Introduction
Acute myocardial infarction (AMI) is a fatal disease
that results in high morbidity and mortality rates. Blood urea
nitrogen (BUN) and creatinine (Cr) are the end products of nitrogen
metabolism in humans. They are small molecules that can be filtered
from nephrons. Usually, 30-40% of BUN is reabsorbed from the kidney
tubules (1). By contrast, Cr is
not as well reabsorbed as BUN (1,2). BUN
is an important parameter that reflects the relationship among the
patient's kidney condition, protein metabolism level and
nutritional status (2). Previous
studies have demonstrated that urea nitrogen levels are closely
related to mortality (3,4). A high BUN level could be a useful
predictor of in-hospital mortality in patients with AMI (5). Clinically, Cr content is often used
to detect changes in renal function, which aids in the detection of
renal failure or improvement in renal function. The use of Cr in
clinical practice is supported by the findings of the study by
Granger et al (6), which
reported that Cr is a marker of renal function and established a
relationship between renal dysfunction and increased mortality in
patients with AMI.
The BUN/Cr ratio is defined as the ratio of BUN to
serum Cr. As a novel biomarker, the BUN/Cr ratio has emerged as an
independent prognostic indicator of poor outcomes in different
disease conditions, such as chronic and acute heart failure (AHF)
(7-9),
acute and chronic kidney injury (10), and ischemic stroke (11). Studies demonstrated that an
elevated BUN/Cr ratio was associated with a poor prognosis in
patients with AHF, and an elevated BUN/Cr ratio was found to be an
independent predictor of all-cause mortality (1,12).
There is existing research on the risk factors for
mortality in patients with HF (1).
However, the relationship between the BUN/Cr ratio and in-hospital
mortality has not been fully investigated in patients with AMI in
the intensive care unit (ICU). In this context, the present study
aimed to comprehensively evaluate the role of the BUN/Cr ratio in
predicting severity and survival of patients with AMI.
Materials and methods
Study design
The present study was a multicentre retrospective
observational study. Analyses were performed on data subsets
(median age, 65.0 years; range, 56.0-75.0 years; 64.2% male)
obtained from participants in the electronic ICU collaborative
research database (eICU-CRD; https://eicu-crd.mit.edu), which is an open-access
de-identified dataset of patients maintained by the Laboratory for
Computational Physiology at the Massachusetts Institute of
Technology (Cambridge, MA, USA). The eICU-CRD includes patients
admitted to 208 US hospitals that were monitored by the eICU
programs between 2014 and 2015 (13,14).
The database stores records of demographic characteristics, hourly
physiological readings from bedside monitors, disease diagnoses
using the International Classification of Diseases Ninth Revision
(ICD-9) code (15) and other
clinical data collected during routine medical care. Since all
protected health information was anonymized, the requirement for
individual patient consent was waived. The use of this database was
approved by the Institutional Review Boards of the Massachusetts
Institute of Technology (Cambridge, MA, USA). All authors of this
manuscript completed the necessary training and received permission
to access the database. One author obtained access to the database
and was responsible for data extraction (certification no.
42039823). Bona fide researchers can apply to access the
eICU-CRD via a standard application procedure (further details
available at https://eicu-crd.mit.edu/about/eicu/). The present
study was performed following the Declaration of Helsinki. All
methods follow the guidelines and regulations stated by the
Strengthening the Reporting of Observational Studies in
Epidemiology (STROBY) Statement.
Data on demographics, comorbidities, vital signs,
laboratory tests, use of vasoactive drugs and operations were
obtained from the eICU-CRD. Used drugs included norepinephrine,
dopamine and epinephrine. The serum laboratory variables measured
during the first 24 h of ICU admission were used in the present
study. If variables were measured multiple times in the first 24 h,
the first measure was used in the present study. Records with
>10% missing variables were excluded. For records with ≤10%
missing variables, the multiple imputation method was used to deal
with the missing data. The multiple imputation methods imputes
multiple values for each missing value. This results in the
creation of multiple complete data sets in which the missing values
have been filled in with plausible values. The analysis of
scientific interest is then conducted separately in each of these
complete data sets and the results are pooled across the imputed
data sets. In this way, the multiple imputation allows the user to
explicitly incorporate the uncertainty about the true value of
imputed variables (16).
Clinical endpoints
The primary endpoint of the present study was
in-hospital mortality. The patients were divided into two groups:
Survivors and non-survivors. The intergroup differences in
parameters measured in the ICU were then evaluated.
Study population
Patients were diagnosed with AMI according to the
ICD-9 code, which was 140. The following inclusion criteria were
applied: i) Age ≥18 years; and ii) first ICU admission with a first
diagnosis of AMI. AMI was identified from the ICD-9 code in the
eICU-CRD. The following exclusion criteria were used: i) Non-first
ICU admission; ii) ICU stay <24 h; iii) missing ICU outcome; iv)
history of confirmed renal failure; v) blood transfusion received
during the 24 h before admission; vi) evidence of thrombocytopenia;
vii) coagulopathy; viii) history of injecting cephalosporins or any
other drug interfering with BUN or Cr evaluation; ix) both upper
and lower gastrointestinal bleeding; and x) missing Cr and BUN
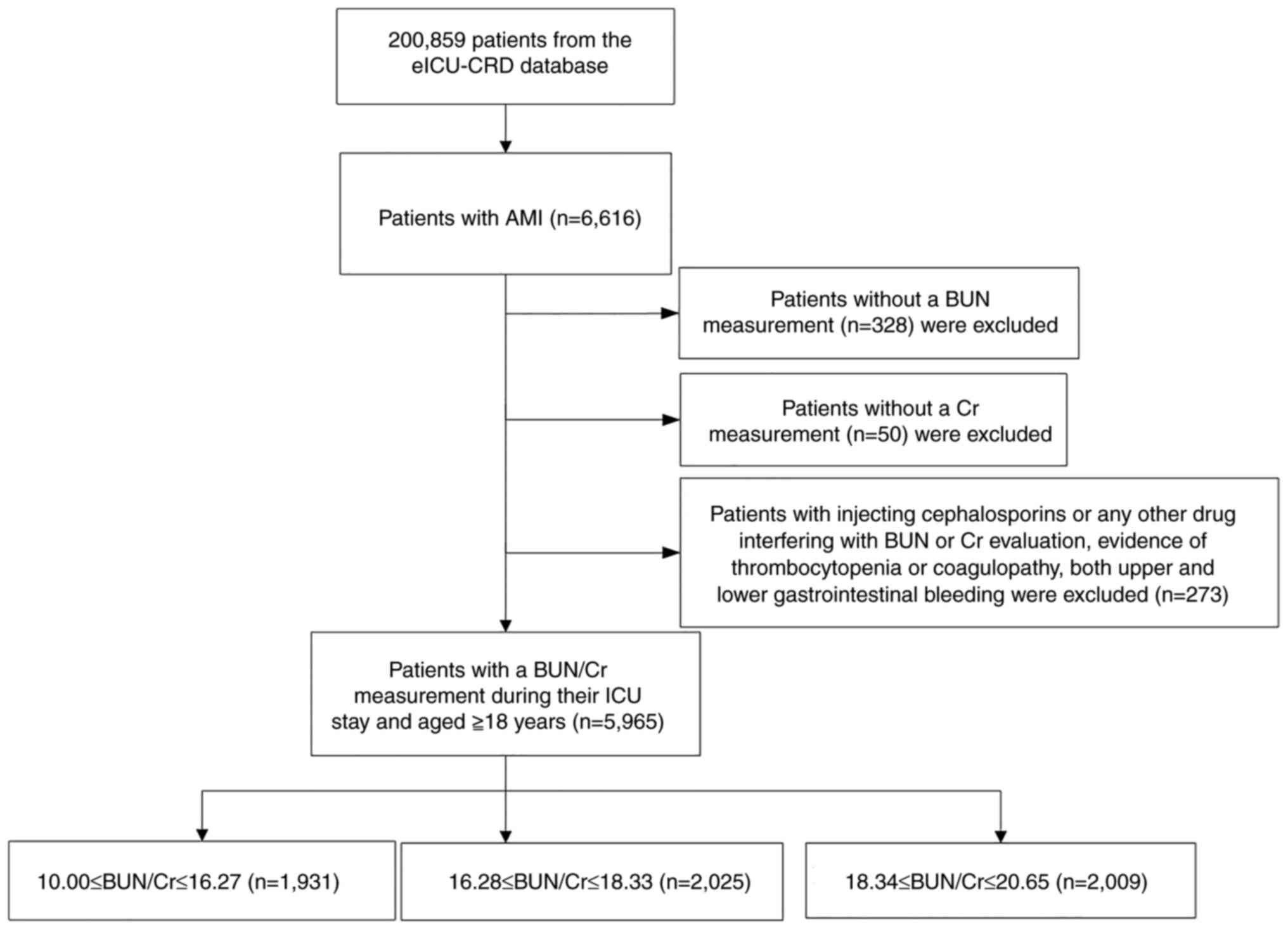
measurements after ICU admission or system error (6). The study population comprised 5,965
patients with AMI [median age, 65.0 years; range, 56.0-75.0 years;
3,832 (64.2%) male]. The selection procedure for the study
participants is summarized in Fig.
1.
Definition of AMI
Clinical evidence of acute myocardial injury was
defined as a rise and/or fall in the cardiac troponin I (cTnI)
values with at least one value >99th percentile of the upper
reference limit and at least one of the following symptoms of
myocardial ischemia: Symptoms of acute myocardial ischemia, new
ischemic electrocardiogram changes, development of pathological Q
waves, and imaging evidence of new loss of viable myocardium or new
regional wall motion abnormality in a pattern consistent with an
ischemic aetiology (17,18).
Definition and assessment of HF
HF is not a single pathological diagnosis, but a
clinical syndrome consisting of cardinal symptoms (e.g.,
breathlessness, ankle swelling and fatigue) that may be accompanied
by signs (e.g., elevated jugular venous pressure, pulmonary
crackles and peripheral oedema). HF is due to a structural and/or
functional abnormality of the heart that results in elevated
intracardiac pressures and/or inadequate cardiac output at rest
and/or during exercise. The criteria for diagnosis of HF require
evidence of increased left ventricle filling pressures at rest,
exercise, or other provocations. The criteria were fulfilled with
findings of elevated levels of natriuretic peptides,
echocardiographic diastolic parameters such as an E/e' ≥15 or other
evidence of elevated filling pressures, or invasive hemodynamic
measurement at rest or exercise (19,20).
Statistical analysis
For continuous variables, the Kolmogorov-Smirnov
test was used to check the normality of data distribution.
Continuous variables with skewed distribution are presented as the
median (interquartile range) and comparison among groups was
performed using the Kruskal-Wallis H test and Dunn's post hoc test.
Categorical or dichotomous variables, which are presented as
absolute values and percentages, were compared using the
χ2 test.
The cumulative survival rate was calculated using
the Kaplan-Meier method and the log-rank test was used for
comparison between groups. Cox proportional hazard models were used
to estimate the hazard ratio (HR) and 95% CI of the second and
third tertiles relative to the first tertile for in-hospital
mortality. Crude regression estimates and estimates adjusted for
covariates are presented. After considering the clinical
significance, the covariates that were significantly associated
with the response variable (P<0.05) or those that changed the
effect estimate by ≥10% were retained in the final adjusted model
(21). The variables adjusted for
in the micro adjustment model (adjusted model I) included age, sex
and ethnicity. The variables adjusted for in the overall adjustment
model (adjusted model II) included age, sex, ethnicity, BMI, heart
rate, oxygen saturation, platelets, total protein, AMI category,
coronary artery bypass grafting (CABG), HF, history of diabetes
mellitus, history of hypertension, percutaneous coronary
intervention (PCI), and administration of norepinephrine, dopamine
and epinephrine.
Subsequently, a generalized additive model was used
to identify the dose-response relationship between the BUN/Cr ratio
and in-hospital mortality. If a non-linear association was
detected, a two-piecewise linear regression model was used to
determine the threshold effect of the BUN/Cr ratio on in-hospital
mortality in accordance with the smoothing plot. If the BUN/Cr and
in-hospital mortality ratio appeared in the smoothing plot, the
inflection point was determined automatically by the recursive
method using the maximum model likelihood (22,23).
Finally, the modification and interaction of the subgroups were
inspected using the likelihood ratio test. Receiver operating
characteristic (ROC) curves were generated to calculate the
sensitivity and specificity of the BUN/Cr ratio, while the area
under the curve (AUC) was calculated to ascertain the quality of
the BUN/Cr ratio as a predictor of in-hospital mortality in
patients with AMI.
All data were analysed using R software (version
3.42; R Foundation for Statistical Computing) and Empower Stats
version 2.17.8 (http://www.empowerstats.com/cn/). P<0.05 was
considered to indicate a statistically significant difference and
all reported P-values were two-sided.
Results
Study participants and baseline
characteristics
The data of a total of 6,616 patients with AMI were
extracted from eICU-CRD. Patients without data for BUN (n=328) or
Cr (n=50) levels were excluded from the study. Patients with a
history of confirmed renal failure, those who had received a blood
transfusion during the 24 h before admission, those showing
evidence of thrombocytopenia, coagulopathy or having a history of
injecting cephalosporins or any other drug interfering with BUN or
Cr evaluation, as well as patients with both upper and lower
gastrointestinal bleeding (n=273), were excluded from the study.
The ICU admission rate of patients without a BUN or Cr level was
5.7% (378 out of 6,616 patients) and a total of 5,965 patients were
included in the statistical analysis. A flow chart of the study is
shown in Fig. 1.
Baseline characteristics according to BUN/Cr
tertiles are shown in Table I. The
mean BUN/Cr ratio was 17.3±1.9. According to the BUN/Cr ratio, a
total of 1,931, 2,025 and 2,009 patients fell into tertile 1, 2 and
3, respectively. The BUN/Cr tertiles were 10.00-16.27 (tertile 1),
16.28-18.33 (tertile 2) and 18.34-20.65 (tertile 3). No
statistically significant differences were detected among the
groups in terms of the levels of aspartate transaminase, alanine
transaminase (ALT), levels of platelets, prothrombin time
international normalized ratio, heart rate, systolic blood
pressure, and diastolic blood pressure. Common characteristics
among patients with high BUN/Cr ratio levels were older age, being
a Caucasian, having a longer hospital stay, a higher white blood
cell count and red blood cell distribution width, and greater
high-density lipoprotein (HDL) and potassium values, CABG, history
of diabetes and history of hypertension (P<0.05). The opposite
trend was observed for BMI, red blood cell count, total
cholesterol, triglycerides, low-density lipoprotein (LDL) and PCI
(P<0.05). Furthermore, patients with higher BUN/Cr levels made
more use of vasoactive drugs (norepinephrine, dopamine and
epinephrine) (P<0.05).
 | Table IBaseline characteristics of
patients. |
Table I
Baseline characteristics of
patients.
| | Tertiles of
BUN/Cr | |
|---|
|
Characteristics | All patients | Tertile 1
(10.00-16.27) | Tertile 2
(16.28-18.33) | Tertile 3
(18.34-20.65) | P-value |
|---|
| No. of
participants | 5,965 | 1,931 | 2,025 | 2,009 | |
| Age, years | 65.00
(56.00-75.0) | 60.00
(52.00-69.00) | 65.00
(56.00-73.00) | 71.00
(63.00-79.00) | <0.001 |
| Sex, n (%) | | | | | <0.001 |
|
Female | 2,133 (35.68) | 662 (34.28) | 650 (32.10) | 821 (40.87) | |
|
Male | 3,832 (64.24) | 1,269 (65.72) | 1,375 (67.90) | 1,188 (59.13) | |
| Ethnicity, n
(%)a | | | | | <0.001 |
|
Caucasian | 4,642 (77.82) | 1,442 (75.78) | 1,604 (80.32) | 1,596 (80.40) | |
|
Non-Caucasian | 1,243 (20.84) | 461 (24.22) | 393 (19.68) | 389 (19.60) | |
| BMI,
kg/m2 | 28.34
(24.79-32.97) | 28.52
(25.05-32.82) | 28.67
(25.14-33.39) | 27.93
(24.20-32.75) | <0.001 |
| Length of hospital
stay, days | 3.80
(2.26-7.59) | 3.04
(2.08-6.05) | 3.43
(2.20-7.14) | 5.21
(2.90-9.07) | <0.001 |
| BUN/Cr | 17.39
(15.87-18.92) | 15.38
(14.52-15.79) | 17.35
(16.85-17.93) | 19.35
(18.92-19.88) | <0.001 |
| Estimated
glomerular filtration rate, ml/min per 1.73 m2 | 71.81
(47.36-93.10) | 70.05
(43.48-89.07) | 73.85
(50.73-93.52) | 71.72
(47.79-96.72) | <0.001 |
| White blood cells,
x109 | 10.80
(8.40-14.00) | 10.44
(8.18-13.20) | 10.80
(8.34-13.70) | 11.28
(8.70-15.20) | <0.001 |
| Red blood cells,
x109 | 4.17
(3.65-4.62) | 4.31
(3.84-4.73) | 4.25
(3.74-4.63) | 3.95
(3.47-4.42) | <0.001 |
| Red blood cell
distribution width, % | 13.90
(13.20-14.90) | 13.70
(13.10-14.60) | 13.70
(13.20-14.70) | 14.30
(13.50-15.40) | <0.001 |
| Platelets,
x109 | 207.00
(169.00-252.00) | 208.00
(173.00-253.00) | 208.00
(169.00-250.00) | 205.50
(164.00-254.00) | 0.165 |
| Aspartate
transaminase, U/l | 66.50
(32.00-163.00) | 70.00
(32.00-155.00) | 66.00
(31.00-169.50) | 64.00
(33.00-171.25) | 0.977 |
| Alanine
transaminase, U/l | 35.00
(22.00-65.50) | 34.00
(22.00-59.00) | 36.00
(23.00-65.00) | 36.00
(22.00-73.00) | 0.165 |
| Total cholesterol,
mmol/l | 158.00
(131.00-188.00) | 165.00
(138.00-197.00) | 158.00
(131.00-186.00) | 150.00
(121.00-181.00) | <0.001 |
| Triglyceride,
mmol/l | 117.00
(83.00-170.00) | 122.00
(89.00-177.00) | 114.00
(84.00-171.00) | 113.00
(78.00-163.50) | 0.002 |
| High-density
lipoprotein, mmol/l | 38.00
(31.00-46.00) | 38.00
(31.00-46.00) | 37.00
(31.00-46.00) | 39.00
(31.00-48.00) | 0.020 |
| Low-density
lipoprotein, mmol/l | 92.00
(67.00-120.00) | 97.00
(71.00-126.00) | 92.00
(68.50-117.00) | 82.50
(59.00-111.75) | <0.001 |
| Potassium,
mmol/l | 4.00
(3.80-4.40) | 4.00
(3.70-4.30) | 4.00
(3.80-4.30) | 4.10
(3.80-4.50) | <0.001 |
| Sodium, mmol/l | 138.00
(136.00-140.00) | 138.00
(135.00-140.00) | 138.00
(136.00-140.00) | 138.00
(136.00-140.00) | 0.025 |
| Prothrombin time
international normalized ratio | 1.20
(1.09-1.40) | 1.20
(1.10-1.40) | 1.20
(1.09-1.40) | 1.20
(1.07-1.40) | 0.369 |
| Heart rate,
beats/min | 81.00
(70.00-94.00) | 81.00
(70.00-94.00) | 81.00
(70.00-94.00) | 80.00
(69.00-93.00) | 0.610 |
| Systolic blood
pressure, mmHg | 122.00
(103.00-142.00) | 122.00
(102.00-142.50) | 122.00
(103.00-143.00) | 123.00
(104.00-142.00) | 0.866 |
| Diastolic blood
pressure, mmHg | 62.00
(51.00-74.00) | 61.00
(50.00-72.00) | 63.00
(51.00-74.00) | 61.00
(51.00-74.00) | 0.440 |
| Percutaneous
coronary intervention, n (%) | | | | | <0.001 |
|
No | 3,788 (63.50) | 1,140 (59.04) | 1,241 (61.28) | 1,407 (70.03) | |
|
Yes | 2,177 (36.50) | 791 (40.96) | 784 (38.72) | 602 (29.97) | |
| Coronary artery
bypass grafting, n (%) | | | | | 0.023 |
|
No | 5,199 (87.16) | 1,714 (88.76) | 1,760 (86.91) | 1,725 (85.86) | |
|
Yes | 766 (12.84) | 217 (13.09) | 265 (13.09) | 284 (14.14) | |
| Heart failure, n
(%) | | | | | <0.001 |
|
No | 5,168 (86.99) | 1,738 (90.19) | 1,822 (90.47) | 1,605 (80.40) | |
|
Yes | 773 (13.01) | 189 (9.81) | 192 (9.53) | 392 (19.60) | |
| History of diabetes
n (%) | | | | | <0.001 |
|
No | 4,057 (68.29) | 1,449 (75.19) | 1,392 (69.12) | 1,216 (60.80) | |
|
Yes | 1,884 (31.71) | 478 (24.81) | 622 (30.88) | 784 (39.20) | |
| History of
hypertension, n (%) | | | | | <0.001 |
|
No | 2,596 (43.70) | 980 (50.86) | 871 (43.25) | 745 (37.25) | |
|
Yes | 3,345 (56.30) | 947 (49.14) | 1,143 (56.75) | 1,255 (62.75) | |
| Acute myocardial
infarction category,n (%) | | | | | <0.001 |
|
Non-STEMI | 3,010 (50.46) | 875 (45.31) | 920 (45.43) | 1,215 (60.48) | |
|
STEMI | 2,955 (49.54) | 1,056 (54.69) | 1,105 (54.57) | 794 (39.52) | |
| Norepinephrine, n
(%) | | | | | <0.001 |
|
No | 4,223 (85.52) | 1,455 (89.48) | 1,428 (85.56) | 1,340 (81.56) | |
|
Yes | 715 (14.48) | 171 (10.52) | 241 (14.44) | 303 (18.44) | |
| Dopamine, n
(%) | | | | | 0.004 |
|
No | 4,661 (94.39) | 1,555 (95.63) | 1,578 (94.55) | 1,528 (93.00) | |
|
Yes | 277 (5.61) | 71 (4.37) | 91 (5.45) | 115 (7.00) | |
| Epinephrine, n
(%) | | | | | 0.001 |
|
No | 4,603 (93.22) | 1,547 (95.14) | 1,533 (91.85) | 1,523 (92.70) | |
|
Yes | 335 (6.78) | 79 (4.86) | 136 (8.15) | 120 (7.30) | |
The overall in-hospital mortality rate was 8.35%
(498 out of 5,965 patients). The in-hospital mortality of different
groups based on tertiles of BUN/Cr is shown in Fig. S1. In-hospital mortality was more
frequently observed in patients with higher BUN/Cr levels (1.73,
2.08 and 4.54% for the first, second and third tertiles,
respectively; P<0.001).
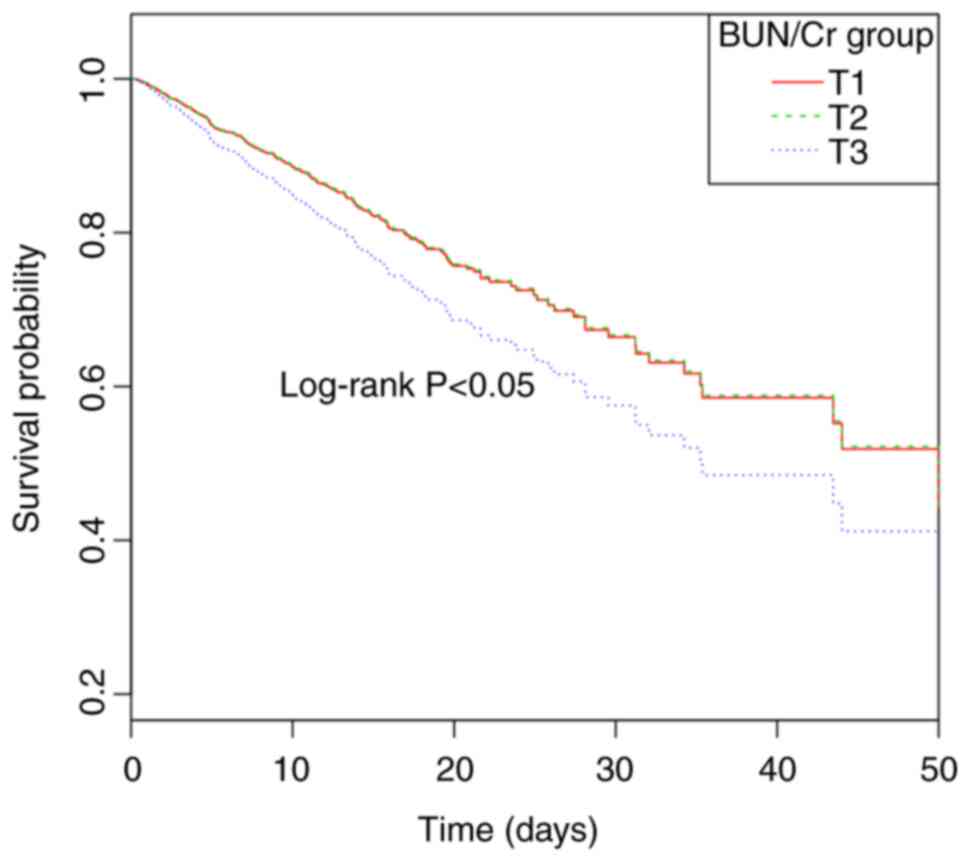
Kaplan-Meier survival curves of the
BUN/Cr ratio for predicting the in-hospital mortality among
patients with AMI
The Kaplan-Meier curves for the tertiles of the
BUN/Cr ratio are shown in Fig. 2.
The figure indicates that in-hospital mortality rates were highest
when the BUN/Cr ratio was ≥18.34 after adjustment for age, sex and
ethnicity (log-rank test P<0.05). Similar results were seen in
patients with AMI without HF. A BUN/Cr ratio was significantly
associated with the increased hospital and ICU mortality in
patients with AMI without HF (Table
SI; Fig. S2). The BUN/Cr
ratio was used to distinguish between different survival statuses
and it was shown to have a good discrimination value.
BUN/Cr ratio as a predictor of
in-hospital mortality
A total of three different models, the non-adjusted
model and adjusted models I and II, were constructed to analyse the
independent effects of the BUN/Cr ratio on the in-hospital
mortality of critically ill patients with AMI that were grouped
according to the BUN/Cr ratio tertiles. As shown in Table II, in adjusted model I, after
adjustment for age, sex and ethnicity, a higher BUN/Cr ratio was
associated with an increased risk of in-hospital mortality compared
with those in the first tertile. In adjusted model II, after
adjusting for more confounding factors, the BUN/Cr ratio was found
to be an independent predictor of in-hospital mortality in
critically ill patients with AMI as well (third vs. first tertile;
adjusted HR, 1.50; 95% CI, 1.08-2.09; P<0.05 for trend).
Consistent results were also obtained in patients with AMI but
without HF (Table SI).
 | Table IIAssociation between the BUN/Cr ratio
and in-hospital mortality in patients with acute myocardial
infarction in different models. |
Table II
Association between the BUN/Cr ratio
and in-hospital mortality in patients with acute myocardial
infarction in different models.
| Exposure | Non-adjusted model
HR (95% CI) | P-value | Adjusted model I HR
(95% CI) | P-value | Adjusted model II
HR (95% CI) | P-value |
|---|
| BUN/Cr | 1.09
(1.04-1.16) | 0.0002 | 1.06
(1.00-1.11) | 0.0447 | 1.07
(1.00-1.13) | 0.0510 |
| BUN/Cr
tertiles | | | | | | |
|
Tertile
1 | Reference | | Reference | | Reference | |
|
Tertile
2 | 1.02
(0.77-1.34) | 0.8974 | 0.99
(0.74-1.32) | 0.9467 | 1.07
(0.73-1.55) | 0.7328 |
|
Tertile
3 | 1.63
(1.28-2.08) | <0.0001 | 1.35
(1.04-1.75) | 0.0220 | 1.50
(1.08-2.09) | 0.0170 |
| P-value for
trend | | <0.0001 | | 0.0094 | | 0.0077 |
In addition, cTnI is a heart-specific protein
released in the circulation upon myocardial injury and serves a
role in the regulation of muscle contraction and cTns (24). Conventional assays for the analysis
of cTnI levels are routinely used to exclude AMI events and to
assess the 30- and 90-day prognoses of patients presenting with
acute coronary syndrome (ACS) (25,26).
Various studies have reported that the circulating levels of cTnI
after ST-segment elevation myocardial infarction (STEMI) are
related to clinical outcomes and are considered a prognostic
predictor of major adverse cardiovascular events (27-29).
The predictive values for in-hospital mortality of cTnI and the
BUN/Cr ratio were compared in patients with AMI. ROC curves
generated for BUN/Cr and cTnI are plotted in Fig. S3. The AUC for the BUN/Cr ratio was
0.619 (range, 0.586-0.652), whereas it was 0.499 (range,
0.467-0.532) for cTnI (P<0.001).
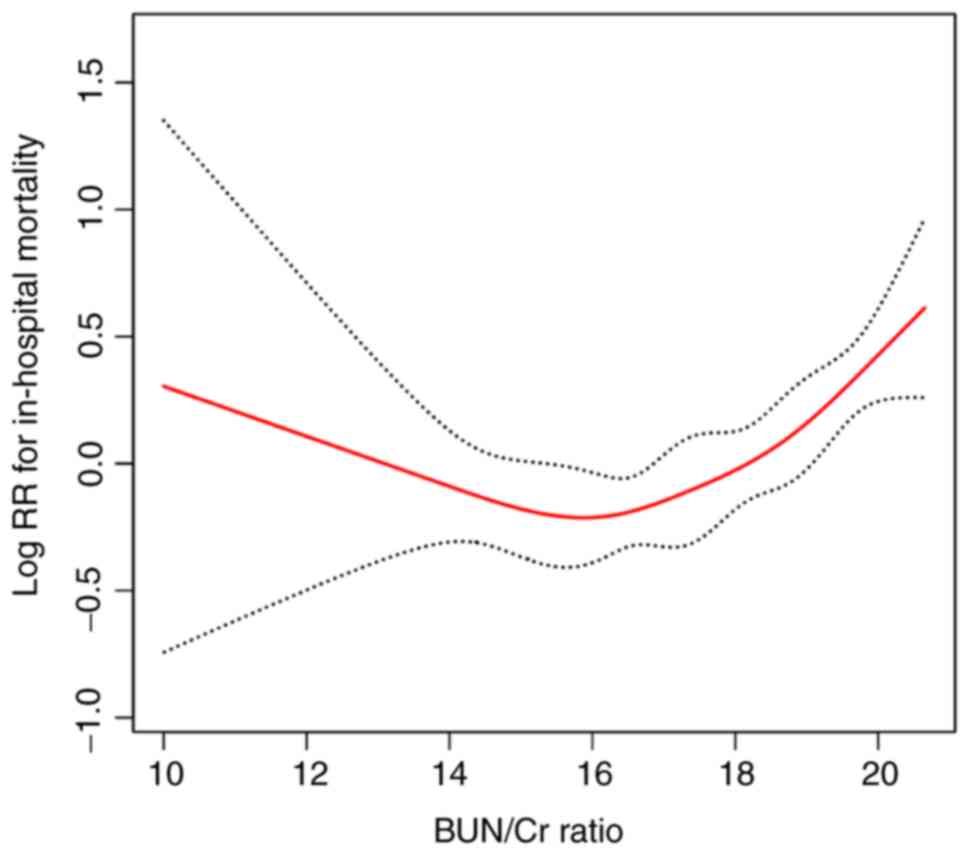
Analysis of the association between
the BUN/Cr ratio and in-hospital mortality
The present study (Fig.
3) revealed a non-linear relationship rather than a linear
interaction between the BUN/Cr ratio and in-hospital mortality
after adjusting for age, sex, ethnicity, BMI, heart rate, HDL, LDL,
ALT, AMI group, PCI, CABG, HF, history of diabetes and history of
hypertension. Using the two-piecewise linear regression model, the
inflection point was calculated as 18. The HR (95% CI) was 1.34
(1.17-1.54) with P<0.001 on the right of the inflection point.
However, on the left of the inflection point, the relationship
between the BUN/Cr ratio and in-hospital mortality was
non-significant (HR, 0.99; 95% CI, 0.91-1.08; P=0.8364; Table III).
 | Table IIIThreshold effect analysis of the
relationship between the BUN/Cr ratio and mortality using a
two-piecewise regression model. |
Table III
Threshold effect analysis of the
relationship between the BUN/Cr ratio and mortality using a
two-piecewise regression model.
| BUN/Cr ratio
inflection point | In-hospital
mortalityhazard ratio (95% CI) | P-value |
|---|
| <18 | 0.99
(0.91-1.08) | 0.836 |
| ≥18 | 1.34
(1.17-1.54) | <0.001 |
| Likelihood-ratio
test | | 0.003 |
Subgroup analyses
The results of the subgroup analyses are presented
in Table IV. After adjusting for
potential confounders, it was found that the interaction (between
the BUN/Cr ratio and AMI group) was statistically significant for
the AMI group (P<0.05). However, statistical significance was
not observed for age, sex, BMI, history of diabetes, history of
hypertension, PCI, CABG, glucose, heart rate, ALT and LDL. Evidence
of the BUN/Cr-AMI group being non-linear was also found. The effect
of the BUN/Cr ratio on in-hospital mortality differed among
patients with different AMI groups. The BUN/Cr ratio was associated
with in-hospital mortality (HR, 1.31; 95% CI, 1.19-1.44) in
patients with non-STEMI. However, there was no significant
relationship between the BUN/Cr ratio and the in-hospital mortality
in patients with STEMI. Furthermore, it was observed that the
BUN/Cr ratio was associated with in-hospital mortality if the
BUN/Cr ratio was ≥18 (P=0.0001).
 | Table IVEffect size of BUN/Cr on in-hospital
mortality in prespecified and exploratory subgroups. |
Table IV
Effect size of BUN/Cr on in-hospital
mortality in prespecified and exploratory subgroups.
|
Characteristics | No. of
participants | Hazard ratio (95%
CI) | Subgroup
P-value | P-value |
|---|
| BUN/Cr ratio | | | | 0.0013 |
|
<18 | 3,462 | 1.03 (0.93,
1.14) | 0.6817 | |
|
≥18 | 2,503 | 1.44 (1.20,
1.73) | 0.0001 | |
| Estimated
glomerular filtration rate, ml/min per 1.73 m2 | | | | 0.1943 |
|
<60 | 2,098 | 1.01 (1.00,
1.03) | 0.0008 | |
|
≥60 | 3,867 | 1.03 (1.02,
1.04) | <0.0001 | |
| Sex | | | | 0.1901 |
|
Female | 2,133 | 0.97 (0.77,
1.22) | 0.0607 | |
|
Male | 3,832 | 1.19 (0.96,
1.47) | 0.0031 | |
| Age, years | | | | 0.2092 |
|
<65 | 2,711 | 1.12 (1.01,
1.20) | 0.0183 | |
|
≥65 | 3,067 | 1.09 (1.01,
1.18) | 0.2078 | |
| BMI,
kg/m2 | | | | 0.5280 |
|
<28 | 2,770 | 1.12 (1.05,
1.19) | 0.0005 | |
|
≥28 | 3,076 | 1.06 (0.99,
1.15) | 0.0981 | |
| Heart failure | | | | 0.0522 |
|
No | 4,465 | 1.10
(0.91,1.32) | 0.0562 | |
|
Yes | 645 | 0.75
(0.53.1.05) | 0.1089 | |
| History of
diabetes | | | | 0.3897 |
|
No | 4,057 | 1.24 (1.00,
1.53) | <0.0001 | |
|
Yes | 1,884 | 1.038 (0.87,
1.35) | 0.4147 | |
| History of
hypertension | | | | 0.6017 |
|
No | 2,596 | 1.12 (1.02,
1.17) | 0.0025 | |
|
Yes | 3,345 | 1.09 (1.02,
1.17) | 0.0252 | |
| Coronary artery
bypass grafting | | | | 0.6173 |
|
No | 5,199 | 1.11 (1.05,
1.17) | <0.0001 | |
|
Yes | 766 | 1.16(0.91,
1.24) | 0.6480 | |
| Percutaneous
coronary intervention | | | | 0.1418 |
|
No | 3,788 | 1.08 (1.02,
1.14) | 0.0005 | |
|
Yes | 2,177 | 1.20 (1.06,
1.35) | 0.0021 | |
| Glucose, mg/dl | | | | 0.4315 |
|
<128 | 2,847 | 1.09 (1.01,
1.17) | 0.0407 | |
|
≥128 | 2,858 | 1.113 (1.05,
1.22) | 0.0030 | |
| Acute myocardial
infarction group | | | | <0.0001 |
|
STEMI | 3,010 | 1.02 (0.97,
1.09) | 0.3638 | |
|
Non-STEMI | 2,955 | 1.31 (1.19,
1.44) | <0.0001 | |
| Heart rate,
beats/min | | | | 0.6369 |
|
<80 | 2,806 | 1.12 (1.04,
1.20) | 0.0102 | |
|
≥80 | 3,115 | 1.09 (1.09,
1.17) | 0.0172 | |
| Alanine
transaminase, U/l | | | | 0.6116 |
|
<36 | 1,585 | 0.98 (0.78,
1.23) | 0.0008 | |
|
≥36 | 1,570 | 1.06 (0.86,
1.32) | 0.4424 | |
| Low density
lipoprotein, mmol/l | | | | 0.7413 |
|
<90 | 1,119 | 1.225 (1.06,
1.46) | 0.0071 | |
|
≥90 | 1,186 | 1.31 (1.05,
1.63) | 0.0175 | |
Discussion
The results of the present study revealed that an
elevated BUN/Cr ratio indicated an increased risk of in-hospital
death in patients with AMI. Even after adjusting for confounding
factors in the multivariate models, the BUN/Cr ratio was associated
with adverse outcomes. The findings of the present study not only
are in agreement with those of the aforementioned previous studies
but also demonstrate a non-linear relationship between the BUN/Cr
ratio and in-hospital mortality in patients with AMI (1,7).
Upon conducting a subgroup analysis, it was found that the BUN/Cr
ratio was associated with an increased risk of in-hospital death in
critically ill patients with AMI.
BUN is not a specific marker of renal insufficiency.
Cr is affected by extra-renal factors, such as muscle mass, sex,
age, nutrition and ethnicity (5).
Therefore, predictions based on BUN or Cr alone might have
limitations. Although estimated glomerular filtration rate (eGFR)
improves the assessment of renal function, overestimation and
underestimation still exist among patients with a wide range of
serum Cr levels (30). Similarly,
the serum concentrations of BUN are influenced by several factors
(neurohormonal activation, protein intake and catabolic processes)
(31). BUN levels reflect
persistent and inappropriate renin-angiotensin-aldosterone system
and vasopressin activation in HF, but are not necessarily related
to a decrease in eGFR. Hence, it is not necessarily a marker of
decreased eGFR (32). Therefore,
the BUN/Cr ratio has been proposed as a useful parameter to reduce
the effect of the aforementioned influencing factors. The BUN/Cr
ratio might be a marker for evaluation of the prognosis of patients
with AMI, which is more stable and accurate than serum Cr or BUN
individually (9,33).
Brisco et al (34) also found an association between
elevated BUN/Cr ratio upon admission and increased mortality. An
elevated BUN/Cr ratio usually indicates serious medical conditions
and a poor prognosis in patients with acute kidney injury (AKI) and
AHF (7,35). Qian et al (1) reported that AHF combined with an
elevated BUN/Cr ratio was associated with an increased risk of
mortality in patients with AMI. This finding suggested that the
BUN/Cr ratio has a predictive value for prognosis in patients with
AMI complicated with AHF. Parrinello et al (36) found that a BUN/Cr ratio ≥22 was
associated with poor survival prognosis in patients with AHF. In
addition, Murata et al (37) indicated that the BUN/Cr ratio was a
factor involved in the treatment and clinical follow-up of patients
with AMI, since there was a strong association between a high
BUN/Cr ratio and long-term mortality in patients with AMI. The
findings of this study are consistent with the present research. In
the current study, the BUN/Cr ratio had a predictive value for the
prognosis of patients with AMI and the risk was highest in patients
with a high BUN/Cr ratio. In further analysis, patients with AMI
and HF were excluded, and the results were still consistent.
However, Núñez (38) demonstrated
that in patients with AMI without AHF, there was no association
between the BUN/Cr ratio and prognosis. In the present study, there
was no significant relationship between the BUN/Cr ratio and the
in-hospital mortality in patients with STEMI. This is consistent
with previous research results. However, the BUN/Cr ratio was
associated with in-hospital mortality in patients with non-STEMI.
The reason may be related to the following aspects: i) Some factors
might have affected the baseline BUN/Cr, such as a high protein
diet and hepatic insufficiency, and the serum composition is
influenced by important extrarenal factors such as muscle mass,
sex, age, nutrition and ethnicity; ii) the sample size of the
present study was larger and the data might be more representative
since the current study investigated patients with AMI, who were
enrolled in a multicentre registry and critically ill, and included
50.46% of patients with non-STEMI and 49.54% of patients with
STEMI; iii) in-hospital mortality was 8.35% (498/5,965) in the
study cohort and the AMI mortality was higher than that in another
study (39), which may be related
to the severity of the illness. Some patients were too sick to
receive standard treatments, including PCI, CABG and medical
therapy; and iv) among patients with AMI, pathophysiology,
management and outcomes differ between those with STEMI and
non-STEMI. Traditionally, patients with non-STEMI have more
frequent risk factors and comorbidities, and a greater burden of
coronary artery disease (40,41).
The present study found that the prevalence of comorbid diseases
was higher among patients with a high BUN/Cr ratio, suggesting that
comorbid disease events are likely to explain the increased risk of
death in these individuals. A higher percentage of patients with HF
and a higher average age among those with a high BUN/Cr ratio were
also reported.
There is a close bidirectional relationship between
the heart and the kidney. HF is a complex syndrome that affects
almost all organs and systems of the body. Renal dysfunction is one
of the most important comorbidities in patients with chronic HF and
is accentuated, or becomes more evident, during episodes of acute
HF. This relationship is reflected in cardiorenal syndrome (CRS)
(32). There are five types of
CRS. CRS type 1 is characterized by the development of AKI and
dysfunction in patients with acute cardiac illness (42). Worsening renal function that occurs
in patients with acute HF has been classified as CRS type 1. In
this setting, worsening renal function is a common finding and is
due to complex, multifactorial, and not fully understood processes
involving hemodynamic (renal arterial hypoperfusion and renal
venous congestion) and non-hemodynamic factors (32). Cardiac function in patients with
AMI has a different degree of reduction in the short term (43,44).
Thus, the BUN/Cr ratio has a greater guiding value in the clinical
treatment of patients with AMI. It is currently widely considered
that activation of the renin-angiotensin-aldosterone system and the
sympathetic nervous system is associated with adverse prognosis
(45). For patients with AMI with
complications, a higher BUN/Cr ratio reflects a more active
neurohormonal system (32). Being
complex and multifactorial, the pathophysiology of renal
dysfunction in AMI remains unclear. Nonetheless, an imbalance among
abnormal hemodynamic, neurohormonal activation inflammatory
responses, intrinsic tubular damage and heterogeneous response to
therapeutic interventions has been proposed as the most common
pathogenic pathway (32).
The present study has several strengths. To the best
of our knowledge, it is the first to investigate the relationship
between the BUN/Cr ratio and in-hospital mortality in patients with
AMI based on a large and diverse population from the publicly
available eICU-CRD (13), which
increased the significance of the present results. In addition,
after adjusting for several confounding factors, multiple Cox
regression analyses were performed and the relationship between the
BUN/Cr ratio and in-hospital mortality was still observed,
indicating the good stability of the present results. Since the
BUN/Cr ratio was the basic index of clinical blood routine, the
parameters were simple to collect. These results can be used to
support other death indexes and improve the accuracy of prognosis
prediction for patients with AMI. Therefore, the BUN/Cr ratio is
recommended for use in predicting the in-hospital mortality of AMI,
as it is cost-effective and easy to apply.
The Global Registry of Acute Coronary Events (GRACE)
risk score was initially established to predict in-hospital
mortality in patients with ACS (6)
and is currently the guideline-recommended risk model for guiding
the management of myocardial infarction (46,47).
The present study extracted the in-hospital mortality and AMI data
from the eICU-CRD, but could not obtain the GRACE risk score.
Therefore, it only compared the predictive value of cTnI with the
BUN/Cr ratio for in-hospital mortality in patients with AMI. In
future studies, the GRACE risk score will be collected to compare
the predictive value of this score with BUN/Cr for in-hospital
mortality.
Although the present study is based on a large
multicentre critical care database, it still has some limitations.
This was a retrospective study derived from an observational study,
which cannot definitively establish causality. As this was an
observational study, although a multifactor analysis was performed,
other confounding factors may still exist. Furthermore, the data
were from the United States, and thus, the results may not apply
fully to ICUs elsewhere with different practices or resources. In
addition, only data from a single BUN/Cr test were available at
admission and repeated measures data were not analysed. Different
blood collection times would also affect the results of BUN/Cr,
which may have resulted in biases in the study results.
Furthermore, the present study did not include clinical follow-up
data and could not predict the long-term outcomes of these patients
with AMI. Finally, data on the use of intra-aortic balloon pump and
left ventricular assist device were not available.
In conclusion, the present findings demonstrated
that the BUN/Cr ratio had a strong association with in-hospital
mortality in patients with non-STEMI, but not in patients with
STEMI. These results may motivate the revision of how the prognosis
of patients with AMI should be predicted. Importantly, these
findings suggest that the BUN/Cr ratio may be a useful risk
stratification factor for critically ill patients with AMI. The
effect of the BUN/Cr ratio on in-hospital mortality should be
recorded and investigated in future prospective studies.
Supplementary Material
Association between BUN/Cr and
in-hospital mortality. BUN, blood urea nitrogen; Cr,
creatinine.
Kaplan-Meier survival curves for
in-hospital mortality among patients with acute myocardial
infarction without heart failure. BUN, blood urea nitrogen; Cr,
creatinine; T, tertile.
Receiver operating characteristic
curves for different indicators to predict in-hospital mortality
for patients with acute myocardial infarction. AUC, area under the
curve; BUN, blood urea nitrogen; Cr, creatinine; cTnI, cardiac
troponin I.
Association between the BUN/Cr ratio
and in hospital mortality in patients with acute myocardial
infarction without heart failure in different models.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the Technology Research and
Development Fund Project of the Changde Science and Technology
Bureau (grant nos. 2019S191, 2018S031 and 2020S025) and The First
People's Hospital of Changde ‘Wings Spreading Program Scientific
Research Fund’ (grant no. 2022ZZ07).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are available from the corresponding author on
reasonable request.
Authors' contributions
SH and LG confirm the authenticity of all the raw
data. SH, LL and XD conceived the study. SH, NG and LL performed
the research. XD, LG, LL, ZZ and QZ analyzed the data. SH, LL and
LG wrote the paper. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The establishment and use of this database was
approved by the Massachusetts Institute of Technology (Cambridge,
MA, USA) and permission was obtained for the original data
collection. The database is released under the Health Insurance
Portability and Accountability Act (HIPAA) safe harbour provision.
The re-identification risk was certified as meeting safe harbour
standards by Privacert (HIPAA certification no. 1031219-2). Since
all protected health information was de-identified, the requirement
for individual patient consent for publication was waived. In
addition, they waived the need for informed consent due to the
retrospective nature of the study. The study was performed in
accordance with the Declaration of Helsinki. All methods were
performed in accordance with the relevant guidelines and
regulations.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Qian H, Tang C and Yan G: Predictive value
of blood urea nitrogen/creatinine ratio in the long-term prognosis
of patients with acute myocardial infarction complicated with acute
heart failure. Medicine (Baltimore). 98(e14845)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ok F, Erdogan O, Durmus E, Carkci S and
Canik A: Predictive values of blood urea nitrogen/creatinine ratio
and other routine blood parameters on disease severity and survival
of COVID-19 patients. J Med Viro. 93:786–793. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Liu J, Sun LL, Wang J and Ji G: Blood urea
nitrogen in the prediction of in-hospital mortality of patients
with acute aortic dissection. Cardiol J. 25:371–376.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Küçükceran K, Ayrancı MK, Girişgin AS,
Koçak S and Dündar ZD: The role of the BUN/albumin ratio in
predicting mortality in COVID-19 patients in the emergency
department. Am J Emerg Med. 48:33–37. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Horiuchi Y, Aoki J, Tanabe K, Nakao K,
Ozaki Y, Kimura K, Ako J, Yasuda S, Noguchi T, Suwa S, et al: A
high level of blood urea nitrogen is a significant predictor for
in-hospital mortality in patients with acute myocardial infarction.
Int Heart J. 59:263–271. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Granger CB, Goldberg RJ, Dabbous O, Pieper
KS, Eagle KA, Cannon CP, Van de Werf F, Avezum A, Goodman SG,
Flather MD, et al: Predictors of hospital mortality in the global
registry of acute coronary events. Arch Intern Med. 163:2345–2353.
2003.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Matsue Y, van der Meer P, Damman K, Metra
M, O'Connor CM, Ponikowski P, Teerlink JR, Cotter G, Davison B,
Cleland JG, et al: Blood urea nitrogen-to-creatinine ratio in the
general population and in patients with acute heart failure. Heart.
103:407–413. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sood MM, Saeed M, Lim V, Cordova F,
Komenda P, Malik A, Rigatto C, Shafer LA, Tangri N, Tappia PS and
Zieroth S: The urea-to-creatinine ratio is predictive of worsening
kidney function in ambulatory heart failure patients. J Card Fail.
21:412–418. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhu X, Cheang I, Liao S, Wang K, Yao W,
Yin T, Lu X, Zhou Y, Zhang H and Li X: Blood urea nitrogen to
creatinine ratio and long-term mortality in patients with acute
heart failure: A prospective cohort study and meta-analysis.
Cardiorenal Med. 10:415–428. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Tanaka S, Ninomiya T, Taniguchi M,
Tokumoto M, Masutani K, Ooboshi H, Kitazono T and Tsuruya K: Impact
of blood urea nitrogen to creatinine ratio on mortality and
morbidity in hemodialysis patients: The Q-cohort study. Sci Rep.
7(14901)2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Schrock JW, Glasenapp M and Drogell K:
Elevated blood urea nitrogen/creatinine ratio is associated with
poor outcome in patients with ischemic stroke. Clin Neurol
Neurosurg. 114:881–884. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Brisco MA, Coca SG, Chen J, Owens AT,
McCauley BD, Kimmel SE and Testani JM: Blood urea
nitrogen/creatinine ratio identifies a high-risk but potentially
reversible form of renal dysfunction in patients with decompensated
heart failure. Circ Heart Fail. 6:233–239. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pollard TJ, Johnson AEW, Raffa JD, Celi
LA, Mark RG and Badawi O: The eICU collaborative research database,
a freely available multi-center database for critical care
research. Sci Data. 5(180178)2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Su D, Li J, Ren J, Gao Y, Li R, Jin X,
Zhang J and Wang G: The relationship between serum lactate
dehydrogenase level and mortality in critically ill patients.
Biomark Med. 15:551–559. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Díaz-Garzón J, Sandoval Y, Smith SW, Love
S, Schulz K, Thordsen SE, Johnson BK, Driver B, Jacoby K, Carlson
MD, et al: Discordance between ICD-coded myocardial infarction and
diagnosis according to the universal definition of myocardial
infarction. Clin Chem. 63:415–419. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Austin PC, White IR, Lee DS and van Buuren
S: Missing data in clinical research: A tutorial on multiple
imputation. Can J Cardiol. 37:1322–1331. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Thygesen K, Alpert JS, Jaffe AS, Chaitman
BR, Bax JJ, Morrow DA and White HD: Executive Group on behalf of
the Joint European Society of Cardiology (ESC)/American College of
Cardiology (ACC)/American Heart Association (AHA)/World Heart
Federation (WHF) Task Force for the Universal Definition of
Myocardial Infarction. Fourth universal definition of myocardial
infarction (2018). Circulation. 138:e618–e651. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Schiele F, Aktaa S, Rossello X, Ahrens I,
Claeys MJ, Collet J, Fox KAA, Gale CP, Huber K, Iakobishvili Z, et
al: 2020 Update of the quality indicators for acute myocardial
infarction: A position paper of the association for acute
cardiovascular care: The study group for quality indicators from
the ACVC and the NSTE-ACS guideline group. Eur Heart J Acute
Cardiovasc Care. 10:224–233. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
McDonagh TA, Metra M, Adamo M, Gardner RS,
Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et
al: 2021 ESC guidelines for the diagnosis and treatment of acute
and chronic heart failure. Eur Heart J. 42:3599–3726.
2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Heidenreich PA, Bozkurt B, Aguilar D,
Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM,
Evers LR, et al: 2022 AHA/ACC/HFSA guideline for the management of
heart failure: A report of the american college of
cardiology/American heart association joint committee on clinical
practice guidelines. Circulation. 145:e895–e1032. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kernan WN, Viscoli CM, Brass LM, Broderick
JP, Brott T, Feldmann E, Morgenstern LB, Wilterdink JL and Horwitz
RI: Phenylpropanolamine and the risk of hemorrhagic stroke. N Engl
J Med. 343:1826–1832. 2000.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Liu S, Wang X, Lu Y, Li T, Gong Z, Sheng
T, Hu B, Peng Z and Sun X: The effects of intraoperative
cryoprecipitate transfusion on acute renal failure following
orthotropic liver transplantation. Hepatol Int. 7:901–909.
2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Deng L, Qiu S, Wang C, Bian H, Wang L, Li
Y, Wu B and Liu M: Effects of the blood urea nitrogen to creatinine
ratio on haemorrhagic transformation in AIS patients with diabetes
mellitus. BMC Neurol. 19(63)2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Thygesen K, Alpert JS, Jaffe AS, Simoons
ML, Chaitman BR and White HD: Joint ESC/ACCF/AHA/WHF Task Force for
the Universal Definition of Myocardial Infarction. Katus HA,
Lindahl B, Morrow DA, et al: Third universal definition of
myocardial infarction. Circulation. 126:2020–2035. 2012.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Morrow DA, Cannon CP, Jesse RL, Newby LK,
Ravkilde J, Storrow AB, Wu A, Christenson RH, Apple FS, Francis GS
and Tang W: National academy of clinical biochemistry laboratory
medicine practice guidelines: Clinical characteristics and
utilization of biochemical markers in acute coronary syndromes.
Clin Chem. 115:552–574. 2007.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Shah ASV, Anand A, Strachan FE, Ferry AV,
Lee KK, Chapman AR, Sandeman D, Stables CL, Adamson PD, Andrews
JPM, et al: High-sensitivity troponin in the evaluation of patients
with suspected acute coronary syndrome: A stepped-wedge,
cluster-randomised controlled trial. Lancet. 392:919–928.
2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chin CWL, Shah ASV, McAllister DA, Joanna
Cowell S, Alam S, Langrish JP, Strachan FE, Hunter AL, Maria Choy
A, Lang CC, et al: High-sensitivity troponin I concentrations are a
marker of an advanced hypertrophic response and adverse outcomes in
patients with aortic stenosis. Eur Heart J. 35:2312–2321.
2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shah ASV, McAllister DA, Mills R, Lee KK,
Churchhouse AM, Fleming KM, Layden E, Anand A, Fersia O, Joshi NV,
et al: Sensitive troponin assay and the classification of
myocardial infarction. Am J Med. 128:493–501.e3. 2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Feldman DN, Minutello RM, Bergman G,
Moussa I and Wong SC: Relation of troponin I levels following
nonemergent percutaneous coronary intervention to short- and
long-term outcomes. Am J Cardiol. 104:1210–1215. 2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kimura K, Morita H, Daimon M, Horio M,
Kawata T, Nakao T, Hirokawa M, Kitao R, Watanabe D, Komori T, et
al: Utility of cystatin C for estimating glomerular filtration rate
in patients with muscular dystrophy. Int Heart J. 57:386–388.
2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Han D, Zhang L, Zheng S, Xu F, Li C, Yang
R, Ma W, Yin H and Lyu J: Prognostic value of blood urea
nitrogen/creatinine ratio for septic shock: An analysis of the
MIMIC-III clinical database. Biomed Res Int.
2021(5595042)2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Núñez J, Miñana G, Santas E and
Bertomeu-González V: Cardiorenal syndrome in acute heart failure:
Revisiting paradigms. Rev Esp Cardiol (Engl Ed). 68:426–435.
2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Otto CM: Heartbeat:Blood urea nitrogen to
creatinine ratio predicts outcome in acute heart failure. Heart.
103:399–401. 2017.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Brisco MA, Zile MR, Ter Maaten JM, Hanberg
JS, Wilson FP, Parikh C and Testani JM: The risk of death
associated with proteinuria in heart failure is restricted to
patients with an elevated blood urea nitrogen to creatinine ratio.
Int J Cardiol. 215:521–526. 2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Uchino S, Bellomo R and Goldsmith D: The
meaning of the blood urea nitrogen/creatinine ratio in acute kidney
injury. Clin Kidney J. 5:187–191. 2012.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Parrinello G, Torres D, Testani JM,
Almasio PL, Bellanca M, Pizzo G, Cuttitta F, Pinto A, Butler J and
Paterna S: Blood urea nitrogen to creatinine ratio is associated
with congestion and mortality in heart failure patients with renal
dysfunction. Intern Emerg Med. 10:965–972. 2015.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Murata A, Kasai T, Matsue Y, Matsumoto H,
Yatsu S, Kato T, Suda S, Hiki M, Takagi A and Daida H: Relationship
between blood urea nitrogen-to-creatinine ratio at hospital
admission and long-term mortality in patients with acute
decompensated heart failure. Heart Vessels. 33:877–885.
2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Núñez J: Blood urea nitrogen to creatinine
ratio in acute heart failure: An old concept brought to reality?
Heart. 103:402–403. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Khera R, Haimovich J, Hurley NC, McNamara
R, Spertus JA, Desai N, Rumsfeld JS, Masoudi FA, Huang C, Normand
SL, et al: Use of machine learning models to predict death after
acute myocardial infarction. JAMA Cardiol. 6:633–641.
2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Steg PG, Goldberg RJ, Gore JM, Fox KA,
Eagle KA, Flather MD, Sadiq I, Kasper R, Rushton-Mellor SK and
Anderson FA: GRACE Investigators. Baseline characteristics,
management practices, and in-hospital outcomes of patients
hospitalized with acute coronary syndromes in the global registry
of acute coronary events (GRACE). Am J Cardiol. 90:358–363.
2002.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Puymirat E, Simon T, Cayla G, Cottin Y,
Elbaz M, Coste P, Lemesle G, Motreff P, Popovic B, Khalife K, et
al: Acute myocardial infarction: Changes in patient
characteristics, management, and 6-month outcomes over a period of
20 years in the FAST-MI program (French registry of acute
ST-elevation or non-ST-elevation myocardial infarction) 1995 to
2015. Circulation. 136:1908–1919. 2017.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Schefold JC, Lainscak M, Hodoscek LM,
Blöchlinger S, Doehner W and von Haehling S: Single baseline serum
creatinine measurements predict mortality in critically ill
patients hospitalized for acute heart failure. ESC Heart Fail.
2:122–128. 2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Ibanez B, James S, Agewall S, Antunes MJ,
Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA,
Halvorsen S, et al: 2017 ESC guidelines for the management of acute
myocardial infarction in patients presenting with ST-segment
elevation: The task force for the management of acute myocardial
infarction in patients presenting with ST-segment elevation of the
European society of cardiology (ESC). Eur Heart J. 39:119–177.
2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Chew DP, Scott IA, Cullen L, French JK,
Briffa TG, Tideman PA, Woodruffe S, Kerr A, Branagan M and Aylward
PEG: NHFA/CSANZ ACS Guideline 2016 Executive Working Group:
National heart foundation of australia & cardiac society of
Australia and New Zealand: Australian clinical guidelines for the
management of acute coronary syndromes 2016. Heart Lung Circ.
25:895–951. 2016.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Borghi C, Omboni S, Reggiardo G, Bacchelli
S, Esposti DD and Ambrosioni E: SMILE Working Project. Effects of
the concomitant administration of xanthine oxidase inhibitors with
zofenopril or other ACE-inhibitors in post-myocardial infarction
patients: A meta-analysis of individual data of four randomized,
double-blind, prospective studies. BMC Cardiovasc Disord.
18(112)2018.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Giannitsis E, Blankenberg S, Christenson
RH, Frey N, von Haehling S, Hamm CW, Inoue K, Katus HA, Lee CC,
McCord J, et al: Critical appraisal of the 2020 ESC guideline
recommendations on diagnosis and risk assessment in patients with
suspected non-ST-segment elevation acute coronary syndrome. Clin
Res Cardiol. 110:1353–1368. 2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Sato T, Saito Y, Matsumoto T, Yamashita D,
Saito K, Wakabayashi S, Kitahara H, Sano K and Kobayashi Y: Impact
of CADILLAC and GRACE risk scores on short- and long-term clinical
outcomes in patients with acute myocardial infarction. J Cardiol.
78:201–205. 2021.PubMed/NCBI View Article : Google Scholar
|