Introduction
Improvements in the field of surgical oncology along
with advancements reported to date in medical oncology and
radiotherapy have led to an increase in the rates of resectability
of pancreatic head tumors and therefore, to an increase in the
proportion of patients reporting a significant benefit in terms of
survival (1,2). However, the close anatomic
relationship between the pancreatic head and the surrounding
vascular structures is still responsible for the presence of local
invasion in a significant number of cases (3). In this respect, attention was focused
on determining whether the presence of such a vascular encasement
should be considered as a formal contraindication for resection or
if, in certain cases, vascular resection makes sense in order to
improve the long-term outcomes (4).
Promising results have been reported to date in regards to portal
vein resection followed by reconstruction; in such cases, similar
rates of long-term survival have been reported when compared to
standard pancreatic resections (5).
Therefore, portal vein resection is no longer a formal
contraindication for resection and attention was focused on
identifying the best graft for portal reconstruction.
Case report
After obtaining the approval of the Ethics Committee
of ‘Fundeni’ Clinical Institute (no. 752/2020), data of the patient
were retrospectively reviewed.
The 49-year-old patient with no significant medical
history was investigated for diffuse abdominal pain, weight loss of
7 kg in the last three months and jaundice. The biochemical tests
revealed the presence of cholestasis, with serum levels of total
bilirubin of 9.2 mg/dl and direct bilirubin of 7.5 mg/dl,
cytolysis, with aspartate aminotransferase (AST) of 344 U/l and
alanine aminotransferase of 599 U/l. Meanwhile the serum levels of
cancer antigen (CA19-9) were significantly increased (CA19-9, 425
U/ml). The patient was submitted to magnetic resonance imaging
(MRI) which demonstrated the presence of a 4/5/3 cm pancreatic head
mass with no demarcation line with the portal vein on a distance of
2.2 cm. No sign of invasion of the hepatic pedicle or of the
superior mesenteric vessels were observed. The patient was further
submitted to an endoscopic ultrasound in order to retrieve a biopsy
which demonstrated the presence of a moderately differentiated
pancreatic adenocarcinoma. Due to the presence of a good general
status and due to the absence of other signs of unresectability,
the patient was submitted to per primam resection, a
pancreatoduodenectomy en bloc with portal vein resection being
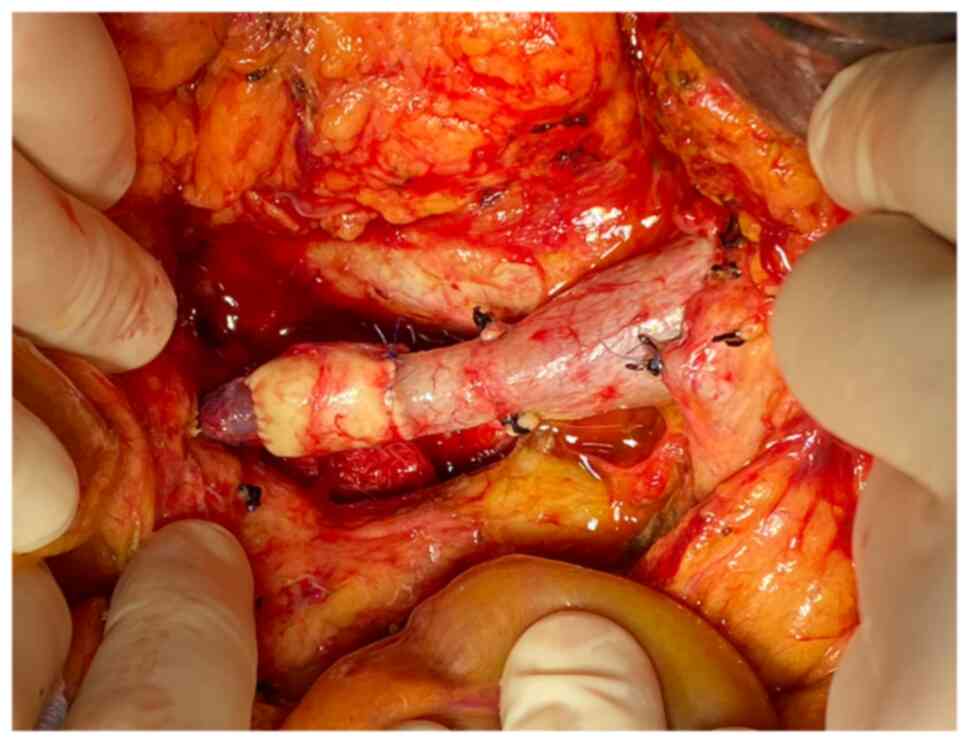
performed. The length of the resected portal vein was of 3.5 cm so
an end to end anastomosis was not feasible. Due to this reason the
decision for using a cadaveric graft was taken, the continuity of
the portal vein being re-established by placing a cadaveric
cryopreserved abdominal aorta graft measuring 3.5 cm. The
anastomosis between the portal vein and the cadaveric aortic graft
were performed by using a running suture of polypropylene 5-0
(Fig. 1). The duration of the
surgery was 230 min while the estimated blood loss was of 200 ml;
no intraoperative complications were encountered. During the
perioperative period, the patient was submitted to low-molecular
heparin injection, the patency of the graft being demonstrated by
Doppler ultrasound which was performed on the second and seventh
postoperative days. The patient was discharged on the eight
postoperative day and received recommendation to continue the
administration of low-molecular heparin for the next 30 days. The
histopathological studies demonstrated the presence of a moderately
differentiated pancreatic adenocarcinoma invading the portal vein
on a total length of 2.8 cm; meanwhile, all the resection margins
of the specimen were free of disease. At the one month follow-up,
the patient reported a good general condition and was deferred to
the oncology department in order to be submitted to adjuvant
chemotherapy.
Discussion
Initially performed in the late 1950's, pancreatic
head resection en bloc with venous resection and reconstruction
were considered at that moment as unjustified due to the high rates
of perioperative complications. Therefore, venous invasion has been
considered for a long period of time as a formal contraindication
for surgery; however recent meta-analyses came to demonstrate that
the method can be safely applied without a significant increase in
perioperative morbidity and meanwhile, with significant benefits in
terms of survival (5-8).
These similar rates of long-term survival which have been reported
after standard pancreatoduodenectomy when compared to
pancreatoduodenectomy en bloc with venous resection have been
explained by the fact that local venous invasion is rather the sign
of a locally advanced disease and not of a biologically aggressive
lesion (9). Meanwhile, improvements
in the surgical techniques concerning vascular reconstruction, of
the perioperative and postoperative management have led to the
successful incorporation of such resections as part of pancreatic
surgery (10-16).
According to the extent of local invasion of the
portal vein, different types of procedures have been proposed to
date; therefore, resection of the portal vein might be a lateral
one or a circumferential one (17-19).
Cases in which the estimated degree of narrowing after lateral
resection is larger than 30% of the portal lumen are rather
submitted to a circumferential resection than to a lateral one
followed by lateral venorrhaphy (18); meanwhile, in cases in which a
circumferential resection is needed, the type of reconstruction is
to be established depending on the length of the resected segment
as well as of the diameter of the two venous stumps (16,17).
In cases in which the extent of portal vein resection is limited
and the two stumps have similar diameters, an end to end
anastomosis might be the option of choice; generally it is
estimated that defects shorter than 2 cm are suitable for an end to
end anastomosis (18). Meanwhile
cases in which the resulting defect does not allow an end to end
anastomosis, a graft may be needed in order to re-establish the
venous continuity. In order to minimize the risks of perioperative
complications, multiple types of reconstructions have been proposed
including: autologous vein, cadaveric arterial or venous grafts,
bovine pericardial or synthetic grafts such as Gore-Tex,
polytetrafluoroethylene or Dacron prostheses (18). Whenever a venous graft of a
synthetic prosthesis is used, there is a significant risk of graft
thrombosis which might reach 17% of cases, depending on the extent
of resection, timing and graft harvesting and type of
reconstruction (19-22).
When it comes to the utility of arterial cadaveric
grafts for vascular reconstructions, the method has been initially
implemented in vascular surgery in order to provide different types
of arterial reconstructions. Cryopreserved aortic graft was
successfully implemented for aortic reconstruction and have proven
to have significant benefits; therefore, according to
Harlander-Locke et al, this method is associated with
decreased risks of graft infection, aneurysm formation and limb
loss. The authors conducted a multicenter retrospective study which
involved 220 patients and demonstrated that at a 5-year follow up
97% of cases reported a patent aortic graft (19). Once the method proved its efficacy
in vascular surgery, it was also successfully implemented in
visceral surgery. Therefore, it avoids the risks associated with
the use of synthetic allografts such as Dacron or Gore-Tex by
diminishing the infectious risks. In a study conducted by Mascoli
et al, aortic graft reconstruction of the portal vein was
successfully reported in three cases; two patients benefited from a
thoracic aorta graft while the third one benefited from an
abdominal aorta graft, the median length of the graft being 6 cm.
Meanwhile the authors reported the superiority of the method when
compared to venous graft reconstruction due to the fact that
arterial grafts have a lower risk of developing postoperative
complications such as thrombosis, stenosis or infection (22). Therefore, it seems that arterial
grafts are more resistant to surgical manipulation, do not have
valves, are more effective in reducing the occlusion risk due to
external visceral compression and are associated with a lower risk
of graft infection (23,24).
In conclusion, cryopreserved cadaveric arterial
grafts appear to be safely used in portal vein reconstruction after
pancreatoduodenectomy en bloc with portal vein resection for
locally advanced pancreatic cancer. Therefore, arterial grafts seem
to have certain advantages when compared to venous grafts or
synthetic prosthesis such as a lower risk of postoperative graft
infection, thrombosis or stenosis. However, findings concerning
this method have been scarcely reported so far, or only for a small
number of cases. Thus, larger studies are necessary in order to
standardize it and to analyze which cases could benefit most after
this type of reconstruction.
Acknowledgements
Not applicable.
Funding
Funding: This research received no external funding.
Availability of data and materials
Data are available at request from the corresponding
author.
Authors' contributions
NB, IB and OS contributed to the conception and
design of the present study. CD, BS, FG, IB, VB consulted the
relevant references and performed the literature data collection.
IB and NB wrote the first draft of the manuscript. VB revised the
manuscript. All authors read and approved the final manuscript for
publication.
Ethics approval and consent to
participate
The Ethics Committee of ‘Fundeni’ Clinical Institute
approved the study (no. 752/2020).
Patient consent for publication
Patient consent for publication was obtained and
signed by the patient on 21/04/2021.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Smeenk HG, van Eijck CH, Hop WC, Erdmann
J, Tran KC, Debois M, van Cutsem E, van Dekken H, Klinkenbijl JH
and Jeekel J: Long-term survival and metastatic pattern of
pancreatic and periampullary cancer after adjuvant chemoradiation
or observation: Long-term results of EORTC trial 40891. Ann Surg.
246:734–740. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Varadhachary GR, Tamm EP, Abbruzzese JL,
Xiong HQ, Crane CH, Wang H, Lee JE, Pisters PWT, Evans DB and Wolff
RA: Borderline resectable pancreatic cancer: Definitions,
management, and role of preoperative therapy. Ann Surg Oncol.
13:1035–1046. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Peparini N and Chirletti P: Mesopancreas:
A boundless structure, namely R1 risk in pancreaticoduodenectomy
for pancreatic head carcinoma. Eur J Surg Oncol. 39:1303–1308.
2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Beger HG, Rau B, Gansauge F, Poch B and
Link KH: Treatment of pancreatic cancer: Challenge of the facts.
World J Surg. 27:1075–1084. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Weitz J, Kienle P, Schmidt J, Friess H and
Büchler MW: Portal vein resection for advanced pancreatic head
cancer. J Am Coll Surg. 204:712–716. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tseng JF, Raut CP, Lee JE, Pisters PW,
Vauthey JN, Abdalla EK, Gomez HF, Sun CC, Crane CH, Wolff RA and
Evans DB: Pancreaticoduodenectomy with vascular resection: Margin
status and survival duration. J Gastrointest Surg. 8:935–950.
2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Siriwardana HP and Siriwardena AK:
Systematic review of outcome of synchronous portal-superior
mesenteric vein resection during pancreatectomy for cancer. Br J
Surg. 93:662–673. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Hartel M, Niedergethmann M, Farag-Soliman
M, Sturm JW, Richter A, Trede M and Post S: Benefit of venous
resection for ductal adenocarcinoma of the pancreatic head. Eur J
Surg. 168:707–712. 2002.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Leach SD, Lee JE, Charnsangavej C, Cleary
KR, Lowy AM, Fenoglio CJ, Pisters PW and Evans DB: Survival
following pancreaticoduodenectomy with resection of the superior
mesenteric-portal vein confluence for adenocarcinoma of the
pancreatic head. Br J Surg. 85:611–617. 1998.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bacalbasa N, Brezean I, Anghel C, Barbu I,
Pautov M, Balescu I and Brasoveanu V: Successful resection and
vascular ligation of a large hepatic artery aneurysm-a case report
and literature review. In Vivo. 31:979–982. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bacalbasa N, Brezean I, Anghel C, Barbu I,
Pautov M, Balescu I and Brasoveanu V: Management of a fulminant
upper gastrointestinal bleeding exteriorized through hemobilia due
to arteriobiliary fistula between the common bile duct and a right
hepatic artery aneurysm-a case report. In Vivo. 31:983–989.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Braşoveanu V, Dumitraşcu T, Bacalbaşa N
and Zamfir R: Splenic artery used for replaced common hepatic
artery reconstruction during pancreatoduodenectomy-a case report.
Chirurgia (Bucur). 104:499–504. 2009.PubMed/NCBI
|
|
13
|
Brasoveanu V, Anghel C, Barbu I, Pautov M,
Ionescu MI, Motthor M, Balescu I, Dima S and Bacalbasa N:
Pancreatoduodenectomy en bloc with portal and superior mesenteric
artery resection-a case report and literature review. Anticancer
Res. 35:1613–1618. 2015.PubMed/NCBI
|
|
14
|
Bacalbasa N, Balescu I, Tanase A, Pautov
M, Brezean I, Vilcu M and Brasoveanu V: Spleno-pancreatectomy en
bloc with parcelar gastrectomy for splenic artery aneurysm-a case
report and literature review. In Vivo. 32:915–919. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bacalbasa N, Balescu I, Tanase A, Brezean
I, Vilcu M and Brasoveanu V: Successful resection of a
non-functional paraganglioma with celiac trunk invasion followed by
common hepatic artery reimplantation-a case report and literature
review. In Vivo. 32:911–914. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ishikawa O, Ohigashi H, Imaoka S, Furukawa
H, Sasaki Y, Fujita M, Kuroda C and Iwanaga T: Preoperative
indications for extended pancreatectomy for locally advanced
pancreas cancer involving the portal vein. Ann Surg. 215:231–236.
1992.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kleive D, Berstad AE, Verbeke CS, Haugvik
SP, Gladhaug IP, Line PD and Labori KJ: Cold-stored cadaveric
venous allograft for superior mesenteric/portal vein reconstruction
during pancreatic surgery. HPB (Oxford). 18:615–622.
2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Glebova NO, Hicks CW, Piazza KM,
Abularrage CJ, Cameron AM, Schulick RD, Wolfgang CL and Black JH
III: Technical risk factors for portal vein reconstruction
thrombosis in pancreatic resection. J Vasc Surg. 62:424–433.
2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Harlander-Locke MP, Harmon LK, Lawrence
PF, Oderich GS, McCready RA, Morasch MD and Feezor RJ: Vascular
Low-Frequency Disease Consortium. Zhou W, Bismuth J, et al: The use
of cryopreserved aortoiliac allograft for aortic reconstruction in
the United States. J Vasc Surg. 59:669–674. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Smoot RL, Christein JD and Farnell MB: An
innovative option for venous reconstruction after
pancreaticoduodenectomy: The left renal vein. J Gastrointest Surg.
11:425–431. 2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Fleming JB, Barnett CC and Clagett GP:
Superficial femoral vein as a conduit for portal vein
reconstruction during pancreaticoduodenectomy. Arch Surg.
140:698–701. 2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Mascoli C, D'Ambra M, Casadei R, Ricci C,
Taffurelli G, Ancetti S, Stella A, Minni F and Freyrie A:
Portal/superior mesenteric vein reconstruction during pancreatic
resection using a cryopreserved arterial homograft. Dig Surg.
32:284–290. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ravikumar R, Sabin C, Abu Hilal M,
Bramhall S, White S, Wigmore S, Imber CJ and Fusai G: UK Vascular
Resection in Pancreatic Cancer Study Group. Portal vein resection
in borderline resectable pancreatic cancer: A United Kingdom
multicenter study. J Am Coll Surg. 218:401–411. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Dodd PD: What tissue bankers should know
about the use of allograft blood vessels. Cell Tissue Bank.
11:3–11. 2010.PubMed/NCBI View Article : Google Scholar
|