclusion criteria were: i) Patients diagnosed with uterine
fibroids after gynecological examination. ii) Family members were
informed about this study. Exclusion criteria were: i) Age (<25
or ≥50); ii) primary ovarian insufficiency or tubal infertility;
iii) a history of hemorrhagic diseases.
This study was approved by the ethics committee of
the Zhangqiu District Maternal and Child Health Care Hospital.
Patients signed the informed consent.
Methods
Patients in group A (n=42) were treated with
laparoscopic myomectomy. Abdominal endoscopy was performed using a
10-mm endoscope equipped with a camera and a high-resolution
monitor (Storz-France).
The following instruments were used: Atraumatic
graspers, Semm fibroids for thermal coagulation, monopolar hooks,
Semm needle holders and suture forceps, pelvicleaner
(Storz-France). The instrument was introduced through three
suprapubic puncture sites (diameter, 5 mm). Laparoscopic myomectomy
was performed in all cases according to the principle of
non-invasive infertility surgery: Enlargement, careful hemostasis
and irrigation with saline. Prior to surgery, the patient was
required to first empty the bladder, then undergo general
anesthesia, select the bladder lithotomy position and indwelling
catheter. A 1-cm incision was made in the skin of the umbilicus
margin, and a pneumoperitoneum needle was inserted to construct a
carbon dioxide pneumoperitoneum with a pressure of 12-14 mmHg.
Subsequently, a laparoscopy device was inserted. Laparoscopy can
prevent myometrial fragmentation after interstitial myomectomy or
prevent the risk of large area (>1 cm2) adhesion
after myomectomy by suturing a fine-closed uterine incision. The
uterus was cut into one or two layers according to the depth of the
incision, interrupting or running 3-0 Vicryl (Polyglactine 910, 20
mm needle; Ethicon) or 4-0 PDS (Polydioxanon, 20-mm needle;
Ethicon) suture. After enlarging the incision (20 mm) with a single
tooth retractor, myoma was removed through the suprapubic puncture
site. The uterine incision was transparently closed using a classic
needle hub placed via the suprapubic incision under laparoscopic
control. In all cases, the peritoneal cavity was flushed with
saline solution after the surgery was terminated.
Patients in group B (n=44) were treated via
traditional laparotomy. For laparoscopic myomectomy, the patient
took the supine position after anesthesia, and a longitudinal
incision was made in the middle of the lower abdomen. After slow
injection of 20 ml of normal saline + 6 U of pituitrin into the
myometrium, blunt separation was performed along the surface of the
myoma capsule until reaching the area with more basal blood
vessels. The myoma was then removed after clamping, and the
myometrium and serosa were sutured.
Birth control lasted for 1 year for patients with
large and frequent fibroids who underwent the intrauterine
operation. This period was 6 months for those who did not undergo
the intrauterine operation, and 3 months for patients without
obvious uterine fibroids under the serosa.
Observation indicators
There were six observation indicators: i) The
general linear data and operative indicators were compared. No
significant differences were observed in the general data between
the two groups (P>0.05). The operative indicators of patients in
groups A and B, including average time of operation, intraoperative
blood loss, hospital stays and anal exhaust time was also
compared.
ii) The pain levels of patients in the two groups
were compared at 3, 6 and 18 h after surgery. The pain levels of
the two groups were compared using the Visual Analogue Scale/Score
(VAS) (13), with a score range of
0-10 points, and the score was proportional to the pain level.
iii) One week following surgery, the expression
levels of IFN-γ, IL-6 and VEGF in the serum were compared., between
the two groups.
iv) The total effective rate was compared between
the two groups. Evaluation criteria were: Markedly effective,
uterine fibroids were completely excised without complications;
effective, uterine fibroids were basically excised with no
complications or complications could be recovered; ineffective,
could not meet the effective standard. Total effective rate was
calculated as marked efficiency + effective rate.
v) Comparison of the pregnancy rate after surgery
between the two groups. Since the patients were childbearing age,
the pregnancy rate after surgery between the two groups was
compared. In order to investigate their pregnancy rate, follow-up
visits were made after 6, 12, 18 and 24 months following the
surgery.
vi) Complications observed in both groups were
compared: There were three common postoperative complications after
uterine fibroids and other laparoscopic surgery and laparotomy,
i.e., urinary tract infection (14), incision pain (15), and pelvic adhesions (16). The complications were investigated
and the incidence of complications was counted.
Statistical analysis
SPSS 19.0 (Asia Analytics Formerly SPSS) was used
for statistical analysis of comprehensive data. The measurement
data were expressed as mean ± standard deviation. Independent
samples t-tests was performed, and multiple group comparisons were
performed using analysis of variance followed by LSD test. The
count data were expressed by rate and composition ratio, and the
Chi-square test was performed. P<0.05 indicated a statistically
significant difference.
Results
Comparison of the general clinical
baseline data of the two groups
There was no statistically significant difference in
the general clinical baseline data including age, hypertension,
hyperlipidemia, diabetes, personal hobbies such as smoking and
drinking, between the groups (P>0.05) (Table I).
 | Table IGeneral clinical baseline data of
groups A and B [n (%)] (mean ± SD). |
Table I
General clinical baseline data of
groups A and B [n (%)] (mean ± SD).
| Variable | Group A (n=42) | Group B (n=44) | t/χ2 | P-value |
|---|
| Age (years) | 35.59±4.02 | 36.01±3.97 | 0.49 | 0.63 |
| Unfertile phase
(month) | 44.57±20.67 | 41.99±20.17 | 0.59 | 0.560 |
| Body mass index
(kg/m2) | 19.04±3.18 | 19.15±2.64 | 0.17 | 0.862 |
| Total number of
myomas | 2.75±1.98 | 2.94±1.53 | 0.50 | 0.619 |
| Total number of large
myomas | 1.12±0.33 | 1.09±0.29 | 0.45 | 0.655 |
| Size of large large
myomas (cm) | 7.47±2.60 | 7.07±2.54 | 0.72 | 0.473 |
| Smoking | | | 0.18 | 0.673 |
|
Yes | 23 (54.76) | 24 (54.55) | | |
|
No | 19 (45.24) | 20 (45.45) | | |
| Drinking | | | 0.19 | 0.666 |
|
Yes | 22 (52.38) | 21 (47.73) | | |
|
No | 20 (47.62) | 23 (52.27) | | |
| Obesity | | | 0.05 | 0.825 |
|
Yes | 20 (47.62) | 22 (50.00) | | |
|
No | 22 (52.38) | 22 (50.00) | | |
| History of
hypertension | | | 0.16 | 0.685 |
|
Yes | 23 (54.76) | 26 (61.90) | | |
|
No | 19 (45.24) | 18 (38.10) | | |
| History of
diabetes | | | 0.40 | 0.526 |
|
Yes | 21 (50.00) | 25 (56.82) | | |
|
No | 21 (50.00) | 19 (43.18) | | |
| Location of myomas
of patients | | | 0.68 | 0.711 |
|
Subserous
myomas (%) | 11 (25.00) | 12 (27.27) | | |
|
Intermural
myomas (%) | 29 (69.05) | 28 (63.64) | | |
|
Intra-uterine
myomas (%) | 2 (5.95) | 4 (9.09) | | |
Comparison of the surgical indicators
of patients between the two groups
The average time of operation, hospital stays,
intra-operative blood loss, and anal exhaust time in the group A
were (70.21±7.83) min, (8.12±2.01) days, (44.4±5.82) ml, and
(13.21±4.13) h, respectively. The average time of operation,
intra-operative blood loss, hospital stays, and anal exhaust time
in the group B were (100.23±38.34) min, (16.01±2.44) days,
(79.22±7.53) ml, and (29.25±5.37), respectively. By comparing the
post-treatment surgical indicators in the two groups, it could be
concluded that patients in group A were significantly better than
those in group B and the results were statistically significant
(P<0.001) (Table II).
 | Table IIComparison of surgical indicators of
patients between groups A and B. |
Table II
Comparison of surgical indicators of
patients between groups A and B.
| Variable | Group A (n=42) | Group B (n=44) | t | P-value |
|---|
| Average time of
operation (min) | 70.21±7.83 | 100.23±38.34 | 4.98 | <0.001 |
| Average length of
stay (days) | 8.12±2.01 | 16.01±2.44 | 16.32 | <0.001 |
| Average
intra-operative blood loss (ml) | 44.4±5.82 | 79.22±7.53 | 23.91 | <0.001 |
| Average anal
exhaust time (h) | 13.21±4.13 | 29.25±5.37 | 15.47 | <0.001 |
VAS score after surgery
The pain scores of group A were (4.21±0.83),
(2.56±0.67), (1.63±0.55) 3, 6 and 18 h after surgery, respectively,
while the pain scores of group B were (8.23±0.94), (5.54±0.85) and
(3.70±0.61) at T0, T1 and T2 after surgery, respectively. As for
intra-group comparison, the VAS score of the two groups decreased
from T0 to T2, and the difference was statistically significant
(P<0.05). As for comparison among groups, the VAS scores of
group A at different time points were significantly lower than
those of group B (P<0.05). More details are presented in
Table III.
 | Table IIIAverage VAS score tables of patients
in groups A and B at different time periods after surgery. |
Table III
Average VAS score tables of patients
in groups A and B at different time periods after surgery.
| Variable | Group A (n=42) | Group B (n=44) | t | P-value |
|---|
| Three hours after
surgery | 4.21±0.83 | 8.23±0.94 | 20.98 | <0.001 |
| Six hours after
surgery | 2.56±0.67 | 5.54±0.85 | 18.000 | <0.001 |
| Eighteen hours
after surgery | 1.63±0.55 | 3.70±0.61 | 16.500 | <0.001 |
| F | 149.40 | 337.10 | | |
| P-value | <0.001 | <0.001 | | |
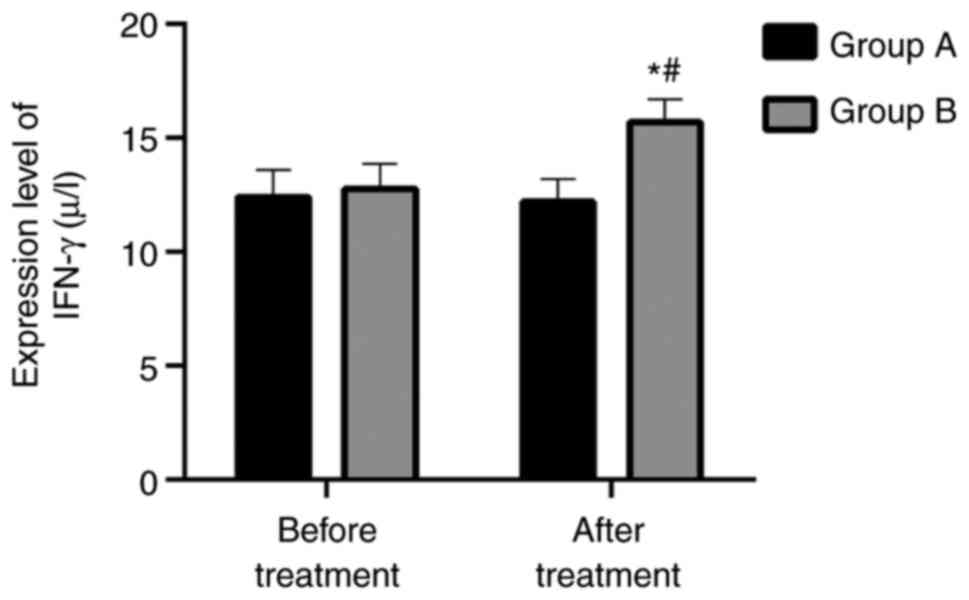
Levels of serum related inflammatory
factors in the two groups IFN-γ
Before and after treatment, the expression levels of
IFN-γ in group A were (12.39±1.20) µg/l and (12.18±1.01) µg/l,
respectively, while the expression levels of IFN-γ in group B were
(12.76±1.09) µg/l and (15.67±1.02) µg/l, respectively. There was no
significant difference between the two groups prior to treatment
(P>0.05). There was no significant difference in group A before
and after treatment (P>0.05). However, the expression level in
group B after treatment was higher than that before treatment
(P<0.05). After treatment, the expression level in group B was
higher than that of group A (P<0.05). More details are shown in
Fig. 1.
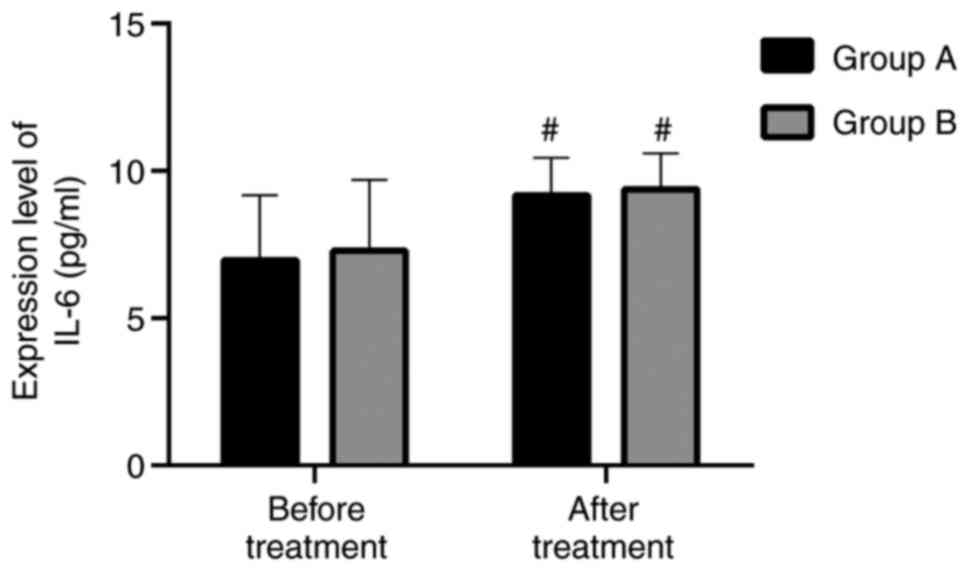
IL6 (pg/ml)
Before and after treatment, the expression levels of
IL6 in group A were (6.97±2.20) pg/ml and (9.16±1.29) pg/ml,
respectively, and the expression levels of IL6 in group B were
(7.28±2.41) pg/ml and (9.37±1.22) pg/ml, respectively. There was no
significant difference between the two groups before treatment
(P>0.05). The expression levels in both groups after treatment
were higher than those levels measured before treatment
(P<0.05). Nevertheless there was no significant difference
between the groups after treatment (P<0.05). More details are
shown in Fig. 2.
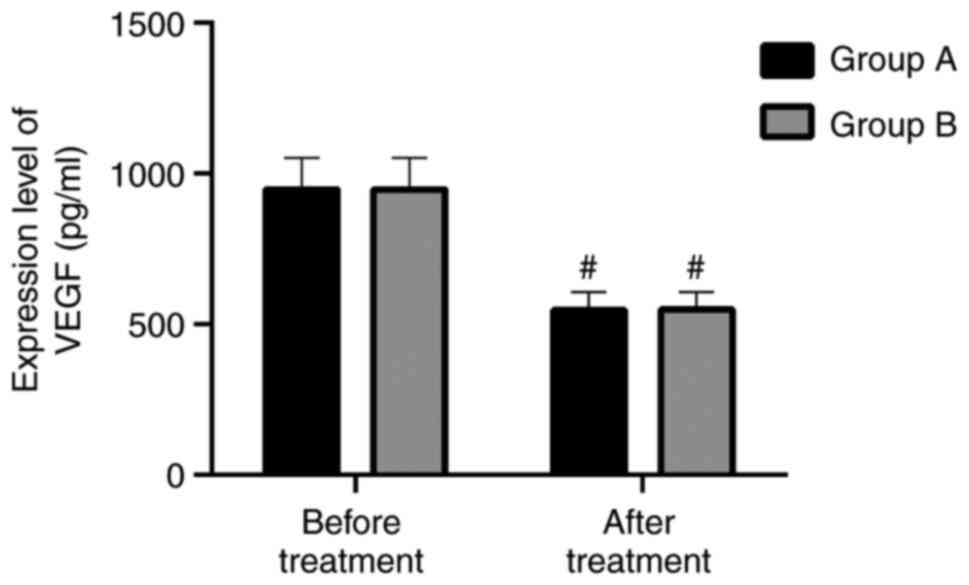
VEGF (pg/ml)
Before and after treatment, the expression levels of
VEGF in group A were (946.42±104.76) pg/ml and (547.36±57.67)
pg/ml, respectively, and the expression levels of VEGF in group B
were (946.55±104.91) pg/ml and (548.18±58.08) pg/ml, respectively.
There was no significant difference between the two groups prior to
treatment (P>0.05). The expression levels in the two groups
after treatment were higher than those levels registered before
treatment (P<0.05). There was no significant difference between
the groups after treatment (P<0.05). More details are presented
in Fig. 3.
Total effective rate of patients in
the two groups
Among the patients in group A, the total effective
rate was: In 22 cases, markedly effective; in 18 cases, effective
while 2 cases were ineffective. The overall total effective rate in
group A were 95.24%. In group B, 18 cases were markedly effective,
15 cases were effective while 11 cases were ineffective. The
overall total effective rate in group B was 75.00%. The total
effective rate of group A was significantly higher than that of
group B, and the difference was statistically significant
(P<0.05). More details are shown in Table IV.
 | Table IVTotal effective rate of patients in
the two groups. |
Table IV
Total effective rate of patients in
the two groups.
| Efficacy | Group A (n=42) | Group B (n=44) | χ2 | P-value |
|---|
| Markedly
effective | 22 (52.38) | 18 (40.91) | - | - |
| Effective | 18 (42.86) | 15 (34.09) | - | - |
| Ineffective | 2 (4.76) | 11 (25.00) | - | - |
| Total effective
rate (%) | 40 (95.24) | 33 (75.00) | 6.86 | 0.009 |
Comparison of the pregnancy rate after
surgery between the two groups
In group A, 9 patients were pregnant at 6 months
after surgery, with a pregnancy rate of 21.43%; 20 at 12 months
after surgery, with a pregnancy rate of 47.62%; 29 at 18 months
after surgery, with a pregnancy rate of 69.05% and 38 were pregnant
at 24 months after surgery, with a pregnancy rate of 90.48%. In
group B, 2 patients were pregnant at 6 months after surgery, with a
pregnancy rate of 4.55%; 10 at 12 months after surgery, with a
pregnancy rate of 22.73%; 19 were pregnant at 18 months after
surgery, with a pregnancy rate of 43.18%, and 26 at 24 months after
surgery, with a pregnancy rate of 59.09%. The pregnancy rate of
group A was significantly higher than that of group B at these four
time points. The difference was statistically significant
(P<0.05). More details are shown in Table V.
 | Table VComparison of pregnancy rates between
groups A and B. |
Table V
Comparison of pregnancy rates between
groups A and B.
| Variable | Group A (n=42) | Group B (n=44) | χ2 | P-value |
|---|
| Six months after
surgery | 9 (21.43) | 2 (4.55) | 5.13 | 0.024 |
| Twelve months after
surgery | 20 (47.62) | 10 (22.73) | 5.86 | 0.015 |
| Eighteen months
after surgery | 29 (69.05) | 19 (43.18) | 5.83 | 0.016 |
| Twenty-four months
after surgery | 38 (90.48) | 26 (59.09) | 11.12 | 0.001 |
Comparison of the complications of the
two groups
The postoperative complications including infection,
incision pain and pelvic adhesion were studied in both groups. In
group A, there was 1 case of infection, 1 case of incision pain and
2 cases of pelvic adhesion, with a total incidence rate of
complications of 9.52%. In group B, there were 4 cases of
infection, 6 cases of incision pain and 4 cases of pelvic adhesion,
with a total incidence rate of complications of 31.82%. The
incidence rate of complications after surgery in group A was
significantly lower than that of group B, with significant
difference (P<0.05). More details are presented in Table VI.
 | Table VIComparison of complications of
patients between the two groups. |
Table VI
Comparison of complications of
patients between the two groups.
| Variable | Group A (n=42) | Group B (n=44) | χ2 | P-value |
|---|
| Urinary tract
infection | 1 (2.38) | 4 (9.09) | - | - |
| Incision pain | 1 (2.38) | 6 (13.64) | - | - |
| Pelvic
adhesion | 2 (4.76) | 4 (9.09) | - | - |
| Incidence rate of
complications | 4 (9.52) | 14 (31.82) | 4.27 | 0.039 |
Discussion
Uterine fibroids are very common in gynecology, and
they have adverse effects on women and pregnancy (17,18).
However, it is very important to choose an effective therapy that
can effectively and safely treat uterine fibroids. The focus of the
present study was to compare laparoscopic myomectomy with
traditional laparotomy methods for treating uterine fibroids.
In this study, the average time of operation, blood
loss, hospital stays and exhaust time of groups A and B were
compared, and results showed that laparoscopic therapy had
significantly shorter time of operation, less blood loss and
significantly less hospital stays and average exhaust time. Results
obtained from prior studies revealed that laparoscopic myomectomy
could simply lead to serious blood loss, resulting in severe
problems such as increased incidence rate of postoperative
illnesses (19,20). However, the blood loss in the
laparoscopic myomectomy method is less than that of laparotomy.
Previous findings showed that compared with laparotomy,
laparoscopic myomectomy method significantly reduced blood loss
(21,22). In addition, compares to laparoscopy,
patients treated with laparoscopic myomectomy recover faster and
better from laparoscopy. Patients treated with laparoscopic
myomectomy also had a shorter hospital stay (23,24).
All these observations could explain the reason for the average
time of operation, blood loss and hospital stays of laparoscopic
myomectomy surgery being better than those of laparotomy.
Compared with laparotomy, laparoscopic myomectomy
could reduce postoperative pain by effectively reducing the
oxidative stress reaction of postoperative uterine fibroids
(25). Results obtained from
comparing the VAS scores between the two groups after 3, 6 and 12
h, demonstrated that patients in group B had a higher pain VAS
score. Bhave Chittawar et al reported that laparoscopic
myomectomy was a less painful surgery compared with traditional
laparotomy (26). Results showed
that laparoscopic surgery caused less postoperative pain compared
to traditional transabdominal surgery.
In the present study, we compared the levels of
serum IFN-γ, IL-6 and VEGF in both groups one week after surgery,
and found that the expression level of IFN-γ in group B after
treatment was significantly higher, while the levels of IL-6 and
VEGF between the two groups were not significantly different after
treatment. Prior findings showed that IFN-γ could inhibit tumor
level in uterine fibroids. High expression level of IFN-γ can
inhibit gonadotropin synthesis and affect the normal body function.
However, the expression level of IFN-γ after surgery in
laparoscopic myomectomy was lower than that in traditional
laparotomy, indicating that laparoscopic myomectomy could improve
IFN-γ and the efficacy was more significant than that of
traditional methods (27). By
comparing the postoperative serum factors such as IFN-γ and the
total effective rate of the disease in the two groups, it was shown
that laparoscopic hysteromyoma surgery has better efficacy than
traditional laparotomy.
The pregnancy rate for patients with uterine
fibroids is usually very low (28),
and this problem can be alleviated only through surgery. After
comparing the pregnancy rates of the two groups at different time
points (6, 12, 18 and 24 months) after surgery, we found that the
pregnancy rate after laparoscopic myomectomy was higher than that
of the alternative method. Results obtained from prior studies
indicated that uterine rupture caused by myomectomy was
particularly risky to pregnancy (29). Koo et al reported that the
uterine rupture caused by laparoscopy was a rare event (30) with minimal effects on pregnancy
rate. Shen et al also showed (31) that the pregnancy rate was higher
after laparoscopic myomectomy.
Sheyn et al reported that, compared with
traditional abdominal myomectomy, laparoscopic myomectomy had a
lower incidence rate of complications (32). The results of the present study
showed that the incidence rate of complications in patients treated
with laparoscopic myomectomy were significantly lower than that of
traditional laparotomy. Our findings are in accordance with
previous reports.
Other studies have reported a close association
among the size of fibroids, number of fibroids and the risk of
complications (33). We also should
not underestimate the importance of traditional laparotomy for
patients with numerous large fibroids (34,35).
From the incidence of these complications, combined
with the previous inflammatory factors, surgical indicators, VAS
scores, and pregnancy rate, patients who underwent laparoscopy have
smaller wounds, less bleeding volume, less inflammation, and less
pain than traditional open surgery. In this way, patients have
fewer postoperative complications and can recover faster. Owing to
its less pain and faster recovery, patients' quality of life is
less affected, which can be very beneficial to their chance for
future pregnancies. In the clinical study of Gueli Alletti et
al (36) on ovarian cancer, it
was found that if a patient needs to get a good recovery, he has to
stay positive, and negative emotions are likely to aggravate the
patient's condition. Therefore, it is necessary to avoid such
negative emotions in the clinical practice. The same is true for
the treatment of uterine fibroids. The use of laparoscopy is
currently a trend. If surgical methods are modified to reduce their
risks, the use of laparoscopy will be more widespread in the
future. In this case, the effect becomes higher, and it is more
beneficial for women's pregnancy rate.
There were some shortcomings associated with this
study, for example the variety of uterine fibroids was limited,
there were no patients with large myoma, and finally our sample
size was small. In summary, laparoscopic myomectomy on uterine
fibroids has advantages over traditional laparotomy. At the same
time, in the future research and treatment, the existing
laparoscopic therapy remains to be ameliorated, the risk of surgery
reduced and the efficacy of surgery should be improved.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XK and XS conceived and designed the study and
drafted the manuscript. LF and YH collected, analyzed and
interpreted the experimental data. JY and XY analyzed data and
revised the manuscript for important intellectual content. XK wrote
the manuscript. XK and LF are responsible for confirming
authenticity of the data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Zhangqiu District Maternal and Child Health Care Hospital. Patients
signed the informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zepiridis LI, Grimbizis GF and Tarlatzis
BC: Infertility and uterine fibroids. Best Pract Res Clin Obstet
Gynaecol. 34:66–73. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Grube M, Neis F, Brucker SY, Kommoss S,
Andress J, Weiss M, Hoffmann S, Taran FA and Krämer B: Uterine
fibroids-current trends and strategies. Surg Technol Int.
34:257–263. 2019.PubMed/NCBI
|
|
3
|
Sparić R: Uterine myomas in pregnancy,
childbirth and puerperium. Srp Arh Celok Lek. 142:118–124.
2014.PubMed/NCBI View Article : Google Scholar : (In Serbian).
|
|
4
|
Stewart EA, Cookson CL, Gandolfo RA and
Schulze-Rath R: Epidemiology of uterine fibroids: A systematic
review. BJOG. 124:1501–1512. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Levast F, Legendre G, Bouet PE and
Sentilhes L: Management of uterine myomas during pregnancy. Gynecol
Obstet Fertil. 44:350–354. 2016.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
6
|
De Vivo A, Mancuso A, Giacobbe A, Savasta
LM, De Dominici R, Dugo N, Dugo C and Vaiarelli A: Uterine myomas
during pregnancy: A longitudinal sonographic study. Ultrasound
Obstet Gynecol. 37:361–365. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Gil-Moreno A, Carbonell-Socias M, Salicrú
S, Bradbury M, García Á, Vergés R, Puig OP, Sánchez-Iglesias JL,
Cabrera-Díaz S, de la Torre J, et al: Nerve-sparing versus
non-nerve-sparing radical hysterectomy: Surgical and long-term
oncological outcomes. Oncotarget. 10:4598–4608. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mettler L, Schollmeyer T, Tinelli A,
Malvasi A and Alkatout I: Complications of uterine fibroids and
their management, surgical management of fibroids, laparoscopy and
hysteroscopy versus hysterectomy, haemorrhage, adhesions, and
complications. Obstet Gynecol Int. 2012(791248)2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Venturella R, Rocca ML, Lico D, La Ferrera
N, Cirillo R, Gizzo S, Morelli M, Zupi E and Zullo F: In-bag manual
versus uncontained power morcellation for laparoscopic myomectomy:
Randomized controlled trial. Fertil Steril. 105:1369–1376.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rossetti A, Sizzi O, Soranna L, Cucinelli
F, Mancuso S and Lanzone A: Long-term results of laparoscopic
myomectomy: Recurrence rate in comparison with abdominal
myomectomy. Hum Reprod. 16:770–774. 2001.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fujimoto A, Morimoto C, Hosokawa Y and
Hasegawa A: Suturing method as a factor for uterine vascularity
after laparoscopic myomectomy. Eur J Obstet Gynecol Reprod Biol.
211:146–149. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Solnik MJ and Munro MG: Indications and
alternatives to hysterectomy. Clin Obstet Gynecol. 57:14–42.
2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pointer JS: A novel visual analogue scale
(VAS) device: An instrument based on the VAS designed to quantify
the subjective visual experience. Ophthalmic Physiol Opt.
24:181–185. 2004.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chigbu B, Onwere S, Kamanu C, Aluka C,
Okoro O, Feyi-Waboso P and Onichakwe C: Lessons learned from the
outcome of bloodless emergency laparotomies on Jehovah's Witness
women presenting in the extremis with ruptured uterus. Arch Gynecol
Obstet. 279:469–472. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wu JL, Wang F, Liang X, Liang X, Xu CF and
Xin G: Effect of thoracoscopic esophagus cancer surgery on
postoperative incision pain as well as non-specific and specific
immune response. J Hainan Med University. 23:153–156. 2017.
|
|
16
|
Indar AA, Efron JE and Young-Fadok TM:
Laparoscopic ileal pouch-anal anastomosis reduces abdominal and
pelvic adhesions. Surg Endosc. 23:174–177. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ikhena DE and Bulun SE: Literature review
on the role of uterine fibroids in endometrial function. Reprod
Sci. 25:635–643. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sabry M and Al-Hendy A: Medical treatment
of uterine leiomyoma. Reprod Sci. 19:339–353. 2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Conforti A, Mollo A, Alviggi C,
Tsimpanakos I, Strina I, Magos A and De Placido G: Techniques to
reduce blood loss during open myomectomy: A qualitative review of
literature. Eur J Obstet Gynecol Reprod Biol. 192:90–95.
2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Clark NV, Wang KC, Opoku-Anane J,
Hill-Lydecker CI, Vitonis AF, Einarsson JI and Cohen SL: The
menstrual cycle and blood loss during laparoscopic myomectomy. Acta
Obstet Gynecol Scand. 96:1446–1452. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ji L, Jin L and Hu M: Laparoscopic
myomectomy with temporary bilateral uterine artery occlusion
compared with traditional surgery for uterine myomas: Blood loss
and recurrence. J Minim Invasive Gynecol. 25:434–439.
2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Choi SH, Hong S, Kim M, Bae HS, Kim MK,
Kim ML, Jung YW, Yun BS and Seong SJ: Robotic-assisted laparoscopic
myomectomy: The feasibility in single-site system. Obstet Gynecol
Sci. 62:56–64. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chen I, Lisonkova S, Joseph KS, Williams
C, Yong P and Allaire C: Laparoscopic versus abdominal myomectomy:
Practice patterns and health care use in British Columbia. J Obstet
Gynaecol Can. 36:817–821. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
D'Silva EC, Muda AM, Safiee AI and Ghazali
WAHW: Five-Year lapsed: Review of laparoscopic myomectomy versus
open myomectomy in putrajaya hospital. Gynecol Minim Invasive Ther.
7:161–166. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Tomasik P, Bomba-Opon D, Krupniewski L,
Palczewski P and Wielgos M: Evaluation of uterine myomas during
pregnancy using magnetic resonance imaging. Neuro Endocrinol Lett.
35:262–264. 2014.PubMed/NCBI
|
|
26
|
Bhave Chittawar P, Franik S, Pouwer AW and
Farquhar C: Minimally invasive surgical techniques versus open
myomectomy for uterine fibroids. Cochrane Database Syst Rev.
21(CD004638)2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ong SJ, Tang YZ and Shaida N: The role of
clinical radiology in the management of uterine fibroids. Br J Hosp
Med (Lond). 80:C66–C69. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Sunkara SK, Khairy M, El-Toukhy T, Khalaf
Y and Coomarasamy A: The effect of intramural fibroids without
uterine cavity involvement on the outcome of IVF treatment: A
systematic review and meta-analysis. Hum Reprod. 25:418–429.
2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Pakniat H, Soofizadeh N and Khezri MB:
Spontaneous uterine rupture after abdominal myomectomy at the
gestational age of 20 weeks in pregnancy: A case report. Int J
Reprod Biomed. 14:483–486. 2016.PubMed/NCBI
|
|
30
|
Koo YJ, Lee JK, Lee YK, Kwak DW, Lee IH,
Lim KT, Lee KH and Kim TJ: Pregnancy outcomes and risk factors for
uterine rupture after laparoscopic myomectomy: A single-center
experience and literature review. J Minim Invasive Gynecol.
22:1022–1028. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Shen Q, Chen M, Wang Y, Zhou Q, Tao X,
Zhang W and Zhu X: Effects of laparoscopic versus minilaparotomic
myomectomy on uterine leiomyoma: A meta-analysis. J Minim Invasive
Gynecol. 22:177–184. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sheyn D, Bretschnieder CE, Mahajan ST,
El-Nashar S, Billow M and Ninivaggio CS: Comparison of 30-day
complication between myomectomy and total hysterectomy for the
treatment of uterine fibroids in women older than age 40. J Minim
Invasive Gynecol. 26:1076–1082. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Lohle PNM, Higué D and Herbreteau D:
Uterine artery embolisation in women with symptomatic uterine
fibroids. Presse Med. 48:440–446. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kotani Y, Tobiume T, Fujishima R, Shigeta
M, Takaya H, Nakai H, Suzuki A, Tsuji I, Mandai M and Matsumura N:
Recurrence of uterine myoma after myomectomy: Open myomectomy
versus laparoscopic myomectomy. J Obstet Gynaecol Res. 44:298–302.
2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Rogers TS and Bieck AM: Management of
uterine fibroids. Am Fam Physician. 99:330–333. 2019.PubMed/NCBI
|
|
36
|
Gueli Alletti S, Vizzielli G, Lafuenti L,
Costantini B, Fagotti A, Fedele C, Cianci S, Perrone E, Gallotta V,
Rossitto C and Scambia G: Single-institution propensity-matched
study to evaluate the psychological effect of minimally invasive
interval debulking surgery versus standard laparotomic treatment:
From body to mind and back. J Minim Invasive Gynecol. 25:816–822.
2018.PubMed/NCBI View Article : Google Scholar
|