Introduction
Fibromyalgia (FM) is one of the most frequent
musculoskeletal disorder and perhaps the most enigmatic one
(1). FM is the third most common
rheumatic disorder after low back pain and osteoarthritis (2). United States findings suggest a
primary care prevalence of 3.4% whereas a European Community study
estimated an overall prevalence of 4.7% (3). The most effective approach for the
treatment of FM depends on the efficient management of
pharmacological treatment combined with cognitive-behavioral
therapy, physical exercise and occupational therapy (4). The combination of these four therapies
has been shown to improve the efficacy of the treatment and to
reduce the global impact of FM on the patient, improving the
quality of life and the capacity to participate in the activities
of daily living (5).
Cognitive-behavioral therapy (CBT) is a form of psychotherapy that
was developed in the mid to late 20th century. It is the most
efficient form of psychological intervention for the treatment of
anxiety and depression, chronic pain, inflammatory pain and FM with
all its associated symptoms (6).
A recent review synthesized the short- and long-term
effects of different psychological interventions on FM and showed
significant improvements in the perception of pain, sleeping
problems, depression and grievous thoughts, besides the benefits on
functional status (7). However, it
has been demonstrated that instructions alone are more effective
when combined with cognitive-behavioral therapy regarding sleep
quality, evaluated by both subjective and objective parameters
(8). In addition, it has been shown
that cognitive-behavioral therapy can be a tool in the management
of sleep dysfunction in adults as well as children with FM
(9). The positive results are also
achieved in other aspects of behavior such as attention disturbance
and daily functioning (10,11). Coming to support all these facts,
the 2008 EULAR recommendations also suggested the beneficial
results of cognitive-behavioral therapy on function and pain
(12).
The importance of physical exercise in the FM
syndrome has been observed for decades. The fact that there are no
pharmacological treatments with undoubted efficacy has led to the
appearance of other types of therapy such as kinetic therapy, among
others. The type of exercise program to influence the majority of
FM symptoms (pain, fatigue, physical function, global health,
depression) in a positive way is aerobic exercise, but the one to
have the best results in improving complaints is strength exercise
(13,14).
The aim of the present study was to monitor patient
response to several types of therapy including cognitive-behavioral
and occupational therapy, kinetic therapy, as compared to a control
group that was not subjected to any form of therapy.
Materials and methods
Ethics statement
This study was approved by the Academic and
Scientific Ethics and Deontology Committee of the University of
Medicine and Pharmacy in Craiova (Registration no. 23/2015) in
accordance with the European Union Guidelines (Declaration of
Helsinki). All the patients signed an information and acceptance
form, i.e., informed consent, to be included in the present
study.
Participants
The objective of our prospective study was to
evaluate the effects of a multidisciplinary interventional program
on disease impact for fibromyalgic patients. The population sample
included three groups of patients, all of them women that had been
previously diagnosed with FM. Two of the groups were subjected to
an interventional program, while the third group participated as a
control sample. One of the interventional groups was subjected to a
program including CBT and occupational therapy (OT), another one
was involved in a kinetic program (KT) including aerobic exercise,
postural hygiene exercise, stretching and Pilates.
We conducted a randomized, longitudinal, controlled
trial on 98 FM patients, all women over 5 years, between March,
2015 and December, 2019. The participants were selected from the
Rehabilitation and Physical Medicine Department of the County
Emergency Hospital of Craiova, Romania. The inclusion criteria that
allowed the patients to participate in this study (both in the
interventional as well as in the control groups) were: Women over
the age of 18 years, a confirmed diagnosis of FM according to the
2010 ACR Preliminary Diagnostic Criteria (2), patients monitored and treated by a
physician for the chronic pain problem, regardless of the
pharmacological treatment the patient is undergoing.
The exclusion criteria that disabled the patients
from participating in this study were: Uncooperative patients,
alcoholism, severe psychiatric disorders, associated conditions
that may otherwise explain the evolution of the symptoms and
patients with severe associated conditions or traumatic injuries
that disabled them from performing a physical exercise program.
Materials and measures
From the total number of 40 patients included in the
cognitive behavioral plus occupational therapy program (CBT+OT)
arm, only 32 attended all evaluations and at least 70% of the
program sessions. The patients with poor compliance to the
treatment were excluded from the statistical analysis. In the group
that underwent kinetic therapy (KT), of all the invited patients,
42 had initially accepted to participate. However, 34 patients were
included in the database (for the complete and correct
participation of all evaluations and for attending at least 70% of
the program sessions). In the control group (Controls), 42
initially accepted to take part in the program even though in the
end 32 participants were included in the data base (for the
complete and correct participation to all evaluations). Therefore,
the total population of this study included 98 FM patients, all
women, out of which 32 received cognitive-behavioral therapy and
occupational therapy, 34 kinetic therapy, and 32 participated as
controls.
Mean age was 52.4 (SD, 7.2) years for
cognitive-behavioral therapy and occupational therapy group. In
kinetic therapy group the mean age was 55.3 (SD 7.2), and in
controls group the mean age was 56.3 (SD 8.8) with small
differences between the groups (P<0.05). The socio-demographic
data for each group is presented in Table I, no significant differences between
groups being observed. As far as the clinical data are concerned,
the patients reported the onset of pain, on average, 9 years before
the diagnoses of FM were set. Notable differences between the
groups were also registered concerning the comorbidities. The most
common associated condition was anxiety or depression registered by
92.8% of participants in CBT+OT, followed by chronic fatigue
syndrome (74%) and tension headaches with an average of 73%, as
shown in Table I.
 | Table IClinical diagnosis data. |
Table I
Clinical diagnosis data.
| Socio-demographic
data Clinical data | CBT+OT (n=32) | Kinetic therapy
(n=34) | Controls (n=32) |
|---|
| Age: mean ± SD | 52.4 (7.2) | 55.3 (7.2) | 56.3 (8.8) |
| Year of diagnosis:
Mean ± SD | 2001.3 (7.5) | 2009.3(2) | 2003.6 (4.6) |
| Year of pain onset:
Mean ± SD | 1995.7 (9.7) | 2000.8 (7.3) | 1990.7 (11.6) |
| Irritable bowel
syndrome (%) | 53.5 | 23.5 | 29 |
| Chronic fatigue
syndrome (%) | 74 | 20.6 | 63.3 |
| Tension headaches
(%) | 73 | 52.9 | 77.4 |
| Endocrine disorders
(%) | 44.8 | 41.2 | 25.8 |
| Rheumatic disorders
(%) | 59.2 | 2.9 | 64.5 |
| Anxiety or depression
(%) | 92.8 | 52.9 | 83.8 |
| Other associated
conditions (%) | 45.4 | 55.8 | 45.4 |
For the individuals that underwent CBT+OT or KT, the
patients that had agreed to participate were telephonically
summoned to a first introductory meeting. The objectives and
development of the study were explained, stating the fact that
their participation was completely voluntary and that they could
abandon the program at any time they wanted to. Once they had
agreed to participate, they were asked to sign an informed consent
form. They also had to fill in an evaluation protocol (Pre). From
that moment on, the subjects attended 12 sessions (one session a
week) in groups of maximum 10-12 patients. The duration of each
session was 2 h for the individual subjected to
cognitive-behavioral plus occupational therapy.
The kinetic sample was divided into 3 groups of
maximum 10-12 patients. The kinetic therapy intervention included
four types of sessions: Aerobic exercise and balance, postural
hygiene, stretching and pilates. Patients attended one session per
week at the gym and were recommended to try to perform the
exercises at home two more times a week, if their physical status
allowed it. Each session initially lasted ~20 min, slowly
increasing in duration and intensity, reaching a maximum duration
of 1 h. Each session began with warm-up and included exercises for
the central axis of the body, as well as for the upper and lower
limbs. Some of the sessions ended with cycloergometer work-out
while others ended with breathing and relaxation exercises. Most
exercises were presented with one or two alternatives, depending on
each patient's physical condition.
Once the program ended, all the participants were
asked to fill in the same evaluation protocol (Post) and were
summoned 4 months later for follow-up monitoring (Follow-up). The
Evaluation Protocol was comprised of two questionnaires developed
in order to assess the patient's condition as fully as possible. It
contained the following: Fibromyalgia Impact Questionnaire (FIQ)
with 10 items referring to the patient's status over the last week
and Fibro Fatigue (FF) scale.
FF is a scale designed to evaluate the changes in
the development and severity of FM and Chronic Fatigue Syndrome
(15). It contains 14 items
regarding pain, muscle tension, fatigue, concentration
difficulties, memory loss, irritability, sadness, sleep problems,
vegetative disorders, irritable bowl, headache, infection, sexual
activity and family life. Each item was rated on a scale of 0 (no
problem) to 6 (incapacity). The higher the score, the more severe
the FM symptoms. The first item (FIQ1-functional impairment)
contained 10 questions that asked the subject how often he was able
to perform household chores and daily activities such as shopping,
vacuuming, cooking, making the beds, washing the dishes, visiting
friends, driving. The answers were rated from 0 (always) to 4
(never). The second and third item asked the number of days during
the last week that the patient had felt well and, respectively, the
number of days the individual could not work owing to FM. For the
last 7 items the patient was asked to assess on a scale from 1
(absent) to 10 (very intense); the level of pain, fatigue,
stiffness, anxiety, depression as well as how tired the individual
felt in the morning or how the FM symptoms affected ability to
work.
Statistical analysis
The Statistical Package for Social Sciences (SPSS)
version 20 (IBM Corporation) was used in order to analyze the
database. Before processing the data, we first verified the
premises of normality and homocedasticity given the fact that the
samples were superior to the limit of 30 subjects. For the
normality part we used the Kolmogorov-Smirnov test whose null
hypothesis claims normality. It was rejected if the significance
was ≤0.05.
Results
FIQ total score
For the sample involved in cognitive-behavioral
therapy and occupational therapy the only significant difference
was between the first and second evaluation (P<0.05). The scores
from the group subjected to kinetic therapy registered a
significant decrease from the initial evaluation to the
post-evaluation (P<0.005) and follow-up (P<0.005). For the
control sample, there was a significant difference noted between
the pre- and follow-up evaluations (P<0.05). The means and
standard deviations obtained by computing the FIQ total score, in
all three groups at all evaluation moments, are presented in
Table II.
 | Table IITotal FIQ scores. |
Table II
Total FIQ scores.
| Group | FIQ total Pre | FIQ total Post | FIQ total
follow-up |
|---|
| CBT+OT mean ± SD | 71 (15.9) | 62.6 (20.2) | 68.6 (15.7) |
| KT mean ± SD | 69.4 (16.1) | 50.8 (17.6) | 52.8 (17.9) |
| Controls mean ±
SD | 74.3 (11.5) | 70.7 (15.9) | 68.9 (17.5) |
At the pre-evaluation there were no significant
inter-group differences. At post-evaluation significant differences
were observed between the control sample and the group subjected to
kinetic therapy (P<0.05). FIQ scores decreased in the CBT+OT
group too, but less than that in the KT group.
At the follow-up, the FIQ scores in CBT+OT group
returned to values close to the initial ones, without a
statistically significant difference between the CBT and control
groups (P<0.05). FIQ values in KT group remain significantly
lower than the control group values, without statistical
significance.
Fibro fatigue scale
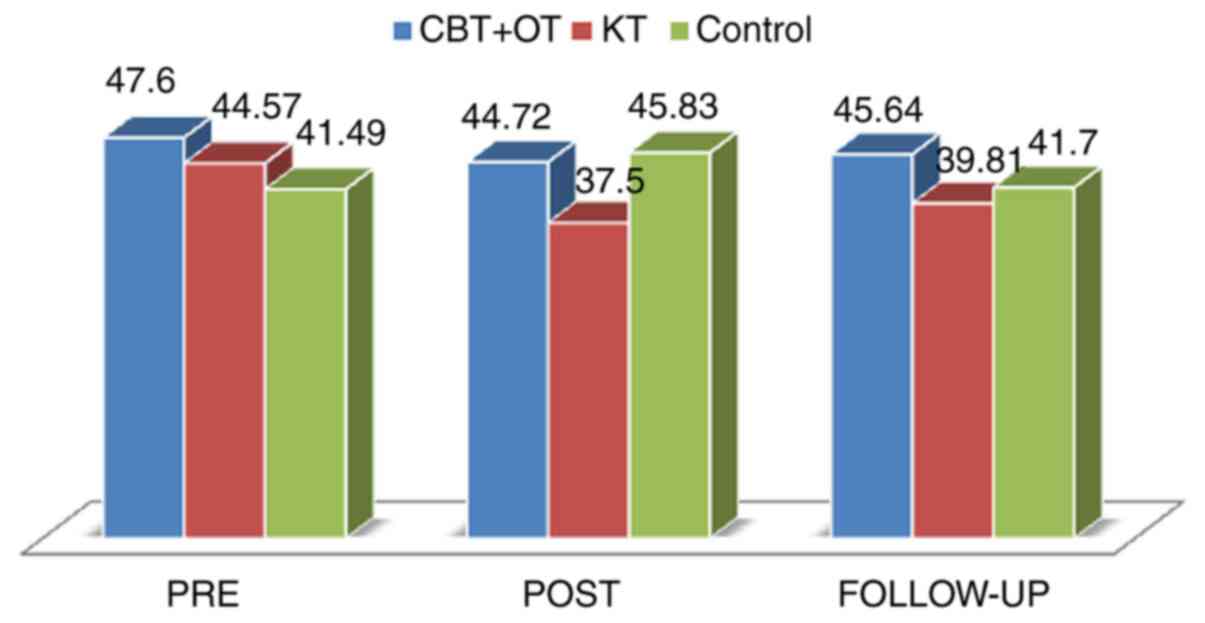
The Fibro Fatigue (FF) scale registered notable
evolutions in time for the group subjected to kinetic therapy. The
initial score (mean=44.57) suffered a decrease until the
post-evaluation (mean=37.5, P<0.05), which then slowly started
to increase up to follow-up (mean=39.81). The most important scores
of the Fibro Fatigue scale are shown in Fig. 1.
Between groups, significant statistical differences
were observed for the pair: Group subjected to kinetic
therapy-control sample (P<0.05 at Pre, P<0.005 at Post,
P<0.01 at follow-up) and the pair of groups involved either in
kinetic therapy or in cognitive-behavioral plus occupational
therapy (P<0.05 at Pre, P<0.005 at Post and P<0.005 at
Follow-up).
Discussion
The two major non-pharmacologic techniques that are
constantly used in the treatment of FM are cognitive-behavioral
therapy and physical exercise. Cognitive-behavioral therapy has
been used in the management of chronic pain for more than 20 years.
It is implemented as a semi-instructive, short-term psychotherapy
where the patient plays an active role in assisting the therapist
(6). Cognitive-behavioral therapy
can help reduce pain, fatigue, improve emotional well-being, lift
the spirit and perhaps enhance physical and social functioning
(6).
By comparing cognitive-behavioral therapy with
kinetic therapy, we hoped to shed some light on the benefits of
each one and on the areas for which each of them is best suited.
Cognitive-behavioral therapy techniques, by offering short-term
goal-oriented psychotherapy, emphasize changes in thought patterns
and behaviors rather than providing deep insight (16). Among their benefits, when compared
to other forms of psychological intervention, we can mention the
facts that the positive effects of cognitive-behavioral therapy can
be reached in as many as 10-20 sessions and that it can be
performed in groups (16). As for
occupational therapy, it represents a rather new area of interest
for FM, given the level of disruption to the employment status of
such patients including reduced working hours, becoming disabled or
taking early retirement (17-19).
To the best of our knowledge, there are no data published
concerning occupational therapy as a unique intervention in FM,
except in combination with other forms of therapy. We chose to
incorporate this type of therapy together with cognitive-behavioral
therapy in order to address one of the significant aspects of the
important economic burden that FM causes, that of the impact on
work. An aspect worth mentioning is the reality that in the case of
interdisciplinary interventions, as was the cognitive-behavioral
therapy and occupational therapy, it is practically impossible to
determine the input of each component separately.
Supervised exercise programs have been demonstrated
to reduce the severity of FM symptoms and successfully improve the
level of pain, functional status and quality of life (20). There is no other mention in
literature, except for a previous study (21), of a mixed program that includes
besides the three major types of exercise, balance exercises and
Pilates. Balance problems, regardless of their cause (increased
age, side effects to medication, reduced muscle strength, impaired
cognition), have been widely reported by FM patients (45% of a
large 2,596 persons survey) (22).
This fact was the basis for introducing balance exercises in the
kinetic program. Moreover, Pilates programs are known to combine
physical, psychological, spiritual and behavioral elements that may
be especially beneficial for subjects with FM (23). These patients present a wide variety
of physical and emotional complaints. We considered that a
combination between conventional exercise training and this
oriental holistic mind and body approach would help make the
interventional program a more appealing one and at the same time it
would offer more consistency in influencing as many FM symptoms as
possible.
Since drop-out rates are significant for FM
patients, ranging from 10% for the untreated control groups to 22%
for the patients involved in physical exercise programs (24), adherence to the interventional
program was one of our major concerns. However, in the present
study, a total of 80% of the initial participants managed to
complete the cognitive-behavioral plus occupational therapy program
and 81%, the kinetic therapy program. The highest drop-out rate was
registered for the control group, 24% of the initially interested
patients having abandoned the study. However, we included in the
analysis only those patients who participated in a certain
percentage of the intervention sessions.
The preservation of the therapy benefits in the long
term as a lasting improved quality of life is one of the main
concerns in treating FM. The disease perception monitored with the
help of the FIQ in the CB and OT group was considerably lower,
possibly due to the direct action of intervention in daily
activities and improving responsibilities. The reality that most of
the improvements registered by the group subjected to
cognitive-behavioral therapy and occupational therapy were still
significant four months after the conclusion of the intervention is
an indicator of the fact that the patients had properly acquired an
important part of the techniques they were supposed to learn and
included them in their own life style.
In the kinetic group, the benefits to each symptom
in particular led to a reduction in the scores of the FIQ and the
FF scale. Moreover, the significant improvement in pain and other
symptoms resulted in lower medication consumption and thus, reduced
medical costs necessary in order to treat the disease. At follow-up
evaluation very significant improvements were still maintained for
the FIQ score and medication intake, but smaller ones for the
FF.
The scores of the parameters vary between different
investigations, as well as between different countries. For
instance, the FIQ total score was on average 54.8 in a French study
(20), 55.8 in a Canadian sample
(25), 68 in a Mexican FM
population (26) and 70.8 in a
Turkish investigation (27). In the
present study, the FIQ average score, prior to commencing the
program was 65.9.
All of our patients were women. Even if recent
studies identified differences by sex in clinical features and
modes of treatment (28,29), little is known about differences in
outcomes by sex for the same modes and intensities of treatment and
which treatment modes best benefit males or females with
fibromyalgia.
The results clearly of the present study showed the
superiority of kinetic therapy even if benefits were also obtained
by cognitive-behavioral plus occupational therapy. Based on the
experience of this study, we can offer some suggestions as
perspectives for future research. In order to control and improve
most of the FM symptoms, besides proper medication, we propose an
interdisciplinary intervention mainly focusing on long-term
individualized kinetic therapy that is initially performed under
the close supervision of specialized professionals and subsequently
continued at home. The simultaneous integration of a
cognitive-behavioral and occupational therapy intervention, which
mainly targets the neglected psychological and labor aspects of
this condition, could be the element that completes the complex
treatment of FM patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SP, VP, FD, RP and DM were involved in the
conception of the study and data analysis; SP, DD, VP, RP and DR
contributed to data curation;, SP, VP, DR and DM were involved in
the writing process; VP, FD, RP, DM and SP performed literature
data review; and SP and VP reviewed the final manuscript All
authors have read and agreed to the published version of the
manuscript.
Ethics approval and consent to
participate
This study was approved by the Academic and
Scientific Ethics and Deontology Committee of the University of
Medicine and Pharmacy in Craiova (registration no. 23/2015) in
accordance with the European Union Guidelines (Declaration of
Helsinki). Written informed consent was obtained for patient
participation.
Patients consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Clauw DJ: Fibromyalgia: A clinical review.
JAMA. 311:1547–1555. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jones GT, Atzeni F, Beasley M, Flüß E,
Sarzi-Puttini P and Macfarlane GJ: The prevalence of fibromyalgia
in the general population: A comparison of the American College of
Rheumatology 1990,. 2010, and modified 2010 classification
criteria. Arthritis Rheumatol. 67:568–575. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Glennon P: Fibromyalgia syndrome. Oxford
University Press InnovAIT. 4:332–337. 2011.
|
|
4
|
Bernardy K, Fuber N, Kollner V and Hauser
W: Efficacy of cognitive-behavioral therapies in fibromyalgia
syndrome-a systematic review and metaanalysis of randomized
controlled trials. J Rheumatol. 37:1991–2005. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lee JW, Lee KE, Park DJ, Kim SH, Nah SS,
Lee JH, Kim SK, Lee YA, Hong SJ, Kim HS, et al: Determinants of
quality of life in patients with fibromyalgia: A structural
equation modeling approach. PLoS One. 12(e0171186)2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Luciano JV, D'Amico F, Cerdà-Lafont M,
Peñarrubia-María MT, Knapp M, Cuesta-Vargas AI, Serrano-Blanco A
and García-Campayo J: Cost-utility of cognitive behavioral therapy
versus U.S. Food and Drug Administration recommended drugs and
usual care in the treatment of patients with fibromyalgia: An
economic evaluation alongside a 6-month randomized controlled
trial. Arthritis Res Ther. 16(451)2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Glombiewski JA, Sawyer AT, Gutermann J,
Koening K, Rief W and Hofmann SG: Psychological treatments for
fibromyalgia: A meta-analysis. Pain. 151:280–295. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tang NKY: Cognitive behavioural therapy in
pain and psychological disorders: Towards a hybrid future. Prog
Neuropsychopharmacol Biol Psychiatry. 87:281–289. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Roizenblatt S, Neto NS and Tufik S: Sleep
disorders and Fibromyalgia. Curr Pain Headache Rep. 15:347–357.
2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Miro E, Lupianez J, Martinez MP, Sanchez
AI, Diaz-Piedra C, Guzman MA and Buela-Casal G:
Cognitive-behavioral therapy for insomnia improves attentional
function in fibromyalgia syndrome: A pilot, randomized controlled
trial. J Health Psychol. 16:770–782. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Popa SL, Leucuta DC and Dumitrascu DL:
Pressure management as an occupational stress risk factor in
irritable bowel syndrome: A cross-sectional study. Medicine
(Baltimore). 97(e13562)2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Macfarlane GJ, Kronisch C, Dean LE, Atzeni
F, Häuser W, Fluß E, Choy E, Kosek E, Amris K, Branco J, et al:
EULAR revised recommendations for the management of fibromyalgia.
Ann Rheum Dis. 76:318–328. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Busch AJ, Webber SC, Richards RS, Bidonde
J, Schachter CL, Schafer LA, Danyliw A, Sawant A, Dal Bello-Haas V,
Rader T and Overend TJ: Resistance exercise training for
fibromyalgia. Cochrane Database Syst Rev.
12(CD010884)2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bidonde J, Busch AJ, Webber SC, Schachter
CL, Danyliw A, Overend TJ, Richards RS and Rader T: Aquatic
exercise training for fibromyalgia. Cochrane Database Syst Rev.
10(CD011336)2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
García-Campayo J, Pascual A, Alda M, Marzo
J, Magallón R and Fortes S: The Spanish version of the FibroFatigue
Scale: Validation of a questionnaire for the observer's assessment
of fibromialgia and chronic fatigue syndrome. Gen Hosp Psychiatry.
28:154–160. 2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Bernardy K, Klose P, Busch AJ, Choy EH and
Häuser W: Cognitive behavioural therapies for fibromyalgia.
Cochrane Database Syst Rev. 2013(CD009796)2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Schaefer C, Chandran A, Hufstader M, Baik
R, McNett M, Goldenberg D, Gerwin R and Zlateva G: The comparative
burden of mild, moderate and severe Fibromyalgia: Results from a
cross-sectional survey in the United States. Health Qual Life
Outcomes. 9(71)2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Perrot S, Schaefer C, Knight T, Hufstader
M, Chandran AB and Zlateva G: Societal and individual burden of
illness among fibromyalgia patients in France: Association between
disease severity and OMERACT core domains. BMC Musculoskelet
Disord. 13(22)2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mihailovici AR, Padureanu V, Albu CV,
Dinescu VC, Pirlog MC, Dinescu SN, Malin RD and Calborean V:
Myocardial Noncompaction. Rev Chim (Bucharest). 69:2209–2212.
2018.
|
|
20
|
Assumpção A, Matsutani LA, Yuan SL, Santo
AS, Sauer J, Mango P and Marques AP: Muscle stretching exercises
and resistance training in fibromyalgia: Which is better? A
three-arm randomized controlled trial. Eur J Phys Rehabil Med.
54:663–670. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Drăgoi D, Trăistaru R, Roşulescu E,
Vasilescu M, Matei D and Popescu R: A 12-week physical training
program-effects on fibromyalgia patients. Medicina Sportiva.
8:1769–1774. 2012.
|
|
22
|
Jones KD, King LA, Mist SD, Bennett RM and
Horak FB: Postural control deficits in people with fibromyalgia: A
pilot study. Arthritis Res Ther. 13(R127)2011.PubMed/NCBI View
Article : Google Scholar
|
|
23
|
Busch AJ, Webber SC, Brachaniec M, Bidonde
J, Bello-Haas VD, Danyliw AD, Overend TJ, Richards RS, Sawant A and
Schachter CL: Exercise therapy for fibromyalgia. Curr Pain Headache
Rep. 15:358–367. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Busch AJ, Overend TJ and Schachter CL:
Fibromyalgia treatment: The role of exercise and physical activity.
Int J Clin Rheumtol. 4:343–380. 2009.
|
|
25
|
Ferrari R: A cohort-controlled trial of
the addition of customized foot orthotics to standard care in
fibromyalgia. Clin Rheumatol. 31:1041–1045. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Vargas-Alarcon G, Alvarez-Leon E, Fragoso
JM, Vargas A, Martinez A, Vallejo M and Martinez-Lavin M: A SCN9A
gene-encoded dorsal root ganglia sodium channel polymorphism
associated with severe fibromyalgia. BMC Musculoskelet Disord.
13(23)2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Akkaya N, Akkaya S, Atalay NS, Balci CS
and Sahin F: Relationship between the body image and level of pain,
functional status, severity of depression and quality of life in
patients with fibromyalgia syndrome. Clin Rheumatol. 31:983–988.
2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hauser W, Kuhn-Becker H, von Wilmoswky H,
Settan M, Brähler E and Petzke F: Demographic and clinical features
of patients with fibromyalgia syndrome of different settings: A
gender comparison. Gend Med. 8:116–125. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Castro-Sanchez AM, Mataran-Penarrocha GA,
Lopez-Rodriguez MM, Lara-Palomo IC, Arendt-Nielsen L and
Fernández-de-las-Peñas C: Gender differences in pain severity,
disability, depression, and widespread pressure pain sensitivity in
patients with fibromyalgia syndrome without comorbid conditions.
Pain Med. 13:1639–1647. 2012.PubMed/NCBI View Article : Google Scholar
|