Introduction
Hepatic portal venous gas (HPVG) was first described
in 1955 as abnormal gas found on abdominal plain radiographs in
infants. In 1978 HPVG was reported to have a mortality rate of 75%
(1,2). HPVG is associated with necrotizing
colitis (2) and was therefore
previously regarded as a lethal condition. However, HPVG is now
known to not be a specific disease entity but merely a rare
condition in patients suffering from acute abdomen (3). HPVG is mostly caused by intestinal
ischemia, intra-abdominal abscesses, necrotizing enterocolitis,
abdominal trauma, infectious enteritis and inflammatory bowel
disease (4).
In recent decades, with an increase in the
popularity of CT scans, the number of patients diagnosed with HPVG
has increased and some patients have been treated without surgery
(5). The clinical features and
management of HPVG have greatly changed with the rapid development
of diagnostic tools and treatments. However, numerous previous
studies of HPVG are reported in the form of single case report and
therefore lack representation. Therefore, the aim of the present
study was to investigate the characteristics, diagnosis, treatment
and prognosis of HPVG in 20 patients.
Materials and methods
Patients
In the present study, 20 patients with HPVG, which
was diagnosed using a CT scan, were selected at the Tongji
University School of Medicine affiliated with Yangpu Hospital
(Shanghai, China) between December 2015 and December 2020. Of the
patients selected 70% were female (mean age of all patients, 75.4
years). The main complaint from the patients was abdominal pain and
among them patients with cancer had a history of surgery or
chemotherapy. Moreover, none of the patients had a history of HPVG.
The medical records and radiology films were reviewed
retrospectively. All patients were enrolled and were identified
using a search engine, whereby all CT radiology reports were
examined that contained the words ‘pneumatosis’ and/or ‘portal
venous’ ‘gas/air’. The data that were collected and analyzed
included sex, age, laboratory evidence, etiologies at admission,
therapeutic method and in-hospital mortality. All patients provided
written informed consent. The research received approval from the
ethics committee of Yangpu hospital (approval no. YP20201102023).
The reporting of this study conformed to Strengthening the
Reporting of Observational Studies in Epidemiology guidelines
(6).
Diagnosis and treatment
Routine blood tests, biochemical examinations and CT
scans were performed at admission. Blood tests and biochemical
examination indicators identified red blood cells, white blood
cells, platelets, hemoglobin, neutrophils, C-reactive protein
(CRP), procalcitonin (PCT), D-dimer (DD-I), alanine
aminotransferase and aspartate aminotransferase levels. The
diagnosis of HPVG was confirmed by a radiologist and surgeon.
Conservative treatment and/or surgery were selected according to
the specific condition of each patient. Conservative treatment
mainly included fluid infusion and antibiotic therapy, atomizing
inhalation and gastrointestinal decompression. Surgery included
enterodialysis and enterectomy, gastrointestinal cancer resection
and hernioplasties of oblique hernia.
Statistical analysis
Continuous parameters are presented as the mean and
ranges. Discrete variables are presented as numbers and
percentages.
Results
A total of 20 patients were diagnosed with HPVG
during the study period. Patient information is presented in
Table I. The results demonstrated
that the average CRP, PCT and DD-I levels were higher compared with
normal levels. The etiologies of the 20 patients with HPVG included
abdominal infection, pulmonary infection and hemorrhage. The
comorbidities included hypertension, diabetes, coronary disease,
cerebrovascular disease and renal insufficiency. The proportions of
each etiology and comorbidity in the enrolled patients are
summarized in Table II.
 | Table ICharacteristics of 20 patients with
HPVG. |
Table I
Characteristics of 20 patients with
HPVG.
| Characteristic | Value |
|---|
| Total | 20 |
| Sex (%) | |
|
Female/Male | 14 (70%)/6 (30%) |
| Age (years) | |
|
Average
(range) | 75.4 (20-94) |
|
Female/Male | 79 (20-94)/67.8
(48-87) |
|
Combined
with MVG (%) | 12 (60%) |
| RBC
(1012/l) | |
|
Normal value
(Female/Male, range) | 3.5-5.0/4.0-5.5 |
|
Average
(range) | 3.9 (2.7-5.7) |
| WBC
(109/l) | |
|
Normal value
(range) | 4-10 |
|
Average
(range) | 9.4 (2.5-20.2) |
| PLT
(109/l) | |
|
Normal value
(range) | 100-400 |
|
Average
(range) | 198.8 (96-385) |
| HB (g/l) | |
|
Normal value
(Female/Male, range) | 110-150/120-160 |
|
Average
(range) | 119.6 (68-166) |
| N (Neutrophil,
%) | |
|
Normal value
(range) | 50-70 |
|
Average
(range) | 75.4 (46.8-96) |
| CRP (mg/l) | |
|
Normal value
(range) | 0-5 |
|
Average
(range) | 46.1 (0.9-200) |
| PCT (ng/l) | |
|
Normal value
(range) | 0-0.3 |
|
Average
(range) | 8.5 (0.1-44.7) |
| DD-I (D-Dimer,
mg/l) | |
|
Normal value
(range) | 0-0.5 |
|
Average
(range) | 4.2 (0.6-8.1) |
| ALT (U/l) | |
|
Normal value
(range) | 0-40 |
|
Average
(range) | 38.6 (6-140) |
| AST (U/l) | |
|
Normal value
(range) | 0-40 |
|
Average
(range) | 50.5 (16-229) |
 | Table IIEtiologies and comorbidities of 20
patients with HPVG. |
Table II
Etiologies and comorbidities of 20
patients with HPVG.
| Type | Value (%) |
|---|
| Etiologies | |
|
Abdominal
infection | 15(75) |
|
Strangulated
intestinal obstruction | 2(10) |
|
Simple
intestinal obstruction | 3(10) |
|
Simple
intestinal obstruction with cerebral infarction | 1(5) |
|
Simple
intestinal obstruction with pulmonary infection | 1(5) |
|
Acute
enteritis | 7(35) |
|
Pulmonary
infection | 5(25) |
|
Simple
pulmonary infection | 2(10) |
|
Pulmonary
infection with simple intestinal obstruction | 1(5) |
|
Pulmonary
infection with pyloric obstruction | 1(5) |
|
Hemorrhage | 2(10) |
|
Hemorrhage
of digestive tract | 1(5) |
|
Cerebellar
hemorrhage | 1(5) |
| Comorbidities | |
|
Hypertension | 10(50) |
|
Diabetes | 6(30) |
|
Coronary
disease | 6(30) |
|
Cerebrovascular
disease | 5(25) |
In the present study, six patients required surgery;
however, two of the patients rejected the operation. The remaining
16 patients received conservative treatment. For one patient with a
strangulated intestinal obstruction, enterodialysis and an
enterectomy were performed. For two patients with gastrointestinal
cancer, resections were performed to relieve the symptoms of the
obstruction. An inguinal hernia was treated with a hernioplasty in
one patient. The overall in-hospital mortality rate was 25%. Among
the 20 cases of HPVG, two patients with strangulated intestinal
obstructions and three patients with a multiplicity of infection
succumbed, which included simple intestinal obstruction with
pulmonary infection, simple intestinal obstruction with cerebral
infarction and severe pulmonary infection with simple intestinal
obstruction. The rate of HPVG absorption ranged from 2-8 days, with
a mean time of 4.2 days. This was determined to be unrelated to the
outcome of the disease. The details that were collected and
analyzed are presented in Table
III.
 | Table IIITreatment and prognosis of
patients. |
Table III
Treatment and prognosis of
patients.
| Variable | Value |
|---|
| Meeting surgical
indications | 6 (30%) |
|
Operation | 4 (20%) |
|
Enterodialysis
and enterectomy | 1 (5%) |
|
Gastrointestinal
cancer resection | 2 (5%) |
|
Hernioplasty
of oblique hernia | 1 (5%) |
|
Conservative
treatment | 16 (80%) |
| In-hospital
mortality (%) | 5 (25%) |
|
Strangulated
intestinal obstruction | 2 (10%) |
|
Simple
intestinal obstruction with pulmonary infection | 1 (5%) |
|
Simple
intestinal obstruction with cerebral infarction | 1 (5%) |
|
Severe
pulmonary infection with simple intestinal obstruction | 1 (5%) |
| Time of gas
absorption, day | |
|
Average
(range) | 4.2 (2-8) |
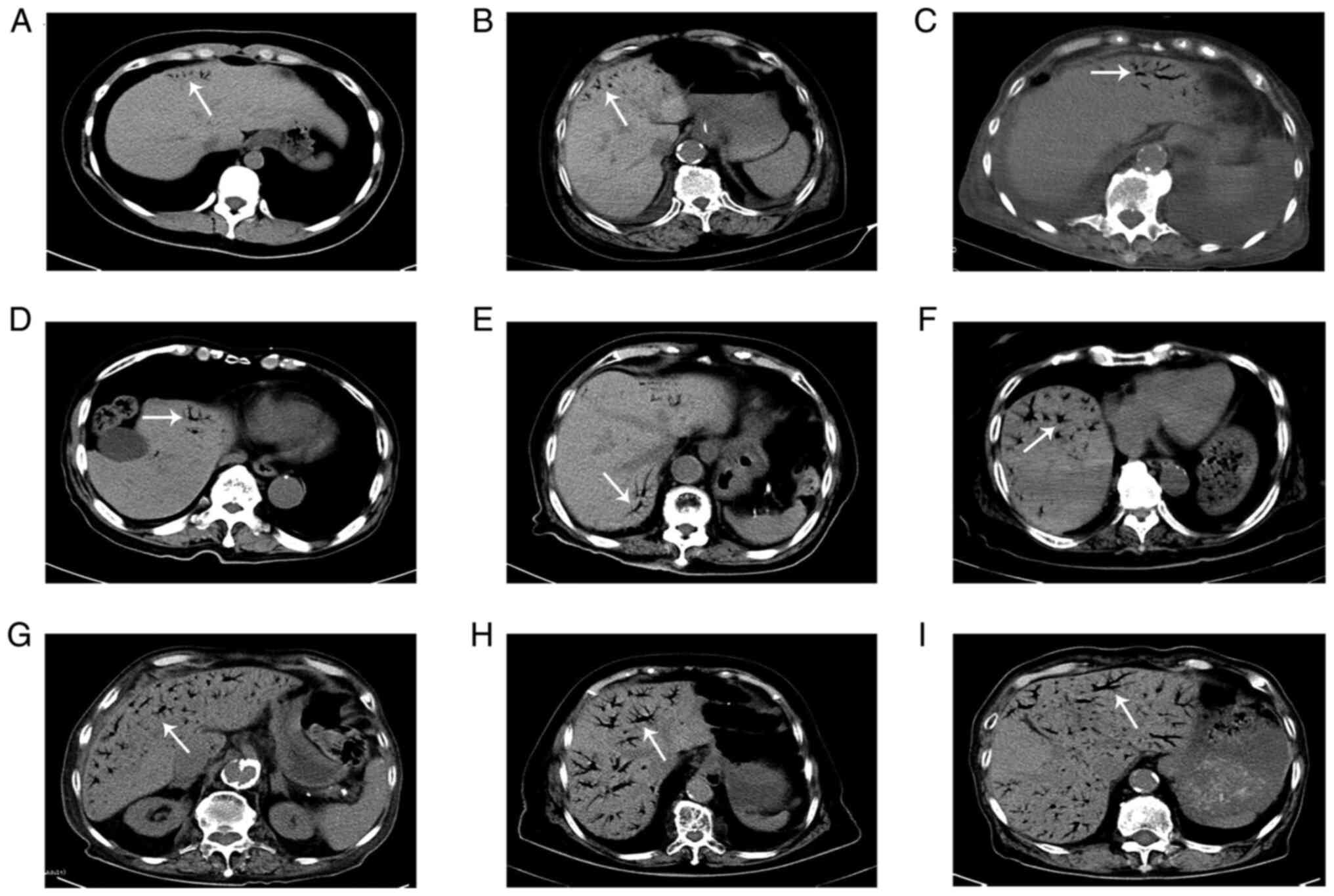
The imaging results for HPVG demonstrated branching
radiolucency that extended to within 2 cm of the liver capsule.
Furthermore, 60% of patients with HPVG also had mesenteric venous
gas. Overall, nine typical imaging results of HPVG were identified
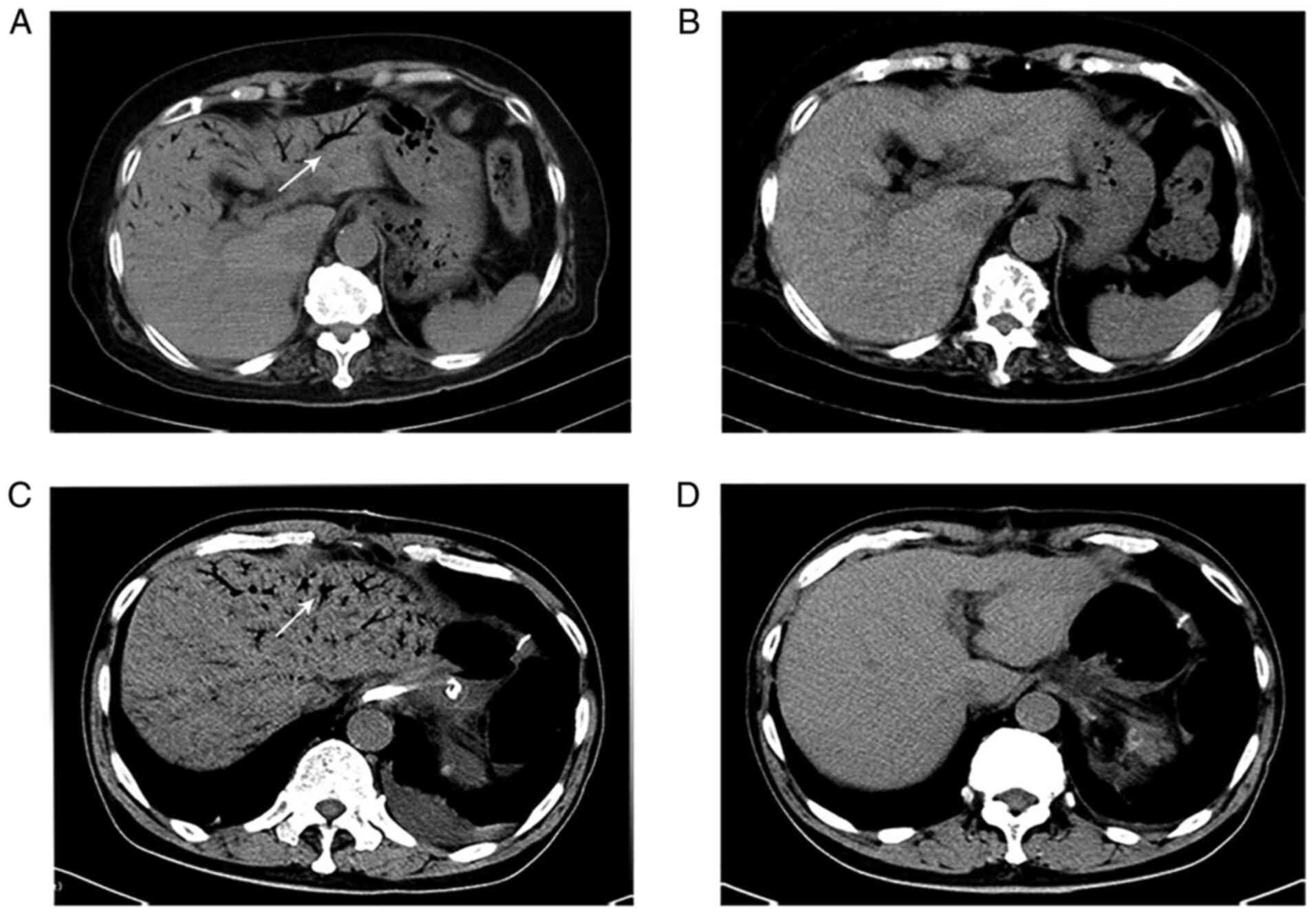
in the present study and are presented in Fig. 1. The CT scans of two recovered
patients, with different degrees of HPVG, were selected to
demonstrate the changes before and after gas absorption; these
images are presented in Fig.
2.
Discussion
HPVG is rare radiological finding and can be
indicative of several diseases, including inflammatory bowel disease
and obstructive gastrointestinal disease, as well as potentially
life-threatening conditions, such as mesenteric ischemia (4). With an increase in the use of CT
scans during the early diagnosis of HPVG, the clinical outcome of
patients has improved due to accurate diagnosis and early
treatment. However, the pathogenesis of HPVG remains to be fully
elucidated. At present two hypotheses of how HPVG originates have
been proposed. One is that high-pressure gas from the bowel lumen
circulates into the venous system via vascular endothelial
injuries, such as abdominal trauma, bowel ischemia, or as a
consequence of diagnostic or therapeutic invasive procedures, such
as enteral nutrition. However, other studies have hypothesized that
abdominal infections can release gas-producing bacteria into the
portal venous system (7-11).
In the present study, patients with HPVG were
relatively older with an average age of 75.4 years. However, the
youngest patient included was 20 years old. These results indicated
that old age may be an important factor in HPVG. Moreover, even
though the majority of enrolled patients were women, there was no
evidence that suggested that sex significantly determined which
individuals would be more likely to get HPVG. A previous study
concerning HPVG that was performed in Japan similarly reported that
a statistical difference was found in the age of patients but not
sex (12). In terms of
inflammatory markers, PCT and CRP were demonstrated to be
important. As a degradation product of cross-linked fibrin, DD-I
induces venous thrombosis when inflammation occurs. In the present
study, the average levels of CRP, PCT and DD-I were higher than the
normal levels, which indicated a severe inflammatory state. From
these results, it can be hypothesized that most etiologies have a
close association with inflammation and vascular injury, which are
potentially triggering factors for HPVG. In the present study
abdominal infection, pulmonary infection and hemorrhage were major
etiologies, whereas hypertension, diabetes, cardio-cerebrovascular
disease and renal insufficiency were major comorbidities. These
results demonstrated that both inflammation and injury of blood
vessels may potentially induce HPVG, which was consistent with the
aforementioned conclusion. However, a single case of hemorrhage in
the present study was a result of cerebellar hemorrhage rather than
abdominal trauma. Furthermore, five cases of infection were caused
by pulmonary infection rather than abdominal infection. These
results also indicated that not only hemorrhage of the digestive
tract and abdominal infection can potentially induce HPVG, but also
injury of the blood vessels and infection in other organs.
In a previous study it was reported that HPVG is a
lethal condition and is related to mesenteric ischemia, which is
associated with extended bowel necrosis (13). However, different conclusions were
drawn from the results of the present study. Most of the enrolled
patients relied on CT examination to confirm the diagnosis of HPVG.
This is because CT has a high sensitivity and is considered to be
the gold standard method for medical imaging (14). Wiesner et al (15) report that contrast-enhanced CT is a
powerful investigatory tool to differentiate HPVG with acute
mesenteric ischemia from HPVG with a non-ischemic pathology, which
exhibits bowel wall thickening, either marked or absent enhancement
of the bowel wall, intramural pneumatosis, mesenteric edema,
ascites, mesenteric or portal venous gas and mesenteric arterial or
venous thromboembolism. CT images in the present study demonstrated
intrahepatic branching radiolucencies with various amounts of gas.
Furthermore, the results determined that a hemodynamic disorder of
the intestinal tract and a combination of different types of severe
infection, which indicated a severe inflammatory state, were more
likely to induce patient mortality. Moser et al (16) report that if HPVG is present in
combination with a necrotic bowel, the mortality risk is >50%.
Therefore, when ischemia is suspected, HPVG is an ominous sign that
indicates progression to necrosis, especially when associated with
a high level of lactate (17).
However, it should be considered that HPVG alone does not lead to
patient mortality. The present study demonstrated that the time of
portal venous gas absorption ranged from 2-8 days, with a mean time
of 4.2 days, which was unrelated to the outcome of the disease.
Moreover, the results of the present study demonstrated that the
prognosis of a patient was not directly proportional to the volume
of HPVG or the number of liver segments containing the venous gas.
However, Kinoshita et al (7) report that the involvement of three or
more segments is an important sign that indicates a potentially
lethal outcome and is correlated with a poor prognosis in 75% of
cases. The main differential diagnosis for HPVG is pneumobilia,
which is detected centrally within the liver rather than extending
to the peripheral parenchyma (18). In certain cases, pneumobilia and
HPVG may coexist depending on the etiology (7). Moreover, in the present study, 60% of
patients were confirmed by abdominal CT to have gas present in the
portal vein, which was accompanied by the presence of gas in the
mesenteric vein. It can therefore be hypothesized that this
phenomenon is related to their interlinked anatomic structure and
that gas potentially moves via connected blood vessels.
Treatment for HPVG is dependent on the clinical
presentation of the patient, imaging and laboratory evidence. Koami
et al (19) report that
HPVG is not a predictor of urgent surgery and high mortality if
there is no obvious clinical evidence of ischemia or necrosis.
Moreover, Wayne et al (17)
demonstrate that treatment for HPVG should be directed at the
underlying disease and the need for an emergency operation should
be determined based on the primary disease, with consideration of
the high mortality rate of HPVG associated with bowel necrosis. In
the present study, six patients met the criteria for surgery;
however, two patients rejected surgery because of the associated
risk. Conservative treatment was therefore performed due to the
absence of clinical and radiographic evidence of a hemodynamic
disorder of the intestinal tract. An urgent exploratory laparotomy
was only mandatory in one patient, in which intestinal ischemia or
infarction was suspected based on clinical and radiologic evidence.
Furthermore, a 92-year-old woman, who underwent enterodialysis and
an enterectomy, succumbed with a strangulated intestinal
obstruction, which had been suspected based on clinical and
radiologic evidence. It was hypothesized that old age and
complicated underlying diseases may have been the cause of the
mortality. However, the HPVG disappeared within two days but the
patient still succumbed. In addition, a previous study reports that
for a patient with extensive comorbidities, in old age, surgery may
also not be survivable (17). In
the present study, the overall in-hospital mortality rate was
determined to be 25%, which was consistent with other previous
studies where mortality rates decreased in the range of 27-47%
(13,20). From the aforementioned results it
can be determined that surgical intervention is not a requisite
therapeutic method but should still be investigated. Furthermore,
surgery should not generally be performed if the patient is
clinically stable and there is only radiological evidence of HPVG
(21,22). At present, gastrointestinal
decompression and antibiotic treatment are routine conservative
therapies. Previous studies have reported that certain cases of
HPVG occur without necrosis and these cases can be treated
successfully with medication, which is consistent with the
conclusion of the present study (23,24).
Moreover, emergency surgery should be performed immediately in the
presence of an obvious peritonitis symptom, which may indicate the
presence of a hemodynamic disorder of the intestinal tract, even if
there are no signs of ischemia on the CT scan (25).
In conclusion, in the present study, the limited
number of HPVG cases restricted any deeper analysis and the
conclusions may be partly controversial, such as the relationship
between HPVG levels or the time of HPVG absorption and the
prognosis of the disease. Furthermore, patients with HPVG caused by
abdominal trauma and/or a consequence of diagnostic or therapeutic
invasive procedures, such as colonoscopy or enteral nutrition, were
not identified and enrolled in the present study. Large-scale data
on HPVG is needed for future investigations.
Acknowledgements
The authors thank Dr Cui Tang (Department of
Radiology, Yangpu Hospital, Tongji University, Shanghai, China) who
provided technical assistance.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YZ analyzed the patient data and wrote the
manuscript. HLL designed the present study. HLL and MBL confirm the
authenticity of all the raw data. MT and HW participated in data
analysis and interpretation. HHJ was involved in the design of the
study and revised the manuscript. MBL made substantial
contributions to conception and agreed to be accountable for all
aspects of the work. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study received ethics approval from the
ethics committee of Yangpu Hospital (approval no. YP20201102023)
and informed consent was obtained from all participants.
Patient consent for publication
All patients provided written informed consent. They
consented to the images being taken for the purpose of research and
also consented to their publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wolfe JN and Evans WA: Gas in the portal
veins of the liver in infants; a roentgenographic demonstration
with postmortem anatomical correlation. Am J Roentgenol Radium Ther
Nucl Med. 74:486–489. 1955.PubMed/NCBI
|
|
2
|
Liebman PR, Patten MT, Manny J, Benfield
JR and Hechtman HB: Hepatic-portal venous gas in adults: Etiology,
pathophysiology and clinical significance. Ann Surg. 53:231–234.
1978.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Capolupo GT, Masciana G, Carannante F and
Caricato M: Hepatic portal venous gas after colonoscopy: A case
report and review. Int J Surg Case Rep. 51:54–57. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Alqahtani S, Coffin CS, Burak K, Chen F,
Gregor JM and Beck P: Hepatic portal venous gas: A report of two
cases and a review of the epidemiology, pathogenesis, diagnosis and
approach to management. Can J Gastroenterol. 21:309–313.
2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hou SK, Chern CH, How CK, Chen JD, Wang LM
and Lee CH: Hepatic portal venous gas: Clinical significance of
computed tomography findings. Am J Emerg Med. 22:214–218.
2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
von Elm E, Altman DG, Egger M, Pocock SJ,
Gøtzsche PC and Vandenbroucke JP: STROBE Initiative. The
Strengthening the Reporting of Observational Studies in
Epidemiology (STROBE) Statement: Guidelines for reporting
observational studies. Int J Surg. 12:1495–1499. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kinoshita H, Shinozaki M, Tanimura H,
Umemoto Y, Sakaguchi S, Takifuji K, Kawasaki S, Hayashi H and
Yamaue H: Clinical features and management of hepatic portal venous
gas: Four case reports and cumulative review of the literature.
Arch Surg. 136:1410–1141. 2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shah PA, Cunningham SC, Morgan TA and Daly
BD: Hepatic Gas: Widening Spectrum of Causes Detected at CT and US
in the Interventional Era. Radiographics. 31:1411–1413.
2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Suzuki S, Takeuchi Y, Ishihara R and
Kawakami H: Hepatic portal venous gas following colonic endoscopic
submucosal dissection. Internal Med. 58:755–756. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Solakoglu T, Sari SO, Koseoglu H, Basaran
M, Akar M, Buyukasik S and Ersoy O: A case of hepatic portal venous
gas after colonoscopy. Arab J Gastroenterol. 17:140–142.
2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Matsuoka T, Kobayashi K, Lefor AK, Sasaki
J and Shinozaki H: Mesenteric ischemia with pneumatosis
intestinalis and portal vein gas associated with enteral nutrition:
A series of three patients. Clin J Gastroenterol. 13:1160–1164.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Koizumi C, Michihata N, Matsui H, Fushimi
K and Yasunaga H: In-hospital mortality for hepatic portal venous
gas: Analysis of 1590 patients using a japanese national inpatient
database. World J Surg. 42:816–822. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
McElvanna K, Campbell A and Diamond T:
Hepatic portal venous gas-three non-fatal cases and review of the
literature Ulster Med. J. 81:74–78. 2012.PubMed/NCBI
|
|
14
|
Moussa M, Marzouk I, Abdelmoula K,
Manamani A, Dali N, Farhat LC and Hendaoui L: Role of Computed
tomography in predicting prognosis of Hepatic portal venous gas.
Int J Surg Case Rep. 30:177–182. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wiesner W, Khurana B, Ji H and Ros PR: CT
of acute bowel ischemia. Radiology. 226:635–650. 2003.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Moser A, Stauffer A, Wyss A, Schneider C,
Essig M and Radke A: Conservative treatment of hepatic portal
venous gas consecutive to a complicated diverticulitis: A case
report and literature review. Int J Surg Case Rep. 23:186–189.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wayne E, Ough M, Wu A, Liao J, Andresen
KJ, Kuehn D and Wilkinson N: Management algorithm for pneumatosis
intestinalis and portal venous gas: Treatment and outcome of 88
consecutive cases. J Gastrointest Surg. 14:437–448. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Soon WC, Liu KY and Blunt D: Hepatic
portal venous gas. Clin Case Rep. 3:518–519. 2015.PubMed/NCBI View
Article : Google Scholar
|
|
19
|
Koami H, Isa T, Ishimine T, Kameyama S,
Matsumura T, Yamada KC and Sakamoto Y: Risk factors for bowel
necrosis in patients with hepatic portal venous gas. Surg Today.
45:156–161. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nelson AL, Millington TM, Sahani D, Chung
RT, Bauer C, Hertl M, Warshaw AL and Conrad C: Hepatic portal
venous gas: The ABCs of management. Arch Surg. 144:575–581.
2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Shah A, Al Furajii H and Cahill RA:
Symptomatic pneumatosis intestinalis (including portal venous gas)
after laparoscopic total colectomy. World J Gastrointest Endosc.
6:564–567. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Iwai N, Handa O, Naito Y, Dohi O, Okayama
T, Yoshida N, Kamada K, Uchiyama K, Ishikawa T, Takagi T, et al:
Stenotic ischemic enteritis with concomitant hepatic portal venous
gas and pneumatosis cystoides intestinalis. Internal Med.
57:1995–1999. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hong I, Hong SW, Chang YG, Lee B, Lee WY,
Ohe HJ and Kim YK: Successful conservative management of hepatic
portal venous gas due to anastomosis leakage after a sigmoidectomy.
Ann Coloproctol. 35:282–284. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yasuda T, Yagi N, Nakahata Y, Kurobe T,
Yasuda Y, Omatsu T, Obora A and Kojima T: A case of phlegmonous
gastritis with hepatic portal venous gas caused by Aeromonas
hydrophila successfully treated with medication. Clin J
Gastroenterol. 13:281–286. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Dibra R, Picciariello A, Trigiante G,
Labellarte G, Tota G, Papagni V, Martines G and Altomare DF:
Pneumatosis intestinalis and hepatic portal venous gas: Watch and
wait or emergency surgery? a case report and literature review. Am
J Case Rep. 21(e923831)2020.PubMed/NCBI View Article : Google Scholar
|