Introduction
Optic nerve sheath meningiomas (ONSMs) are rare
tumors that constitute 1-2% of all meningiomas and ~2% of all
orbital tumors (1,2). ONSMs involve the optic nerve and
extend to intracranial. In ONSMs having both an intraorbital and
intracranial segment, clinical management to preserve visual
function of optic apparatus adjacent to intracranial tumor may be
challenging. Although meningioma is a benign tumor, it tends to be
more aggressive during pregnancy. This is likely the result of
tumor response to pregnancy-circulating hormones and homodynamic
changes (3-7).
We report a patient with right visual impairment
during two pregnancies, who was ultimately diagnosed with ONSM with
positive immunostaining for progesterone receptor (PR). This study
provides clinical features of ONSM associated with pregnancy. As
ONSMs are originally slow-growing benign tumor, treatment strategy,
combination of resection and advanced radiotherapy, based on
long-term perspective seems to be necessary to prevent further
spreading of the tumor not only to contralateral optic nerve but
also to other intracranial structures involved in visual
function.
Case report
A 41-year-old woman felt visual impairment in the
right eye, late in her first pregnancy. After the delivery, she
received an ophthalmic examination and both visual acuity and field
were normal. After 2 years, during late pregnancy with her second
child, she became aware of slowly progressive visual deterioration
in the right eye again. Two months after the second delivery,
fundus examination showed swelling of the right optic disc. She was
diagnosed with optic neuritis and received steroid pulse therapy.
After 1 year, swelling of the right optic disc and right visual
impairment had progressed. Her right eye's visual field was
impaired, and she had developed lateral lower quadrantanopia.
Furthermore, her right visual acuity worsened from 20/20 to 20/200
corrected visual acuity over the course of 1 year. She was admitted
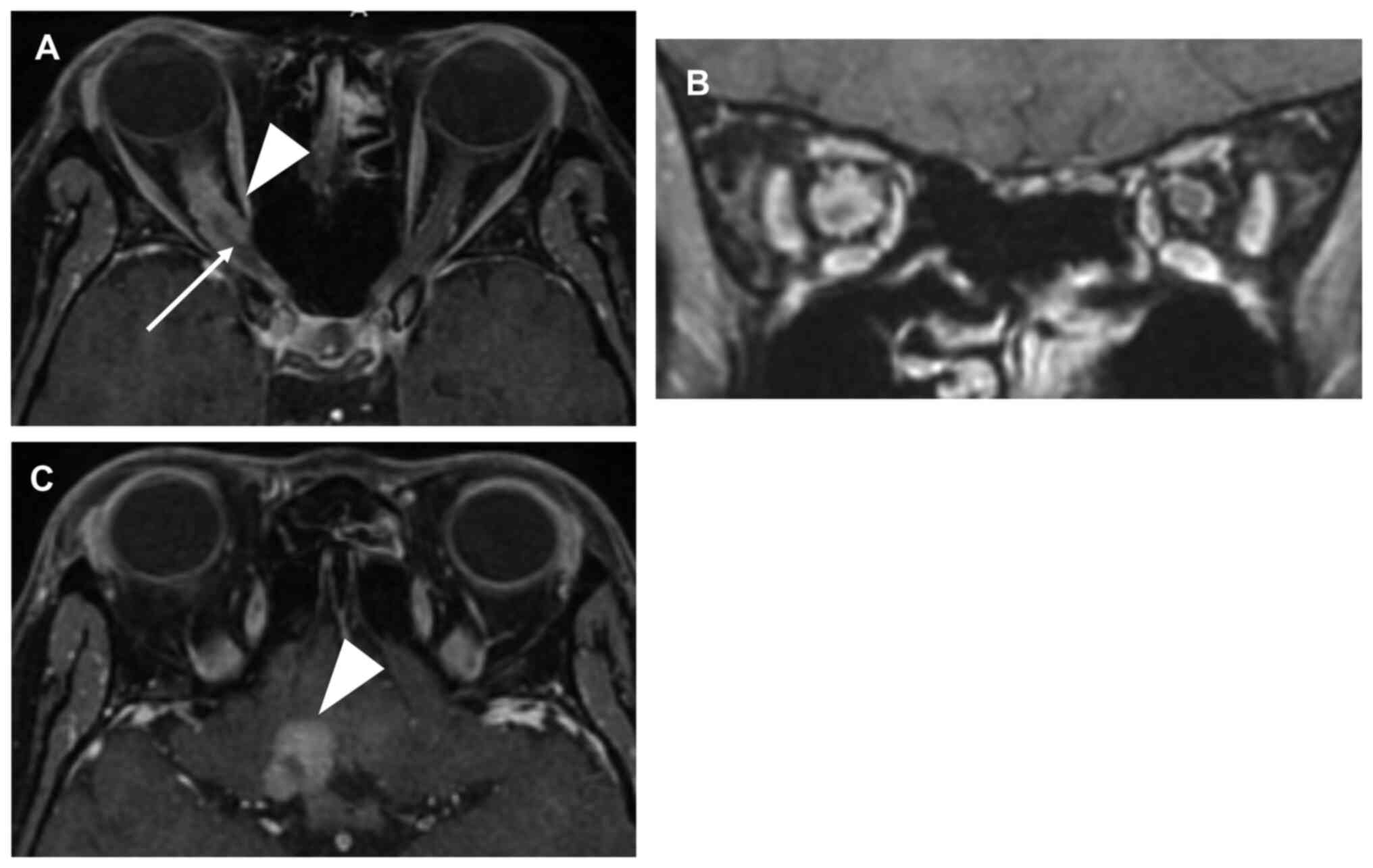
at our hospital and underwent magnetic resonance imaging (MRI). MRI
revealed an intraconal tumor encasing the right optic nerve
(Fig. 1A and B). The tumor extended through the optic
canal to the right carotid artery and close to the optic chiasm
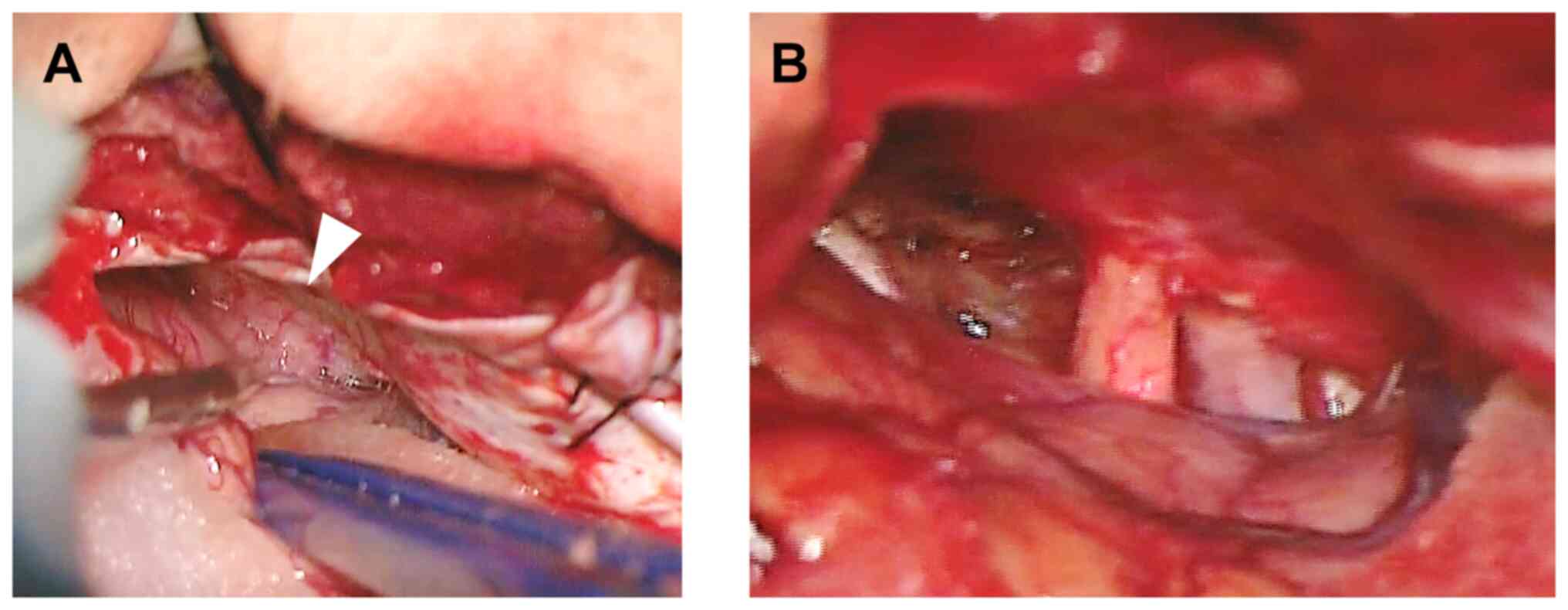
(Figs. 1C and 2A). Surgical resection of the
intracranial extension of the tumor was performed to prevent tumor
invasion of the left optic nerve and the optic chiasm (Fig. 2B). After resection, the bilateral
optic nerves were confirmed to be intact. The dura of the frontal
base was coagulated and incised using a low-power bipolar system
and micro dissection needle to prevent tumor invasion of the left
optic nerve along the dura matter. The intraconal portion of the
tumor encasing the right optic nerve was not resected to prevent
compromising visual function. After intracranial tumor resection,
her visual acuity maintained the presurgical value of 20/200
corrected visual acuity. The pathological findings suggested
angiomatous meningioma, WHO Grade 1 with positive immunostaining
for PR and negative for estrogen receptor (ER). Seven months after
operation, her visual function did not deteriorate. MRI revealed no
tumor size change during the 7-month observative follow-up period.
There is a possibility that tumor size may be stable due to reduced
influence of progesterone after delivery. We have planned adding
high-precision radiotherapy when the tumor grows to achieve our
goals of tumor control and preservation of visual function.
Discussion
ONSMs are rare and slow-growing benign tumors.
Meningiomas may grow during pregnancy because of hormone receptor
expression and homodynamic changes (3-7).
Progesterone is thought to be a significant factor for meningioma
growth during pregnancy. It has been shown that meningioma growth
is enhanced in the progesterone-dominated luteal phase of the
menstrual cycle (8). Sex steroid
of a meningioma was associated with pregnancy, and showed
significant expression of PR; whereas no significant expression of
ER was observed (9). Surgery after
pregnancy was found to be more frequent in patients with PR
positive meningioma (3). Our
patient presented with transient visual impairment during her first
pregnancy, resolved after delivery, which reoccurred and gradually
worsened with the second pregnancy. PR positive meningioma appears
to be exacerbated by hormones circulating during pregnancy.
However, it is controversial whether the growth of meningiomas
during pregnancy is only due to the expression of PR. A study of
the pathology of meningiomas during pregnancy found that the
frequency of PR positivity during pregnancy was similar with the
control group (6,10). Meningioma growth during pregnancy
have the possibility to be affected by not only hormone receptor
expression but also tumor location (6,11).
Tumors adjacent to the optic apparatus may cause visual impairment
during pregnancy. Pituitary adenoma, meningioma in skull base, and
orbital schwannoma showed tumor growth and presented with visual
impairment during pregnancy (11-15).
In our case, the right optic nerve was encased by intraconal tumor
and seemed to be vulnerable to visual impairment for tumor growth.
On the other hand, in a few meningioma cases, symptoms subside and
tumor size regresses after delivery (4,16,17).
In our case, visual function and tumor size did not change during
the 7-month observative follow-up period after delivery. We have
planned adding high-precision radiotherapy when the tumor
grows.
The primary treatment is complicated by the need to
balance tumor curability and preservation of visual function.
Conservative management is usually advocated when there is no
significant visual dysfunction or progression of visual loss
(18). Total resection is strongly
associated with visual impairment because of pial vascular plexus
damage, as well as incomplete resection of the tumor with local
recurrence (1,19). As surgical intervention for ONSM
has technical difficulty and postoperative deterioration of visual
function, surgery for ONSM has largely been disregarded in favor of
radiotherapy (20). Surgery is
recommended for intracranial tumor extension that could cause loss
of vision in the contralateral eye (1,18,19).
In our case, the patient's right visual function gradually worsened
during pregnancy but was still preserved. Our treatment goal was to
not exacerbate right visual impairment and to preserve left visual
function. Therefore, we not only resected the intracranial tumor
segment, but also coagulated and incised the frontal base dura to
prevent tumor invasion of the contralateral optic nerve.
Conventional radiotherapy has been widely used for
ONSMs (21). Radiotherapy for
ONSMs has the potential for late toxicity of the optic nerve and
adjacent tissues, such as the optic chiasm, if included in the
irradiation field. Recently intensity-modulated radiation therapy
(IMRT) and stereotactic radiosurgery can result in significant
visual improvements in selected cases, especially in cases with
preservation of vision (22-24).
In our case, the tumor had extended intracranially, close to the
optic chiasm. Thus, surgery combined with new radiation modalities
such as IMRT and stereotactic radiosurgery can be effective to
avoid late radiotherapy toxicity of the optic nerve and the optic
chiasm. In order to preserve contralateral visual function, our
treatment plan involved resecting the portion of the tumor close to
the optic chiasm and excluding the optic chiasm from the
irradiation field. As ONSMs are originally slow-growing benign
tumor, a careful treatment strategy based on long-term perspective,
combining surgical resection and targeted radiotherapy, was
necessary to prevent further spread of the tumor to the
contralateral optic nerve and other intracranial structures.
In conclusion, this report describes a patient with
ONSM who presented with progressive visual impairment during two
pregnancies. ONSMs should be considered in cases of visual
impairment that develop during pregnancy. Although ONSMs are
typically slow-growing benign tumors, the treatment strategy should
be based on preventing further spread of the tumor and preserving
contralateral visual function. In ONSM patients who developed
visual impairment, surgery may serve as an important but restricted
adjuvant to radiotherapy.
Acknowledgements
Not applicable.
Funding
Funding: This work was supported by JST (grant no.
JPMJPF2009).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YO conceived and designed the study. RU acquired the
data. RU, YO, NK and HK analyzed and interpreted the data and
drafted the manuscript. YO and HK confirm the authenticity of all
the raw data. All authors critically revised the manuscript for
important intellectual content. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was conducted according to the guidelines
of the Declaration of Helsinki and approved by the Ethics Committee
of Osaka University Hospital. Written informed consent was obtained
from the patient.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of the data and images in this case
report.
Competing interest
The authors declare that they have no competing
interests.
References
|
1
|
Dutton JJ: Optic nerve sheath meningiomas.
Surv Ophthalmol. 37:167–183. 1992.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Parker RT, Ovens CA, Fraser CL and
Samarawickrama C: Optic nerve sheath meningiomas: Prevalence,
impact, and management strategies. Eye Brain. 10:85–99.
2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Carbone L, Somma T, Iorio GG, Vitulli F,
Conforti A, Raffone A, Bove I, Pagano S, Pontillo M, Carbone IF, et
al: Meningioma during pregnancy: What can influence the management?
A case series and review of the literature. J Matern Fetal Neonatal
Med. 35:8767–8777. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chakravarthy V, Kaplan B, Gospodarev V,
Myers H, De Los Reyes K and Achiriloaie A: Houdini tumor: Case
report and literature review of pregnancy-associated meningioma.
World Neurosurg. 114:e1261–e1265. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Iplikcioglu AC, Hatiboglu MA, Ozek E and
Ozcan D: Is progesteron receptor status really a prognostic factor
for intracranial meningiomas? Clin Neurol Neurosurg. 124:119–122.
2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lusis EA, Scheithauer BW, Yachnis AT,
Fischer BR, Chicoine MR, Paulus W and Perry A: Meningiomas in
pregnancy: A clinicopathologic study of 17 cases. Neurosurgery.
71:951–961. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pravdenkova S, Al-Mefty O, Sawyer J and
Husain M: Progesterone and estrogen receptors: Opposing prognostic
indicators in meningiomas. J Neurosurg. 105:163–173.
2006.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hatiboglu MA, Cosar M, Iplikcioglu AC and
Ozcan D: Sex steroid and epidermal growth factor profile of giant
meningiomas associated with pregnancy. Surg Neurol. 69:356–362;
discussion 362-3. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Smith JS, Quinones-Hinojosa A,
Harmon-Smith M, Bollen AW and McDermott MW: Sex steroid and growth
factor profile of a meningioma associated with pregnancy. Can J
Neurol Sci. 32:122–127. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Giraldi L, Lauridsen EK, Maier AD, Hansen
JV, Broholm H, Fugleholm K, Scheie D and Munch TN: Pathologic
characteristics of pregnancy-related meningiomas. Cancers (Basel).
13(3879)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Nossek E, Ekstein M, Barkay G, Shahar T,
Gonen L, Rimon E, Kesler A and Margalit N: Visual deterioration
during pregnancy due to skull base tumors compressing the optic
apparatus. Neurosurg Rev. 38:473–479; discussion 479.
2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hannon AM, Frizelle I, Kaar G, Hunter SJ,
Sherlock M, Thompson CJ and O'Halloran DJ: Irish Pituitary Database
Group. Octreotide use for rescue of vision in a pregnant patient
with acromegaly. Endocrinol Diabetes Metab Case Rep. 2019:19–0019.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Johnson N, Sermer M, Lausman A and Maxwell
C: Obstetric outcomes of women with intracranial neoplasms. Int J
Gynaecol Obstet. 105:56–59. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Moscovici S, Fraifeld S, Cohen JE, Dotan
S, Elchalal U, Shoshan Y and Spektor S: Parasellar meningiomas in
pregnancy: Surgical results and visual outcomes. World Neurosurg.
82:e503–e512. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sugo N, Yokota K, Nemoto M, Hatori T, Kano
T, Goto S and Seiki Y: Accelerated growth of an orbital schwannoma
during pregnancy. J Neuroophthalmol. 27:45–47. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chacko JG, Miller JL and Angtuaco EJ:
Spontaneous postpartum resolution of vision loss caused by a
progesterone receptor-positive tuberculum sellae meningioma. J
Neuroophthalmol. 30:132–134. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kerschbaumer J, Freyschlag CF, Stockhammer
G, Taucher S, Maier H, Thomé C and Seiz-Rosenhagen M:
Hormone-dependent shrinkage of a sphenoid wing meningioma after
pregnancy: Case report. J Neurosurg. 124:137–140. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Miller NR: New concepts in the diagnosis
and management of optic nerve sheath meningioma. J Neuroophthalmol.
26:200–208. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Douglas VP, Douglas KAA and Cestari DM:
Optic nerve sheath meningioma. Curr Opin Ophthalmol. 31:455–461.
2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Turbin RE, Wladis EJ, Frohman LP, Langer
PD and Kennerdell JS: Role for surgery as adjuvant therapy in optic
nerve sheath meningioma. Ophthalmic Plast Reconstr Surg.
22:278–282. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Turbin RE, Thompson CR, Kennerdell JS,
Cockerham KP and Kupersmith MJ: A long-term visual outcome
comparison in patients with optic nerve sheath meningioma managed
with observation, surgery, radiotherapy, or surgery and
radiotherapy. Ophthalmology. 109:890–899; discussion 899-900.
2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Inoue T, Mimura O, Ikenaga K, Okuno Y and
Nishiguchi I: The rapid improvement in visual field defect observed
with weekly perimetry during intensity-modulated radiotherapy for
optic nerve sheath meningioma. Int Cancer Conf J. 8:136–140.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Liu D, Xu D, Zhang Z, Zhang Y, Li Y, Liu
X, Jia Q, Zheng L and Song G: Long-term results of Gamma Knife
surgery for optic nerve sheath meningioma. J Neurosurg. 113
(Suppl):S28–S33. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sasano H, Shikishima K, Aoki M, Sakai T,
Tsutsumi Y and Nakano T: Efficacy of intensity-modulated radiation
therapy for optic nerve sheath meningioma. Graefes Arch Clin Exp
Ophthalmol. 257:2297–2306. 2019.PubMed/NCBI View Article : Google Scholar
|