Introduction
Budd-Chiari syndrome (BCS) is a rare condition that
is a result of thrombotic or non-thrombotic obstruction of the
hepatic venous outflow, characterized by ascites, hepatomegaly and
pain in the abdomen. The estimated incidence rate of BCS is
1:100,000 in the general population, with <300 cases reported by
three tertiary referral centers in France, the USA and the
Netherlands. Although Western countries consider BCS to be a rare
disease, its presence in a population is largely affected by
region; BCS is more common in Asian countries such as India, China
and Nepal, with some regions of China reaching 6.8 to 12 cases per
100,000 people, while in the West, the disorder is estimated to
affect one in 2.5 million individuals (1).
BCS is classified into two types: Primary BCS, when
obstruction originates in the vein and thrombosis is the main
cause; or secondary BCS, when there is external compression of the
vein (such as from an abscess or tumor) (2). Most patients with BCS have an
underlying thrombotic diathesis, for example, patients who are
pregnant or those with a tumor, a chronic inflammatory disease, an
infection or a myeloproliferative disorder. In >75% of patients,
one hereditary or acquired hypercoagulable state can be identified,
whereas more than one etiological factor is observed in the
remaining 25% (3). Hepatic vein
thrombosis is caused by a myeloproliferative disease, as diagnosed
in 20% of cases (4); polycythemia
vera accounts for 10-40% of all cases. Gene mutations in factor V
Leiden and factor II have been recorded in ~25 and 5% of patients
with BCS, respectively (4). Oral
contraceptive use has also been identified as a risk factor for BCS
(5,6).
The presentation of BCS ranges from asymptomatic to
fulminant hepatic failure, passing through the development of acute
(rapid) or chronic (progressive) symptoms in a period of weeks to
months prior to the diagnosis. The following circumstances are
indicative of BCS: i) simultaneous presentation of ascites,
hepatomegaly and upper abdominal pain; ii) massive ascites with
mildly altered liver function tests; iii) sinusoidal dilation upon
liver biopsy, without heart disease; iv) fulminant hepatic failure
in association with hepatomegaly and ascites; and v) unexplained
chronic liver disease following exclusion of diagnoses of
alcoholism, autoimmunity, chronic viral hepatitis B or C, Wilson's
disease, iron overload and α-1 antitrypsin deficiency (6-8).
Doppler ultrasonography of the liver, with a
sensitivity and specificity of ≥85%, is the technique of choice for
detecting obliteration of hepatic veins, thrombosis or stenosis,
spider web vessels, large collateral vessels or a hyper echoic cord
replacing a normal vein (6,9). If
the results of the ultrasonography are unclear, magnetic resonance
imaging (MRI) of the blood vessels (magnetic resonance angiography)
or computed tomography (CT) represent the second-line imaging
investigations (10,11).
Treatment of BCS starts with anticoagulant therapy,
treatment of the underlying disease and also symptomatic therapy of
portal hypertension complications. In patients with short-length
stenosis unresponsive to medical therapy, angioplasty/stenting is
the second-line treatment, while transjugular intrahepatic
portosystemic shunt represents the next step. In severe cases of
BCS, liver transplantation is the last option (1,11).
The natural course of the disease is severe, with a
3-year survival rate of <10% in patients who do not receive
treatment. Following a rapid diagnosis and the early initiation of
treatment, the 5-year survival rate is 76%. The long-term prognosis
depends on the associated risk factors for thrombosis (11,12).
Since this pathology is so rare, any encounter with a case is worth
reporting in order to increase the awareness of the disorder. The
present study discusses two cases of BCS in women aged 35 and 61,
who presented to the Emergency Department (ED) of the Emergency
Clinical Municipal Hospital (Timisoara, Romania) 1 month apart.
Case report
Case 1
A 35-year-old woman presented to the ED of the
Emergency Clinical Municipal Hospital in July 2020 with asthenia, a
low appetite, abdominal distension and a marked decrease in weight
of 13 kg in 1 month. A physical examination revealed a distended
and painful abdomen, edema of the legs, palmar erythrosis and
angioma stellaire on the chest. Vital parameters were recorded as
follows: Blood pressure (BP), 110/70 mmHg; oxygen saturation
(SpO2), 97%; heart rate (HR), 100 beats/min.
Abdominal ultrasound performed in the ED identified
a slightly enlarged liver, with a homogenous surface and a medium
amount of ascites. CT scan of the abdomen confirmed the presence of
hepatomegaly and a nutmeg appearance of the liver after the
administration of the contrast substance.
The pathological values of the laboratory tests
performed in the ED and during hospitalization are shown in dynamic
in Table I. Serial gastroscopies
were performed on the 4th and 5th days after admittance, as the
hemoglobin level had demonstrated a constant decrease since the
admittance of the patient to the hospital. The gastroscopies
revealed gastric ulcers, covered with fibrin, with no visible
source of active bleeding and no esophageal or gastric varices.
 | Table ICase 1: Pathological values of the
laboratory tests performed in the Emergency Department, at 1 and 6
days post-admittance. |
Table I
Case 1: Pathological values of the
laboratory tests performed in the Emergency Department, at 1 and 6
days post-admittance.
| Laboratory
parameter | Conventional
units | Value 1 (in the
ED) | Value 2 (1 day
post-admittance) | Value 3 (6 days
post-admittance) | Reference range
value |
|---|
| WBC |
x103/µl | 12.2 | 21.6 | 17.8 | 4-10 |
| RBC |
x106/µl | 2.39 | 2.72 | 1.76 | 3.8-4.8 |
| HGB | g/dl | 9.2 | 8 | 5.4 | 12-15 |
| HCT | % | 28.3 | 24.4 | 16 | 36-46 |
| PLT |
x103/µl | 212 | 112 | 103 | 150-410 |
| AST | U/l | 118 | 171 | 500 | 15-37 |
| ALT | U/l | 29 | 44 | 234 | 14-59 |
| Blood glucose | mg/dl | 77 | 64 | 107 | 74-106 |
| BT | mg/dl | 3.3 | 5.65 | 6.5 | 0.2-1 |
| BD | mg/dl | 2.81 | 4.83 | 5.01 | 0.0-0.2 |
| Cholinesterase | U/l | 3522 | 3789 | 4321 | 5320-12920 |
| Creatinine | mg/dl | 0.45 | 1.22 | 2.02 | 0.55-1.02 |
| FAL | U/l | 250 | 304 | 320 | 35-105 |
| INR | INR | 1.63 | 1.75 | 2.5 | 0.8-1.2 |
| aPTT | Sec | 44.9 | 50 | 52 | 21.6-28.7 |
Prompt intravascular volume replacement was
initiated using crystalloid fluids and blood transfusions. Proton
pump inhibitor (omeprazole) was administered as an intravenous
bolus, followed by continuous infusion (80 mg, then 8 mg/h) for the
entire hospitalization period. Despite the medication given, the
patient had an episode of massive hematemesis and died 7 days from
the initial presentation in the ED.
Case 2
A 61-year-old woman who had previously been
diagnosed with breast cancer, for which mastectomy was performed 5
years before the current presentation, plus carcinomatous
meningitis in the same year and bone metastases, presented to the
ED of the Emergency Clinical Municipal Hospital in June 2020 with
nausea and vomiting that had been persisting for 1 month, as well
as abdominal pain, fatigability and edema of the legs. A physical
examination revealed icteric skin, sclera and mucous membranes,
diffuse abdominal pain and hepatomegaly (6 cm below the costal
margin), with no pathological cardiac or respiratory findings.
Vital parameters were recorded as follows: BP, 125/75 mmHg; HR, 70
beats/min; SpO2, 96% (without supplemental oxygen).
An abdominal ultrasound exam was performed in the
ED, which revealed an enlarged inhomogeneous liver, without
splenomegaly, and a medium amount of ascites. Initial lab tests
included a complete blood count, a comprehensive metabolic panel
and a coagulation panel (Table
II).
 | Table IICase 2: Pathological values of the
laboratory tests performed in the Emergency Department. |
Table II
Case 2: Pathological values of the
laboratory tests performed in the Emergency Department.
| Laboratory
parameter | Conventional
units | Value (upon
presentation in ED) | Reference range
value |
|---|
| RBC |
x106/µl | 3.35 | 3.8-4.8 |
| HGB | g/dl | 10.8 | 12-15 |
| AST | U/l | 289 | 15-37 |
| ALT | U/l | 82 | 14-59 |
| Lipase | U/l | 1033 | 73-393 |
| Blood glucose | mg/dl | 112 | 74-106 |
| BT | mg/dl | 4.6 | 0.2-1 |
| BD | mg/dl | 3.41 | 0.0-0.2 |
| Cholinesterase | U/l | 3065 | 5320-12920 |
| Creatinine | mg/dl | 1.22 | 0.55-1.02 |
| FAL | U/l | 565 | 35-105 |
| Ferritin | ng/ml | 1417 | 15-150 |
| CRP | mg/l | 50.1 | 0.0-5.0 |
| INR | INR | 1.48 | 0.8-1.2 |
| aPTT | Sec | 29.1 | 21.6-28.7 |
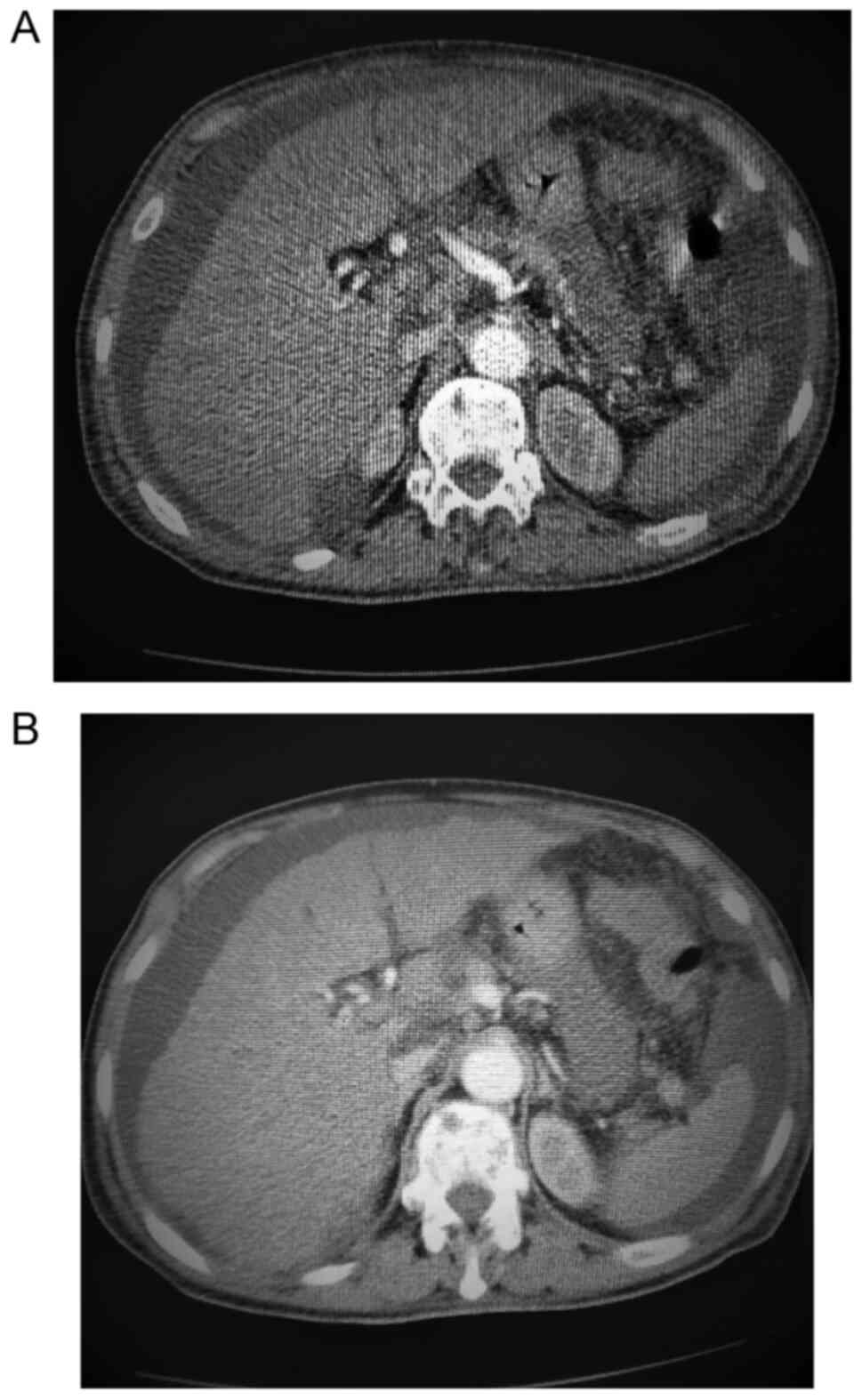
An abdominal and pelvic CT scan with contrast was
also performed, which found hepatomegaly with an enlarged right
hepatic lobe (20 cm), with scratchy structure, and two cysts in the
4th and 8th segments. Additional findings included the absence of
visualization of the supra-hepatic veins after contrast
administration, and the small caliber of the retro-hepatic segment
of the inferior vena cava, suggestive of BCS. Furthermore, a
medium/large amount of ascites, a normal spleen, a portal vein with
a diameter of 0.8 cm (normal range, 0.7-1.5 cm), a common bile duct
with a diameter of 0.7 cm (normal value, 0.4 cm), a dilated
pancreatic duct of 4 mm measured at the level of pancreatic body
(normal value, 2.00 mm) and normal kidneys, uterus and urinary
bladder were recorded. Bilateral basal pleural effusions of ~2.2 cm
on the right side and 3.8 cm on the left side were noted, as well
as thoraco-lumbar osteolytic lesions (Fig. 1A and B).
The patient was admitted to the Department of
Gastroenterology. Following treatment with antalgics, antispastics,
oral anticoagulants and gastric protection medication, the
patient's condition improved, and they were discharged from the
hospital with the recommendation to continue the oral anticoagulant
treatment (4 mg acenocumarol, half a tablet per day) until further
follow-up at 1 month.
Discussion
The cause of BCS remains unknown in a large number
of cases. In a series of 163 cases, the etiology was reported as
either unidentified or inadequately established in 70.1%, while in
the rest of the patients, myeloproliferative neoplasm, celiac
disease, antiphospholipid syndrome, factor V Leiden mutation and
hyperhomocysteinemia were found as causes (13). In the present study, case 1
experienced a rapid fatal evolution and extensive blood tests were
not possible to identify the cause of the BCS. Since the
uncontrolled bleeding led to the death of the patient, it may be
hypothesized that an imbalance of pro- and anti-coagulation factors
was present, which was also demonstrated to be the case in patients
with BCS in a study by Chen et al (14). In case 2 of the present study, the
most relevant etiological factor appeared to be thrombosis,
probably secondary to the neoplastic disease, similar to 7 patients
out of 163 from the study by Seijo et al (13). Patients with cancer have an altered
hemostatic system, increasing the risk of both hemorrhagic and
thrombotic complications, particularly venous thromboembolism. This
association is well described for solid tumors (15). In both cases in the present study,
the association of ascites, hepatomegaly and upper abdominal pain,
presented simultaneously, was highly suggestive of BCS; however, it
was the CT scan that confirmed the diagnosis.
Complications of BCS are generally related to
underlying conditions and the severity of liver failure. Left
untreated, BCS can lead to hepatic encephalopathy, variceal
hemorrhage, hepato-renal syndrome, portal hypertension, bacterial
peritonitis if ascites is present and hepatocellular carcinoma
(16,17). Case 1 of the present study had a
fatal outcome, although it is hard to confirm whether this was due
to complications from BCS. The serial gastroscopies performed did
not reveal any variceal hemorrhage as the source of the massive
bleeding. The blood tests demonstrated altered liver function and
mild thrombocytopenia, either in the context of liver injury or due
to the platelet consumption secondary to BCS acute thrombosis
(18). Case 2 had a favorable
evolution despite the patient comorbidities. The patient was
discharged with anticoagulant therapy, which represents the
first-line treatment in BCS (19,20).
In conclusion, BCS is an uncommon life-threatening
hepatic vascular disorder. With regard to the present cases, the
following should be highlighted: i) The pro-thrombotic state
associated with neoplastic disease; and ii) that emergency
physicians should be aware of the association of ascites,
hepatomegaly and upper abdominal pain, which are commonly
encountered in the ED, and therefore perform an extensive work-up
for BCS. Since the outcome is poor in numerous cases, a timely
diagnostic and therapeutic approach is of vital importance.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
AS and AP were responsible for the study concept and
visualization, the original draft preparation, writing and
reviewing the manuscript. SDC, MI, MVB, NB and OAM analyzed the
patient data contributed to writing, reviewing and editing the
manuscript. OAM and NB confirm the authenticity of all the raw
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patients provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zu M, Xu H, Zhang Q, Gu Y, Wei N, Xu W,
Cui Y and Liu H: Review of Budd-Chiari syndrome. J Interv Med.
3:65–76. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mancuso A: An update on management of
Budd-Chiari syndrome. Ann Hepatol. 13:323–326. 2014.PubMed/NCBI
|
|
3
|
Denninger MH, Chaït Y, Casadevall N,
Hillaire S, Guillin MC, Bezeaud A, Erlinger S, Briere J and Valla
D: Cause of portal or hepatic venous thrombosis in adults: The role
of multiple concurrent factors. Hepatology. 31:587–591.
2000.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Janssen HL, Meinardi JR, Vleggaar FP, van
Uum SH, Haagsma EB, van Der Meer FJ, van Hattum J, Chamuleau RA,
Adang RP, Vandenbroucke JP, et al: Factor V Leiden mutation,
prothrombin gene mutation, and deficiencies in coagulation
inhibitors associated with Budd-Chiari syndrome and portal vein
thrombosis: Results of a case-control study. Blood. 96:2364–2368.
2000.PubMed/NCBI
|
|
5
|
Niknam R, Hajizadegan N, Mohammadkarimi V
and Mahmoudi L: A study of the different parameters in acute and
chronic Budd-Chiari syndrome. Egypt Liver J. 10(48)2020.
|
|
6
|
Aydinli M and Bayraktar Y: Budd-Chiari
syndrome: Etiology, pathogenesis and diagnosis. World J
Gastroenterol. 13:2693–2696. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Darwish Murad S, Plessier A,
Hernandez-Guerra M, Fabris F, Eapen CE, Bahr MJ, Trebicka J, Morard
I, Lasser L, Heller J, et al: Etiology, management, and outcome of
the Budd-Chiari syndrome. Ann Intern Med. 151:167–175.
2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Marudanayagam R, Shanmugam V, Gunson B,
Mirza DF, Mayer D, Buckels J and Bramhall SR: Aetiology and outcome
of acute liver failure. HPB (Oxford). 11:429–434. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ohta M, Hashizume M, Tomikawa M, Ueno K,
Tanoue K and Sugimachi K: Analysis of hepatic vein waveform by
Doppler ultrasonography in 100 patients with portal hypertension.
Am J Gastroenterol. 89:170–175. 1994.PubMed/NCBI
|
|
10
|
Erden A, Erden I, Karayalçin S and
Yurdaydin C: Budd-Chiari syndrome: Evaluation with multiphase
contrast-enhanced three-dimensional MR angiography. AJR Am J
Roentgenol. 179:1287–1292. 2002.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hemachandran N, Shalimar Acharya S, Kedia
S, Gunjan D, Saraya A, Sharma R and Gamanagatti S: Long-Term
outcomes of endovascular interventions in more than 500 patients
with Budd-Chiari Syndrome. J Vasc Interv Radiol. 32:61–69.e1.
2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sharma A, Keshava SN, Eapen A, Elias E and
Eapen CE: An update on the management of Budd-Chiari syndrome. Dig
Dis Sci. 66:1780–1790. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Seijo S, Plessier A, Hoekstra J, Dell'Era
A, Mandair D, Rifai K, Trebicka J, Morard I, Lasser L, Abraldes JG,
et al: Good long-term outcome of Budd-Chiari syndrome with a
step-wise management. Hepatology. 57:1962–1968. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chen H, Liu L, Qi X, He C, Yin Z, Wu F,
Fan D and Han G: Imbalance of pro-vs. anti-coagulation factors in
Chinese patients with Budd-Chiari syndrome and non-cirrhotic portal
vein thrombosis. PLoS One. 10(e0119909)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chang H, Kuo MC, Shih LY, Wu JH, Lin TL,
Dunn P, Tang TC, Hung YS and Wang PN: Acute promyelocytic
leukemia-associated thrombosis. Acta Haematol. 130:1–6.
2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Dilawari JB, Bambery P, Chawla Y, Kaur U,
Bhusnurmath SR, Malhotra HS, Sood GK, Mitra SK, Khanna SK and Walia
BS: Hepatic outflow obstruction (Budd-Chiari syndrome). Experience
with 177 patients and a review of the literature. Medicine
(Baltimore). 73:21–36. 1994.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Okuda K, Kage M and Shrestha SM: Proposal
of a new nomenclature for Budd-Chiari syndrome: hepatic vein
thrombosis versus thrombosis of the inferior vena cava at its
hepatic portion. Hepatology. 28:1191–1198. 1998.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Costa ARG, Freitas I, Raposo J, Barbosa G,
Miranda HP and Nery F: Budd-Chiari syndrome and acute liver
failure: An uncommon presentation of acute myeloid leukaemia. GE
Port J Gastroenterol. 28:62–66. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pavri TM, Herbst A, Reddy R and Forde KA:
Budd-Chiari syndrome: A single-center experience. World J
Gastroenterol. 20:16236–16244. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nozari N, Vossoghinia H, Malekzadeh F,
Kafami L, Mirheidari M and Malekzadeh R: Long-term outcome of
Budd-Chiari syndrome: A single center experience. Middle East J Dig
Dis. 5:146–150. 2013.PubMed/NCBI
|