Introduction
Odontogenic keratocysts (OKCs) account for 11.7% of
all jaw cysts worldwide, making them the third most common type of
cyst in the jaws after radicular and dentigerous cysts (1). OKCs are characterized by aggressive
behavior and have a relatively high recurrence rate (2). Similar to other entities with an
odontogenic origin, OKCs originate in tooth-bearing regions, and
they occur twice as often in the mandible as in the maxilla
(3). When OKCs originate in the
mandible, the most common location is the posterior sextant, the
angle or the ramus (4,5). Cases of OKCs often progress to the
condyle because of their aggressive nature (6,7);
however, to the best of our knowledge, only two reports of OKCs in
the condyloid process that are not continuous with the surrounding
areas have been reported (8,9). In
both cases, OKCs occurred in the condylar head, which was resected.
The present study reports on the case of an OKC that occurred
discretely in the base of the condyle, which was treated
successfully to preserve the condylar process.
Case report
Patient information
A 31-year-old man was referred to the University of
the Ryukyus Hospital (Nishihara, Japan) in November 2020 with a
complaint of repeated inflammatory symptoms around the condylar
process. Cysts were first detected from the right mandibular body
to the base of the condyle when the patient visited a dental clinic
for scaling in January 2019. The patient was referred to another
hospital, where a cystectomy and wisdom tooth extraction were
performed in March 2019; however, the cyst at the base of the
condyle was rediscovered. In January 2020, inflammatory symptoms
around the condylar process appeared. The patient was then referred
to the University of the Ryukyus Hospital. The patient had used
antibiotics repeatedly and for an extended period at the time of
his first visit to the University of the Ryukyus Hospital. The
patient had no medical history and no family history of congenital
anomalies. The patient had a smoking habit (one pack a day for 12
years) and he denied having any allergies. A general physical
examination revealed normal physical and nutritional status.
Investigations
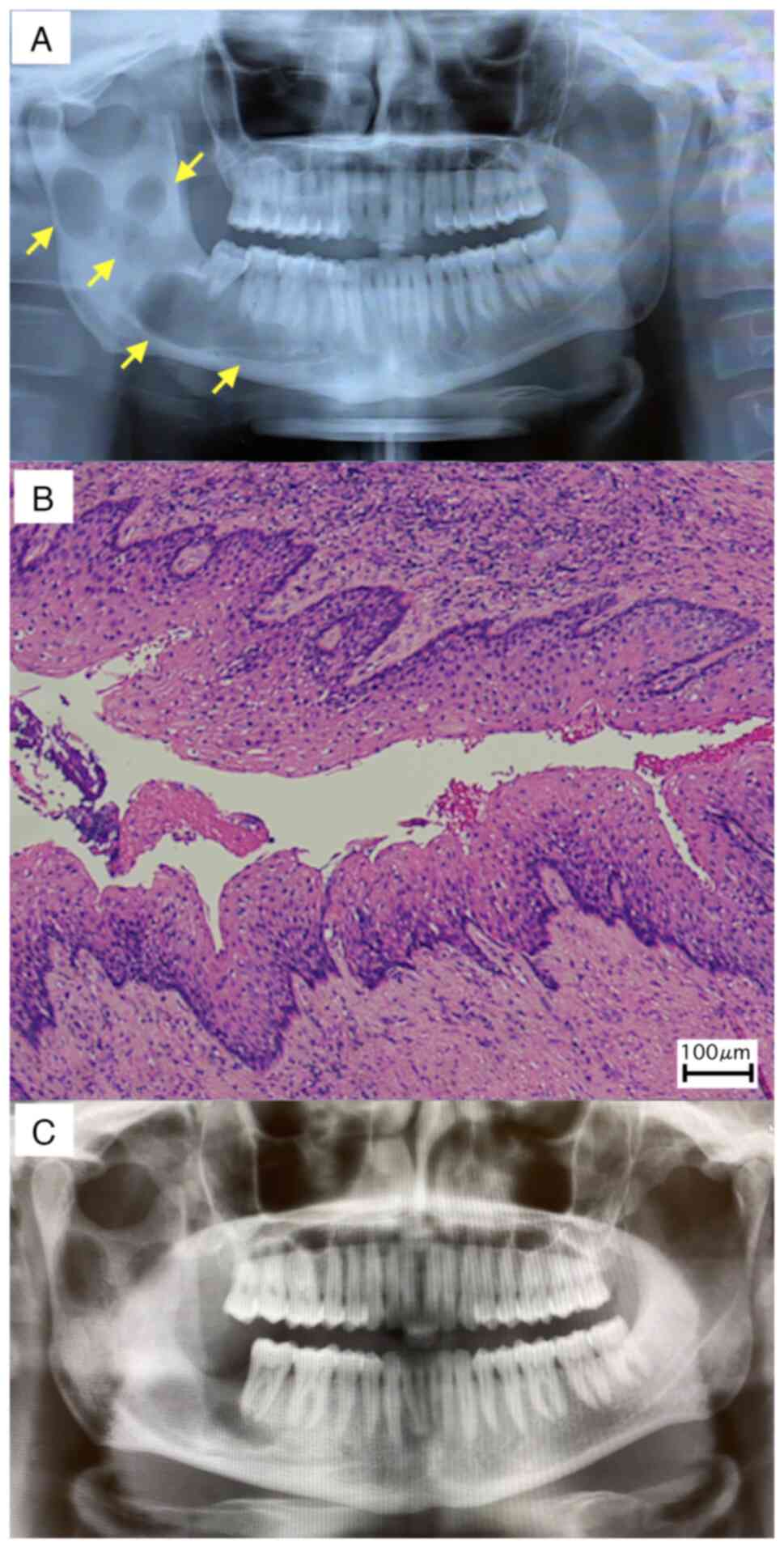
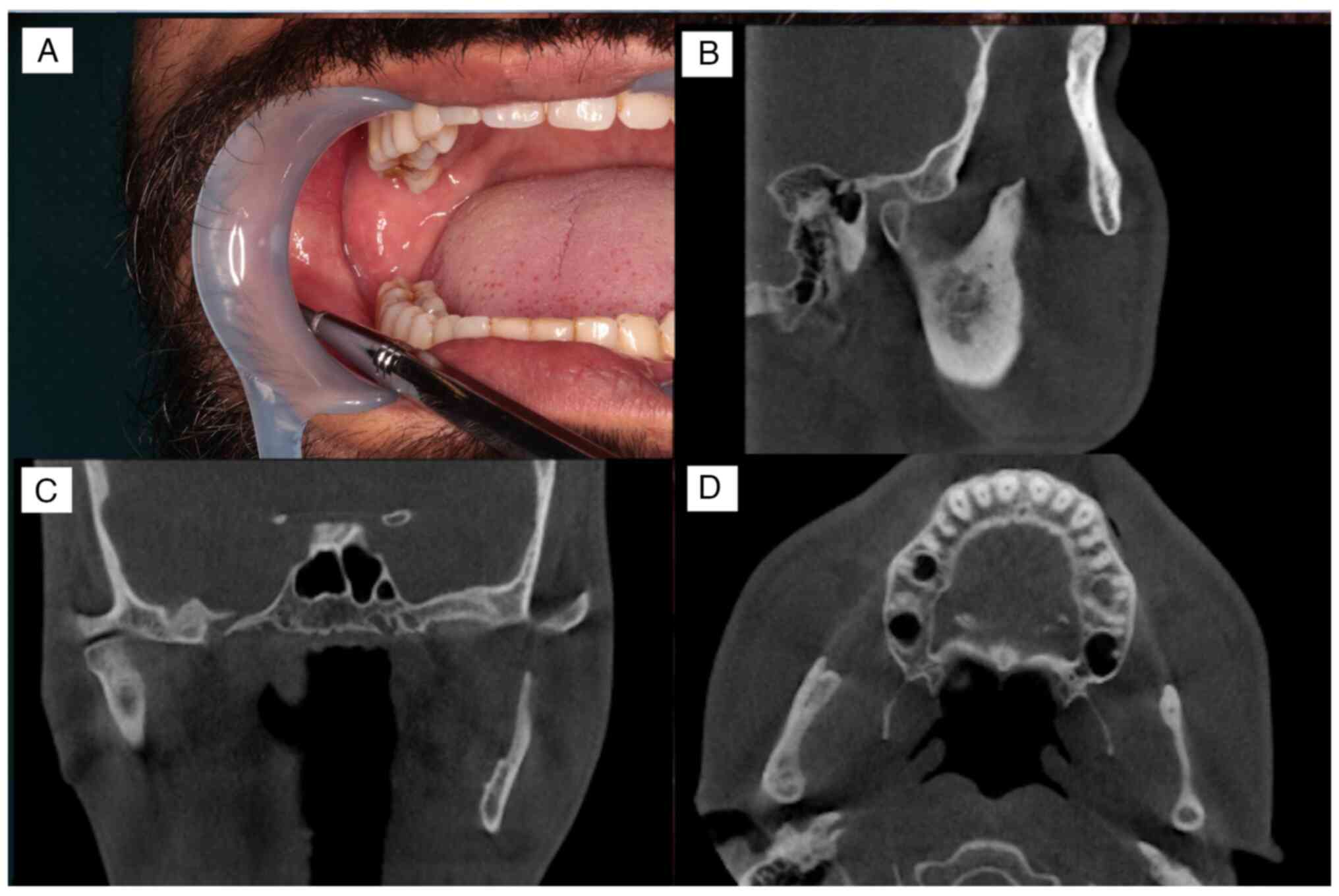
On the first visit to the referral hospital, a
panoramic radiographic examination revealed a multivesicular cyst
formation extending from the right mandibular body to the base of
the condyle (Fig. 1A).
The histopathological result of the cyst excised
during surgery was OKC (Fig. 1B).
Furthermore, the postoperative panoramic radiographic examination
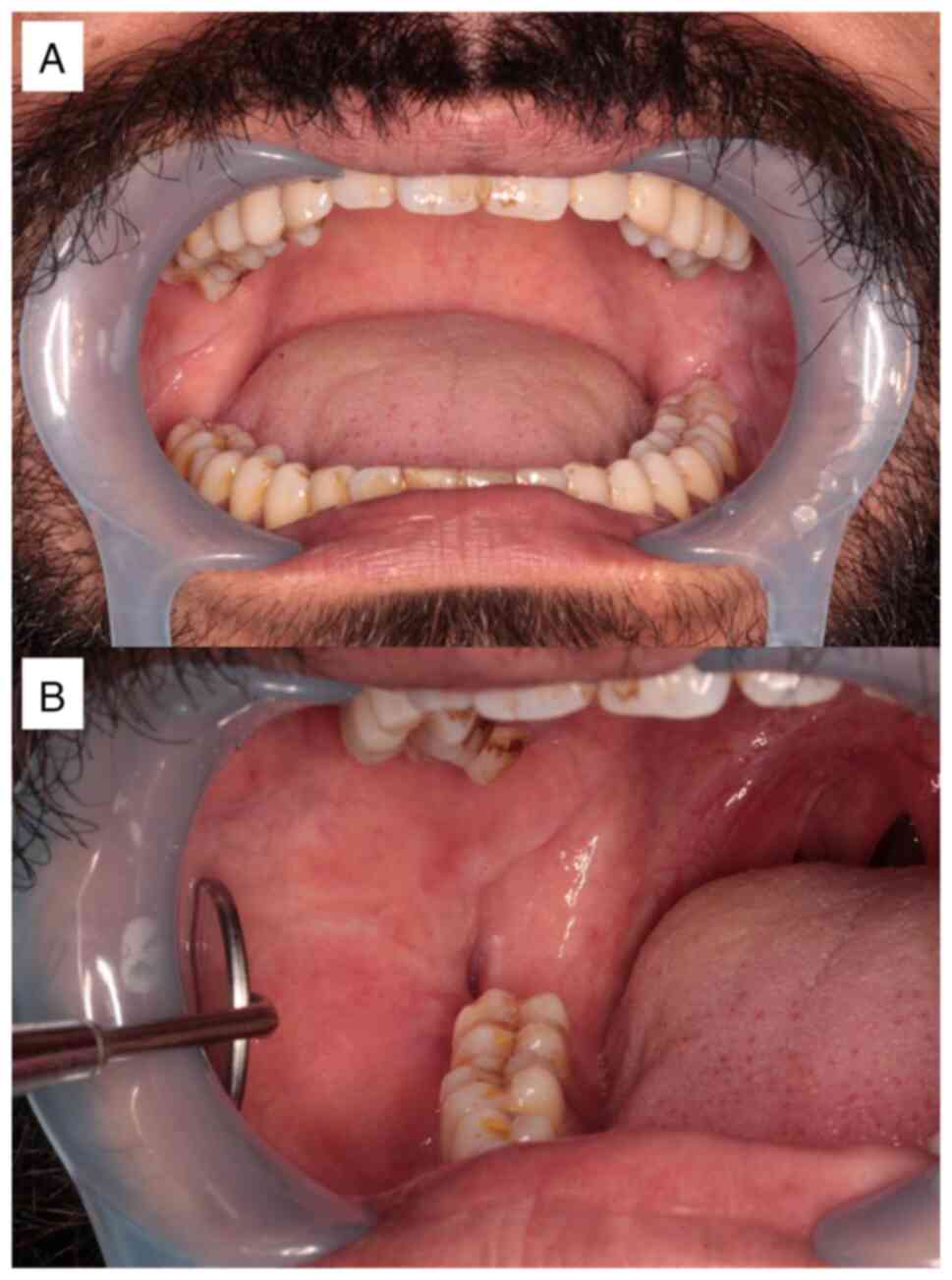
showed that all cysts were removed (Fig. 1C). At the time of their first visit
to the University of the Ryukyus Hospital, an intraoral examination
showed that the buccal gingiva corresponding to the lower right
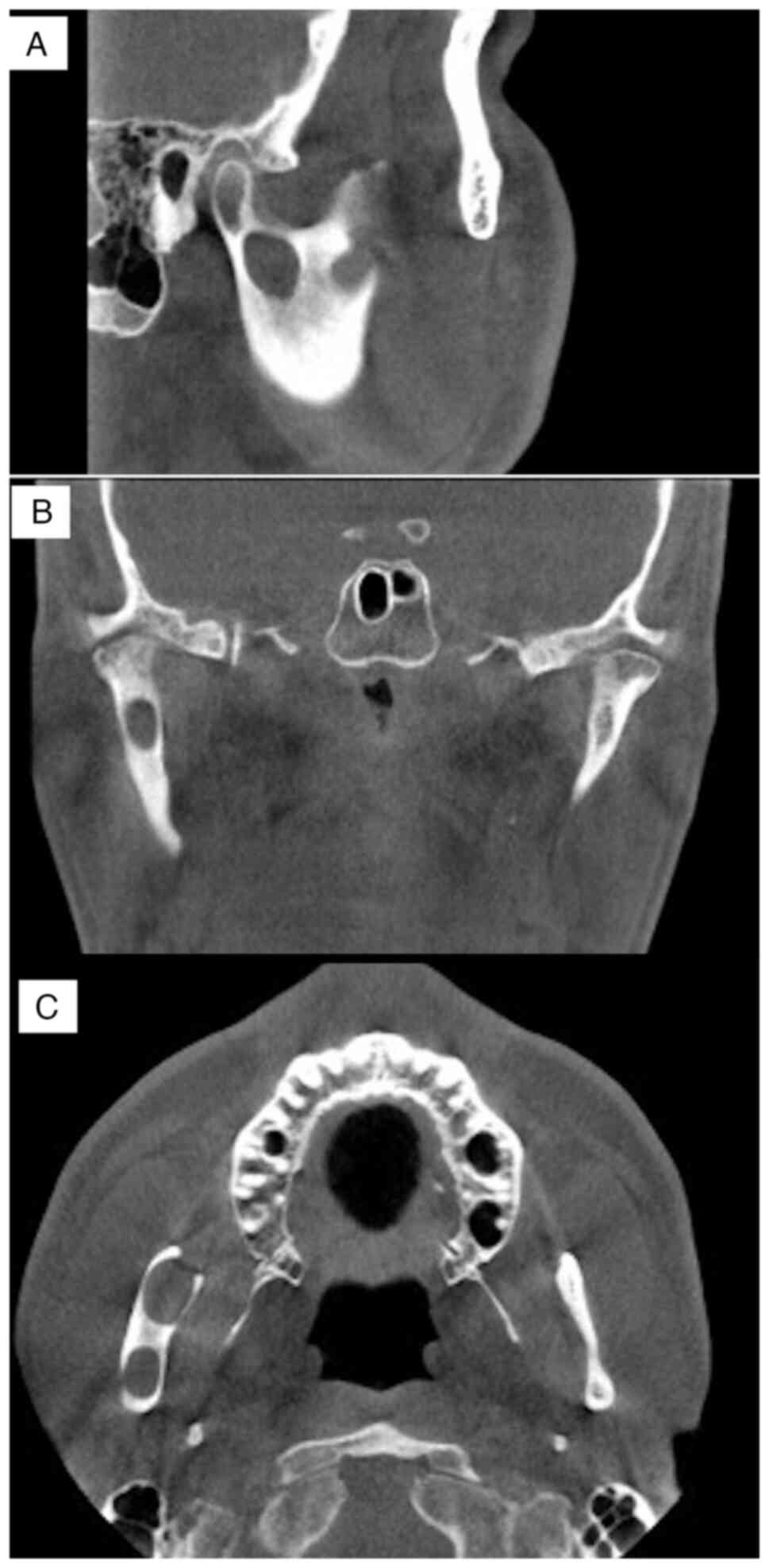
wisdom tooth was depressed owing to previous surgery (Fig. 2A and B). Panoramic radiographic examination
showed an isolated cyst-like transmission in the base of the
condyle and the anterior margin of the right mandibular ramus
(Fig. 3). Cone-beam computed
tomography examination disclosed a cyst-like transmission image
measuring 13x12x6 mm in the base of the condyle. A suspected
residual cyst was detected in the anterior margin of the right
mandibular ramus. The cysts were not connected and both were not in
contact with the inferior alveolar nerve (Fig. 4A-C). The long-term, continuous use
of antibiotics was terminated because no inflammatory symptoms were
observed. Although the patient was scheduled to undergo surgery in
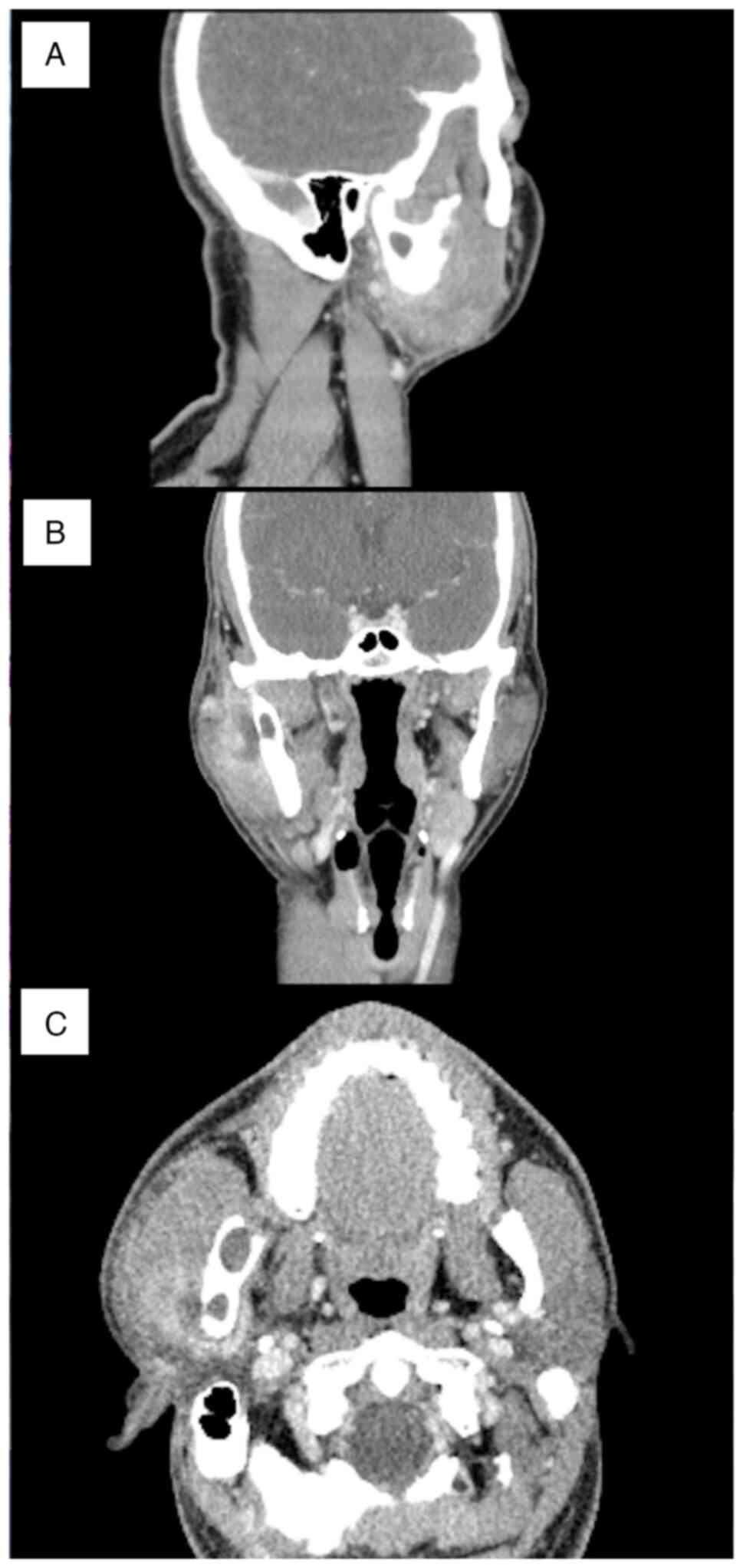
the General Anesthesia Department, symptoms of swelling and pain
occurred around the condylar process in December 2020. A contrast
computed tomography examination showed the formation of an abscess
at the cyst at the base of the condyle. Swelling of the surrounding
tissues, including the parotid gland, was also observed (Fig. 5A-C). Anti-inflammatory treatment
included incision, drainage and antibiotics.
Treatment and follow-up
In January 2021, the patient underwent surgery under
general anesthesia. The packed open technique (10,11)
was selected to preserve the condyle process. To avoid damaging the
mandibular nerve as it entered the mandibular foramen before
approaching the cyst, the lingual side of the mandible was
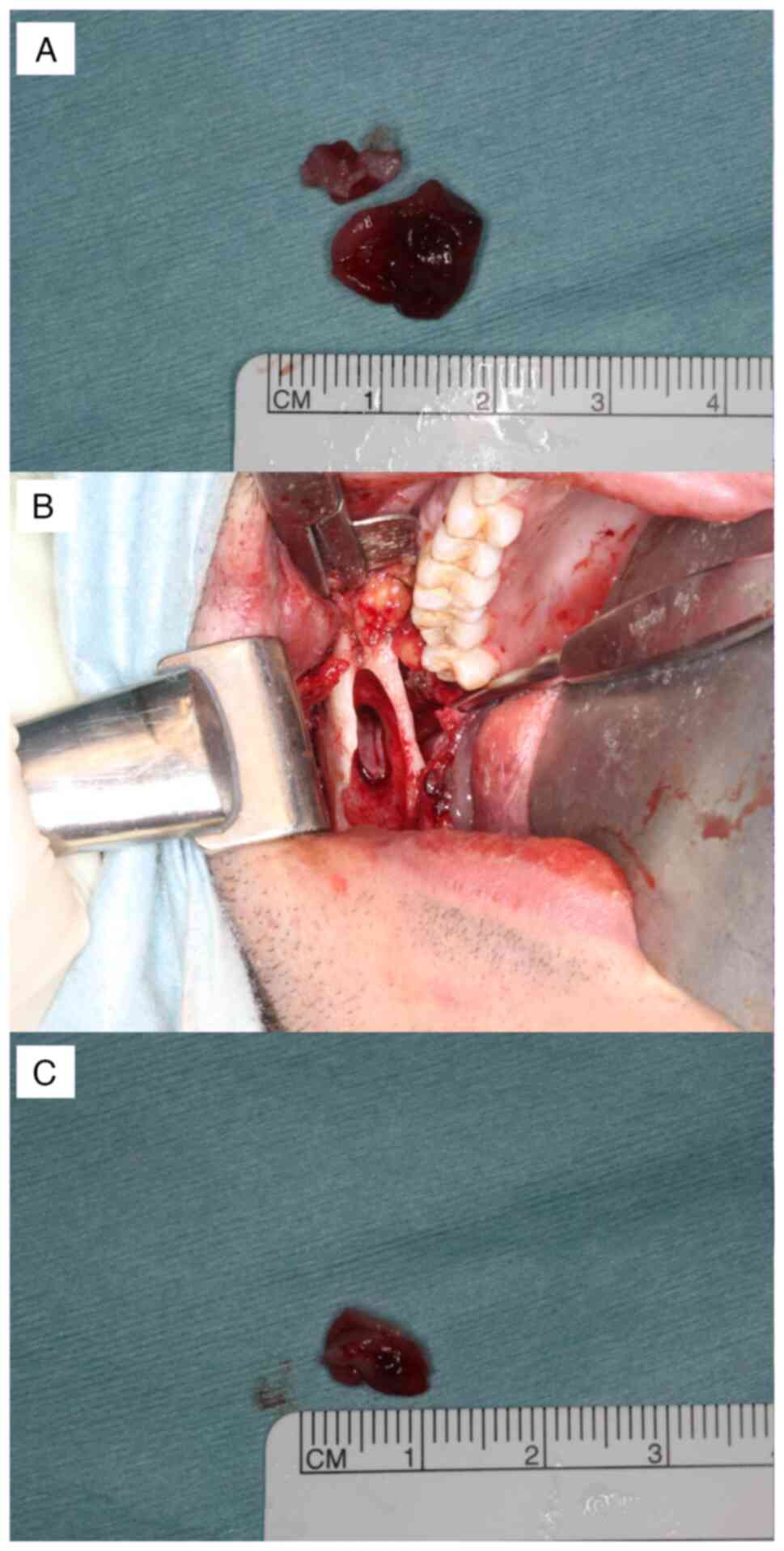
carefully detached. First, the anterior cyst left behind from the
anterior margin of the mandibular ramus was removed (Fig. 6A). After removing the anterior
cyst, an osteotomy was performed at the height between the
mandibular notch and the mandibular foramen. Care was taken to
protect the buccal and lingual sides of the base of the condyle and
to ensure that only the bone was scraped and the burs did not
penetrate to prevent damage to the jaw artery around the mandibular
head. An ultrasonic bone scalpel was used as needed. The posterior
cyst was confirmed and excised (Fig.
6B and C) after further
grinding of the surrounding bone to remove the daughter cyst, which
caused OKC recurrence. The method of enucleation was chosen
followed by open packing. Because the open cavity width was so
small, it might close prematurely, creating a dead space. The oral
mucosa and bone were sutured with absorbent thread. To reduce pain
when changing the packing gauze, a bovine collagen sheet
(TERUDERMIS®, Terumo Co., Ltd.) was attached to the cyst
cavity and tetracycline hydrochloride ointment gauze was inserted.
Hospitalization was managed with attention paid to postoperative
fractures as the bone at the articular process was thinned. After
surgery, the patient followed an oral liquid diet for 6 days.
During hospitalization, the patient's mouth opening was restricted,
with only a minimum opening allowed when eating or brushing teeth.
A total of 7 days after surgery, the tetracycline hydrochloride
ointment gauze was replaced and the thread was removed. The patient
was discharged 14 days after surgery owing to good progress. From
February to May 2021, an obturator was attached to prevent the
cavity from closing. A total of 20 months post-operation, the
patient showed no signs of local recurrence (Fig. 7A-D). In addition, there was no
reappearance of inflammation after surgery.
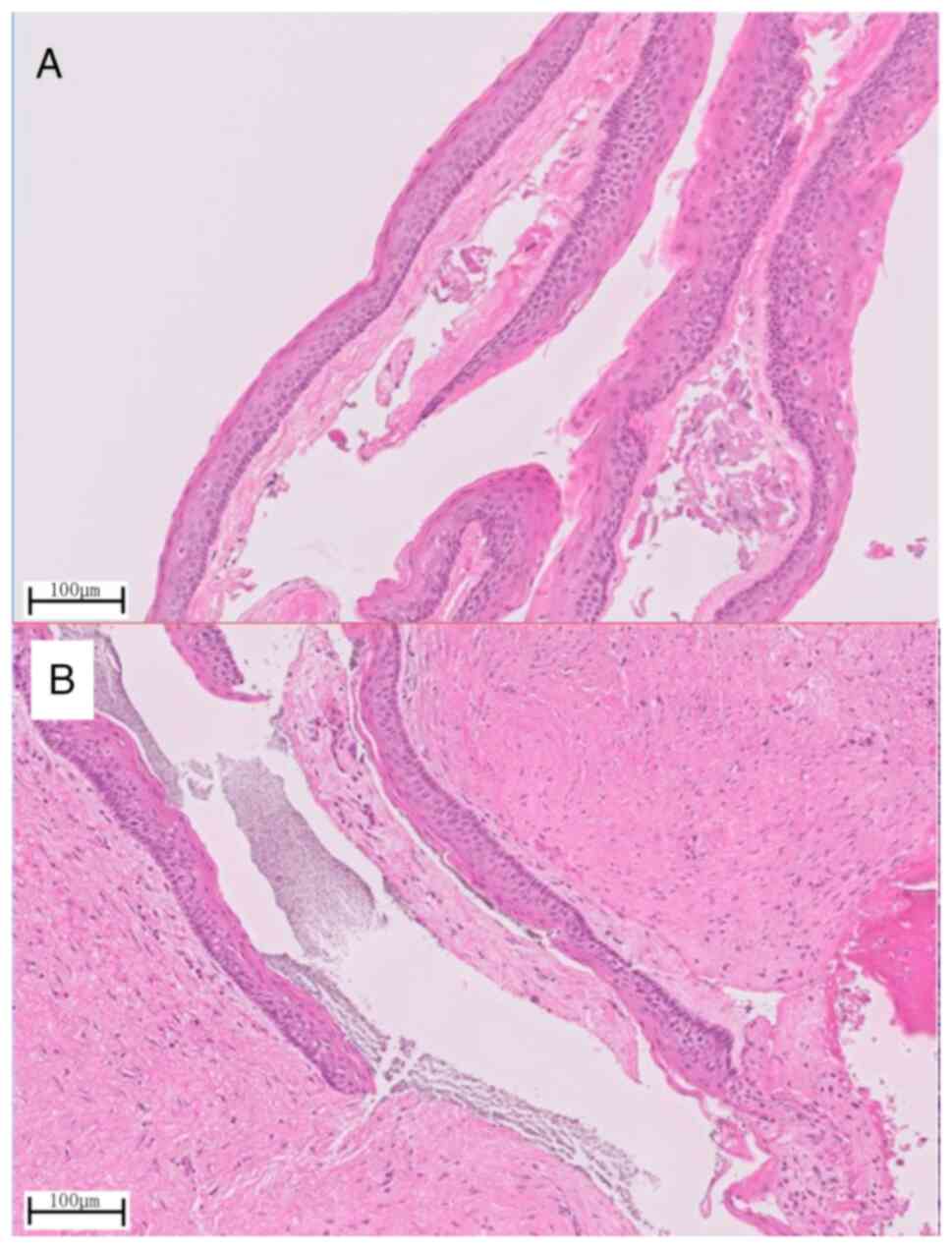
Histopathological examination of the removed
specimen showed cyst walls with a well-ordered squamous epithelial
lining in both the anterior (Fig.
8A) and posterior (Fig. 8B)
cysts. These were typical findings of OKCs showing a palisade
arrangement of basal cells and a wavy structure on the surface.
Discussion
OKCs were initially described in 1876 and were named
in 1956 by Phillipsen (12) to
describe an odontogenic cyst lined with keratinized stratified
squamous epithelium (13). In
1992, the term ‘odontogenic keratocyst’, which is synonymous with
‘primordial cyst’, was introduced by the World Health Organization
(WHO) to denote benign cysts of odontogenic origin with a specific
histological appearance. However, in 2005, this pathology was
reclassified as a benign keratocystic odontogenic tumor (KCOT) in
the third edition of the WHO classification of head and neck tumors
because of the high risk of recurrence, aggressive clinical course,
mutations in the protein patched homolog tumor suppressor gene, the
occurrence of satellite cysts and the association with Gorlin-Goltz
syndrome (14,15). However, due to insufficient
evidence to categorize this pathology as a neoplastic lesion, in
the fourth edition of the WHO classification of head and neck
tumors, KCOT was moved back into the cyst category under the name
OKC (16) and it is still
categorized as a cyst in the current classification (fifth edition)
(17).
The recurrence rate of OKC ranges between 7 and 28%
(2). Since the 1980s, it has been
suggested that to reduce the high recurrence rate of OKCs, surgery
should include marginal resection, including a rim of uninvolved
bone, which is similar to the treatment for unicystic ameloblastoma
(18). Various suggestions have
been made regarding surgical methods for OKCs. The main suggestions
are as follows: Enucleation; enucleation plus adjunctive therapy,
such as enucleation plus curettage, enucleation with Carnoy's
solution, enucleation with cryotherapy and enucleation with
peripheral ostectomy and Carnoy's solution; marsupialization;
resection; or combinations of these techniques (2). Although the difference in recurrence
rates due to the surgical method has been examined, several factors
other than the surgical method contribute to the recurrence rate,
such as multilocular cysts or unilocular cysts and perforated or
nonperforated bony walls; therefore, there is no one-size-fits-all
surgical procedure for OKC (2,19).
There is another important consideration when choosing jawbone cyst
surgery, which is the size of the cyst. Enucleation and primary
closure are often selected. This technique is accepted for lesions
<2 cm, in which angiogenic and osteogenic cells from the
adjacent bone and periosteum can reach the remaining blood clot and
could promote ossification (20).
It was predicted that the OKC described in the present case report
would create a cavity of >2 cm, including a reduction of the
bone. Enucleation, followed by open packing, has been reported to
be a less invasive method for the treatment of OKCs with a lower
recurrence rate and this method was thus used in the present study
(10,11). In the present case, after the
packing became open, the tetracycline hydrochloride ointment gauze
was replaced once a week and an impression was taken 1 month after
the operation to create an obturator to prevent a dead space from
collecting food or debris (21).
As a result, a good healing course was observed without
recurrence.
To the best of our knowledge, there have only been
two reports of OKCs in the condyloid process that are not
continuous with the surrounding areas (8,9). In
both cases, OKCs occurred in the head of the condyle, which was
resected. Although there is a difference between the condylar heads
and the base of the condyle, the present case is the first in which
the condylar process was successfully preserved. Although the
details of the subsequent course were not described in the previous
two cases, the excision of the articular process without
reconstruction may result in malocclusion and facial deformity. In
the present case, because the bone at the articular process was
thinned, a hospitalization plan was made to avoid fractures. The
patient received an oral liquid diet in the first 6 days after
surgery, and during hospitalization, the patient was allowed only a
minimum amount of mouth opening while eating or when brushing their
teeth. In addition, from February to May 2021, an obturator was
attached. A total of 20 months post-operation, the patient showed
no signs of local recurrence.
In conclusion, this report presents a rare case of
an OKC in the mandibular condyle base region of a 31-year-old man.
Resection was performed under general anesthesia and the condylar
process was successfully preserved. The patient has remained
disease-free for 20 months post-operation.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author contributions
SM, TG, JS, TK, MM, KI, NM, AM and KN examined and
treated the patient and collected the data. SM, TG, JS, KN and HN
analyzed and discussed the case and data. SM, TK, AM and KN confirm
the authenticity of all the raw data. SM wrote the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for both the surgical treatment and publication of any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Johnson NR, Gannon OM, Savage NW and
Batstone MD: Frequency of odontogenic cysts and tumors: A
systematic review. J Investig Clin Dent. 5:9–14. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Antonoglou GN, Sándor GK, Koidou VP and
Papageorgiou SN: Non-syndromic and syndromic keratocystic
odontogenic tumors: Systematic review and meta-analysis of
recurrences. J Craniomaxillofac Surg. 42:e364–e371. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Harmon M, Arrigan M, Toner M and O'Keeffe
SA: A radiological approach to benign and malignant lesions of the
mandible. Clin Radiol. 70:335–350. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
MacDonald D: Lesions of the jaws
presenting as radiolucencies on cone-beam CT. Clin Radiol.
71:972–985. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kaneda T, Minami M and Kurabayashi T:
Benign odontogenic tumors of the mandible and maxilla. Neuroimaging
Clin N Am. 13:495–507. 2003.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Farzad P: A case of an extensive
keratocystic odontogenic tumor in the mandible reconstructed with a
custom-made total joint prosthesis. Craniomaxillofac Trauma
Reconstr. 11:131–137. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fidele NB, Bing L, Sun Y, Wu T, Zheng Y
and Zhao Y: Management of mandibular odontogenic keratocyst through
radical resection: Report of 35 cases. Oncol Lett. 18:733–741.
2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kallalli B, Rawson K, Telkar S and
Penumatcha M: Keratocystic odontogenic tumor of the right
mandibular condyle: A rare case. J Indian Acad Oral Med Radiol.
26(103)2014.
|
|
9
|
Managutti A, Managutti S, Patel H and
Menat S: Orthokeratinized odontogenic cyst (OOC) of condylar head:
A rare entity. J Maxillofac Oral Surg. 15 (Suppl 2):S315–S319.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kshirsagar RA, Bhende RC, Raut PH, Mahajan
V, Tapadiya VJ and Singh V: Odontogenic Keratocyst: Developing a
protocol for surgical intervention. Ann Maxillofac Surg. 9:152–157.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yildirim G, Ataoglu H, Kalayci A, Özkan
BT, Kucuk K and Esen A: Conservative treatment protocol for
keratocystic odontogenic tumour: A follow-up study of 3 cases. J
Oral Maxillofac Res. 1(e7)2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Philipsen HP: OM Keratocysts (kole
steatoma). Tandlaegebladet. 60:963–980. 1956.(In Danish).
|
|
13
|
Chi AC, Owings JR Jr and Muller S:
Peripheral odontogenic keratocyst: Report of two cases and review
of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 99:71–78. 2005.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tomasz K, Jadwiga S and Romana T: Update
of the WHO classification of odontogenic and maxillofacial bone
tumours. Journal of Stomatology. 23:484–506. 2017.
|
|
15
|
Soluk-Tekkeşin M and Wright JM: The World
Health Organization Classification of Odontogenic Lesions: A
summary of the changes of the 2017 (4th) Edition. Turk Patoloji
Derg 34, 2018.
|
|
16
|
Speight PM and Takata T: New tumour
entities in the 4th edition of the World Health Organization
Classification of Head and Neck tumours: Odontogenic and
maxillofacial bone tumours. Virchows Arch. 472:331–339.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Soluk-Tekkesin M and Wright JM: The World
Health Organization Classification of Odontogenic Lesions: A
summary of the changes of the 2022 (5th) Edition. Turk Patoloji
Derg. 38:168–184. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ahlfors E, Larsson A and Sjögren S: The
odontogenic keratocyst: A benign cystic tumor? J Oral Maxillofac
Surg. 42:10–19. 1984.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Forssell K, Forssell H and Kahnberg KE:
Recurrence of keratocysts. A long-term follow-up study. Int J Oral
Maxillofac Surg. 17:25–28. 1988.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Carbonell-Asins P and Sánchez Aniceto G: A
retrospective risk factor analysis of infection and wound
dehiscence following guided bone regeneration in cystectomy defects
of the jaws. J Craniomaxillofac Surg. 50:657–663. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Troiano A, Lo Giudice G, De Luca R, Lo
Giudice F, D'Amato S, Tartaro G and Colella G: Salvage of dental
implant located in mandibular odontogenic Cyst. A conservative
surgical treatment proposal. Dent J (Basel). 8(E49)2020.PubMed/NCBI View Article : Google Scholar
|