Introduction
Human hydatid disease is caused by the larval stages
of tapeworms of the genus Echinococcus. Cystic
echinococcosis is a parasitic disease which infects humans when the
ova, found in dog feces, are swallowed (1,2). In
Europe, hydatid disease is a common health problem, especially in
sheep-farming countries. Balkan countries, southern and insular
Italy, and central Spain have reported high incidence rates of
echinococcosis (1,2). When slowly growing cysts are found in
the viscera, echinococcosis must be considered. ELISA is a test
with a high sensitivity to detect antibodies against
Echinococcus granulosus (3). The liver is the most frequent primary
site of Echinococcus granulosus infection (60-70%), followed
by the lungs (10-15%) and spleen (2). Cardiac echinococcosis is a rare
occurrence and clinical manifestation depends on the location, size
and integrity of the cyst (1,2).
Among all infected patients, 0.5-2% exhibit cardiac involvement
(4,5). The prevalence of right ventricular
hydatid cysts is low (~10%) compared with the prevalence of left
ventricular cysts (60%) (5).
Cardiac hydatidosis can cause fatal complications, such as
anaphylactic shock, systemic embolism when the cyst is located in
the left ventricular outflow tract, or pulmonary embolism when it
is located in the right ventricular outflow tract (6-8).
Macroscopically, it has a uni- or multi-cystic cavity, filled with
fluid, containing small daughter cysts and hydatid sand (9). Microscopic examinations are essential
in order to establish the diagnosis. Surgery is the treatment of
choice (10), but the risk-benefit
ratio must be considered. The complete surgical removal of the
cyst(s) is the major prognostic factor of the cardiac manifestation
(3). Adjunctively, albendazole
should be adimistrated several days before surgery and a few weeks
after resection (11). The hydatid
cyst occurrence rate is 10% after surgery, but if medical treatment
is given, this rate can decrease (12). The present study emphasizes the
importance of considering cardiac echinococcosis as a potential
diagnosis in patients from endemic or farming areas.
Case report
The case of a 19-year-old male from a rural area,
who was admitted to a local Emergency Department (Hospital of
Buzau, Buzau, Romania) in April 2016 with anaphylactic shock, is
presented. Considering the patient's symptoms, including a mild
fever (37.5˚C), sharp right-sided thoracic pain and a dry cough, he
was referred to the Department of Pneumology. Chest radiography
indicated left lower lobe pneumonia and as the patient's CURB-65
(scored based on confusion; BUN, >20 mg/dl; respiratory rate,
≥30 breaths/min; blood pressure: Systolic, <90 mmHg; diastolic,
≤60 mmHg; and age, ≥65 years) score was 0, the patient received
amoxicillin and clavulanic acid (875/125 mg) twice-daily for 7 days
and was discharged. Over the next 10 days the patient's symptoms
worsened and he was admitted again to the same hospital and a
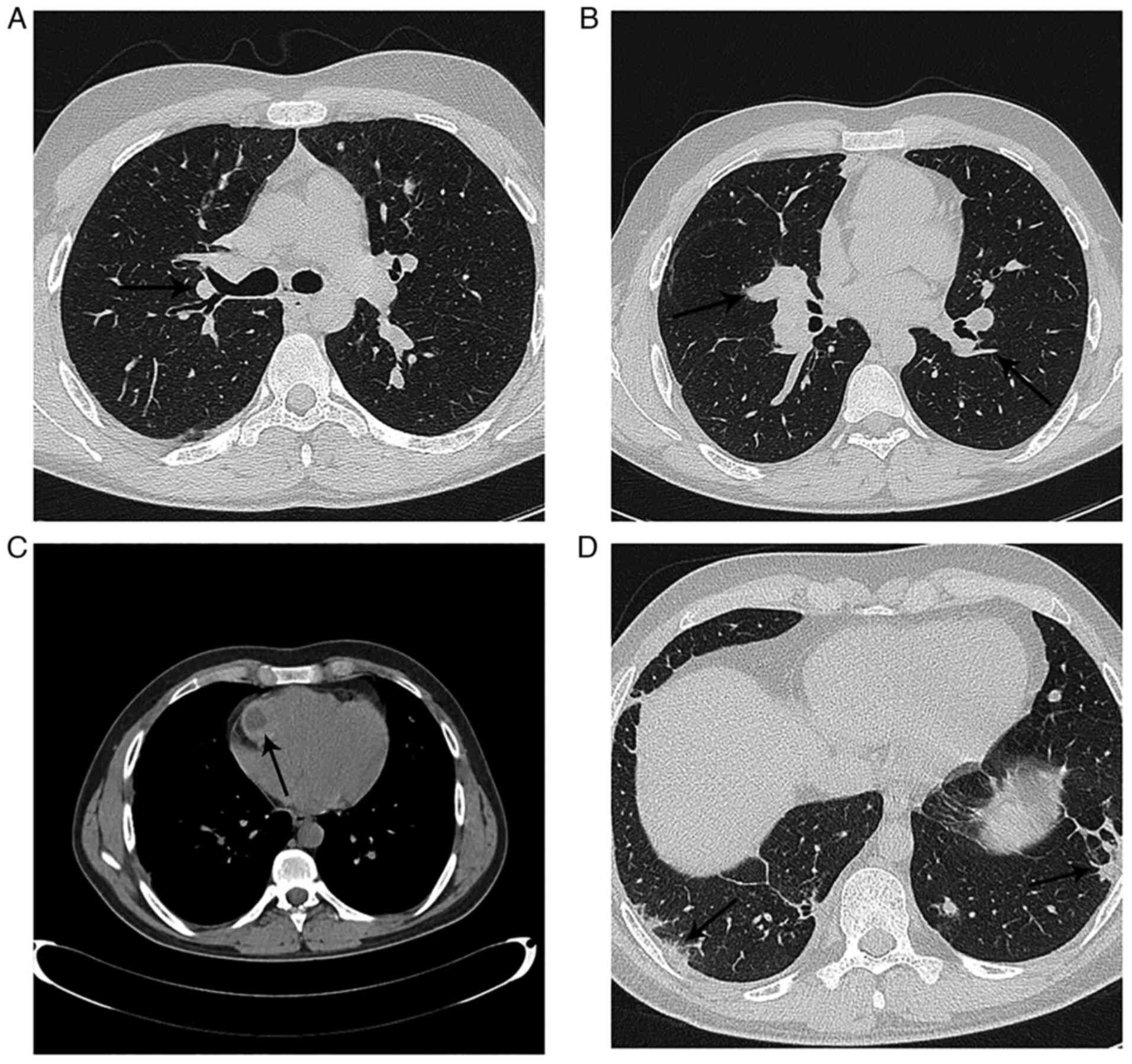
pulmonary CT scan was performed. The pulmonary CT-scan demonstrated
a bilateral pulmonary embolism of the segmental arteries (Fig. 1A and B), as well as a cystic mass on the right
ventricular free wall (Fig. 1C).
The patient was therefore referred to the Department of Cardiology
of the ‘Coltea’ Clinical Hospital (Bucharest, Romania).
Following admission to the Department of Cardiology,
the patient had no fever, was hemodynamically stable, had a normal
respiratory rate, had 94% oxygen saturation while breathing ambient
air and exhibited barely audible respiratory sounds in his left
lung basal segment, as well as fine rales. Routine laboratory tests
demonstrated eosinophilia (12.2%; normal cut off, 5%), elevated
D-dimer (464 ng/ml; normal cut off, 250 ng/ml) and elevated
C-reactive protein (3.9 mg/dl; normal cut off, 0.3 mg/dl) levels. A
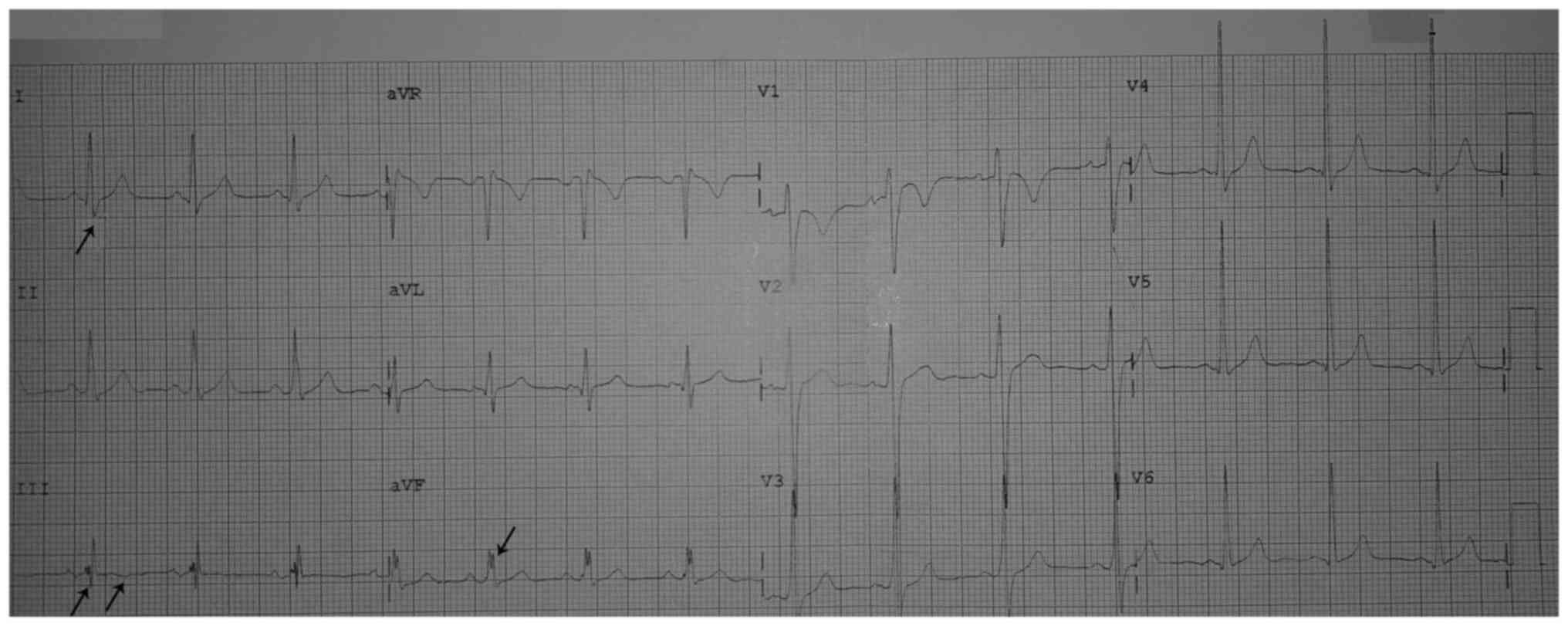
standard electrocardiogram demonstrated an S1Q3T3 pattern and
nonspecific intraventricular conduction delay in the inferior leads
(Fig. 2). Furthermore,
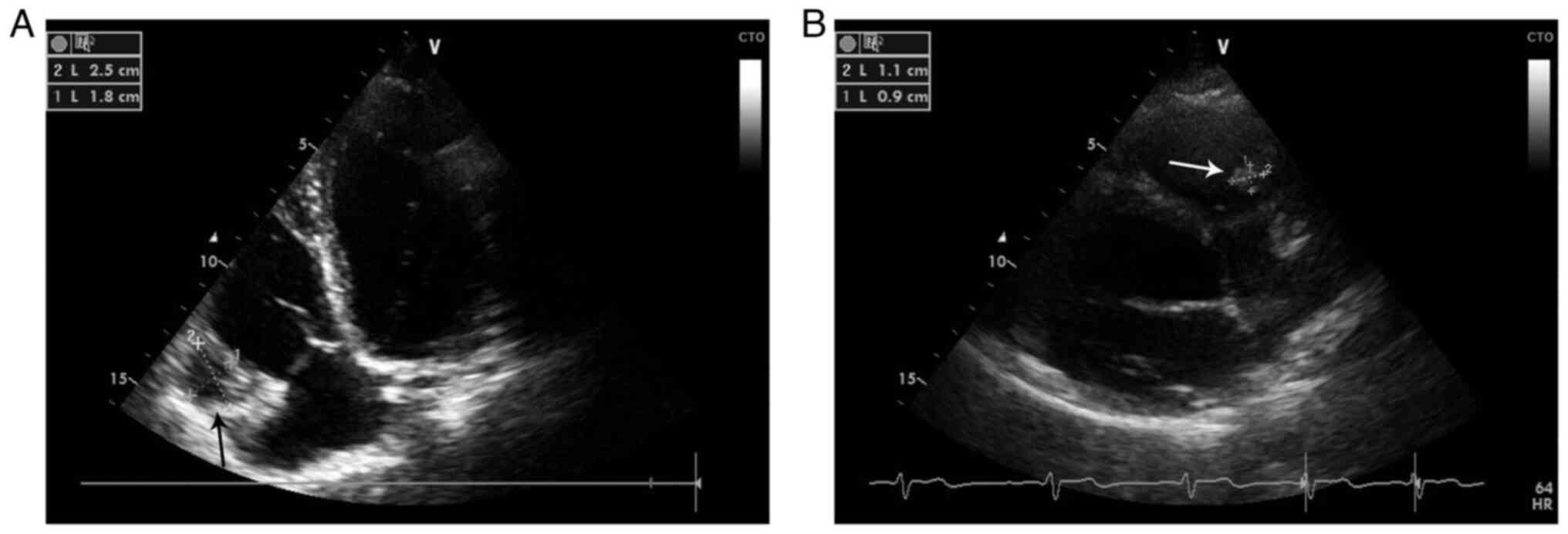
transthoracic echocardiography (TTE) revealed a slightly enlarged
right ventricle (RV), with moderate RV systolic dysfunction, as
well as a bi-lobular mass attached to the right ventricular free
wall adjacent to the right ventricular inflow, without causing any
inflow obstruction (Fig. 3A).
Transesophageal echocardiography did not provide any additional
information. Furthermore, at that time, the patient had no other
organ involvement. During hospitalization, the patient received low
molecular weight heparin (enoxaparin, 60 mg/0.6 ml twice-daily by
subcutaneous injection) and a parasitology exam was requested. The
ELISA assay (SERION ELISA Classic; SERION Diagnostics) was positive
for E. granulosus IgG antibodies (10.18 U/ml; normal cut
off, 1.1 U/ml) and therefore antiparasitic treatment using
albendazole (400 mg, twice daily) was administered. During
hospitalization, the clinical evolution improved and the patient
became stable and asymptomatic. The patient was discharged with
conservative treatment (albendazole, 400 mg twice-daily;
levocetirizine, 5 mg twice-daily) and a recommendation for cardiac
surgery evaluation, which the patient refused. In the first year of
clinical evolution, the patient was assessed in the Department of
Cardiology twice and was stable and asymptomatic. Serial
transthoracic echocardiograms demonstrated a marked reduction in
the dimensions of the RV cardiac cyst and an increase in its
echogenicity (Fig. 3B).
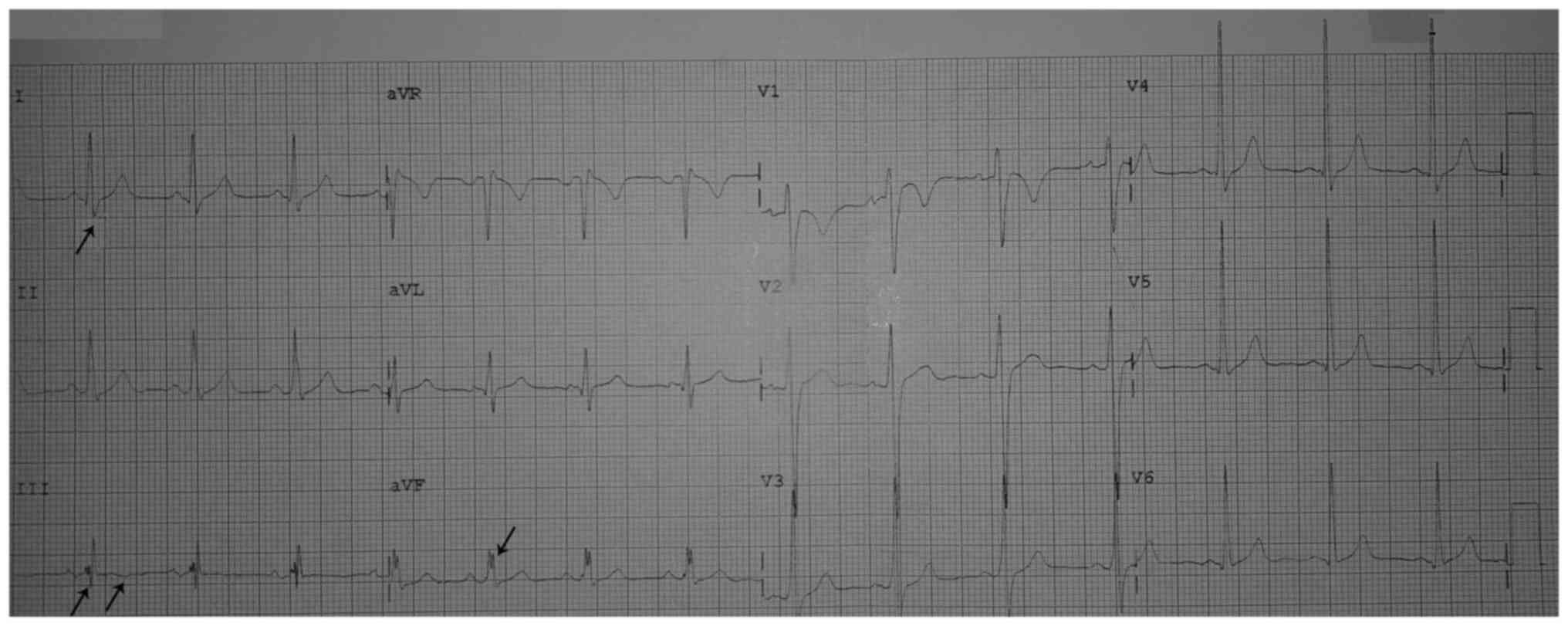 | Figure 2Standard electrocardiogram presenting
(on the initial presentation) normal sinus rhythm, normal QRS axis
(at 50˚), QRSD 120 msec, ventricular rate 80/min, S1Q3T3 pattern
(arrows) and nonspecific intraventricular conduction delay in DIII,
and aVF, QTc 404 msec. QTc, corrected QT interval; QRSD, QRS
duration; aVR, augmented right vector; aVL, augmented left vector;
aVF, augmented vector foot. |
After the first year, the patient was lost to
follow-up for 2 years, and during the subsequent year, the patient
presented at the Department of Pneumology with hemoptysis after
abandoning the antiparasitic treatment. A pulmonary CT-scan showed
bilateral central pulmonary nodules and subpleural pulmonary
nodules (Fig. 1D) and the patient
was referred for thoracic surgery where four hydatid cysts were
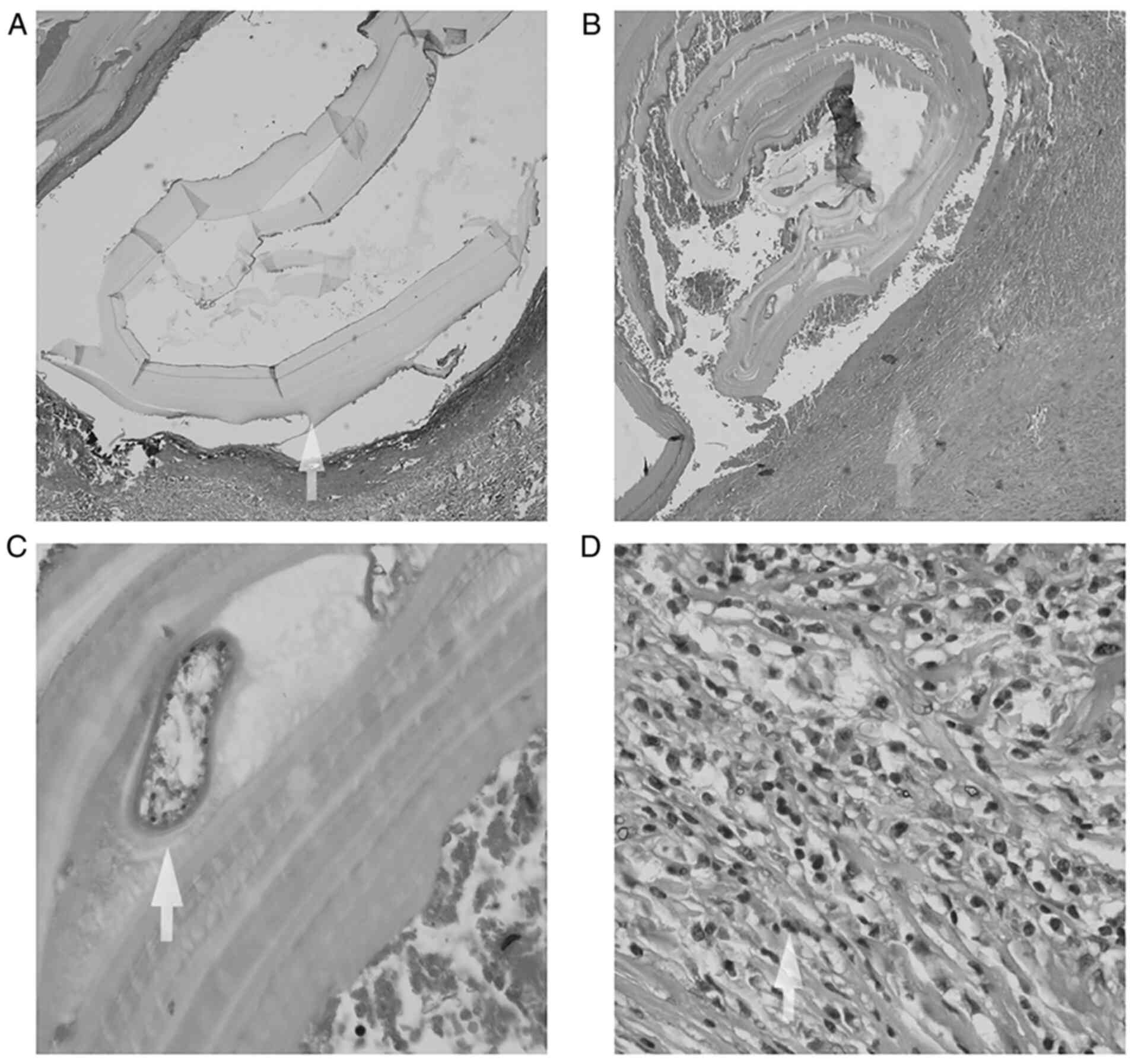
excised. Histological analysis confirmed the presence of pulmonary
hydatid cysts (Fig. 4) and it was
recommended that the patient resume antiparasitic treatment.
Literature review
A short PubMed (https://pubmed.ncbi.nlm.nih.gov/) literature review on
cardiac echinococcosis was performed. Search criteria included the
following keywords: ‘cardiac hydatid cyst echinococcosis’.
Considering that other reviews included cases that were published
up until 2018 (11,13), it was determined that cases
reported between 2018-2021 would be analyzed in the present study.
The collected data are presented in Table I.
 | Table IPubMed literature review of cases
reported between 2018 and 2021. |
Table I
PubMed literature review of cases
reported between 2018 and 2021.
| First author/s,
year | Age, years | Sex | Country | Symptom/s | Diagnostic
method/s | Localization | Size of cyst/s
(mm) | Medication/s | Surgery | Follow-up | (Refs.) |
|---|
| Firouzi et
al, 2019 | 57 | Male | Iran | Atypical chest
pain | TTE | Left ventricle/
right AV groove | 107x75 27x25 | Albendazole | Yes | - | (44) |
| Yimamu et
al, 2021 | 39 | Male | China | Asymptomatic | CT/TTE | Pericardium | 72x86 85x75 | Albendazole | Yes | 12 months no
recurrence | (49) |
| Singh et al,
2019 | 57 | Male | India | Syncope | TEE/CMR | Right
ventricle | 10x10 | Albendazole/
mebendazole | No | 12 months no
recurrence | (50) |
| Separovic
Hanzevacki et al, 2018 | 21 | Male | Croatia | Palpitations/
fatigue | TTE/CMR | Interventricular
septum | 68x28x51 (by
CMR) | Albendazole/
praziquantel | Yes | 6 months no
recurrence | (51) |
| Emam Hadi et
al, 2018 | 30 | Female | Iran | Shortness of
breath, heaviness on the chest, sudden death | Autopsy | Inferior vena
cava/right atrium/right ventricle | Multiple cysts, 30
(average) | - | - | - | (52) |
| Mesrati et
al, 2020 | 26 | Male | Tunisia | Mild chest pain,
syncope, sudden death | Autopsy | Right
ventricle | 50x49 | - | - | - | (53) |
| Kumar et al,
2020 | 32 | Female | India | Atypical chest
pain | TTE/CMR | Right
ventricle | 60x40 (by TTE)
35x59x45 (by CMR) | Albendazole | Yes | No data | (14) |
| Jamli et al,
2020 | 27 patients (mean
age, 35 years) | Male/ female,
1.7 | Tunisia | Atypical chest pain
(n=17), dyspnea (n=10), palpitations (n=16), other | TTE/TEE/ CMR | Right ventricle
(n=7) left ventricle (n=5) septal (n=5) other | No data | Albendazole | Yes (all) | 19 patients
follow-up (8.4±3.9 years) No recurrence | (64) |
| Wadhawa et
al, 2018 | 10 patients (mean
age, 35.9+12.04 years) | Male/ female,
1.4 | India | Dyspnea (n=7),
chest pain (n=7), fatigue (n=6), other | TTE/CT/ CMR | Left ventricle
(n=7)/ interventricular septum (n=2)/ pericardial (n=2) | 40x20 (minimum)
120x110 (maximum) | Albendazole | Yes (all) | 10 patients
follow-up (2 months- 5 years) No recurrence | (54) |
| Giri et al,
2020 | 79 | Female | Bhutan | Dyspnea | TTE/CT | Interventricular
septum | 67x76x82 | Albendazole | Yes | No data | (15) |
| Lu et al,
2019 | 44 | Female | China | Palpitations | CMR | Interventricular
septum and posterior apex of the left ventricle | 61x46 | No data | Yes | 16 months No
recurrence | (65) |
| Kuemmerl et
al, 2021 | 29 | Male | Southern
Europe | Syncope | CMR | Pericardium | 130 | Albendazole | Yes | 3 months No
recurrence | (16) |
| Çankaya et
al, 2021 | 20 | Female | Turkey | Dyspnea, chest
pain | TTE/CMR | Right
ventricle | 43x35x28 | Albendazole | Yes | No data | (17) |
| Iriz et al,
2020 | 15 | Female | Turkey | Atypical chest
pain | TTE/ CT/CMR | Interventricular
septum | 57x44x42 | Albendazole | Yes | No data | (18) |
| de Gregorio et
al, 2021 | 50 | Male | Italy | Dyspnea, atypical
chest pain | TTE/CT/ CMR | Interventricular
septum/ pericardium/ right ventricle outflow tract | No data | Albendazole | Yes | No data | (8) |
| Singh et al,
2019 | 28 | Male | India | Dyspnea | TTE/CT | Left ventricle/
pericardium | No data | Albendazole | No | No data | (50) |
| Singh et al,
2021 | 25 | Male | India | Dyspnea, chest
pain | TTE/TEE | Interventricular
septum | 69x56 | Albendazole/
praziquatel | Yes | Died on
postoperative day zero | (20) |
| Shakerian et
al, 2021 | 34 | Male | Iran | Dyspnea | TTE/CT | Right ventricle
outflow tract | 40x40 | Albendazole | Yes | No data | (21) |
| Alami et al,
2019 | 43 | Male | Morocco | Dyspnea, chest
pain | CT/MRI | Interventricular
septum | No data | Albendazole | Yes | 12 weeks No
recurrence | (22) |
| Cheng et al,
2021 | 48 | Male | China | Chest pain | TTE/CMR | Right
ventricle | 29x26 | Albendazole | No | No data | (23) |
| De et al,
2020 | 50 | Female | Vietnam | Dyspnea, chest
pain | Chest MRI | Left ventricle | 30x33 | Albendazole | Yes | 2 months No
recurrence | (24) |
| Rhissassi et
al, 2021 | 23 | Male | Morocco | Asymptomatic | TTE/CMR | Right
ventricle | 53x56 | Albendazole | Yes | No data | (25) |
| Jain et al,
2021 | 46 | Male | Turkmenistan | Dyspnea | TTE/ MRI/CT | Pericardium | No data | Albendazole | Yes | 1 month No
recurrence | (26) |
| Madisson- Bernardo
et al, 2019 | 49 | Male | Brazil | Dyspnea, atypical
chest pain | Chest MRI/ TTE | Pericardium | No data | Albendazole | No | 1 year No
recurrence | (27) |
| Kaskar et
al, 2020 | 14 | Female | India | Dyspnea | CT/TTE/ TEE | RV | 29x12 | Albendazole | Yes | 3 months No
recurrence | (28) |
| Handran et
al, 2020 | 47 | Male | Sudan | Syncope | CT/MRI | Interventricular
septum | 50x50 | No data | Yes | No data | (29) |
| Kohlmaier et
al, 2018 | 16 | Female | Austria | Dyspnea | TTE/CT/ MRI | RV | 40x40 | Albendazole/
praziquantel | Yes | 7 months Pulmonary
arterial hypertension (systolic arterial pressure, 50 mmHg) | (30) |
| Vural et al,
2019 | 22 | Male | Turkey | Angina | TTE/ Cineangio-
graphy | Left ventricle/
intracoronary | 20x20 | Albendazole | Yes | 1 year No
recurrence | (31) |
| Derbel et
al, 2019 | 37 | Male | Tunisia | Acute blurred
vision | CT/TTE | Interventricular
septum | 30x30 | Albendazole | Yes | No data | (32) |
| Orhana et
al, 2018 | 26 | Male | Turkey | Dyspnea,
hemoptysis | TTE | RV | No data | Albendazole | Yes | No recurrence | (6) |
| Stiru et al,
2019 | 24 | Male | Romania | Facial paralysis,
headaches | TTE/CT | Interventricular
septum | 23x19 | Albendazole | Yes | 1 year No
recurrence | (33) |
| Sarr et al,
2019 | 65 | Male | Senegal | Limb edema | TTE/CT | Pericardium | 86x61 | Albendazole | No | 2 months Fatal
outcome | (55) |
| Sonsoz and Gunes,
2020 | 32 | Male | Turkey | Constitutional
symptoms | TTE/CMR | RV | 25x21 | Albendazole | Yes | Died on
postoperative day 2 | (34) |
| Al-Hakkak et
al, 2019 | 18 | Male | Iraq | Acute right lower
limb pain | TTE/CT | Left ventricle | 36x40 | Albendazole | Yes | No data | (35) |
| Rossetti et
al, 2018 | 15 | Male | Argentina | Acute right lower
limb pain | TTE | Left ventricle | 30x30 | Albendazole/
praziquantel | Yes | 2 years No
recurrence | (7) |
| Wedin et al,
2021 | 38 | Male | Sweden | Chest pain | TTE/TEE/
CMR/CT | Interventricular
septum | 35x65 | Albendazole | Yes | 1 year No
recurrence | (36) |
| Guha et al,
2021 | 18 | Male | India | Chest pain,
fever | TTE/TEE/ CT | Interatrial
septum | 73x32 | Albendazole | Yes | 1 year No
recurrence | (37) |
| Verma et al,
2020 | 17 | Male | India | Cough, fever | CT | RV | No data | Albendazole | Yes | No data | (38) |
| Fennira et
al, 2019 | 26 | Male | Tunisia | Chest pain,
asthenia | TTE | Interventricular
septum | 48x49 | Albendazole | Yes | 8 months No
recurrence | (13,39) |
| Zhang et al,
2020 | 31 | Female | China | Cough, fever,
hemoptysis, palpitations | TTE/MRI | Right atrium/
pericardium | 25x50 | Albendazole | Yes | 1 year No
recurrence | (40) |
| Zghal et al,
2020 | 68 | Male | Tunisia | Stroke, sudden
deaths | TTE | Left ventricle | 25x25 | - | No | Died | (41) |
| İyigün et
al, 2020 | 18 | Male | Turkey | Asymptomatic | TTE/TEE/ CMR | Interventricular
septum | 47x47x74 | Albendazole | Yes | No date | (42) |
| Modani et
al, 2018 | 57 | Male | India | Chest pain | TTE/CMR | Interventricular
septum | 40x45 | Albendazole | Yes | 30 days No
recurrence | (43) |
| Berarducci et
al, 2021 | 48 | Male | Mexico | Palpitations,
drowsiness | TTE/CMR/ 3D CT | RV | No data | No data | Yes | No recurrence | (45) |
| Meimand et
al, 2020 | 31 | Male | Iran | Dyspnea,
hemoptysis | TTE/TEE/ CT | RV | 48x20 | Albendazole | Yes | Died on
postoperative day 3 | (46) |
| Meimand et
al, 2020 | 31 | Male | Iran | Right
hemiparesis | CT/MRI/
TTE/TEE | Interventricular
septum | 85x60 | Albendazole | Yes | 2 months No
recurrence | (46) |
| Vazhev et
al, 2018 | 18 | Female | Bulgaria | No data | TTE/CT | Left ventricle | 63x53 | Albendazole | Yes | 1 year No
recurrence | (47) |
| Lyazidi et
al, 2021 | 14 | Female | Morocco | Dyspnea,
palpitations | TTE | RV | 47x33 | Albendazole | Yes | 6 months No
recurrence | (48) |
| Harmouchi et
al, 2022 | 15 | N/A | Morocco | Cough,
arthralgia | TTE/CMR | Right atrium | 23x32 | Albendazole | Yes | No data | (66) |
Cardiac hydatid cysts are more often diagnosed in
men living in underdeveloped countries (1,11).
Among 47 reported cases identified in the present literature
review, >70% of patients were male (4-6,12-53).
The median age of patients with cardiac echinococcosis was 36
years. Cardiac echinococcosis symptoms varied greatly, with chest
pain and dyspnea being the most common (34%). The most common
cardiac tissue involved was the RV (32%), followed by the
interventricular septum (27%) and pericardium (13%) (12-50).
Moreover, cardiac hydatid cysts were reported to vary in size. The
largest cysts identified in the present review were >100 mm long
(16,44,54),
whereas the median cyst length was 47.5 mm. The most useful imaging
technique was TTE. Furthermore, the review data indicated that
>80% of patients underwent cardiac surgery. Most of the patients
were followed-up for 12 months (surgical and non-surgical
patients). A total of four patients died shortly after diagnosis;
three deaths were caused by postoperative complications and one was
caused by stroke (20,34,41,53).
From the present literature review it was concluded
that cardiac echinococcosis is more common in men <40 years old
and patients may present with various symptoms. Their size can vary
greatly, reaching >100 mm in length (16,44,54).
TTE is the most useful imaging technique due to its availability,
reproducibility, accuracy and safety. To improve the
characterization of the tumor, cardiac MRI can be performed.
Surgery is the treatment of choice, but the risk-benefit ratio and
shared decision making with the patient must be considered. The
available data from non-surgical patients shows that three of them
died shortly after diagnosis (<2 months) (19,41,55)
and two of them had a good outcome (23,27).
In the present case, the patient refused cardiac surgery and chose
medical treatment. Albendazole is an active agent against
Echinococcus and should be administrated adjunctively, pre-
and post-surgery (11). No disease
recurrence was observed in patients who underwent surgery and
pharmaceutical treatment with albendazole.
Discussion
Human hydatid cysts are caused by the larval stages
of tapeworms of the genus Echinococcus (56). In most cases, multiple organs are
affected. Cardiac echinococcosis appears in 0.5-2% of patients,
usually with multiple organ involvement, following the invasion of
the myocardium via the coronary artery (57). Most commonly cardiac hydatid cysts
involve the left ventricular cavity (60%), followed by the right
ventricular cavity (10-15%), pericardium (7%), the atria and the
interventricular septum (2).
Moreover, clinical manifestations of benign cardiac tumors depend
on the size and location of the mass and the infiltration of
adjacent tissues (58). Most
patients with cardiac hydatid cysts are asymptomatic. Signs and
symptoms of cardiac echinococcosis are nonspecific and are directly
related to the location and the size of the cysts. They may develop
because of compression or rupture of the hydatid cyst, which is the
most important and potentially fatal complication. Generally,
nonspecific chest pain is the most common symptom, whereas dyspnea
following exertion is often related to multiple hydatic cysts in
the lungs (59). The major
complications of cardiac hydatid cysts include anaphylactic shock,
cardiac tamponade, systemic or pulmonary embolism, arrhythmias,
valvular dysfunction and sudden death (11). Anaphylactic shock was the first
symptom in the present case, which was treated with adrenaline,
according to the available protocols (60). Shortly after anaphylactic shock,
the patient developed a pulmonary embolism requiring low-molecular
weight heparin (enoxaparin, 60 mg/0.6 ml twice daily).
The diagnosis of hydatid cysts is based on imaging
results and specific serological tests (3). The method of choice to detect cardiac
hydatic cysts and determine their number, size, location and
relation to other anatomical structures is 2D TTE. Cardiac MRI may
be useful for improved characterization of cardiac tumors, but it
requires appropriate experience to be used effectively. ELISA is
the most specific serologic test that can be used and a positive
result for Echinococcus antibodies confirms the diagnosis
(61). Surgery is the treatment of
choice (10,11), but the risk-benefit ratio must be
considered and shared decision making with the patient must be
taken into account. Shared decision-making is not commonly used in
Romania and it depends on numerous factors, including the level of
education of the patient (62). In the present case report,
the patient refused cardiac surgery. If complete removal of
the cysts is possible the prognosis is good, with a low rate of
recurrence (11). Medical
treatment with albendazole has a role in reducing the size of cysts
and stopping their development and represents the only therapeutic
option in inoperable cases (63).
In the present study the echocardiographic
assessments at serial evaluation (four times in 3 years) documented
marked reductions in the dimensions and increases in echogenicity
of the right ventricular hydatid cyst under antiparasitic
treatment. These results suggested a low risk of rupture; however,
symptoms of pulmonary embolism occurred in the evolution of the
present case. Therefore, in the absence of cardiac surgery, the
prognosis and further evolution are unpredictable and long-term
antiparasitic treatment and frequent clinical, imagistic and
biological evaluation are required.
Cardiac echinococcosis infection can clinically have
a wide range of symptoms, from none at all to sudden death.
Diagnosis must be suspected in patients who come from regions where
tapeworms of the genus Echinococcus are endemic. The patient
in the present study lived in a rural area of an endemic country
and the symptomatology at the first hospital admission was
anaphylactic shock. Moreover, blood tests showed eosinophilia,
which led to the consideration of a parasitic infection in the
differential diagnosis. The clinical history of the patient is
important and echocardiography is a reliable, safe and effective
imaging method for the initial diagnosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MB wrote the initial draft, collected data by
performing the experiments, performed the review, constantly
revised the article according to reviewers and participated in the
final design of the article. DM was involved in the acquisition of
data and described the patient evolution and management. AT
performed and described the microscopic examination. MO performed
the thoracic surgery, revised the initial draft and analyzed data
from the literature. AG was involved in the analysis and
interpretation of data, performed the literature review and revised
the final manuscript. MB and AG confirm the authenticity of all the
raw data. All authors read and agreed to the final manuscript.
Ethics approval and consent to
participate
Ethics approval was obtained from the Medical Ethics
Commission for Clinical Studies in the ‘Coltea’ Clinical Hospital
(Bucharest, Romania; approval number 24216/86; 2021/12/09).
Patient consent for publication
Written informed consent for publication was
obtained from the patient prior to publication at the time of
admission.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Tamarozzi F, Legnardi M, Fittipaldo A,
Drigo M and Cassini R: Epidemiological distribution of
Echinococcus granulosus s.l. infection in human and domestic
animal hosts in European mediterranean and balkan countries: A
systematic review. PLoS Negl Trop Dis. 14(e0008519)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Eckert J and Deplazes P: Biological,
epidemiological, and clinical aspects of echinococcosis, a zoonosis
of increasing concern. Clin Microbiol Rev. 17:107–135.
2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kahlfuß S, Flieger RR, Roepke TK and
Yilmaz K: Diagnosis and treatment of cardiac echinococcosis. Heart.
102:1348–1353. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gençpınar T, Guzeloglu M, Aykut K,
Albayrak G and Hazan E: A rare localization of hydatid cyst: Right
ventricular free wall cyst fistulized to the ventricular cavity. J
Cardiovasc Surg. 1(13)2013.
|
|
5
|
L'aarje A, Lyazidi S, Kitane Y, Alami A
and Habbal R: Cardiac hydatid cyst of the right ventricle: Severe
localization. J Cardiol Cases. 16:138–140. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Orhana G, Bastopcua M, Aydemirb B and
Ersoz MS: Intracardiac and pulmonary artery hydatidosis causing
thromboembolic pulmonary hypertension. Eur J Cardiothorac Surg.
53:689–690. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rossetti E, Boto A, González Cambaceres C,
Ruvinsky S and Sagray E: Colaboradores. Acute arterial embolism as
the clinical presentation of a disseminated hydatidosis: Case
report. Arch Argent Pediatr. 116:e616–e620. 2018.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
8
|
de Gregorio C, Ferrazzo G, Ceresa F, De
Donno BF and Patanè F: Dynamic right ventricular outflow tract
obstruction by cardiac hydatic cysts: A multimodality imaging
study. J Clin Ultrasound. 49:690–692. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gurzu S, Beleaua MA, Egyed-Zsigmond E and
Jung I: Unusual location of hydatid cysts: Report of two cases in
the heart and hip joint of Romanian patients. Korean J Parasitol.
55:429–431. 2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Thameur H, Abdelmoula S, Chenik S, Bey M,
Ziadi M, Mestiri T, Mechmeche R and Chaouch H: Cardiopericardial
hydatid cysts. World J Surg. 25:58–67. 2001.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yaman ND and Sirlak M: Cardiac hydatid
cysts-review of recent literature. J Vet Med Res. 4(1102)2017.
|
|
12
|
Wen H, Zou PF, Yang WG, Lu J, Wang YH,
Zhang JH, New RR and Craig PS: Albendazole chemotherapy for human
cystic and alveolar echinococcosis in north-western China. Trans R
Soc Trop Med Hyg. 88:340–343. 1994.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fennira S, Kamoun S, Besbes B, Ben Mrad I,
Zairi I, Ben Moussa F, Mzoughi K and Kraiem S: Cardiac hydatid cyst
in the interventricular septum: A literature review. Int J Infect
Dis. 88:120–126. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kumar A, Ballal P, Nagamani AC and Sheriff
SA: Surgical excision of an epicardial ventricular hydatid cyst.
Asian Cardiovasc Thorac Ann. 28:273–275. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Giri S, LeVine S and Watts MR: Ventricular
tachycardia and the cystic heart: A case report. J Emerg Med.
58:e243–e246. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kuemmerli C, Sánchez-Velázquez P, Tschuor
C, Oberkofler C, Lachat M, Müllhaupt B, Clavien PA and Petrowsky H:
When Echinococcus granulosus transmigrates from the liver
into the pericardium: A case report. J Surg Case Rep.
2021(rjaa492)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Çankaya BY and Çolak A: Cystic
echinococcosis involving the cardiac interventricular septum. Rev
Soc Bras Med Trop. 54:e0499–2020. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Iriz E, Yayll S and Kula S: Cystic
echinococcosis of the interventricular septum: A rare clinical
presentation. Cardiol Young. 30:1515–1516. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Singh S and Yadav MK: Extensive myocardial
calcification mimicking giant honey-bee associated with cardiac
hydatid cyst. Int J Cardiovasc Imaging. 37:163–164. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Singh A, Negi S, Kumar R, Toshkani D and
Niyogi SG: Honeycomb in the heart: A rare case of hydatid cyst of
the interventricular septum. J Clin Ultrasound. 49:803–804.
2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Shakerian B and Mandegar MH: Huge hydatid
cyst of the right ventricular outflow tract. Sultan Qaboos Univ Med
J. 21:485–487. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Alami B, Boujraf S, Alaoui-Lamrani Y,
Boubbou M and Maaroufi M: Hydatid cyst in interventricular septum.
Ann Card Anaesth. 22:343–344. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cheng Z, Fang T and Guo Y: Typical MRI of
cardiac hydatid involvement: A case report. Acta Cardiol.
76:324–325. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
De NV, Minh PN, Duyet LV, Bich NN, Son TN,
Jung BK and Chai JY: Two human cases of Echinococcus
ortleppi infection in the lung and heart in vietnam. Korean J
Parasitol. 58:451–456. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Rhissassi J, Bouhdadi H, Wazaren H, El
aamadi W, Bouchikh M and Laaroussi M: Incidental finding of
multiple pulmonary and cardiac hydatid cysts. Ann Cardiol Angeiol
(Paris). 70:122–124. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jain SK, Jha VK and Mani GK: Concurrent
intrapericardial-pulmonary hydatidosis: An unusual multisystem
echinococcosis. Indian J Thorac Cardiovasc Surg. 37:438–441.
2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Madisson-Bernardo M, Bernardo D, Trad HS,
Meneghelli U, Villanova M and Schmidt A: Intense pericardial
involvement in polycystic echinococcosis submitted to successful
medical treatment. Circ Cardiovasc Imaging.
12(e009826)2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kaskar A, Shetty V and Shetty D: Chronic
pulmonary thromboembolism due to intracardiac and pulmonary
hydatidosis. Asian Cardiovasc Thorac Ann. 28:610–612.
2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Handran CB, Hurwitz Koweek LM and
Mammarappallil JG: Case 274: Cardiac Echinococcus.
Radiology. 294:478–481. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kohlmaier B, Trobisch A, Pfurtscheller K,
Knez I, Klepetko W, Pilhatsch A, Schweintzger S and Zenz W: Cardiac
and pulmonary cystic echinococcosis with massive obstruction of the
pulmonary vessel system in a 16-year-old girl. Pediatr Infect Dis
J. 37:e273–e275. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Vural U, Aglar AA and Kayacioglu İ:
Intracoronary hydatid cyst resulted in coronary artery disease in a
young patient. Braz J Cardiovasc Surg. 34:107–110. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Derbel B, Ziadi J, Besbes T, Dougaz W,
Mleyhi S, Zairi I and Denguir R: Intracardiac echinococcosis cyst
mimicking a septal cardiac tumor with neurological symptoms. Int J
Infect Dis. 88:152–153. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Stiru O, Carmen Geana R, Antohi L, David
L, Goicea M, Paunescu A, Chioncel O and Anton Iliescu V:
Incidentally detected cardiac and hepatic hydatid cyst after sudden
onset facial paralysis: A case report. Arch Clin Med Case Rep.
3:190–198. 2019.
|
|
34
|
Sonsoz MR and Gunes SC: An intra-cardiac
mass in a patient with Behçet's disease: Cardiac hydatid cyst.
Echocardiography. 37:646–648. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Al-Hakkak SMM, Al-Faham FSM and Al-Awwady
AN: Acute limb ischemia caused by ruptured cardiac hydatid cyst-a
case report. Int J Surg Case Rep. 55:18–22. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wedin JO, Astudillo RM, Kurland S,
Grinnemo KH, Astudillo R, Vikholm P and Schiller P: A rare case of
cardiac echinococcosis: The role of multimodality imaging. CASE
(Phila). 5:230–234. 2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Guha A, Ranjan R, Saxena P and Mehta Y: A
rare case of cardiac hydatid cyst. Ann Card Anaesth. 24:470–472.
2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Verma PK, Rohilla R, Natarajan V and Gupta
PK: A rare case of coexisting tuberculosis with hydatid disease
from North India with review of literature. BMJ Case Rep.
13(e235301)2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Fennira S, Sarray H, Kammoun S, Zoubli A,
Kammoun Y, Kraiem S and Jerbi S: A large cardiac hydatid cyst in
the interventricular septum: A case report. Int J Infect Dis.
78:31–33. 2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Zhang X, Wei X, Ran L and Tang H: A rare
case of cardiac alveolar echinococcosis. Eur Heart J.
41(2698)2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zghal FM, Boudiche S, Zongo T, Rekik B,
Ouali S and Mourali MS: An unusual cause of stroke and sudden
death: Intracavitary left ventricular echinococcosis. Int J Infect
Dis. 90:26–27. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
İyigün T, Kyaruzi MM, Kutay V and Karakurt
ST: Asymptomatic huge cardiac hydatid cyst located in the
interventricular septum. Braz J Cardiovasc Surg. 35:235–238.
2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Modani S, Karthik DK, Heda S and Deshpande
A: Atypical chest pain in a patient with hydatid cyst of the
interventricular septum. BMJ Case Rep.
2018(bcr2018224833)2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Firouzi A, Neshati Pir Borj M and Alizadeh
Ghavidel A: Cardiac hydatid cyst: A rare presentation of
echinococcal infection. J Cardiovasc Thorac Res. 11:75–77.
2019.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Berarducci J, Armenta-Moreno JI,
Garcia-Cardenas AM, Armendáriz-Ferrari JC and Espinola-Zavaleta N:
Cardiac echinococcosis: A multimodality approach. Eur Heart J Case
Rep. 5(ytab475)2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Meimand SE, Sadeghpour A, Pakbaz M,
Ghavidel AA, Pouraliakbar H, Kamali M and Safaei A: Cardiac
echinococcosis associated with other organ involvement: Report of
two challenging cases. CASE (Phila). 5:33–38. 2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Vazhev ZG and Stoev HA: Cardiac
echinococcosis involving left ventricular myocardium in an
18-year-old patient. Folia Med (Plovdiv). 60:308–313.
2018.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Lyazidi S, Abetti A, Abdellaoui A, El
Adaoui A, Habbal R and Ettaoumi Y: Cardiac hydatid cyst in the
right ventricle-a rare case report of echinococcosis presentation.
Ann Med Surg (Lond). 66(102427)2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Yimamu R, Qing-Qing L and Wei-Min Z:
Primary pericardial hydatid cyst in an asymptomatic butcher.
Cardiol Young. 31:479–481. 2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Singh SK, Singh V, Kumar S, Devenraj V,
Bhandari M and Pandey AK: Right ventricular hydatid cyst presented
as tachyarrhythmia. Asian Cardiovasc Thorac Ann. 27:489–491.
2019.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Separovic Hanzevacki J, Gasparovic H,
Reskovic Luksic V, Ostojic Z and Biocina B: Staged management of a
giant cardiac hydatid cyst: A case report. BMC Infect Dis.
18(694)2018.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Emam Hadi MA, Najari F and Soleimani L:
Sudden death due to hydatid cyst emboli; a case report. Emerg
(Tehran). 6(e20)2018.PubMed/NCBI
|
|
53
|
Mesrati MA, Mahjoub Y, Ben Abdejlil N,
Boussaid M, Belhaj M, Limem H, Chadly A, Zakhama A and Aissaoui A:
Case report: Sudden death related to unrecognized cardiac hydatid
cyst. F1000Res. 9(286)2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Wadhawa V, Shah J, Doshi C, Ramani J,
Lakhia K, Rathod D, Tavar R and Kothari J: Surgical overview of
cardiac echinococcosis: A rare entity. Interact Cardiovasc Thorac
Surg. 27:191–197. 2018.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Sarr SA, Aw F, Ndiaye M, Mingou J, Bodian
M, Dioum M, Ngaidé AA, Ndiaye MB, Kane A, Diao M and Ba SA: Chronic
right ventricular failure revealing a large compressive hydatid
cyst at the cardiology department of the aristide le dantec
hospital (Dakar, Senegal). Bull Soc Pathol Exot. 112:202–205.
2019.PubMed/NCBI View Article : Google Scholar : (In French).
|
|
56
|
Gessese AT: Review on epidemiology and
public health significance of hydatidosis. Vet Med Int.
2020(8859116)2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Dighiero J, Canabal EJ, Aguirre CV, Hazan
J and Horjales JO: Echinococcus disease of the heart.
Circulation. 17:127–132. 1958.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Bussani R, Castrichini M, Restivo L,
Fabris E, Porcari A, Ferro F, Pivetta A, Korcova R, Cappelletto C,
Manca P, et al: Cardiac tumors: Diagnosis, prognosis, and
treatment. Curr Cardiol Rep. 22(169)2020.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Ben-Hamda K, Maatouk F, Ben-Farhat M,
Betbout F, Gamra H, Addad F, Fatima A, Abdellaoui M, Dridi Z and
Hendiri T: Eighteen-year experience with echinococcosus of the
heart: Clinical and echocardiographic features in 14 patients. Int
J Cardiol. 91:145–151. 2003.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Bălan H and Gurghean A: Anaphylactic
shock: Are we doing enough and with the right timing and order? Rom
J Intern Med. 53:191–198. 2015.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Sağlıcan Y, Yalçın Ö and Kaygusuz E:
Cystic echinococcosis: One entity, two unusual locations. Turkiye
Parazitol Derg. 40:51–53. 2016.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Baicus C, Balanescu P, Zeh S, Oprisan E,
Lapadatu R, Gurghean A, Padureanu V, Rezus C, Mitu F, Jurcut R, et
al: Characteristics of shared decision making in Romania from the
patient perspective: A cross-sectional multicentric study. J Eval
Clin Pract. 25:1152–1159. 2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Dumitru IM: Medical treatment of cystic
echinococcosis. In: Derbel F, Braiki M (eds). Overview on
Echinococcosis, 2019.
|
|
64
|
Jamli M, Cherif T, Ajmi N, Besbes T,
Mgarrech I, Jerbi S, Kortas C and Tarmiz A: Surgical management and
outcomes of cardiac and great vessels echinococcosis: A 16-year
experience. Ann Thorac Surg. 110:1333–1338. 2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Lu YM, Zhang L, Xing Q, Zhou XH, Li YD,
Zhang JH, Zukela T and Tang BP: Ventricular tachycardia as the
initial symptom of cardiac hydatidosis. Chin Med J (Engl).
132:2765–2766. 2019.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Harmouchi H, Kouache ME, Lakranbi M,
Ouadnouni Y and Smahi M: Cardiac hydatid cyst interposed between
the right atrium and right ventricle on the tricuspid valve. Asian
Cardiovasc Thorac Ann. 30:199–201. 2022.PubMed/NCBI View Article : Google Scholar
|