Introduction
Breast cancer (BC) is the second leading cause of
cancer-associated deaths amongst women worldwide (1,2) with
>450,000 BC-associated deaths each year in the world according
to the statistical analysis from World Cancer Research Fund
(3). China is one of the countries
with the top 3 highest incidence of BC worldwide (4). Despite the wide use of curative
surgery and adjuvant chemotherapy for patients with BC, distant
metastasis and tumor recurrence remains a major issue for improving
BC prognosis (2,5). Therefore, understanding the
pathological mechanisms underlying BC development and progression
and identifying the specific targets, may provide an effective
strategy for diagnosis and therapy for treating patients with
BC.
Metastasis accounts for 90% of all BC-associated
deaths, during which epithelial-mesenchymal transition (EMT) is a
pivotal process which allows cancer progression and metastasis
(2,6). EMT involves a transformational change
of epithelial cells to mesenchymal cells characterized by loss of
adhesion, invasive and metastatic properties and acquisition of a
cancer stem cell phenotype (2,7). Tumor
cells undergoing EMT demonstrate gain of mesenchymal markers such
as fibronectin (FN) and smooth muscle actin α (α-SMA) (5,8,9), and a
downregulation of epithelial markers, such as E-cadherin and CK18
(9-11).
MicroRNAs (miRNAs/miRs) are small (18-22
nucleotides) single-stranded non-coding RNAs that regulate gene
expression at the post-transcriptional level by recognizing
specific target mRNAs resulting in their targeted degradation or
inhibition of translation (12,13).
Various miRNAs have been demonstrated to serve varying roles in
numerous tumor progressing biological behaviors, including
proliferation, apoptosis, differentiation, migration, invasion,
metastasis and angiogenesis (14-16).
miRNAs are involved in the occurrence and development of cancer,
functioning either as tumor suppressors or oncogenes (17,18).
Abnormal expression of miRNAs has been demonstrated in a number of
different types of cancer and is closely associated with cancer
progression (17,18). Previous studies have shown that the
levels of miR-155 were significantly increased in BC tissue, and
this was positively associated with the occurrence and metastasis
of BC, suggesting the oncogenic function of miR-155 (19,20).
However, the mechanisms underlying miR-155 function are not
completely understood, and it is unknown whether miR-155 functions
partially by mediating EMT.
Transforming growth factor β receptor type II
(TGFBR2) is a crucial signaling in tumor epithelial cells. Lower
levels of TGFBR2 expression have been detected in BC tissue and the
reduced expression of TGFBR2 is associated with adverse
pathological characteristics and poor prognosis of patients with BC
(21,22). TGFBR2 acts as bona fide
metastasis suppressor gene (23).
TGFBR2 pathways regulate various processes like EMT, angiogenesis
and immunomodulation (24). To the
best of our knowledge, a direct interaction between miR-155 and
TGFBR2 has not been previously demonstrated.
The aim of the present study was to assess the
expression levels of miR-155 and TGFBR2 in BC tissue, determine
whether miR-155 directly interacted with TGFBR2, and examine the
effects of miR-155 on proliferation and invasion of MCF-7 cells.
The present study may improve the understanding of the role of
miR-155 in the pathological mechanisms underlying development and
progression of BC.
Materials and methods
Tissue samples
A total of 30 pairs of BC and corresponding normal
tissue were collected from patients who underwent surgery in
Xinganmeng People's Hospital (Inner Mongolia, China) from January
1st 2016 to April 30th, 2017 and all the specimens were confirmed
using routine pathological examinations and staged according to the
tumor-node-metastasis (TNM) system (25,26).
The patient (female) age range was 41-68 (median age=59).
Radiotherapy and chemotherapy were not performed prior to surgery.
Written informed consent was obtained from all the patients and the
experiments were approved by The Ethics Committee of Xinganmeng
People's Hospital (Inner Mongolia, China). Clinicopathological
characteristics of patients collected, included age, sex, tumor
size, pathological stage, lymph node metastasis, ER status, PR
status and HER2 status. The characteristics and prevalence of each
are listed in Table I.
 | Table IExpression of miR-155 in patients with
breast cancer. |
Table I
Expression of miR-155 in patients with
breast cancer.
| Clinicopathological
characteristic | n | miR-155 High | miR-155 Low | P-value |
|---|
| Age, years | | | | 0.4642 |
|
≥50 | 16 | 7 | 9 | |
|
<50 | 14 | 8 | 6 | |
| Tumor size, cm | | | | 0.0303a |
|
<3 | 13 | 4 | 9 | |
|
≥3 | 17 | 12 | 5 | |
| TNM stage | | | | 0.0253a |
|
I-II | 18 | 6 | 12 | |
|
III-IV | 12 | 9 | 3 | |
| Lymph node
metastasis | | | | 0.0295a |
|
No | 11 | 3 | 8 | |
|
Yes | 19 | 13 | 6 | |
| Estrogen receptor
status | | | | 0.7125 |
|
Positive | 15 | 8 | 7 | |
|
Negative | 15 | 9 | 6 | |
| Progesterone
receptor status | | | | 0.7851 |
|
Positive | 17 | 7 | 10 | |
|
Negative | 13 | 6 | 7 | |
| Human epidermal
growth factor receptor 2 status | | | | 0.6956 |
|
Positive | 16 | 8 | 8 | |
|
Negative | 14 | 8 | 6 | |
Cell culture and treatment
MCF-7 BC cells were purchased from The Cell Bank of
Type Culture Collection of the Chinese Academy of Sciences and
cultured in RPMI-1640 medium (Invitrogen; Thermo Fisher Scientific
Inc.) supplemented with 10% FBS (Invitrogen; Thermo Fisher
Scientific Inc.) and 1% (w/v) penicillin/streptomycin
(Sigma-Aldrich; Merck KGaA) at 37˚C in a 5% CO2
incubator. Cells were passaged at 80-90% confluence, and the cells
in the logarithmic growth phase were used for further
experiments.
MCF-7 cells were divided into three groups according
to the treatment as follows: No treatment (control group), miR-155
mimics group, miR-155 inhibitor (inhibitor group) and miR-155
negative control (NC) group. Cells were transfected with miR-155
mimics (5'-UUAAUGCUAAUCGUGAUAGGGG-3') miR-NC mimics
(5'-CAGUACUUUUGUGUAGUACAA-3'), miR-155 inhibitor
(5'-CCCCUAUCACGAUUAGCAUUAA-3') or NC (5'-CAGUACUUUUGUGUAGUACAA-3')
(Guangzhou RiboBio Co., Ltd.) using Lipofectamine™ 2000 according
to the manufacturer's protocols. The expression of miR-155 in each
group was detected by reverse transcription quantitative (RT-q)PCR
48 h after transfection.
Cell proliferation assay
Cells in each group were seeded into a 96-well
culture plate at a density of 1x105 cells/well and
cultured for 12, 24 or 48 h. Cell proliferation was assessed using
an MTT assay (Bio-Rad Laboratories, Inc.). According to the
manufacturer's protocol, 10 µl MTT reagent (5 mg/ml) was added to
each well. After incubation for 4 h at 37˚C, the medium was
discarded and the cells were incubated with 150 µl DMSO (Bio-Rad
Laboratories, Inc.). The plates were shaken on a microvibrator for
10 min and the optical density of each well was measured using an
microplate reader (Bio-Rad Laboratories, Inc.) at 490 nm. The
results are expressed as a percentage of the untreated control.
RT-qPCR
Total RNA was extracted from cells (48 h
post-transfection) or tissue using TRIzol® reagent
(Thermo Fisher Scientific, Inc.), and subsequently transcribed into
cDNA using PrimeScript™ RT reagent kit (Takara Bio, Inc., Otsu,
Japan) at 42˚C for 15 min. qPCR was performed using
SYBR® Premix Ex Taq™ kit (Takara Bio, Inc.) on an ABI
7300 Real-Time PCR system (Applied Biosystems; Thermo Fisher
Scientific, Inc.) with customized primer sets for TGFBR2, CK18,
E-cadherin, FN and α-SMA. The relative expression of mRNA in each
sample was normalized to the level of GAPDH using the
2-ΔΔCq method (27). The
expression of miR-155 was examined using the Hairpin-it™ miRNAs
qPCR Quantitation kit (Shanghai GenePharma Co., Ltd.) according to
manufacturer's protocol, and U6 was used as an internal control for
normalization. Primers were synthesized by GenScript and the
sequences are listed in Table
II.
 | Table IISequences of the primers. |
Table II
Sequences of the primers.
| Gene | Primer
sequence |
|---|
| microRNA-155 | |
|
Forward |
5'-UAAUACCGUCUUAAAACCGU-3' |
|
Reverse |
5'-UUCUGGGAACGUGAAACCT-3' |
| U6 | |
|
Forward |
5'-CTCGCTTCGGCAGCACA-3' |
|
Reverse |
5'-AACGCTTCACGAATTTGCGT-3' |
| Transforming growth
factor β receptor type II | |
|
Forward |
5'-TCTGGGCTCCTGATTGCT-3' |
|
Reverse |
5'-TGAGGCAGCTTTGTAAGT-3' |
| E-Cadherin | |
|
Forward |
5'-GTGGCCCGGATGTGAGAAG-3' |
|
Reverse |
5'-GGAGCCCTTGTCGGATGATG-3' |
| CK18 | |
|
Forward |
5'-AAGAAAACCCGAAGAGG-3' |
|
Reverse |
5'-CTGACTCAAGGTGCAGC-3' |
| Fibronectin | |
|
Forward |
5'-TTGTTCGGTGGAGTAGACCC-3' |
|
Reverse |
5'-GTGCCAGTGGTCTCTTGTTG-3' |
| Smooth muscle
actin-α | |
|
Forward |
5'-TTCCTTCGTGACTACTGCTGAG-3' |
|
Reverse |
5'-CAATGAAAGATGGCTGGAAGAG-3' |
| GAPDH | |
|
Forward |
5'-GCACCACCAACTGCTTAGC-3' |
|
Reverse |
5'-GGCATGGACTGTGGTCATGAG-3' |
Western blotting
Cells (48 h post-transfection) from each group or
tissue samples were collected and lysed using RIPA lysis buffer
(Beyotime Institute of Biotechnology), Shanghai, China) on ice.
After centrifugation, the supernatant was obtained and the protein
concentration was measured using a Pierce® BCA Protein
assay kit (Thermo Fisher Scientific, Inc.). The protein extracts
were mixed with loading buffer, and denatured in a boiling water
bath for 10 min. Equivalent quantities 20 µg of protein were loaded
onto a 10% SDS gel, resolved using SDS-PAGE and transferred to PVDF
membranes. The membranes were blocked with tris-buffered saline
Tween 20 (TBST) containing 5% skimmed milk and subsequently
incubated with primary antibodies against human TGFBR2 (cat. no.
ab186838), CK18 (cat. no. ab133263), E-cadherin (cat. no.
ab256580), FN (cat. no. ab2413), α-SMA (cat. no. ab32575; 1:200 for
anti-CK18 antibody, 1:100 for all other antibodies) at 4˚C
overnight. The membranes were washed and then incubated with
Horseradish Peroxidase (HRP)-conjugated secondary antibodies (cat.
no. ab6721; 1:5,000) at room temperature for 60 min. All the
antibodies were purchased from Abcam. Target proteins were detected
using Novex® ECL Chemiluminescent Substrate Reagent kit
(Thermo Fisher Scientific, Inc.) using a ChemiDoc™ XRS+ imaging
system (Bio-Rad Laboratories, Inc.). The density of protein bands
was analyzed using Gel-Pro analyzer software 4.0 (Media
Cybernetics, Inc.) and the data are expressed as the ratio of each
target protein to the internal control, GAPDH (cat. no. ab181602,
1:10,000; Abcam) at 4˚C overnight.
Dual luciferase activity assay
The target of miR-155 was predicted by the online
database Targetscan 7.2 [http://www.targetscan.org/vert_72/ (28)]. The 3'UTR of TGFBR2 containing the
predicted miR-155 specific binding site was amplified by PCR from
genomic DNA, and inserted into the pMIR-REPORT™ luciferase reporter
vector (Thermo Fisher Scientific, Inc.) to obtain the wild-type
luciferase reporter plasmid p-TGFBR2-wt. PCR was performed using
the following thermocycling conditions: 94˚C for 2 min, followed by
35 cycles of 94˚C for 2 sec, 60˚C for 60 sec and 72˚C for 1 min.
The PCR products were amplified using cDNA and fused to the firefly
luciferase gene of the pGL3-control plasmid (Promega Corporation)
with the restriction enzyme sites of KpnI and XhoI. Two site
mutations were introduced to WT-TGFBR2-3'-UTR to construct the
mutant (MUT) TGFBR2-3'-UTR using a Quick Site-directed mutation kit
(Agilent Technologies, Inc.). The cells were co-transfected with
pGL3 constructions including 200 ng pGL3-WT-TGFBR2 and 200 ng
pGL3-Mut-TGFBR2, 10 nM miR-NC or 10 nM miR-155 mimics and 26 ng
pRL-TK in 24-well plates using Lipofectamine® 2000 (Invitrogen,
USA). At 24 h of transfection, luciferase activity (firefly and
Renilla) was determined using the dual-luciferase reporter
assay system (Promega, USA).
Statistical analysis
All data were analyzed using SPSS version 20.0 (IBM,
Corp.). Data are presented as the mean ± standard deviation SD.
Statistical significance between groups was analyzed using ANOVA
analysis and a Bonferroni post-hoc test. A χ2 test was
used to analyze the association between miR-155 expression and
clinicopathological characteristics. P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinical features
As showed in Table
I, overexpression of miR-155 was significantly associated with
larger breast tumor sizes, TNM stage and lymph node metastasis.
However, there was no significant difference between ages, ER
status, PR status and HER2 status between the patients with high or
low miR-155 expression levels.
miR-155 expression is increased in
human BC tissue and is negatively associated with TGFBR2
expression
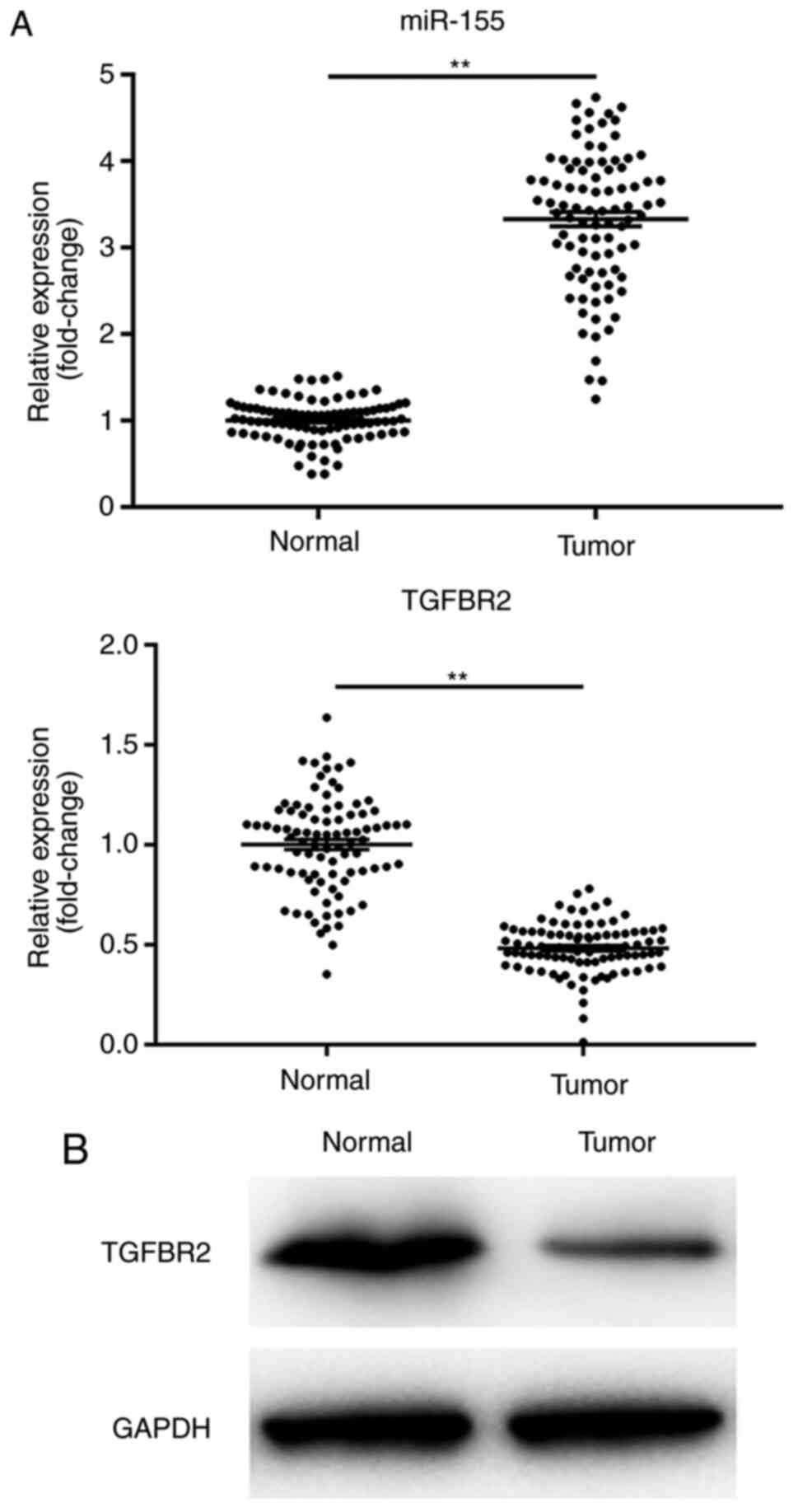
The levels of miR-151 and TGFBR2 were detected in
all 30 pairs of human BC tissues and adjacent normal controls.
RT-qPCR data showed that the levels of miR-151 were significantly
increased in BC tissues compared with their paired normal tissues
(Fig. 1A; P<0.01). Furthermore,
human BC tissues exhibited a significant reduction in TGFBR2
expression, both at the mRNA and protein levels compared with the
normal control tissues (Fig. 1A and
B; P<0.01). These data are
consistent with the previous studies, and suggested an inverse
association between the expression levels of miR-155 and its target
TGFBR2.
miR-155 inhibitor downregulates the
expression of miR-155
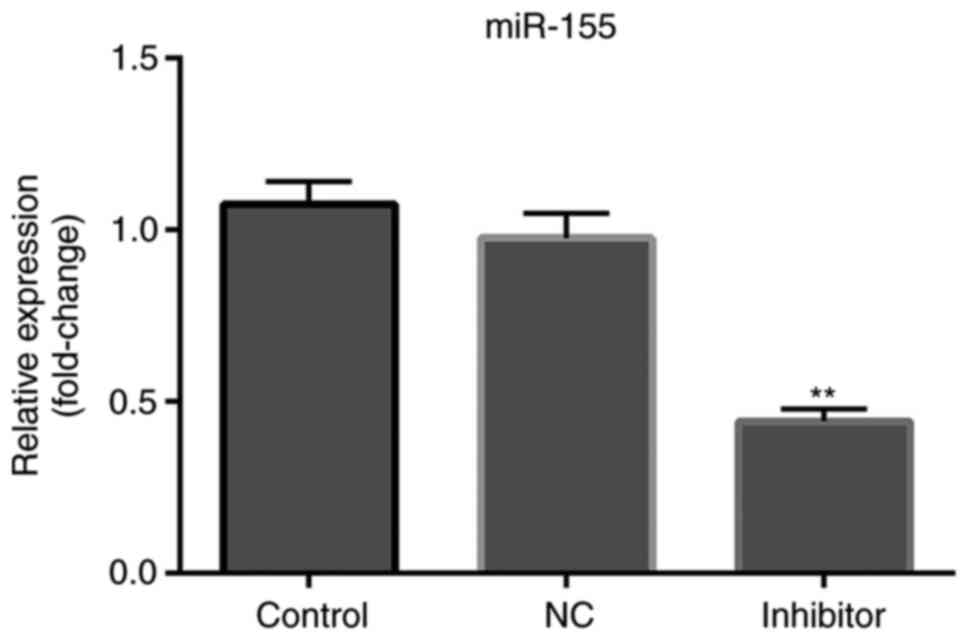
MCF-7 cells were transfected with miR-155 NC
inhibitor or miR-155 inhibitor. As shown in Fig. 2, the expression levels of miR-155 in
cells transfected with miR-155 inhibitor was significantly lower
compared with the control and NC group (P<0.01).
miR-155 inhibitor suppresses
proliferation of MCF-7 cells
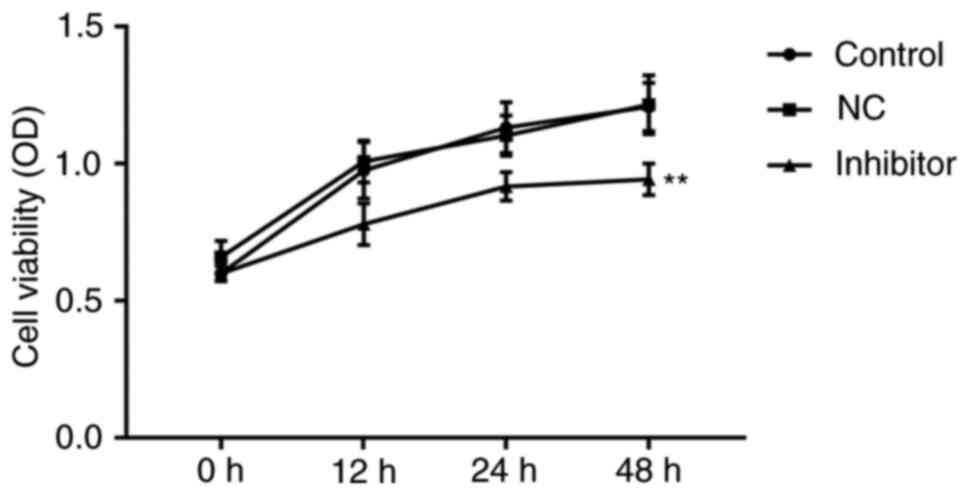
miR-155 inhibitor or miR-155 NC inhibitor were
transfected into MCF-7 cells and MTT assays were performed to
assess the effects of miR-155 on cell proliferation. As shown in
Fig. 3, miR-155 levels were lower
in the miR-155 inhibitor transfected cells, compared with the
NC-transfected or control cells. miR-155 inhibitor resulted in a
slight decrease in cell proliferation 12 and 24 h after
transfection (P>0.05), and a significant reduction in
proliferation after 48 h (P<0.01).
miR-155 inhibitor enhances the
expression of TGFBR2 and mediates the expression of EMT-associated
molecules
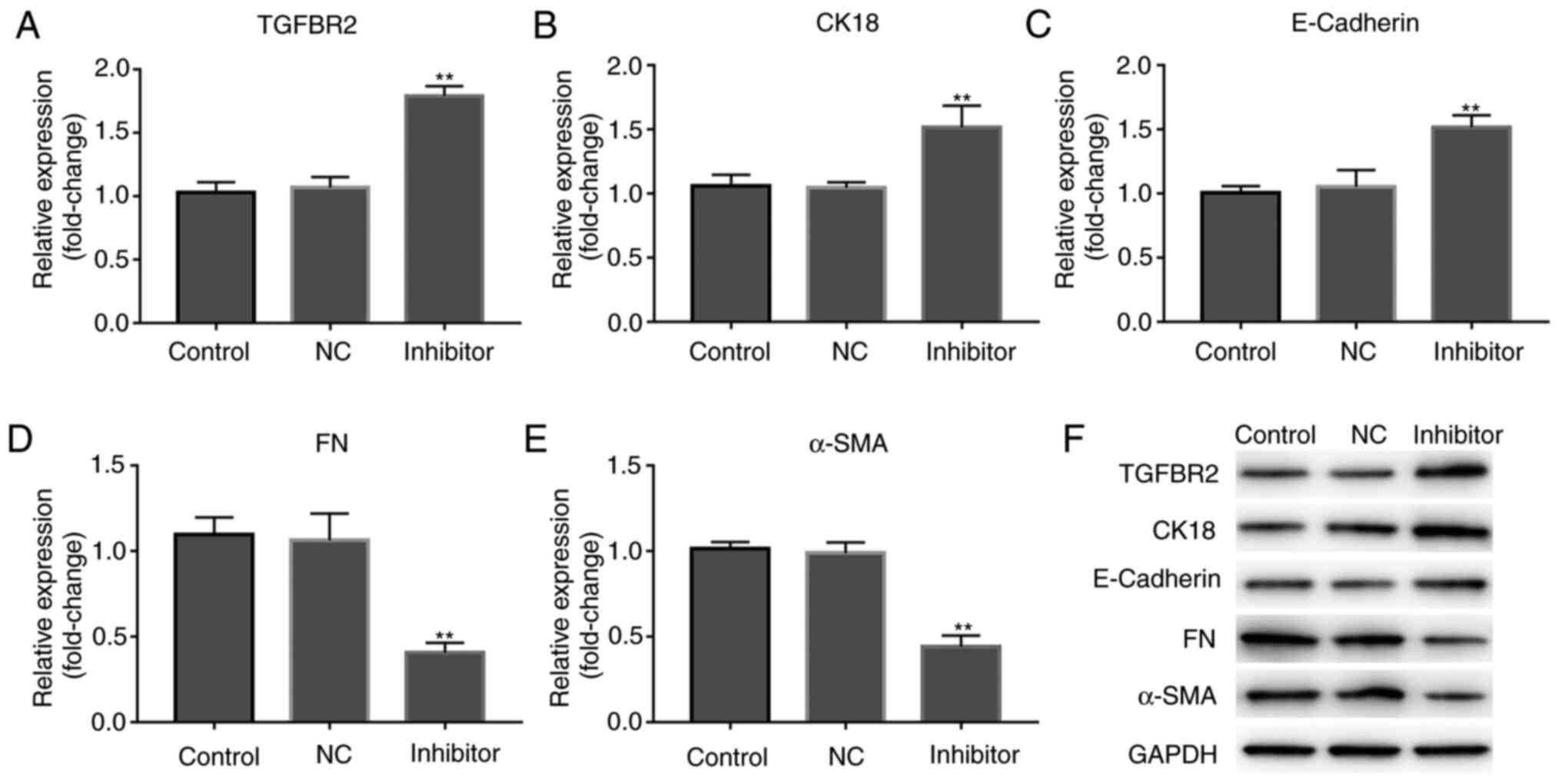
As there was an inverse association between miR-155
and TGFBR2 expression levels in human BC tissues, MCF-7 cells were
transfected with miR-155 inhibitor, and the expression of TGFBR2
was shown to be increased. As shown in Fig. 4A and F, miR-155 inhibitor resulted in a
significant increase in TGFBR2 expression, both at the mRNA and
protein expression levels (P<0.01).
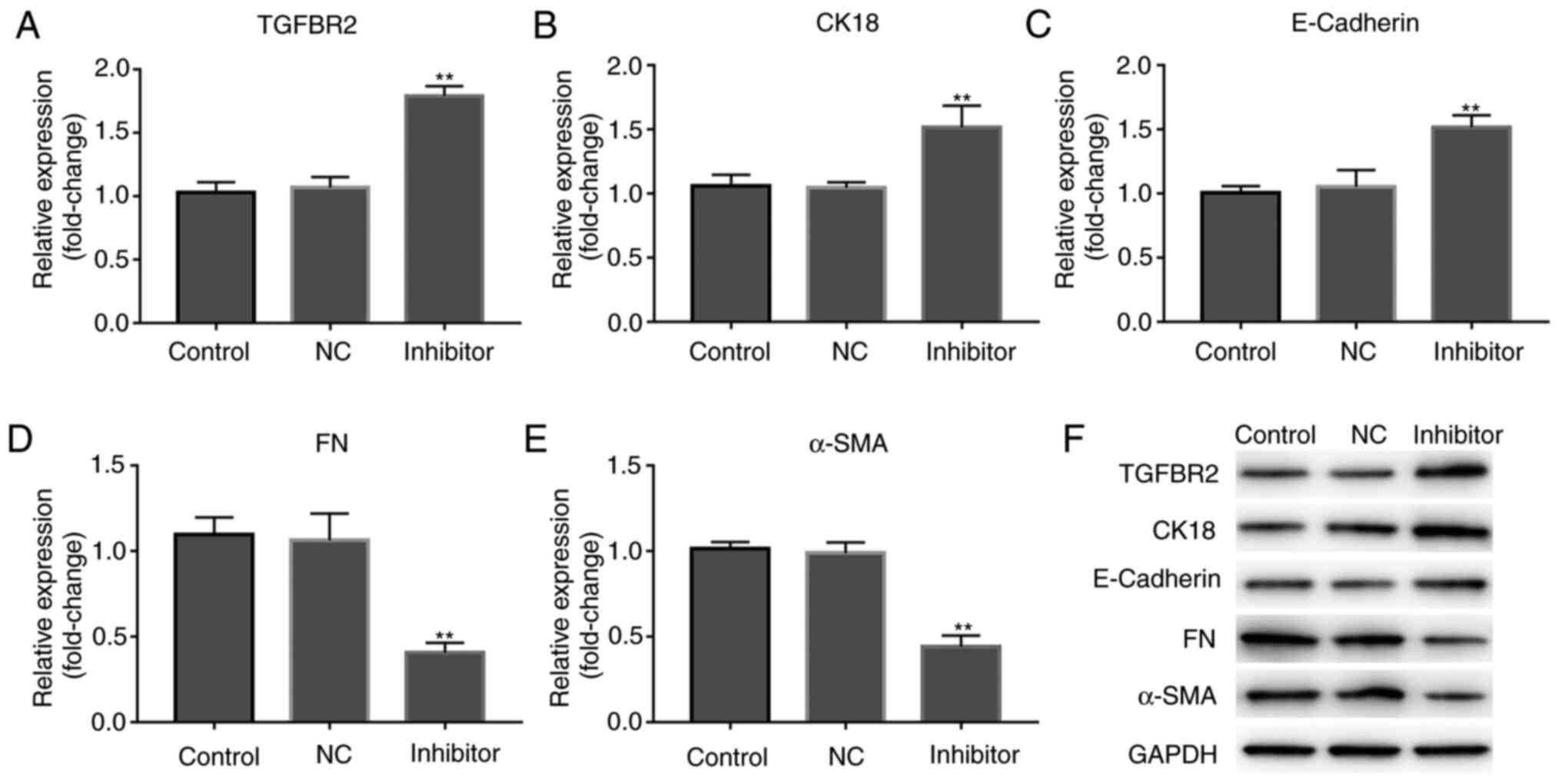 | Figure 4miR-155 inhibitor enhances the
expression of TGFBR2 and mediates the expression of EMT-related
molecules. Reverse transcription-quantitative PCR analysis of the
effect of miR-155 inhibitor on the expression of (A) TGFBR2, (B)
CK18, (C) E-cadherin, (D) FN and (E) α-SMA. Results are expressed
relative to the value of the controls that were assigned a value of
1. **P<0.01 vs. the control group. (F) Representative
western blots showing the expression of TGFBR2, CK18, E-cadherin,
FN and α-SMA in each cell group. GAPDH was used as the loading
control. miR-155, microRNA-155; TGFBR2, transforming growth factor
β receptor type II; EMT, epithelial-mesenchymal transition; FN,
fibronectin; SMA-α, smooth muscle actin α. |
Subsequently, whether miR-155 mediated expression of
EMT-associated markers was assessed. As shown in Fig. 4B-F, miR-155 inhibitor resulted in
alterations in the expression of epithelial markers, including a
significant increase in E-cadherin and CK18 expression levels, and
significant decrease in the expression of the mesenchymal markers,
FN and α-SMA in MCF-7 cells. These data suggest that miR-155
inhibitor suppressed the metastatic properties of MCF-7 cells.
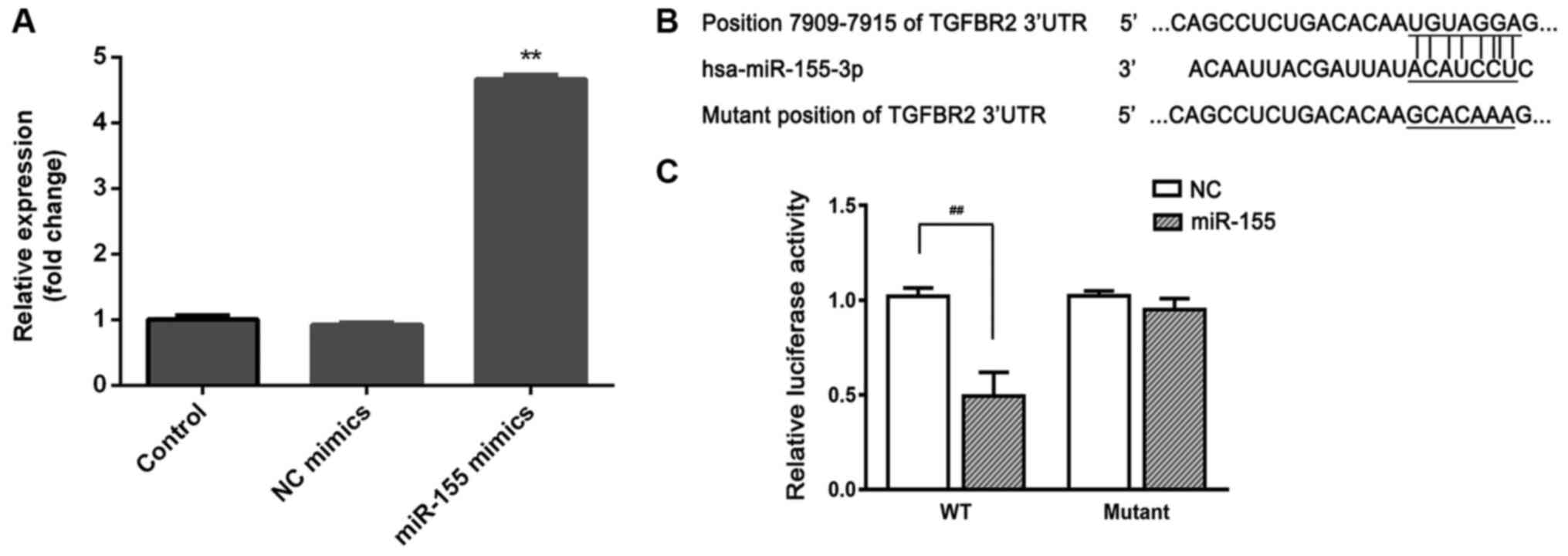
TGFBR2 is a direct target of
miR-155
To confirm whether the observed reduction in TGFBR2
mRNA and protein levels was the result of direct binding between
miR-155 and the 3'UTR of TGFBR2, first, cells were transfected
miR-155 mimics or its negative control. As shown in Fig. 5A, and the expression of miR-155 was
significantly increased in cells transfected with miR-155 mimics,
suggesting successful transfection. Subsequently, the segment of
TGFBR2 3'UTR containing the putative binding site for miR-155 was
cloned and inserted into a firefly luciferase reporter vector to
obtain p-TGFBR2-wt or p-TGFBR2-mut (Fig. 5B). When co-transfected in HEK-293T
cells, miR-155 significantly repressed the luciferase activity of
p-TGFBR2-wt, whereas luciferase expression was significantly higher
in cells transfected with p-TGFBR2-mut and miR-155 (Fig. 5C). These data suggest that miR-155
binds directly binds to TGFBR2 3'UTR and thereby reduced mRNA and
protein expression levels of TGFBR2.
Discussion
miRNAs exhibit notable potential for use in the
diagnosis and treatment of BC (29,30).
miR-155 has been reported to be strongly associated with BC
progression (16,17). Combining previous studies (16,17)
with the results of the present study, it was confirmed that the
levels of miR-155 were significantly increased in human BC tissues
compared with paired normal controls. These data suggest that
miR-155 may function as an oncogene.
To determine the roles of miR-155 in the
pathogenesis of BC, in vitro studies using MCF-7 human BC
cells were performed. Cell proliferation and metastasis are
essential events accounting for tumor progression. The results of
the present study data showed that transfection of a miR-155
inhibitor resulted in reduced proliferation and survival of MCF-7
cells. miR-155 has also been shown to increase BC metastasis in
vivo in previous studies (19,20).
Thus, whether miR-155 modulated expression of EMT markers in MCF7
cells was assessed, as EMT is a major cause of tumor metastasis. A
decrease in the expression of the mesenchymal markers (FN and
α-SMA), and an increase in the expression epithelial markers
(E-cadherin and CK18) was observed in MCF-7 cells following
treatment with miR-155 inhibitor, suggesting that downregulation of
miR-155 reduced EMT in MCF-7 cells.
Bioinformatics analysis showed that TGFBR2 was a
potential direct target of miR-155. Lower levels of TGFBR2
expression were observed in human BC tissues, consistent with
previous studies (21,22). Therefore, it was hypothesized that
miRNA-155 could directly negatively regulate TGFBR2 mRNA and
protein expression levels. To confirm this hypothesis, MCF-7 cells
were transfected with miR-155 inhibitor. The miR-155 inhibitor
induced enhanced expression of TGFBR2, suggesting that miR-155
inversely regulated TGFBR2 expression. Subsequently, direct binding
of miR-155 to the TGFBR2 3'UTR was confirmed through the use of a
dual luciferase assay.
Taken together, the results of the present study
demonstrate that miR-155 promoted proliferation and metastasis of
MCF-7 cells, and negatively regulated expression of its target,
TGFBR2, by directly binding to its mRNA transcript. These results
suggest that miR-155 may serve an important role in BC pathogenesis
and potentially be used for development of novel diagnostic and
therapeutic strategies for treatment of patients with BC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TH conceived and designed the study. XL performed
the majority of the experiments and wrote the manuscript. YL
assisted with the experiments. ZL participated in the analysis and
data interpretation. All authors read and approved the final
manuscrip.
Ethics approval and consent to
participate
The present study was performed in accordance with
standard guidelines and was approved by the Ethics Committee of
Xinganmeng People’s Hospital (Inner Mongolia, China). Written
informed consent was obtained from all the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zohrap N, Saatci Ö, Ozes B, Coban I, Atay
HM, Battaloglu E, Şahin Ö and Bugra K: SIK2 attenuates
proliferation and survival of breast cancer cells with simultaneous
perturbation of MAPK and PI3K/Akt pathways. Oncotarget.
9:21876–21892. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wang Y, Liu J, Ying X, Lin PC and Zhou BP:
Twist-mediated epithelial-mesenchymal transition promotes breast
tumor cell invasion via inhibition of hippo pathway. Sci Rep.
6(24606)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cancer Genome Atlas Network. Comprehensive
molecular portraits of human breast tumours. Nature. 490:61–70.
2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fan L, Strasser-Weippl K, Li JJ, St Louis
J, Finkelstein DM, Yu KD, Chen WQ, Shao ZM and Goss PE: Breast
Cancer in China. Lancet Oncol. 15:e279–e289. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Li CL, Yang D, Cao X, Wang F, Hong DY,
Wang J, Shen XC and Chen Y: Fibronectin induces
epithelial-mesenchymal transition in human breast cancer MCF-7
cells via activation of calpain. Oncol Lett. 13:3889–3895.
2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Al Moustafa AE, Achkhar A and Yasmeen A:
EGF-receptor signaling and epithelial-mesenchymal transition in
human carcinomas. Front Biosci (Schol Ed). 4:671–684.
2012.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Thiery JP, Acloque H, Huang RY and Nieto
MA: Epithelial-mesenchymal transitions in development and disease.
Cell. 139:871–890. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lupia A, Peppicelli S, Witort E, Bianchini
F, Carloni V, Pimpinelli N, Urso C, Borgognoni L, Capaccioli S,
Calorini L and Lulli M: CD63 tetraspanin is a negative driver of
epithelial-to-mesenchymal transition in human melanoma cells. J
Invest Dermatol. 134:2947–2956. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jeong H, Ryu YJ, An J, Lee Y and Kim A:
Epithelial-mesenchymal transition in breast cancer correlates with
high histological grade and triple-negative phenotype.
Histopathology. 60:E87–E95. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Yang D, Ma M, Zhou W, Yang B and Xiao C:
Inhibition of miR-32 activity promoted EMT induced by PM2.5
exposure through the modulation of the Smad1-mediated signaling
pathways in lung cancer cells. Chemosphere. 184:289–298.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Na Y, Kaul SC, Ryu J, Lee JS, Ahn HM, Kaul
Z, Kalra RS, Li L, Widodo N, Yun CO and Wadhwa R: Stress chaperone
mortalin contributes to epithelial-mesenchymal transition and
cancer metastasis. Cancer Res. 76:2754–2765. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hujie G, Zhou SH, Zhang H, Qu J, Xiong XW,
Hujie O, Liao CG and Yang SE: MicroRNA-10b regulates
epithelial-mesenchymal transition by modulating KLF4/KLF11/Smads in
hepatocellular carcinoma. Cancer Cell Int. 18(10)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Li C, Jiang Y, Miao R, Qu K, Zhang J and
Liu C: MicroRNA-1271 functions as a metastasis and
epithelial-mesenchymal transition inhibitor in human HCC by
targeting the PTP4A1/c-Src axis. Int J Oncol. 52:536–546.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
He L and Hannon GJ: MicroRNAs: Small RNAs
with a big role in gene regulation. Nat Rev Genet. 5:522–531.
2004.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Wang Z, Sha HH and Li HJ: Functions and
mechanisms of miR-186 in human cancer. Biomed Pharmacother.
119(109428)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Iacona JR and Lutz CS: miR-146a-5p:
Expression, regulation, and functions in cancer. Wiley Interdiscip
Rev RNA. 10(e1533)2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lages E, Ipas H, Guttin A, Nesr H, Berger
F and Issartel JP: MicroRNAs: Molecular features and role in
cancer. Front Biosci (Landmark Ed). 17:2508–2540. 2012.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Calin GA and Croce CM: MicroRNA signatures
in human cancers. Nat Rev Cancer. 6:857–866. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
19
|
Chernyy V, Pustylnyak V, Kozlov V and
Gulyaeva L: Increased expression of miR-155 and miR-222 is
associated with lymph node positive status. J Cancer. 9:135–140.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bašová P, Pešta M, Sochor M and Stopka T:
Prediction potential of serum miR-155 and miR-24 for relapsing
early breast cancer. Int J Mol Sci. 18(E2116)2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wei CY, Tan QX, Zhu X, Qin QH, Zhu FB, Mo
QG and Yang WP: Expression of CDKN1A/p21 and TGFBR2 in breast
cancer and their prognostic significance. Int J Clin Exp Pathol.
8:14619–14629. 2015.PubMed/NCBI
|
|
22
|
Volinia S, Calin GA, Liu CG, Ambs S,
Cimmino A, Petrocca F, Visone R, Iorio M, Roldo C, Ferracin M, et
al: A microRNA expression signature of human solid tumors defines
cancer gene targets. Proc Natl Acad Sci USA. 103:2257–2261.
2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Li X, Nadauld L, Ootani A, Corney DC, Pai
RK, Gevaert O, Cantrell MA, Rack PG, Neal JT, Chan CWM, et al:
Oncogenic transformation of diverse gastrointestinal tissues in
primary organoid culture. Nat Med. 20:769–777. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
24
|
Fricke F, Lee J, Michalak M, Warnken U,
Hausser I, Suarez-Carmona M, Halama N, Schnölzer M, Kopitz J and
Gebert J: TGFBR2-dependent alterations of exosomal cargo and
functions in DNA mismatch repair-deficient HCT116 colorectal cancer
cells. Cell Commun Signal. 15(14)2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gao H, Li P, Hei Y, Li S, Wang J, Lv X and
Zhang J: Long Non-coding RNA-ZNF281 promotes cancer cell migration
and invasion in gastric cancer via downregulation of microRNA-124.
Oncol Lett. 19:1849–1855. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhang J, Zhao B and Jin F: The assessment
of 8th edition AJCC prognostic staging system and a simplified
staging system for breast cancer: The analytic results from the
SEER database. Breast J. 25:838–847. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kang W, Tong JH, Lung RW, Dong Y, Zhao J,
Liang Q, Zhang L, Pan Y, Yang W, Pang JC, et al: Targeting of YAP1
by microRNA-15a and microRNA-16-1 exerts tumor suppressor function
in gastric adenocarcinoma. Mol Cancer. 14(52)2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wu J, Wang Y, Shang L, Qi L and Song M:
Five common functional polymorphisms in microRNAs and
susceptibility to breast cancer: An updated meta-analysis. Genet
Test Mol Biomarkers. 22:350–358. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sandiford OA, Moore CA, Du J, Boulad M,
Gergues M, Eltouky H and Rameshwar P: Human Aging and Cancer: Role
of miRNA in Tumor Microenvironment. Adv Exp Med Biol. 1056:137–152.
2018.PubMed/NCBI View Article : Google Scholar
|