Introduction
In contrast to the adult population, the pediatric
patient is subject to continuous, dynamic growth and physiological
changes. Therefore, treating and thus preventing dysphagia in
children should also be considered vital subject matter of
pediatrics since aspiration may lead to life-threatening
complications and failure to thrive or malnourishment can generate
serious repercussions on both the intellectual and physical
development of the latter adult (1). Dysphagia appears to be a consequence
of an esophageal motility disorder or a craniofacial malformation,
but often is the result of a narrowing of the esophageal lumen, a
condition that may be congenital or acquired. Congenital esophageal
stenosis is present from birth but may not be associated with
dysphagia in early life. Acquired esophageal strictures primarily
occur following esophageal anastomoses in esophageal atresia. Other
causes of acquired esophageal obstructions are caustic injuries,
peptic or inflammatory disorders (2).
As mentioned in Spitz (3), to emphasize the frailty of an
esophageal anastomosis in children, Potts reported in 1950 that,
‘to anastomose the ends of an infant's esophagus, the surgeon must
be as delicate and precise as a skilled watchmaker; no other
operation offers a greater opportunity for pure technical artistry’
(3). The anastomosis technique in
esophageal atresia (EA) has been a controversial subject since the
early years of modern pediatric surgery. In 1968, Cloud (4) was clear on the issue: ‘What is the
best way to do an anastomosis?’ In the same article, Cloud revealed
his personal communications with Potts over tips and tricks in
esophageal anastomosis, with Potts claiming that using ductus
clamps to hold up both esophageal segments tension-free while
placing all the sutures before releasing them, constituted a
favorable step in order to avoid trauma by excessive stress over
the first stiches (4).
Anastomotic leakage is directly related to tension
of the suture and albeit minor or consecutive to major dehiscence;
it represents one of the most frequent and threatening
complications of esophageal atresia repair (5). In the early ages of EA surgery this
event had an extremely adverse effect on the survival rate varying
from 30 to 60% (4), data that
justified the surgeon's anxiety over esophageal anastomosis tension
which is obviously variable and related to the gap length between
the upper and lower esophageal pouch. At present, anastomotic leak
incidence varies from 4 to 16% and is associated with significant
morbidity and mortality (6).
Considerable breakthroughs were made with regard to
EA patient prognosis and survival. The surgical and intensive care
management of EA patients allowed centers to report an overall
survival rate of 75% (in the 1980s) to 100% (in 2009) in cases with
a birth weight over 2,000 g) and without major cardiac
malformations (7,8). Alongside this evolution, Puri et
al reported in 1981 the opportunity of a delayed primary
anastomosis considering a spontaneous postnatal growth of the two
esophageal segments (9), concluding
in 1992, following the first series of long-term positive outcomes
applying this principle that, ‘the best esophagus is the patient's
own esophagus and, therefore, every effort should be made toward
esophageal preservation by delayed primary anastomosis’. Together
with Puri's observations (10), the
use of esophageal substitution procedures started to cease
(11). Instead of this approach,
primary esophageal anastomosis became the primary technique
utilized although the challenge of the long esophageal gap
remained. Consequently, willing to preserve the native esophagus by
all means, surgeons opt for anastomotic tension even in long gap
EA, which constitutes a risk factor for leakage, dehiscences or
esophageal strictures. In addition, anastomotic tension may
displace the gastroesophageal junction, leading to incompetence of
the gastric cardia and consecutive high gastroesophageal reflux,
adding to the risk of recurrent stricture formation or anastomotic
leakage (12-14).
Besides tension, other factors have been
incriminated to precipitate anastomotic leaks in EA including
small, fragile lower segments, esophageal wall ischemia at the two
esophageal ends, suture technique and materials used, excessive
mobilization of the distal end and increased gap length (14-16).
In extremely rare cases, the trachea-esophageal fistula may
integrate duplication cysts; thus, ischemia or tissue sacrifice may
be inevitable, creating a common esophageal gap into a longer gap,
thereby manifesting challenges in the use of the anastomosis
technique and decision-making (17). Nevertheless, even if at first glance
low birth weight and prematurity are considered risk factors for
anastomotic complications, recent findings do not show any
correlation between these risk factors (18,19).
Regarding anastomotic complications and the surgical approach,
postoperative morbidity following thoracoscopy appears to be
insufficiently studied and reported. In addition, thoracotomy
should remain the gold standard in the absence of experienced teams
and careful patient selection (20).
Classically, anastomosis under tension is made by
dividing it into a posterior layer and an anterior layer, each of
it being closed separately after placing a set of 5/0, 6/0
interrupted sutures on each side. Progressive tension is applied on
one half until upper and lower esophageal segments stick together
and then stitches are tied (21).
Patients and methods
The aim of this study was is to present our
experience in the surgical treatment of esophageal strictures on 11
cases. The ages of the patients ranged from 3 to 12 years with a
mean age of 7 years. All the cases included in the study presented
symptomatic esophageal strictures in which the minimally-invasive
approach failed or it was not indicated and presented to the
Pediatric Surgery Department over a period of 5 years. Patient
medical charts were retrospectively reviewed for causes of
strictures, imagistic tools used, surgical solutions and results.
All the patients were treated by a single pediatric surgical team
at the ‘Marie S. Curie’ Emergency Clinical Hospital for Children in
Bucharest.
Subsequently, a novel device was designed and
registered at the State Office of Inventions and Trademarks (no.
4/87/30.04.2014) recommending it for reducing the tension in the
esophageal anastomosis when required. Informed consent was obtained
in all cases and the study obtained ethics approval (no.
16460/2021) from the ‘M.S. Curie’ Children's Hospital Ethical
Council.
Results
General
Ten consecutive cases of esophageal strictures were
identified: in 5 cases these were secondary to corrosive esophageal
injury, 3 cases were complications of esophageal anastomosis in EA
repair, 2 cases were congenital esophageal stenosis and 1 case was
the consequence of chemotherapy-induced esophageal necrosis and
ulcers in acute lymphoblastic leukemia treatment. In all cases
dysphagia was the cardinal symptom.
Esophageal strictures secondary to
caustic injury in the 5 cases
The mean age at surgery was 70 months for the 5
cases. The youngest patient was 3 years of age and the eldest was
aged 12 years. All 5 cases underwent Stamm gastrostomy at the acute
phase of the corrosive injury and repeated sessions of bougienage
dilations were initiated. In one case, esophageal fistula and
mediastinitis occurred. After at least 1 year of conservative
treatment attempts retrosternal isoperistaltic transverse colon
esophageal replacement was the procedure of choice. The main reason
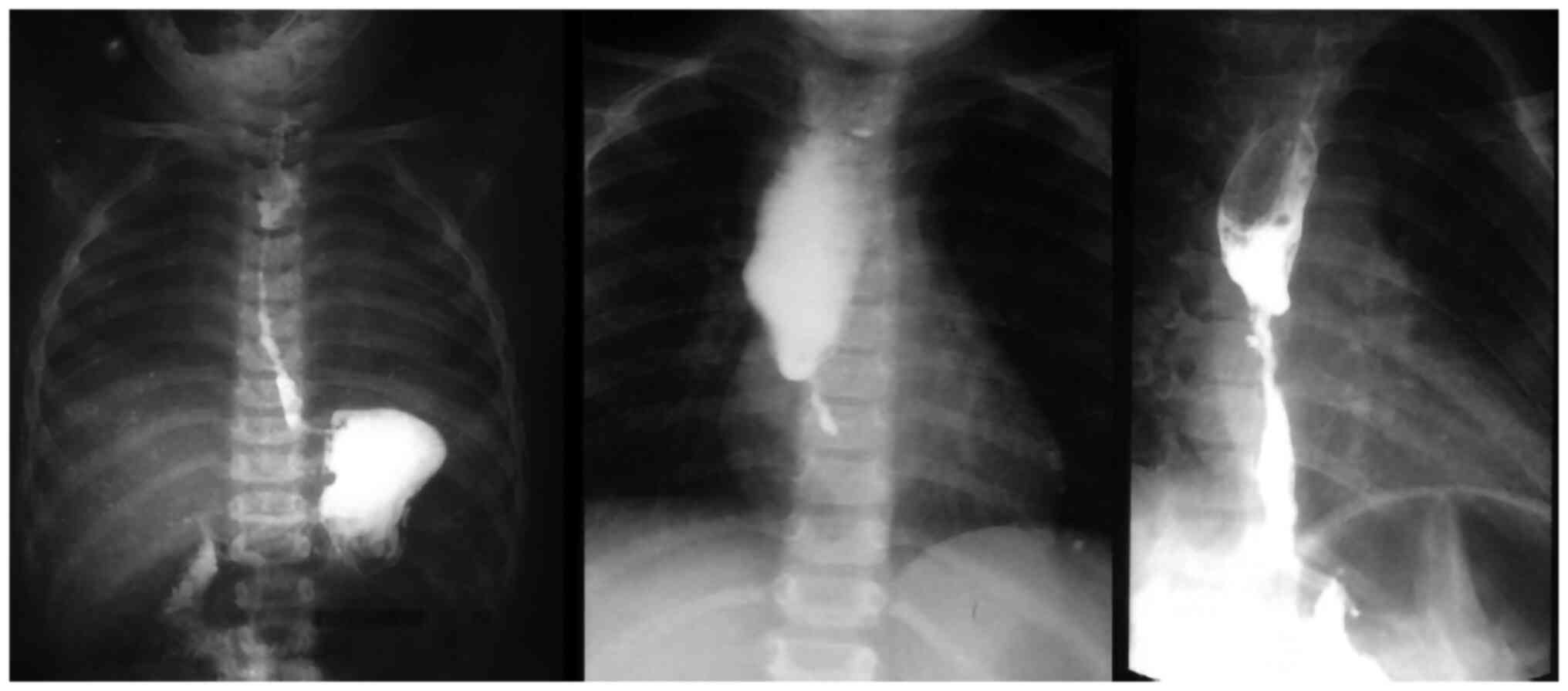
for selecting this solution was the long extension (Fig. 1) of the stricture, which was
unmanageable by bougienage. Early complications included 1 case of
leakage at proximal esophageal-colic anastomosis which was managed
conservatively.
Esophageal strictures secondary to
esophageal anastomosis in EA repair in 2 cases
Three patients had surgery at the age of 4, 5, and 7
years, all three being cases with a poor follow-up after primary
esophageal repair and subsequently failed dilatation procedures.
Resection and re-anastomosis of the esophagus was considered. In
one case, Nissen fundoplication and gastrostomy was initially
performed because of high gastro-esophageal reflux with presenting
high risk of chronic aspiration.
Congenital esophageal stenosis in 2
cases
Two cases of congenital esophageal stenoses were
included in our series. The first case was a 4-month-old female
admitted for repeated episodes of regurgitation, initially
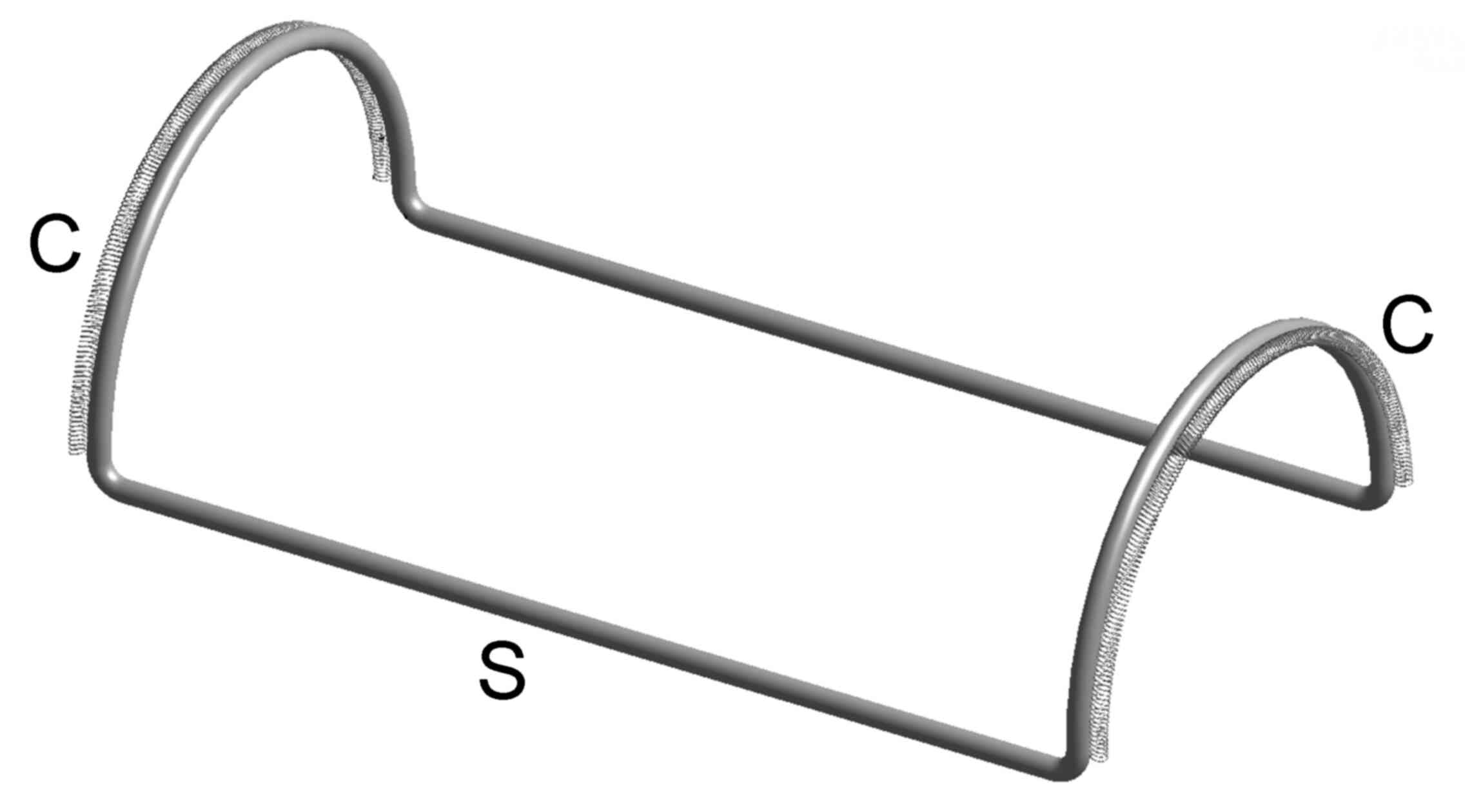
considered as gastroesophageal reflux. An esophagogram was
performed showing the narrowing of the esophagus at T4 level and
aspiration of the barium in the bronchial tree (Fig. 2). Bougienage dilatation was carried
out but without any benefits. Resection of the stenotic segment (~2
cm) and end-to-end anastomosis was performed. Histopathological
examination of the resected esophagus revealed fibro-muscular
thickening of the esophageal wall.
The second case of congenital esophageal stenosis
was a 2-year-old male who was admitted in the Department of
Pediatric Surgery for repeated episodes of regurgitation. The
esophagogram showed a tight, long, esophageal segment (Fig. 3). The patient also had associated
trisomy 21, and was previously operated for ventricular septal
defect and cleft palate. Bougienage was attempted without any
results. Lower esophageal substitution with distal ileum was
performed with a favorable outcome.
Chemotherapy-induced esophageal ulcer
and necrosis complicated with esophageal stricture in 1 case
A 4 year-old-girl was referred to the Department of
Pediatric Surgery by the oncologist for evaluation of achronic
dysphagia. She was previously treated, starting at 2 years of age,
for acute lymphoblastic leukemia. High doses of dexamethasone were
used in the leukemia treatment and she also had a history of
systemic candidiasis. We presumed the esophageal narrowing etiology
was multifactorial in this situation. Resection of the stenotic
segment objectified on the esophagogram and esophageal anastomosis
was performed with favorable outcome.
Tension-releasing device for
end-to-end esophageal anastomosis
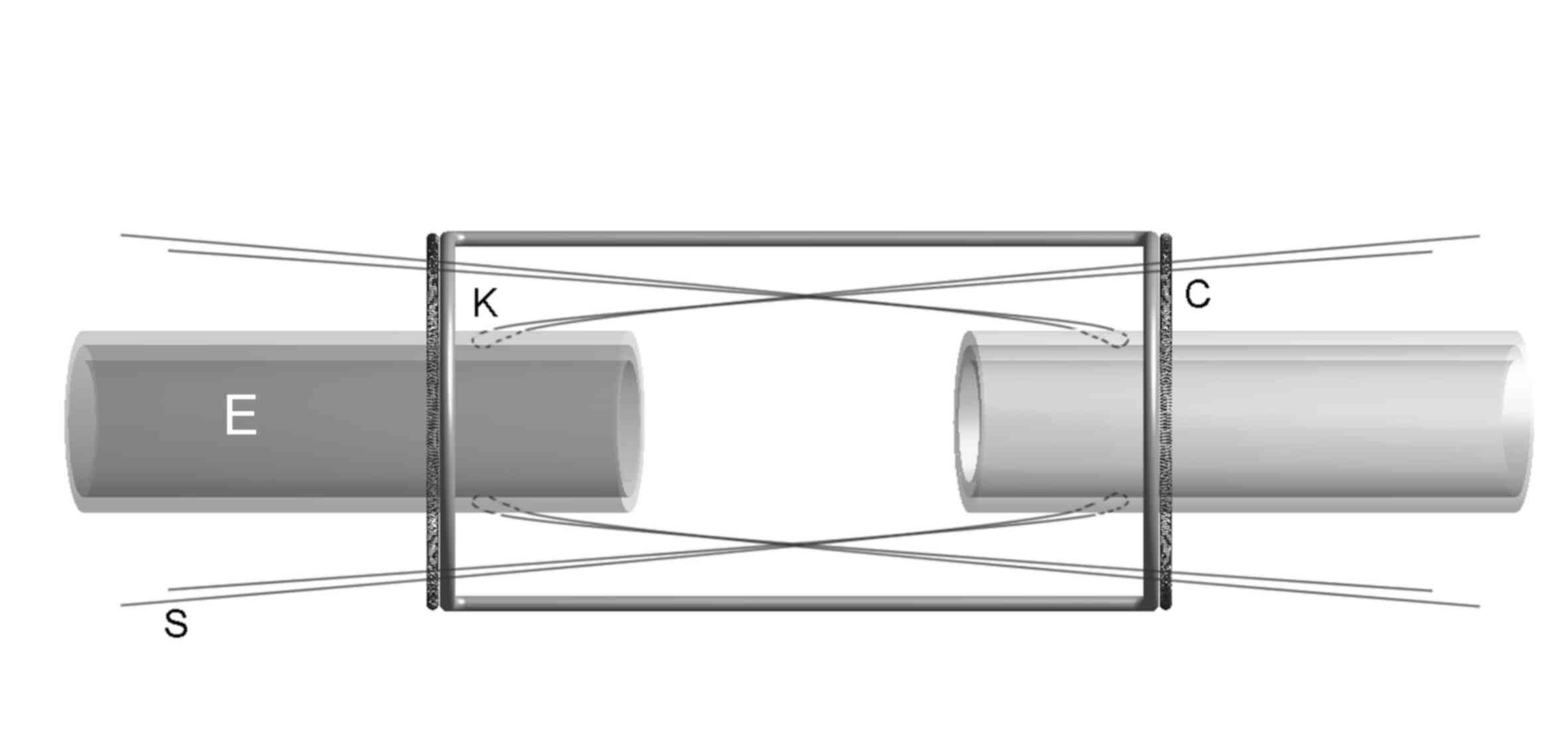
Technically, the device we developed is a metallic
structure following the contour of a half-cylinder divided by a
longitudinal plane (a ditch-like skeleton). Each of the
semi-circular cylinder base halves has 2 set of coils attached for
anchoring the stay sutures (Fig.
4).
The device overtakes the mechanical tension in the
two esophageal ends, adjusting it in order to place all the sutures
tension-free (or under minimal tension) and releasing the tension
only after the complete anastomosis is achieved; therefore, the
force is divided and equally allocated on each of the sutures.
After dissection of the two esophageal ends is
completed, the device is inserted into the thoracic cavity,
parallel to the esophagus and over the anastomosis site. The
surgeon divides the anastomosis into two quadrants by placing two
stay sutures (S) on each esophageal ending, through the adventitia
and muscularis of the esophageal wall (K), respecting the
submucosal layer, at a relative distance from the two esophageal
endings that will further constitute the final anastomosis. The
stay sutures are stretched and fixed to the coils of the device
(C), each pair in opposite directions thereby narrowing the gap
between the two esophageal endings without applying any kind of
mechanical effort on the future site of the anastomosis (Fig. 5). The full anastomosis is then
performed without any tension, the stay sutures are removed
individually and the device is removed allowing each of the
anastomosis sutures to overtake a small amount of tension equal to
the others.
We conceived this considering that unequally divided
tension, ischemia and esophageal mucosal or submucosal tears during
surgical manipulation are significant factors in anastomotic leaks
and dehiscence incidence. Equidistant and uniform forces in the
anastomoses may prevent stricture formation or may attribute benign
aspects to the esophageal stricture.
Discussion
Esophageal stenosis in children is congenital or
acquired. Congenital esophageal stenosis may embrace various
histopathological aspects. These types of stenosis can be secondary
to tracheo-bronchial remnants, fibro-muscular hypertrophy of the
esophagus or they can present as a membranous diaphragm in the wall
of the esophagus. Minimally invasive treatment of congenital
esophageal stenosis, depending on their nature, varies widely,
including dilatations of the esophagus, endoscopic resection of the
diaphragm or longitudinal myotomy. Invasive surgery should be
considered in cases where endoscopy is ineffective (22).
Secondary esophageal stenoses in pediatric
population are mainly encountered as a complication of esophageal
anastomoses in EA. Other causes of acquired esophageal obstructions
are caustic injuries, peptic or inflammatory disorders (2). Chemotherapy in acute leukemia of
childhood is known to induce esophageal ulcer or necrosis.
Moreover, during administration of oncologic treatments, the
altered immune status led to esophageal candidiasis. Regarding the
side effects of the drugs administered, esophageal strictures in
acute leukemia are related to esophagitis as a consequence of
high-dose dexamethasone, doxorubicin, citarabin and methotrexate
(23).
Regardless of the etiology of esophageal stenosis,
when surgical treatment is required to preserve the native
esophagus and to reduce tension between the two esophageal ends
making anastomosis possible, use of several techniques and
procedures has been suggested to narrow the gap length. Some of
them can be applied while attempting both initial and delayed
anastomosis, while others are reserved for delayed primary
esophageal repair (Table I). All
these are reported more or less with associated morbidities,
prolonged hospital stays, or requirement of multiple surgical
reinterventions (24). Such
interventions are possible in tertiary centers, having well-trained
multidisciplinary teams for congenital and acquired various
difficult/rare conditions (25,26).
 | Table ITechniques of esophageal
reconstruction. |
Table I
Techniques of esophageal
reconstruction.
| Proximal
esophagomyotomy (circular or spiral): using or without using
balloon catheters to facilitate mobilization |
| Upper pouch (and
lower pouch) bougienage |
| Using magnetic
attraction between the two pouc |
| Bridging the gap with
sutures between the two esophageal ends and progressively reducing
the gap |
| Extrathoracic
elongation of the upper pouch by progressively migrating a proximal
esophagostomy down the chest wall |
| Placing traction
sutures on both the proximal and distal esophageal pouches,
externally or internally |
| Creating a
full-thickness anterior flap from the upper pouch which can be
tubularized and anastomosed to a lower esophageal segment |
| Gastric transposition
into the chest; resection of the distal esophagus, division of the
left gastric vessels and moving the fornix upwards through the
diaphragmatic hiatus, where it will be anastomosed to the proximal
esophagus; pyloroplasty systematically performed. |
In addition to previously mentioned preoperative or
intraoperative surgical techniques whose purpose is gap narrowing
or releasing the anastomosis tensions, other postoperative
approaches are used, including keeping the neck flexed which
reduces esophageal stretching or keeping up to one-week mechanical
ventilation together with elective paralysis (27). Other methods have been reported to
be useful in an isolated case series, including using a
trans-anastomotic balloon catheter passed into the stomach and
then, subsequent to a gentle force from outside the
gastroesophageal junction, reducing the anastomotic tension, the
tube is fixed externally to the skin (28).
Besides endoscopic dilatations, using balloon or
bougienage may be considered, esophageal self-expandable stents
placing may be considered in case of recurrent strictures; however,
most patients may experience chest pain, nausea or stent migration.
Esophageal stenting in pediatric patients is reported to have
successful results or is considered to be a bridge to definitive
surgery (2,29).
For all our patients, we obtained an appropriate
informed consent from their parents (30,31).
The tension-releasing device for end-to-end
esophageal anastomosis was designed due to its advantages including
that, it builds up a high quality anastomosis permitting an
improved overview on the symmetry of the surgical suturing,
eliminates from the operatory field (albeit extremely small) the
use of unnecessary forceps employed in suture tying leading to an
improved view and more space for maneuvers, and allows optimal and
synchronous stretching on the common longitudinal axis of both
esophageal endings. However, there are disadvantages to consider
including, the suture passing through auxiliary parts of the
esophageal wall, unnecessary mainly in anastomosis, thus the
possibility of unwanted laceration (although this may depend solely
on the surgeon's skill), the device should fit to each patient's
size, and the present tool cannot be used by surgeons who prefer
the thoracoscopic approach.
In conclusion, esophageal stenosis of childhood may
present by various anatomic aspects depending on their underlying
etiology. Case selection should always be carefully made. Treatment
should initially follow a conservative endoscopic approach. If
refractory, surgery should be considered and depending on
characteristics of strictures it can consist of esophagomyotomy,
stenotic area resection followed by end-to-end anastomosis or
esophageal replacement procedures. The surgical procedure should
always be adapted on a careful evaluation of the stricture
appearance and the patient's history. When the gap between the
esophageal ends resulting from removal of the lesion is long,
esophageal anastomosis is challenging. The tool we designed may be
useful in this situation, reducing the mechanical tension when
performing the anastomosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DAI and RIS performed surgical procedures and
confirm the authenticity of all the raw data. OS, LFT and AT
conducted the preoperative investigations; IB, RIS and DR
contributed to the literature review; NB, IB and OS analyzed the
data; RIS, AT, FG and FF contributed to critical revisions on the
intellectual content; DAI finally revised the draft of the
manuscript. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Informed consent from the parents/legal guardians
was obtained in all cases and the study obtained ethics approval
from the ‘M.S. Curie’ Children's Hospital Ethical Council,
registered with no. 16460/2021.
Patient consent for publication
Parents/legal guardian consent for publication of
images or clinical data was obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dodrill P and Gosa MM: Pediatric
dysphagis: Physiology, assessment, and management. Ann Nutr Metab.
66 (Suppl 5):S24–S31. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Vandenplas Y: Management of benign
esophageal strictures in children. Pediatr Gastroenterol Hepatol
Nutr. 20:211–215. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Spitz L: Oesophagealatresia. Orphanet J
Rare Dis. 2(24)2007.
|
|
4
|
Cloud DT: Anastomotic technic in
esophageal atresia. J Ped Surg. 3:561–564. 1968.PubMed/NCBI View Article : Google Scholar
|
|
5
|
D'Urzo C, Bunuomo V, Rando G and Pintus C:
Major anastomotic dehiscence after repair of esophageal atresia:
Conservative management or reoperation? Dis Esophagus. 18:120–123.
2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gupta M, Mahajan JK, Bawa M and Rao KLN:
Esophageal atresia and tracheoesophageal fistula: Effect of pleural
cover on anastomotic dehiscence. J Indian Assoc Pediatr Surg.
16:50–53. 2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Spitz L, Kiely EM, Morecroft JA and Drake
DP: Oesophageal atresia: At-risk groups for the 1990s. J Ped Surg.
29:723–725. 1994.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Okamoto T, Takamizawa S, Arai H, Bitoh Y,
Nakao M, Yokoi A and Nishijima E: Esophageal atresia: Prognostic
classification revisited. Surgery. 145:675–681. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Puri P, O'Donnell B and Guiney EJ: Delayed
primary anastomosis following spontaneous growth of esophageal
segments in esophageal atresia. J Ped Surg. 16:180–183.
1981.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Puri P, Ninan GK, Blake NS, Fitzgerald RJ,
Guiney EJ and O'Donnell B: Delayed primary anastomosis for
esophageal atresia: 18 Months' to 11 years' follow-up. J Pediatr
Surg. 27:1127–1130. 1992.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kelly JP, Shackelford GD and Roper CL:
Esophageal replacement with colon in children: Functional results
and long-term growth. Ann Thorac Surg. 36:634–643. 1983.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sri Paran T, Decaluwe D, Corbally M and
Puri M: Long-term results of delayed primary anastomosis for pure
oesophageal atresia: A 27-year follow up. Pediatr Surg Int.
23:647–651. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nagaya M, Kato J, Niimi N, Tanaka S and
Iio K: Proposal of a novel method to evaluate anastomotic tension
in esophageal atresia with a distal tracheoesophageal fistula.
Pediatr Surg Int. 21:780–785. 2005.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mckinnon LJ and Koloske AM: Prediction and
prevention of anastomotic complications of esophageal atresia and
tracheoesophageal fistula. J Pediatr Surg. 25:778–781.
1990.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Upadhyaya VD, Gangopadhyaya AN, Gupta DK,
Sharma SP, Kumar V, Pandey A and Updhyaya AD: Prognosis of
congenital tracheoesophageal fistula with esophageal atresia on the
basis of gap length. Pediatr Surg Int. 23:767–771. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chittmittrapap S, Spitz L, Kiely EM and
Brereton RJ: Anastomotic leakage following surgery for esophageal
atresia. J Pediatr Surg. 27:29–32. 1992.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Spataru RI, Popoiu MC and Ivanov M:
Foregut duplication cyst associated with esophageal
atresia-one-stage neonatal surgical repair. Indian J Surg. 77
(Suppl 1):S52–S55. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Teimourian A, Donoso F, Stenström P,
Arnadottir H, Arnbjörnsson E, Lilja H and Salö M: Gender and birth
weight as risk factors for anastomotic stricture after esophageal
atresia repair: A systematic review and meta-analysis. BMC Pediatr.
20(400)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Dingemann C, Brendel J, Wenskus J, Pirr S,
Schukfeh N and Reinshagen K: Low gestational age is associated with
less anastomotic complications after open primary repair of
esophageal atresia with tracheoesophageal fistula. BMC Pediatr.
20(267)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Laberge JM and Blair GK: Thoracotomy for
repair of esophageal atresia: Not as bad as they want you to think!
Dis Esophagus. 26:365–371. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Spitz L and Pierro A: Operative Pediatric
Surgery. Spitz L and Coran A (eds). CRC Press, Inc., Boca Raton, FL
pp135, 2013.
|
|
22
|
Takamizawa S, Tsugawa C, Naruaki M, Satoh
S, Kanegawa K, Nishijuma E and Muraji T: Congenital esophageal
stenosis: Therapeutic strategy based on etiology. J Pediatr Surg.
37:197–201. 2002.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kelly K, Storey L, O'Sullivan M, Butler K,
McDermott M, Corbally M, McMahon C, Smith OP and O'Marcaigh A:
Esophageal strictures during treatment for acute lymphoblastic
leukemia. J Pediatr Hematol Oncol. 32:124–127. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Harmon CM and Coran AG: Congenital
anomalies of the esophagus. In: Pediatric Surgery. Coran AG, Adzick
NS, Krummel TM, Laberge J, Shamberger RC and Caldmone AA (eds). 7th
edition. Elsevier Saunders, Philadelphia, PH, pp893-918, 2012.
|
|
25
|
Suciu N, Serban A, Toader O, Oprescu D and
Spataru RI: Case report of fetal lingual tumor-perinatal care and
neonatal surgical intervention. J Matern Fetal Neonatal Med.
27:314–319. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Spătaru RI, Iozsa DA and Ivanov M:
Preputial calculus in a neurologically-impaired child. Indian
Pediatr. 52:149–150. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Pinheiro PF, Simões e Silva AC and Pereira
RM: Current knowledge on esophageal atresia. World J Gastroenterol.
18:362–372. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Boia ES, Nicodin A, Popoiu MC, Trailescu M
and David VL: An effective method to release anastomotic tension
after repair of esophageal atresia using a Foley catheter.
Chirurgia (Bucur). 108:189–192. 2013.PubMed/NCBI
|
|
29
|
Tandon S, Burnand KM, De Coppi P, McLaren
CA, Roebuck DJ and Curry JI: Self-expanding esophageal stents for
the management of benign refractory esophageal strictures in
children: A systematic review and review of outcomes at a single
center. J Pediatr Surg. 54:2479–2486. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Șerban D, Spătaru RI, Vancea G, Bălășescu
SA, Socea B, Tudor C and Dascălu AM: Informed consent in all
surgical specialties: From legal obligation to patient
satisfaction. Rom J Leg Med. 28:317–321. 2020.
|
|
31
|
Șerban D, Smarandache AM, Cristian D,
Tudor C, Duta L and Dascălu AM: Medical errors and patient safety
culture-shifting the healthcare paradigm in Romanian hospitals. Rom
J Leg Med. 28:195–201. 2020.
|