Introduction
In the United States, 83,730 patients were diagnosed
with bladder cancer and 17,200 patients succumbed to bladder cancer
in 2021(1). Bladder cancer is the
fourth most common cancer among men in the United States. The
incidence of bladder cancer is also high in China (2). Radical cystectomy is the gold
standard treatment for muscular invasive bladder cancer. Total
cystectomy and urinary diversion are complicated procedures with a
perioperative morbidity rate of nearly 40% (3). Urinary fistula rarely occurs after
ileal conduit urinary diversion; Vetterlein et al reported
that the incidence of urinary fistula was 3% among 506 patients who
underwent total bladder surgery, but its management is challenging
(4). There is no satisfactory
treatment for urine leakage, and a second surgery may be required,
which may be painful and increase the financial burden on the
patient (5). Ureteral stent
implantation is sometimes used to treat urine leakage, but it is
very difficult to locate the anastomosis and insert the guide wire
and ureteral stent (6).
Furthermore, urine leakage may occur before the stent is removed,
and this is even more difficult to manage. Negative-pressure
drainage systems (NPS) are generally used to treat complicated
wounds (7). They have been widely
used with favorable results in patients with abdominal trauma and
postoperative intestinal fistula. Negative-pressure suction helps
to keep the fistula relatively dry and clean, which aids healing.
Therefore, NPS was used to treat patients with urine leakage after
Bricker surgery at our institution. Herein, the case of a patient
who received this treatment and was cured, is reported.
Case report
A 63-year-old woman visited Hexi University
Affiliated Zhangye People's Hospital (Zhangye, China) due to gross
hematuria. Computed tomography urography revealed posterior bladder
wall thickening, but no obvious upper urinary tract abnormalities
were noted. Cystoscopy examination revealed the presence of a tumor
in the bladder. The patient was subsequently hospitalized for
biopsy and transurethral resection of the bladder tumor. The tumor
size was 1.5 cm. The pathological diagnosis was high-grade muscular
invasive urothelial carcinoma with vascular tumor thrombus and
without nerve invasion.
The patient was advised to undergo radical
cystectomy. Antibiotics were administered on the day before the
surgery, and the patient was routinely administered an enema
preoperatively. Intraoperatively, adhesions between the left side
of the bladder and the uterus and ovaries of the patient were
found, and a conventional ureteroileal anastomosis scheme was used.
Two 8-mm incisions were made at the proximal end of the ileum, and
the distal ends of the left and right ureters were cut by 5 mm. The
ureter was then implanted into the ileum with a 5-0 absorbable
thread and indwelling the ureteral stent and the uterus was removed
and an indwelling ileostomy drainage tube was placed during the
surgery. No abnormalities were noted on postoperative lymph node
examination. A ureteral stent was placed during the anastomosis and
found no leakage of urine. Postoperatively, the patient received
routine antibiotic therapy, and no other special medication was
administered. However, 1 week postoperatively, the drainage tube in
the ileum was routinely removed and urine leakage from the vagina
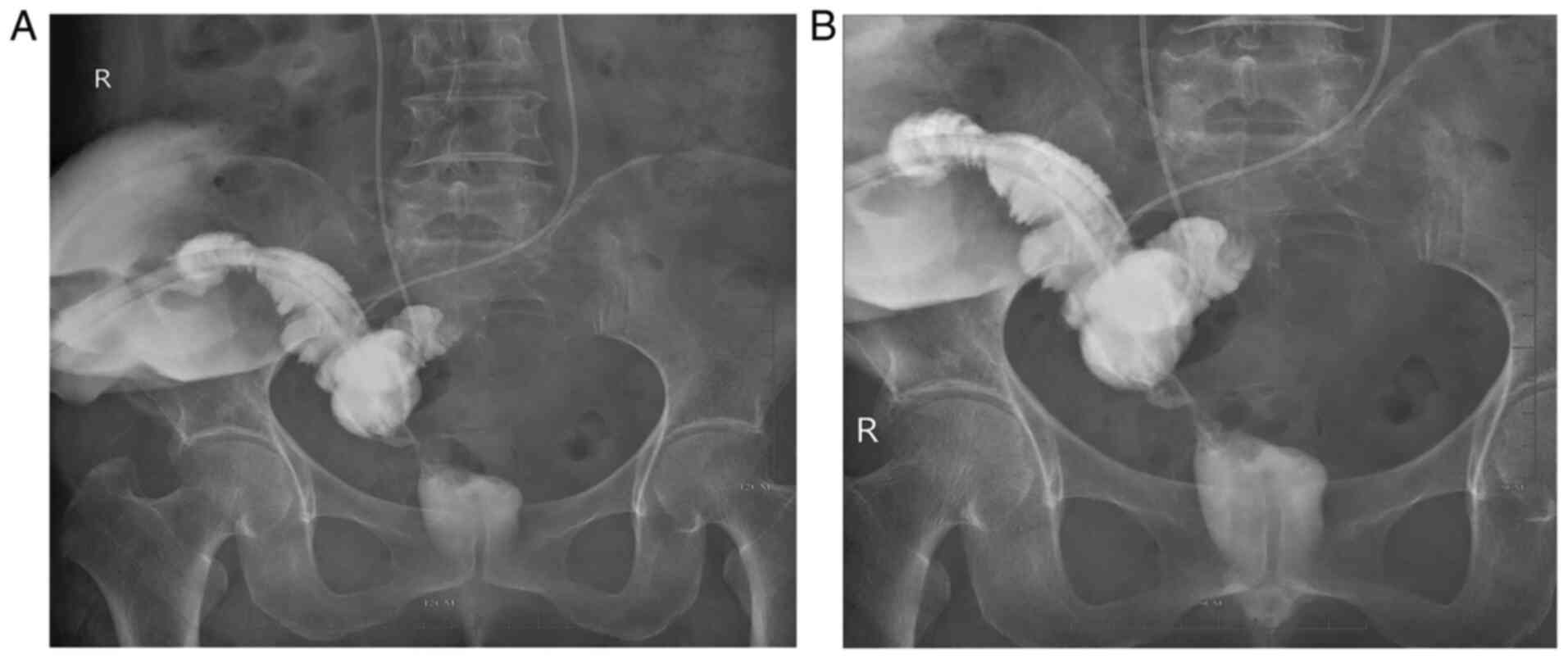
was found (Fig. 1). The ureteral
stent was not replaced. There was a large amount of leakage, and
the patient used three diapers per day. The patient was in severe
pain due to the urine leakage and requested to undergo reoperation.
Percutaneous nephroscopy was performed to determine the leakage
site by examining the vagina without using anesthesia. Upon
checking the vaginal fistula, methylene blue was injected from the
double cannula, and the vagina was observed. Methylene blue was
observed flowing out of the vaginal fistula. A fistula was observed
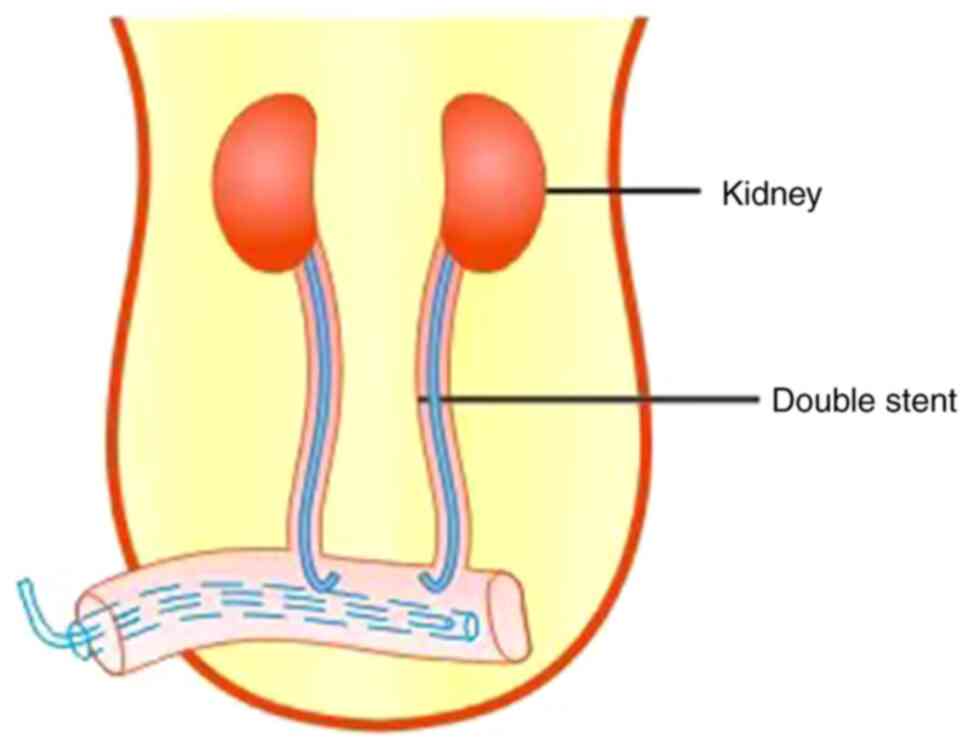
in the vaginal wall (Video S1), and a double-cannula
negative-pressure drainage was performed. The outer tube of the
double cannula is a soft rubber drainage cannula (F24) and the
inner tube is a sputum suction cannula (F12). The cannula is
inserted through the ileostomy without anesthesia.
The double ureteral stent (double-J stent) could
then be observed in the proximal ileum. The double cannula was
successfully inserted and fixed using a zebra guide wire and a
continuous NPS was set up (Fig.
2). The patient was then transferred to the general ward.
Subsequently, the urine leakage per day gradually decreased. There
was no urine leakage after 3 weeks. One week later, the catheter
and double cannula were removed. After the issue of urine leakage
was completely resolved, the ureteral stent 3 months after the
surgery was removed (no replacement). The patient recovered well as
noted during the regular follow-up examinations. Physical
examination conducted at the 3-month, 6-month and 1-year follow-up
revealed that the patient has recovered well.
Discussion
In women, radical cystectomy involves total pelvic
resection, which includes the removal of the anterior vaginal wall
and urethra. Urinary fistula after ileal conduit urinary diversion
is quite rare and its treatment is challenging, especially in
patients who have undergone complicated pelvic organ resection and
urinary diversion (8). The
treatment of urinary fistula should be as less invasive as
possible. Surgical treatment is usually avoided as it may lead to
postoperative complications and stickiness. In recent years,
urologists have developed several methods, including the retrograde
ureteral approach and percutaneous nephrostomy, to treat this
complicated condition; however, if complications of Clavien-Dindo
classification grade III or higher occur, anesthesia surgery is
required for treatment, and such treatment is challenging (4,9).
Vacuum-assisted closure and NPS have been used in the treatment of
persistent abdominal wounds for numerous years. They involve the
use of negative pressure to remove edema fluid, improve
circulation, promote the growth of granulation tissue, and inhibit
bacterial growth (10).
Inspired by this, these techniques are used on our
patients for the conservative treatment of urine leakage after
Bricker surgery. The present patient, who had a urinary fistula
following ileal conduit urinary diversion, was successfully treated
with intra-conduit NPS. Although the duration of treatment was
long, the technique used was extremely simple, safe, minimally
invasive, and well-tolerated. Intraoperatively, percutaneous
nephroscopy was performed to view the vagina and ileostomy. The
patient did not require anesthesia. After inserting the double
cannula using the guide wire, the nephroscope was reinserted to
confirm the location of the fistula. The present technique
undertaken by the authors of this study, is more reliable than
surgery performed in the ward. Ileal catheter leakage after urinary
diversion is most commonly caused by a ureteral anastomotic fistula
or high pressure in the intestine. Therefore, timely drainage of
urine and decompression is key to treating urine leakage. The use
of an NPS is a favorable method to achieve this. In recent years,
an increasing number of studies in the field of endourology have
shown that upper urinary tract lesions can be treated. In clinical
practice, endoscopy has been found to be feasible and relatively
safe for treating ureteral anastomotic stricture (11,12).
However, patients with urine leakage after ileal conduit urinary
diversion often have no ureteral obstruction. Retrograde stent
placement is much safer than nephrostomy, but it is time-consuming
and mucosal edema in the ileum and ureter renders the surgery
difficult to perform. In addition, there is a risk of abdominal
infection. Intraductal NPS is less invasive and more convenient
than urological interventions and transperitoneal surgery. The
fistula and double-J stent can be clearly visualized using a
prostate resectoscope and percutaneous nephroscope. Furthermore,
the double cannula is inserted under endoscopic guidance to ensure
successful implantation and to avoid placing the silicon tube too
superficially as it may lead to insufficient drainage and treatment
failure.
Currently, the use of an NPS is contraindicated in
patients with non-enteric fistulas such as urinary fistulas. During
treatment with an NPS, the suction pressure is adjusted to ensure
that there is no discomfort to the patient. Thereafter, it is
necessary to observe the patient carefully to confirm that the
patient does not display urine leakage. Simultaneously, the lowest
negative pressure value must be observed to ensure that the patient
does not leak urine at that point; the lowest negative pressure
value should be used in the continuation of suction. In the present
patient, a nephroscope was inserted through the ileostomy to
clearly observe the position of the double-J stent and the double
cannula of the NPS was placed under direct vision to ensure that it
is accurately positioned near the ureteral and ileal anastomosis
and away from the mucosa. A continuous low-intensity negative
pressure suction was started, and urine flowed through the
ileostomy instead of into the vagina. This kept the fistula
relatively dry and the microenvironment clean. Therefore, it is
considered that it will not hinder the recovery of the fistula. The
fact that the patient was successfully treated indicates that NPS
may be a favorable alternative to surgery for treating urinary
fistula following ileal conduit urinary diversion. At present, the
cause of the urine leakage is unclear. It is surmised that it did
not leak from the ureteroileal anastomosis because it was sutured
tightly during the surgery. Combined with the angiography, it is
considered that the leakage came from the proximal ileum and
vaginal remnants since there was a connection between those two
parts when the leakage occurred. Therefore, treatment was actively
carried out and favorable results were achieved. It is our aim to
gain more insight into this treatment method in future
research.
Intra-conduit NPS is less invasive than other
methods, and it should be used in clinical practice. Since urine
leakage is rare, this technique could not be performed on more
patients. Furthermore, as NPS is a new technique for treating urine
leakage following ileal conduit urinary diversion, further research
and long-term follow-up are required. Intra-conduit NPS is
minimally invasive and suitable for the conservative treatment of
urine leakage after ileal conduit urinary diversion in specific
patients.
Supplementary Material
Supplementary Data
Fistula in the vaginal wall was
observed using percutaneous nephroscopy.
Acknowledgements
The authors would like to thank Dr Belinda Mitchell
(Wits Health Consortium, Johannesburg, South Africa) for English
language editing.
Funding
Funding: The present study was funded by grants from NHC Key
Laboratory of Diagnosis and Therapy of Gastrointestinal Tumor
(grant no. NLDTG2020015), and Gansu Province Science and Technology
Planning Project (grant no. 20JR10RG310).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
ZJW and YJQ provided substantial contributions to
the conception and design of the work and drafting and revision of
the manuscript. CJY and XYW contributed substantially to
conceptualization and assisted in the completion of the surgery. JQ
collected clinical information and assisted with the drafting of
the manuscript. ST and JXY provided substantial contributions to
the design of the work, drafting, confirmed the authenticity of all
raw data and agreed to be accountable for all aspects of the work
in ensuring that questions related to the accuracy or integrity of
any part of the work are appropriately investigated and resolved.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki, and approved by the Ethics
Committee of Hexi University Affiliated Zhangye People's Hospital
(Zhangye, China) and informed consent was obtained from the
patient.
Patient consent for publication
Consent was obtained for publication of the
patient's data/images in this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD, Fuchs HE and Jemal
A: Cancer statistics, 2021. CA Cancer J Clin. 71:7–33.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Feng RM, Zong YN, Cao SM and Xu RH:
Current cancer situation in china: Good or bad news from the 2018
global cancer statistics? Cancer Commun (Lond).
39(22)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tyritzis SI and Wiklund NP: Is the open
cystectomy era over? An update on the available evidence. Int J
Urol. 25:187–195. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Vetterlein MW, Klemm J, Gild P, Bradtke M,
Soave A, Dahlem R, Fisch M and Rink M: Improving estimates of
perioperative morbidity after radical cystectomy using the european
association of urology quality criteria for standardized reporting
and introducing the comprehensive complication index. Eur Urol.
77:55–65. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kimura T, Ishikawa H, Kojima T, Kandori S,
Kawahara T, Sekino Y, Sakurai H and Nishiyama H: Bladder
preservation therapy for muscle invasive bladder cancer: The past,
present and future. Jpn J Clin Oncol. 50:1097–1107. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Muzzonigro G and Tombolini F:
Ureterovaginal fistulae. Urologia. 82:22–29. 2015.PubMed/NCBI View Article : Google Scholar : (In Italian).
|
|
7
|
Núñez Cerezo V, Romo Muñoz MI, Amesty
Morello MV, Vilanova Sánchez A, Dore Reyes M, Gómez Cervantes M,
Andrés Moreno AM, Martínez-Ojinaga Nodal E, Martínez Martínez L and
López Santamaría M: Negative pressure system in the treatment of
enterocutaneous fistulas in the pediatric population. Cir Pediatr.
29:166–170. 2016.PubMed/NCBI(In Spanish).
|
|
8
|
Stein R, Hohenfellner M, Pahernik S, Roth
S, Thüroff JW and Rübben H: Urinary diversion-approaches and
consequences. Dtsch Arztebl Int. 109:617–622. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li X, Wang P, Liu Y and Liu C: . Minimally
invasive surgical treatment on delayed uretero-vaginal fistula. BMC
Urol. 18(96)2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Perez D, Wildi S and Clavien PA: The use
of an abdominal vacuum-dressing system in the management of
abdominal wound complications. Adv Surg. 41:121–131.
2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zhang Z, Zhang C, Wu C, Yang B, Wang H,
Hou J, Xu C and Sun Y: Progressive ureteral dilations and
retrograde placement of single-j stent guided by flexible
cystoscope for management of ureteroenteral anastomotic stricture
in patients after radical cystectomy and bricker urinary diversion.
J Endourol. 29:90–94. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Packiam VT, Agrawal VA, Cohen AJ, Pariser
JJ, Johnson SC, Bales GT, Smith ND and Steinberg GD: Lessons from
151 ureteral reimplantations for postcystectomy ureteroenteric
strictures: A single-center experience over a decade. Urol Oncol.
35:112.e19–112.e25. 2017.PubMed/NCBI View Article : Google Scholar
|