Introduction
Neurosyphilis (NS) is a neurological disorder of the
central nervous system caused by Treponema pallidum (T. pallidum)
infection, which may occur at any stage of syphilis. NS is named
‘the great imitator’ due to various clinical manifestations such as
headache, progressive cognitive decline and stroke; however,
patients may also be asymptomatic (1). Due to these varied symptoms, NS may be
easily misdiagnosed or ignored. Clinical abnormalities are more
likely to resolve in early NS than in late NS; therefore, early
recognition of NS is an important issue. Currently, the diagnosis
of NS relies on clinical and laboratory results. The cerebrospinal
fluid venereal disease research laboratory (CSF-VDRL) tests, the
CSF rapid plasma reagin (RPR) or CSF-serum toluidine red unheated
serum test (TRUST) are not reactive in all cases of NS (2,3).
Lumbar puncture (LP) for CSF examinations is currently the
imperfect gold standard for NS. However, differing opinions of
clinicians, poor patient acceptance and invasiveness are
limitations for using LP as a disease course monitoring tool. Thus,
simple and noninvasive indices based on routine laboratory tests to
monitor the disease course are of great importance.
The neutrophil to lymphocyte ratio (NLR) is a stable
complete blood count parameter that is used as a marker of
inflammation for diseases such as stroke, systemic lupus
erythematosus, pulmonary tuberculosis, psoriasis arthritis and
dermatomyositis (4-8).
A positive association of the NLR with disease activity has
emerged; the NLR is positively associated with lupus nephritis,
psoriatic arthritis and pulmonary involvement in patients with
dermatomyositis (4,6,7).
Furthermore, associations of the NLR with other conditions, such as
Hashimoto's disease, diabetes mellitus, thyroid nodules, cardiac
conditions, numerous cancer types and vitamin D deficiency has been
reported (9-16);
however, the association between the NLR and NS has remained to be
determined.
All individuals with syphilis and HIV co-infection
are recommended to undergo LP (17); however, whether and when to perform
LP in patients with HIV-negative NS is controversial. A recent
study reported that a serum T. pallidum agglutination assay (TPPA)
titer ≥1:2,560, a serum RPR titer ≥1:4 and increased levels of
serum creatine kinase are able to predict symptomatic NS (18). However, indicators for symptomatic
NS and asymptomatic NS prior to LP in HIV-negative patients have
remained to be determined. In the present study, it was assessed
whether NLRs and serum TRUST titers are different between NS and
Non-NS patients. Furthermore, the performance of the two markers
for predicting NS was also determined.
Subjects and methods
Subjects
NS and Non-NS patients, as well as age- and
gender-matched healthy controls, who attended Yijishan Hospital of
Wannan Medical College (Wuhu, China) between January 2015 and
August 2018, were retrospectively reviewed. The NS patients met all
of the following requirements: i) Serum TPPA and TRUST titer were
positive; ii) serological tests were combined with CSF-TRUST
positivity; or CSF white blood cell (WBC) count >5 cells/µl or
CSF-protein >45 mg/dl and CSF-TPPA reactivity (10). Non-NS was defined as a seropositive
for TPPA and TRUST but a negative for the CSF-TRUST and CSF-TPPA
with all of the following: i) CSF WBC ≤5 cells/µl and CSF protein
≤45 mg/dl; ii) absence of any characteristic symptoms or signs of
NS. Healthy controls who underwent normal health check-ups that
revealed no diseases with a normal erythrocyte sedimentation rate
(ESR) and C-reactive protein (CRP) levels were recruited from the
database of Yijishan Hospital of Wannan Medical College between
January 2015 and August 2018 (Wuhu, China).
The following exclusion criteria were applied:
Pregnancy, incomplete documentation, the existence of other chronic
inflammatory disorders (e.g., autoimmunity) and other infectious
diseases (e.g., tuberculosis, urinary tract infection and
pneumonia), and treatment with anti-inflammatory or
immunosuppressive drugs or antibiotics within the last 6 months.
All patients were positive for serum TRUST and TPPA and negative
for HIV.
Data
Demographic, clinical and laboratory data were
retrieved from the hospital's information system. The following
data were included: Age, sex, complete blood count, serum TRUST,
CSF-WBC count, CSF protein level, CSF-TPPA, CSF-TRUST and
serological testing (TRUST, TPPA). The above-mentioned data of 24
NS patients were collected after treatment at a 6-month follow-up.
The NLR was calculated as the neutrophil count divided by the
lymphocyte count.
Statistical analysis
The TRUST titers were transferred to log2
transformations (log2 1/TRUST titer) for analysis.
Quantitative variables are presented as the mean ± standard
deviation or median (interquartile range) as appropriate.
Qualitative variables are expressed as the number and percentage.
Univariate analyses were performed by Student's t-test or the
Mann-Whitney U-test for quantitative variables as appropriate.
Qualitative variables were compared by the χ² test or Fisher's
exact test as appropriate. Independent predictors for NS were
analyzed using standard binomial logistic regression analysis. The
Spearman test was performed to estimate the correlation between
variables. Receiver operating characteristic (ROC) curves were used
to identify cutoff values of the NLR and the serum TRUST titer for
discriminating between NS and Non-NS. To evaluate the changes in
parameters between the baseline and the designated follow-up
time-point, a two-tailed Wilcoxon rank-sum test was employed.
Statistical analysis was performed using SPSS Statistics 22.0 (IBM
Corp). P-values were two-sided and P<0.05 was considered to
indicate statistical significance.
Results
Comparison of variables between NS
patients or Non-NS patients and healthy controls
The demographic data and laboratory findings of 87
NS patients, 80 Non-NS patients and 1:1 age- and gender-matched
healthy individuals are presented in Table SI. The mean age of NS group was
51.03±13.09 years (range, 21-81), and the group included 54 males
and 33 females. The mean age of Non-NS patients was 35.20±11.26
years (range, 20-76), and these patients included 18 males and 62
females. The mean age in the healthy control patient group that was
compared with the NS group was 49.53±11.18 years (range, 21-68),
the sex distribution was 48 men and 39 women. The mean age of the
healthy control patients that were compared to the Non-NS group was
34.65±10.30 years (range, 20-67), the sex distribution was 19 men
and 61 women. Peri-WBC, neutrophil, ESR and the NLR were
significantly higher in the NS group compared with the healthy
controls (P<0.001; except for the peri-WBC count, P=0.01).
Lymphocyte counts were lower in the NS group than in the healthy
controls (P<0.001). The peri-WBC and neutrophil counts were
higher in the Non-NS group than that in healthy controls
(P<0.001). However, the lymphocyte counts were not significantly
different between the Non-NS group and healthy controls (P=0.741).
The NLR was higher in the Non-NS groups than that in the healthy
group (P=0.01). No significant difference in CRP was observed
between the NS or the Non-NS and healthy controls (P>0.05).
Comparison of laboratory parameters
between NS and Non-NS patients
In comparison to the Non-NS group, in NS patients
male sex was predominant, the mean age was older and ESR was higher
in the NS group (P<0.001), while no significant difference was
observed for CRP (P>0.05). The median serum TRUST titer was
significantly higher in the NS group compared with that in the
Non-NS group [1:16 (1:8-1:32) vs. 1:2 (1:2-1:4), P<0.001)].
Lymphocyte counts in NS patients were significantly decreased
compared with those in Non-NS patients (1.58±0.71 vs. 1.98±0.72,
P<0.001). Furthermore, the NLR in the NS group was significantly
higher compared with that in the Non-NS group (P=0.004; Table I).
 | Table IComparison of patients with NS and
non-NS. |
Table I
Comparison of patients with NS and
non-NS.
| Parameter | NS (n=87) | Non-NS (n=80) | P-value |
|---|
| Age (years) | 51.03±13.09 | 35.20±11.26 | <0.001 |
| Male sex | 54 (62.1) | 18 (22.5) | <0.001 |
| Serum-TRUST | 1:16 (1:8-1:32) | 1:2 (1:2-1:4) | <0.001 |
| CSF-WBC | 12.89±14.95 | 5.26±1.75 | <0.001 |
| CSF-protein
(mg/dl) | 62.99±43.32 | 30.45±11.18 | <0.001 |
| CSF-TRUST | 1:1
(negative-1:4) | Negative | <0.001 |
| Peri-WBC
(x109/l) | 6.93±2.62 | 6.83±1.77 | 0.61 |
| Neutrophil | 4.59±2.61 | 4.27±1.53 | 0.72 |
| Lymphocyte | 1.58±0.71 | 1.98±0.72 | <0.001 |
| NLR | 2.87 (2.04-3.89) | 1.89 (1.50-3.37) | 0.004 |
| ESRa | 16.28±16.98 | 6.07±4.24 | <0.001 |
| CRPb | 3.95±4.36 | 3.38±1.34 | 0.57 |
Predictive value of the NLR and serum
TRUST titer
Binomial logistic regression analysis indicated a
significant association of age, NLR and serum TRUST titer with NS
[odds ratio (OR)=1.099, 95% CI=1.052-1.149, P<0.001; OR=1.363,
95% CI=1.035-1.795, P=0.028; and OR=3.065, 95% CI=2.094-4.487,
P<0.001, respectively; Table
II]. The ESR was not included in a further logistic regression
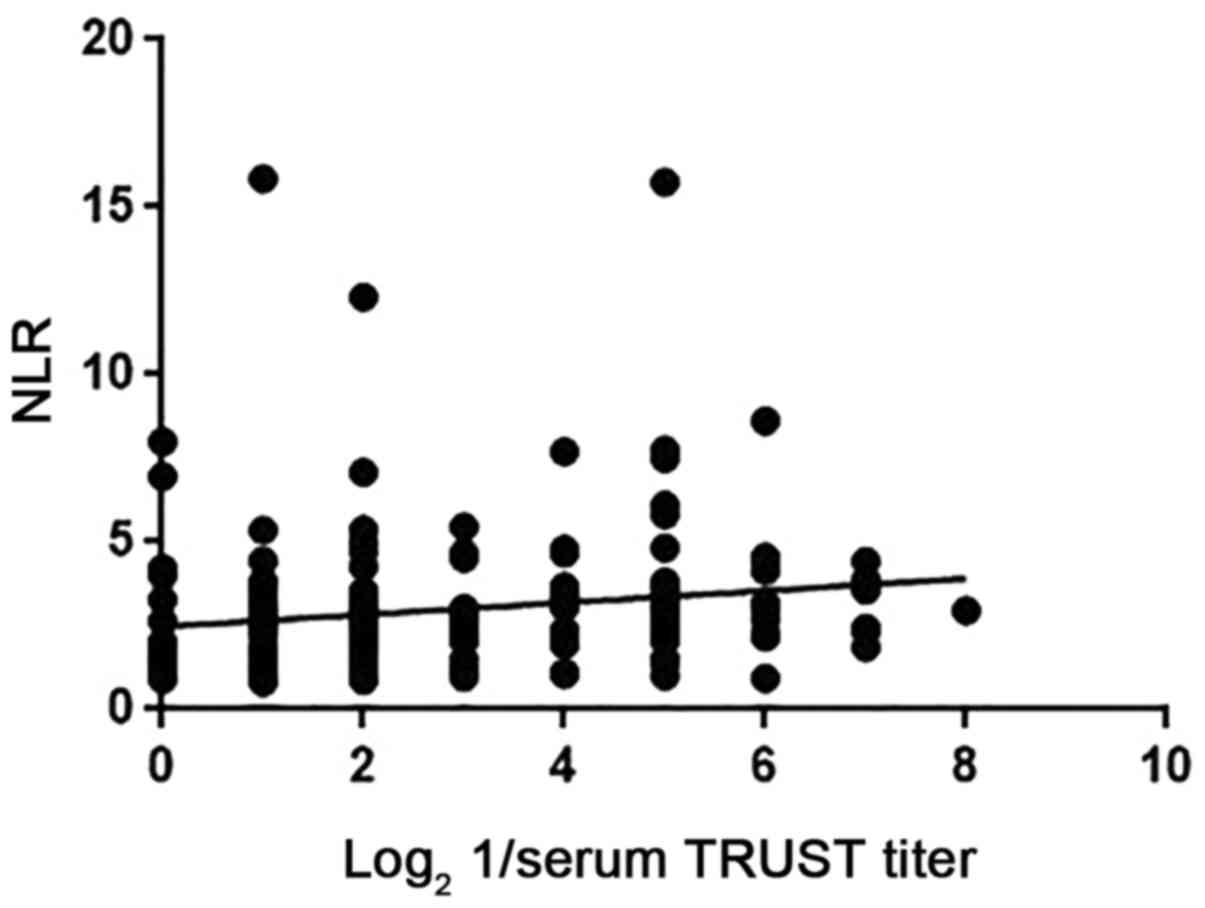
analysis due to incomplete data. Spearman's rank correlation
analysis indicated that the NLR in patients with NS was positively
correlated with the serum TRUST titer (r=0.288, P<0.001;
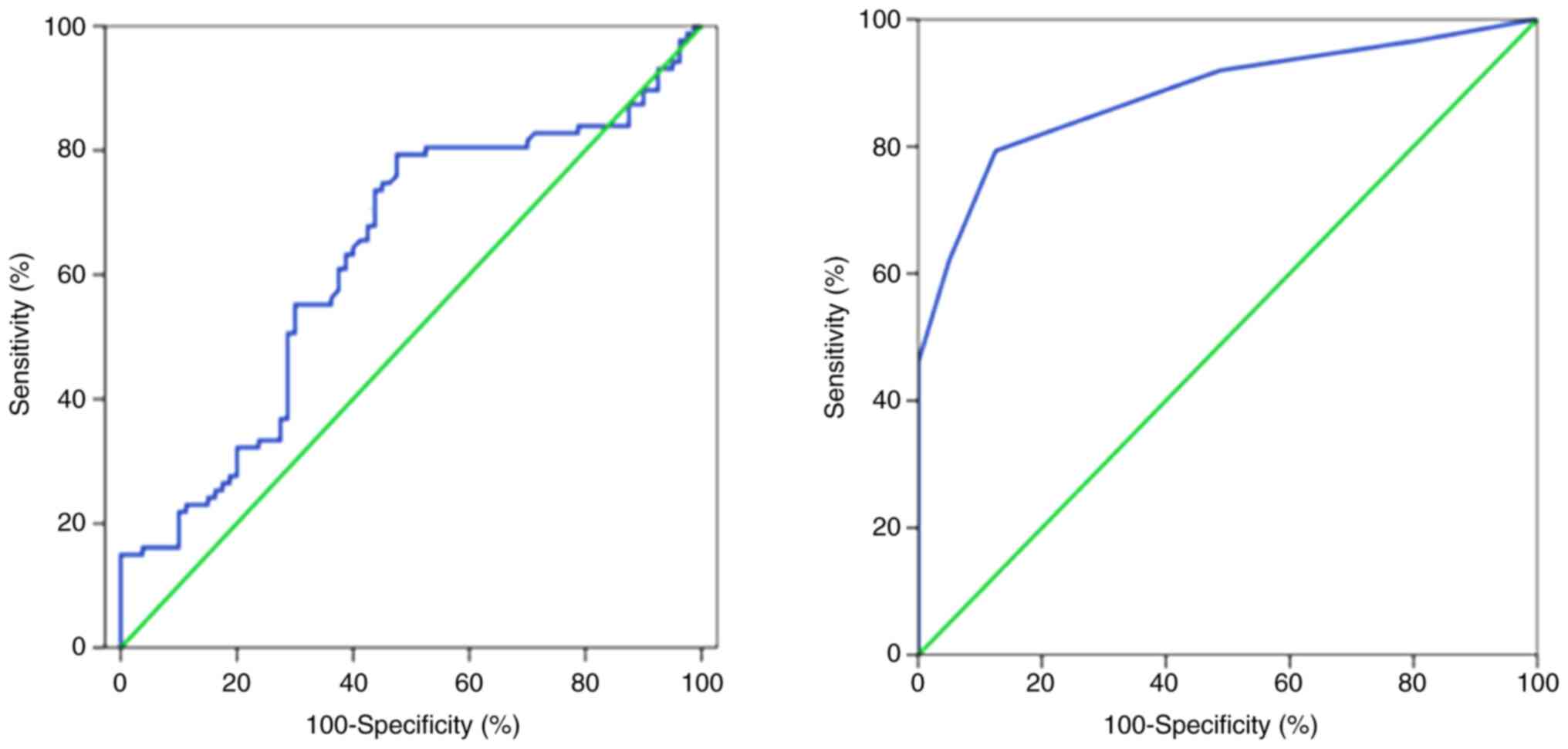
Fig. 1). ROC curve analyses
indicated that the area under the curve values of the NLR and serum
TRUST titer were 0.628 (95% CI=0.542-0.714; P=0.01) and 0.882 (95%
CI=0.798-0.911; P<0.001), respectively (Fig. 2); the optimal cut-off values of the
NLR and serum TRUST titer to predict NS were 1.97 (79.3%
sensitivity, 52.5% specificity) and 1:8 (79.3% sensitivity, 87.5%
specificity), respectively. For the NS group, 67.8% of patients had
a high NLR and serum TRUST titer and 9.2% had a low level, while
23.0% of patients had discordant levels. The serum TRUST test with
the NLR test was also combined in a parallel and serial testing
format. In the parallel testing format (with either serum TRUST
titer ≥1:8 or NLR ≥1.97, or both), 90.8% sensitivity and 50.0%
specificity were obtained for predicting NS. In the serial testing
format (with serum TRUST titer ≥1:8 and NLR ≥1.97), 67.8%
sensitivity and 90.0% specificity were obtained for predicting NS.
In addition, the NLR, serum TRUST titer, CSF-WBC count, CSF-protein
level and CSF-TRUST titer parameters were significantly decreased
at the 6-month follow-up after treatment with penicillin
(P<0.05; Table SII).
 | Table IIBinomial logistic regression model
for the presence of neurosyphilis. |
Table II
Binomial logistic regression model
for the presence of neurosyphilis.
| Variable | OR | 95% CI | P-value |
|---|
| Age | 1.099 | 1.052-1.149 | <0.001 |
| NLR | 1.363 | 1.035-1.795 | 0.028 |
| Serum TRUST
titer | 3.065 | 2.094-4.487 | <0.001 |
| Lymphocyte | 2.024 | 0.869-4.715 | 0.102 |
Discussion
The present study indicated that age, the NLR and
serum TRUST titer were independent risk factors of NS, i.e.,
elevated NLR and serum TRUST titer were able to predict the
presence of NS. Furthermore, the NLR was positively associated with
the serum TRUST titer and was reduced when the clinical
manifestations were resolved and the serum TRUST titer and CSF
parameters were reduced. The cut-off values for the serum TRUST
titer and the NLR were 1:8 and 1.97, respectively. Combination of
the NLR and serum TRUST titer had a substantially higher
sensitivity (90.8%) for identifying NS than the NLR or serum TRUST
titer alone.
The NLR, as a marker of chronic systemic
inflammation, is a prognostic indicator for numerous cancer types,
acute stroke, multiple sclerosis and Parkinson's disease (5,9,12,19,20),
while the NLR is used for the diagnosis of numerous inflammatory
diseases, including subacute thyroiditis, psoriatic arthritis and
lupus nephritis (4,7,21).
Inflammation has a significant role in the pathogenesis of NS.
Certain inflammatory factors, including B lymphocyte
chemoattractant chemokine (C-X-C motif) ligand 13 and the
macrophage migration inhibitory factor, interleukin 10, increased
markedly in both the serum and CSF of patients with NS (22-24).
In vivo, T. pallidum stimulated the expression of
inflammatory cytokines in THP-1 cells and induced the
transformation of macrophages to a pro-inflammatory M1 macrophage
type (25); furthermore, the T.
pallidum proteins, including Tp92, Tp0751 and T. pallidum
flagellins, may also enhance the release of inflammatory cytokines
in HMEC-1/THP-1 cells (26-28).
In light of these results, inflammation in the course of NS was
confirmed. The ESR in patients with NS was higher than that in
patients with Non-NS and it was speculated that differences in the
gender distribution and age between NS and Non-NS groups may cause
ESR-related differences, as the ESR itself is easily affected by
gender and age; however, patients with NS had low and normal levels
of CRP, which confirmed that NS is a low-grade inflammatory
disease. This, in turn, may account for low lymphocyte counts
observed in patients with NS. Furthermore, decreased lymphocyte
counts in patients with NS compared with Non-NS patients may cause
the NLR to be elevated in patients with NS in the present study,
and it was speculated that lymphocyte or lymphocytes-associated
signaling pathways may be important for controlling inflammation
involved in NS, as T lymphocytes, particularly CD3+CD8+
lymphocytes, natural killer cells and B lymphocytes, are involved
in NS (29,30). However, further studies are required
to explore the associated molecular mechanisms. In addition, the
NLR was determined to be an indicator of disease activity in
autoimmune diseases, such as primary Sjögren's syndrome, systemic
lupus erythematosus and rheumatoid arthritis (4,31,32).
In the present study, binary logistic analysis determined that the
NLR was positively associated with the presence of NS; the best NLR
cut-off value was 1.97 with 79.3% sensitivity and 52.5% specificity
and the AUC value was 0.628. Of note, the NLR was positively
associated with the serum TRUST titer, which was determined to be a
risk factor of NS, and was decreased at the 6-month follow-up after
treatment with penicillin when clinical symptoms and laboratory
parameters (serum TRUST titer, CSF-WBC count and CSF-protein level)
were resolved. Thus, it was confirmed that the NLR may be an
additional marker for diagnosing NS and assessing disease
activity.
Risk factors for NS include an age of ≥45 years,
high serum RPR titer and HIV (33,34).
HIV-positive subjects with RPR titers ≥1:32 or a CD4+ cell count
≥350 cells/µl are recommended to undergo LP for CSF examination
(35). Conventionally, patients
exhibiting signs of at least one of the following, namely
neurological, ocular or auricular symptoms, serological failure or
serological fast, are recommended to undergo LP to exclude NS
(2). In addition, the TRUST test
has become commercially and widely available in China. Jiang et
al (36) indicated that among
HIV-negative patients, those with serum-TRUST titers ≥1:16 have a
higher probability of developing NS. The present study confirmed
that age and the serum TRUST titer were risk factors for NS, which
is in accordance with previous studies (37). A serum TRUST titer ≥1:8 with 79.3%
sensitivity and 87.5% specificity was a strong predictor of NS. Of
note, 67.82% of patients with NS had a concomitantly high serum
TRUST titer and a high NLR, indicating that patients with a serum
TRUST titer ≥1:8 and an NLR ≥1.97 are more likely to have NS.
Furthermore, a parallel testing and serial testing format were
applied, revealing that the NLR plus serum TRUST titer may be a
potential predictor of NS (90.8% sensitivity and 50.0% specificity,
67.8% sensitivity and 90.0% specificity, respectively). Although
the sensitivity of a combination of the NLR (≥1.97) and serum TRUST
titer (≥1:8) was 90.8% with low specificity (50%), there is
currently no non-invasive test with this high sensitivity and
specificity to predict NS; thus, this may still encourage
physicians to perform LP to screen out underlying NS. Furthermore,
the sensitivity and specificity obtained with the serial testing
format was similar to the CSF-VDRL, which was considered as a
standard test with 33.3-70% sensitivity and 99% specificity for
diagnosing NS (2,38). Thus, this indicated that the NLR
(≥1.97) and serum TRUST titer (≥1:8) are useful biomarkers for
NS.
Non-invasive markers for predicting NS are currently
insufficient. In the present study, two easily accessible indices
related to NS were assessed and their diagnostic value for NS was
evaluated. Several limitations must be acknowledged in the current
study. First, the results are applicable to subjects with suspected
NS. Furthermore, the patients with Non-NS were not stratified
according to the stage of syphilis and whether there is a
difference between Non-NS at different stages and NS requires to be
confirmed with further large samples. Finally, the present study
was a single-center retrospective analysis of prospectively
collected data, and thus, a prospective, multi-center, large-sample
study is warranted.
In conclusion, the combination of the NLR and serum
TRUST titer is a useful indicator of NS. The NLR and serum TRUST
titer were reduced at the 6 month follow-up with resolved clinical
manifestations and CSF laboratory parameters, suggesting that these
simple, rapid and easily obtainable prognostic biomarkers may be
utilized to monitor the disease course.
Supplementary Material
Comparison of the parameters between
neurosyphilis and non-neurosyphilis patients and age- and
gender-matched healthy controls.
Changes in parameters after treatment
with penicillin at 6-month follow up of 24 NS patients.
Acknowledgements
Not applicable.
Funding
This work was supported by the scientific research
fund of Wannan Medical College in Anhui Province, Wuhu, China
(grant no. WK2017F08 to CH).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CH planned and conceived the study. CH, XS and CC
collected the data. WL, SH and JC interpreted the data. CH and CC
wrote and critically revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the ethics committee of
Yijishan Hospital of Wannan Medical College (Wuhu, China) and all
participants provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zheng D, Zhou D, Zhao Z, Liu Z, Xiao S,
Xing Y, Suo WZ and Liu J: The clinical presentation and imaging
manifestation of psychosis and dementia in general paresis: A
retrospective study of 116 cases. J Neuropsychiatry Clin Neurosci.
23:300–307. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Janier M, Hegyi V, Dupin N, Unemo M,
Tiplica GS, Potocnik M, French P and Patel R: 2014 European
guideline on the management of syphilis. J Eur Acad Dermatol
Venereol. 28:1581–1593. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Marra CM, Tantalo LC, Maxwell CL, Ho EL,
Sahi SK and Jones T: The rapid plasma reagin test cannot replace
the venereal disease research laboratory test for neurosyphilis
diagnosis. Sex Transm Dis. 39:453–457. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Soliman WM, Sherif NM, Ghanima IM and
El-Badawy MA: Neutrophil to lymphocyte and platelet to lymphocyte
ratios in systemic lupus erythematosus: Relation with disease
activity and lupus nephritis. Reumatol Clin. 16:255–261.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Goyal N, Tsivgoulis G, Chang JJ, Malhotra
K, Pandhi A, Ishfaq MF, Alsbrook D, Arthur AS, Elijovich L and
Alexandrov AV: Admission neutrophil-to-lymphocyte ratio as a
prognostic biomarker of outcomes in large vessel occlusion strokes.
Stroke. 49:1985–1987. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Yang W, Wang X, Zhang W, Ying H, Xu Y,
Zhang J, Min Q and Chen J: Neutrophil-lymphocyte ratio and
platelet-lymphocyte ratio are 2 new inflammatory markers associated
with pulmonary involvement and disease activity in patients with
dermatomyositis. Clin Chim Acta. 465:11–16. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kim DS, Shin D, Lee MS, Kim HJ, Kim DY,
Kim SM and Lee MG: Assessments of neutrophil to lymphocyte ratio
and platelet to lymphocyte ratio in Korean patients with psoriasis
vulgaris and psoriatic arthritis. J Dermatol. 43:305–310.
2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Abakay O, Abakay A, Sen HS and Tanrikulu
AC: The relationship between inflammatory marker levels and
pulmonary tuberculosis severity. Inflammation. 38:691–696.
2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Russo A, Russano M, Franchina T,
Migliorino MR, Aprile G, Mansueto G, Berruti A, Falcone A, Aieta M,
Gelibter A, et al: Neutrophil-to-lymphocyte ratio (NLR),
platelet-to-lymphocyte ratio (PLR), and outcomes with nivolumab in
pretreated non-small cell lung cancer (NSCLC): A large
retrospective multicenter study. Adv Ther. 37:1145–1155.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jiang Y, Weng R, Zhang Y, Fan R, Liu Y,
Chen Z, Peng F, Chen Y and Chen X: The performance of rapid plasma
reagin (RPR) titer in HIV-negative general paresis after
neurosyphilis therapy. BMC Infect Dis. 18(144)2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Erkus E, Aktas G, Atak BM, Kocak MZ, Duman
TT and Savli H: Haemogram parameters in vitamin D deficiency. J
Coll Physicians Surg Pak. 28:779–782. 2018.PubMed/NCBI
|
|
12
|
Sakamoto T, Saito H, Uchinaka EI, Morimoto
M, Amisaki M, Tokuyasu N, Honjo S, Ashida K and Fujiwara Y: The
combination of neutrophil-to-lymphocyte ratio and serum
carbohydrate antigen 19-9 level as a prognostic indicator in
patients with recurrent pancreatic cancer. Anticancer Res.
38:5497–5503. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Aktas G, Sit M, Dikbas O, Erkol H,
Altinordu R, Erkus E and Savli H: Elevated neutrophil-to-lymphocyte
ratio in the diagnosis of Hashimoto's thyroiditis. Rev Assoc Med
Bras (1992). 63:1065–1068. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ackland GL, Abbott TEF, Cain D, Edwards
MR, Sultan P, Karmali SN, Fowler AJ, Whittle JR, MacDonald NJ,
Reyes A, et al: Preoperative systemic inflammation and
perioperative myocardial injury: Prospective observational
multicentre cohort study of patients undergoing non-cardiac
surgery. Br J Anaesth. 122:180–187. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Duman TT, Aktas G, Atak BM, Kocak MZ,
Erkus E and Savli H: Neutrophil to lymphocyte ratio as an
indicative of diabetic control level in type 2 diabetes mellitus.
Afr Health Sci. 19:1602–1606. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sit M, Aktas G, Erkol H, Yaman S, Keyif F
and Savli H: Neutrophil to lymphocyte ratio is useful in
differentiation of malign and benign thyroid nodules. P R Health
Sci J. 38:60–63. 2019.PubMed/NCBI
|
|
17
|
Wong T, Fonseca K, Chernesky MA, Garceau
R, Levett PN and Serhir B: Canadian public health laboratory
network laboratory guidelines for the diagnosis of neurosyphilis in
Canada. Can J Infect Dis Med Microbiol. 26 (Suppl A):18A–22A.
2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Xiao Y, Tong ML, Liu LL, Lin LR, Chen MJ,
Zhang HL, Zheng WH, Li SL, Lin HL, Lin ZF, et al: Novel predictors
of neurosyphilis among HIV-negative syphilis patients with
neurological symptoms: An observational study. BMC Infect Dis.
17(310)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hemond CC, Glanz BI, Bakshi R, Chitnis T
and Healy BC: The neutrophil-to-lymphocyte and
monocyte-to-lymphocyte ratios are independently associated with
neurological disability and brain atrophy in multiple sclerosis.
BMC Neurol. 19(23)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Haghshomar M, Rahmani F, Hadi Aarabi M,
Shahjouei S, Sobhani S and Rahmani M: White matter changes
correlates of peripheral neuroinflammation in patients with
Parkinson's disease. Neuroscience. 403:70–78. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Calapkulu M, Sencar ME, Sakiz D, Duger H,
Ozturk Unsal I, Ozbek M and Cakal E: The prognostic and diagnostic
use of hematological parameters in subacute thyroiditis patients.
Endocrine. 68:138–143. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lin LR, Lin DH, Tong ML, Liu LL, Fan JY,
Zhu XZ, Gao K, Chen MJ, Zheng WH, Zhang HL, et al: Macrophage
migration inhibitory factor as a novel cerebrospinal fluid marker
for neurosyphilis among HIV-negative patients. Clin Chim Acta.
463:103–108. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hu R, Lu C, Lu S, Hu Y, Ma H, Lai W, Zhu
G, Feng P, Lu R and Li Y: Value of CXCL13 in diagnosing
asymptomatic neurosyphilis in HIV-infected patients. Int J STD
AIDS. 27:141–146. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Pastuszczak M, Jakiela B, Jaworek AK,
Wypasek E, Zeman J and Wojas-Pelc A: Association of Interleukin-10
promoter polymorphisms with neurosyphilis. Hum Immunol. 76:469–472.
2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Lin LR, Gao ZX, Lin Y, Zhu XZ, Liu W, Liu
D, Gao K, Tong ML, Zhang HL, Liu LL, et al: Akt, mTOR and NF-KB
pathway activation in Treponema pallidum stimulates M1 macrophages.
Int Immunopharmacol. 59:181–186. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Xu M, Xie Y, Jiang C, Xiao Y, Kuang X, Wen
Y, Tan Y, Tan M, Zhao F, Zeng T and Wu Y: Treponema pallidum
flagellins elicit proinflammatory cytokines from human monocytes
via TLR5 signaling pathway. Immunobiology. 222:709–718.
2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Luo X, Zhang X, Zhao T, Zeng T, Liu W,
Deng M and Zhao F: A preliminary study on the proinflammatory
mechanisms of Treponema pallidum outer membrane protein Tp92 in
human macrophages and HMEC-1 cells. Microb Pathog. 110:176–183.
2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Liu S, Wang S, Wu Y, Zhao F, Zeng T, Zhang
Y, Zhang Q and Gao D: Production of proinflammatory cytokines in
the human THP-1 monocyte cell line following induction by Tp0751, a
recombinant protein of Treponema pallidum. Sci China Life Sci.
53:229–233. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Liu LL, Chao PL, Zhang HL, Tong ML, Liu
GL, Lin LR, Su YH, Wu JY, Dong J, Zheng WH and Yang TC: Analysis of
lymphocyte subsets in HIV-negative neurosyphilis patients. Diagn
Microbiol Infect Dis. 75:165–168. 2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Yu Q, Cheng Y, Wang Y, Wang C, Lu H, Guan
Z, Huang J, Gong W, Shi M, Ni L, et al: Aberrant humoral immune
responses in neurosyphilis: CXCL13/CXCR5 play a pivotal role for
B-cell recruitment to the cerebrospinal fluid. J Infect Dis.
216:534–544. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sargin G, Senturk T, Yavasoglu I and Kose
R: Relationship between neutrophil-lymphocyte, platelet-lymphocyte
ratio and disease activity in rheumatoid arthritis treated with
rituximab. Int J Rheum Dis. 21:2122–2127. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Hu ZD, Sun Y, Guo J, Huang YL, Qin BD, Gao
Q, Qin Q, Deng AM and Zhong RQ: Red blood cell distribution width
and neutrophil/lymphocyte ratio are positively correlated with
disease activity in primary Sjogren's syndrome. Clin Biochem.
47:287–290. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Shi M, Peng RR, Gao Z, Zhang S, Lu H, Guan
Z, Gao Y, Wang C and Zhou P: Risk profiles of neurosyphilis in
HIV-negative patients with primary, secondary and latent syphilis:
Implications for clinical intervention. J Eur Acad Dermatol
Venereol. 30:659–666. 2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Pastuszczak M, Zeman J, Jaworek AK and
Wojas-Pelc A: Cerebrospinal fluid abnormalities in HIV-negative
patients with secondary and early latent syphilis and serum VDRL
≥1:32. Indian J Dermatol. 58(325)2013.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Marra CM, Maxwell CL, Smith SL, Lukehart
SA, Rompalo AM, Eaton M, Stoner BP, Augenbraun M, Barker DE,
Corbett JJ, et al: Cerebrospinal fluid abnormalities in patients
with syphilis: Association with clinical and laboratory features. J
Infect Dis. 189:369–376. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
36
|
Jiang Y, Chen X, Ma X, Yang Y, Peng F and
Hu X: The usefulness of toluidine red unheated serum test in the
diagnosis of HIV-negative neurosyphilis. Sex Transm Dis.
38:244–245. 2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Sun JJ, Wang ZY, Shen JY, Shen YZ, Liu L,
Wang JR, Zhang RF and Lu HZ: Serum TRSUT Titer ≥1: 16 is a
predictor for neurosyphilis among HIV-infected patients with
concurrent syphilis and no neurological symptoms. Medicine
(Baltimore). 94(e2023)2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Castro R, Prieto ES and da Luz Martins
Pereira F: Nontreponemal tests in the diagnosis of neurosyphilis:
An evaluation of the Venereal disease research laboratory (VDRL)
and the rapid plasma reagin (RPR) tests. J Clin Lab Anal.
22:257–261. 2008.PubMed/NCBI View Article : Google Scholar
|