Introduction
There is an increasing incidence and prevalence of
cases of obstructive sleep apnea (OSA) syndrome worldwide. More
than 1 billion individuals are affected in developed countries, as
well as in middle- and low-income countries, regardless of the
northern or southern hemisphere (1). The most common tool used for the
assessment and management of OSA is the apnea-hypopnea frequency
per hour index (AHI). Nonetheless, newer tools, such as heart rate
variability (HRV) or oximetry and peripheral arterial tonometry
(PAT) are available (2). OSA has
systemic influence triggering or exacerbating cardiovascular
disease, a fact underlined by the correlation between the
cardio-ankle vascular index (CAVI), a measure of arterial
stiffness, and OSA severity (3).
Metabolic syndrome and obesity are strongly associated with OSA,
and current guidelines recommend targeting a normal body mass index
(BMI) before attempting any other treatment modalities (4). For the nasal obstruction component in
OSA syndrome, performing a complete flexible endoscopy and imaging
studies in order to exclude allergic rhinitis or tumors should be
considered (5). The first line of
treatment in OSA is continuous positive airway pressure (CPAP)
treatment, with a clear impact on the prevention of cardiovascular
risk (6). The increasing incidence
of OSA in the pediatric population, due to major lifestyle changes
with access to unhealthy food and decrease in physical activity, is
even more alarming (7). Surgery
should represent the last line in the treatment of OSA, procedures
ranging from turbinate reduction to uvulopalatopharyngoplasty and
maxillomandibular advancement (8).
The new situation of the COVID-19 pandemic brought to attention
other aspects of using CPAP and the risk of increasing air droplets
and aerosols in sleep medicine practice (9). Although the awareness of the general
population towards OSA and treatment modalities have increased,
patients with OSA still present an impaired quality of
socio-professional life (10).
The goal of the present study was to obtain and
analyze the data of patients with OSA recorded before the beginning
of the COVID-19 pandemic, and use these data in a future study
during and after the end of the pandemic.
Patients and methods
A retrospective study was conducted of cases of OSA,
diagnosed before the beginning of the COVID-19 pandemic, in order
to analyze the demographic, anthropometric and metabolic
characteristics correlated with the severity of OSA.
Study population
We gathered a study group of 80 adult male patients
with the following inclusion criteria: body mass index (BMI) ≥24,
associated major OSA symptoms, snoring and presenting an AHI ≥5.
This retrospective study was performed at the ‘Galenus’ Medical
Center, Targu Mures, Romania, on records dating from January to
December 2019, prior to the beginning of the Covid-19 pandemic.
Patients already diagnosed with OSA under treatment, pregnant
women, and patients with carcinomas were not included in the study
group. For more consistent statistical data we did not include the
very few female patients addressing to our clinic. All patients
signed a written consent for medical procedures and scientific
analysis of their data in accordance with the Declaration of
Helsinki. The study was supervised and approved by the Ethics
Committee of the ‘Galenus’ Medical Center (Targu Mures,
Romania).
Diagnostic procedures
According to our objectives, we queried our database
for variables recorded with metabolic blood tests, anthropometric
measurements, and polysomnography.
Polysomnography
We use a 6-h protocol for recording data during
physiological sleep using the SOMNOscreen™ Plus
(SOMNOmedics GmbH). The sleep study gathered data from
electroencephalography (EEG), electromyography, electrooculography,
pulse oximetry, heart rate, thorax movement and abdominal wall
movement. OSA is defined as the stop of respiration for at least 10
sec and maintaining respiratory effort. The reduction in airflow
below 50% for more than 10 sec and a decrease in O2
saturation with 3% defines hypopnea. AHI index was obtained by
dividing the number of sleep-related events to the number of sleep
hours. Respiratory disturbance index (RDI) was automatically
obtained from the polysomnography device.
Anthropometric measures
We recorded the height (cm) and weight (kg) of the
subjects, neck circumference (cm) at the level of the cricothyroid
membrane, abdominal circumference (cm) at the level of the
umbilicus with the patient in an erect position. Thus, we were able
to calculate the body mass index (BMI) for each subject.
Metabolic characteristics
Blood tests were performed in the morning after the
sleep study ended. We recorded serum concentration of HDL (mg/dl),
cholesterol (mg/dl), triglycerides (mg/dl) and testosterone
(nmol/l) using ARCHITECT ci4100 (Abbott).
Statistical analysis
The patients were divided into 3 subgroups according
to the AHI: subjects with snoring and AHI <15 were considered
low severity patients; subjects with snoring and AHI between 15 and
30 were medium severity patients; and subjects with AHI >30 were
considered to be high severity patients.
The data were analyzed using GraphPad Prism 7.01.
The threshold for statistical significance was 0.05. The
descriptive statistics for contiguous variables are presented as
mean ± [standard deviation (SD)]. Other data were analyzed using
the Kruskal-Wallis test. For the linear regression analysis, AHI
was defined as a dependent variable, in order to evaluate the
correlation between OSA severity and the characteristics studied
for each of the 3 subgroups.
Results
The low severity subgroup (Subgroup 1) included 14
cases with a mean age of 51.71 (±14.84 SD) years. The second
subgroup of medium severity (Subgroup 2) included 14 cases with a
mean age 49.07±10.52 years. The third subgroup of high severity
(Subgroup 3) included 52 cases with a mean age of 45.75±11.36
years. There were no statistical differences between the three
subgroups regarding age. All cases presented snoring, OSA symptoms
and BMI >24 (kg/m2). When comparing the BMI for
Subgroup 1, which was 28.41±4.172, for Subgroup 2, which was
31.61±4.317 and for Subgroup 3, which was 34.75±5.335, P=0.0005 was
obtained, a significant difference.
Table I summarizes
the anthropometric and metabolic characteristics of the study
groups. RDI was significantly different between the three subgroups
(P<0.0001). RDI was calculated as the number of apnea events/h
plus the number of hypopnea events/h plus the number of
respiratory-effort-related arousals (RERAs) per hour of sleep.
 | Table IAnthropometric and metabolic
characteristics of the 3 study subgroups with OSA. |
Table I
Anthropometric and metabolic
characteristics of the 3 study subgroups with OSA.
| Parameters | Abdomen circumference
(cm) | Neck circumference
(cm) | RDI | Testosterone
(nmol/l) | HDL (mg/dl) | Cholesterol
(mg/dl) | Triglycerides
(mg/dl) | AHI |
|---|
| 5≥ AHI <15
Subgroup 1 (n=14) | 118.9 (27.76) | 41.64 (2.925) | 78.14 (33.93) | 39.97 (23.27) | 42.59 (8.585) | 196.4 (28.43) | 95.5 (27.79) | 9.04 (2.37) |
| 15≥ AHI <30
Subgroup 2 (n=14) | 128.9 (17.63) | 43.36 (2.951) | 141.5 (62.29) | 22.49 (19.62) | 47.14 (8.486) | 208.5 (32.83) | 147.9 (69.83) | 21.69 (4.29) |
| AHI >30 Subgroup 3
(n=52) | 138.3 (23.34) | 45.46 (4.07) | 221.6(133) | 40.26 (25.26) | 42.6 (8.284) | 214.9 (36.99) | 164.9 (106.4) | 64.28 (19.58) |
| P-values | 0.0125 | 0.003 | <0.0001 | 0.6382 | 0.1118 | 0.2363 | 0.0752 | 0.10 |
Variables recorded for Subgroup 3 were significantly
higher regarding the abdominal and neck circumference.
Unfortunately, we could not correlate the AHI index
with the values recorded for testosterone, HDL cholesterol, total
cholesterol, and triglycerides.
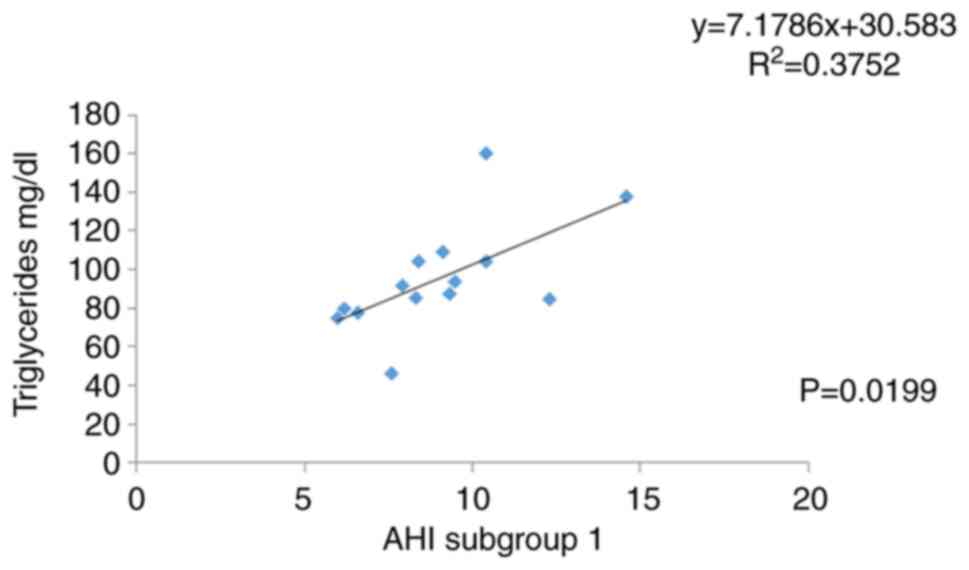
We discovered a significant correlation between the
level of triglycerides (mg/dl) and AHI in the low severity Subgroup
1 (R²=0.3752, P=0.0199; Fig.
1).
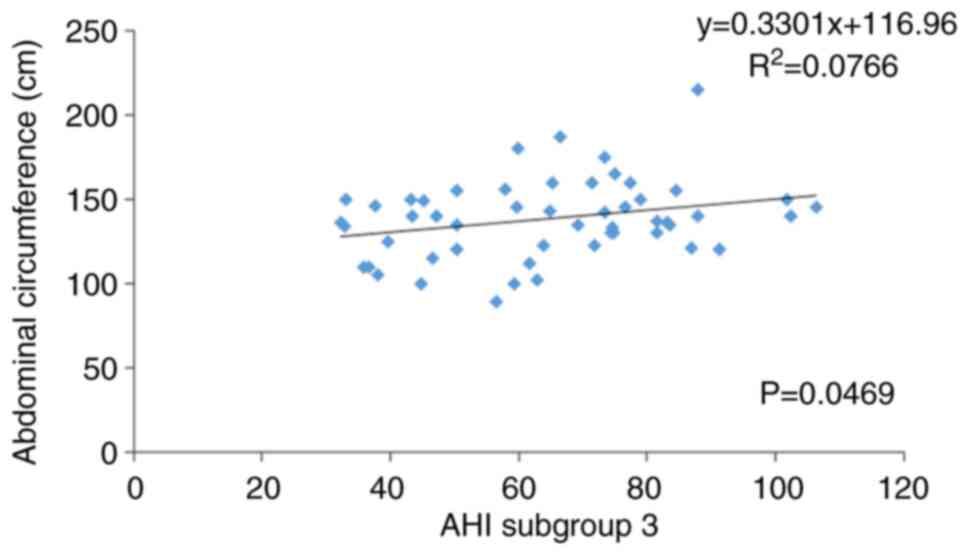
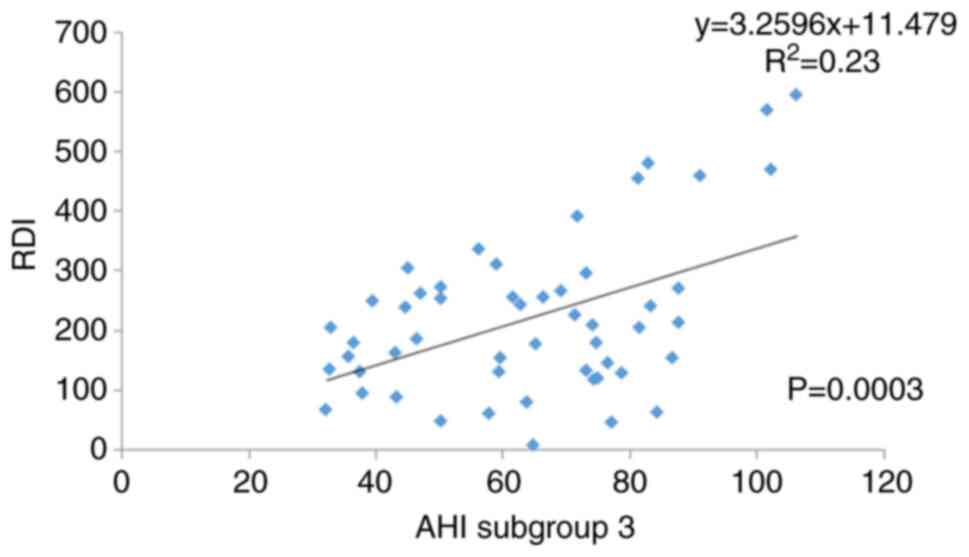
In the case of Subgroup 3 with severe OSA, we
discovered a correlation between the AHI and abdominal
circumference (cm) (R²=0.0766, P=0.0469; Fig. 2) and between OSA (AHI) and the RDI
(R²=0.23, P=0.0003; Fig. 3).
Discussion
In Romania, we recorded a low addressability of
females towards sleep clinics, mainly due to socio-cultural
background and the fact that males develop the clinical background
for obstructive sleep apnea (OSA) (11). Metabolic syndrome is one of the
factors that aggravates the symptoms of OSA. However, due to our
small study group, we could not correlate plasmatic levels of
cholesterol with OSA severity in the subgroups (12). Currently, we have observed an
increase in BMI values due to life style changes and a decrease in
height in the general population (13). Moreover, OSA cases tend to be
associated also with laryngopharyngeal reflux (14). There is also an increased number of
cases associated with thyroid pathology and OSA (15). One aspect of our study is that we
eliminated the few female patients we had from our study group for
a more consistent statistical power. A future goal of our research
could include analysis of the influence of female hormonal changes
on OSA aggravation (16,17). Our data are consistent with other
studies in developing countries such as Iran regarding body mass
index (BMI) over 35 kg/m2, age over 50 years, neck
circumference over 43 cm in men, and OSA patients worldwide face
increased risks due to the COVID-19 pandemic (18). The COVID-19 pandemic has limited the
access of patients with OSA to healthcare services and this has
diminished their quality of life (19). Cases with OSA should be recommended
to undergo vaccination against SARSCov2 with priority (20).
Conclusion
In conclusion, our data regarding demographic,
anthropometric and metabolic characteristics of OSA patients are
consistent with literature reviews. However, there are some aspects
specific to our country. The current data set was obtained prior to
the unfolding of the COVID-19 pandemic, and we plan to use them as
reference for a future comparative study regarding OSA challenges
during the pandemic.
Acknowledgements
Professional editing, linguistic and technical
assistance performed by Irina Radu, Individual Service
Provider.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
AN and AC contributed substantially to the
conception and design of the study, the acquisition, analysis, and
interpretation of the data, and were involved in the drafting of
the manuscript. DV and MD contributed substantially to the analysis
and interpretation of the data and were involved in the drafting of
the manuscript. RC contributed substantially to the interpretation
of the data and was involved in the critical revisions of the
manuscript for important intellectual content. AN, AC and RC were
responsible for confirming the authenticity of all raw data. All
authors agreed to be accountable for all aspects of the work in
ensuring that questions related to the accuracy or integrity of any
part of the work are appropriately investigated and resolved. All
authors read and approved the final version of the manuscript for
publication.
Ethics approval and consent to
participate
The study followed the international regulations in
accordance with the Declaration of Helsinki. The study was approved
by the Ethics Committee of Galenus Medical Center (no. 20210105).
Patient informed consent for publication of the data/images
associated with the manuscript was obtained.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cao W, Luo J and Xiao Y: A review of
current tools used for evaluating the severity of obstructive sleep
apnea. Nat Sci Sleep. 12:1023–1031. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
O'Mahony AM, Garvey JF and McNicholas WT:
Technologic advances in the assessment and management of
obstructive sleep apnoea beyond the apnoea-hypopnoea index: A
narrative review. J Thorac Dis. 12:5020–5038. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tomita Y and Kasai T: Relationship between
cardio-ankle vascular index and obstructive sleep apnea. Rev
Cardiovasc Med. 21:353–363. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Enache G, Rusu E, Ilinca A, Rusu F,
Costache A, Jinga M, Pănuş C and Radulian G: Prevalence of
overweight and obesity in a Roma population from southern
Romania-Calarasi county. Acta Endocrinol (Buchar). 14:122–130.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Vrinceanu D, Dumitru M, Stefan A, Neagos
A, Musat G and Nica EA: Severe DRESS syndrome after carbamazepine
intake in a case with multiple addictions: A case report. Exp Ther
Med. 20:2377–2380. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Resano-Barrio MP, Arroyo-Espliguero R,
Viana-Llamas MC and Mediano O: Obstructive sleep apnoea syndrome:
Continuous positive airway pressure therapy for prevention of
cardiovascular risk. Eur Cardiol. 15(e65)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Verhulst S: Long term continuous positive
airway pressure and non-invasive ventilation in obstructive sleep
apnea in children with obesity and down syndrome. Front Pediatr.
8(534)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tserenpil G, Gebre M, Zergham AS, Sekhon
AK and Malik BH: Managements for obstructive sleep apnea in adults:
Review. Cureus. 12(e9905)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Voulgaris A, Ferini-Strambi L and
Steiropoulos P: Sleep medicine and COVID-19. Has a new era begun?
Sleep Med. 73:170–176. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Neagos A, Costache A, Gheorghe D, Necula
V, Martu C, Paduraru L, Budacu C, Olariu R, Vrinceanu D, Hinganu D,
et al: Sleep disturbances and their impact on socio-professional
capacities in patients with obstructive sleep apnea. Rev Cercet
Interv So. 72:338–352. 2021.
|
|
11
|
Bonsignore MR, Saaresranta T and Riha RL:
Sex differences in obstructive sleep apnoea. Eur Respir Rev.
28(190030)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Borel AL: Sleep apnea and sleep habits:
Relationships with metabolic syndrome. Nutrients.
11(2628)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rundo JV: Obstructive sleep apnea basics.
Cleve Clin J Med. 86 (9 Suppl 1):S2–S9. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bărboi OB, Prelipcean CC, Cobzeanu MD,
Palade D, Albu-Soda A, Floria M, Chirilă I, Drug VL and Bălan G:
The tribes and tribulations of laryngopharyngeal reflux: A review
of recent studies with implications for interdisciplinary
collaborations between otolaryngologists and gastroenterologists.
Rev Med Chir Soc Med Nat Iasi. 119:967–973. 2015.PubMed/NCBI
|
|
15
|
Giulea C, Enciu O, Toma EA, Martin S, Fica
S and Miron A: Total thyroidectomy for malignancy-is central neck
dissection a risk factor for recurrent nerve injury and
postoperative hypocalcemia? A tertiary center experience in
Romania. Acta Endocrinol (Buchar). 5:80–85. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lee J, Han Y, Cho HH and Kim MR: Sleep
disorders and menopause. J Menopausal Med. 25:83–87.
2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zgură A, Galeş L, Hăineală B, Brătilă E,
Mehedinţu C, Andreescu CV, Berceanu C, Petca A, Barac RI, Ionescu A
and Anghel R: Correlations between known prognostic markers and
tumor-infiltrating lymphocytes in breast cancer. Rev Chim.
70:2362–2366. 2019.
|
|
18
|
Sarokhani M, Goli M, Salarvand S and
Ghanei Gheshlagh R: The prevalence of sleep apnea in Iran: A
systematic review and meta-analysis. Tanaffos. 18:1–10.
2019.PubMed/NCBI
|
|
19
|
Docea AO, Tsatsakis A, Albulescu D,
Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou
M, Drakoulis N, et al: A new threat from an old enemy: Re-emergence
of coronavirus (Review). Int J Mol Med. 45:1631–1643.
2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Calina D, Docea AO, Petrakis D, Egorov AM,
Ishmukhametov AA, Gabibov AG, Shtilman MI, Kostoff R, Carvalho F,
Vinceti M, et al: Towards effective COVID-19 vaccines: Updates,
perspectives and challenges (Review). Int J Mol Med. 46:3–16.
2020.PubMed/NCBI View Article : Google Scholar
|