Introduction
Bronchogenic cyst is a congenital, dysplastic
disease derived from the foregut, with pseudostratified ciliated
columnar epithelium (1). It most
frequently occurs in the mediastinum and lung, whilst it can also
occur in the diaphragm and retroperitoneum on rare occasions
(2). The majority of bronchogenic
cysts are benign lesions with a slow growth rate and an insidious
onset (3). Retroperitoneal
bronchogenic cysts are mostly located above the pancreas and the
left adrenal gland, but rarely cause clinical symptoms. Therefore,
they are usually discovered coincidentally during a physical
examination for other conditions (4). It may occur at any age and may affect
both males and females equally (5). In a small number of cases, clinical
symptoms may occur when the cyst is infected or compresses adjacent
structures (3).
The present report describes a case of bronchogenic
cyst originating from the left diaphragmatic crus and extending
into the retroperitoneal space. MRI revealed that there was a
fluid-fluid level in the cyst. Due to the severe back pain and the
inefficacy of conservative treatment, the cyst was completely
resected with a favorable post-operative recovery. The presence of
a fluid-fluid level in a bronchogenic cyst is rare. When the cyst
contents have a high density and precipitate, a CT scan, MRI or
B-ultrasound may reveal the density or signal stratification in the
cyst. It may be related to protein, hemorrhage and
calcium-containing mucus deposition in cysts. Fluid-fluid levels
have also been reported in other mediastinal masses, including
cystic teratoma and mediastinal lymphangioma, which may be
misdiagnosed. In addition, the present report performed a
literature review, summarizing the findings on bronchogenic cysts
with fluid-fluid level reported in previous studies.
Case report
A 48-year-old male patient presented at Xiamen
University Affiliated Southeast Hospital (Zhangzhou, China) in
October 2018 complaining of ‘back pain for 2 days’. The pain was
relieved when bending over and the patient had no other
symptoms/complaints, including fever, night sweats, abdominal pain
or abdominal distension. The patient denied any history of trauma
or surgery. The patient was in a forced position of bending and
crouching due to extensive thoracic and lumbar spine tenderness and
percussion pain. The visual analogue scale score of pain was 7 out
of 10. There was no abdominal tenderness or rebound tenderness.
Muscle strength, muscle tension, skin sensation and leg activity
were all normal. Laboratory tests, such as white blood cell count,
neutrophils, biochemistry, erythrocyte sedimentation rate,
C-reactive protein and tumor markers all yielded normal results. A
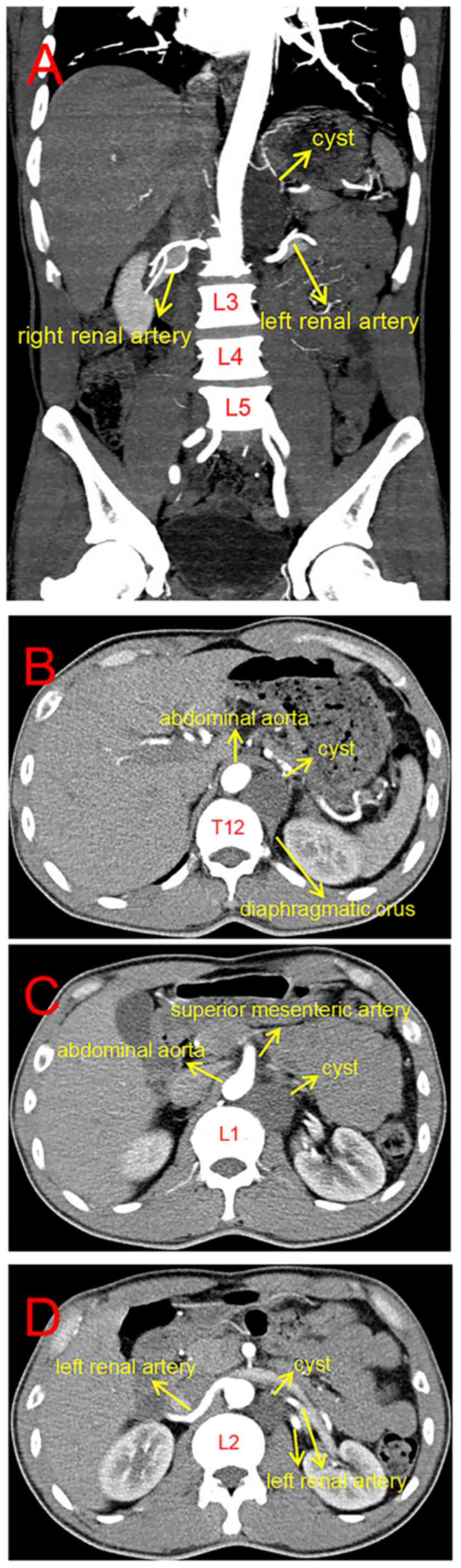
CT angiography of the abdominal aorta (Siemens Sensation 16;
Siemens AG) revealed that there was a low-density cystic mass with
a Hounsfield units value of 30 originating from the left diaphragm
foot on the left front of the T12-L2, mildly compressing the aorta.
The size of the cyst was ~3x4x6 cm (Fig. 1A). There was no change in the
density of the cyst in all images. The upper segment of the cyst
was in the retrocrural space, whereas the lower segment was in the
retroperitoneal space (Fig. 1B-D).
The CT scanning parameters were as follows: Slice thickness, 5 mm;
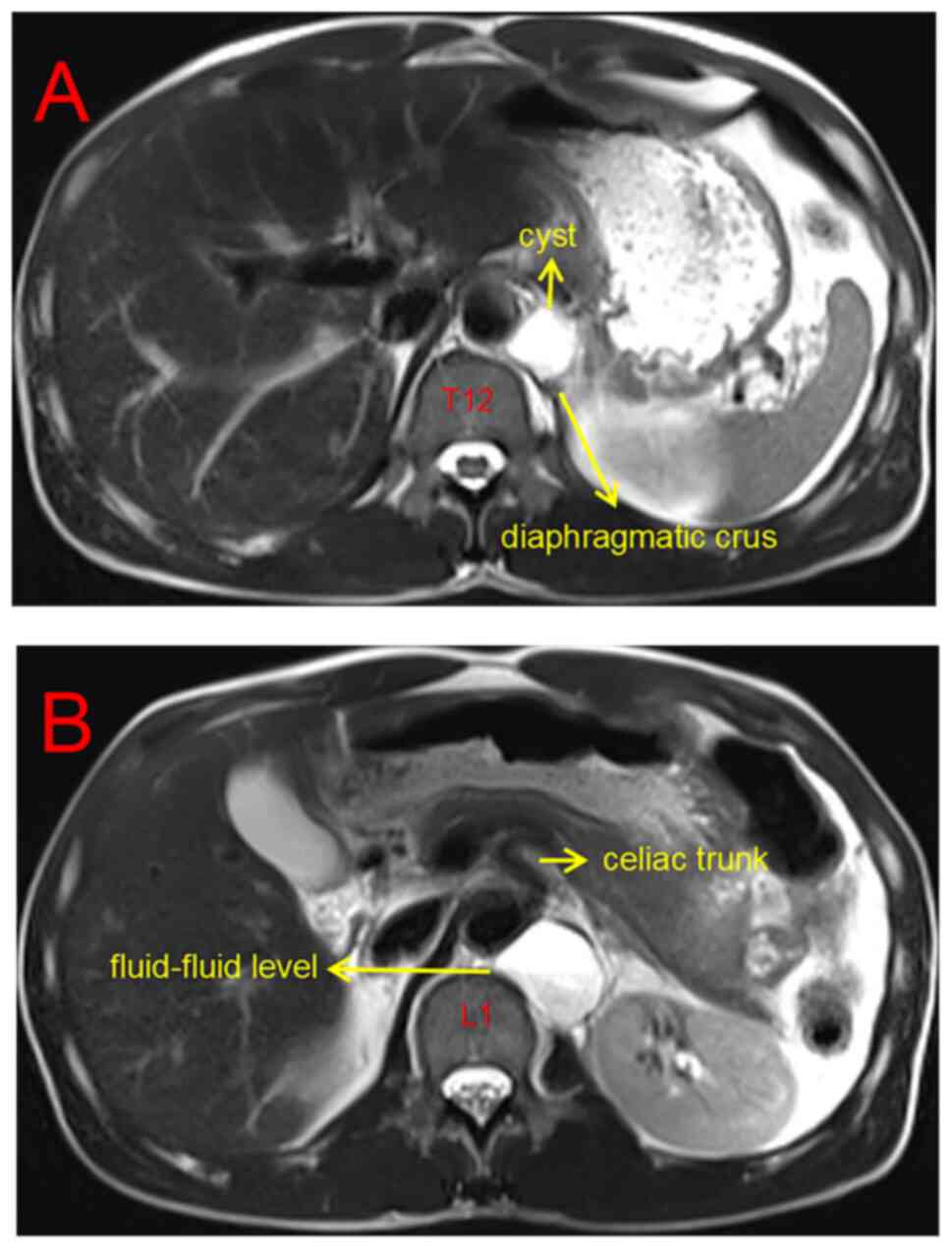
tube voltage, 120 kV; tube current, 200 mA. An MRI scan (Siemens
Magnetomveri 3.0T; Siemens AG) revealed that the cyst originated
from the left diaphragmatic crus, close to the spine and abdominal
aorta, with a fluid-fluid level in the cyst (Fig. 2A). An enhanced scan indicated that
the fluid signal in the upper layer of the cyst was higher compared
with that in the lower layer (Fig.
2B). The contents of the cyst had no enhancement, whereas the
cyst wall was smooth with mild enhancement (Fig. 2B). The MRI scanning parameters were
as follows: Repetition time/echo time, 2,000 msec/96 msec; matrix,
256x256; and section thickness, 5 mm. Celecoxib and tramadol were
used to relieve pain after admission. However, their effectiveness
was poor.
To confirm the diagnosis and relieve the symptoms,
an anterior thoracolumbar surgery was performed. Following the
surgical exposure, the size of the cyst was confirmed to be ~3x4x6
cm. The upper segment was located in the retrocrural space, closely
connected to the left diaphragmatic crus, whereas the lower segment
was located in the retroperitoneal space. A transparent fluid
flowed out of the cyst after puncturing the cyst, following which a
large amount of viscous white liquid was drawn out using a syringe.
The cyst wall was then completely scraped off using a spatula. No
bacterial or fungal growth was observed in the culture of the
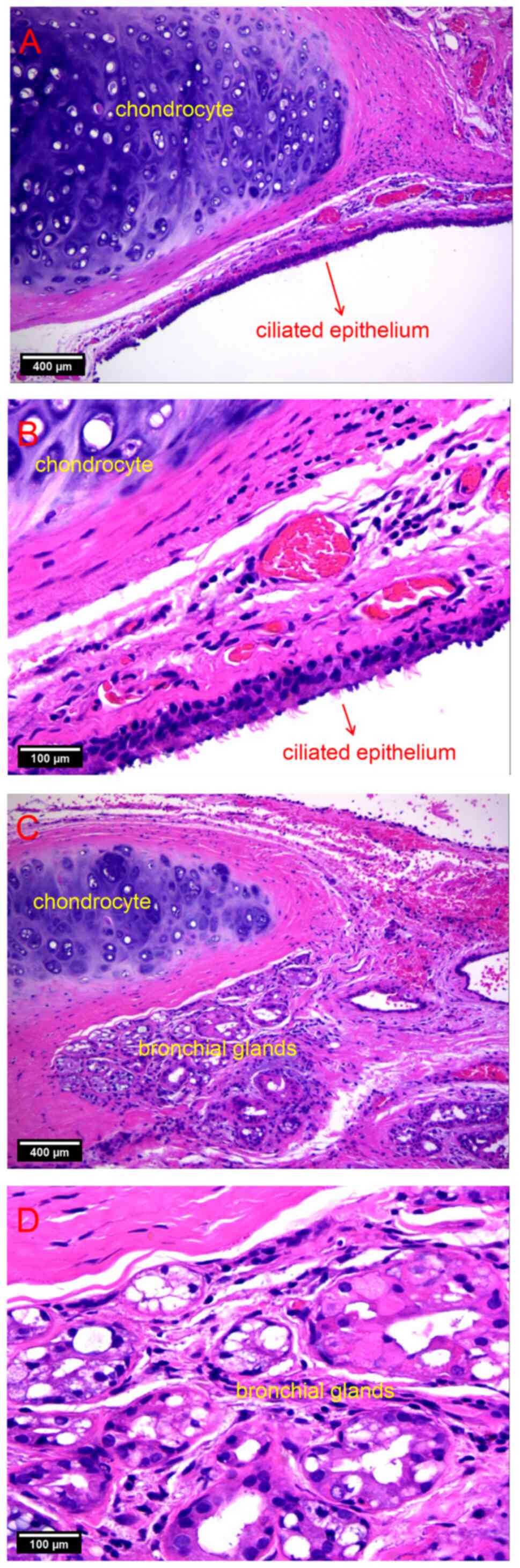
liquid. The cysts were analyzed pathologically by hematoxylin and
eosin staining, the protocols as follows: The tissue of cyst was
fixed in 4% paraformaldehyde for 24 h and then dehydrated and
embedded in paraffin. The specimen was cut into 10-µm slices, then
dewaxed and immersed in hematoxylin solution for 5 min. After
rinsing with water, the slices were stained with eosin Y solution
for 2 min. After dehydration with alcohol and clearing with xylene,
the slices were sealed with neutral resin and prepared for
pathological analysis under the light microscope. The results
revealed that the cyst wall was covered with pseudostratified
columnar epithelium (Fig. 3A and
B). In addition, there were
chondrocytes and bronchial glands but no blood cells or calcium
components in the cyst, which was suggestive of a bronchogenic cyst
(Fig. 3C and D). After surgery, the pain symptoms of
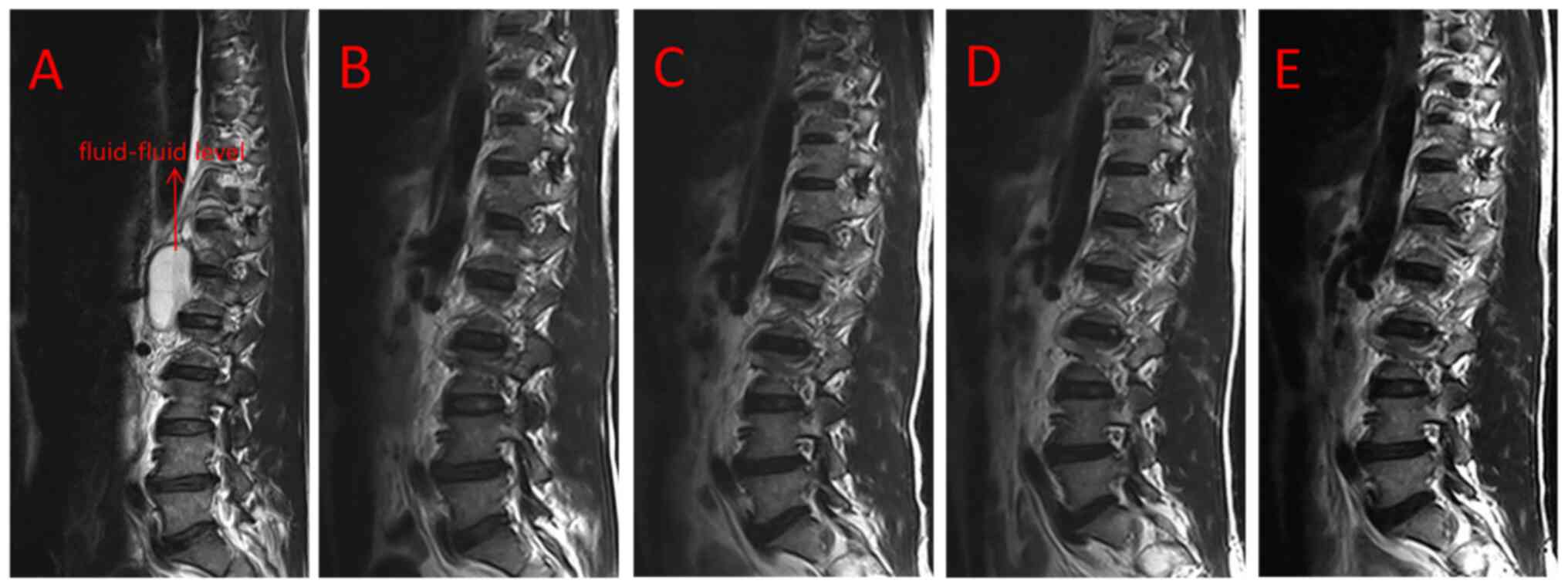
the patient markedly improved. Re-examination using MRI revealed
that the cyst had been completely removed. Of note, no recurrence
of the cyst and any clinical symptom was observed at the immediate,
3 months, 1 year and 3 years postoperatively (Fig. 4A-E).
Discussion
Bronchogenic cyst (also known as bronchial cyst) is
a rare, mostly benign, cystic mass caused by congenital dysplasia
of the respiratory system (6).
According to the location of the cyst, it may be classified as the
intrapulmonary type, mediastinal type or ectopic type (7). The ectopic type may occur in various
parts of the body, including the brain, spinal canal, diaphragm,
retroperitoneum and neck (2,8-12).
A systematic review in the PubMed database was conducted using the
following keywords: [Bronchogenic cyst (title)] and [fluid level
(title)]. Articles with a diagnosis of bronchogenic cysts without
fluid level were excluded. A total of 31 articles were searched and
27 articles were excluded based on title screening and abstract
screening. Only 4 relevant articles have been described in previous
case reports (Table I) (13-16).
In the present case, the fluid-fluid level in the cyst was
considered to be caused by calcium or protein deposition and
symptoms were usually related to compression of adjacent
structures. Fluid-fluid level is mainly detected by CT scans, MRI
and B-ultrasound, which may be related to the precipitation of
protein, hemorrhage or calcium-containing mucus deposition in the
cyst (17). Retroperitoneal
bronchogenic cysts are rare, the majority of which occur in the
posterior triangle of the stomach composed of the midline of the
abdomen, the splenic vein and the diaphragm (4). In the case described in the present
report, the cyst was in the left front of T12-L2 and adjacent to
the abdominal aorta in the posterior pararenal space. This cyst
originated from the left diaphragmatic crus. The upper segment was
in the retrocrural space, whereas the lower segment was in the
retroperitoneal space. Since this presentation has been rarely
reported in the literature, the pathogenesis of this disease
remains elusive (18). At present,
the hypothesis of a pinched and migratory bud is generally accepted
(19). During embryonic
development, certain abnormal buds of the tracheobronchial tree are
‘pinched off’ and migrate to an aberrant location. In cases where
the endocrine cells produced by the buds cannot be discharged, an
ectopic bronchogenic cyst may form at the transfer site (20).
 | Table ISummary of clinical characteristics of
previously reported cases of fluid-fluid level in bronchogenic cyst
and the present case. |
Table I
Summary of clinical characteristics of
previously reported cases of fluid-fluid level in bronchogenic cyst
and the present case.
| Author, year | Sex | Age, years | Symptoms | Tumor size, cm | Location | Treatment | (Refs.) |
|---|
| Lyon, 1993 | F | 33 | Dysphagia | Unknown | Middle
mediastinum | Surgery | (13) |
| Bargalló, 1993 | F | 55 | Asymptomatic | 3 | Right paraspinal
region | Surgery | (14) |
| Aydingöz, 1997 | M | 38 | Chest pain | 7x6x5 | Aortopulmonary
window | Transbronchial needle
aspiration | (15) |
| Han, 2017 | F | 31 | Chest and back
pain | 2.2 | Right lower posterior
mediastinum | Surgery | (16) |
| Han, 2017 | F | 74 | Asymptomatic | 3 | Right lower
paratracheal region | Imaging
follow-up | (16) |
| Present case | M | 48 | Acute back pain | 6x4x3 | Retroperitoneal
space | Surgery | N/A |
Bronchogenic cyst lacks a characteristic clinical
presentation guideline and is frequently detected by accident upon
physical examination (21). When
the cyst becomes too large in size, compression may cause abdominal
and back pain. In rare cases, symptoms similar to hypertension and
hypokalemia may occur due to compression of the adrenal glands
(22,23). In addition, if the cyst becomes
infected, secondary infection manifestations may then occur, such
as chills and fever (22,23). The severe back pain observed in the
case of the present study may be caused by the cyst compressing the
sympathetic nerves and the lateral communicating branches in front
of the spine. Bending over may reduce pain, as it may relieve
compression by reducing the tension of the fascia around the
cyst.
Pathological examination remains to be the gold
standard for detecting bronchogenic cysts (21). The typical pathological finding is
a cyst wall covered with pseudostratified ciliated columnar
epithelial cells. Furthermore, this type of cyst contains cartilage
or bronchial glands without any cell atypia (24). A respiratory epithelial cyst
lacking cartilage or glands should be diagnosed as a foregut cyst
(4). Due to the lack of specific
imaging guidelines, auxiliary examinations unfortunately provides
minimal assistance for the diagnosis of retroperitoneal
bronchogenic cysts. A typical bronchogenic cyst exhibits as a
well-circumscribed, round, low-density lesion on a CT scan.
However, if the protein content in the cyst fluid is relatively
high, the cyst may manifest as a soft tissue density shadow, which
can easily be misdiagnosed as an adrenal tumor or neurogenic cyst
(1). MRI is superior to CT scan
with regard to diagnosis of cysts. Fat-suppressed images may be
used to identify fat-containing masses, such as teratomas and
chylocysts (7). The case of the
present study exhibited a fluid-fluid level in the cyst, as
revealed using MRI. This is a rare phenomenon, as suggested by
previous literature reports (13).
The lower layer was a denser, protein-containing precipitate. Due
to the potential risk of malignant transformation, the majority of
clinicians tend to select surgical treatment for retroperitoneal
bronchial cysts, which is associated with a more favorable
prognosis (25). In the case
described in the present study, no blood cells or calcium
components were found in the fluid in the cyst. All of the cases
listed in Table I were found in
mediastinal and retroperitoneal regions. The fluid-fluid level was
frequently detected by CT or MRI, the formation of which was
indicated to be related to calcium or protein deposition.
Consistent with the clinical manifestations of bronchogenic cysts,
those bronchogenic cysts with fluid-fluid level also tended to lack
clinical symptoms, which only occur when the cyst became too large
or infected. For patients able to endure surgical treatment
according to their age and physical condition, surgical treatment
may result in a favorable prognosis.
In conclusion, the presence of a fluid-fluid level
in a retroperitoneal bronchogenic cyst is rare and can be easily
misdiagnosed, particularly in the abdominal aorta and the
paravertebral region. Surgical resection would be ideal in
providing a definitive diagnosis and relieving symptoms, with
favorable patient prognosis.
Acknowledgements
Not applicable.
Funding
Funding: The present report was supported by the National
Natural Science Foundation of China (grant nos. 82172477 and
81600696) and the Natural Science Foundation of Fujian Province of
China (grant no. 2019J01144).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WX and ZeH designed and performed the study,
collected data and wrote the manuscript. ZiH, LX, ZC and BZ
performed the literature search and pathological analysis. LZ and
KL collected data and approved the manuscript. DL conceived and
designed the study, collected data and wrote the manuscript. WX and
DL checked and confirmed the authenticity of the raw data. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present report was approved by Xiamen University
Ethics Committee (Zhangzhou, China) and was conducted in accordance
with the Declaration of Helsinki.
Patient consent for publication
The patient provided written informed consent for
the publication of his data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yang DM, Jung DH, Kim H, Kang JH, Kim SH,
Kim JH and Hwang HY: Retroperitoneal cystic masses: CT, clinical,
and pathologic findings and literature review. Radiographics.
24:1353–1365. 2004.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tang J, Zeng Z, Deng S and Lin F: Ectopic
bronchogenic cyst arising from the diaphragm: A rare case report
and literature review. BMC Surg. 21(321)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hamad AM, Rea F and Haroon S: Bronchial
atresia and bronchogenic cyst with saprophytic aspergilloma. Am J
Respir Crit Care Med. 203:e33–e34. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Liang MK, Yee HT, Song JW and Marks JL:
Subdiaphragmatic bronchogenic cysts: A comprehensive review of the
literature. Am Surg. 71:1034–1041. 2005.PubMed/NCBI
|
|
5
|
Tu C, Zhu J, Shao C, Mao W, Zhou X, Lin Q,
Li Z, Zhang J, Zhou Q and Chen W: Gastric bronchogenic cysts: A
case report and literature review. Exp Ther Med. 11:1265–1270.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Syred K and Weissferdt A: Non-neoplastic
mediastinal cysts. Adv Anat Pathol. 27:294–302. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
McAdams HP, Kirejczyk WM,
Rosado-de-Christenson ML and Matsumoto S: Bronchogenic cyst:
Imaging features with clinical and histopathologic correlation.
Radiology. 217:441–446. 2000.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Xu Q, Feng Y, Ye K, Zhou Y and Zhan R:
Bronchogenic cyst in left anterior cranial fossa. Neurology.
84:1181–1182. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yilmaz C, Gulsen S, Sonmez E, Ozger O,
Unlukaplan M and Caner H: Intramedullary bronchogenic cyst of the
conus medullaris. J Neurosurg Spine. 11(477)2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jiang C, Wang H, Chen G, Jiang G and Zhang
P: Intradiaphragmatic bronchogenic cyst. Ann Thoracic Surg.
96:681–683. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sun B, Wang A, Chen H, Qian B, Yi X, Jiang
Y, Li Q, Fu W and Li J: Bronchogenic cyst of the stomach: A case
report and literature review. Exp Ther Med. 20(166)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sanli A, Onen A, Ceylan E, Yilmaz E,
Silistreli E and Açikel U: A case of a bronchogenic cyst in a rare
location. Ann Thoracic Surg. 77:1093–1094. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lyon RD and Mcadams HP: Mediastinal
bronchogenic cyst: Demonstration of a fluid-fluid level at MR
imaging. Radiology. 186:427–428. 1993.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bargallo J, Luburich P, Garcia-Barrionuevo
J and Sanchez-Gonzalez M: Fluid-fluid level in bronchogenic cysts.
Radiology. 188:881–882. 1993.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Aydingöz U, Ariyürek M, Selçuk ZT,
Demirkazik FB and Bariş YI: Calcium within a bronchogenic cyst with
a fluid level. Brit J Radiol. 70:761–763. 1997.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Han SE, Kwon WJ, Cha HJ, Lee YJ, Lee T,
Seo KW, Jegal Y, Ahn J and Ra SW: Mediastinal bronchogenic cysts:
Demonstration of fluid-fluid level in bronchoscopic US imaging. J
Bronchology Interv Pulmonol. 24:153–155. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Park JW, Jeong WG, Lee JE, Lee HJ, Ki SY,
Lee BC, Kim HO, Kim SK, Heo SH, Lim HS, et al: Pictorial review of
mediastinal masses with an emphasis on magnetic resonance imaging.
Korean J Radiol. 22:139–154. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jo W, Shin JS and Lee IS:
Supradiaphragmatic bronchogenic cyst extending into the
retroperitoneum. Ann Thoracic Surg. 81:369–370. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kunisaki SM: Narrative review of
congenital lung lesions. Transl Pediatr. 10:1418–1431.
2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sumiyoshi K, Shimizu S, Enjoji M, Iwashita
A and Kawakami K: Bronchogenic cyst in the abdomen. Virchows Arch A
Pathol Anat Histopathol. 408:93–98. 1985.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Díaz Nieto R, Naranjo Torres A, Gómez
Alvarez M, Ruiz Rabelo JF, Pérez Manrique MC, Ciria Bru R, Valverde
Martínez A, Roldán de la Rúa J, Alonso Gómez J and Rufián Peña S:
Intraabdominal bronchogenic cyst. J Gastrointest Surg. 14:756–758.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Anderson MI, O'Reilly KJ and Costabile RA:
Retroperitoneal bronchogenic cyst mimicking a pheochromocytoma. J
Urol. 166:1379–1380. 2001.PubMed/NCBI
|
|
23
|
Kawaguchi Y, Hanaoka J, Asakura S and
Fujita T: Infected bronchogenic cyst treated with drainage followed
by resection. Ann Thoracic Surg. 98:332–334. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Altieri MS, Zheng R, Pryor AD, Heimann A,
Ahn S and Telem DA: Esophageal bronchogenic cyst and review of the
literature. Surg Endosc. 29:3010–3015. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kirmani B, Kirmani B and Sogliani F:
Should asymptomatic bronchogenic cysts in adults be treated
conservatively or with surgery? Interact Cardiovasc Thorac Surg.
11:649–659. 2010.PubMed/NCBI View Article : Google Scholar
|