Introduction
Giant condyloma acuminatum (GCA), also known as
Buschke-Löwenstein tumor (BLT), represents an infrequent sexually
transmitted disease (STD) triggered most frequently by HPV (human
papilloma virus) 6 and 11(1), and
exceptionally 16 and 18 (2,3), having common risk factors with
condyloma acuminatum (including multiple partners, prostitution,
men having sex with men, poor hygiene as well as other STDs)
(1,4,5).
BLT is always preceded by condyloma acuminatum, with
certain authors considering that it is the midway between condyloma
acuminatum and squamous cell carcinoma, and the malignant
transformation risk is 40-60% (4,6). It is
associated with the immunosuppressive status: Congenital or
acquired immunodeficiencies, diabetes mellitus, alcoholism,
chemotherapy, immunosuppressive therapy (7).
BLT may occur at any age, particularly after
puberty. Men are more affected than women, usually between 30 and
50 years old, with a male/female sex ratio of 3:1. The general
incidence in the US is 0.1%, similar with the one from the
developed countries in Europe (4).
It is considered that almost everyone will manifest a minimum of
one HPV infection during their lifetime, often asymptomatic,
transient, spontaneously resolved, without being aware of it and 2%
will develop condyloma acuminata (8).
Clinically, it presents as an exophytic, vegetative
tumor, frequently cauliflower-like, white-yellowish, slowly or
rapidly growing depending on the immune status of the patient, that
may invade and destroy the surrounding tissue, without spontaneous
resolution (1,9). The risk of distant metastases is low
(6). In 81-94% of the cases, the
lesion is located on the penis. The anorectal area is affected in
10-17% of the cases and the urethra in 5% of the cases. In females,
the vulva is generally the most affected, in 90% of the cases,
while the anorectal location is less frequent (4). From a histopathological perspective,
the hyperplastic epithelium is well-differentiated, with
hyperkeratosis, parakeratosis, koilocytes, a bulging granular
layer, papillomatosis and minimal atypia (1,9).
The treatment is classified into topical therapy
(podophyllin, 5-FU, radiotherapy), excisional therapy
(CO2 laser, cryotherapy, electrotherapy, surgery) and
immunotherapy (imiquimod). A rather new therapy to be considered is
the photodynamic therapy, that uses aminolevulinic acid
hydrochloride; photosensitizers have been revealed to have
antiviral action (1). The
association with invasive genital carcinoma, as well as its
aggressive character, require multidisciplinary collaboration,
including colonoscopy for the rectal invasion (10). Selecting the right treatment option
depends on the tumor characteristics and on the skills of the
physician, with surgical treatment remaining as the first line
therapy, with a lower recurrence risk (3,4). If
the tumors are invasive, the patients could require a colostomy and
nephrostomy (10).
Case reports
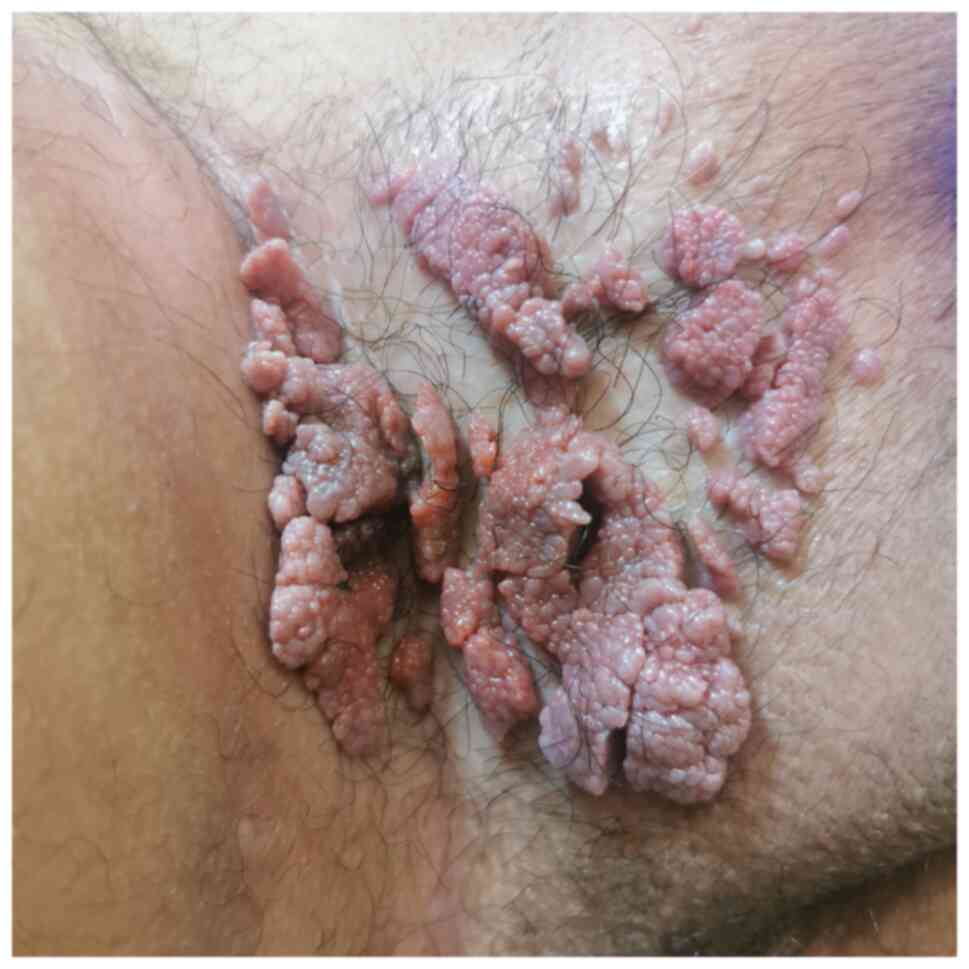
Case 1
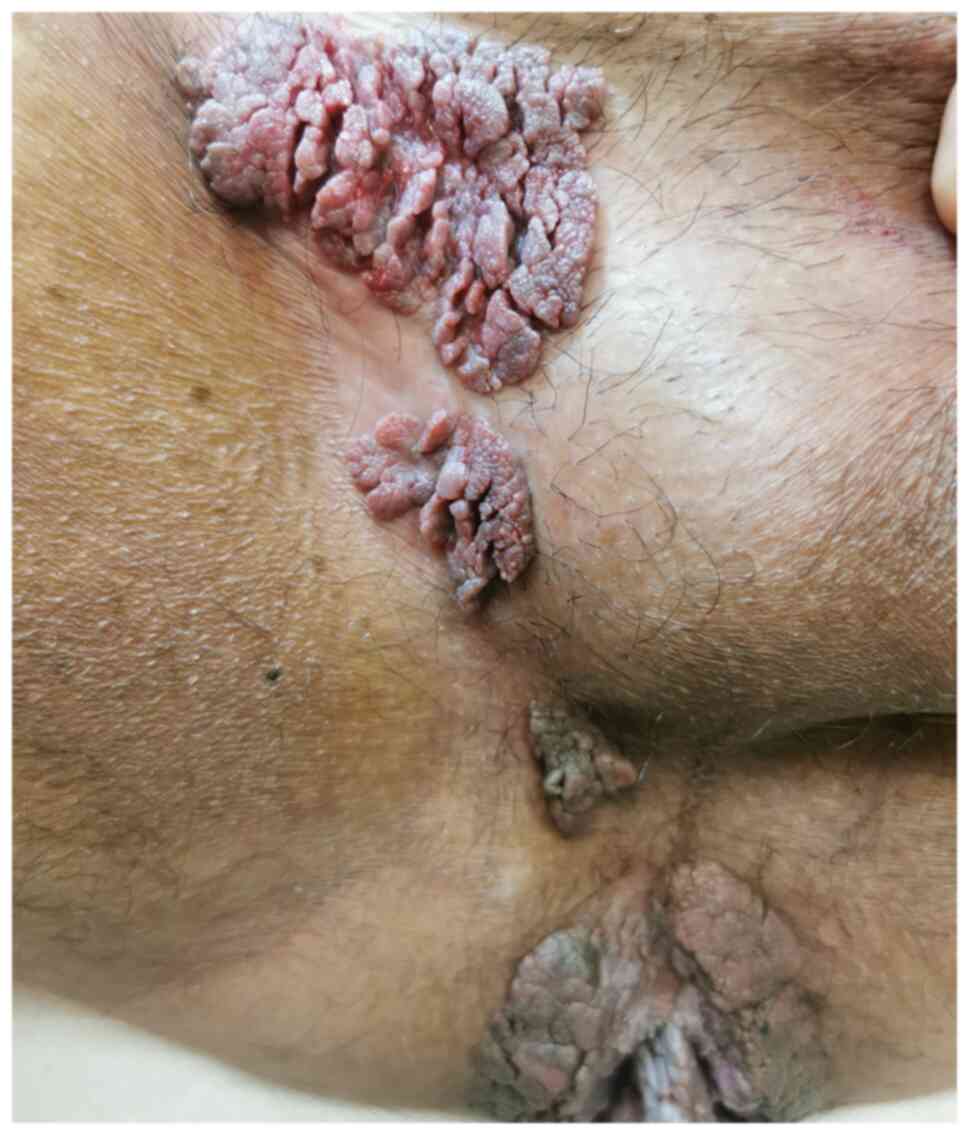
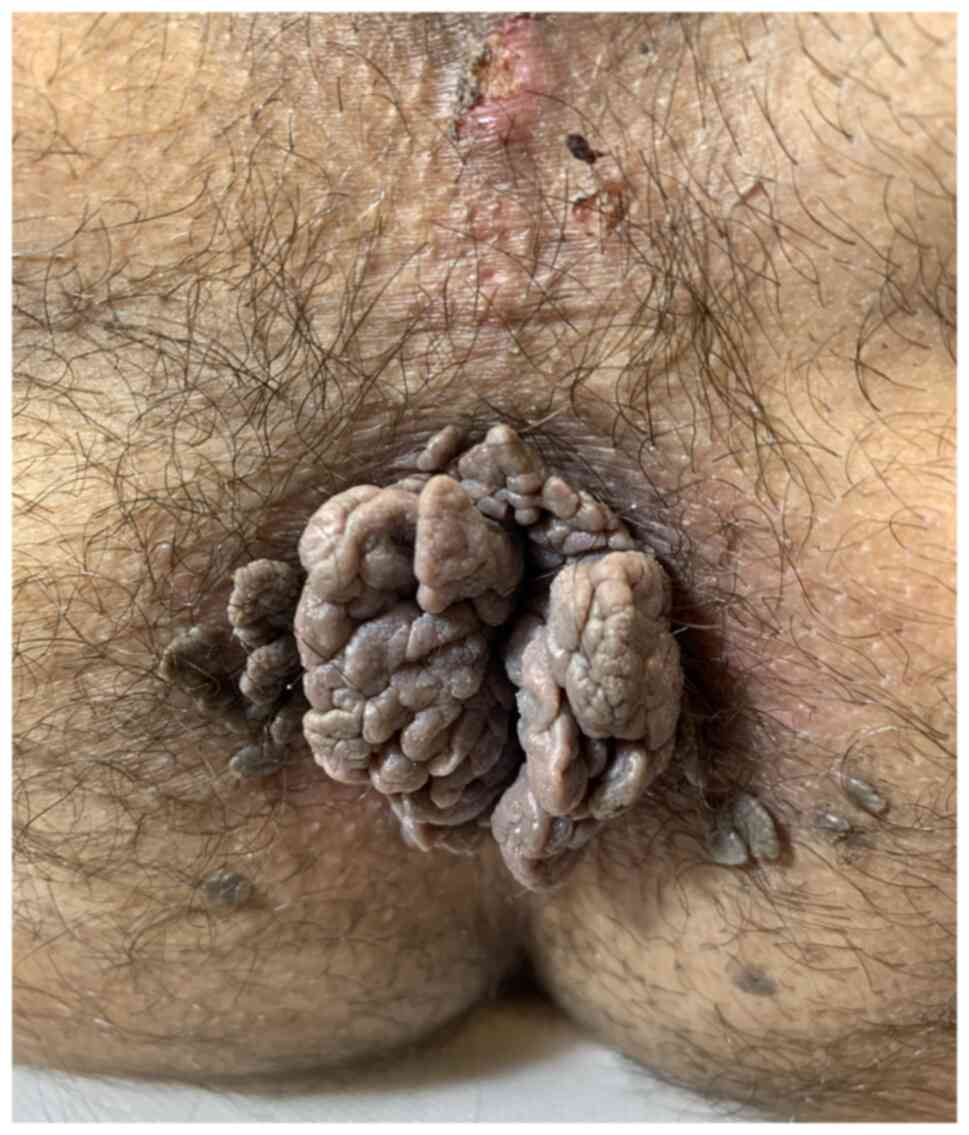
A 39-year-old male patient with no notable medical
history, smoker, and sexual intercourse debut at 15 years old,
presented to the Department of Dermatology of Ponderas Academic
Hospital for a large exophytic cauliflower-like verrucous tumor in
the perianal area and smaller similar lesions localized in the
genital, supra-penile, scrotal and crural areas. The patient was
negative for STDs and the genotyping was positive for HPV 16. The
colonoscopy revealed no rectal invasion and the patient refused a
colostomy.
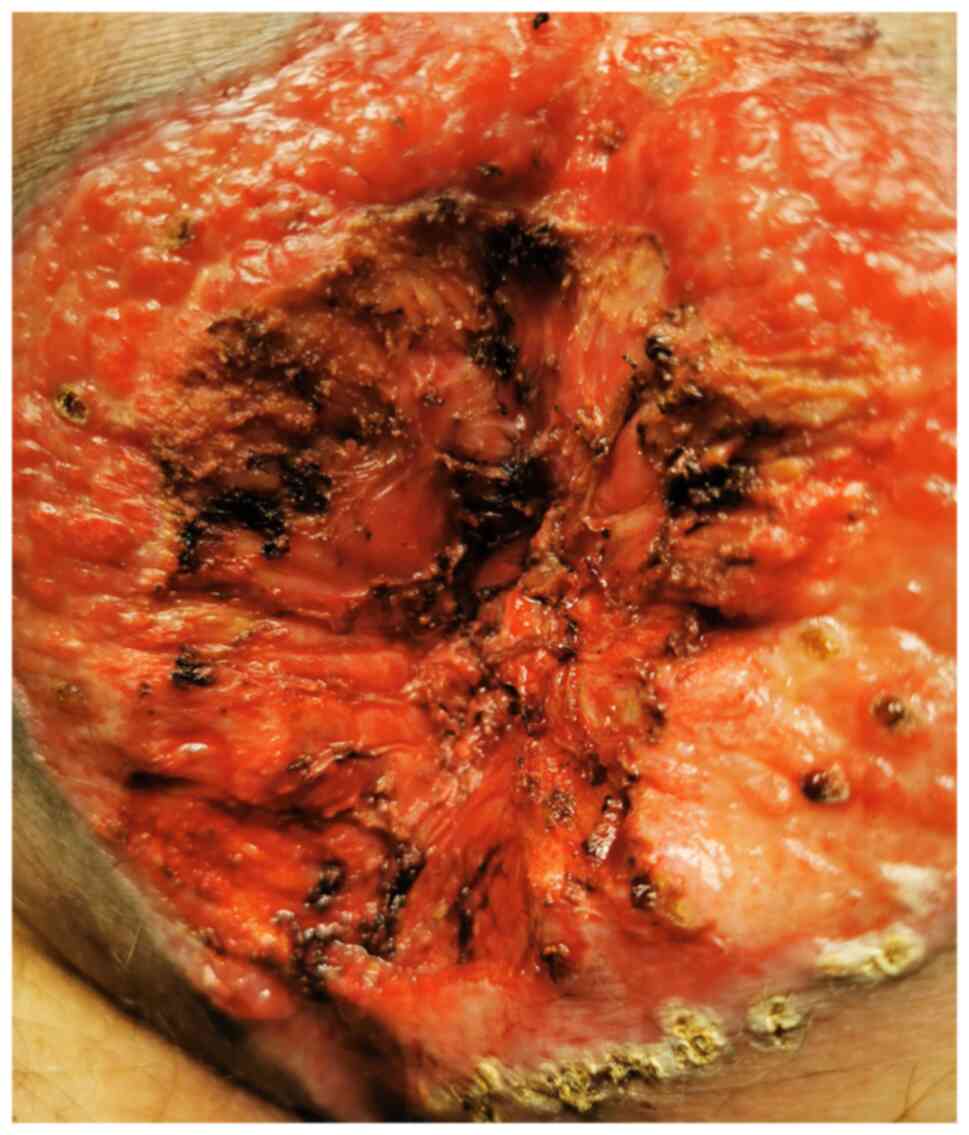
A reduction of the tumor volume was performed with
radiosurgical excision under general anesthesia and all the smaller
lesions were excised in 10 sessions of CO2 laser under
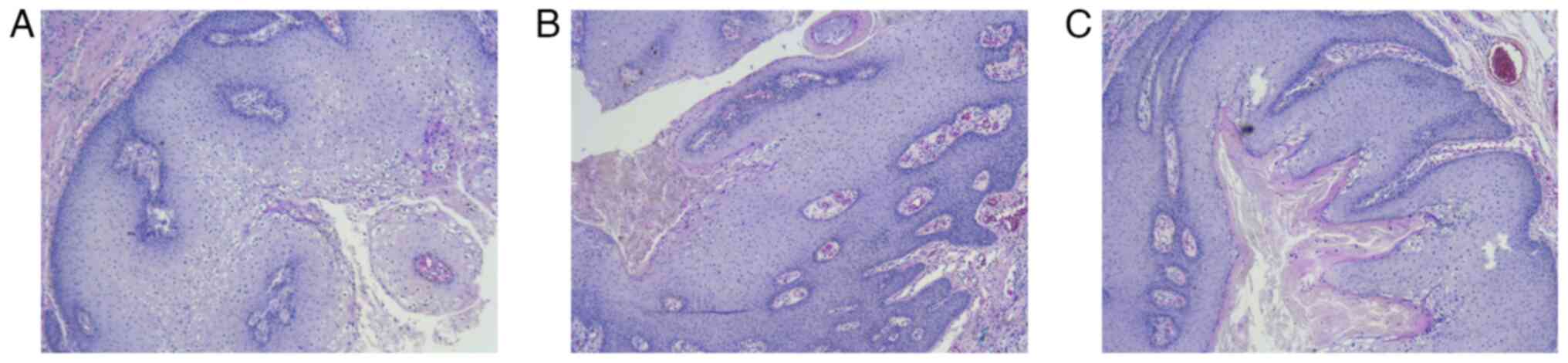
local anesthesia. The histopathological report revealed epidermal
hyperplasia, hyperkeratosis, papillomatosis, koilocytes, HPV
6-positive intra-tissue and no signs of malignant
transformation.
The healing occurred by secondary intention, in 60
days. The patient received systemic antibiotic therapy with
levofloxacin (500 mg/day for 15 days), then cefuroxime (1 g twice a
day for 3 weeks), local and intrarectal sinecatechins (twice a day
for 4 months), nonspecific immune stimulation with inosine pranobex
(3 tablets twice a day for 10 days per month), alternately with
Coriolus versicolor (3 tablets twice a day for 4 months).
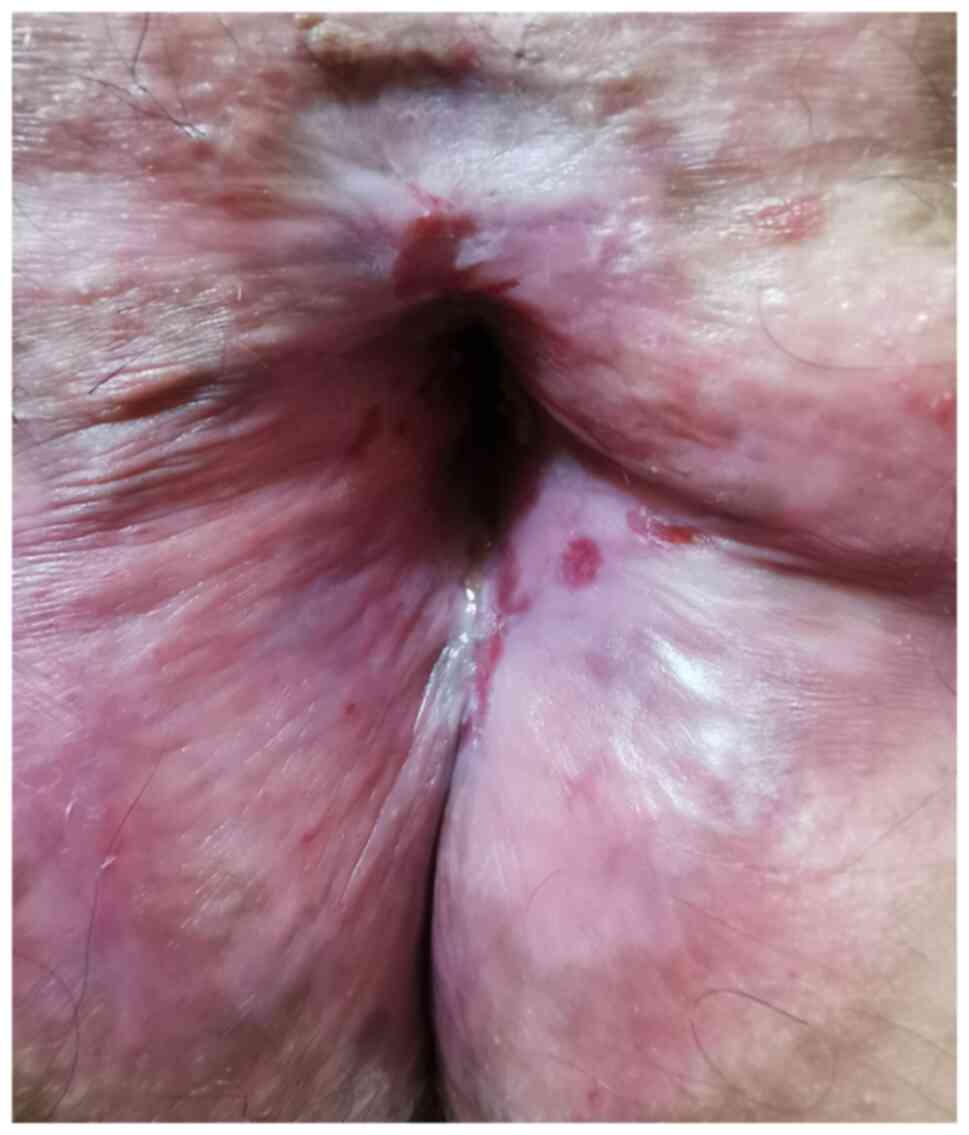
The peniscopy and the microscopic examination of the anogenital
region revealed residual subclinical lesions. They were excised
with CO2 laser, 3 sessions of fractional photodynamic
therapy with 8% levulinic acid applied topically under occlusion
for 2 h, then 20 min of 635-nm red light at 70 mJ/cm2
fluency, followed by 10 min of 411-nm blue light at 80
mF/cm2 fluency, and finally 10 min of 635-nm red light
at 70 mJ/cm2 fluency. A total of 3 doses of Gardasil
vaccine were administered (months 0-2-6) (Fig. 1, Fig.
2, Fig. 3, Fig. 4, Fig.
5, Fig. 6 and Fig. 7).
Case 2
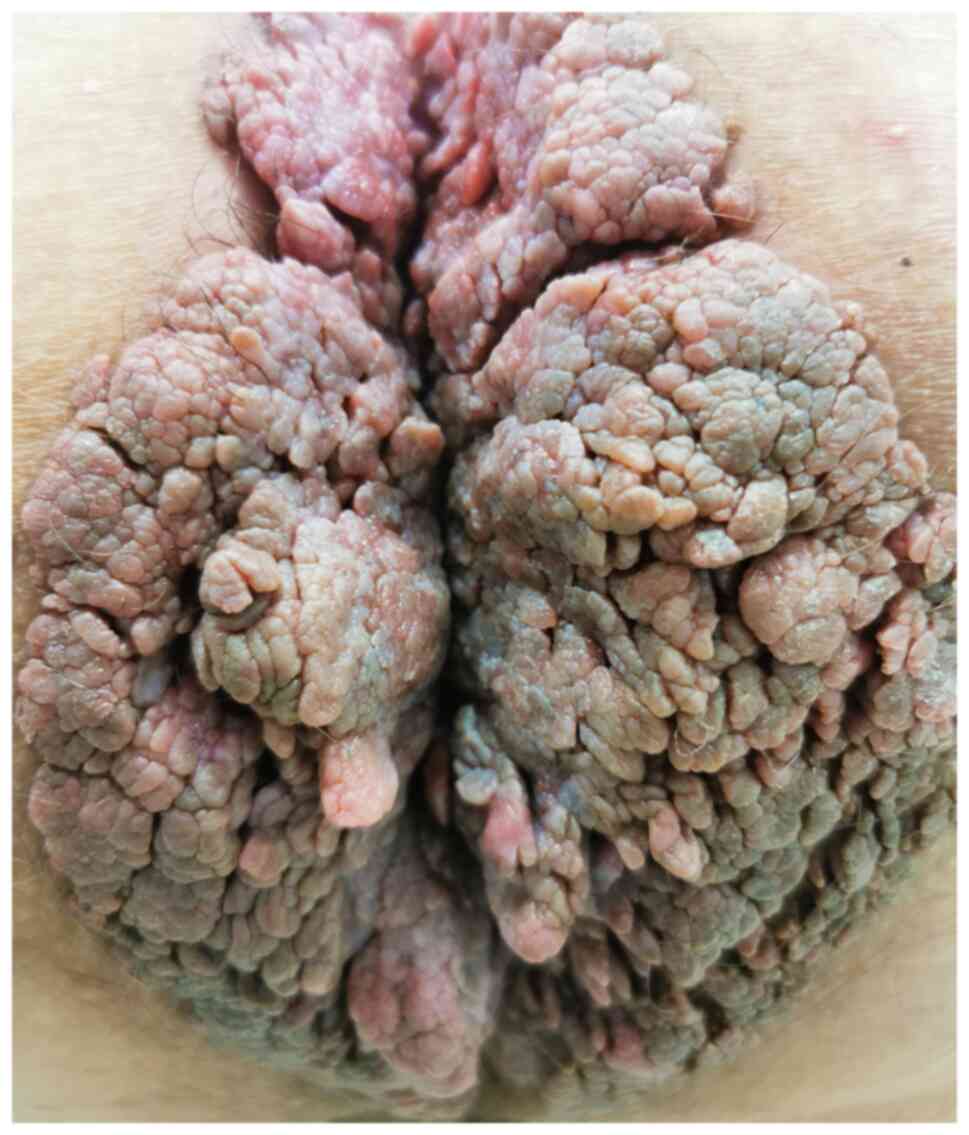
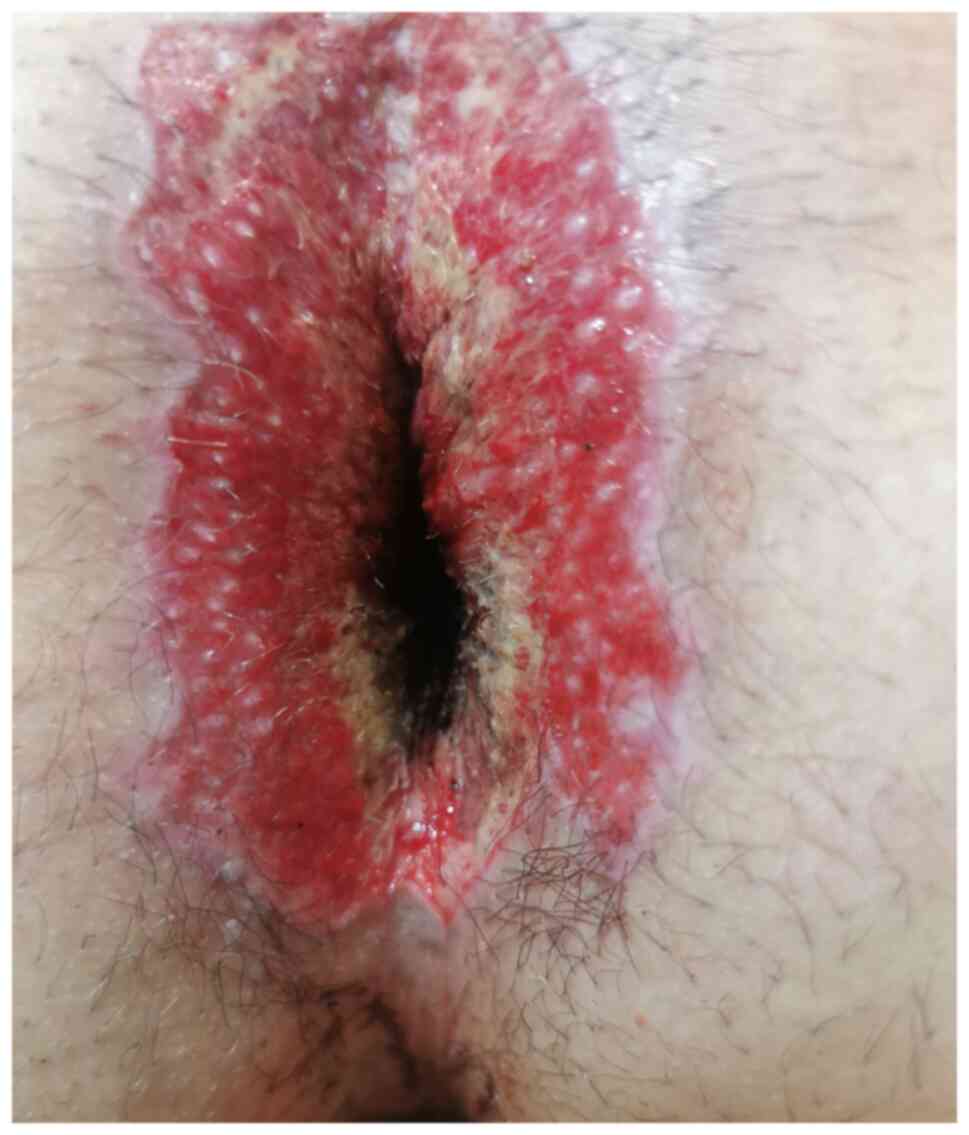
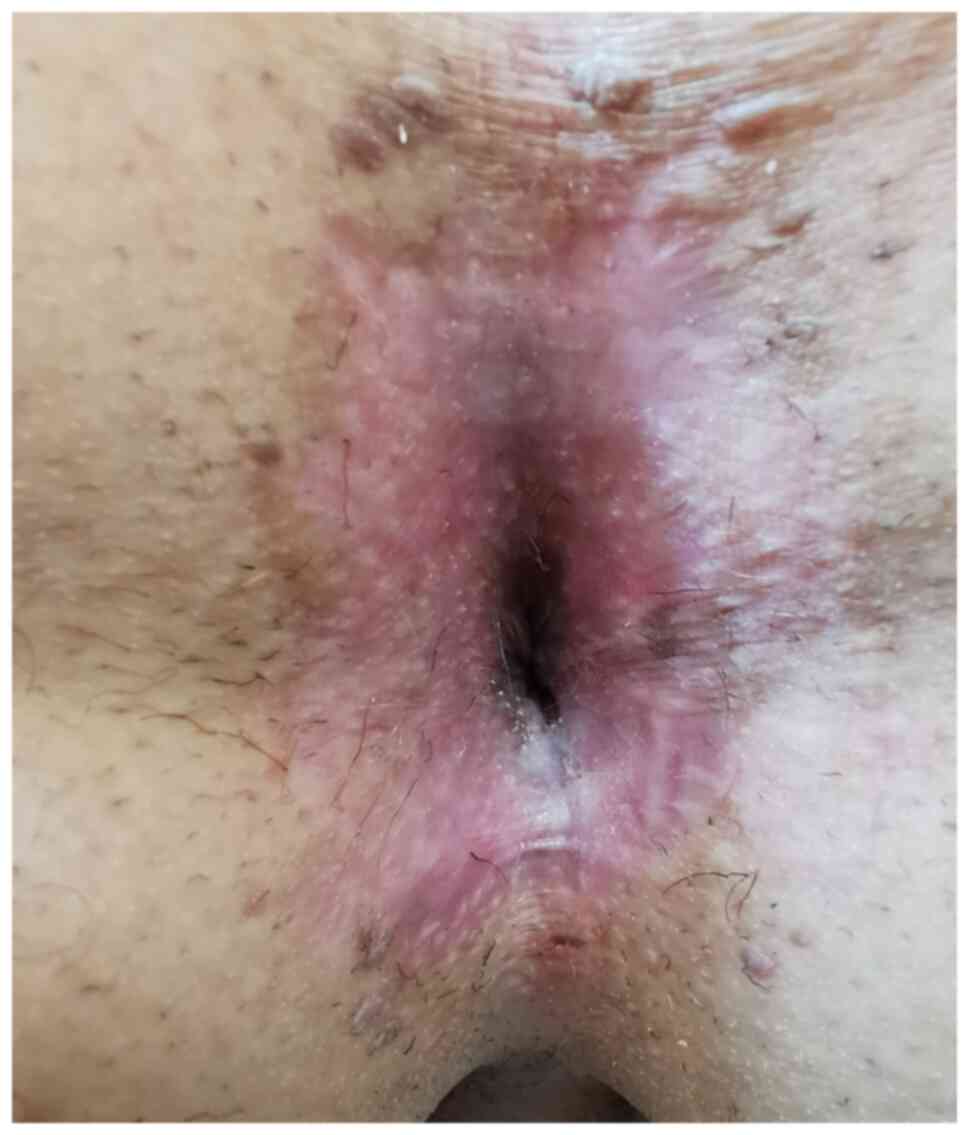
A 26-year-old male homosexual patient, smoker,
sexual intercourse debut at 15 years old, and multiple sexual
partners, presented to the Department of Dermatology of Ponderas
Academic Hospital for a large exophytic cauliflower-like verrucous
tumor in the perianal area. The patient had asymptomatic urethral
co-infection with Haemophilus influenzae, was negative for
STDs and the intra-anal and intra-urethral genotyping was positive
for HPV 6 and 16. The colonoscopy revealed no rectal invasion.
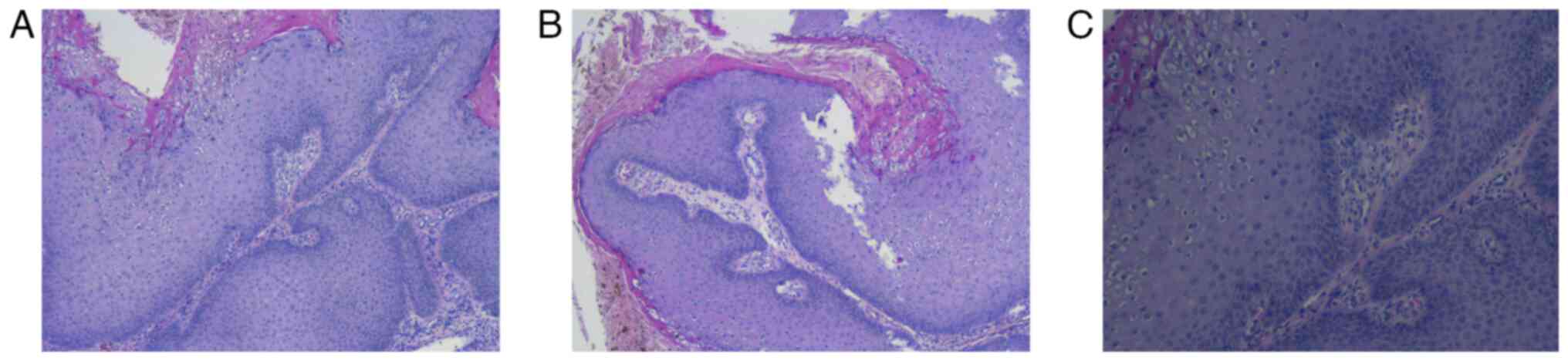
The peniscopy and the microscopic examination of the
anogenital region revealed 30 subclinical genital, supra-penile and
crural lesions, which were excised with CO2 laser in 4
sessions under local anesthesia. The histopathological report
revealed epidermal hyperplasia, hyperkeratosis, papillomatosis,
koilocytes and HPV 6-positive intra-tissue.
The patient received local and intrarectal
sinecatechins (twice a day for 4 months), inosine pranobex (3
tablets twice a day, 10 days per month) alternately with
Coriolus versicolor (3 tablets twice a day for 4 months).
The peniscopy and the microscopic examination of the anogenital
region revealed residual subclinical lesions that were excised with
CO2 laser, 3 sessions of fractional photodynamic therapy
with 8% levulinic acid applied topically under occlusion for 2 h,
then 20 min of 635-nm red light at 70 mJ/cm2 fluency,
followed by 10 min of 41-nm blue light at 80 mF/cm2
fluency, and finally 10 min of 635-nm red light at 70
mJ/cm2 fluency. A total of 3 doses of Gardasil vaccine
were administered (months 0-2-6) (Fig.
8, Fig. 9, Fig. 10, Fig.
11 and Fig. 12).
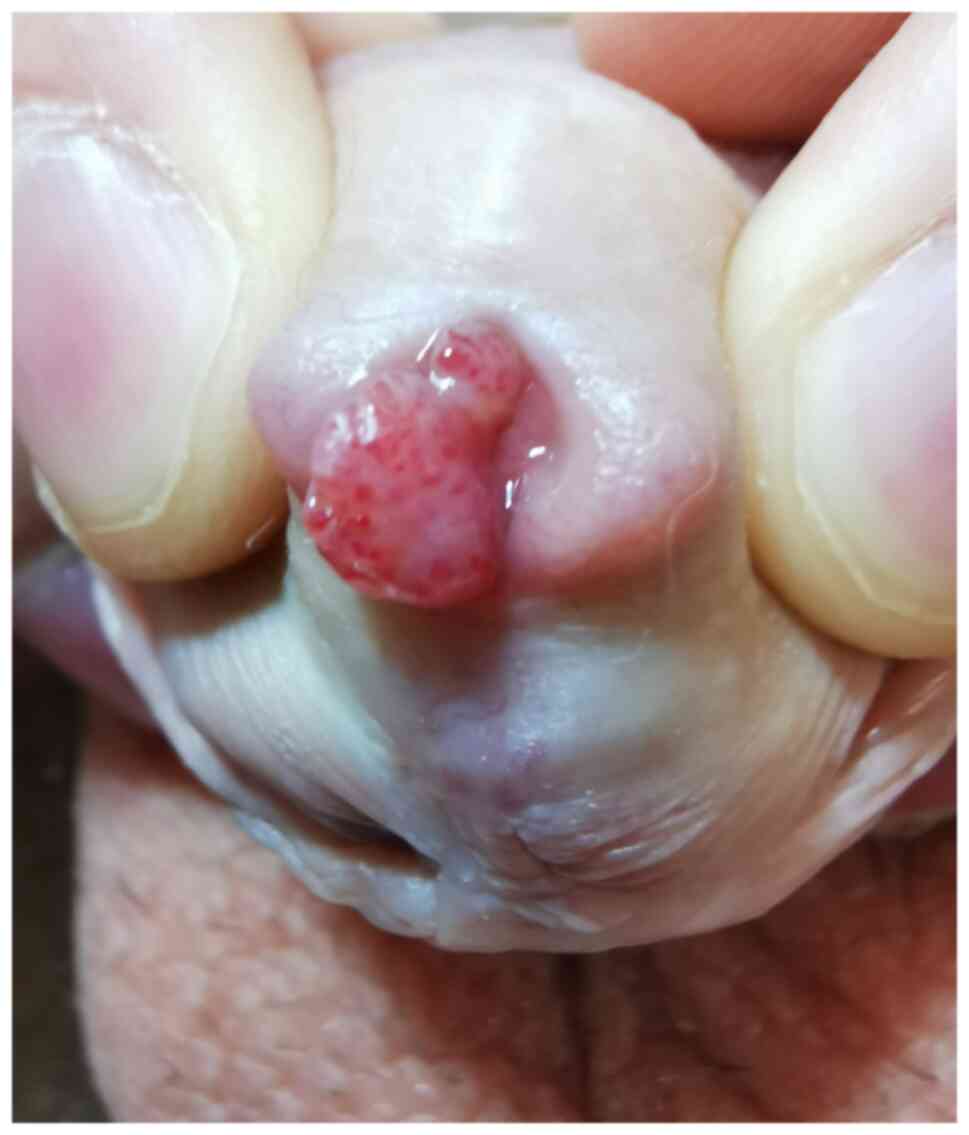
Case 3
A 24-year-old male patient, smoker, and sexual
intercourse debut at 14 years, consulted us at the Deparment of
Dermatology of Ponderas Academic Hospital for a vegetative,
exophytic, intra-urethral tumor. The patient had asymptomatic
urethral co-infection with Ureaplasma urealiticum and
Klebsiella pneumoniae. The intra-urethral genotyping was
positive for HPV 16 and 52.
The peniscopy and the microscopic examination of the
anogenital region revealed 10 subclinical genital lesions and 15
subclinical lesions supra-penile and perigenital, which were
excised in one session of CO2 laser under local
anesthesia.
The patient received systemic antibiotherapy with
levofloxacin (500 mg/day for 30 days), meloxicam (15 mg/day for 30
days), Sunvert (1 tablet twice a day for 60 days), local and
intrarectal sinecatechins (twice a day for 4 months), inosine
pranobex (3 tablets twice a day for 10 days per month), alternately
with Coriolus versicolor (3 tablets twice a day for 4
months). The peniscopy and the microscopic examination of the
anogenital region revealed residual subclinical lesions, which were
excised with CO2 laser, 2 sessions of fractional
photodynamic therapy with 8% levulinic acid applied topically under
occlusion for 2 h, then 20 min of 635-nm red light at 70
mJ/cm2 fluency, followed by 10 min of 411-nm blue light
at 80 mF/cm2 fluency, and finally 10 min of 635-nm red
light at 70 mJ/cm2 fluency. A total of 3 doses of
Gardasil vaccine were administered (months 0-2-6) (Fig. 13).
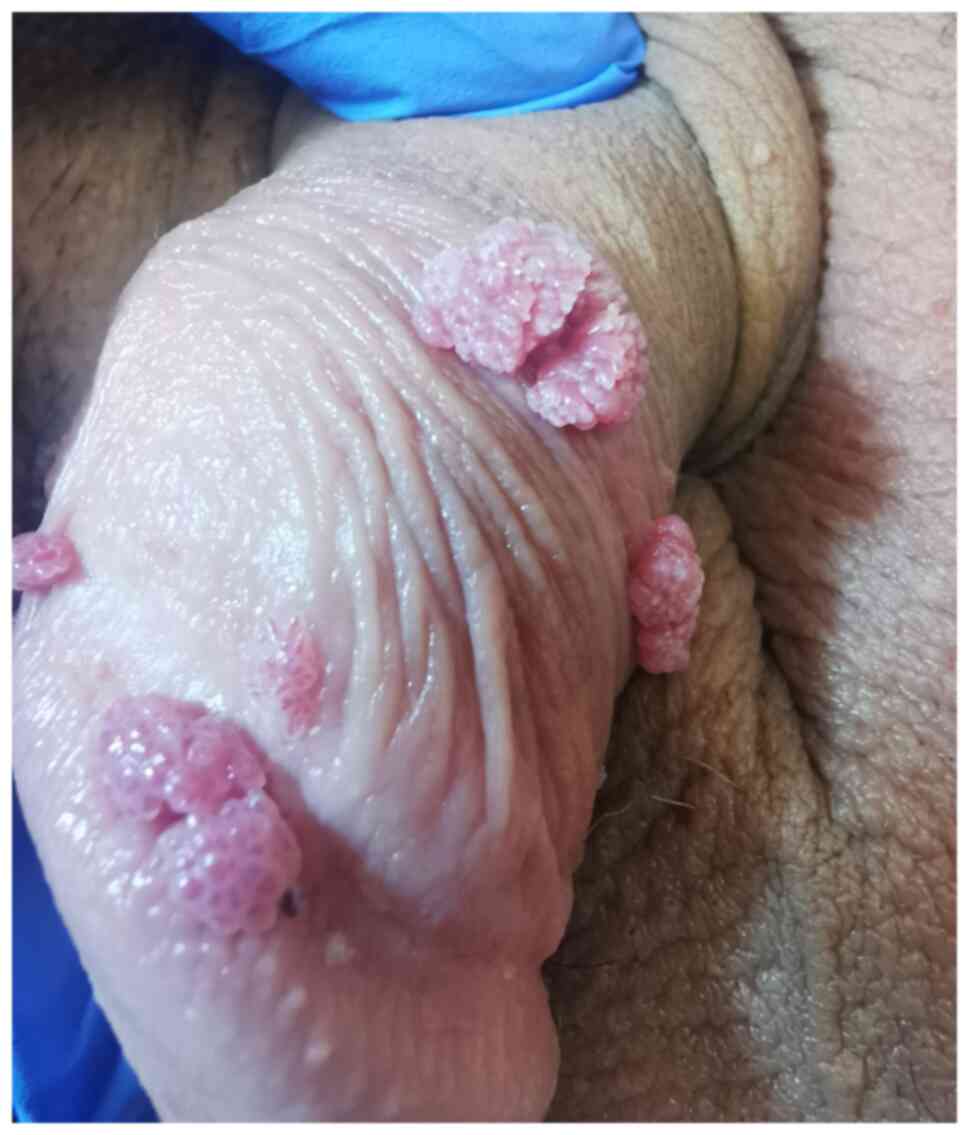
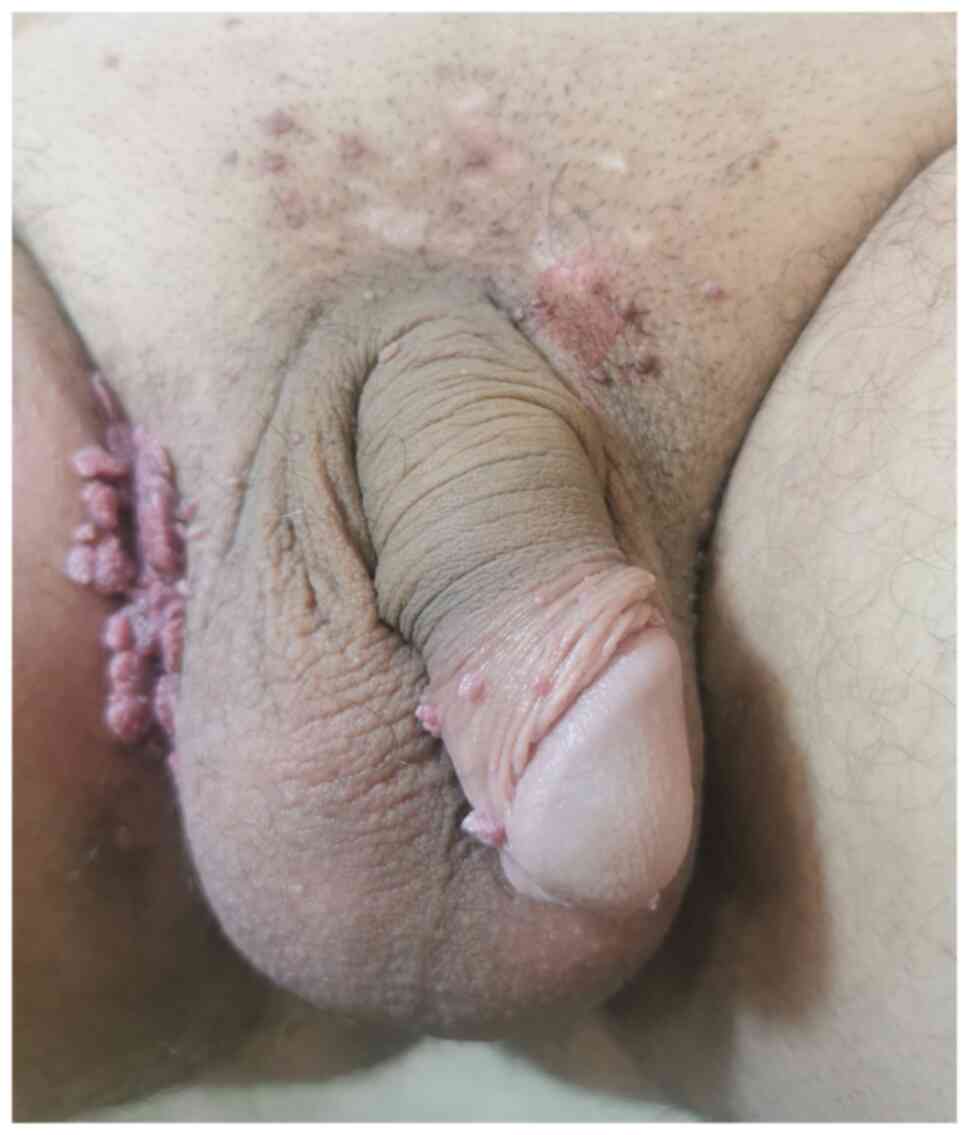
Case 4
A 32-year-old uncircumcised male patient presented
to the Department of Dermatology of Ponderas Academic Hospital for
multiple, giant flesh-colored, cauliflower-like growths involving
the penis, the supra-penile and the right inguinal region. The
patient denied experiencing pain, bleeding or dysuria. The patient
had been sexually active since 16 years old and provided history of
multiple sexual partners. Laboratory tests were performed in order
to verify the status of the patient for STDs and the patient tested
positive for an asymptomatic urethral coinfection with
Mycoplasma hominis. The HPV genotyping revealed HPV 6, 11
and 54.
The treatment consisted of 5 sessions of
CO2 laser with local anesthesia, followed by 2 daily
applications of sinecatechins ointment for 4 consecutive months in
the affected areas. In addition, the patient was prescribed inosine
pranobex (500 mg x 6/day, 10 days/month for 4 months), alternating
with Coriolus versicolor (6 cps/day 20 days/month for 4
months). The patient was advised to get vaccinated against HPV with
3 shots of Gardasil 9 vaccine.
At the follow-up visit, the microscopic analysis of
the genital skin revealed certain persistent subclinical lesions,
for which the patient underwent 2 sessions of topical photodynamic
therapy. Briefly, 8% aminolevulinic acid (ALA) was applied and
after 2 h, the dressing was removed and the lesions were irradiated
using a red light for 20 min (the peak emission of 635 nm was used
and the total dose was 70 mJ/cm2), then a blue light was
used for another 10 min (80 mJ/cm2), followed again by a
red light (635 nm, 70 mJ/cm2) (Fig. 14, Fig.
15 and Fig. 16).
Case 5
An 18-year-old bisexual man presented to the
Department of Dermatology of Ponderas Academic Hospital for a
giant, indurated, flesh-colored, cauliflower-like tumor mass around
the anus and certain other small lesions dispersed on the
suprapubic area and around the penis. The patient had been recently
diagnosed with HIV, and had been started on antiretroviral therapy.
STD screening was positive for syphilis, Ureaplasma
urealyticum, Mycoplasma hominis and Candida. The
colonoscopy revealed no rectal invasion and the patient refused a
colostomy.
The tumor was excised with radiosurgery under
general anesthesia and all the smaller lesions were excised in 1
session of CO2 laser under local anesthesia. A biopsy
was sent to the pathologist.
The healing occurred by secondary intention, in 60
days. The patient received systemic antibiotic therapy with
gentamicin (80 mg every 12 h), benzathine benzylpenicillin (2.4
MUI/week for 10 weeks) for the syphilitic infection, doxycycline
(100 mg 2 tablets/day for 30 days), fluconazole (50 mg 1 tablet/day
for 30 days), local and intrarectal sinecatechins (twice a day for
4 months), inosine pranobex (3 tablets twice a day, 10 days per
month), alternately with Coriolus versicolor (3 tablets
twice a day for 4 months) and was administered 3 doses of Gardasil
9 vaccine (months 0-2-6) (Fig. 17,
Fig. 18 and Fig. 19).
Case 6
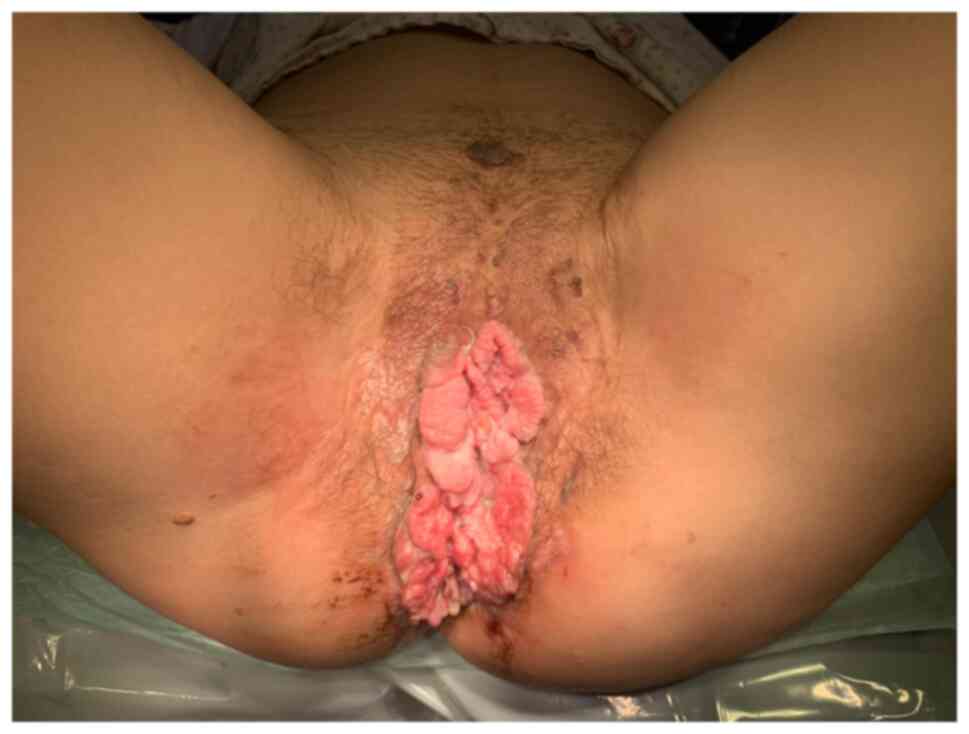
A 34-year-old smoking woman presented to the
Department of Dermatology of Ponderas Academic Hospital for a
giant, indurated, flesh-colored, cauliflower-like tumor mass
involving the vulvar area and certain verrucous papules distributed
over the suprapubic area and buttocks. The medical history revealed
that the patient had been HIV-positive for 23 years due to an
erroneous blood transfusion (CD4 count, 750 cells/mm3).
The patient tested positive for HPV 16, 18, 39, 6, 11 and 53
genotypes. The biopsy revealed poorly differentiated squamous cell
carcinoma (T4N2MXV0L1). The patient underwent pelvectomy with
nephrostomy, followed by localized radiotherapy (Figs. 20 and 21).
Case 7
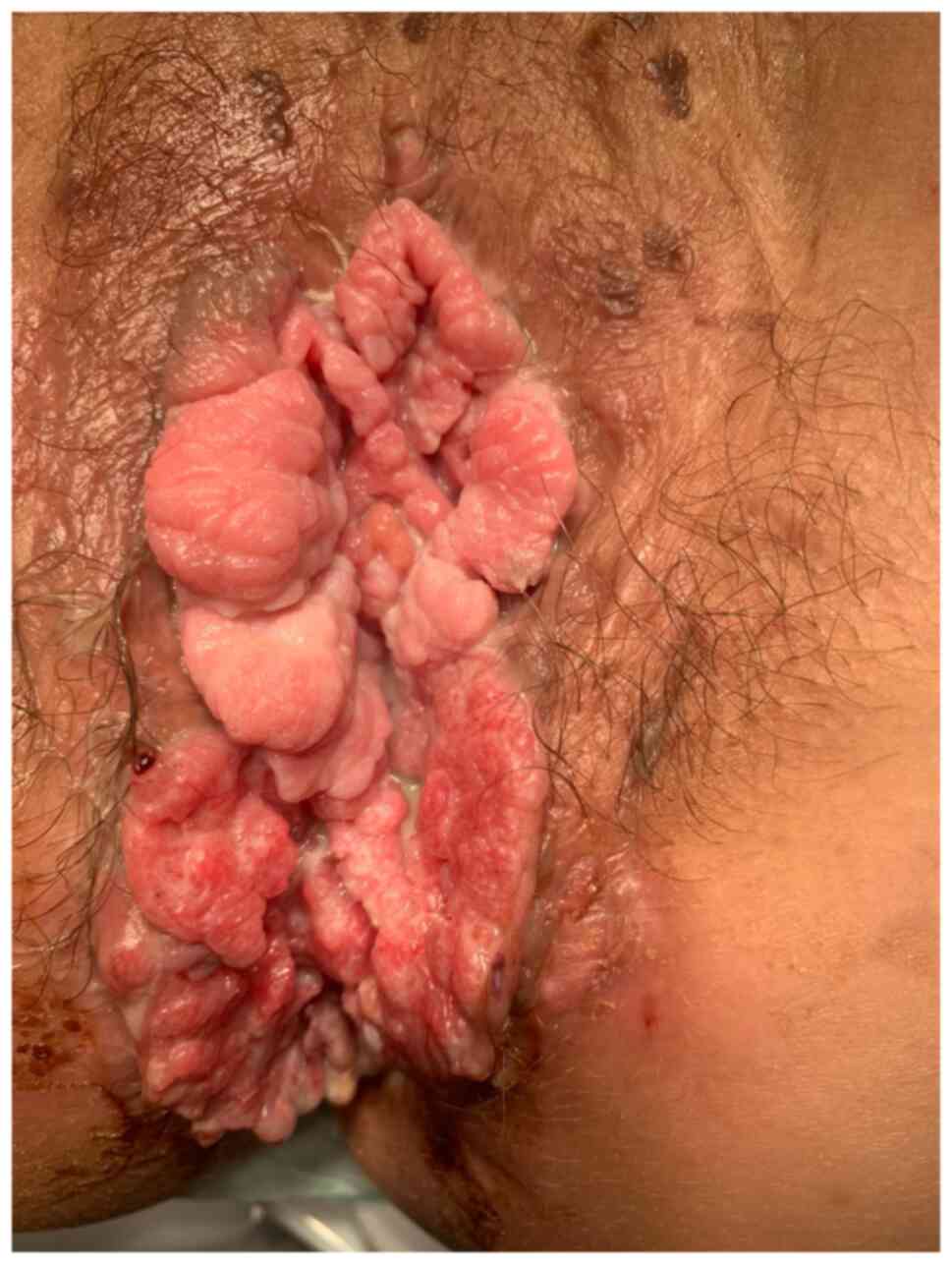
A 75-year-old female patient presented to the
Department of Dermatology of Ponderas Academic Hospital for an
indurated tumor mass located in the vulvar area. The lesion had
been growing progressively for numerous years. The PCR test
conducted on the vaginal brushing revealed the presence of HPV 6,
16 and 18. The tumor was excised with radiosurgery under general
anesthesia. The biopsy of the lesion identified HPV 6 and 16
genotypes and revealed moderately differentiated squamous cell
carcinoma. Therefore, the patient underwent pelvectomy with
nephrostomy, followed by radiotherapy (Fig. 22).
Discussion
In 1925, Buschke and Löwenstein described BLT for
the first time. They examined a penile lesion, which resembled both
common condyloma acuminata and squamous cell carcinoma from a
clinical point of view; however, it presented differences from both
of these diseases concerning the biological behavior and the
histopathological findings (9).
BLT represents an infrequent STD, caused by HPV,
mostly genotype 6 or 11. There are numerous risk factors for HPV,
such as multiple sexual partners, homosexuality, prostitution,
chronic genital infections, as well as the lack of proper hygiene
(4,9).
BLT is invariably preceded by condyloma acuminatum
and it is more common in individuals with a suppressed immune
system caused by AIDS, chemotherapy with immunosuppressive therapy
alcoholism or diabetes. HPV screening for HIV-positive and
immunocompromised patients should always be a priority in this
category of patients (1,4).
A high prevalence of GCA has been reported in the
homosexual and bisexual communities. Recurrent aggressive GCA has
been reported in HIV-positive patients. BLT could occur at any age,
particularly following puberty. However, the elderly should also be
tested for HPV infection. Men are more affected than women, and the
main affected areas are the penis, the anorectal area and the
urethra in males, and the vulva in females (4,11).
From a clinical view, it presents as a voluminous
cauliflower-like, flesh-colored tumor of papillomatous and
irregular surface, ultimately surpassing 10 cm2 in size
(4).
From a histopathological point of view, BLT is
characterized by papillomatosis and severe acanthosis. Generally,
the hyperplastic epithelium is well-differentiated; nevertheless,
the vacuolated epidermal cells reveal clear cytoplasm and
hyperchromatic nuclei. The basal membrane is undamaged and there is
a lymphohistiocytic inflammatory infiltrate present in the upper
dermis. When a biopsy is performed, it should be deep enough to
contain the whole tumor, particularly the epidermal/dermal
interface (4).
The multiplication cycle of HPV needs stratified
squamous epithelium (the junction between it and the columnar or
cuboid epithelium being the election site), explaining the
HPV-associated cancers on the lips, oral cavity, cervix, prostate,
penis, scrotum and rectum. The first structure infected is the
basal keratinocyte nucleus and if the host defense mechanism is
overcome, the virus multiplies and the DNA copies, during cell
division, are distributed to daughter cells, which are hard to
identify if the viral gene expression is low. The risk of malignant
transformation of infected cells is high if the infection persists
more than 6 months; however, ~90% of the cases have a self-limited
evolution of 2 years. There are numerous co-factors participating
in HPV-related carcinogenesis. The oncogenes E6 and E7 are the key
viral oncogenes from HPV 16 and other high-risk HPVs that
inactivate p53 and members of the retinoblastoma protein family
leading to inhibition of apoptosis, progression of the cellular
cycle and accumulation of genetic alterations, viral integration
and uncontrolled cell proliferation. The tumor-induced inflammation
promotes the proliferation, the survival of the malignant cells and
the alteration of the response to chemotherapy. The HPV infection
requires either intact skin tissue or wound healing and an active
inflammatory process in the skin in order to multiply. This theory
has a great impact on the treatment plan, healing per
secundam being an improved approach in comparison with grafting
after excision, since there is no risk for recurrences on fibrotic
tissue (as aforementioned HPV requires stratified squamous
epithelium for replication) (12-14).
The main differential diagnoses include Bowen's
disease (its dyskeratotic condylomatous form), squamous cell
carcinoma, as well as keratotic pseudoepitheliomatous balanitis
(4).
It is very difficult to differentiate between BLT
and verrucous carcinoma. There are authors who consider these
lesions to have numerous similarities. Nevertheless, other authors
have strongly suggested that BLT is the midway lesion between
condyloma acuminatum and verrucous carcinoma, considering it a
condyloma-like precancerous lesion (4).
The most frequent complications of BLT include
superinfection, fistulae or necrosis (15). Spontaneous regression is extremely
rare, while recurrence following an incomplete excision is very
frequent. In the case of GCA, histology does not reveal any
evidence of malignancy, such as infiltration of the basement
membrane, lymphatic invasion, angioinvasion or distant metastases.
Bleeding, infiltration of the tumor basis or lymph node enlargement
may lead to the suspicion of a malignant transformation into
micro-invasive carcinoma or into well-differentiated squamous cell
carcinoma, occurring in 30-50% of the cases (4,5,15).
The incidence of perianal GCA has slightly increased
during the last few years, but it remains very hard to
differentiate GCA from common condylomas or well-differentiated
squamous cell carcinomas. There is a well-known association between
HPV 16, 18, 31 and 33 and anogenital squamous cell carcinoma
(5,16).
Numerous factors need to be considered when deciding
on the most appropriate type of treatment, such as the size, the
location of the giant condyloma, as well as previous therapies that
have proven unsuccessful. The microscopic analysis of the genital
skin for subclinical HPV lesions has a crucial role for an early
detection of HPV lesions or recurrences and for selecting the best
treatment plan (8).
The ‘gold standard’ therapy is represented by
surgical treatment, which consists of full thickness excision and
tumor-free margin control. According to the clinical condition of
the patient, extensive abdominopelvic surgery may be recommended in
cases of visceral involvement.
Preoperative imagistic investigations (CT and MRI)
are required before surgery in order to assess the extensiveness of
local and systemic disease, and to select the optimal treatment
approach. Temporary colostomy followed by reintegration in cases of
rectum involvement is also recommended. Despite the fact that
numerous authors consider wide local excision followed by
split-thickness skin grafts the mainstay of therapy, it is
considered that healing per secundam is an improved
approach, since grafting represents a risk factor for HPV (6-8).
HPV infection is a field infection, where large
areas of cells at a tissue surface are affected by the HPV virus;
therefore, once the GCA is excised, focus on treating the whole
affected genital area is required. In literature, certain treatment
methods for BLT are stated, but the risk of recurrence is very high
(podophyllotoxin, usually used for common condyloma acuminata;
5-FU, with improved results for the intraurethral BLT; imiquimod,
very aggressive therapy with numerous side effects; cryotherapy,
CO2 laser and sinecatechins, very effective with less
side effects; and topical photodynamic therapy using both red and
blue lights, which was successfully used in our cases) (11,17).
However, the best specific immunostimulation is the HPV vaccination
with Gardasil 9. In case of verrucous carcinoma, chemotherapy needs
to be added to the treatment plan. Radiotherapy, however, appears
to be responsible for the alteration of BLT into anaplastic
carcinoma (8,18).
In conclusion, despite the fact that numerous
authors consider wide local excision followed by split-thickness
skin grafts the mainstay of therapy, it is considered in the
present study that healing per secundam is an improved
approach, since there is no risk for recurrences on fibrotic
tissue. For an improved understanding of this phenomenon, further
studies are required.
Microscopic analysis of the genital skin for
subclinical HPV lesions has a crucial role for an early detection
of HPV lesions/recurrences and an improved outcome for the health
and social life of the patient.
In case of BLT, there are cases that exceed the
qualifications of the dermatologist; therefore, there may be a need
for a multidisciplinary approach: Colonoscopy/proctoscopy for
rectal invasion, cystoscopy and gynecological exam. The importance
of gynecological examination and HPV screening for every female
patient should not be overlooked, regardless of age (case 7), nor
the importance of HPV screening for HIV-positive and
immunocompromised patients (cases 5 and 6) (17,19).
Most importantly, a set of complete STD tests should
be performed for all young male patients, as well as smokers and
patients who have started their sexual activities early in life. In
addition, non-specific immune stimulation and HPV vaccination with
Gardasil 9 should be integrated in the treatment plan for every
patient with an HPV infection.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
DBo performed the biopsies, the CO2 laser
excisions, the topical photodynamic therapy and participated in the
therapeutic management of the cases. AC and DBr performed the photo
documentation of the cases and performed critical review of the
literature findings. NB performed the histopathologic examination.
RC performed the wide local excision of the lesions. DBo and AC
confirm the authenticity of all the raw data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
A written informed consent for clinical examination,
surgery, treatment and obtaining images for publication was
obtained from the patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chu GY, Chang TCC and Chang CH:
Buschke-Löwenstein tumor (giant condyloma acuminatum) successfully
treated by topical PDT: A case report. Dermatol Sin. 31:94–97.
2013.
|
|
2
|
Indinnimeo M, Impagnatiello A, D'Ettorre
G, Bernardi G, Moschella CM, Gozzo P, Ciardi A, Bangrazi C, De
Felice F, Musio D and Tombolini V: Buschke-Löwenstein tumor with
squamous cell carcinoma treated with chemo-radiation therapy and
local surgical excision: Report of three cases. World J Surg Oncol.
11(231)2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Martin JM, Molina I, Monteagudo C, Marti
N, Lopez V and Jorda E: Buschke-Lowenstein tumor. J Dermatol Case
Rep. 2:60–62. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hicheri J, Jaber K, Dhaoui MR, Youssef S,
Bouziani A and Doss N: Giant condyloma (Buschke-Löwenstein tumor).
A case report. Acta Dermatovenerol Alp Pannonica Adriat.
15:181–183. 2006.PubMed/NCBI
|
|
5
|
Ahsaini M, Tahiri Y, Tazi MF, Elammari J,
Mellas S, Khallouk A, El Fassi MJ, Farih MH, Elfatmi H, Amarti A
and Stuurman-Wieringa RE: Verrucous carcinoma arising in an
extended giant condyloma acuminatum (Buschke-Löwenstein tumor): A
case report and review of the literature. J Med Case Rep.
7(273)2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Papiu HS, Dumnici A, Olariu T, Onita M,
Hornung E, Goldis D, Aiordachioae G and Vasca V: Perianal giant
condyloma acuminatum (Buschke-Löwenstein tumor). Case report and
review of the literature. Chirurgia (Bucur). 106:535–539.
2011.PubMed/NCBI
|
|
7
|
Spinu D, Rădulescu A, Bratu O, Checheriţă
IA, Ranetti AE and Mischianu D: Giant condyloma
acuminatum-Buschke-Lowenstein disease-a literature review.
Chirurgia (Bucur). 109:445–450. 2014.PubMed/NCBI
|
|
8
|
Tripoli M, Cordova A, Maggì F and
Moschella F: Giant condylomata (Buschke-Löwenstein tumours): Our
case load in surgical treatment and review of the current
therapies. Eur Rev Med Pharmacol Sci. 16:747–751. 2012.PubMed/NCBI
|
|
9
|
Agarwal S, Nirwal GK and Singh H:
Buschke-Lowenstein tumour of glans penis. Int J Surg Case Rep.
5:215–218. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
De Toma G, Cavallaro G, Bitonti A,
Polistena A, Onesti MG and Scuderi N: Surgical management of
perianal giant condyloma acuminatum (Buschke-Löwenstein tumor).
Report of three cases. Eur Surg Res. 38:418–422. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Iorga L, Dragos Marcu R, Cristina Diaconu
C, Maria Alexandra Stanescu A, Pantea Stoian A, Liviu Dorel
Mischianu D, Surcel M, Bungau S, Constantin T, Boda D, et al:
Penile carcinoma and HPV infection (Review). Exp Ther Med.
20:91–96. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lehn H, Ernst TM and Sauer G:
Transcription of episomal papillomavirus DNA in human condylomata
acuminata and Buschke-Löwenstein tumours. J Gen Virol. 65 (Pt
11):2003–2010. 1984.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Boshart M and zur Hausen H: Human
papillomaviruses in Buschke-Löwenstein tumors: Physical state of
the DNA and identification of a tandem duplication in the noncoding
region of a human papillomavirus 6 subtype. J Virol. 58:963–966.
1986.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Boda D, Docea AO, Calina D, Ilie MA,
Caruntu C, Zurac S, Neagu M, Constantin C, Branisteanu DE,
Voiculescu V, et al: Human papilloma virus: Apprehending the link
with carcinogenesis and unveiling new research avenues (Review).
Int J Oncol. 52:637–655. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Neagu M, Caruntu C, Constantin C, Boda D,
Zurac S, Spandidos DA and Tsatsakis AM: Chemically induced skin
carcinogenesis: Updates in experimental models (Review). Oncol Rep.
35:2516–2528. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Boda D, Neagu M, Constantin C, Voinescu
RN, Caruntu C, Zurac S, Spandidos DA, Drakoulis N, Tsoukalas D and
Tsatsakis AM: HPV strain distribution in patients with genital
warts in a female population sample. Oncol Lett. 12:1779–1782.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Boda D, Negrei C, Arsene AL, Caruntu C,
Lupuleasa D and Ion RM: Spectral and photochemical properties of
hyperbranched nanostructures based on gardiquimod and TPPS4.
Farmacia. 63:218–223. 2015.
|
|
18
|
Sandhu R, Min Z and Bhanot N: A gigantic
anogenital lesion: Buschke-lowenstein tumor. Case Rep Dermatol Med.
2014(650714)2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Caruntu C, Zurac SA, Jugulete G and Boda
D: Extramammary Paget's disease in an HIV-positive patient. Rom J
Morphol Embryol. 58:1009–1015. 2017.PubMed/NCBI
|