Introduction
Neuroblastoma is the most common solid tumor in
children (1). With the development
of pediatric anesthesia and endoscopic minimally invasive
technology, children's abdominal tumors can be completely removed
by laparoscopy. Laparoscopic minimally invasive surgery has little
trauma and quick recovery and children can receive postoperative
chemotherapy as early as possible, which is conducive to good
recovery. However, laparoscopic surgery for malignant solid tumors
is still in the stage of clinical exploration. The laparoscopic
surgical approach can be intraperitoneal and retroperitoneal. The
two approaches are safe and effective in the resection of adrenal
neurogenic tumors. The transperitoneal approach is the standard
approach for the treatment of adrenal tumors. When the tumor
diameter is >6 cm, the tumor is malignant, or the tumor
surrounds important blood vessels or invades surrounding tissues,
it is more suitable to choose the transperitoneal approach.
At present, there are few literature reports on the
successful treatment of stage III-IV neuroblastoma by laparoscopy.
The present study discussed the significance and feasibility of
complete resection of stage III neuroblastoma by laparoscopic
surgery while comparing its safety and effectiveness with
traditional surgery.
Case report
A 4-year-old girl was admitted to the First
Affiliated Hospital of Xiamen University on 26 February 2021 with a
6-month history of right intercostal pain. Physical examination
revealed that right abdominal distention and a hard mass could be
palpable under the right lower costa. Abdominal enhancement
computed tomography scan (CT) on 1 March 2021 had revealed a large
malignant mass in the right retroperitoneal and adrenal area, with
a size of 8.9x6.5x4.6 cm. The possibility of neuroblastoma was
taken into consideration; it had caused an serious effect on the
inferior vena cava, bilateral renal veins and right renal artery
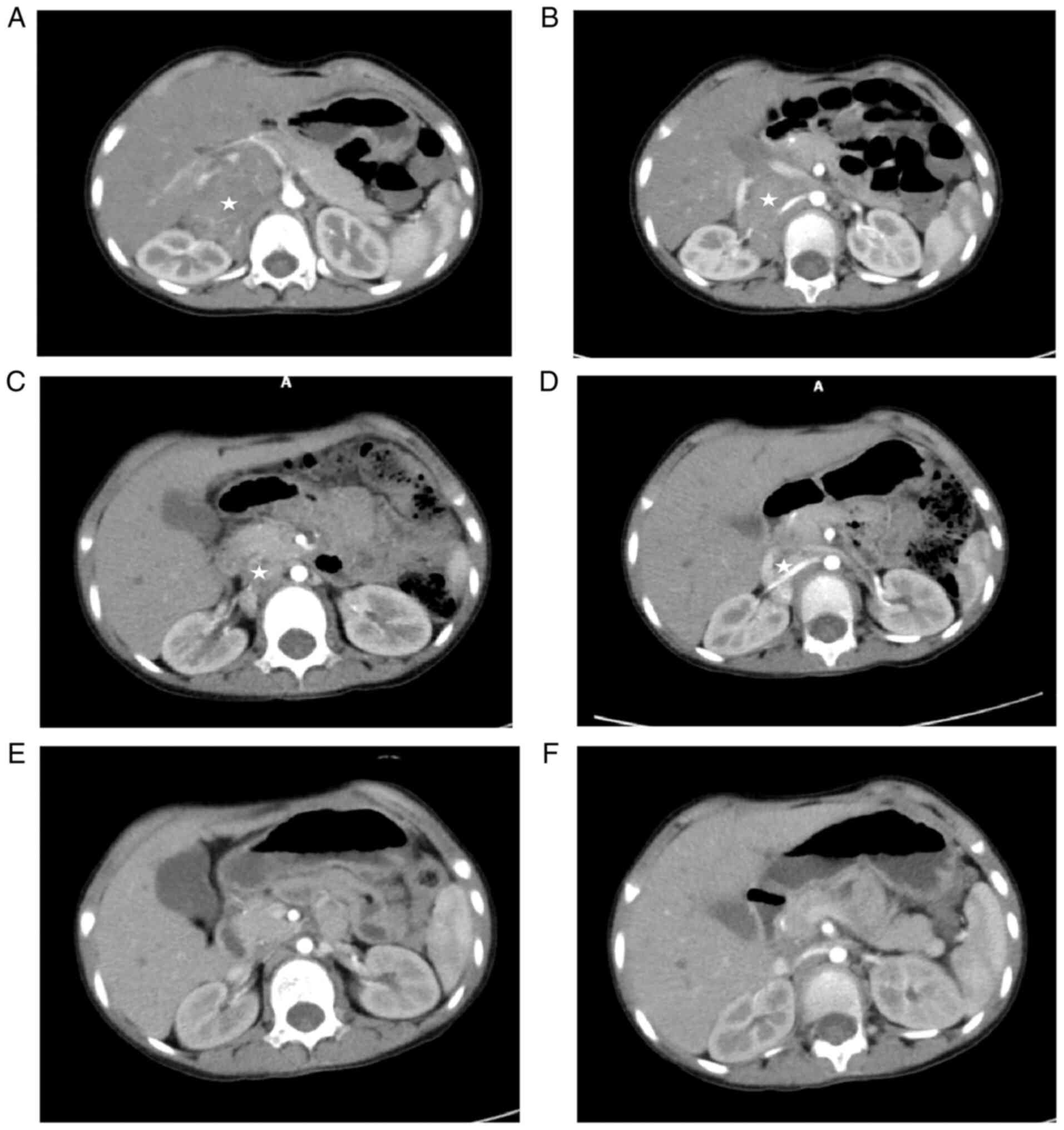
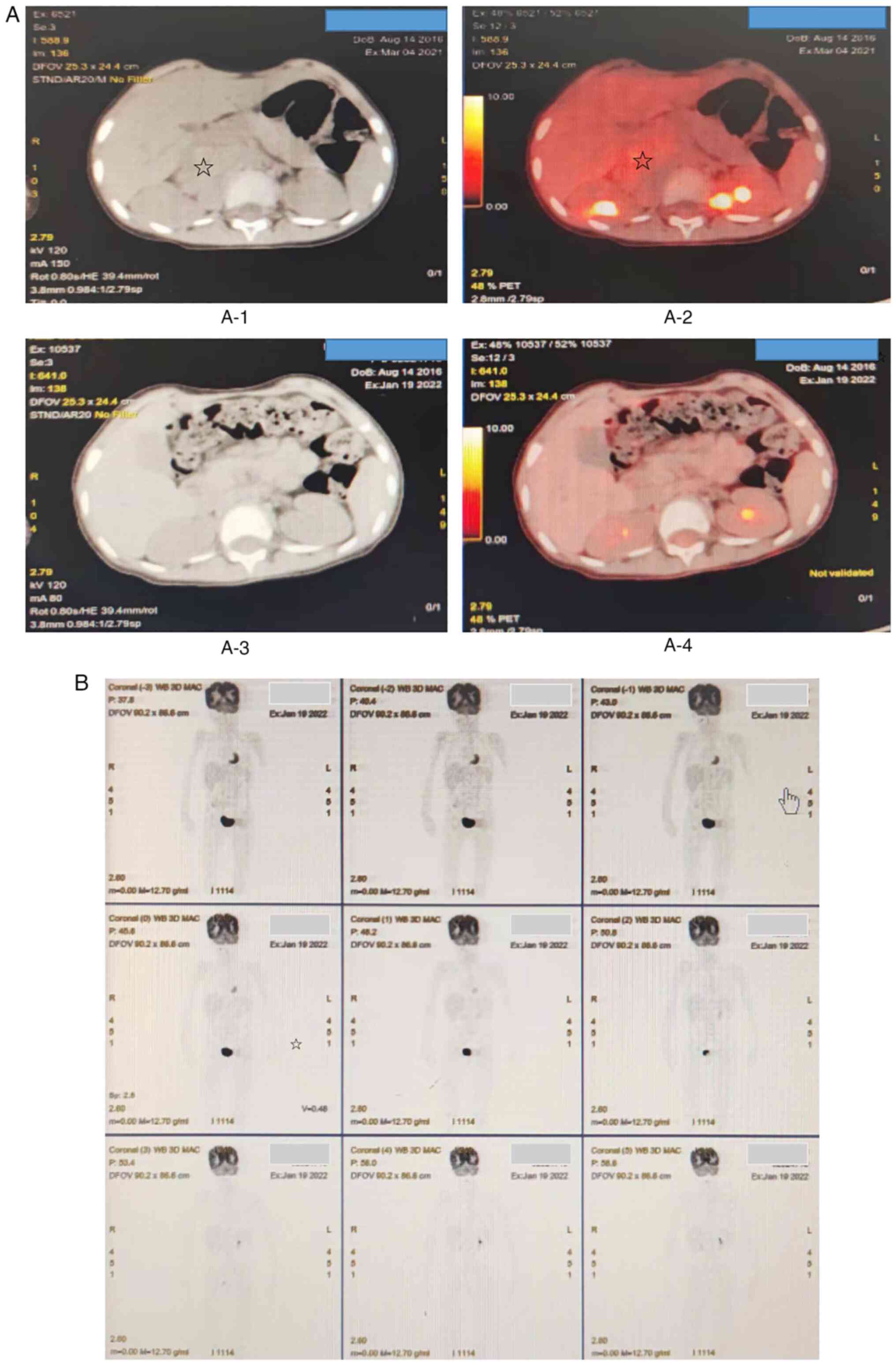
and multiple enlarged lymph nodes retroperitoneally (Fig. 1A and B). Positron emission tomography (PET)-CT
(4 March 2021) revealed a large right adrenal neuroblastoma
surrounding right renal artery, right renal vein and inferior vena
cava, with multiple retroperitoneal lymph node metastases (Fig. 2A-1 and A-2). Considering the large size of the
tumor and its invasion of important blood vessels, resection by
operation was not suggested. Ultrasound-guided peritoneal biopsy
was performed on 11 March, 2021. Pathological results suggested a
diagnosis of neuroblastoma. Bone marrow biopsy indicated there was
no metastasis. Due to the tumor crossed the midline of the abdomen
and the patient's age at >18 months, she was assessed as ʻstage
III, high riskʼ and three courses of chemotherapy were performed
(Table I). CT re-examination on 22
June, 2021 showed a right adrenal tumor with a size of 5.5x3.8x3.1
cm, multiple enlarged lymph nodes retroperitoneally reduced
compared with the previous states (Fig. 1C and D). Following preoperative evaluation, the
conditions for surgical resection was achieved (it was determined
the patient could undergo laparoendoscopic resection and surgery
proceeded with). Laparoscopic right adrenal neuroblastoma resection
was performed on 9 July, 2021.
 | Table IPreoperative and postoperative
chemotherapy schedule and time. |
Table I
Preoperative and postoperative
chemotherapy schedule and time.
| Dates,
year.month.day | Cycles | Plan | Evaluation |
|---|
|
2021.3.27-2021.4.3 | 1 | VCR + CDDP + VP16 +
CTX | |
|
2021.4.18-2021.4.22 | 2 | IFOS + CBP + ADR | |
|
2021.5.09-2021.5.16 | 3 | VCR + CDDP + VP16 +
CTX | Complete
assessment |
| | | | Surgery and
postoperative evaluation |
|
2021.7.24-2021.7.31 | 4 | VCR + CDDP + VP16 +
CTX | |
|
2021.8.23-2021.8.28 | 5 | IFOS + CBP + THP | |
|
2021.9.14-2021.9.21 | 6 | VCR + CDDP + VP16 +
CTX | |
|
2021.10.11-2021.1016 | 7 | IFOS + CBP + THP | |
|
2021.11.02-2021.11.09 | 8 | VCR + CDDP + VP16 +
CTX | |
|
2021.12.03-2021.12.07 | 9 | IFOS + CBP + THP | Complete assessment
end of chemo |
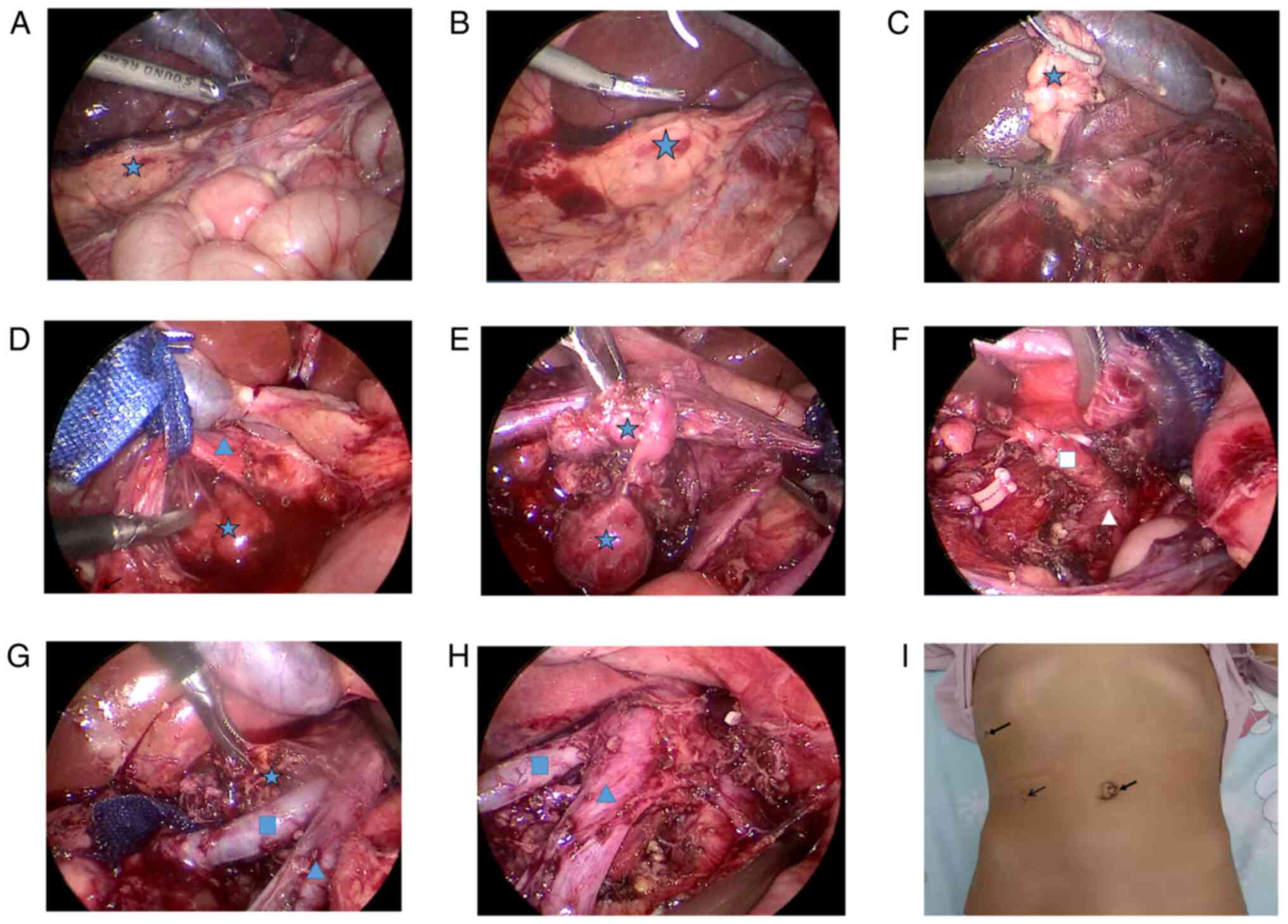
The procedure was as follows (Fig. 3A-H): A 2 cm incision was made
through the umbilicus, a TRIPORT was inserted and another 5 mm
Trocar was inserted into the right upper abdomen as an auxiliary
working port. The ascending colon ligament, hepatic colon ligament
and duodenal collateral mesentery were released to fully expose the
surgical visual field. Exploration revealed that the tumor
originated from the right adrenal gland, crossed the midline and
was located behind the inferior vena cava, encompassing the artery
and vein of the right kidney and multiple enlarged lymph nodes
adjacent to the abdominal aorta. The tumor was dissected at the
right renal hilum and the tumor tissue surrounding the right renal
vessel was carefully dissected and segmented with an ultrasound
knife to bare the right renal vessel. Then the inferior vena cava
was dissociated and gently pulled by traction wire to expose the
tumor tissue located in the adrenal gland and paravertebral area.
Finally, lymph nodes adjacent to the abdominal aorta and the right
hilum were dissected. Abdominal drainage tube was indwelled and the
incision was closed to complete the operation. Red blood cells (2
units) were transfused intraoperatively. Postoperative recovery was
satisfactory. According to the postoperative pathology,
ganglioneuroblastoma was diagnosed and metastasis was seen in 3/5
lymph nodes, with the DNA of tumor tissue being polyploid and the
amplification of N-myc gene positive. Chemotherapy was introduced
in the two weeks following the operation, with a total of six
courses. Abdominal enhancement CT re-examination on 2 November,
2021 showed no clear signs of tumor recurrence and metastasis
(Fig. 1E and F). On 19 January, 2022, PET-CT
examination (Fig. 2B) showed no
clear abnormal hypermetabolic foci in the whole body. After a
comprehensive evaluation, the patient achieved clinical treatment
and chemotherapy was ended. The treatment has been finished and
follow-up is continuing.
Discussion
Laparoscopic surgery for malignant solid tumors in
children is still in the stage of clinical exploration. The adrenal
gland is the most common site of neurogenic tumors in children. Due
to the deep anatomical location and narrow space of adrenal tumors,
traditional laparotomy requires a large incision and is truly
difficult to expose. Laparoscopic technology has a broad surgical
field which can accurately determine the location of the tumor and
the relationship with the surrounding tissues; surgical trauma is
small, postoperative recovery is fast and patients can also receive
chemotherapy and radiotherapy earlier following surgery compared
with conventional surgery and thus is gradually gaining favor among
surgeons. At present, a series of problems related to neuroblastoma
and the indications of laparoscopic surgery are still a hot
topic.
The survival of patients with high risk
neuroblastoma has improved significantly with the use of intensive
multimodality treatment regimens including chemotherapy, surgery,
radiation therapy, myeloablative chemotherapy followed by stem cell
rescue and immunotherapy (2).
Complete resection of the tumor is still the most important key to
improve the prognosis. Several details regarding the role of
aggressive surgery in high-risk neuroblastoma remain controversial
(2). The present study reported
the comprehensive treatment and operation process of this patient
with high risk neuroblastoma in detail. The purpose of this paper
was to introduce the successful experience of minimally invasive
treatment of stage III neuroblastoma, in the hope that it might
become a treatment scheme.
Abdominal neurogenic tumors are often concealed,
large and easy to invade the surrounding tissues and blood vessels,
resulting in the difficulty of laparoscopy. The indications and
complications of laparoscopic surgery are still the focus of
attention. With the development of laparoscopic technology, reports
of successful laparoscopic neurogenic tumor resection in children
have gradually increased and satisfactory surgical results have
been achieved. However, there are few literature reports on the
successful treatment of stage III-IV neuroblastoma by laparoscopy.
Complications of laparoscopic surgery of neurogenic tumors mainly
include intraoperative bleeding, conversion to laparotomy, renal
atrophy or renal infarction, diaphragm injury and intestinal
obstruction (3-5).
There has been no reports of tumor recurrence at the puncture site
of Trocar after laparoscopic neurogenic tumor resection (6). Leclair et al (7) report that laparoscopic minimally
invasive technology is suitable for children with complete tumor
capsule and negative image-defined risk factors (IDRFs). Tumors
crossing the midline of abdomen and positive IDRFs should be
contraindications for laparoscopic surgery, as due to the large
size of the tumor, safe and effective complete resection cannot be
achieved. Al-Shanafey and Habib (5) report that among 18 children with
abdominal neurogenic tumors treated by laparoscopic surgery, two
cases were converted to laparotomy due to renal vein tumor invasion
and limited visual field and three cases with stage IV
neuroblastoma had in situ recurrence following operation.
Although there are no absolute contraindications for endoscopic
neuroblastoma, tumor diameter >6 cm, blocked venous return and
invasion of adjacent organs or blood vessels should be relative
contraindications for laparoscopy. Owing to the lack of a large
number of statistical analysis results of clinical data, the
International Pediatric Endosurgery Group (IPEG) suggests that the
indication of laparoscopic surgery should be tumor diameter <6
cm, IDRFs negative and no obvious surrounding tissue invasion
adhesion (8). In the present case,
the tumor size was >6 cm at the initial diagnosis, IDRFs was
positive and the tumor surrounded the right renal artery, vein and
inferior vena cava, which was not suitable for surgery. Although
the tumor still involved the right renal artery and vein after
three cycles of preoperative chemotherapy, laparoscopic surgery was
performed for the child because the tumor size was significantly
reduced to <6 cm, which provided sufficient procedure space for
operation and the surgeon had professional skills in laparoscopic
surgery.
In laparoscopic surgery, the tumor is removed by
splitting it into small pieces. In the present case, the tumor was
difficult to expose and the right kidney artery and vein passed
through the tumor. Even if open surgery was performed, the tumor
needed to be split and segmented. Depending on the surgeon's
experience in laparoscopic technology, combined with preoperative
IDRFs, an ultrasound knife was used to split the tumor along the
blood vessels, remove the tumor in pieces and complete lymph node
dissection, so as to achieve the same effect as open surgery.
Meanwhile, the patient could suffer less trauma and experience fast
recovery. Ultrasonic knife was used for precise dissection. When
cutting tumor tissue with ultrasonic knife, a high enough
temperature (controlled at 100˚C) inactivated the tumor cells in
the cutting plane. At the same time, the tumor bed was washed with
sterilized water. This can effectively prevent the spread of tumor
cells during tumor resection. It was safe and effective to split
and free the tumor along the blood vessels without spreading
pollution and the wound surface was clean and dissected clearly. In
addition, TRIPORT was used through the umbilical fossa and the
protective sleeve was used to protect the incision to avoid tumor
planting and, at the same time, it was convenient to remove the
specimen while the tumor was cut into small pieces. The incision
scar was not obvious (Fig. 3I) and
the aesthetic effect was good. Moreover, local chemotherapy
immersion irrigation after resection of tumor can effectively
reduce tumor recurrence in situ. Postoperative chemotherapy
was started two weeks after the operation, which benefited from the
rapid recovery of minimally invasive technology of laparoscopic
surgery, indicating that the timely continuation of postoperative
chemotherapy is also an important factor for the good treatment
effect of this case.
To sum up, for children suffering from neuroblastoma
with large tumor volume and vascular invasion, preoperative
chemotherapy can be given and minimally invasive laparoscopic
surgery can be one of options to be considered when the tumor size
is <6 cm. During the operation, the tumor tissue can be removed
by segmental resection and the removal of as much tumor tissue as
possible is an important factor to improve the prognosis.
Laparoscopic minimally invasive surgery has little trauma and quick
recovery and children can receive postoperative chemotherapy as
early as possible, which is conducive to good recovery. Basically,
the prerequisite and requirements for performing this operation are
professional laparoscopic skills and an experienced team.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article
Authors' contributions
GH analysed the data and wrote the original draft.
GY was responsible for data acquisition and participated in the
writing of the original manuscript. GH an GY agreed to be
accountable for all aspects of the work in ensuring that questions
related to the accuracy or integrity of any part of the work are
appropriately investigated and resolved. WH and YS made substantial
contributions to conception and acquisition of data. ML made
substantial contributions to analysis and interpretation of data.
SL made substantial contributions to conception and design of the
study, replied to the reviewers' comments and took responsibility
for communication with the journal. ML and WH confirm the
authenticity of all the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was conducted in accordance with the
principles of the Declaration of Helsinki and the study protocol
was approved by the ethics committee of Xiamen University.
Patient consent for publication
The data and pictures used in the present study were
authorized by the parents of the child.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liu KX and Joshi S: ʻRe-educatingʼ tumor
associated macrophages as a novel immunotherapy strategy for
neuroblastoma. Front Immunol. 11(1947)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chung C, Boterberg T, Lucas J, Panoff J,
Valteau-Couanet D, Hero B, Bagatell R and Hill-Kayser CE:
Neuroblastma. Pediatr Blood Cancer. 68 (Suppl
2)(e28473)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Acker SN, Bruny JL, Garrington TP and
Partrick DA: Minimally invasive surgical techniques are safe in the
diagnosis and treatment of pediatric malignancies. Surg Endosc.
29:1203–1208. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fascetti-Leon F, Scotton G, Pio L, Beltrà
R, Caione P, Esposito C, Mattioli G, Saxena AK, Sarnacki S and
Gamba P: Minimally invasive resection of adrenal masses in infants
and children: Results of a European multi-center survey. Surg
Endosc. 31:4505–4512. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Al-Shanafey S and Habib Z: Feasibility and
safety of laparoscopic adrenalectomy in children: Special emphasis
on neoplastic lesions. J Laparoendosc Adv Surg Tech A. 18:306–309.
2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gurria JP, Malek MM, Heaton TE, Gehred A,
Lautz TB, Rhee DS, Tracy ET, Grant CN, Baertshiger RM, Bruny J, et
al: Minimally invasive surgery for abdominal and thoracic
neuroblastic tumors: A systematic review by the APSA cancer
committee. J Pediatr Surg. 55:2260–2272. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Leclair MD, de Lagausie P, Becmeur F,
Varlet F, Thomas C, Valla JS, Petit T, Philippe-Chomette P, Mure
PY, Sarnacki S, et al: Laparoscopic resection of abdominal
neuroblastoma. Ann Surg Oncol. 15:117–124. 2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
International Pediatric Endosurgery Group.
IPEG guidelines for the surgical treatment of adrenal masses in
children. J Laparoendosc Adv Surg Tech A. 20:7–9. 2010.PubMed/NCBI View Article : Google Scholar
|