Introduction
Migraines are a common post-surgical and puerperal
complaint, consistent with a myriad of etiologies, encompassing
physiological changes, hormonal modifications, peri-surgical
procedures and unknown prenatal conditions. The primary causes
include tension-type headaches, cluster headaches and other
trigeminal nerve cephalgia (1,2).
Secondary headaches are are less common but can have severe
consequences with significant mortality and morbidity if they are
overlooked. Diagnosis of a secondary cause is a daunting task,
taking into account that headache can be the only symptom of
multiple conditions such as postdural puncture headache (PDPH),
pneumocephalus, preeclampsia and eclampsia, meningitis, cerebral
venous thrombosis, ischemic or hemorrhagic stroke, subarachnoid
haemorrhage, reversible cerebral vasoconstriction syndromes,
posterior reversible leukoencephalopathy syndrome and pituitary
adenoma. Therefore, a high index of suspicion is required, and a
low threshold for a neuroimaging investigation when dealing with
postpartum headaches is needed (3,4).
Needless to say, any suspicion of a secondary headache should be
investigated by a multidisciplinary team due to the challenges
posed by such wide-ranging conditions. Although pituitary adenoma
is seldom a differential diagnosis in pregnancy and postpartum
headache, it is part of a differential diagnosis when associated
with visual loss. Ocular visual impairment is the next common
symptom in pituitary adenoma after headache. We present the case of
postpartum pituitary apoplexy, following an emergency Caesarean
section.
Case report
After obtaining approval of the Ethics Committee of
the National Institute of Mother and Child Care (Bucharest,
Romania) (no. 25/2019), data of the patient were reviewed and
presented in the current case report. A 26-year-old primigravida,
40 weeks gestation, was admitted to our maternity ward at the
National Institute of Mother and Child Care, in spontaneous labour.
She delivered a 3,150 g female baby, Apgar score 9, through
Category II Caesarean section for failure to progress. The
anaesthetist performed spinal anaesthesia with bupivacaine and
fentanyl. Caesarean section was routine and pain-free, with an
estimated blood loss of approximately 400 ml. Pre-delivery
haemoglobin was 11.5 g/dl and at post-delivery the value was
slightly decreased at 10.2 g/dl. She had no prior medical history,
and her antenatal care was uneventful. The immediate postpartum
period was unremarkable. The patient remained alert and orientated
with normal vital signs. The following day she was transferred to
the postnatal ward. Approximatively 48 h post-delivery she
presented frontal and temporal throbbing headaches, nausea, and
photophobia, but no nuchal rigidity or backache. On examination,
she presented left ptosis, anisocoria, incomplete 3rd cranial nerve
paresis and normal fundoscopy. Vital signs were: temperature,
38˚C; blood pressure, 135/75 mmHg; heart rate, 68 beats
per minute; and significant polyuria (3.9 cc/kg/h). An urgent
neurological exam followed by an endocrinological appointment was
required and indicated no signs of meningeal irritation or
neurological deficiency. Consistent with her clinical examination,
polyuria and polydipsia, pituitary apoplexy was a presumptive
diagnosis and a magnetic resonance imaging (MRI) examination was
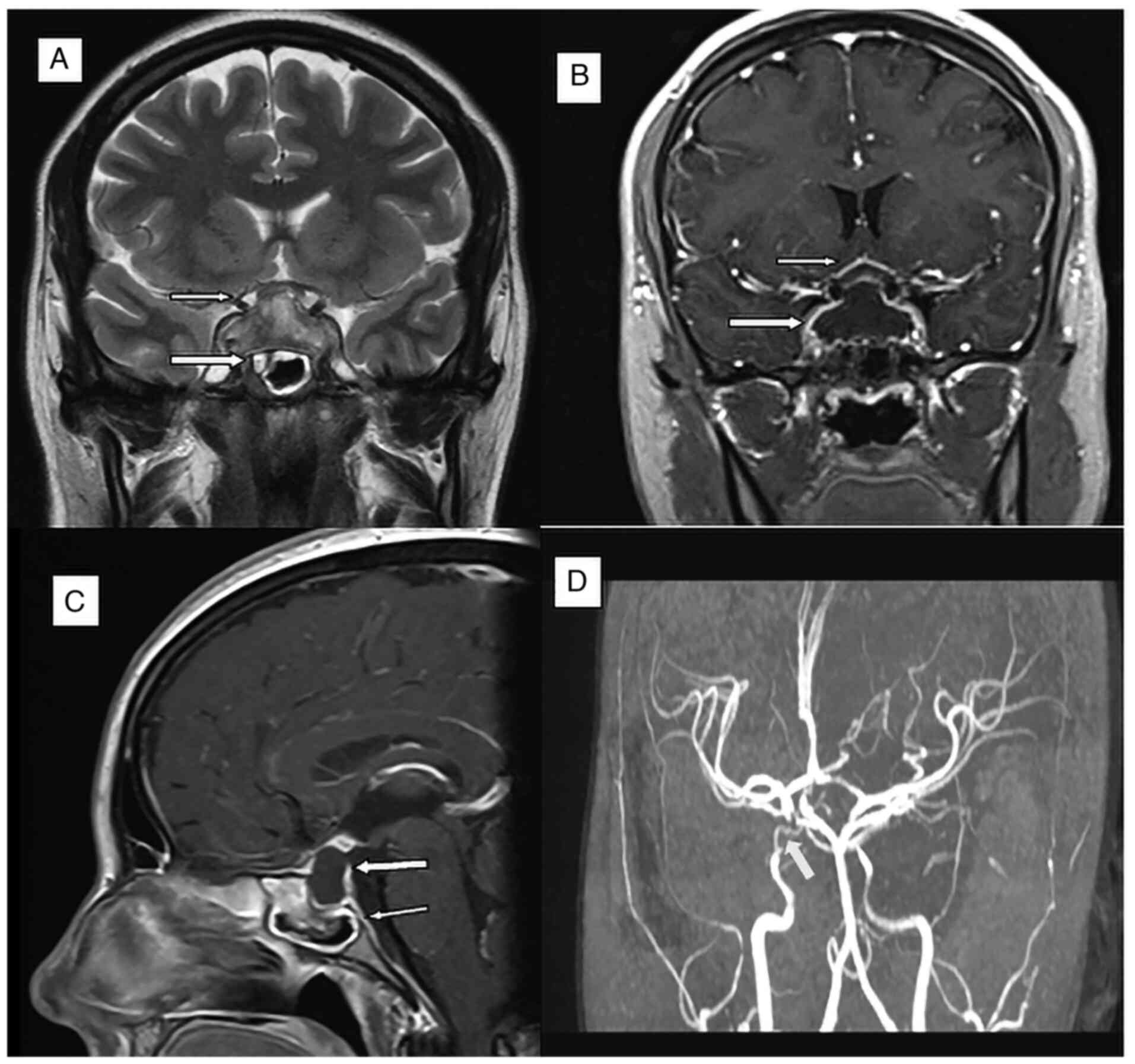
performed. Head MRI showed a cystic pituitary tumour with a 33 mm
transverse diameter, 10.5 mm anteroposterior, 15.5 mm craniocaudal.
The tumour was bulging bilaterally in the cavernous sinus (into the
sella turcica), encasing partially the right carotid artery. The
tumour was in contact with the optic chiasm without signs of
displacement or compression. The MRI diagnosis was of a pituitary
macroadenoma, possible Rathcke cleft cyst (Fig. 1). Electrolytic and endocrinological
tests were carried out, the results being displayed in Table I (day 4 post-delivery, 8 a.m.)
showing hypopituitarism involving corticotrophin, lactotrophic and
thyrotropin dysfunction with hyponatremia and hypochloremia.
 | Table IElectrolytic and endocrinological
blood test results of the patients with pituitary apoplexy. |
Table I
Electrolytic and endocrinological
blood test results of the patients with pituitary apoplexy.
| Parameter | Value | Normal range |
|---|
| Cortisol | 43.1 nmol/l | 123-626 |
| Adrenocorticotropic
hormone (ACTH) | 25.14 | 7.0-63 |
| Prolactine | 162 nmol/l | 64-395 |
| Thyroid-stimulating
hormone (TSH) | 0.211 mIU/l | 0.46-4.68 |
| T3 | 1.19 nmol/l | 1.49-2.60 |
| Free T4 | 8.57 pmol/l | 10.0-28.2 |
| Cl | 92.00 | 97-108 |
| K | 4.4 mmol/l | 3.5-5.1 |
| Na | 122 mmol/l | 136-145 |
| Serum osmolality
(mOs/kg) | 269.9 | 280-300 |
Treatment with intravenous dexamethasone, thyroxin
50 µg, fluid and electrolyte replacement was initiated immediately.
On the following day, a multidisciplinary meeting took place with
obstetricians, anaesthesiologists, endocrinologists, neurologists
and neurosurgeons in order to define a postpartum management plan.
Initially, conservative management was started but as her condition
worsened with a deteriorating level of conciseness, treatment was
converted to surgical decompression. Endoscopic transsphenoidal
pituitary surgery was performed to remove the 3x2x1 cm encapsulated
tumour. Histopathology result showed a non-functional pituitary
macroadenoma. Post-surgical clinical examination revealed normal
neurological condition while the oculomotor paresis was wholly
resolved. Two years after surgery, the patient is well under
hormone replacement therapy. Currently, she is receiving oral
medication, prednisolone 50 µg/day, thyroxine 75 µg and
cycloprogynova (estradiol, norgestrel).
Discussion
Pituitary adenomas represent approximatively 10-15%
of all intracranial tumours. Microadenomas are tumours of less than
10 mm while macroadenomas include tumours larger than 10 mm. Giant
adenomas are more than 40 mm in size. Between 14 and 54% are
non-functional adenomas while the rest secrete excess hormones:
8-12% growth hormones, 2-6% release adrenocorticotropic hormone and
less than 1% secrete thyrotropin (1-6).
Despite solid research regarding pituitary adenoma, the
pathogenesis remains unknown (5,6).
Because of the associated hypertrophy of lactotrophic cells and the
increase in normal pituitary volume, pregnancy is also considered a
risk factor for pituitary apoplexy (7). Hereditary transmission is responsible
for less than 5% of the cases (8).
The pituitary gland also represents a location for metastatic
deposits in 0.1-0.2% of cases, the most common primary tumours
being represented by lung and breast (9-11).
Pituitary apoplexy is a rare endocrinological emergency, which can
occur without any eliciting factors. Nevertheless, in most cases,
there are known risk factors such as major surgery, hypertension,
coagulopathies or postpartum haemorrhage (Sheehan syndrome).
Sheehan syndrome is the most common reason of postpartum pituitary
insufficiency, which is caused by a massive blood loss during
delivery or during the early postpartum period. Whenever Sheehan
syndrome is suspected, two conditions should be part of the
differential diagnosis, postpartum necrosis of a preexisting
hypophyseal tumor and lymphocytic hypophysitis.
Diagnosis of postpartum apoplexy is a challenging
one as many patients do not have any pituitary history. The most
commonly encountered symptom is headache, which is frequently
associated with various pathological conditions. Alongside
headache, blurred vision, diplopia, photophobia, or bitemporal
hemianopsiavision loss have all been reported in pituitary adenoma.
Symptomatology in cases of known adenoma is due to a sharp increase
in size, which is an estrogen-driven one (9). This will raise intrasellar pressure
causing compression and necrosis of the pituitary gland with
subsequent pituitary insufficiency. Increased intracranial pressure
leads to neurologic symptoms such as nausea and vomiting. Quite
often, patients can lose their consciousness or have at least a
mild degree of lethargy (10). The
clinical picture can mimic multiple neurological conditions, and
this is why a high index of suspicion should prompt investigation
for pituitary apoplexy.
When it comes to the laboratory tests which are
required in order to provide a positive diagnosis, it should be
emphasized that pregnancy is a condition presenting with hormonal
imbalance making interpretation of endocrine and dynamic tests more
difficult. Increased levels of prolactin are normal during
pregnancy, although low levels of prolactin can suggest pituitary
insufficiency (11). Patients with
pituitary apoplexy and low prolactin levels are the most affected
and it is unlikely that they will have a successful post-surgical
recovery (12). Adrenocorticotropic
hormone (ACTH) deficiency is commonly present in pituitary
apoplexy, but thyroid-stimulating hormone (TSH), growth hormone
(GH), and gonadotropin deficiency have also been reported. Adrenal
insufficiency is the most serious complication as it is
life-threatening (10).
Hyponatremia complicates pituitary apoplexy as it is a sign of
adrenal insufficiency or of the syndrome of inappropriate
antidiuretic hormone (ADH) secretion (13). Therefore, whenever pituitary
apoplexy is part of a working diagnosis, a full endocrine
(cortisol, ACTH, prolactine, follicle-stimulating hormone,
luteinizing hormone, insulin-like growth factor 1, free T4, TSH)
and blood assessment (full blood count, glycemia, electrolytes
(serum sodium and potassium), and renal and liver function) should
be performed urgently.
The gold standard for pituitary apoplexy diagnosis
is MRI as it confirms the diagnosis in over 90% of cases. On
T1-weighed images, haemorrhage typically manifests with
hyperintensity related with the rest of the brain (14). MRI and MR angiogram techniques also
help to differentiate an aneurism from pituitary apoplexy. MRI is
safe during pregnancy, and to date no damaging fetal effects have
been reported. MRI is the investigation of choice compared with any
other ionising technique. The majority of radiologist avoid using
gandolinum in pregnancy as it crosses the placenta, enters fetal
circulation, is eliminated by kidneys and secreted in amniotic
fluid. To date, no deleterious effects have been reported regarding
using gandolinum in pregnancy (15).
Based on the review of the literature [Table II (4,7,10,13,16-50)],
we found 48 cases of pregnancy-related pituitary tumour apoplexy.
Statistical analysis of the gestational age at diagnosis showed an
average value of 27.9 weeks (range 10-39 weeks) with the caveat
that three of these cases, including ours, occurred during the
postpartum period. Extremely rare, pituitary apoplexy can occur
even in the first trimester as reported by Janssen et al at
10 weeks of gestation (16).
Prolactinoma (21 cases) was the most common tumor encountered and
in many occasions in patients who were under treatment. This is in
line with published literature where prolactinoma is present in
approximately 50% of all cases (17). There were 17 cases of non-secreting
adenoma, 2 cases of GH-oma, 3 cases of hypophysitis, one case of
Neslon syndrome, one case of enlarged pituitary gland, one case of
pituitary apoplexy followed by reversible cerebral vasoconstrictive
syndrome and one case of normal size pituitary gland but with a
histopathological diagnosis of adenoma post-surgery (Table II). In many hospitals, current
practice is to halt cabergoline/bromocriptine, although there is no
robust evidence for this decision (17). Onset of symptoms in a patient with a
known adenoma should trigger imagistic investigations that will
clarify if this is a case of progressive adenoma or a different
aetiology. A real challenge is the diagnosis of pituitary apoplexy
in patients with unknow adenomas. Precious time can be lost by
interpreting a headache as a migraine type. There are several
cases, including ours, where pituitary apoplexy was the main cause
(9,10,18,19,51).
Migraine is rather an exclusion diagnosis, and for this reason,
failure to consider a different diagnosis can cause significant
mortality and morbidity. Only a small proportion of these cases
were diagnosed during the postpartum period. Symptoms such as
dizziness, headache, nausea and vomiting are thought to be
connected to surgery and anaesthesia and not necessarily to
neurological or endocrinological conditions. This is why it is
important to pay attention to ‘red flags’ to avoid diagnostic
errors.
 | Table IIOutcomes of pregnancy-related
pituitary tumour apoplexy cases submitted to surgical decompression
during pregnancy. |
Table II
Outcomes of pregnancy-related
pituitary tumour apoplexy cases submitted to surgical decompression
during pregnancy.
| Authors (ref.) | Year | Age (years) | Diagnosis | Onset | Treatment | Outcome |
|---|
| Oguz et al
(17) | 2020 | 26 |
Macroprolactinoma | 22 weeks | Surgical | Hypothyroidism |
| Jemel et al
(27) | 2019 | 37 | Prolactinoma | 32 weeks | Surgical | Hypothyroidism |
| Bachmeier et
al (4) | 2019 | 30 | Macroadenoma | 36+5 weeks | Surgical
decompression | Full recovery |
| Annamalai et
al (36) | 2017 | 25 |
Microprolactinoma | 37+4 weeks | Conservative
treatment | Full recovery |
| O'Neal (32) | 2017 | 27 | Macroadenoma | 29 weeks | Surgical
decompression | Diabetes
insipidus |
| Galvao et al
(46) | 2017 | 30 |
Macroprolactioma | 28 weeks | Conservative
treatment | N/A |
| Abraham et
al (22) | 2016 | 32 | Enlarged
pituitary | 23 weeks | Surgical
decompression | N/A |
| Grand'Maison et
al (7) | 2015 | 33 | Macroadenoma | 39 weeks | Conservative | Full recovery |
| Watson (42) | 2015 | 33 | Macroadenoma | 37+4 weeks | Conservative | Full recovery |
| Querol Ripoll et
al (34) | 2015 | 37 | Cystic
microprolactinoma | 24 | Surgery |
Panhypopituitarism |
| De Ycaza et
al (47) | 2015 | 26 |
Macroprolactinoma | 28 weeks | Conservative | Partial
hypopituitarism |
| Bedford et
al (48) | 2015 | 35 | Adenoma | N/A | N/A | N/A |
| Piantanida et
al (9) | 2014 | 27 | Adenoma | 35 weeks | Surgery | Central
hypothyroidism |
| Hayes et al
(26) | 2014 | 41 |
Microprolactinoma | 18 weeks | Surgery | Full recovery |
| Tandon et al
(49) | 2014 | 27 | Prolactinoma | 36 weeks | Surgery | Temporary diabetus
insipidus (DI) |
| Chegour and El
Ansari (38) | 2014 | 29 | Prolactinoma | 19 weeks | Conservative | Resolution of
visual visual symptoms |
| Mathur (51) | 2014 | 34 | Pituitary apoplexy
spinal anaesthesia | Postpartum | Surgical
decompression | Reversible cerebral
vasoconstrictive syndrome; Full recovery |
| Kita et al
(28) | 2012 | 26 | Macroadenoma | 26 weeks | Surgical
decompression | Diabetus
inspidus |
| Witek et al
(35) | 2012 | 25 |
Macroprolactinoma | 19 weeks | Surgical
decompression | Full recovery |
| Janssen et
al (16) | 2012 | 27 | Prolactinoma | 10 weeks | Conservative | Partial recovery;
Adrenal insufficiency |
| Couture et
al (39) | 2012 | 37 |
Microprolactinoma | 19 weeks | Conservative | Full recovery |
| Tonda and Rizvi
(45) | 2011 | 22 | Hypophysitis | 36 weeks | Conservative |
Panhypopituitarism |
| Murao et al
(44) | 2011 | 35 | Normal
pituitary | 39 weeks | Conservative |
Panhypopituitarism |
| Bamfo et al
(37) | 2011 | 31 | Macroadenoma | 23 weeks | Conservative | Full recovery |
| Iuliano and Laws
(40) | 2011 | 28 | Acroadenoma | 29 weeks | Conservative | Full recovery |
| Ginath and Golan
(24) | 2010 | 31 | Prolactinoma | 39 weeks | Surgery | Full recovery |
| Perotti and Dexter
(33) | 2010 | 29 | Pituitary
macroadenoma | Postpartum | Surgery |
Panhypopituitarism |
| Parihar et
al (41) | 2009 | 20 |
Macroprolactinoma | 20 weeks | Surgical
decompression | Full recovery |
| Okafor et al
(21) | 2009 | 30 |
Macroprolactinoma | 33 weeks | Conservative | Death |
| Gheorghiu et
al (50) | 2009 | 33 | Nelson
syndrome | 22 weeks | Conservative | Diabetus
inspidus |
| Krull et al
(13) | 2010 | 7 | Normal
pituitary | 7 weeks | Conservative | Miscarriage 9th
week; Ischemic encephalopathy whichwas resolved; Persistent
panhypopituitarism and DI |
| Atmaca et al
(18) | 2006 | 33 | Macroadenoma
(GH-oma) | 29 weeks | Surgical
decompression |
Panhypopituitarism |
| Paech (20) | 2006 | 21 | Macroadenoma | Postpartum | Conservative | Full recovery |
| Fujimaki (43) | 2005 | 23 | Hypophysitis | 34 weeks | Conservative | Adrenal
insufficiency |
| De Heide et
al (10) | 2004 | 26 |
Macroprolactinoma | 23 weeks | Conservative |
Panhypopituitarism |
| Gondim et al
(25) | 2003 | 29 | Macroadenoma | 30 weeks | Surgical
decompression | Full recovery |
| Lee and Pless
(30) | 2003 | 26 | Hypophysitis | 28 weeks | Surgical
decompression | Full recovery |
| Freeman et
al (23) | 1992 | 22 | Prolactinoma | 32 weeks | Surgical
decompression | Diabetus
inspidus |
| Lunardi et
al (19) | 1991 | 21 | Macroadenoma
(GH-oma) | 24 weeks | Surgical
decompression | Full recovery |
| O'Donovan et
al (31) | 1986 | 37 |
Macroprolactinoma | 8 weeks | Left frontotemporal
craniotomy | Left-sided cranial
nerve palsy |
| Lamberts et
al (29) | 1979 | N/A | Prolactinoma | 23 weeks | Surgical
decompression | Resolution of
visual symptoms |
| Our case | 2020 | 26 | Macroadenoma | Postpartum | Surgical
decompression |
Panhypoituitarism |
Mathur et al described a case of postpartum
pituitary apoplexy following spinal anaesthesia which was treated
conservatively. Ten days later, continuous thunderclap headache
prompted computed tomography (CT) angiography and contrast-enhanced
MRI. Images were suggestive of stenoses in the anterior and right
middle cerebral arteries as well as of the vertebrobasilar
segments. Based on the clinical picture, history and imagistic
investigation, the final diagnosis was of reversible cerebral
vasoconstrictive syndrome (RCVS). The patient's condition improved
after treatment with nimodipine and lamotrigine (51). Perotti and Dexter described a
postpartum pituitary apoplexy after a spontaneous delivery. The
mother presented with headache, nausea and photophobia. A contrast
CT scan showed a 6.1x3.9x5.2 cm giant macroadenoma which required
trans-sphenoidal craniotomy (33).
Paech et al published a case of a 15x13x12 mm macroadenoma,
which was diagnosed post-delivery. Similar to our patient, this
case presented initially with drooping eyelid and dilated left
pupil. She reported no headaches, facial weakness or any other
neurological symptom. She was managed conservatively and 14 months
after her first presentation she delivered a second baby. Pregnancy
course and postpartum period were unremarkable (20). We only found one case of pregnancy
pituitary adenoma, which ended with the demise of the patient. A
30-year-old patient diagnosed with pituitary adenoma at 24 weeks of
gestation was prescribed bromocriptine with a plan for a postnatal
neurosurgery. Following a preterm delivery at 35 weeks through
Caesarean section she developed hypertension, acute encephalopathy
and fatal cardiac arrest on day three postpartum (21).
At this moment, there is no robust evidence
regarding the best management. This is a matter of debate between
surgical vs. a conservative method. Whenever pituitary apoplexy
occurs in pregnancy, initial treatment consists of fluid,
electrolyte, and hormonal replacement. In a normal pregnancy,
cortisol levels are two to four times above the average values due
to placental function, pituitary production, and changes in
hormone-binding globulin. Criteria that are used outside pregnancy
cannot be used during gestation or early puerperium. Meanwhile, it
should be emphasized that adrenal insufficiency is a
life-threatening condition. Therefore, glucocorticoid input is
vital and should be started as soon as pituitary apoplexy is
suspected. UK guidelines for pituitary apoplexy recommend 100-200
mg hydrocortisone as intravenous bolus, followed by 2-4 mg/h
intravenous continuous administration or by 50-100 mg every six
hours by intramuscular injection. Once the acute episode is
overcome, the steroid regimen should be reduced to a standard
maintenance dose of 20-30 mg (52).
After stabilization of the patient, the critical
question is whether surgery is necessary or medical treatment is an
option. Due to the rarity of this condition, there are no
randomized control trials only case reports and case series being
reported to date. It is practical to carry on with medical
treatment, and if there is no improvement or a deterioration in
clinical condition then surgery must be performed. In seriously ill
patients, the current literature and expert opinion favors surgical
decompression. Analysis of 22 cases from Table II showed that surgical
decompression in pregnancy is safe without any teratogenic effects
(4,9,17-19,22-35,51).
The majority of cases were able to deliver in the late 3rd
trimester as was exemplified by Oguz et al and Querol Ripoll
et al; the authors showed that surgery performed even in the
second trimester does not alter pregnancy course (17,34).
Analysis of cases treated conservatively showed that this is a
viable and safe option in a patient without visual field defects.
Overall, in 16 cases there was full recovery of endocrinological
function and in 21 cases, various degree of insufficiency ranging
from diabetes insipidus to panhypopituitarism and cranial nerve
palsy being encountered (4,7,9,19,24,26,29,30,35-42,51).
For 11 cases, long-time consequences were not noted. Most patients,
while they were receiving multiple medications, reported a good
quality of life (9,10,16,18,31-34,43-45).
In conclusion, to the best of our knowledge, this is
the third case reported of postpartum gestational pituitary
apoplexy arising in the context of a previous macroprolactinoma
which shows the rarity of this condition. To date, there are no
clear guidelines regarding the most efficacious treatment for
pituitary apoplexy. This issue is more complex in pregnancy. As
pituitary apoplexy is unpredictable, it is imperative to inform
patients with known adenoma about apoplexy symptoms. Antenatal care
should be individualised with urgent MRI and visual field test if
the situation requires. A high index of suspicious, a
multidisciplinary approach and good clinical judgement can ensure
the best decision in terms of management and patient
counselling.
In pregnancy and puerperium alike, headache is
common and although it is usually benign can herald serious and
detrimental intracranial issues.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Further information regarding the case presentation
is available upon request.
Authors' contributions
NB contributed to the conception of the study,
collected, analyzed and interpreted data from the literature and
critically revised the manuscript. IB contributed to the conception
of the study, performed the literature research, drafted the
manuscript and is responsible for confirming the authenticity of
all the raw data. LGP contributed to the conception of the study,
performed the literature research, drafted the manuscript and is
responsible for confirming the authenticity of all the raw data;
ODT and TG contributed to the interpretation of the data from the
literature, collected, analyzed and interpreted the data
corresponding to the patient and critically revised the manuscript.
AI collected, analyzed and interpreted the data corresponding to
the patient and critically revised the manuscript. All authors read
and approved the final manuscript for publication.
Ethics approval and consent to
participate
The Ethics Committee of the National Institute of
Mother and Child Care (Bucharest, Romania) (no. 25/2019) approved
the study.
Patient consent for publication
Patient consent for publication was obtained and
signed by the patient on 11/05/2019.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Goldszmidt E, Kern R, Chaput A and
Macarthur A: The incidence and etiology of postpartum headaches: A
prospective cohort study. Can J Anaesth. 52:971–977.
2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gonzalez JG, Elizondo G, Saldivar D, Nanez
H, Todd LE and Villarreal JZ: Pituitary gland growth during normal
pregnancy: An in vivo study using magnetic resonance imaging. Am J
Med. 85:217–220. 1988.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chestnut DH, Wong CA, Tsen LC, Kee WDN,
Beilin Y and Mhyre J: Postpartum Headache. Obstetric Anesthesia,
Principles and Practice 5th edition. Philadelphia, Elsevier,
pp713-718, 2014.
|
|
4
|
Bachmeier CA, Snell C and Morton A: Visual
loss in pregnancy. BMJ Case Rep. 12(e228323)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Freda PU, Beckers AM, Katznelson L,
Molitch ME, Montori VM, Post KD and Vance ML: Endocrine Society.
Pituitary incidentaloma: An endocrine society clinical practice
guideline. J Clin Endocrinol Metab. 96:894–904. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Molitch ME: Diagnosis and treatment of
pituitary adenomas: A Review. JAMA. 317:516–524. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Grand'Maison S, Weber F, Bédard MJ, Mahone
M and Godbout A: Pituitary apoplexy in pregnancy: A case series and
literature review. Obstet Med. 8:177–183. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Vandeva S, Jaffrain-Rea ML, Daly AF,
Tichomirowa M, Zacharieva S and Beckers A: The genetics of
pituitary adenomas. Best Pract Res Clin Endocrinol Metab.
24:461–476. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Piantanida E, Gallo D, Lombardi V, Tanda
ML, Lai A, Ghezzi F, Minotto R, Tabano A, Cerati M, Azzolini C, et
al: Pituitary apoplexy during pregnancy: A rare, but dangerous
headache. J Endocrinol Invest. 37:789–797. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
de Heide LJ, van Tol KM and Doorenbos B:
Pituitary apoplexy presenting during pregnancy. Neth J Med.
62:393–396. 2004.PubMed/NCBI
|
|
11
|
Abbassi-Ghanavati M, Greer LG and
Cunningham FG: Pregnancy and laboratory studies: A reference table
for clinicians. Obstet Gynecol. 114:1326–1331. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ranabir S and Baruah MP: Pituitary
apoplexy. Indian J Endocrinol Metab. 15 (Suppl 3):S188–S196.
2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Krull I, Christ E, Kamm CP, Ganter C and
Sahli R: Hyponatremia associated coma due to pituitary apoplexy in
early pregnancy: A case report. Gynecol Endocrinol. 26:197–200.
2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lee JS, Park YS, Kwon JT, Nam TK, Lee TJ
and Kim JK: Radiological apoplexy and its correlation with acute
clinical presentation, angiogenesis and tumor microvascular density
in pituitary adenomas. J Korean Neurosurg Soc. 50:281–287.
2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Eastwood AK and Mohan AR: Imaging in
pregnancy. Obstetrician Gynaecol. 21:255–262. 2019.
|
|
16
|
Janssen NM, Dreyer K and van der Weiden
RM: Management of pituitary tumour apoplexy with bromocriptine in
pregnancy. JRSM Short Rep. 3(43)2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Oguz SH, Soylemezoglu F, Dagdelen S and
Erbas T: A case of atypical macroprolactinoma presenting with
pituitary apoplexy during pregnancy and review of the literature.
Gynecol Endocrinol. 36:109–116. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Atmaca A, Dagdelen S and Erbas T:
Follow-up of pregnancy in acromegalic women: Different
presentations and outcomes. Exp Clin Endocrinol Diabetes.
114:135–139. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lunardi P, Rizzo A, Missori P and Fraioli
B: Pituitary apoplexy in an acromegalic woman operated on during
pregnancy by transphenoidal approach. Int J Gynaecol Obstet.
34:71–74. 1991.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Paech MJ: An unusual presentation of a
pituitary tumour in the early postpartum period. Anaesth Intensive
Care. 34:79–82. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Okafor UV, Onwuekwe IO and Ezegwui HU:
Management of pituitary adenoma with mass effect in pregnancy: A
case report. Cases J. 2(6350)2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Abraham RR, Pollitzer RE, Gokden M and
Goulden PA: Spontaneous pituitary apoplexy during the second
trimester of pregnancy, with sensory loss. BMJ Case Rep.
2016(bcr2015212405)2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Freeman R, Wezenter B, Silverstein M, Kuo
D, Weiss KL, Kantrowitz AB and Schubart UK: Pregnancy-associated
subacute hemorrhage into a prolactinoma resulting in diabetes
insipidus. Fertil Steril. 58:427–429. 1992.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Ginath S and Golan A: Images in clinical
medicine. Gestational pituitary-tumor apoplexy. N Engl J Med.
363(e10)2010.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gondim J, Ramos Júnior F, Pinheiro I,
Schops M and Tella Júnior OI: Minimally invasive pituitary surgery
in a hemorrhagic necrosis of adenoma during pregnancy. Minim
Invasive Neurosurg. 46:173–176. 2003.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Hayes AR, O'Sullivan AJ and Davies MA: A
case of pituitary apoplexy in pregnancy. Endocrinol Diabetes Metab
Case Rep. 2014(140043)2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Jemel M, Kandara H, Riahi M, Gharbi R,
Nagi S and Kamoun I: Gestational pituitary apoplexy: Case series
and review of the literature. J Gynecol Obstet Hum Reprod.
48:873–881. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kita D, Hayashi Y, Sano H, Takamura T,
Hayashi Y, Tachibana O and Hamada J: Postoperative diabetes
insipidus associated with pituitary apoplexy during pregnancy.
Neuro Endocrinol Lett. 33:107–112. 2012.PubMed/NCBI
|
|
29
|
Lamberts SW, Klijn JG, de Lange SA, Singh
R, Stefanko SZ and Birkenhäger JC: The incidence of complications
during pregnancy after treatment of hyperprolactinemia with
bromocriptine in patients with radiologically evident pituitary
tumors. Fertil Steril. 31:614–649. 1979.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lee MS and Pless M: Apoplectic lymphocytic
hypophysitis. Case report. J Neurosurg. 98:183–185. 2003.PubMed/NCBI View Article : Google Scholar
|
|
31
|
O'Donovan PA, O'Donovan PJ, Ritchie EH,
Feely M and Jenkins DM: Apoplexy into a prolactin secreting
macroadenoma during early pregnancy with successful outcome. Case
report. Br J Obstet Gynaecol. 93:389–391. 1986.PubMed/NCBI
|
|
32
|
O'Neal MA: Headaches complicating
pregnancy and the postpartum period. Pract Neurol. 17:191–202.
2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Perotti V and Dexter M: Post-partum
pituitary apoplexy with bilateral third nerve palsy and bilateral
carotid occlusion. J Clin Neurosci. 17:1328–1330. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Querol Ripoll R, Cámara Gómez R, Del Olmo
García M, Simal Julián JA and Merino Torres JF: Pituitary apoplexy
in a pregnant woman with cystic microprolactinoma. Endocrinol Nutr.
62:200–202. 2015.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
35
|
Witek P, Zieliński G, Maksymowicz M and
Zgliczyński W: Transsphenoidal surgery for a life-threatening
prolactinoma apoplexy during pregnancy. Neuro Endocrinol Lett.
33:483–488. 2012.PubMed/NCBI
|
|
36
|
Annamalai AK, Jeyachitra G, Jeyamithra A,
Ganeshkumar M, Srinivasan KG and Gurnell M: Gestational pituitary
apoplexy. Indian J Endocrinol Metab. 21:484–485. 2017.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Bamfo JE, Sharif S, Donnelly T, Cohen MA
and Golara M: A case of pituitary apoplexy masquerading as
hyperemesis gravidarum. J Obstet Gynaecol. 31(662)2011.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Chegour H and El Ansari N: Pituitary
apoplexy during pregnancy. Pan Afr Med J. 17(211)2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Couture N, Aris-Jilwan N and Serri O:
Apoplexy of a microprolactinoma during pregnancy: Case report and
review of literature. Endocr Pract. 18:e147–e150. 2012.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Iuliano S and Laws ER Jr: Management of
pituitary tumors in pregnancy. Semin Neurol. 31:423–428.
2011.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Parihar V, Yadav YR and Sharma D:
Pituitary apoplexy in a pregnant woman. Ann Indian Acad Neurol.
12:54–55. 2009.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Watson V: An unexpected headache:
Pituitary apoplexy in a pregnant woman on anticoagulation. BMJ Case
Rep. 2015(bcr2015210198)2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Fujimaki T, Hotta S, Mochizuki T, Ayabe T,
Matsuno A, Takagi K, Nakagomi T and Tamura A: Pituitary apoplexy as
a consequence of lymphocytic adenohypophysitis in a pregnant woman:
A case report. Neurol Res. 27:399–402. 2005.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Murao K, Imachi H, Muraoka T and Ishida T:
Hemolysis, elevated liver enzymes, and low platelet count (HELLP)
syndrome with pituitary apoplexy. Fertil Steril. 96:260–261.
2011.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Tonda C and Rizvi AA: Headache, pituitary
lesion and panhypopituitarism in a pregnant woman: Tumor, apoplexy
or hypophysitis? Am J Med Sci. 342:247–249. 2011.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Galvao A, Gonçalves D, Moreira M,
Inocêncio G, Silva C and Braga J: Prolactinoma and pregnancy-a
series of cases including pituitary apoplexy. J Obstet Gynaecol.
37:284–287. 2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
De Ycaza AE, Chang AY, Jensen JR, Khan Z
and Erickson D: Approach to the management of rare clinical
presentations of macroprolactinomas in reproductive-aged women.
Case Rep Womens Health. 8:9–12. 2015.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Bedford J, Dassan P, Harvie M and Mehta S:
An unusual cause of headache in pregnancy. BMJ.
351(h4681)2015.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Tandon A, Alzate J, LaSala P and Fried MP:
Endoscopic endonasal transsphenoidal resection for pituitary
apoplexy during the third trimester of pregnancy. Surg Res Pract.
2014(397131)2014.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Gheorghiu ML, Chirita C and Coculescu M:
Partial remission of Nelson's syndrome after pituitary apoplexy
during pregnancy. Society for Endocrinology BES 2009 Harrogate, UK
Endocrine, Abstracts 19 P191, 2019.
|
|
51
|
Mathur D, Lim LF, Mathur M and Sng BL:
Pituitary apoplexy with reversible cerebral vasoconstrictive
syndrome after spinal anaesthesia for emergency caesarean section:
An uncommon cause for postpartum headache. Anaesth Intensive Care.
42:99–105. 2014.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Rajasekaran S, Vanderpump M, Baldeweg S,
Drake W, Reddy N, Lanyon M, Markey A, Plant G, Powell M, Sinha S
and Wass J: UK guidelines for the management of pituitary apoplexy.
Clin Endocrinol (Oxf). 74:9–20. 2011.PubMed/NCBI View Article : Google Scholar
|