|
1
|
Patel D, Shah Y, Thakkar N, Shah K and
Shah M: Implementation of artificial intelligence techniques for
cancer detection. Augment Hum Res. 5:1–10. 2020.
|
|
2
|
Burugu S, Dancsok AR and Nielsen TO:
Emerging targets in cancer immunotherapy. Semin Cancer Biol.
52:39–52. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Liu S, Zhou X, Yao Y, Shi K, Yu M and Ji
F: Resection of the gastric submucosal tumor (G-SMT) originating
from the muscularis propria layer: Comparison of efficacy,
patients' tolerability, and clinical outcomes between endoscopic
full-thickness resection and surgical resection. Surg Endosc.
34:4053–4064. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Pirisinu M, Pham TC, Zhang DX, Hong TN,
Nguyen LT and Le MT: Extracellular vesicles as natural therapeutic
agents and innate drug delivery systems for cancer treatment:
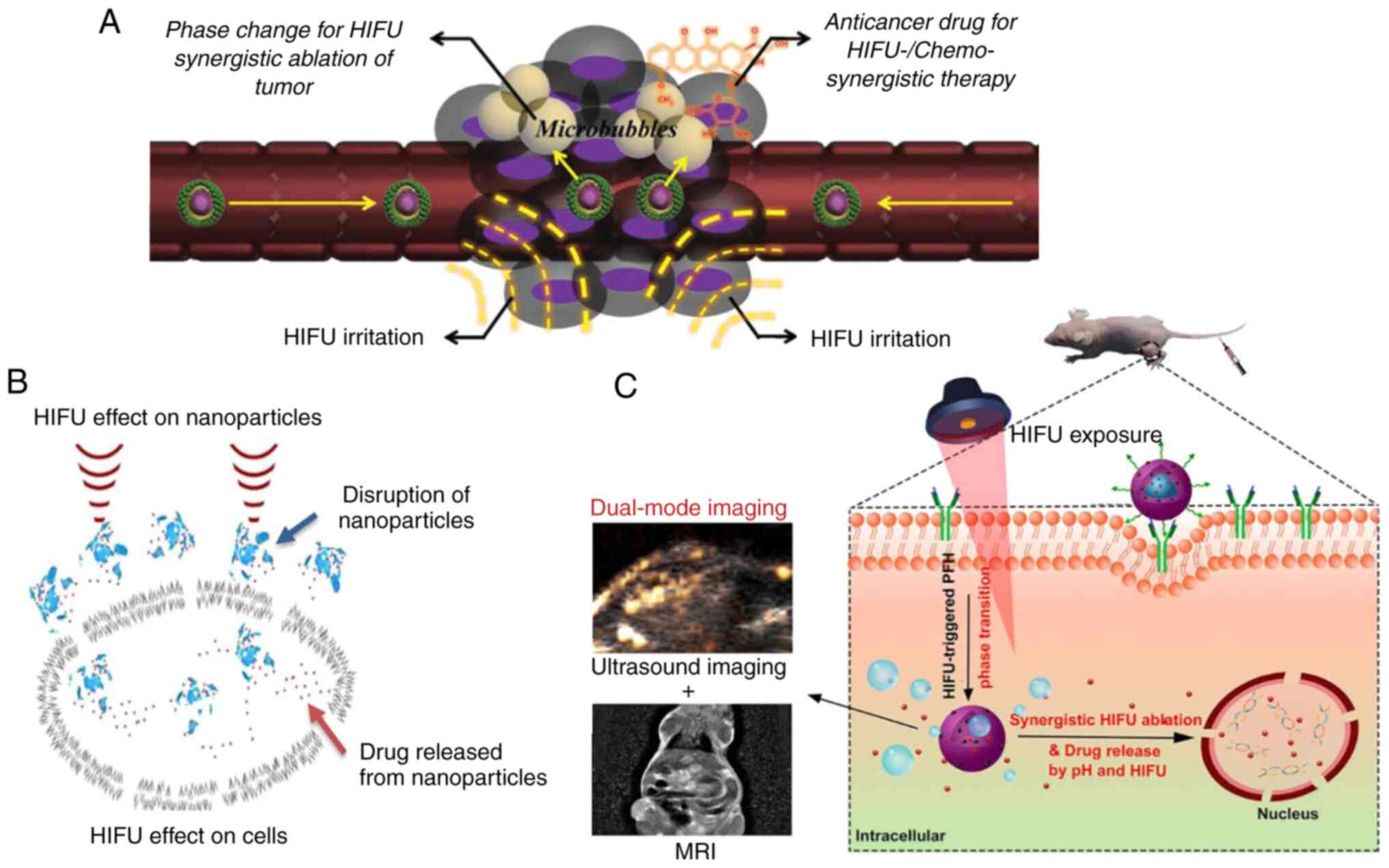
Recent advances, current obstacles, and challenges for clinical
translation. Semin Cancer Biol. 80:340–355. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Westhoff N, Ernst R, Kowalewski KF, Derigs
F, Neuberger M, Nörenberg D, Popovic ZV, Ritter M, Stephan Michel M
and von Hardenberg J: Medium-term oncological efficacy and
patient-reported outcomes after focal high-intensity focused
ultrasound: The FOXPRO trial. Eur Urol Focus. 22:S2405–S4569.
2022.PubMed/NCBI View Article : Google Scholar
|
|
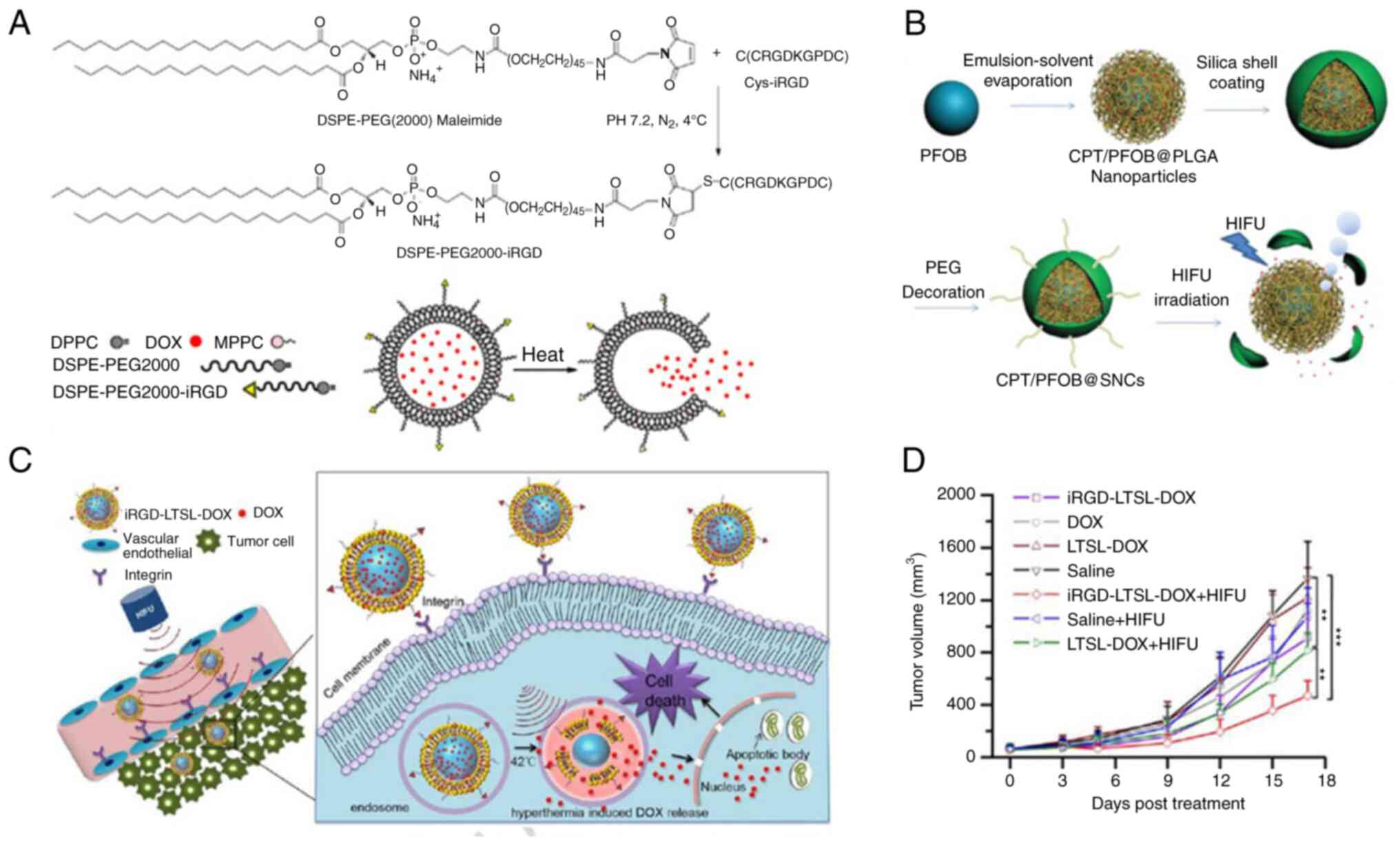
6
|
Li Y, Wang S, Chen L, Feng Y, Shen Z, Chen
X, Huang G and Ni Y: Sequential administrations of a
vascular-disrupting agent, high-intensity focused ultrasound, and a
radioactively labeled necrosis avid compound for eradicating solid
malignancies. Technol Cancer Res Treat.
21(15330338221136716)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhong Q, Tang F, Ni T, Chen Y, Liu Y, Wu
J, Zhou W, Feng Z, Lu X, Tan S and Zhang Y: Salvage high intensity
focused ultrasound for residual or recurrent cervical cancer after
definitive chemoradiotherapy. Front Immunol.
13(995930)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
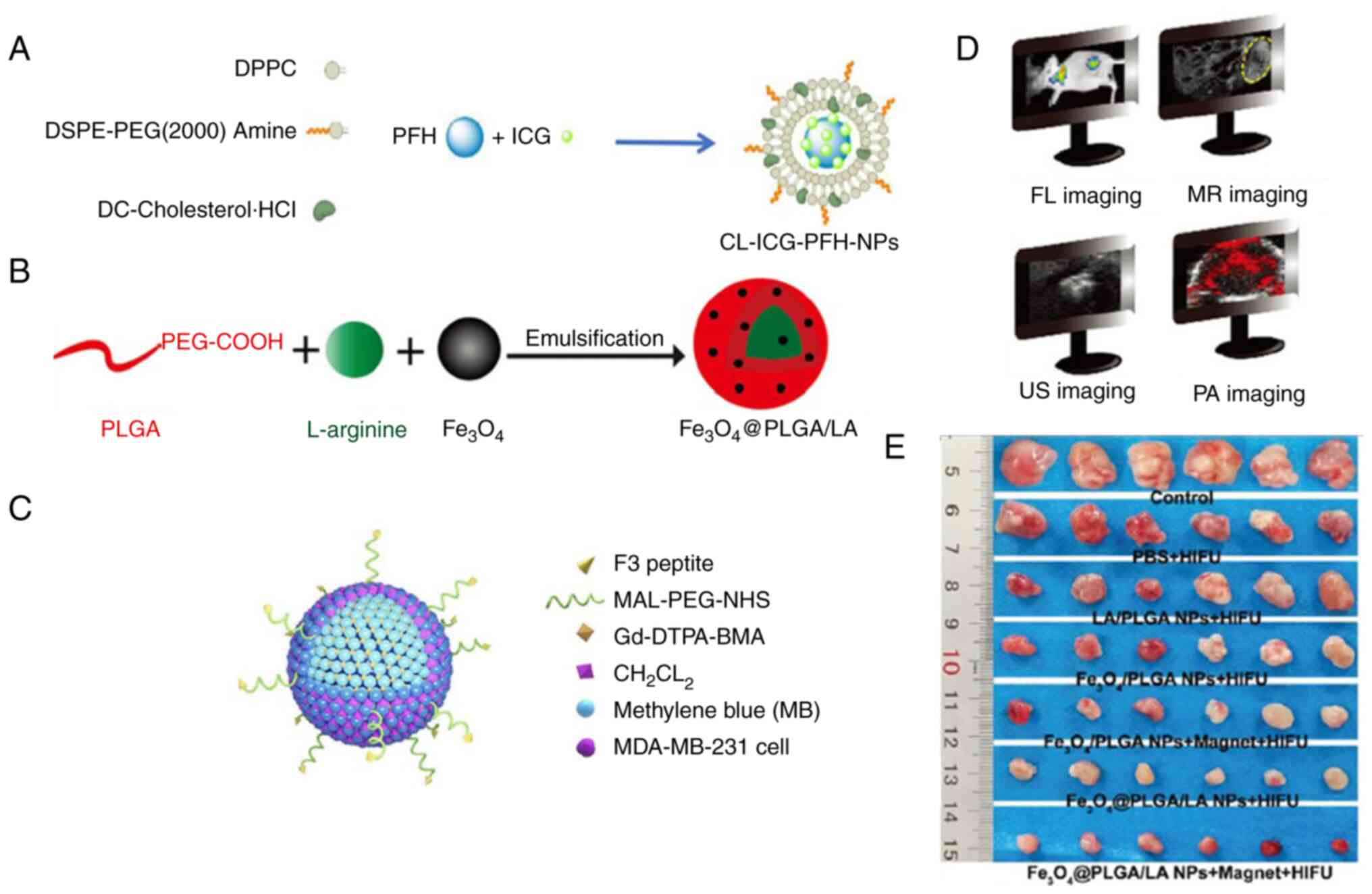
Lindstrom PA: Prefrontal ultrasonic
irradiation-a substitute for lobotomy. AMA Arch Neurol Psychiatry.
72:399–425. 1954.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Fry WJ, Barnard JW, Fry EJ, Krumins RF and
Brennan JF: Ultrasonic lesions in the mammalian central nervous
system. Science. 122:517–518. 1955.PubMed/NCBI
|
|
10
|
ter Haar G: Intervention and therapy.
Ultrasound Med Biol 26 Suppl. 1:S51–S54. 2000.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu L, Wang T and Lei B: High-intensity
focused ultrasound (HIFU) ablation versus surgical interventions
for the treatment of symptomatic uterine fibroids: A meta-analysis.
Eur Radiol. 32:1195–1204. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wang C, Li Z and Bai J: Bubble-assisted
HIFU ablation enabled by calcium peroxide. J Mater Chem B.
10:4442–4451. 2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chaussy CG and Thüroff S: High-Intensity
focused ultrasound for the treatment of prostate cancer: A review.
J Endourol. 31(S1):S30–S37. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Napoli A, Alfieri G, Scipione R, Leonardi
A, Fierro D, Panebianco V, De Nunzio C, Leonardo C and Catalano C:
High-intensity focused ultrasound for prostate cancer. Expert Rev
Med Devices. 17:427–433. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fishman PS and Fischell JM: Focused
ultrasound mediated opening of the blood-brain barrier for
neurodegenerative diseases. Front Neurol. 12(749047)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Martínez-Fernández R, Máñez-Miró JU,
Rodríguez-Rojas R, Del Álamo M, Shah BB, Hernández-Fernández F,
Pineda-Pardo JA, Monje MHG, Fernández-Rodríguez B, Sperling SA, et
al: Randomized trial of focused ultrasound subthalamotomy for
Parkinson's Disease. N Engl J Med. 383:2501–2513. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Moosa S, Martínez-Fernández R, Elias WJ,
Del Alamo M, Eisenberg HM and Fishman PS: The role of
high-intensity focused ultrasound as a symptomatic treatment for
Parkinson's disease. Mov Disord. 34:1243–1251. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Giordano M, Caccavella VM, Zaed I, Foglia
Manzillo L, Montano N, Olivi A and Polli FM: Comparison between
deep brain stimulation and magnetic resonance-guided focused
ultrasound in the treatment of essential tremor: A systematic
review and pooled analysis of functional outcomes. J Neurol
Neurosurg Psychiatry. 91:1270–1278. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Abe K, Horisawa S, Yamaguchi T, Hori H,
Yamada K, Kondo K, Furukawa H, Kamada H, Kishima H, Oshino S, et
al: Focused ultrasound thalamotomy for refractory essential tremor:
A Japanese multicenter single-arm study. Neurosurgery. 88:751–757.
2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jeng CJ, Ou KY, Long CY, Chuang L and Ker
CR: 500 cases of high-intensity focused ultrasound (HIFU) ablated
uterine fibroids and adenomyosis. Taiwan J Obstet Gynecol.
59:865–871. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sequeiros RB, Joronen K, Komar G and
Koskinen SK: High intensity focused ultrasound (HIFU) in tumor
therapy. Duodecim. 133:143–149. 2017.PubMed/NCBI
|
|
22
|
Marinova M, Wilhelm-Buchstab T and Strunk
H: Advanced pancreatic cancer: High-Intensity Focused Ultrasound
(HIFU) and other local ablative therapies. RoFo. 191:216–227.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhou YF: High intensity focused ultrasound
in clinical tumor ablation. World J Clin Oncol. 2:8–27.
2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bachu VS, Kedda J, Suk I, Green JJ and
Tyler B: High-Intensity Focused Ultrasound: A Review of Mechanisms
and Clinical Applications. Ann Biomed Eng. 49:1975–1991.
2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Izadifar Z, Izadifar Z, Chapman D and
Babyn P: An introduction to high intensity focused ultrasound:
Systematic review on principles, devices, and clinical
applications. J Clin Med. 9(460)2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Miller DL, Smith NB, Bailey MR, Czarnota
GJ, Hynynen K and Makin IR: Bioeffects Committee of the American
Institute of Ultrasound in Medicine. Overview of therapeutic
ultrasound applications and safety considerations. J Ultrasound
Med. 31:623–634. 2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Awad NS, Paul V, AlSawaftah NM, Ter Haar
G, Allen TM, Pitt WG and Husseini GA: Ultrasound-responsive
nanocarriers in cancer treatment: A review. ACS Pharmacol Transl
Sci. 4:589–612. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhang Q, Dai X, Zhang H, Zeng Y, Luo K and
Li W: Recent advances in development of nanomedicines for multiple
sclerosis diagnosis. Biomed Mater. 16(024101)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zeng Y, Li Z, Zhu H, Gu Z, Zhang H and Luo
K: Recent advances in nanomedicines for multiple sclerosis therapy.
ACS Appl Bio Mater. 3:6571–6597. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Zhou Y, Wang Z, Chen Y, Shen H, Luo Z, Li
A, Wang Q, Ran H, Li P, Song W, et al: Microbubbles from
gas-generating perfluorohexane nanoemulsions for targeted
temperature-sensitive ultrasonography and synergistic HIFU ablation
of tumors. Adv Mater. 25:4123–4130. 2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Du Y, Lin L, Zhang Z, Tang Y, Ou X, Wang Y
and Zou J: Drug-loaded nanoparticles conjugated with genetically
engineered bacteria for cancer therapy. Biochem Biophys Res Commun.
606:29–34. 2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Manthe RL, Foy SP, Krishnamurthy N, Sharma
B and Labhasetwar V: Tumor ablation and nanotechnology. Mol Pharm.
7:1880–1898. 2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chen D and Wu J: An in vitro feasibility
study of controlled drug release from encapsulated nanometer
liposomes using high intensity focused ultrasound. Ultrasonics.
50:744–749. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
O'Neill BE, Vo H, Angstadt M, Li KP, Quinn
T and Frenkel V: Pulsed high intensity focused ultrasound mediated
nanoparticle delivery: Mechanisms and efficacy in murine muscle.
Ultrasound Med Biol. 35:416–424. 2009.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chen J, Nan Z, Zhao Y, Zhang L, Zhu H, Wu
D, Zong Y, Lu M, Ilovitsh T, Wan M, et al: Enhanced HIFU
Theranostics with dual-frequency-ring focused ultrasound and
activatable perfluoropentane-loaded polymer nanoparticles.
Micromachines (Basel). 12(1324)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Sadeghi-Goughari M, Jeon S and Kwon HJ:
Analytical and numerical model of high intensity focused ultrasound
enhanced with nanoparticles. IEEE Trans Biomed Eng. 67:3083–3093.
2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Chen Y, Chen H and Shi J:
Nanobiotechnology promotes noninvasive high-intensity focused
ultrasound cancer surgery. Adv Healthc Mater. 4:158–165.
2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Poh S, Chelvam V and Low PS: Comparison of
nanoparticle penetration into solid tumors and sites of
inflammation: Studies using targeted and nontargeted liposomes.
Nanomedicine (Lond). 10:1439–1449. 2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Tang H, Guo Y, Peng L, Fang H, Wang Z,
Zheng Y, Ran H and Chen Y: In Vivo targeted, responsive, and
synergistic cancer nanotheranostics by magnetic resonance
imaging-guided synergistic high-intensity focused ultrasound
ablation and chemotherapy. ACS Appl Mater Interfaces.
10:15428–15441. 2018.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Tharkar P, Varanasi R, Wong WSF, Jin CT
and Chrzanowski W: Nano-Enhanced drug delivery and therapeutic
ultrasound for cancer treatment and beyond. Front Bioeng
Biotechnol. 7(324)2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Wang X, Yan F, Liu X, Wang P, Shao S, Sun
Y, Sheng Z, Liu Q, Lovell JF and Zheng H: Enhanced drug delivery
using sonoactivatable liposomes with membrane-embedded porphyrins.
J Control Release. 286:358–368. 2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Chaudhuri A, Kumar DN, Shaik RA, Eid BG,
Abdel-Naim AB, Md S, Ahmad A and Agrawal AK: Lipid-Based
nanoparticles as a pivotal delivery approach in triple negative
breast cancer (TNBC) therapy. Int J Mol Sci.
23(10068)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Yudina A and Moonen C: Ultrasound-induced
cell permeabilisation and hyperthermia: Strategies for local
delivery of compounds with intracellular mode of action. Int J
Hyperthermia. 28:311–319. 2012.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Cha JM, You DG, Choi EJ, Park SJ, Um W,
Jeon J, Kim K, Kwon IC, Park JC, Kim HR and Park JH: Improvement of
Antitumor Efficacy by Combination of Thermosensitive Liposome with
High-Intensity Focused Ultrasound. J Biomed Nanotechnol.
12:1724–1733. 2016.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Deng Z, Xiao Y, Pan M, Li F, Duan W, Meng
L, Liu X, Yan F and Zheng H: Hyperthermia-triggered drug delivery
from iRGD-modified temperature-sensitive liposomes enhances the
anti-tumor efficacy using high intensity focused ultrasound. J
Control Release. 243:333–341. 2016.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Yang Q, Zhou Y, Chen J, Huang N, Wang Z
and Cheng Y: Gene therapy for drug-resistant glioblastoma via
lipid-polymer hybrid nanoparticles combined with focused
ultrasound. Int J Nanomedicine. 16:185–199. 2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Arsiwala TA, Sprowls SA, Blethen KE,
Adkins CE, Saralkar PA, Fladeland RA, Pentz W, Gabriele A,
Kielkowski B, Mehta RI, et al: Ultrasound-mediated disruption of
the blood tumor barrier for improved therapeutic delivery.
Neoplasia. 23:676–691. 2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Luo Z, Jin K, Pang Q, Shen S, Yan Z, Jiang
T, Zhu X, Yu L, Pang Z and Jiang X: On-Demand drug release from
dual-targeting small nanoparticles triggered by high-intensity
focused ultrasound enhanced glioblastoma-targeting therapy. ACS
Appl Mater Interfaces. 9:31612–31625. 2017.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Sokka S, King R and Hynynen K: MRI-guided
gas bubble enhanced ultrasound heating in in vivo rabbit thigh.
Phys Med Biol. 48:223–241. 2003.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Clark A, Bonilla S, Suo D, Shapira Y and
Averkiou M: Microbubble-Enhanced Heating: Exploring the effect of
microbubble concentration and pressure amplitude on high-intensity
focused ultrasound treatments. Ultrasound Med Biol. 47:2296–2309.
2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Xin Y, Zhang A, Xu LX and Fowlkes JB:
Numerical study of bubble cloud and thermal lesion evolution during
acoustic droplet vaporization enhanced HIFU treatment. J Biomech
Eng. 144(031007)2022.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Okita K, Sugiyama K, Takagi S and Matsumto
Y: Microbubble behavior in an ultrasound field for high intensity
focused ultrasound therapy enhancement. J Acoust Soc Am.
134:1576–1585. 2013.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Hamano N, Negishi Y, Takatori K,
Endo-Takahashi Y, Suzuki R, Maruyama K, Niidome T and Aramaki Y:
Combination of bubble liposomes and high-intensity focused
ultrasound (HIFU) enhanced antitumor effect by tumor ablation. Biol
Pharm Bull. 37:174–177. 2014.PubMed/NCBI View Article : Google Scholar
|
|
54
|
VanOsdol J, Ektate K, Ramasamy S, Maples
D, Collins W, Malayer J and Ranjan A: Sequential HIFU heating and
nanobubble encapsulation provide efficient drug penetration from
stealth and temperature sensitive liposomes in colon cancer. J
Control Release. 247:55–63. 2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Zhou LQ, Li P, Cui XW and Dietrich CF:
Ultrasound nanotheranostics in fighting cancer: Advances and
prospects. Cancer Lett. 470:204–219. 2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Li K, Liu Y, Zhang S, Xu Y, Jiang J, Yin
F, Hu Y, Han B, Ge S, Zhang L and Wang Y: Folate receptor-targeted
ultrasonic PFOB nanoparticles: Synthesis, characterization and
application in tumor-targeted imaging. Int J Mol Med. 39:1505–1515.
2017.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Sheeran PS, Matsunaga TO and Dayton PA:
Phase change events of volatile liquid perfluorocarbon contrast
agents produce unique acoustic signatures. Phys Med Biol.
59:379–401. 2014.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Picheth G, Houvenagel S, Dejean C, Couture
O, Alves de Freitas R, Moine L and Tsapis N: Echogenicity
enhancement by end-fluorinated polylactide perfluorohexane
nanocapsules: Towards ultrasound-activable nanosystems. Acta
Biomater. 64:313–322. 2017.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Ashida R, Kawabata K, Maruoka T, Asami R,
Yoshikawa H, Takakura R, Ioka T, Katayama K and Tanaka S: New
approach for local cancer treatment using pulsed high-intensity
focused ultrasound and phase-change nanodroplets. J Med Ultrason
(2001). 42:457–466. 2015.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Xu T, Cui Z, Li D, Cao F, Xu J, Zong Y,
Wang S, Bouakaz A, Wan M and Zhang S: Cavitation characteristics of
flowing low and high boiling-point perfluorocarbon phase-shift
nanodroplets during focused ultrasound exposures. Ultrason
Sonochem. 65(105060)2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Rapoport N: Phase-shift,
stimuli-responsive perfluorocarbon nanodroplets for drug delivery
to cancer. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 4:492–510.
2012.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Sheeran PS and Dayton PA: Phase-change
contrast agents for imaging and therapy. Curr Pharm Des.
18:2152–2165. 2012.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Kwizera EA, Stewart S, Mahmud MM and He X:
Magnetic nanoparticle-mediated heating for biomedical applications.
J Heat Transfer. 144(030801)2022.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Zhang Y, Yong L, Luo Y, Ding X, Xu D, Gao
X, Yan S, Wang Q, Luo J, Pu D and Zou J: Enhancement of HIFU
ablation by sonosensitizer-loading liquid fluorocarbon
nanoparticles with pre-targeting in a mouse model. Sci Rep.
9(6982)2019.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Sun Y, Zheng Y, Ran H, Zhou Y, Shen H,
Chen Y, Chen H, Krupka TM, Li A, Li P, et al: Superparamagnetic
PLGA-iron oxide microcapsules for dual-modality US/MR imaging and
high intensity focused US breast cancer ablation. Biomaterials.
33:5854–5864. 2012.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Sun Y, Zheng Y, Li P, Wang D, Niu C, Gong
Y, Huang R, Wang Z, Wang Z and Ran H: Evaluation of
superparamagnetic iron oxide-polymer composite microcapsules for
magnetic resonance-guided high-intensity focused ultrasound cancer
surgery. BMC Cancer. 14(800)2014.PubMed/NCBI View Article : Google Scholar
|
|
67
|
You Y, Wang Z, Ran H, Zheng Y, Wang D, Xu
J, Wang Z, Chen Y and Li P: Nanoparticle-enhanced synergistic HIFU
ablation and transarterial chemoembolization for efficient cancer
therapy. Nanoscale. 8:4324–4339. 2016.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Ho VH, Smith MJ and Slater NK: Effect of
magnetite nanoparticle agglomerates on the destruction of tumor
spheroids using high intensity focused ultrasound. Ultrasound Med
Biol. 37:169–175. 2011.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Dibaji SAR, Al-Rjoub MF, Myers MR and
Banerjee RK: Enhanced heat transfer and thermal dose using magnetic
nanoparticles during HIFU thermal ablation-an in-vitro study. J
Nanotechnol Eng Med. 4(040902)2014.
|
|
70
|
Devarakonda SB, Myers MR, Giridhar D,
Dibaji SA and Banerjee RK: Enhanced thermal effect using magnetic
nano-particles during high-intensity focused ultrasound. PLoS One.
12(e0175093)2017.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Devarakonda SB, Myers MR and Banerjee RK:
Comparison of heat transfer enhancement between magnetic and gold
nanoparticles during HIFU sonication. J Biomech Eng.
140:2018.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Kaczmarek K, Hornowski T, Kubovčíková M,
Timko M, Koralewski M and Józefczak A: Heating induced by
therapeutic ultrasound in the presence of magnetic nanoparticles.
ACS Appl Mater Interfaces. 10:11554–11564. 2018.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Sadeghi-Goughari M, Jeon S and Kwon HJ:
Magnetic nanoparticles-enhanced focused ultrasound heating: Size
effect, mechanism, and performance analysis. Nanotechnology.
31(245101)2020.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Kimura NT, Taniguchi S, Aoki K and Baba T:
Selective localization and growth of Bifidobacterium bifidum in
mouse tumors following intravenous administration. Cancer Res.
40:2061–2068. 1980.PubMed/NCBI
|
|
75
|
Li X, Fu GF, Fan YR, Liu WH, Liu XJ, Wang
JJ and Xu GX: Bifidobacterium adolescentis as a delivery system of
endostatin for cancer gene therapy: Selective inhibitor of
angiogenesis and hypoxic tumor growth. Cancer Gene Ther.
10:105–111. 2003.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Luo CH, Huang CT, Su CH and Yeh CS:
Bacteria-Mediated hypoxia-specific delivery of nanoparticles for
tumors imaging and therapy. Nano Lett. 16:3493–3499.
2016.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Xu D, Zou W, Luo Y, Gao X, Jiang B, Wang
Y, Jiang F, Xiong J, Chen C, Tang Y, et al: Feasibility between
bifidobacteria targeting and changes in the acoustic environment of
tumor tissue for synergistic HIFU. Sci Rep. 10(7772)2020.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Jiang BL, Gao X, Xiong J, Zhu PY, Luo Y,
Xu D, Tang Y, Wang YT, Chen C, Yang HY, et al: Experimental study
on synergistic effect of HIFU treatment of tumors using
Bifidobacterium bound with cationic phase-change nanoparticles. Eur
Rev Med Pharmacol Sci. 24:5714–5725. 2020.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Zhu C, Ji Z, Ma J, Ding Z, Shen J and Wang
QW: Recent advances of nanotechnology-facilitated bacteria-based
drug and gene delivery systems for cancer treatment. Pharmaceutics.
13(940)2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Yin T, Diao Z, Blum NT, Qiu L, Ma A and
Huang P: Engineering bacteria and bionic bacterial derivatives with
nanoparticles for cancer therapy. Small.
18(e2104643)2022.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Kalia VC, Patel SKS, Cho BK, Wood TK and
Lee JK: Emerging applications of bacteria as antitumor agents.
Semin Cancer Biol. 86(Pt 2):1014–1025. 2022.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Tang Y, Chen C, Jiang B, Wang L, Jiang F,
Wang D, Wang Y, Yang H, Ou X, Du Y, et al: Bifidobacterium
bifidum-Mediated specific delivery of nanoparticles for tumor
therapy. Int J Nanomedicine. 16:4643–4659. 2021.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Wang D, Jiang F, Wang L, Tang Y, Zhang Z,
Du Y and Zou J: Polyethylenimine (PEI)-modified poly
(lactic-co-glycolic) acid (PLGA) nanoparticles conjugated with
tumor-homing bacteria facilitate high intensity focused
ultrasound-mediated tumor ablation. Biochem Biophys Res Commun.
571:104–109. 2021.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Tee JK, Yip LX, Tan ES, Santitewagun S,
Prasath A, Ke PC, Ho HK and Leong DT: Nanoparticles' interactions
with vasculature in diseases. Chem Soc Rev. 48:5381–5407.
2019.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Wang Y, Chen C, Luo Y, Xiong J, Tang Y,
Yang H, Wang L, Jiang F, Gao X, Xu D, et al: Experimental study of
tumor therapy mediated by multimodal imaging based on a biological
targeting synergistic agent. Int J Nanomedicine. 15:1871–1888.
2020.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Han H, Lee H, Kim K and Kim H: Effect of
high intensity focused ultrasound (HIFU) in conjunction with a
nanomedicines-microbubble complex for enhanced drug delivery. J
Control Release. 266:75–86. 2017.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Frazier N, Payne A, Dillon C, Subrahmanyam
N and Ghandehari H: Enhanced efficacy of combination heat shock
targeted polymer therapeutics with high intensity focused
ultrasound. Nanomedicine. 13:1235–1243. 2017.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Li Q, Zhang J, Li J, Ye H, Li M, Hou W, Li
H and Wang Z: Glutathione-Activated NO-/ROS-Generation
nanoparticles to modulate the tumor hypoxic microenvironment for
enhancing the effect of HIFU-Combined Chemotherapy. ACS Appl Mater
Interfaces. 13:26808–26823. 2021.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Kang Y, Kim J, Park J, Lee YM,
Saravanakumar G, Park KM, Choi W, Kim K, Lee E, Kim C and Kim WJ:
Tumor vasodilation by N-Heterocyclic carbene-based nitric oxide
delivery triggered by high-intensity focused ultrasound and
enhanced drug homing to tumor sites for anti-cancer therapy.
Biomaterials. 217(119297)2019.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Li H, Yu C, Zhang J, Li Q, Qiao H, Wang Z
and Zeng D: pH-sensitive pullulan-doxorubicin nanoparticles loaded
with 1,1,2-trichlorotrifluoroethane as a novel synergist for high
intensity focused ultrasound mediated tumor ablation. Int J Pharm.
556:226–235. 2019.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Yildirim A, Shi D, Roy S, Blum NT,
Chattaraj R, Cha JN and Goodwin AP: Nanoparticle-Mediated acoustic
cavitation enables high intensity focused ultrasound ablation
without tissue heating. ACS Appl Mater Interfaces. 10:36786–36795.
2018.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Yildirim A, Chattaraj R, Blum NT, Shi D,
Kumar K and Goodwin AP: Phospholipid capped mesoporous
nanoparticles for targeted high intensity focused ultrasound
ablation. Adv Healthc Mater. 6:2017.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Yildirim A, Blum NT and Goodwin AP:
Colloids, nanoparticles, and materials for imaging, delivery,
ablation, and theranostics by focused ultrasound (FUS).
Theranostics. 9:2572–2594. 2019.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Jain K and Zhong J: Theranostic
applications of nanomaterials. Curr Pharm Des.
28(77)2022.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Hartl D, de Luca V, Kostikova A, Laramie
J, Kennedy S, Ferrero E, Siegel R, Fink M, Ahmed S, Millholland J,
et al: Translational precision medicine: An industry perspective. J
Transl Med. 19(245)2021.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Sisodiya SM: Precision medicine and
therapies of the future. Epilepsia. 62 (Suppl 2):S90–S105.
2021.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Li H, Zeng Y, Zhang H, Gu Z, Gong Q and
Luo K: Functional gadolinium-based nanoscale systems for cancer
theranostics. J Control Release. 329:482–512. 2021.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Kavros SJ and Coronado R: Diagnostic and
therapeutic ultrasound on venous and arterial ulcers: A focused
review. Adv Skin Wound Care. 31:55–65. 2018.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Meng Y, Pople CB, Budiansky D, Li D,
Suppiah S, Lim-Fat MJ, Perry J, Sahgal A and Lipsman N: Current
state of therapeutic focused ultrasound applications in
neuro-oncology. J Neurooncol. 156:49–59. 2022.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Blum NT, Yildirim A, Chattaraj R and
Goodwin AP: Nanoparticles formed by acoustic destruction of
microbubbles and their utilization for imaging and effects on
therapy by high intensity focused ultrasound. Theranostics.
7:694–702. 2017.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Zhu J, Li Z, Zhang C, Lin L, Cao S, Che H,
Shi X, Wang H and van Hest JCM: Single enzyme loaded nanoparticles
for combinational ultrasound-guided focused ultrasound ablation and
hypoxia-relieved chemotherapy. Theranostics. 9:8048–8060.
2019.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Li C, Lu Y, Cheng L, Zhang X, Yue J and
Liu J: Combining mechanical high-intensity focused ultrasound
ablation with chemotherapy for augmentation of anticancer immune
responses. Mol Pharm. 18:2091–2103. 2021.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Zhu S, Zhang T, Zheng L, Liu H, Song W,
Liu D, Li Z and Pan CX: Combination strategies to maximize the
benefits of cancer immunotherapy. J Hematol Oncol.
14(156)2021.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Chen J, Tan Q, Yang Z and Jin Y:
Engineered extracellular vesicles: Potentials in cancer combination
therapy. J Nanobiotechnology. 20(132)2022.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Barisano G, Sepehrband F, Ma S, Jann K,
Cabeen R, Wang DJ, Toga AW and Law M: Clinical 7 T MRI: Are we
there yet? A review about magnetic resonance imaging at ultra-high
field. Br J Radiol. 92(20180492)2019.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Lutz NW and Bernard M: Contactless
Thermometry by MRI and MRS: Advanced methods for thermotherapy and
biomaterials. iScience. 23(101561)2020.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Sparacia G and Sakai K: Temperature
measurement by diffusion-weighted imaging. Magn Reson Imaging Clin
N Am. 29:253–261. 2021.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Devarakonda SB, Myers MR, Lanier M,
Dumoulin C and Banerjee RK: Assessment of gold
nanoparticle-mediated-enhanced hyperthermia using MR-Guided
high-intensity focused ultrasound ablation procedure. Nano Lett.
17:2532–2538. 2017.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Devarakonda SB, Stringer K, Rao M, Myers M
and Banerjee R: Assessment of enhanced thermal effect due to gold
nanoparticles during MR-Guided high-intensity focused ultrasound
(HIFU) procedures using a mouse-tumor model. ACS Biomater Sci Eng.
5:4102–4111. 2019.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Kuai X, Zhu Y, Yuan Z, Wang S, Lin L, Ye
X, Lu Y, Luo Y, Pang Z, Geng D and Yin B: Perfluorooctyl bromide
nanoemulsions holding MnO2 nanoparticles with
dual-modality imaging and glutathione depletion enhanced
HIFU-eliciting tumor immunogenic cell death. Acta Pharm Sin B.
12:967–981. 2022.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Mattrey RF: Perfluorooctylbromide: A new
contrast agent for CT, sonography, and MR imaging. AJR Am J
Roentgenol. 152:247–252. 1989.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Li X, Sui Z, Li X, Xu W, Guo Q, Sun J and
Jing F: Perfluorooctylbromide nanoparticles for ultrasound imaging
and drug delivery. Int J Nanomedicine. 13:3053–3067.
2018.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Pellico J, Ellis CM and Davis JJ:
Nanoparticle-based paramagnetic contrast agents for magnetic
resonance imaging. Contrast Media Mol Imaging.
2019(1845637)2019.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Cai X, Zhu Q, Zeng Y, Zeng Q, Chen X and
Zhan Y: Manganese oxide nanoparticles As MRI contrast agents in
tumor multimodal imaging and therapy. Int J Nanomedicine.
14:8321–8344. 2019.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Das D, Sharma A, Rajendran P and Pramanik
M: Another decade of photoacoustic imaging. Phys Med Biol.
66(5)2021.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Jacques SL: Optical properties of
biological tissues: A review. Phys Med Biol. 58:R37–R61.
2013.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Wu D, Huang L, Jiang MS and Jiang H:
Contrast agents for photoacoustic and thermoacoustic imaging: A
review. Int J Mol Sci. 15:23616–23639. 2014.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Palma-Chavez J, Pfefer TJ, Agrawal A,
Jokerst JV and Vogt WC: Review of consensus test methods in medical
imaging and current practices in photoacoustic image quality
assessment. J Biomed Opt. 26(090901)2021.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Steinberg I, Huland DM, Vermesh O, Frostig
HE, Tummers WS and Gambhir SS: Photoacoustic clinical imaging.
Photoacoustics. 14:77–98. 2019.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Brunker J, Yao JJ, Laufer J and Bohndiek
SE: Photoacoustic imaging using genetically encoded reporters: A
review. J Biomed Opt. 22:2017.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Feng G, Hao L, Xu C, Ran H, Zheng Y, Li P,
Cao Y, Wang Q, Xia J and Wang Z: High-intensity focused
ultrasound-triggered nanoscale bubble-generating liposomes for
efficient and safe tumor ablation under photoacoustic imaging
monitoring. Int J Nanomedicine. 12:4647–4659. 2017.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Attia ABE, Balasundaram G, Moothanchery M,
Dinish US, Bi R, Ntziachristos V and Olivo M: A review of clinical
photoacoustic imaging: Current and future trends. Photoacoustics.
16(100144)2019.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Gao H, Wang Z, Tan M, Liu W, Zhang L,
Huang J, Cao Y, Li P, Wang Z, Wen J, et al: pH-Responsive
nanoparticles for enhanced antitumor activity by high-intensity
focused ultrasound therapy combined with sonodynamic therapy. Int J
Nanomedicine. 17:333–350. 2022.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Chen Q, Qin W, Qi W and Xi L: Progress of
clinical translation of handheld and semi-handheld photoacoustic
imaging. Photoacoustics. 22(100264)2021.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Neprokin A, Broadway C, Myllylä T, Bykov A
and Meglinski I: Photoacoustic Imaging in Biomedicine and Life
Sciences. Life (Basel). 12(588)2022.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Yan S, Lu M, Ding X, Chen F, He X, Xu C,
Zhou H, Wang Q, Hao L and Zou J: HematoPorphyrin Monomethyl Ether
polymer contrast agent for ultrasound/photoacoustic dual-modality
imaging-guided synergistic high intensity focused ultrasound (HIFU)
therapy. Sci Rep. 6(31833)2016.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Zhang N, Cai X, Gao W, Wang R, Xu C, Yao
Y, Hao L, Sheng D, Chen H, Wang Z and Zheng Y: A multifunctional
theranostic nanoagent for dual-mode image-guided
HIFU/Chemo-Synergistic cancer therapy. Theranostics. 6:404–417.
2016.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Park EY, Lee H, Han S, Kim C and Kim J:
Photoacoustic imaging systems based on clinical ultrasound
platform. Exp Biol Med (Maywood). 247:551–560. 2022.PubMed/NCBI View Article : Google Scholar
|
|
129
|
Li Y, Hao L, Liu F, Yin L, Yan S, Zhao H,
Ding X, Guo Y, Cao Y, Li P, et al: Cell penetrating
peptide-modified nanoparticles for tumor targeted imaging and
synergistic effect of sonodynamic/HIFU therapy. Int J Nanomedicine.
14:5875–5894. 2019.PubMed/NCBI View Article : Google Scholar
|
|
130
|
Yang H, Jiang F, Zhang L, Wang L, Luo Y,
Li N, Guo Y, Wang Q and Zou J: Multifunctional l-arginine-based
magnetic nanoparticles for multiple-synergistic tumor therapy.
Biomater Sci. 9:2230–2243. 2021.PubMed/NCBI View Article : Google Scholar
|
|
131
|
Isoda K, Nagata R, Hasegawa T, Taira Y,
Taira I, Shimizu Y, Isama K, Nishimura T and Ishida I:
Hepatotoxicity and drug/chemical interaction toxicity of nanoclay
particles in mice. Nanoscale Res Lett. 12(199)2017.PubMed/NCBI View Article : Google Scholar
|
|
132
|
Dai X, Zeng Y, Zhang H, Gu Z, Gong Q and
Luo K: Advances on Nanomedicines for Diagnosis and Theranostics of
Hepatic Fibrosis. Adv Biomed Res. 1(2000091)2021.
|
|
133
|
Federau C, Goubran M, Rosenberg J,
Henderson J, Halpern CH, Santini V, Wintermark M, Butts Pauly K and
Ghanouni P: Transcranial MRI-guided high-intensity focused
ultrasound for treatment of essential tremor: A pilot study on the
correlation between lesion size, lesion location, thermal dose, and
clinical outcome. J Magn Reson Imaging. 48:58–65. 2018.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Huber PM, Afzal N, Arya M, Boxler S,
Dudderidge T, Emberton M, Guillaumier S, Hindley RG, Hosking-Jervis
F, Leemann L, et al: An exploratory study of dose escalation vs
standard focal high-intensity focused ultrasound for treating
nonmetastatic prostate cancer. J Endourol. 34:641–646.
2020.PubMed/NCBI View Article : Google Scholar
|