Introduction
Endoscopic retrograde cholangiopancreatography
(ERCP) has become the preferred diagnostic and therapeutic option
for a number of pancreaticobiliary conditions. However, it is not
always successful even with experienced hands or in high-volume
medical centers (1,2). It is known that selective biliary
cannulation is key to ERCP and the following treatments, according
to studies, bile duct cannulation fails in patients at a rate
ranging between 5 and 15% (3,4). In
most cases, patients with small duodenal papilla, papilla opening
sclerosis, papilla looseness, peripapillary diverticulum and
surgically altered anatomy are more likely to undergo unsuccessful
biliary cannulation (5-8).
Alternative methods, including repeat ERCP, percutaneous-endoscopic
or endoscopic ultrasound-guided rendezvous procedures, percutaneous
transhepatic biliary therapy and surgical intervention, can be
chosen to gain biliary access following the failure of initial ERCP
(9-14).
However, these technical alternatives to a second ERCP following
the initial failure procedure still have several limitations, such
as their invasiveness and morbidity, and they are not as widely
available as ERCP (9,10). Furthermore there is no consensus in
the guidance of handling patients with failed biliary cannulation
at the initial ERCP and the issues of a second ERCP, such as the
optimal interval time and risk factors for cannulation failure,
need to be solved.
Therefore, this retrospective study investigated
whether it is justifiable to conduct a second ERCP within a short
time interval following an initial failure caused by a difficult
cannulation. It also aimed to identify risk factors for a second
ERCP.
Materials and methods
Data collection
A retrospective study of all patients who underwent
ERCP between June 2016 and September 2020 in the Department of
Hepatobiliary Surgery at the First Affiliated Hospital of Chongqing
Medical University was conducted. All patients with native papilla
who underwent ERCP for the first time with an initial failure of
these procedures that was attributed to difficult biliary
cannulation were included. The exclusion criteria were as follows:
Age <18 years, invisible major duodenal papilla, selective
pancreatic duct cannulation and lack of requested data in the
database.
Data for each ERCP procedure were retrieved from the
database system of the First Affiliated Hospital of Chongqing
Medical University (Chongqing, China). Patients' main details,
indications for ERCP, technical details of the procedures, final
diagnoses, procedure-related complications, perioperative
biochemical indices and follow-up data were recorded. All patients
gave written informed consent before ERCP. The study was approved
by the ethical review board at the First Affiliated Hospital of
Chongqing Medical University (no. 2020-668).
ERCP procedure
An experienced endoscopist and a professional nurse
(performing >200 ERCPs per year) performed all endoscopic
procedures with fluoroscopic assistance and using a therapeutic
duodenoscope (PENTAX ED34-i10T 4.2; Pentax Medical) and endoscopic
accessories (Boston Scientific and Olympus Corporation). The
commonly used advanced cannulation techniques included
double-guidewire (DGW) technique and needle-knife sphincterotomy
(NKS).
All patients fasted routinely for 8 h before the
operation. At 30 min before the procedure, patients were
consciously sedated with intramuscular anisodamine 10 mg, pethidine
and diazepam (the dose was determined according to the condition of
patients). Usually, standard biliary cannulation was performed with
the guidewire-assisted technique. A double lumen pull-type
sphincterotome (Olympus Corporation) preloaded with a hydrophilic
guidewire (Hydra Jagwire; Boston Scientific) was used in this
technique. However, if the guidewire was put into the pancreatic
duct more than twice, the guidewire had to be kept in the
pancreatic duct and the DGW technique had to be used. If standard
biliary cannulation was unsuccessful and DGW was not performed or
failed, NKS would be used. NKS was performed with a needle-knife
sphincterotome (Triple-lumen Microknife XL; Boston Scientific). The
needle tip was anchored over the incarcerated calculus or directly
on the summit of the protuberant papilla and then a puncture was
made in the papilla above the orifice. If biliary cannulation could
not succeed through this opening, a more extended incision was made
upward stepwise along the axis of the bile duct from the papillary
orifice. When the opening of the distal bile duct was exposed, it
became possible to cannulate selectively with a guide wire passed
through a sphincterotome. In addition, NKS or DGW was performed in
the second ERCP procedure when standard cannulation could not be
achieved.
The criteria of conducting second ERCP were as
follows: i) Patients' clinical condition was stable; ii) patients
agreed to attempt a second ERCP; iii) The endoscopist in the
department recommended a second attempt at biliary cannulation; iv)
other experts in the department agreed that a successful second
ERCP might be more beneficial than other options.
Outcomes and definition
The primary outcome measure was the efficacy and
safety of a second ERCP following initially failed. ERCP was deemed
successful if biliary access was achieved enabling appropriate
therapy.
Difficult biliary cannulation was defined by the
presence of ≥1 of the following: >5 contacts with the papilla
whilst attempting to cannulate, inability to achieve selective
biliary cannulation by standard technique within 10 min, >1
unintended pancreatic duct cannulation or failure of access to the
major papilla (15,16).
‘Expert endoscopist’ was defined as one having
performed >1,000 ERCPs during their career and who could perform
procedures equivalent to Grade 3 of the grading scale for the
difficulty of ERCP, based on the ERCP core curriculum, without
assistance (17-20).
Procedure-related complications were defined as
adverse clinical events or unexpected clinical outcomes related to
the procedure. Specifically, the present study assessed 30-day
mortality, post-ERCP pancreatitis (PEP), bleeding, cholangitis,
perforation and any unexpected adverse clinical event (21). PEP was defined as abdominal pain
and an increase of serum amylase levels at least three times
greater than the normal upper limit requiring hospitalization for
at least 2 nights (21).
The secondary outcomes were the risk factors for
cannulation failure of the second ERCP.
Statistical analysis
Continuous variables were measured as median with
range and categorical variables were measured as frequencies
(percentages). Statistical analyses for comparing outcomes of the
two groups were performed with Mann-Whitney U test. For categorical
data, the Chi-square or the Pearson's corrected Chi-square test was
used where appropriate. Unconditional logistic regression analysis
was performed to identify predictors associated with the second
ERCP cannulation failure. Differences were considered statistically
significant with a two-sided P-values of <0.05. All statistical
analyses were performed by using SPSS software (v 24.0; IBM
Corp.).
Results
General description
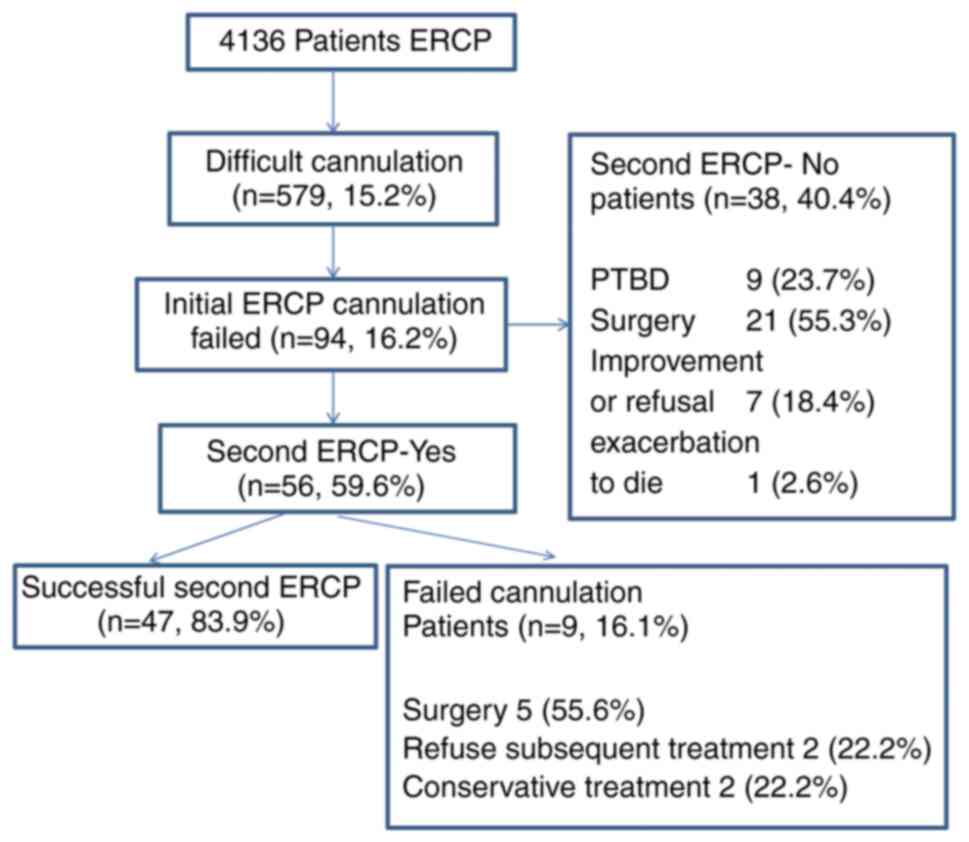
A total of 4,136 ERCPs were performed during this
period. Of these, 579 (15.2%) ERCPs referred to difficult
cannulation. A total of 94 patients (2.3%) who met the study
inclusion criteria were identified. The median age of the cohort
was 68 years (range 18-92); 57 (60.6%) were female. The indications
for ERCP included benign stricture (32 patients, 34%), malignant
stricture (25 patients, 26.6%) and choledocholithiasis (37
patients, 39.4%). The baseline characteristics of the study cohort
are summarized in Table I. A
second ERCP was performed in 56 patients with persistence of the
initial clinical indication and stable condition following initial
failure to gain biliary access. Among the remaining 38 patients,
nine underwent percutaneous transhepatic biliary drainage (PTBD),
21 underwent surgery, seven did not undergo a second ERCP due to
clinical improvement or patient refusal and one died due to rapid
clinical deterioration and could not undergo any treatment
(Fig. 1).
 | Table IDemographic and baseline
characteristics of patients and procedures with initial biliary
cannulation failed. |
Table I
Demographic and baseline
characteristics of patients and procedures with initial biliary
cannulation failed.
| Initial failed
biliary cannulation patients | n=94 |
|---|
| Median age, years
(range) | 68.0
(18.0-92.0) |
| Sex female, n | 57 (60.6%) |
| Indications, n | |
|
Benign
stricture | 32 (34%) |
|
Malignant
stricture | 25 (26.6%) |
|
Choledocholithiasis | 37 (39.4%) |
| Initial median
operative time, minutes (range) | 60.5 (25-141) |
| Median hospital
stay, days (range) | 14 (1-41) |
| Total bilirubin
before first ERCP, median (range) (µmol/l) | 37.7
(6.9-562.9) |
| Days between ERCP,
median (range) | 3 (1-9) |
| Adverse events
after first ERCP, n | 9 (9.6%) |
|
Perforation | 1 (1.1%) |
|
Pancreatitis | 5 (5.3%) |
|
Cholangitis | 2 (2.1%) |
|
Hemorrhage | 1 (1.1%) |
| 30-day mortality,
n | 6 (6.25%) |
| Second ERCP, n | 56 (59.6%) |
| Second cannulation
success, n (%) | 47/56 (83.9%) |
| Adverse events
after second ERCP, n | 5/56 (8.9%) |
|
Perforation | 0 |
|
Pancreatitis | 3/56 (5.3%) |
|
Cholangitis | 2/56 (3.6%) |
|
Hemorrhage | 0 |
Second ERCP outcomes
For the 56 patients in whom a second ERCP was
attempted, biliary access was achieved in 47 cases, equating to a
success rate of 83.9%. The nine failed second ERCP patients did not
undergo a third ERCP. Of these, two were discharged with
conservative treatment, two refused subsequent therapy and left the
hospital and five chose to accept surgery. The second ERCP was
performed a median of 3 days (interquartile range 2-4.25 days)
following the initial unsuccessful biliary cannulation. Table II shows that the median operative
time was significantly shorter (47 vs. 65 min, P<0.001) and the
number of applications of auxiliary cannulation techniques was
significantly higher (39 vs. 30, P=0.036) in the second ERCP
compared with the first ERCP. The biochemistry indices of serum
amylase and total bilirubin levels 24 h following the operation
showed no obvious changes. A total of 6 of 94 (6.25%) patients
succumbed within 30 days of their latest ERCP. Table III shows that the 30-day
mortality in the patients who did not undergo a second ERCP was
significantly higher compared with that in the patients who
underwent a second ERCP. The causes of mortality were not related
to ERCP; 1 patient underwent a second ERCP and 2 patients underwent
PTBD, all of them succumbed from underlying advanced malignancy.
The other 3 patients underwent radical surgery and died from
surgery-related complications.
 | Table IICharacteristics of patients underwent
a successful second ERCP. |
Table II
Characteristics of patients underwent
a successful second ERCP.
|
Characteristics | First ERCP | Second ERCP | P-value |
|---|
| Median operative
time, minutes (range) | 65 (31-120) | 47 (26-127) |
<0.001a |
| Adverse events,
n | 4 (8.5%) | 3 (6.4%) | >0.999 |
| Serum amylase 24 h
after operation, median (range) (U/l) | 65 (30-1265) | 86 (30-1135) | 0.482 |
| Total bilirubin 24
h after operation, median (range) (µmol/l) | 30.8
(5.5-559.9) | 29.8 (9-645.9) | 0.623 |
| Cannulation
techniques, n | 30 (63.8%) | 39 (74.5%) | 0.036a |
|
NKS | 16 | 21 | |
|
DGT | 14 | 18 | |
 | Table IIIResults of comparison between the two
groups with or without second ERCP. |
Table III
Results of comparison between the two
groups with or without second ERCP.
| Variables | No repeat ERCP
group (n=38) | Second ERCP group
(n=56) | P-value |
|---|
| Median age, years
(range) | 68.5 (41-92) | 67 (18-89) | 0.755 |
| Sex (female),
n | 24 (63.2%) | 33 (58.9%) | 0.680 |
| Hospital stay,
median days (range) | 13 (1-41) | 15 (5-38) | 0.227 |
| First operation
time, minutes | 58.5 (25-140) | 64.5 (31-120) | 0.280 |
| Cannulation
technique on the first ERCP | 20 (52.6%) | 35 (62.5%) | 0.341 |
|
NKS | 12 | 19 | |
|
DGT | 8 | 16 | |
| Adverse events
after the first ERCP, n | 5 (13.2%) | 4 (7.1%) | 0.538 |
| 30-day mortality,
any causes, n | 5 (13.2%) | 1 (1.8%) | 0.038a |
| 30-day mortality
related to the ERCP, n | 0 | 0 | - |
Adverse events
Among the 94 patients in whom initial cannulation
failed, 9 adverse events were recorded (9.6%); 5 occurred in
patients who underwent a second ERCP. In total, the adverse events
were not severe. After the first ERCP, 5 patients experienced mild
PEP, 1 patient suffered duodenal perforation, 2 patients
experienced mild cholangitis and 1 patient suffered delayed
bleeding. After the second ERCP, 3 patients suffered moderate PEP
and 2 patients experienced mild cholangitis. The duodenal
perforation was repaired through the endoscopic channel. All cases
of PEP and cholangitis were treated conservatively and the patients
recovered within a few days. There was no significant difference in
adverse events following two ERCPs (4 vs. 3, P=1.000). There were
also no adverse events between the second ERCP group and the no
repeat ERCP group (Table
III).
Risk factors for cannulation in the
second ERCP failure
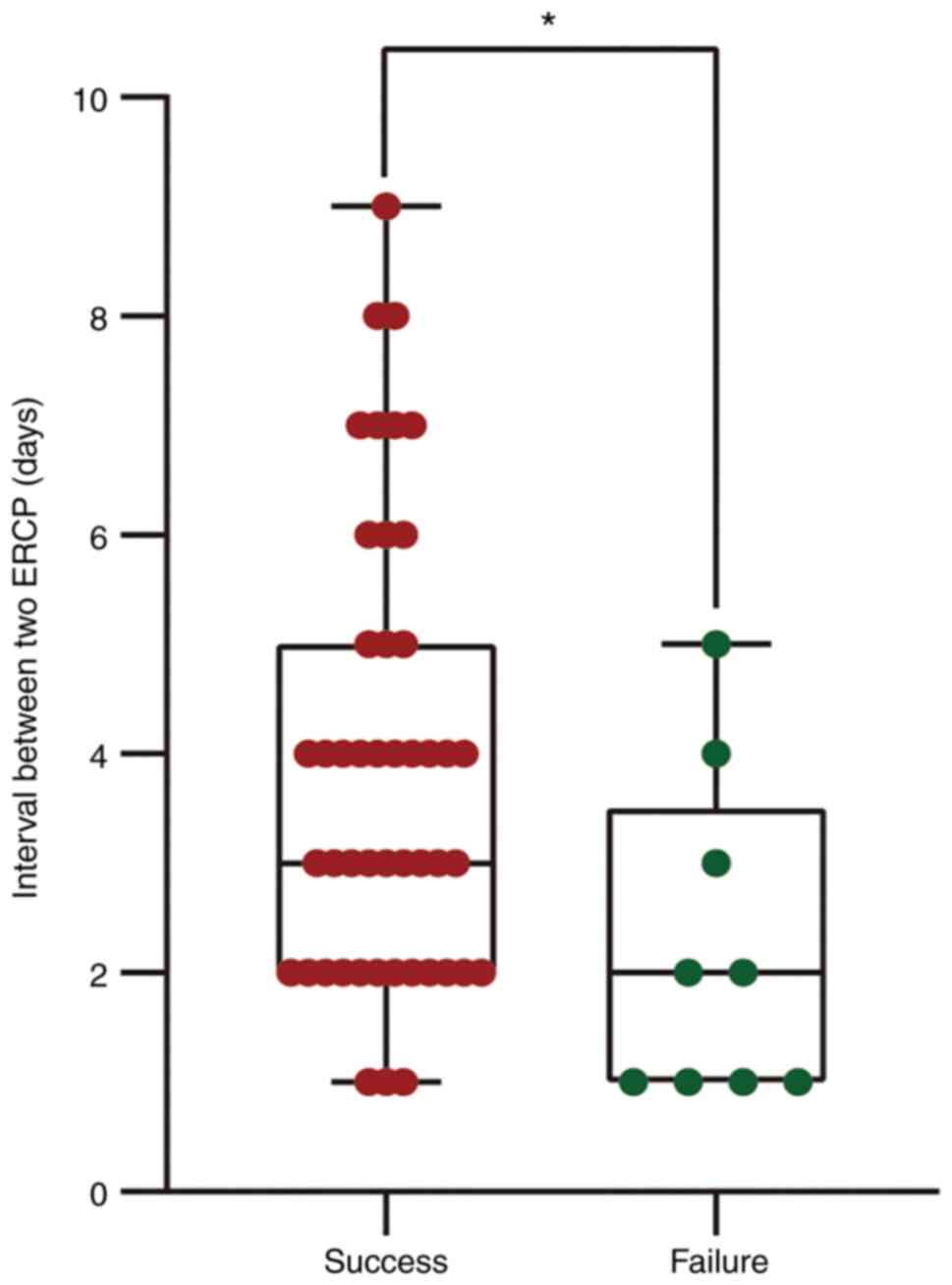
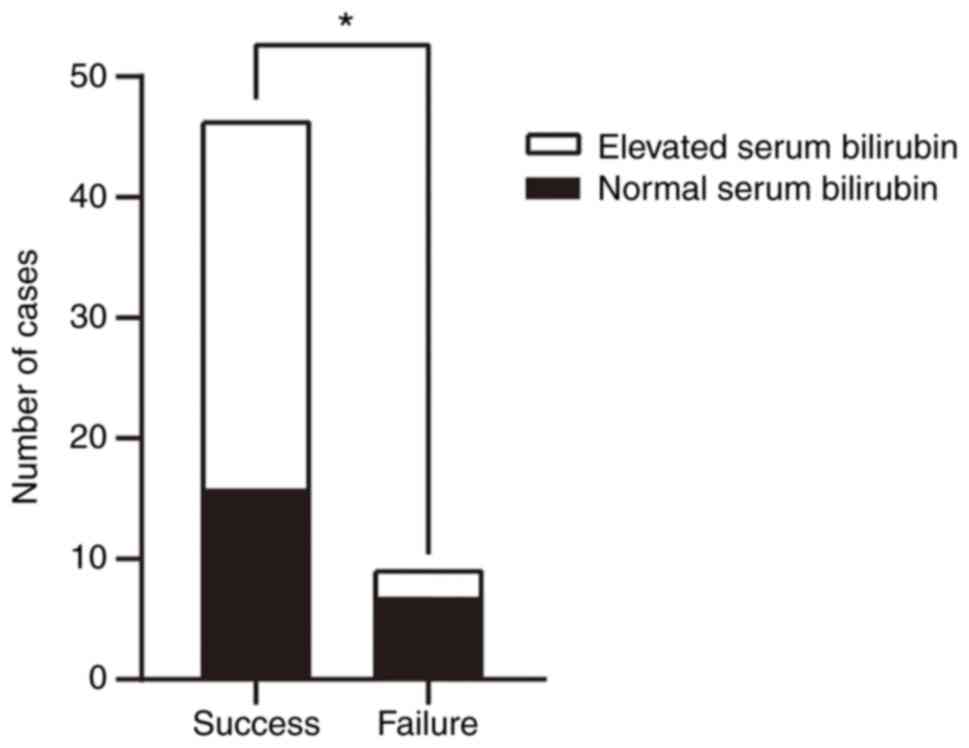
Table IV shows the
results of univariate analysis for factors predicting cannulation
failure in the second ERCP. Accordingly, the days between the two
ERCP procedures (Fig. 2) and
normal serum bilirubin levels (Fig.
3) were identified as significant factors for predicting
cannulation failure in a second ERCP (3 days vs. 2 days, P=0.019,
16 vs. 7, P=0.038, respectively). Table V outlines the multivariate analysis
results of the potential factors predicting cannulation failure of
a second ERCP. Preoperative normal serum bilirubin levels
(OR=9.211, P=0.019) and an interval between the two ERCP procedures
of <3 days (OR=6.765, P=0.041) were identified as significant
predictive factors for cannulation failure of a second ERCP.
 | Table IVResults of univariate analysis for
factors predicting cannulation failure in the second ERCP. |
Table IV
Results of univariate analysis for
factors predicting cannulation failure in the second ERCP.
| Factors | Success (n=47) | Failure (n=9) | P-value |
|---|
| Median age, years
(range) | 68 (18-89) | 66 (23-80) | 0.746 |
| Gender (female),
n | 28 (59.6%) | 5 (55.6%) | >0.999 |
| Normal serum
bilirubin, n | 16 (34%) | 7 (77.8%) | 0.038a |
| Indications,
malignant, n | 22 (46.8%) | 3 (33.3%) | 0.705 |
| Complications after
second ERCP, n | 4 (8.5%) | 1 (11.1%) | >0.999 |
| NKS on the second
ERCP, n | 15 (31.9%) | 6 (66.7%) | 0.143 |
| Days between ERCP,
median (range) | 3 (1-9) | 2 (1-5) | 0.019a |
 | Table VResults of multivariate analysis for
factors predicting cannulation failure in the second ERCP
(unconditional logistic regression). |
Table V
Results of multivariate analysis for
factors predicting cannulation failure in the second ERCP
(unconditional logistic regression).
| Factors | Odds ratio | 95% CI | P-value |
|---|
| Normal serum
bilirubin | 9.211 | 1.446-58.658 | 0.019a |
| Indications,
malignant | 2.765 | 0.485-15.768 | 0.225 |
| NKS on the second
ERCP | 2.698 | 0.414-17.579 | 0.299 |
| Interval between
two ERCP <3 days | 6.765 | 1.086-42.151 | 0.041a |
Discussion
ERCP is now the primary minimally invasive approach
for the diagnosis and treatment of a number of pancreaticobiliary
diseases. Although studies have reported that the cannulation
success rate has increased to 85 to 99% in experienced endoscopists
with needle-knife assistance (22-24),
the topic of selecting an optimal alternative among the multiple
techniques that can be used subsequently following initial ERCP
failure remains attractive. Previous studies have shown that a
second ERCP within a few days is an efficient and safe treatment
for clinically stable patients, with a success rate of 68-79%
(9,10,25-30).
In the present study, the results showed that the overall success
rate was 82.1% (47/56), which supports the feasibility of a second
ERCP.
Repeated attempts often result in papilla edema and
hyperemia, which makes the biliary cannulation more difficult.
However, papilla edema can pathologically be alleviated over time
and performing a second ERCP a few days following the initial
failure may be an appropriate strategy to increase the success
rate. A consensus has not yet been reached regarding the optimal
interval time. Several studies have suggested that the interval
time from the initial failed ERCP to the second one should be
within the first 24-72 h (16,29-34),
while other studies suggested a delayed time of 4-7 days (9,10,25,27).
Only one study revealed that the 4-day interval time was the only
significant factor associated with failure in a second ERCP
(9). In the present study, the
median interval time between the two ERCP procedure was 3 days and
there was a statistically significant difference in the interval
time between the successful and failed groups (3 days vs. 2 days,
P=0.019). It was found by multivariate analysis that an interval
time less than 3 days was closely associated to the second ERCP
failure. According to previous studies, the papilla edema caused by
initial cannulation attempts and cautery always resolves in 3-5
days and the papilla can be detected with a clear appearance
following this period (10,26).
However, in the practical work, it was observed that the mild
edematous papilla at the first 1~2 days was clear enough for
cannulation. Moreover, with the improvement of perioperative
management, patients can recover quickly from the initial
procedure. Thus, there is no need to spend more than 4 days waiting
for the improvement of hyperemia and edema, because there is
evidence showing that the incidence of adverse events might
increase. Since an interval time <1 day is the highest risk
factor reported by most previous studies (10,26,32,33),
the present study suggested that a 2-4 day interval time might be
suitable for most patients with stable clinical conditions.
Currently, a number of advanced cannulation
techniques have been applied that can help to significantly
increase the cannulation success rate. Most previous studies
reported the data of patients who underwent a second ERCP following
the initial failure following precut sphincterotomy (9,10,25-27,31,33,34).
However, both patients with or without initial precut were included
in the present study. One reason for this was that some studies
have reported that in experienced hands, the early implementation
of precut and persistent cannulation attempts have similar overall
cannulation rates and the need for precut sphincterotomy decreased
(4,33,34).
On the other hand, to preserve the function of the sphincter of
Oddi and reduce the incidence of complications where possible, we
did not routinely use the precut technique. The results in the
present study also showed that the initial needle-knife
sphincterotomy was not a risk factor for a second failure
cannulation. It was observed that compared with the first ERCP, the
frequencies of advanced cannulation techniques were increased (30
vs. 39, P=0.036) and the operative time was decreased (65 min vs.
47 min, P<0.001) for the second ERCP. These results might
indicate that it was more conducive to apply the advanced
techniques which would make the procedure easier, than the initial
ERCP.
It is known that difficult biliary cannulation can
increase the risk of post-ERCP adverse events, such as PEP,
cholangitis, bleeding and perforation and contribute to a negative
impact on a variety of clinical outcomes (35,36).
In the present study, severe ERCP-related complications or other
adverse events in relation to the operation delay were not
observed. In addition, following the second ERCP, there was no
significant difference in the incidence of adverse events compared
to the initial procedure. The second ERCP did not increase the
additional risk of adverse events, which was consistent with
previous studies (10,25-29).
Therefore, it is a safe option of performing a second ERCP
following the initial ERCP failed.
When the 30-day mortality of the included patients
was followed up, it was observed that the mortality within 30 days
was higher in the group without a second ERCP than in the group
with a second ERCP. Meanwhile, for all the 6 patients who
succumbed, their indication for ERCP was malignant stricture. The
causes of death were not associated with ERCP. To the authors'
knowledge, most patients with malignant stricture had to receive
palliative biliary drainage when they missed the opportunity for
radical surgery. These patients often died from diseases
progression. In addition, the possible complications associated
with radical surgery could also increase mortality. These results
were similar to some other studies (10,28,37).
The results of the present study meant that successful biliary
access might be a good prognostic factor for malignant patients
within a certain period of time.
At present, our knowledge about failure in a second
ERCP is limited. The likelihood of successful cannulation is
influenced by operator factors (experience) and patient factors
(anatomy), which is stated in the ESGE guidelines for papillary
cannulation (15). In the present
retrospective study, all of the ERCP procedures were performed by
one experienced endoscopist, which may limit possible confounding
factors resulting from the varying skill of the operators. However,
patient factors, including abnormal duodenal papilla, twisting or
stenosis of the distal bile duct, fast bowel motility,
intradivertiucular or peridiverticular papilla and surgically
altered anatomy, usually directly increase the operating
difficulty, which may result in a decreased success rate (5-7,18,38).
The present study found that preoperative normal serum bilirubin
level was a risk factor that correlated with failure in a second
ERCP (OR=6.702, P=0.034) by multivariate analysis. Normal
preoperative serum bilirubin levels always indicate the presence of
a small common bile duct diameter or sphincter of Oddi dysfunction,
which could contribute to difficult cannulation (15,21,39-42).
Meanwhile, for the patients with asymptomatic common bile duct
stones, their bilirubin levels are always normal (43,44).
Generally, a smaller papillary orifice is associated with difficult
cannulation (45). Compared to
symptomatic common bile duct stones, the papillary orifice might be
smaller in asymptomatic common bile duct stones because of low bile
duct pressure secondary to the absence of cholestasis (44). Although previous studies and the
ESGE guidelines for ERCP-related adverse events have stated that
normal serum bilirubin is an independent risk factor for PEP
(35,39,46),
to the best of the authors' knowledge, the relationship between
normal serum bilirubin and unsuccessful outcomes in second ERCP has
not been well reported. Based on the results of the present study,
it is suggested that endoscopists should give careful consideration
to select patients with normal serum bilirubin levels when
performing a second ERCP.
As this was a retrospective nonrandomized study, it
has limitations such as selection bias, a single center, incomplete
data and an insufficient number of patients. Perhaps the one
endoscopist in our center was highly experienced, so the overall
number of initial failure patients was not large enough and it was
also difficult to conduct a prospective randomized study. Other
confounding factors, such as the sizes and morphologies of the
papilla and the duodenum diverticulum, were not included due to
incomplete data. In spite of these limitations the present study
summarized the available data from our database and these results
are meaningful for clinical practice to some extent.
In conclusion, a second ERCP following failure of an
initial biliary cannulation appeared to be safe and effective. For
most clinically stable patients with an unsuccessful initial ERCP,
a second ERCP after 2-4 days may be an optimal strategy.
Preoperative normal serum bilirubin levels may be a risk factor
that can be used for predicting cannulation failure of a second
ERCP procedure.
Acknowledgements
Not applicable.
Funding
Funding: This study was funded by the Basic and Advanced
Research Project of Science and Technology Commission of Chongqing
Municipality (grant no. cstc2018jcyjAX0162).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XD and QW confirm the authenticity of all the raw
data. XD and QW designed the study. CD reviewed the study proposal.
XD, RL and LP collected and analyzed the data. XD, QW and CD
interpreted the results. XD and RL prepared the figures and drafted
the manuscript. QW, LP and CD edited and revised the manuscript.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the ethics committee
of the First Affiliated Hospital of Chongqing Medical University
(approval no. 2020-668). Informed consent was obtained from all
subjects involved in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee YS, Cho CM, Cho KB, Heo J, Jung MK,
Kim SB, Kim KH, Kim TN, Lee DW, Han J, et al: Difficult biliary
cannulation from the perspective of post-endoscopic retrograde
cholangiopancreatography pancreatitis: Identifying the optimal
timing for the rescue cannulation technique. Gut Liver. 15:459–465.
2021.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
Nakai Y, Isayama H, Sasahira N, Kogure H,
Sasaki T, Yamamoto N, Saito K, Umefune G, Akiyama D, Kawahata S, et
al: Risk factors for post-ERCP pancreatitis in wire-guided
cannulation for therapeutic biliary ERCP. Gastrointest Endosc.
81:119–126. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chen Q, Jin P, Ji X, Du H and Lu J:
Management of difficult or failed biliary access in initial ERCP: A
review of current literature. Clin Res Hepatol Gastroenterol.
43:365–372. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cennamo V, Fuccio L, Zagari RM, Eusebi LH,
Ceroni L, Laterza L, Fabbri C and Bazzoli F: Can early precut
implementation reduce endoscopic retrograde
cholangiopancreatography-related complication risk? Meta-analysis
of randomized controlled trials. Endoscopy. 42:381–388.
2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Williams EJ, Ogollah R, Thomas P, Logan
RF, Martin D, Wilkinson ML and Lombard M: What predicts failed
cannulation and therapy at ERCP? Results of a large-scale
multicenter analysis. Endoscopy. 44:674–683. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Altonbary AY and Bahgat MH: Endoscopic
retrograde cholangiopancreatography in periampullary diverticulum:
The challenge of cannulation. World J Gastrointest Endosc.
8:282–287. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Krutsri C, Kida M, Yamauchi H, Iwai T,
Imaizumi H and Koizumi W: Current status of endoscopic retrograde
cholangiopancreatography in patients with surgically altered
anatomy. World J Gastroenterol. 25:3313–3333. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
ASGE Technology Committee. Enestvedt BK,
Kothari S, Pannala R, Yang J, Fujii-Lau LL, Hwang JH, Konda V,
Manfredi M, Maple JT, et al: Devices and techniques for ERCP in the
surgically altered GI tract. Gastrointest Endosc. 83:1061–1075.
2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Colan-Hernandez J, Aldana A, Concepción M,
Chavez K, Gómez C, Mendez-Bocanegra A, Martínez-Guillen M, Sendino
O, Villanueva C, Llach J, et al: Optimal timing for a second ERCP
after failure of initial biliary cannulation following precut
sphincterotomy: An analysis of experience at two tertiary centers.
Surg Endosc. 31:3711–3717. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pavlides M, Barnabas A, Fernandopulle N,
Bailey AA, Collier J, Phillips-Hughes J, Ellis A, Chapman R and
Braden B: Repeat endoscopic retrograde cholangiopancreaticography
after failed initial precut sphincterotomy for biliary cannulation.
World J Gastroenterol. 20:13153–13158. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bokemeyer A, Muller F, Niesert H, Brückner
M, Bettenworth D, Nowacki T, Beyna T, Ullerich H and Lenze F:
Percutaneous-transhepatic-endoscopic rendezvous procedures are
effective and safe in patients with refractory bile duct
obstruction. United European Gastroenterol J. 7:397–404.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lorenz JM: Management of malignant biliary
obstruction. Semin Intervent Radiol. 33:259–267. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Abbas AM, Strong AT, Diehl DL, Brauer BC,
Lee IH, Burbridge R, Zivny J, Higa JT, Falcão M, El Hajj II, et al:
Multicenter evaluation of the clinical utility of
laparoscopy-assisted ERCP in patients with Roux-en-Y gastric
bypass. Gastrointest Endosc. 87:1031–1039. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Huang RJ, Thosani NC, Barakat MT,
Choudhary A, Mithal A, Singh G, Sethi S and Banerjee S: Evolution
in the utilization of biliary interventions in the United States:
Results of a nationwide longitudinal study from 1998 to 2013.
Gastrointest Endosc. 86:319–326.e5. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Testoni PA, Mariani A, Aabakken L,
Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M,
Dumonceau JM, Giovannini M, et al: Papillary cannulation and
sphincterotomy techniques at ERCP: European society of
gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy.
48:657–683. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Liao WC, Angsuwatcharakon P, Isayama H,
Dhir V, Devereaux B, Khor CJ, Ponnudurai R, Lakhtakia S, Lee DK,
Ratanachu-Ek T, et al: International consensus recommendations for
difficult biliary access. Gastrointest Endosc. 85:295–304.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Haraldsson E, Kylänpää L, Grönroos J,
Saarela A, Toth E, Qvigstad G, Hult M, Lindström O, Laine S,
Karjula H, et al: Macroscopic appearance of the major duodenal
papilla influences bile duct cannulation: A prospective multicenter
study by the scandinavian association for digestive endoscopy study
group for ERCP. Gastrointest Endosc. 90:957–963. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chen PH, Tung CF, Peng YC, Yeh HZ, Chang
CS and Chen CC: Duodenal major papilla morphology can affect
biliary cannulation and complications during ERCP, an observational
study. BMC Gastroenterol. 20(310)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
ASGE Training Committee. Jorgensen J,
Kubiliun N, Law JK, Al-Haddad MA, Bingener-Casey J, Christie JA,
Davila RE, Kwon RS, Obstein KL, et al: Endoscopic retrograde
cholangiopancreatography (ERCP): Core curriculum. Gastrointest
Endosc. 83:279–289. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wani S, Han S, Simon V, Hall M, Early D,
Aagaard E, Abidi WM, Banerjee S, Baron TH, Bartel M, et al: Setting
minimum standards for training in EUS and ERCP: Results from a
prospective multicenter study evaluating learning curves and
competence among advanced endoscopy trainees. Gastrointest Endosc.
89:1160–1168.e9. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
ASGE Standards of Practice Committee.
Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D,
Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, et al: Adverse
events associated with ERCP. Gastrointest Endosc. 85:32–47.
2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Williams EJ, Taylor S, Fairclough P,
Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson M,
Williamson PR, et al: Are we meeting the standards set for
endoscopy? Results of a large-scale prospective survey of
endoscopic retrograde cholangio-pancreatograph practice. Gut.
56:821–829. 2007.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Jin YJ, Jeong S and Lee DH: Utility of
needle-knife fistulotomy as an initial method of biliary
cannulation to prevent post-ERCP pancreatitis in a highly selected
at-risk group: A single-arm prospective feasibility study.
Gastrointest Endosc. 84:808–813. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Fiocca F, Fanello G, Cereatti F, Maselli
R, Ceci V and Donatelli G: Early ‘shallow’ needle-knife papillotomy
and guidewire cannulation: An effective and safe approach to
difficult papilla. Therap Adv Gastroenterol. 8:114–120.
2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kevans D, Zeb F, Donnellan F, Courtney G
and Aftab AR: Failed biliary access following needle knife
fistulotomy: Is repeat interval ERCP worthwhile? Scand J
Gastroenterol. 45:1238–1241. 2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kim J, Ryu JK, Ahn DW, Park JK, Yoon WJ,
Kim YT and Yoon YB: Results of repeat endoscopic retrograde
cholangiopancreatography after initial biliary cannulation failure
following needle-knife sphincterotomy. J Gastroenterol Hepatol.
27:516–520. 2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Donnellan F, Enns R, Kim E, Amar J,
Telford J and Byrne MF: Outcome of repeat ERCP after initial failed
use of a needle knife for biliary access. Dig Dis Sci.
57:1069–1071. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lo MH, Lin CH, Wu CH, Tsou YK, Lee MH,
Sung KF and Liu NJ: Management of biliary diseases after the
failure of initial needle knife precut sphincterotomy for biliary
cannulation. Sci Rep. 11(14968)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Peñaloza Ramírez A, Rodríguez Tello D,
Murillo Arias A, Barreto Pérez J and Aponte Ordóñez P: Endoscopic
retrograde cholangiopancreatography results three days after a
failed pre-cut. Rev Esp Enferm Dig. 113:486–489. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Flumignan VK, Seike MG, Souza VS,
Cirqueira MI, Silva AB and Artifon ELA: Difficult biliary
cannulation: Should we always try a second ercp after a failed
needle-knife fistulotomy? Arq Gastroenterol. 58:509–513.
2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kaffes AJ, Sriram PV, Rao GV, Santosh D
and Reddy DN: Early institution of pre-cutting for difficult
biliary cannulation: A prospective study comparing conventional vs.
a modified technique. Gastrointest Endosc. 62:669–674.
2005.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ang TL, Kwek AB, Lim KB, Teo EK and Fock
KM: An analysis of the efficacy and safety of a strategy of early
precut for biliary access during difficult endoscopic retrograde
cholangiopancreatography in a general hospital. J Dig Dis.
11:306–312. 2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Harewood GC and Baron TH: An assessment of
the learning curve for precut biliary sphincterotomy. Am J
Gastroenterol. 97:1708–1712. 2002.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Akaraviputh T, Lohsiriwat V, Swangsri J,
Methasate A, Leelakusolvong S and Lertakayamanee N: The learning
curve for safety and success of precut sphincterotomy for
therapeutic ERCP: A single endoscopist's experience. Endoscopy.
40:513–516. 2008.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Dumonceau JM, Kapral C, Aabakken L,
Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro
M, Hritz I, Mariani A, et al: ERCP-related adverse events: European
society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy.
52:127–149. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Fung BM, Pitea TC and Tabibian JH:
Difficult biliary cannulation in endoscopic retrograde
cholangiopancreatography: Definitions, risk factors, and
implications. Eur Med J Hepatol. 9:64–72. 2021.PubMed/NCBI
|
|
37
|
Halttunen J, Meisner S, Aabakken L, Arnelo
U, Grönroos J, Hauge T, Kleveland PM, Nordblad Schmidt P, Saarela
A, Swahn F, et al: Difficult cannulation as defined by a
prospective study of the scandinavian association for digestive
endoscopy (SADE) in 907 ERCPs. Scand J Gastroenterol. 49:752–758.
2014.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Watanabe M, Okuwaki K, Kida M, Imaizumi H,
Yamauchi H, Kaneko T, Iwai T, Hasegawa R, Miyata E, Masutani H, et
al: Transpapillary biliary cannulation is difficult in cases with
large oral protrusion of the duodenal papilla. Dig Dis Sci.
64:2291–2299. 2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Freeman ML, DiSario JA, Nelson DB,
Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna
GS, et al: Risk factors for post-ERCP pancreatitis: A prospective,
multicenter study. Gastrointest Endosc. 54:425–434. 2001.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Saito H, Kadono Y, Shono T, Kamikawa K,
Urata A, Nasu J, Imamura H, Matsushita I, Kakuma T and Tada S:
Factors predicting difficult biliary cannulation during endoscopic
retrograde cholangiopancreatography for common bile duct stones.
Clin Endosc: Nov 12, 2021 (Epub ahead of print).
|
|
41
|
Zhou PH, Yao LQ, Xu MD, Zhong YS, Gao WD,
He GJ, Zhang YQ, Chen WF and Qin XY: Application of needle-knife in
difficult biliary cannulation for endoscopic retrograde
cholangiopancreatography. Hepatobiliary Pancreat Dis Int.
5:590–594. 2006.PubMed/NCBI
|
|
42
|
Lopes L, Canena J, Fernandes J, Moreira M,
Costa I, Gomes-Fonseca J, Araújo T, Alexandrino G, Lourenço L,
Horta D, et al: Should we use papilla morphology to estimate the
size of the terminal common bile duct during endoscopic retrograde
cholangiopancreatography? Eur J Gastroenterol Hepatol. 32:181–186.
2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Xiao L, Geng C, Li X, Li Y and Wang C:
Comparable safety of ERCP in symptomatic and asymptomatic patients
with common bile duct stones: A propensity-matched analysis. Scand
J Gastroenterol. 56:111–117. 2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Kadokura M, Takenaka Y, Yoda H, Yasumura
T, Okuwaki T, Tanaka K and Amemiya F: Asymptomatic common bile duct
stones are associated with increased risk of post-endoscopic
retrograde cholangiopancreatography pancreatitis. JMA J. 4:141–147.
2021.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Kuo CM, Chiu YC, Changchien CS, Tai WC,
Chuah SK, Hu TH, Kuo YH and Kuo CH: Endoscopic papillary balloon
dilation for removal of bile duct stones: Evaluation of outcomes
and complications in 298 patients. J Clin Gastroenterol.
46:860–864. 2012.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Testoni PA, Mariani A, Giussani A, Vailati
C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N and
Mutignani M: , et al: Risk factors for post-ERCP
pancreatitis in high- and low-volume centers and among expert and
non-expert operators: A prospective multicenter study. Am J
Gastroenterol. 105:1753–1761. 2010.PubMed/NCBI View Article : Google Scholar
|