Introduction
In Romania, the incidence of breast cancer is
constantly on the increase with a higher distribution in urban
areas, being the first cause of mortality (8.68%) in women aged
between 15 and 49 years and the third cause for women aged 50-69
years, after cardiovascular pathology (1).
Treatment in breast cancer is multidisciplinary,
being individualized according to several factors such as the
histological type of the tumor, its size, the presence or absence
of lymphadenopathy, the patient's age and other associated risk
factors or comorbidities. The treatment of choice remains surgery
in combination with adjuvant therapies such as hormone therapy,
immunotherapy, radiotherapy or chemotherapy, considerably
increasing life expectancy, especially in the early stages of the
disease. In the late stages, the primary aim is palliation and
improving the quality of life. Early diagnosis is vital, thus
periodic mammographic evaluation of the female population is the
main way in which early forms of breast cancer can be detected.
Confirmation of the diagnosis of malignancy is the first and most
important stage in the management of this disease, being decisive
for the patient's prognosis (2).
Surgical resection is one of the first effective
treatments utilized in breast cancer and continues to play a
critical role in the treatment of this pathology. The current
standard is the multidisciplinary approach involving a coordinated
effort of the surgeon and oncologist to achieve the best possible
result.
The main aim of the present study was a comparative
analysis of patients who have benefited from modern multimodal
treatment versus those who have benefited exclusively from surgical
treatment. At the same time, the importance of the applicability of
hormonal treatment depending on the immunohistochemical result and
the adjuvant radiotherapy treatment was considered, in order to
reduce the loco-regional recurrence.
Given the continuous advances in modern breast
biopsy techniques, a comparative analysis of the patients included
in the study group was performed depending on the type of biopsy
performed. The comparative analysis was also followed up depending
on the type of surgery and the impact on postoperative
complications.
Patients and methods
Patient data
The present study is an extensive retrospective one
on 125 patients with breast cancer hospitalized between January
2015 and December 2020, in the First Surgery Department, Sibiu
County Emergency Clinical Hospital (Sibiu, Romania). The
statistical research was performed based on data from the analysis
of observation sheets from the SCJU Sibiu archive, operating
protocols, laboratory and intensive care. Patients diagnosed with
intraoperative and preoperative breast cancer based on biological
and imaging investigations were included in the study. Breast
cancer patients who underwent prior surgery and presented to our
clinic directly with relapses, cases in which patients refused
surgical treatment, as well as patients diagnosed with benign
tumors, were excluded.
A study protocol was developed to analyze the
particularities of each patient diagnosed with breast cancer,
selecting the necessary data from the observation sheet. Several
parameters, including the annual distribution of breast cancer
cases, patient demographics (age and environment), topographic
location of the tumor, unilateral or bilateral involvement,
staging, adjuvant/neoadjuvant chemotherapy, type of biopsy, type of
surgery, associated comorbidities, type of oncological treatment
applied depending on the immunohistochemical result, including
chemotherapy, biologic therapy and hormone therapy, histological
type of tumor and immediate postoperative complications, were
evaluated. Depending on these parameters, the evolution and
postoperative prognosis of the patients in the study group were
analyzed.
Ethics approval and consent
The study was conducted according to the World
Medical Association Declaration of Helsinki, and was waived for
ethical approval due to its retrospective nature. Written informed
consent was obtained from all 125 patients during the
hospitalization.
Results
Demographic and clinical
evaluation
A total of 125 patients that underwent surgery for
breast cancer between January 2015 and December 2020, were included
in the study group. There was a constant increase in the number of
breast cancer cases admitted to our clinic during the study period
from 13 cases admitted in 2015 (10.4%) to 42 cases in 2020 (33.6%).
One explanation may be the employment of the national screening
program, which allowed early diagnosis. On the other hand,
epidemiological studies showed a global increase in the incidence
of breast cancer in recent years, due both to higher addressability
and the development of screening modalities over time (3).
Regarding the demographic data of the patients, a
higher number of breast cancer patients were from urban areas,
i.e., 64 cases (77%) compared to rural areas, i.e., 19 cases (23%).
This was explained by the more developed health education system in
the urban areas, the greater accessibility of patients to medical
services and the possibility of earlier diagnosis.
Of the 125 patients included in the study group, the
majority were aged 51-70 years (52.8%), with a mean age of 67.3
years (Table I). The most frequent
location was encountered in the supero-external quadrant (48%),
followed by the infero-external quadrant (20.8%). This distribution
coincides with previously published findings, the most common
location of tumor formation being in the supero-external quadrant
and being associated with an improved prognosis, while tumors in
the central quadrant were associated with a more reserved prognosis
and mortality that was twice as high, most likely due to later
diagnosis of neoplasms with this localization (4). Bilateral involvement was diagnosed in
21%, more often in advanced cases and involving a genetic component
(Table I).
 | Table IDemographic and clinical evaluation
of the patients in the study group. |
Table I
Demographic and clinical evaluation
of the patients in the study group.
| Parameter | No (%) |
|---|
| Age | |
|
<40 | 8 (6.4) |
|
41-50 | 20(16) |
|
51-60 | 27 (21.6) |
|
61-70 | 39 (31.2) |
|
71-80 | 22 (17.6) |
|
>80 | 9 (7.2) |
| Comorbidities | |
|
Heart
disease | 68 (54.4) |
|
Liver
disease | 3 (2.4) |
|
Neurological
disorder | 16 (12.8) |
|
Diabetes | 21 (16.8) |
|
Hypothyroidism | 2 (1.6) |
|
Chronic
renal failure | 3 (2.4) |
|
Obesity | 12 (9.6) |
| Type of biopsy | |
|
Incisional
biopsy | 45 (36.4) |
|
Excisional
biopsy | 30 (23.6) |
|
Ultrasound
guided core needle biopsy | 27 (21.8) |
|
Fine needle
aspiration biopsy | 23 (18.2) |
| Tumor location
(quadrants) | |
|
Supero-external | 60(48) |
|
Infero-external | 26 (20.8) |
|
Central | 19 (15.2) |
|
Supero-internal | 11 (8.8) |
|
Infero-internal | 9 (7.2) |
| Uni-/bilateral
involvement | |
|
Unilateral | 99(79) |
|
Bilateral | 26(21) |
| Histopathological
type | |
|
Invasive
ductal carcinoma (NST) | 94(75) |
|
Invasive
lobular carcinoma | 19(15) |
|
Mixed or
unassociated carcinomas | 12(10) |
| Staging
(p-TNM) | |
|
Tis | 12 (9.6) |
|
I | 16 (12.8) |
|
II | 29 (23.2) |
|
III | 44 (35.2) |
|
IV | 24 (19.2) |
| Neoadjuvant
therapy | 101/125(81) |
|
Chemotherapy | |
|
Early
stages | 48/57 (84.2) |
|
Advanced
stages | 53/68 (77.9) |
| Chemotherapy +
biologic therapy anti Her-2 | 21 (16.8) |
| Chemotherapy +
hormone therapy | 38 (30.4) |
Staging of breast cancer is a mandatory step in the
diagnosis of this pathology, as it is essential to establish
therapeutic behavior and prognosis of patients. For the analysis of
the distribution of cases according to the stage of the disease,
the p-TNM staging indicated by the histopathological examination
was used. In the present study, most cases were diagnosed in stage
III disease (35.2%) and only 9.6% of cases were diagnosed in the
early stages of carcinoma in situ. The early stages at the
time of diagnosis have the advantage of a more favorable prognosis
and benefit from much less invasive treatments. The diagnosis of
breast cancer in advanced stages can be explained by the lack of
national screening programs, low level of education on maintaining
health and the importance of self-examination, and difficult access
to medical services and treatments. Thus, late diagnosis has major
consequences on the survival rate and quality of life, correlating
with more invasive treatments (5,6).
Breast cancer biopsy is the gold standard for
pathological evaluation guiding the therapeutic conduct for each
case. In the present study group, of the 125 cases, 55 (44%)
received a biopsy at our department, while for the remaining
patients the biopsy was performed in other departments, prior to
admission. The types of biopsies performed included incisional,
excisional biopsy, most patients benefited from incisional biopsy
(36.4%), followed by excisional biopsy (23.6%). Ultrasound guided
core needle biopsy (21.8%) and fine needle aspiration biopsy
(18.2%) were also used (Table I).
This result coincided with data from the literature, incisional
biopsy being indicated if the lesion was highly likely to be
malignant or could not be reached through needle biopsy. However,
while surgical methods of biopsy have a higher degree of accuracy,
they also have a higher degree of complications, such as bleeding
or infection compared to needle biopsy (7,8).
Recent findings, however, have shown that
imaging-guided percutaneous breast biopsies have almost completely
replaced diagnostic surgical excisions that have been associated
with longer hospitalization, higher costs, and possible
complications (9). In 2010, the
European Society of Breast Cancer Specialists, EUSOMA, suggested
that 90% of women with breast cancer (invasive or ductal carcinoma
in situ) should have a preoperative diagnosis by
percutaneous biopsy, which is essential in the management of breast
lesions (9).
Histopathological examination plays an important
role in selecting the therapeutic strategy in patients with breast
cancer that allows detailed analysis of the samples sent
(biopsy/surgery). The correct approach of the samples requires the
integration of both clinical and imaging results. The result
obtained after the histopathological examination, guides the
therapeutic options for each patient. The appearance of modern
molecular techniques has suggested the disappearance of
histopathological examinations. However, currently and in the near
future, this examination remains a key element of the integrated
multidisciplinary team involved in the treatment of patients with
malignant breast disease (10).
Considering the importance of the histopathological analysis, the
analysis of the study group according to this result was deemed
crucial, with the highlighting of the histological types of breast
neoplasm (Table I). Thus, of the
total number of patients included in the group, most were diagnosed
with NST invasive carcinoma representing 75% of the total group,
followed by invasive ductal carcinoma identified in 19 patients,
representing 15% of the total group. Other types of neoplasms,
mixed or non-associated, were identified in 12 patients. These
results coincided with data from the literature mentioning invasive
ductal carcinoma NST as the most common form of invasive breast
cancer (11).
The treatment of breast cancer has evolved over time
from a strictly surgical approach with an emphasis on loco-regional
disease control to multidisciplinary management, with an emphasis
on systemic therapy, significantly improving survival. The optimal
time of radio-chemotherapy in relation to operating time has been
studied for several decades, with solid evidence supporting the
neoadjuvant approach (12). The
study group was divided into two groups to evaluate the
applicability of neoadjuvant chemotherapy. Of the total patients
included in the group, 101 (81%) benefited from neoadjuvant
chemotherapy, of which 84.2% of the patients were diagnosed in
early stages and 77.9% of the patients were diagnosed in advanced
stages (Table I). Notably, in the
early stages, the percentage of patients who did not benefit from
neo-adjuvant chemotherapy was lower than that of patients in
advanced stages; 21 patients received biologic treatment with
anti-HER-2 in combination with neoadjuvant chemotherapy.
Neoadjuvant hormone therapy for intensely positive hormone
receptors but with HER-2 negative, was applied to 38 patients. Most
patients received sequential neoadjuvant chemotherapy, of whom 15
for early breast cancer and 27 for loco-regional advanced cancer
(Table I).
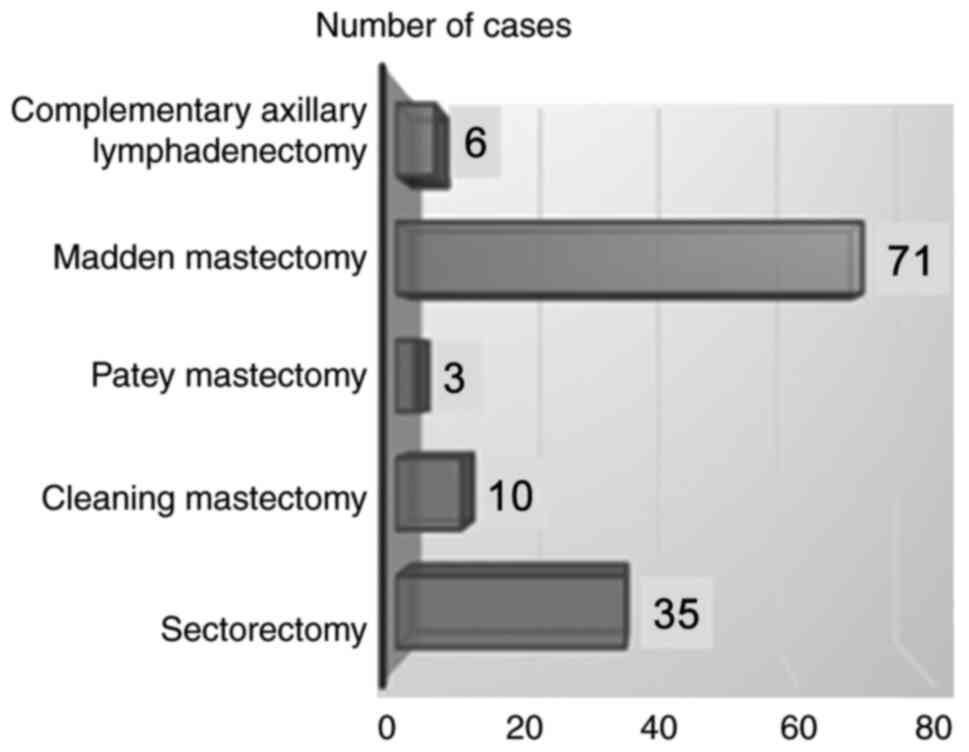
Surgical treatment in breast cancer plays a central
role, aiming at both the resection of the tumor in oncological
limits and a favorably aesthetic appearance. In the studied group,
the choice of surgical therapy was made depending on the stage,
histological type and size of the tumor, the general condition,
associated comorbidities and the patient's decision. Of note is the
fact that in the therapeutic decision of breast cancer, the
solution offered by the oncology commission had a categorical role,
each patient being presented to the oncology commission in order to
choose the optimal individualized therapeutic option. The most used
surgical technique was the Madden modified radical mastectomy,
performed in 54.16% of patients, which was associated with a lower
rate of postoperative complications and is less mutilating,
preserving both pectoral muscles compared to other radical surgical
techniques (13).
In 35 cases, conservative surgery was performed,
respectively, sectorectomy followed by axillary lymphadenectomy
(28%), followed by a cleaning mastectomy performed in 10 patients
and a complementary axillary lymphadenectomy, which was performed
in 6 cases due to local recurrence. The lowest percentage was
recorded at the modified radical Patey mastectomy, i.e., 3 patients
(2.4%) (Fig. 1).
The constant, slow growth each year included in the
current study, of conservative surgeries to the detriment of the
radical classical techniques is crucial. In 2015, 3 conservative
surgeries were performed, but they increased steadily to a peak in
2020 when 10 conservative surgeries were performed (Table II). The results obtained were
consistent with other clinical studies that showed a steady
increase in the number of patients receiving conservative surgery
over conventional ones (14).
 | Table IIAnnual distribution of performed
surgeries and complications in the study group. |
Table II
Annual distribution of performed
surgeries and complications in the study group.
| | Year |
|---|
| Performed
surgeries/complications | 2015 (%) | 2016 (%) | 2017 (%) | 2018 (%) | 2019 (%) | 2020 (%) | Total |
|---|
| No. of surgeries
for breast cancer, n (%) | 13 (10.4) | 14 (11.2) | 15(12) | 15(12) | 26 (20.8) | 42 (33.6) | 125 |
| No. of conservative
surgeries, n (%) | 3(23) | 4 (28.5) | 5(30) | 6(40) | 7 (26.9) | 10 (23.8) | 35 |
| Complications, n
(%) | 6(46) | 4 (28.5) | 4 (26.6) | 3(20) | 1 (3.8) | 1 (2.3) | 19 (15.2%) |
Associated comorbidities with accompanying life risk
play an important role in the prognosis and postoperative evolution
of the disease. These data correspond to those in the specialized
articles, the high rate of associated cardiovascular diseases can
be explained by the advanced age at which the neoplastic pathology
was diagnosed. There was also a significant increase in mortality
and an improved prognosis in patients with cardiovascular disease
and diabetes. The presence of these pathologies requires a
multidisciplinary approach and a much more complex therapeutic
strategy (15).
The most common immediate postoperative
complications in breast cancer are local. In the analyzed group,
immediate postoperative complications were present in 19 patients,
representing 15.2% of the studied group. Among the complications,
the most common was prolonged lymphorrhagia, present in 13 patients
(68.4%), while in 3 patients (15.8%) there was postoperative
hematoma. The rarest complications were represented by the wound
infection: 2 cases (10.5%) and the axillary lymphocele: 1 case
(5.3%). The results obtained were partially correlated with recent
data from the literature indicating seroma as the most common
postoperative complication followed by wound infection, hematoma
and flap necrosis (16). Of note is
the absence of seroma in patients who underwent surgery, which can
be explained by the use of drainage tubes at the end of the
surgery.
The study group was analyzed according to the annual
incidence of immediate postoperative complications. Thus, the
majority of complications occurred during the period 2015-2017 (14
patients) and the minority, in 2019 and 2020, each with one case
(Table II).
Correlating these results with the type of modern
surgery, an annual decrease in the number of immediate and late
postoperative complications can be observed, with the annual
increase in the number of conservative interventions. These results
coincide with specialized studies showing a decrease in the number
of patients with postoperative complications with the introduction
of conservative surgery (17).
Following a comparative study of postoperative complications after
mastectomy and conservative surgery, the latter has been shown to
be superior to modified mastectomy in the incidence of
postoperative complications (18).
Radiation therapy (RT) is an integrated component of the
multidisciplinary management of breast cancer, significantly
reducing locoregional recurrence and improving overall survival in
both patients undergoing breast-conserving surgery (BCS) and
patients with advanced breast cancer in which mastectomy is
performed (19). All 125 patients
in the study group underwent radiotherapy, of whom 80% received
adjuvant radiotherapy and 25 patients (20%) received palliative
radiotherapy.
These results correlate with specialized studies
demonstrating the efficacy of adjuvant radiotherapy by improving
local disease control and overall survival after mastectomy
(20). In addition, some randomized
studies have shown that adjuvant radiotherapy after conservative
breast surgery results in overall long-term survival, which are
comparable to modified radical mastectomy. Postoperative
radiotherapy leads to a significant reduction in local recurrences
compared to conservative surgical treatment, used as the only
therapeutic option. A recent meta-analysis of the ‘Early Breast
Cancer Trialists Collaborative Group (EBCTCG)’ highlighted the
major advantage of adjuvant radiotherapy after conservative surgery
in terms of survival in positive lymph node breast cancer. For most
older women diagnosed with early breast cancer, the current
standard treatment after BCS is adjuvant radiotherapy and adjuvant
endocrine therapy (21).
Discussion
In the present study, most of the patients were aged
between 50 and 70 years, which could be explained by longer
exposure to risk factors for breast cancer. Although breast cancers
diagnosed at older ages are more common and more numerous, they
have an improved prognosis, progress more slowly, and are less
aggressive than cancers diagnosed at a young age, where the genetic
component plays a key role (22).
Detection of BRCA1 and BRCA2 mutations can lead to
both a decrease in the incidence of breast cancer and a decrease in
morbidity through early detection. In addition, the early age
associated with the mutation of these genes has a major impact on
contralateral breast cancers (23).
Previous findings confirm the existence of an increased risk of
contralateral breast cancer in patients with this disease from
families with mutations in the BRCA1 and BRCA2 genes
(23). However, little information
is available on bilateral breast cancer in patients from families
at high risk for this disease but with negative results for
BRCA1 and BRCA2 gene mutations. A large multicenter
retrospective study of a group of 6,235 women with unilateral
breast cancer from high-risk families showed that the risk of
contralateral breast cancer was significantly higher in patients
from families with BRCA1 mutation compared to patients from
families with the BRCA2 gene mutation. In comparison,
patients from families testing negative for the BRCA 1-2
gene mutation have a much lower risk of developing contralateral
breast cancer (23). The same study
suggests that the cumulative risk of contralateral breast cancer,
25 years after the first breast cancer, was 44.1% in
BRCA1-positive patients, 33.5% in BRCA2-positive
patients, and only 17% in family patients. tested negative for the
BRCA genes. Family members with the BRCA1 mutation
had a 3-fold higher risk of breast cancer contralateral than family
members without the BRCA1-2 mutations (23).
Additionally, early age in the first breast cancer
was associated with a higher risk of bilateralization. In patients
who developed breast cancer prior to the age of 40, the cumulative
risk of contralateral breast cancer after 25 years was >55% for
BRCA1, >38% for BRCA2, and only 28.4% for patients
from families testing negative for the BRCA1 and 2 genes.
Compared to patients >50 years of age, the cumulative risk of
contralateral breast cancer after 25 years was >21% for
BRCA1, >15% for BRCA2 and 12.9% in patients from
BRCA1 and 2-negative families (23).
The therapy of patients with breast cancer involves
three main treatment modalities: surgical, systemic therapy and
radiotherapy. According to the national protocols, systemic therapy
was administered to patients with breast cancer after surgery.
However, previous findings suggest that systemic neoadjuvant
therapy (NA) is an equally effective option compared to adjuvant
therapy. Although neoadjuvant anti-hormone therapy is recommended
mainly for patients with positive hormone receptors in the
postmenopausal period, neoadjuvant chemotherapy is increasingly
used for all subtypes of breast cancer. It increases the rate of
breast preservation surgery and allows monitoring of the response
to treatment by providing unique opportunities for the development
of both individualized treatment strategies and the development of
new generation drugs. Modern treatment strategies are adapted to
molecular subtypes, allowing a more individualized approach to
therapy (24).
Tumor biopsy in the mammary gland is essential in
the diagnosis of breast cancer. Although it is a more or less
invasive method (depending on the type of biopsy), it allows the
diagnosis of certainty. In addition, it provides information on the
type of cancer and the degree of tumor differentiation. The biopsy
complements the information obtained from the clinical and imaging
examination so that the patient can benefit from a correct and
targeted treatment depending on the outcome of the
histopathological examination (7).
The cytological and histological diagnosis of a
palpable/nonpalpable mass can be obtained by performing a
percutaneous biopsy [fine needle aspiration biopsy (FNA) or cutting
needle biopsy (CNB)] or surgically (incisional or excisional
biopsy). Among the main objectives of percutaneous biopsy
techniques are: achieving the maximum degree of accuracy and
providing as much information about the tumor (histological type,
degree of differentiation, invasion, immunohistochemical data). To
achieve these goals, percutaneous biopsy devices have evolved from
fine needle aspiration, to CNB and later vacuum-assisted biopsy
(VAB) (8-10).
Currently, ultrasound-guided breast biopsy has become the first
choice for performing a percutaneous biopsy in most lesions
detected by ultrasonography. The sensitivity of the
ultrasound-guided biopsy is about 97.5%, which makes this technique
optimal for performing a breast biopsy. Ultrasound-guided needle
biopsy (CNB) is a modern, safe and accurate technique that is
currently considered the method of choice in all lesions classified
as BI-RADS 3, 4 and 5, while stereotaxis and MRI should be reserved
for lesions that are not clearly visible on ultrasound (25). Although incisional surgical biopsy
was the most commonly used type of biopsy, the trend is to replace
it with modern, minimally invasive techniques, represented by
imaging-guided core-needle biopsies (CNBs) that are cost effective,
and have fewer complications and high accuracy.
The histopathological examination of a breast biopsy
or fragment of surgery must specify the histological type of the
tumor, the histological grade and the performance of
immunohistochemistry tests (26).
The development and progression of breast cancer have been linked
to the interaction between tumor cells and the microenvironment
formed by breast cancer cells, fibroblasts, adipocytes, immune and
endothelial cells (27).
Angiogenesis is essential for the tumor to grow and it can be
considered as a specific mark of the neoplastic process (28). Immunohistochemical testing is a
special staining procedure performed on tissue fragments resulting
from biopsy and which reveals the presence or absence of hormone
receptors and/or HER2 receptors on the surface of cancer cells.
This information plays an essential role in the subsequent planning
of treatment (29). Hormone
receptors (estrogenic-ER and progesterone-PR) are specialized
proteins located on the surface or inside the neoplastic cell.
Cells of certain tumors have a higher number of hormone receptors,
thus indicating a favorable response to hormone therapy. Patients
who are positive for these receptors have a more favorable
prognosis and a higher survival rate (30). By contrast, patients with
triple-negative breast cancer, who are negative for ER and PR and
HER2 protein receptors have a more unfavorable prognosis and
hormone therapy is ineffective in this case (26,31).
Women with only one type of positive receptor but with the other
negative, can benefit from hormone therapy although the therapeutic
response is variable (32,33). The presence of tumor-infiltrating
lymphocytes is another important factor of prognosis, being
associated with a better neoadjuvant chemotherapy response and
prognosis in HER2+ and HER2-breast cancers (34).
HER2 protein has a significant role in inducing
breast carcinogenesis in vitro and in vivo.
HER2 gene amplification or overexpression occurs in
approximately 15-30% of cases of invasive breast cancer and has
implications for both predictive and prognostic implications
(10). Breast cancers with
HER2/neu gene amplification or HER2 protein
overexpression are known as HER2-positive breast cancer and
are associated with faster evolution and an increased risk of
recurrence compared to Her2-negative neoplasm. HER2 should be
determined in all patients with invasive breast cancer (9). Another useful test is the
determination of the Ki67 marker. This index of cell proliferation
is expressed as a percentage and is directly proportional to the
proliferative activity of the neoplastic cell. Low levels are
associated with low proliferative activity and high levels are
associated with an unfavorable prognosis (11).
Genetic factors are known as the main etiopathogenic
factors of breast cancer; thus, the genetic predisposition is
responsible for 3-10% of all cases of breast cancer and up to 30%
of all those with early onset. Hereditary breast cancer is
associated with mutations in the tumor suppressor genes
BRCA1 (17q21) and BRCA2 (13q12-13) (34). This type of neoplasia has an
autosomal dominant transmission, with more frequent appearance in
an early form, of high intensity and with a tendency to become
bilateral. Carriers of these mutations have a higher risk of
developing this disease but also other types of neoplasms, such as
ovarian cancer. These mutations are commonly seen in patients with
a family history and those affected by multiple forms of the
disease. Therefore, detecting mutations in these two genes is
important in counselling family members and reducing the incidence
of breast cancer. In the selection of patients for screening for
germline mutations in the BRCA1 gene, it is important to
combine information about family history, age of diagnosis, and
tumor morphology (34).
Hormonal factors are also correlated with the
incidence of breast cancer. Yalagachin et al found that the
prevalence of nodular goiter was higher in patients with malignant
breast diseases than patients with benign breast diseases; however,
the exact pathological mechanisms involved in these two diseases
are still a subject of research (35).
A new risk factor for breast cancer was reported,
i.e., breast augmentation surgery with silicone implant. In those
cases, the histopathological aspect encountered was that of
anaplastic large cell lymphoma (36). Surgeons should be aware of the
association, as the number of plastic surgeries is currently an
emerging trend.
A large part of the patients included in the study
group received neoadjuvant systemic treatment. These are part of
new treatment strategies adapted to molecular subtypes that allow
an individualized approach in the administration of therapy.
Adjuvant radiotherapy reduces locoregional
recurrence and improves overall survival, being an integral part of
the multidisciplinary treatment of breast cancer.
Surgical resection was the first effective treatment
for breast cancer and remains the most important treatment
modality. Improvements in surgical techniques, along with the use
of adjuvant radiotherapy and advanced chemotherapeutic agents, have
helped to orient them towards more focused and, at the same time,
less invasive surgical techniques. Surgical management of breast
cancer has changed, from extensive procedures with a fairly high
morbidity rate, to modern surgical techniques in order to achieve
the most favorable possible cosmetic result in tandem with adequate
cancer resection (37).
Recent clinical studies proved the importance of
neoadjuvant therapy in improving the possibility of resectability
and reducing intraoperative morbidity. In fact, neoadjuvant therapy
has other roles, including that it increases the likelihood of
conservative breast surgery in stage II-III patients who would
otherwise require mastectomy due to an unfavorable ratio between
breast and tumor formation, and reduces morbidity and the extent of
lymph node in patients with significant axillary metastases. After
neoadjuvant treatment, recommendations for surgery depend on the
extent of the disease at presentation, the patient's decision, and
the tumor response to systemic therapy. Modified radical mastectomy
remains the standard for patients with inflammatory breast cancer,
regardless of the response to neoadjuvant therapy (12,38).
Conservative surgery for breast cancer aims to
deliver a radical oncological result as effectively as possible,
with negative resection margins confirmed histopathologically, but
also with a favorable aesthetic appearance, which is extremely
important for preventing psychological distress and body image
disorders in breast cancer patients (39). Optimal local control of breast
cancer by this method can be achieved only in combination with
adjuvant radiotherapy, even if negative oncological margins have
been obtained, because cancer cells may be present in the
apparently unaffected breast tissue. In addition to being
equivalent to radical mastectomy in terms of oncological safety,
conservative surgery offers certain advantages in terms of quality
of life and aesthetic results. This type of surgery allows both the
preservation of the morphology of the breast and skin, as well as
the preservation of sensitivity with a much lower psychological
impact. Conservative surgery is currently the standard for patients
with invasive breast cancer in stage 0, I or II (40). However, some studies suggest a
higher incidence of locoregional recurrence in patients treated
with conservative surgery as opposed to those who received radical
surgical treatment (41,42).
Breast cancer continues to be a major public health
problem, with its incidence continuing to rise both nationally and
globally. Screening of patients with a genetic predisposition to
breast cancer is important. Most of the patients included in the
present study were diagnosed in advanced stages, with major
consequences on survival rate and quality of life.
The treatment of breast cancer has undergone
significant changes with the introduction of modern oncology and
conservative surgical options. The involvement of a
multidisciplinary team in this pathology represents the new
therapeutic standard for both patients and clinicians, being
individualized for each patient. The introduction of neoadjuvant
chemotherapy in the treatment of breast cancer has led to an
undeniable benefit both surgically and ontologically, it is
becoming increasingly used for all subtypes of breast cancer,
increasing the rate of conservative surgery. Immunohistochemical
testing for the detection of HER2 receptors, estrogenic and
progesterone, has an essential role in the subsequent planning of
individualized treatment.
Surgical treatment has been and will remain the most
important treatment for curative purposes. The most used surgical
technique was the modified Madden mastectomy, being preferred to
other radical surgical techniques. There is a steady annual
increase in the number of conservative surgeries to the detriment
of the radical radicals, which highlights the current trend towards
conservative surgery, being an integral part of modern treatment in
breast cancer. Postoperative complications were present in a small
number of patients, the most common being lymphorrhagia. The annual
increase in the number of conservative surgeries is associated with
an annual decrease in immediate and late postoperative
complications.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
CiT, DS, AM, BS, DOC and CP were involved in the
conception and design of this study. RC, AM, CP, GI, MST, CGS, LCT,
CoT and GAG were responsible for the data collection and analysis.
CiT, RC, CGS, LCT, MST and DS were responsible for drafting the
manuscript. GI, DOC, BS, CoT and GAG provided critical perspective
for important intellectual content. CiT, RC and AM are responsible
for confirming the authenticity of the raw data. The final version
was read and approved by all the authors.
Ethics approval and consent to
participate
The study was conducted according to the World
Medical Association Declaration of Helsinki, and was waived for
ethical approval by the Bioethics Committee due to its
retrospective nature. All patients previously signed written
informed consent in regards to hospitalization and
investigations.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Furtunescu F, Bohiltea RE, Voinea S,
Georgescu TA, Munteanu O, Neacsu A and Pop CS: Breast cancer
mortality gaps in Romanian women compared to the EU after 10 years
of accession: Is breast cancer screening a priority for action in
Romania? (Review of the Statistics). Exp Ther Med.
21(268)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Brom L, Pasman HR, Widdershoven GA, van
der Vorst MJ, Reijneveld JC, Postma TJ and Onwuteaka-Philipsen BD:
Patients' preferences for participation in treatment
decision-making at the end of life: Qualitative interviews with
advanced cancer patients. PLoS One. 9(e100435)2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Momenimovahed Z and Salehiniya H:
Epidemiological characteristics of and risk factors for breast
cancer in the world. Breast Cancer (Dove Med Press). 11:151–164.
2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rummel S, Hueman MT, Costantino N, Shriver
CD and Ellsworth RE: Tumor location within the breast: Does tumour
site have prognostic ability? Ecancermedicalscience.
9(552)2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Caplan L: Delay in breast cancer:
Implications for stage at diagnosis and survival. Front Public
Health. 2(87)2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ben Fatma L, Belaid I, Said N, Gahbiche S,
Hochlef M, Chabchoub I, Ezzairi F and Ben Ahmed S: What could be
the reasons of late diagnosis of breast cancer in Tunisia? Tunis
Med. 96:665–671. 2018.PubMed/NCBI
|
|
7
|
Hegde V, Burke ZDC, Park HY, Zoller SD,
Johansen D, Kelley BV, Levine B, Motamedi K, Federman NC, Seeger
LL, et al: Is core needle biopsy reliable in differentiating
between aggressive benign and malignant radiolucent bone tumors?
Clin Orthop Relat Res. 476:568–577. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang YJ, Wei L, Li J, Zheng YQ and Li XR:
Status quo and development trend of breast biopsy technology. Gland
Surg. 2:15–24. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bick U, Trimboli RM, Athanasiou A,
Balleyguier C, Baltzer PAT, Bernathova M, Borbély K, Brkljacic B,
Carbonaro LA, Clauser P, et al: Image-guided breast biopsy and
localisation: Recommendations for information to women and
referring physicians by the European society of breast imaging.
Insights Imaging. 11(12)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hanby AM: The pathology of breast cancer
and the role of the histopathology laboratory. Clin Oncol (R Coll
Radiol). 17:234–239. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Makki J: Diversity of breast carcinoma:
Histological subtypes and clinical relevance. Clin Med Insights
Pathol. 8:23–31. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Masood S: Neoadjuvant chemotherapy in
breast cancers. Womens Health (Lond). 12:480–491. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Feigenberg Z, Zer M and Dintsman M:
Comparison of postoperative complications following radical and
modified radical mastectomy. World J Surg. 2:207–211.
1977.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Morris CR, Cohen R, Schlag R and Wright
WE: Increasing trends in the use of breast-conserving surgery in
California. Am J Public Health. 90:281–284. 2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Nechuta S, Lu W, Zheng Y, Cai H, Bao PP,
Gu K, Zheng W and Shu XO: Comorbidities and breast cancer survival:
A report from the Shanghai breast cancer survival study. Breast
Cancer Res Treat. 139:227–235. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Rizvi FH, Khan MK, Almas T, Ullah M, Shafi
A, Murad MF, Ali A and Nadeem F: Early postoperative outcomes of
breast cancer surgery in a developing country. Cureus.
12(e9941)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hu C, Song H, Wang L, Jin L, Zhou X and
Sun L: Clinical efficacy of anesthesia with intensive care nursing
in attenuating postoperative complications in patients with breast
cancer. J Int Med Res. 48(300060520930856)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Vishwakarma M and Sahani IS: Comparative
study of complications of modified radical mastectomy and breast
conservation therapy in early invasive breast cancer. Int J Surg
Sci. 3:1–3. 2019.
|
|
19
|
Jagsi R, Abrahamse P, Morrow M, Hawley ST,
Griggs JJ, Graff JJ, Hamilton AS and Katz SJ: Patterns and
correlates of adjuvant radiotherapy receipt after lumpectomy and
after mastectomy for breast cancer. J Clin Oncol. 28:2396–2403.
2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wöckel A, Wolters R, Wiegel T,
Novopashenny I, Janni W, Kreienberg R, Wischnewsky M and Schwentner
L: BRENDA study group. The impact of adjuvant radiotherapy on the
survival of primary breast cancer patients: A retrospective
multicenter cohort study of 8935 subjects. Ann Oncol. 25:628–632.
2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Matuschek C, Bölke E, Haussmann J,
Mohrmann S, Nestle-Krämling C, Gerber PA, Corradini S, Orth K,
Kammers K and Budach W: The benefit of adjuvant radiotherapy after
breast conserving surgery in older patients with low risk breast
cancer-a meta-analysis of randomized trias. Radiat Oncol.
12(60)2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Han W, Kim SW, Park IA, Kang D, Kim SW,
Youn YK, Oh SK, Choe KJ and Noh DY: Young age: An independent risk
factor for disease-free survival in women with operable breast
cancer. BMC Cancer. 4(82)2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Rhiem K, Engel C, Graeser M, Zachariae S,
Kast K, Kiechle M, Ditsch N, Janni W, Mundhenke C, Golatta M, et
al: The risk of contralateral breast cancer in patients from
BRCA1/2 negative high risk families as compared to patients from
BRCA1 or BRCA2 positive families: A retrospective cohort study.
Breast Cancer Res. 14(R156)2012.PubMed/NCBI View
Article : Google Scholar
|
|
24
|
Untch M, Konecny GE, Paepke S and von
Minckwitz G: Current and future role of neoadjuvant therapy for
breast cancer. Breast. 23:526–537. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Apesteguía L and Pina LJ:
Ultrasound-guided core-needle biopsy of breast lesions. Insights
Imaging. 2:493–500. 2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Perry N, Broeders M, de Wolf C, Törnberg
S, Holland R and von Karsa L (eds): European guidelines for quality
assurance in breast cancer screening and diagnosis. 4th edition.
European Commission, Office for official publications of the
European communities, Luxembourg, 2006. https://screening.iarc.fr/doc/ND7306954ENC_002.pdf.
Accessed July 1, 2020.
|
|
27
|
Pantelimon I, Gales LN, Zgura A,
Serbanescu GL, Georgescu DE, Nita I, Manolescu LSC, Stancu AM,
Gruia MI, Anghel RM and Badiu DC: Analysis of oxidative stress in
patients with breast cancer and obesity. Ann Med Health Sci Res.
11:1578–1585. 2021.
|
|
28
|
Ardeleanu V, Georgescu C, Frincu LD,
Frincu LL and Vesa C: Angiogenesis as prospective molecular biology
technique for cancer study. Rom Biotech Lett. 19:9637–9648.
2014.
|
|
29
|
Williams SL, Birdsong GG, Cohen C and
Siddiqui MT: Immunohistochemical detection of estrogen and
progesterone receptor and HER2 expression in breast carcinomas:
Comparison of cell block and tissue block preparations. Int J Clin
Exp Pathol. 2:476–480. 2009.PubMed/NCBI
|
|
30
|
Sleightholm R, Neilsen BK, Elkhatib S,
Flores L, Dukkipati S, Zhao R, Choudhury S, Gardner B, Carmichael
J, Smith L, et al: Percentage of hormone receptor positivity in
breast cancer provides prognostic value: A single-institute study.
J Clin Med Res. 13:9–19. 2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Bacinschi XE, Zgura A, Safta I and Anghel
R: Biomolecular factors represented by Bcl-2, p53, and
tumor-infiltrating lymphocytes predict response for adjuvant
anthracycline chemotherapy in patients with early triple-negative
breast cancer. Cancer Manag Res. 12:11965–11971. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
El Sayed R, El Jamal L, El Iskandarani S,
Kort J, Abdel Salam M and Assi H: Endocrine and targeted therapy
for hormone-receptor-positive, HER2-negative advanced breast
cancer: Insights to sequencing treatment and overcoming resistance
based on clinical trials. Front Oncol. 9(510)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Mehrgou A and Akouchekian M: The
importance of BRCA1 and BRCA2 genes mutations in breast cancer
development. Med J Islam Repub Iran. 30(369)2016.PubMed/NCBI
|
|
34
|
Mehedintu C, Bratila E, Berceanu C,
Cirstoiu MM, Barac RI, Andreescu CV, Badiu DC, Gales L, Zgura A and
Bumbu AG: Comparison of tumor-infiltrating lymphocytes between
primary and metastatic tumors in Her2+ and HER2-breast cancer
patients. Rev Chim. 69:3133–3137. 2018.
|
|
35
|
Yalagachin G, Lakshmikantha N and Mashal
SB: Prevalence of nodular goiter in patients with breast diseases.
J Clin Invest Surg. 5:91–95. 2020.
|
|
36
|
Mehrabani D and Manafi A: Breast implants
and breast cancer. World J Plast Surg. 1:62–63. 2012.PubMed/NCBI
|
|
37
|
Rostas JW and Dyess DL: Current operative
management of breast cancer: An age of smaller resections and
bigger cures. Int J Breast Cancer. 2012(516417)2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Franceschini G, Di Leone A, Natale M,
Sanchez MA and Masett R: Conservative surgery after neoadjuvant
chemotherapy in patients with operable breast cancer. Ann Ital
Chir. 89(290)2018.PubMed/NCBI
|
|
39
|
van Oers H and Schlebusch L: Indicators of
psychological distress and body image disorders in female patients
with breast cancer. J Mind Med Sci. 7:179–187. 2020.
|
|
40
|
White J, Achuthan R, Turton P and Lansdown
M: Breast conservation surgery: State of the art. Int J Breast
Cancer. 2011(107981)2011.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Ursaru M, Jari I, Negru D and Scripcariu
V: Local and distant recurrences-a comparative study on
conservative and radical surgery for breast cancer. Chirurgia
(Bucur). 110:38–42. 2015.PubMed/NCBI
|
|
42
|
Veronesi U, Cascinelli N, Mariani L, Greco
M, Saccozzi R, Luini A, Aguilar M and Marubini E: Twenty-year
follow-up of a randomized study comparing breast-conserving surgery
with radical mastectomy for early breast cancer. N Engl J Med.
347:1227–1232. 2002.PubMed/NCBI View Article : Google Scholar
|