Introduction
Hepatolenticular degeneration, also known as
Wilson's disease (WD), is a rare autosomal recessive genetic
disease associated with copper ion metabolism disorder that is
caused by ATPase copper transporting β gene mutation and
dysfunction. It involves a large amount of copper ion deposition in
the liver, brain, cornea, kidney and other organs, which leads to
liver damage, renal dysfunction, neurological impairment and
dyskinesia (1). The liver is the
primary affected organ. The patient develops liver fibrosis and
even cirrhosis, resulting in abnormal liver function and portal
hypertension, which further leads to splenomegaly and
hypersplenism. The patient exhibits a decrease in peripheral
hemogram, especially the blood platelet (PLT) count (2), followed by bleeding, immunity
decline, susceptibility to infection and other clinical
manifestations. Treatment-associated side effects, including bone
marrow suppression caused by copper-excreting drugs such as
penicillamine, aggravate the symptoms (3).
Splenectomy, as an effective method for the
treatment of WD with hypersplenism, is more affordable and feasible
compared with liver transplantation and has been proven to improve
liver fibrosis and cirrhosis by reducing portal pressure and
reducing the inflammatory response (4). However, studies have shown that
splenectomy in WD may aggravate neurological dysfunction and cause
death (5,6). Cai et al (7) studied 42 patients with hypersplenism
of WD and found that neurological symptoms did not worsen after
splenectomy, with a total success rate of 90.48%. Therefore, an
increasing number of patients with hypersplenism of WD have chosen
surgical splenectomy for treatment and domestic reports on this
topic are also gradually increasing (8-13).
The present study reviewed the medical records of
patients with hypersplenism of WD at The First Affiliated Hospital
of Anhui University of Traditional Chinese Medicine (Hefei, China)
and used inverse probability weighting and a propensity score model
to balance the differences in covariates between splenectomy vs.
non-splenectomy treatment groups, including age, sex, course of the
disease and other factors. By decreasing confounding bias between
different groups and improving the accuracy of efficacy evaluation,
the causal association between treatment factors and effects was
further explored (14) to evaluate
the impact of splenectomy on PLT count, liver function,
psychoneurological symptoms and survival prognosis.
Materials and methods
Case source, diagnosis and exclusion
criteria
The present was a retrospective single-centre cohort
study that included individuals who sought medical advice at the
First Affiliated Hospital of Anhui University of Traditional
Chinese Medicine from January 1, 2012, to January 1, 2022, and met
the diagnostic criteria of WD, which include history of liver
disease, presence or absence of extrapyramidal symptoms, notably
decreased serum ceruloplasmin or increased liver copper levels,
positive corneal K-F ring examined under the slit lamp or positive
family history (15-17).
Additional criteria for inclusion were (18): Moderate or severe splenomegaly
based on colour Doppler ultrasound or laboratory examination;
absent or mild ascites; pancytopenia, especially PLT
<60x109/l and confirmation of the diagnosis by
clinical follow-up at ≥1 year. Patients with viral, toxic alcoholic
or immune hepatitis and their complications, as well as those who
had hepatic encephalopathy, hepatorenal syndrome, severe ascites
infection, serious cardiopulmonary disease or coagulation
dysfunction, severe psychoneurological symptoms or those aged <5
or >45 years old, were excluded. The present study was approved
by The Institutional Review Committee of The First Affiliated
Hospital of Anhui University of Traditional Chinese Medicine
(approval NO. 2022AH-25).
Liver and psychoneurological function
evaluation
At the initial visit, the patient age, sex,
symptoms, course of the disease and diagnostic test results were
collected. PLT levels were recorded at each visit. Concomitantly,
the Child-Pugh classification system (19) was used to assign patients to three
categories based on their liver function (A, good hepatic function;
B, moderately impaired hepatic function; and C, advanced hepatic
dysfunction; patients in the category C were not treated with
surgery) that is determined through a scoring system that uses five
clinical and laboratory criteria: Hepatic encephalopathy; ascites;
serum bilirubin; albumin and prothrombin time.
In addition, improved Young scale was used to
evaluate psychoneurological function (20). The survival time and status of
patients receiving surgical and non-surgical treatment were
recorded during follow-up. The follow-up time of surgical patients
was 13.16±2.43 years, and that of non-surgical patients was
11.57±3.05 years.
Surgical procedure
Patients who underwent splenectomy for WD were
routinely treated with Gandouling (The First Affiliated Hospital of
Anhui University of Traditional Chinese Medicine) combined with
2,3-dimercapto-1-propane-sulfonate for 4-6 courses before surgery.
The operation was a simple splenectomy. After entering the
abdominal cavity, the gastrocolic and inferior pole gastrosplenic
ligaments were separated, and the splenic artery was routinely
revealed and ligated to allow adequate return of splenic blood; the
spleen was removed after dissecting and ligating the 2nd to 3rd
level vessels of the spleen one by one in a near bloodless state,
with all traumatic surfaces plasmapheresis sutured. Homeostatic,
anti-infection agents and sodium salt restriction and diuretics
were used to treat patients with coagulation dysfunction, infection
or ascites, respectively. All patients underwent regular
anti-copper treatment including long-term oral copper excretion
drugs and regular intravenous copper excretion treatment.
Statistical analysis
Propensity score and inverse probability weighting
were used to adjust the covariate imbalance caused by
non-randomization in patients with WD after splenectomy (21-23).
Baseline data and the preoperative data of patients were scored by
the propensity score model to evaluate the probability of
splenectomy in patients with WD. The obtained probability was
adjusted by inverse probability weighting and the influence of
splenectomy on time-weighted PLT, liver function levels and
modified Young scale scores in patients with WD was analysed by a
regression model after adjusting for confounding factors. The
time-weighted average was calculated by multiplying the index or
score of each visit by the time interval between this visit and the
previous visit. Paired t test was used for continuous variables
while a χ2 test was used for categorical variables. A
Cox proportional hazard model landmark analysis and Kaplan-Meier
curve were used to predict the effect of splenectomy on the
survival and prognosis of patients with WD and hypersplenism.
Schoenfeld, deviation and martingale residual tests were used to
test whether the diagnostic requirements of Cox proportional risk
model were met. Log-rank test was used to test the difference of
survival distribution Statistical analysis was performed using SPSS
23.0 (IBM Corp) and R language software 4.2.2 (r-project.org). P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient selection
Of 287 patients initially screened, a total of 86
patients met the inclusion criteria. Of these, 40 patients
underwent splenectomy and 46 received drugs to increase their
leukocytes and PLTs. Of patients that were excluded from the study,
eight did not obtain a final diagnosis, 10 presented with other
vascular diseases, including aneurysms and arteriovenous
malformations, 13 were complicated with autoimmune hepatitis,
systemic lupus erythematosus and vasculitis, eight had meningioma,
glioma and other central nervous system tumour disease, 45 were
excluded due to insufficient medical records and 117 had
insufficient clinical follow-up time.
Baseline population and preoperative
data
Compared with the non-surgical group, the patients
with hypersplenism of WD in the surgical group were older and had
fewer women, a shorter course of disease, fewer patients with
preoperative time-weighted Child-Pugh scores of grades A and B and
higher preoperative time-weighted modified Young scores, but the
difference was not statistically significant (Table I). Preoperative time-weighted PLT
level may associated with splenectomy.
 | Table IBaseline demographic and clinical data
of patients with hypersplenism of Wilson's disease. |
Table I
Baseline demographic and clinical data
of patients with hypersplenism of Wilson's disease.
| Characteristic | Splenectomy,
n=40 | Non-splenectomy,
n=46 | P-value | Standard mean
difference |
|---|
| Mean age, years | 22.33±7.23 | 21.50±8.43 | 0.630 | 0.105 |
| Female (%) | 16.00 (40.00) | 20.00 (43.48) | 0.915 | 0.071 |
| Mean disease course,
years | 7.66±2.95 | 7.78±3.97 | 0.870 | 0.036 |
| Mean time-weighted
platelet count before surgery, x109/l | 49.49±6.19 | 51.47±6.38 | 0.150 | 0.315 |
| Time-weighted
Child-Pugh score before surgery | | | | |
|
Class A
(%) | 13.00 (32.50) | 15.00 (32.61) | 1.000 | 0.020 |
|
Class B
(%) | 27.00 (67.50) | 31.00 (67.39) | | |
| Mean time-weighted
modified Young score before surgery | 12.3±4.33 | 11.85±3.92 | 0.613 | 0.109 |
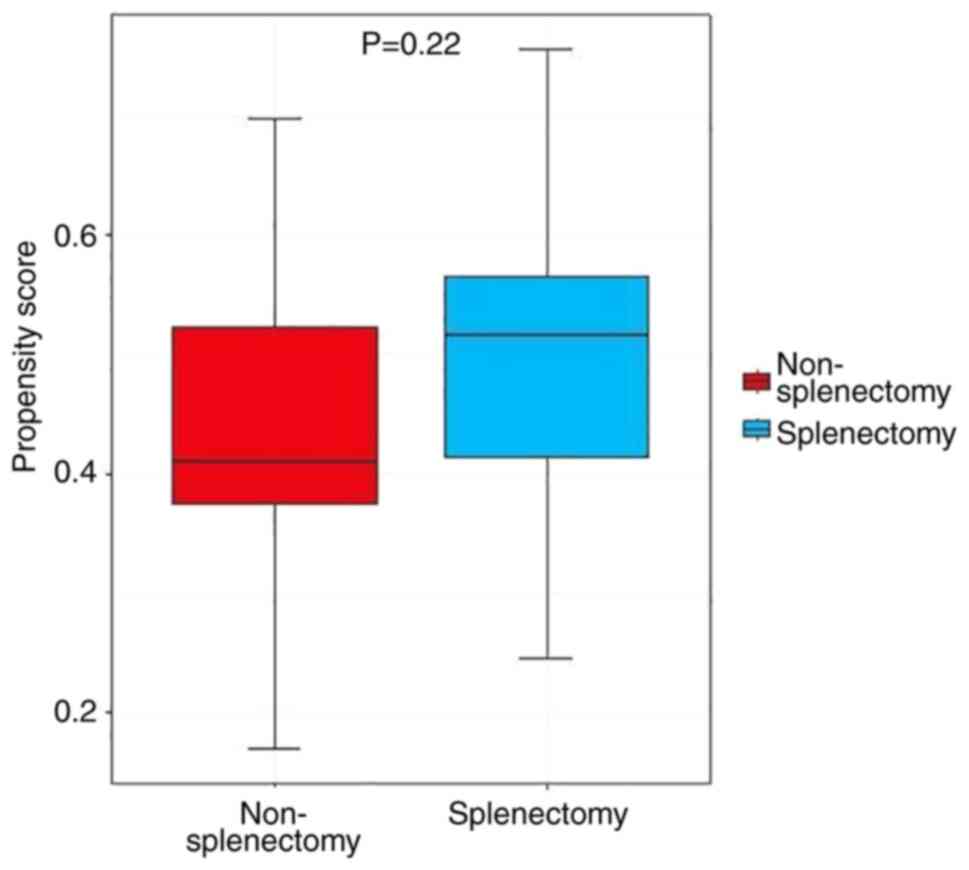
Predicting the probability of
propensity score model
Baseline and preoperative data of the cases were
sorted and propensity score model was used to predict the
probability of splenectomy in patients with hypersplenism of WD.
The median propensity score of patients in the surgical group was
0.517 [interquartile range (IQR), 0.412-0.566], while that in the
non-surgical group was 0.410 (IQR, 0.373-0.524). In addition, the
difference in distribution of data between the two groups was not
statistically significant (Fig.
1).
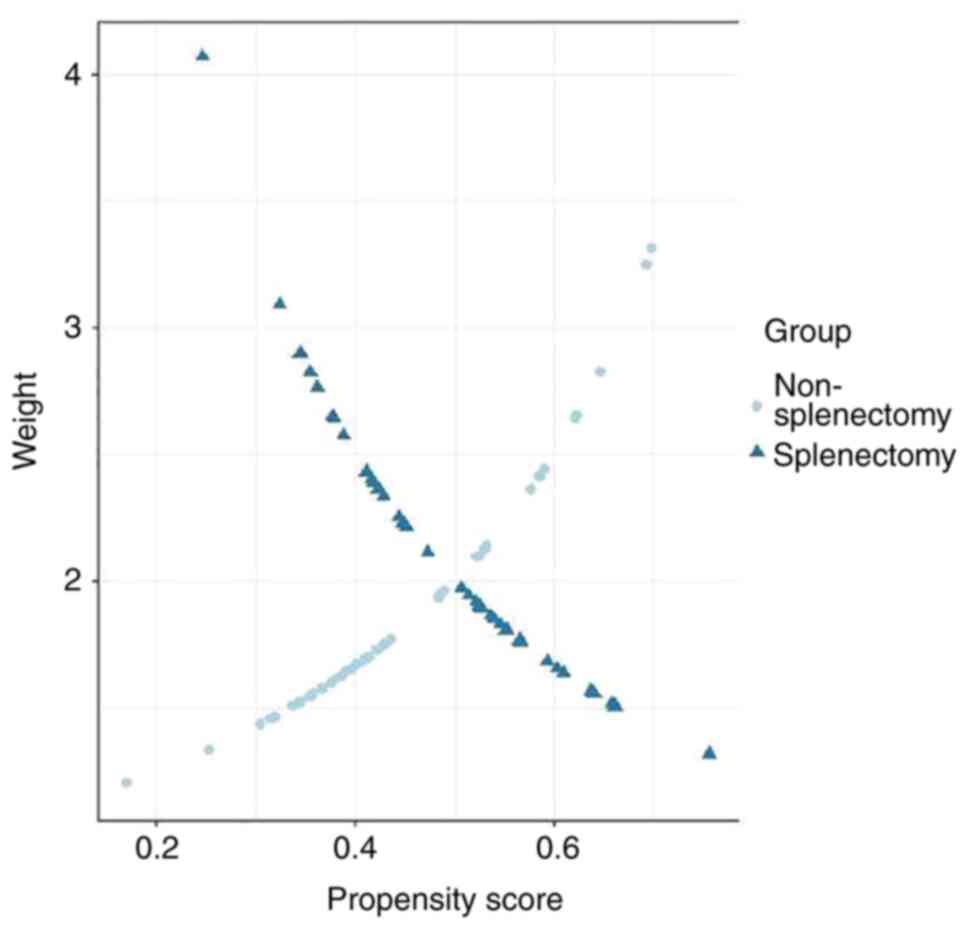
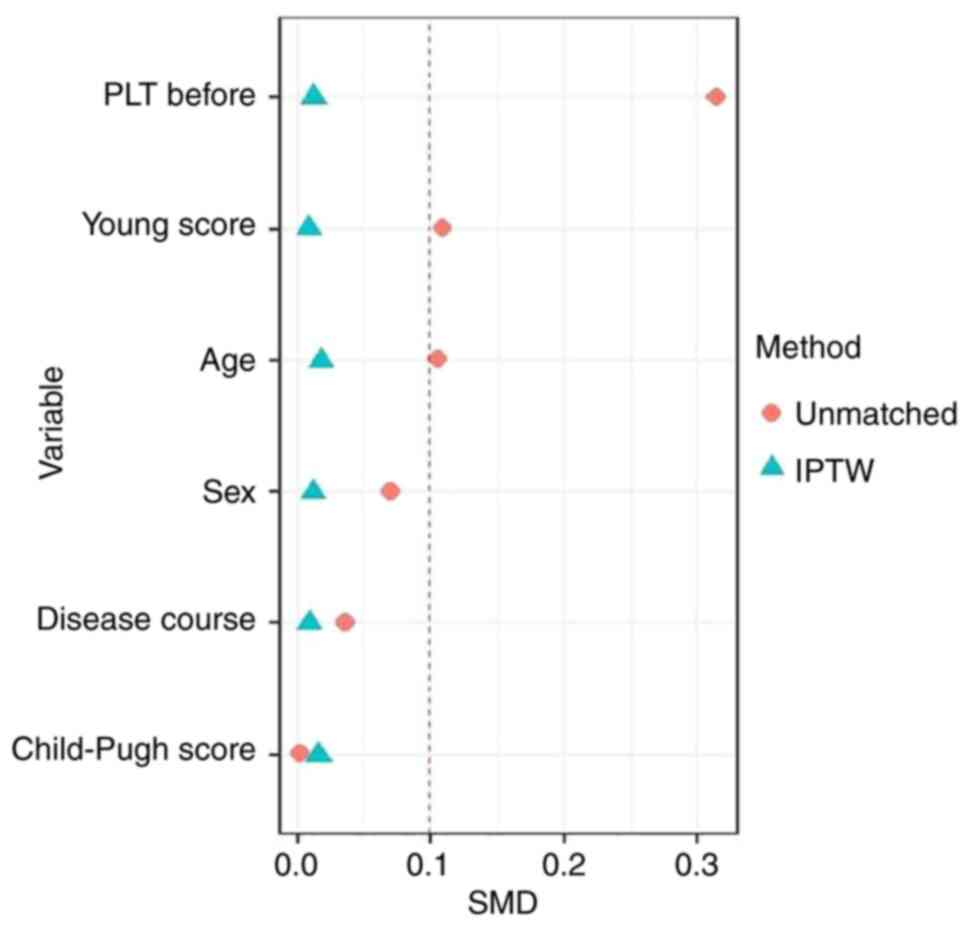
Inverse probability weighting to
correct confounding factors
According to the propensity scores, data with
inverse probability were weighted. The two groups had similar
distribution of weights, suggesting that when both groups had a
high prediction probability, the weight of the splenectomy group
was lower than that of the non-splenectomy group; by contrast, when
the two groups had the same weight, the prediction probability of
the splenectomy group was lower than that of the non-splenectomy
group (Fig. 2). Analysis of
weighted data suggested that the confounding factors of baseline
and preoperative data were corrected (P>0.05; standard mean
difference <10%; Table II);
thus, the covariate imbalance caused by non-randomization was
adjusted (Fig. 3).
 | Table IIBaseline demographic and clinical
data of patients with Wilson's disease complicated with
hypersplenism after inverse probability weighting. |
Table II
Baseline demographic and clinical
data of patients with Wilson's disease complicated with
hypersplenism after inverse probability weighting.
| Characteristic | Splenectomy,
n=40 | Non-splenectomy,
n=46 | P-value | Standard mean
difference |
|---|
| Mean age,
years | 21.91±7.21 | 21.77±8.33 | 0.934 | 0.018 |
| Female (%) | 35.30 (41.20) | 36.00 (41.80) | 0.958 | 0.012 |
| Disease course,
years | 7.71 (3.08) | 7.68 (3.77) | 0.966 | 0.009 |
| Mean time-weighted
platelet count before surgery, x109/l | 50.42± 6.08 | 50.34±6.84 | 0.957 | 0.012 |
| Time-weighted
Child-Pugh score before surgery | | | | |
|
Class A
(%) | 27.10 (31.60) | 28.00 (32.40) | 0.943 | 0.016 |
|
Class B
(%) | 58.60 (68.40) | 58.30 (67.60) | | |
| Mean time-weighted
modified Young score before surgery | 12.01±4.34 | 11.97±3.98 | 0.969 | 0.009 |
Postoperative indices by inverse
probability weighting
Changes in time-weighted PLT and Child-Pugh and
modified Young scale scores of patients with hypersplenism of WD
were compared before and after weighting. Significant differences
were found both before and after adjustment in time-weighted PLT
levels in patients with hypersplenism of WD [before adjustment,
odds ratio (OR)=0.011; 95% CI, 0.0015-0.049; after adjustment,
OR=0.010; 95% CI, 0.0013-0.047; P<0.001; Table III], suggesting these were
relatively stable. Time-weighted Child-Pugh scores also suggested
significant differences (before adjustment, OR=0.0682; 95% CI,
0.018-0.211; after adjustment, OR=0.0684; 95% CI, 0.018-0.207;
P<0.001; Table III).
Furthermore, the data of the time-weighted modified Young scale
scores also indicated that splenectomy was not associated with the
scores of the modified Young scale (before adjustment, OR=0.293;
95% CI, 0.073-1.013; after adjustment, OR=0.294; 95% CI,
0.074-1.001; P>0.05; Table
III).
 | Table IIITime-weighted platelet count and
Child-Pugh and modified Young scale score in patients with
hypersplenism of Wilson's disease. |
Table III
Time-weighted platelet count and
Child-Pugh and modified Young scale score in patients with
hypersplenism of Wilson's disease.
| Characteristic | Splenectomy,
n=40 | Non-splenectomy,
n=46 | Adjusted difference
(95% CI) |
|---|
| Mean time-weighted
platelet count before surgery, x109/l | 141±32.56 | 49.27±6.58 | 0.010
(0.001-0.047) |
| Time-weighted
Child-Pugh score before surgery | | | 0.070
(0.023-0.212) |
|
Class A
(%) | 31.00 (77.50) | 13.00 (28.30) | |
|
Class B
(%) | 9.00 (22.50) | 33.00 (71.70) | |
| Mean time-weighted
modified Young scores before surgery | 10.85±5.56 | 10.98±3.69 | 0.290
(0.071-1.001) |
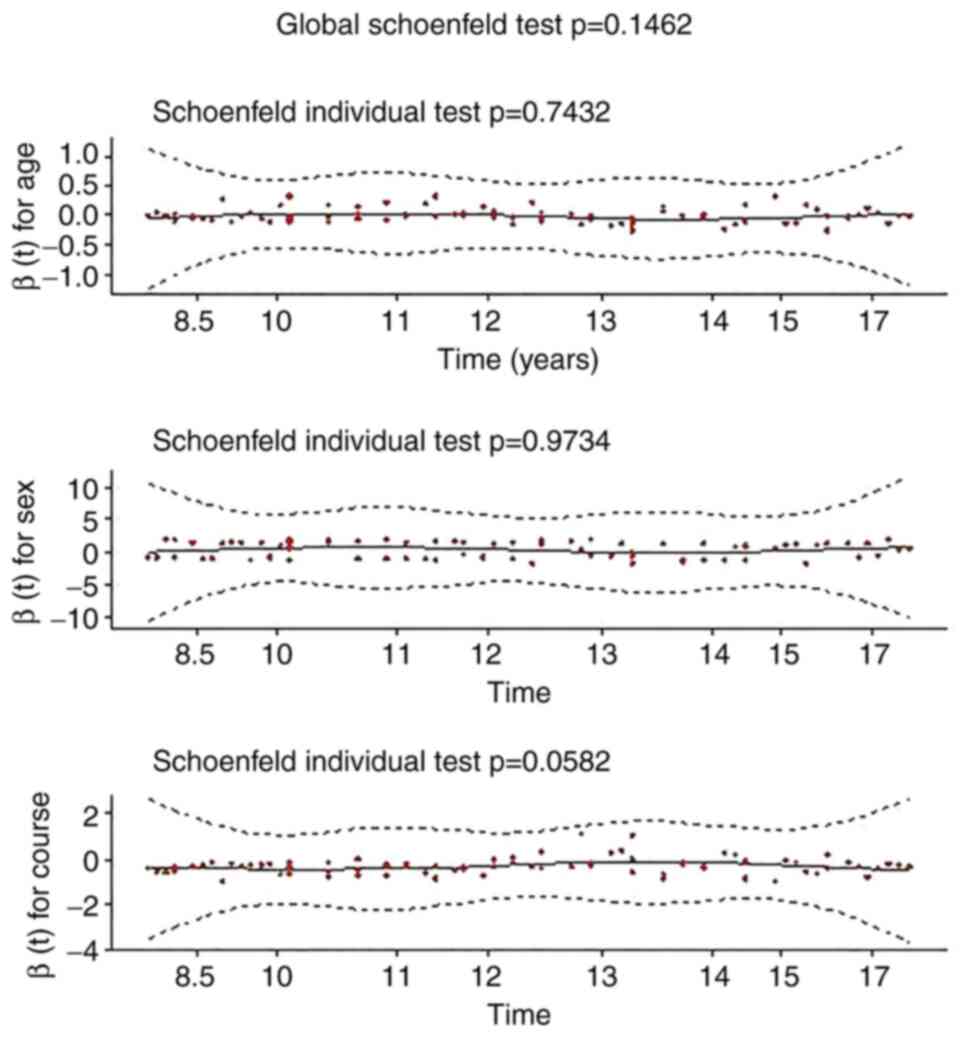
Cox proportional hazard model to
predict the effect of splenectomy on the survival and prognosis of
patients with hypersplenism
Statistical analysis on the survival time and status
of patients with hypersplenism was performed. After weighting,
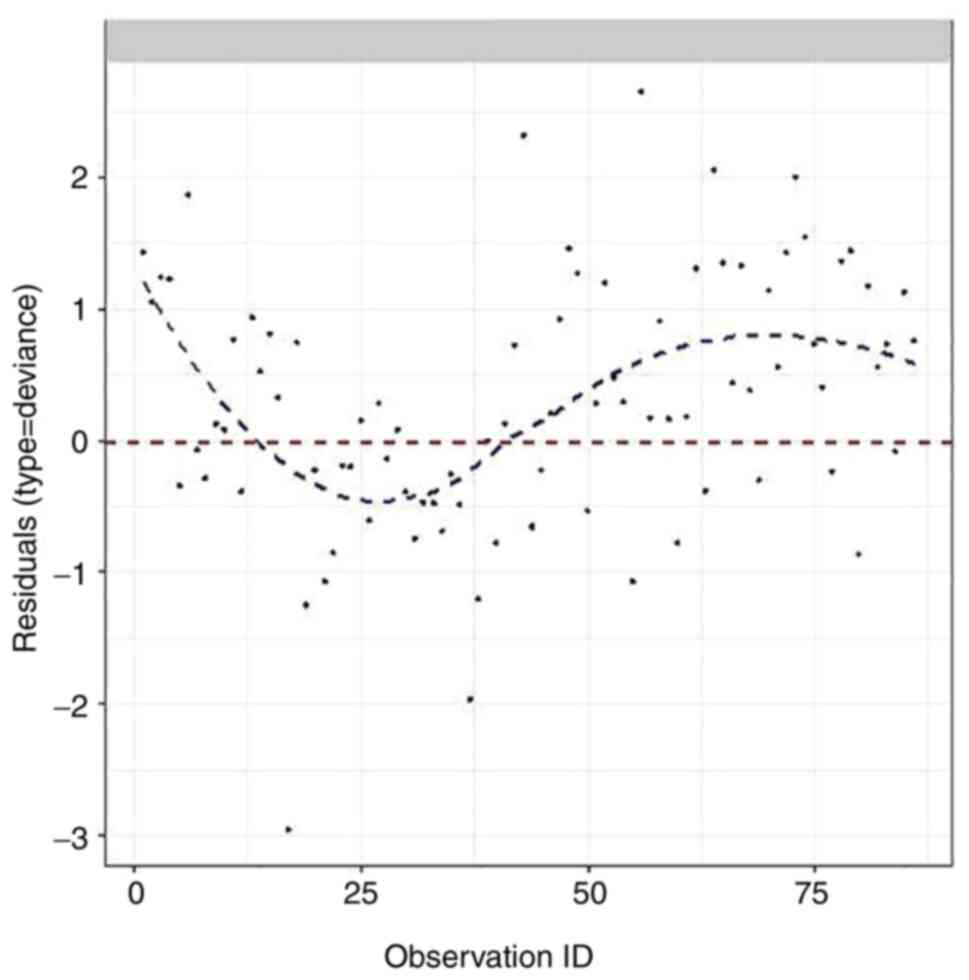
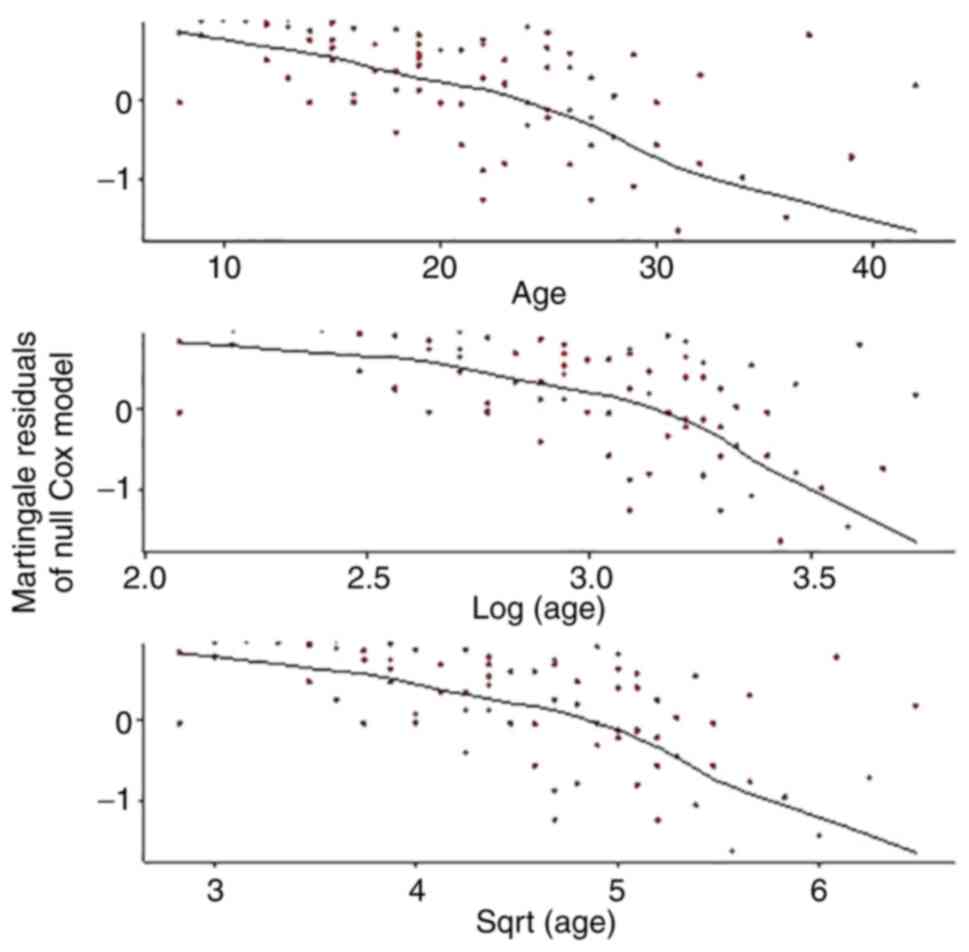
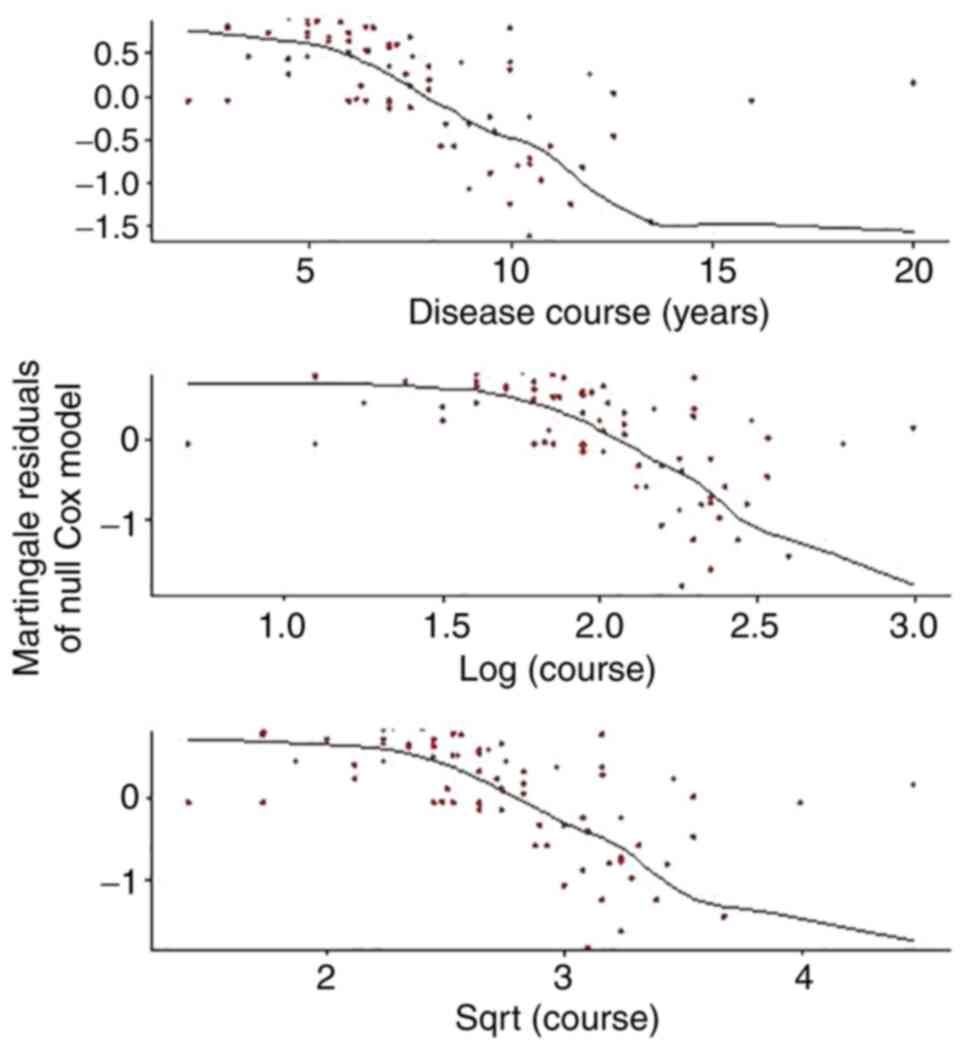
Schoenfeld, deviance and martingale residual tests were performed.
The Schoenfeld residual diagram (Fig.
4; P>0.05) suggested that the model as a whole met the
requirements of the equal scale model. The deviance residual
diagram (Fig. 5) demonstrated that
the residual values of each point were evenly distributed at ~0 and
relatively symmetric, suggesting that the assumption that the model
conforms to the risk proportional model was met. Moreover, the
martingale residual diagram Figs.
6 and 7) revealed that
continuous covariates had degree of non-linearity. Therefore, the
residual tests indicated that the data met the diagnostic
requirements of the Cox proportional hazard model.
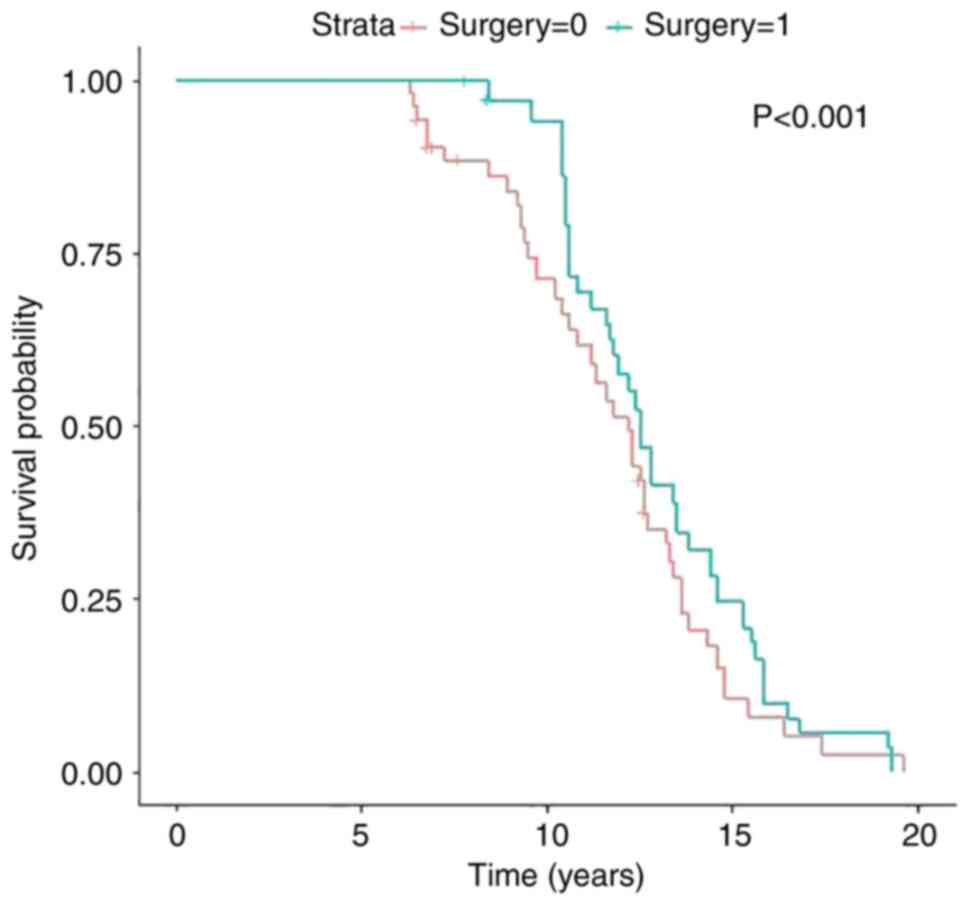
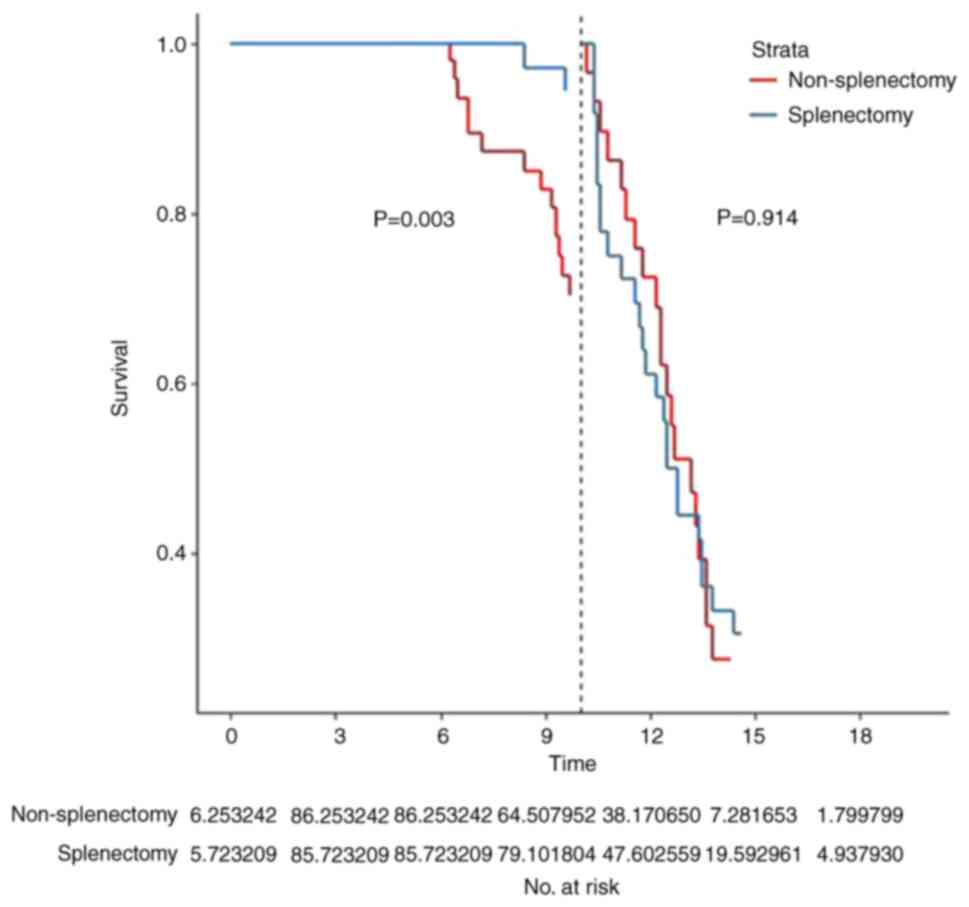
There was a mean survival time of 11.2±3.15 years
with a 10-year survival rate of 64.97% in the non-splenectomy and
12.9±2.62 years with a 10-year survival rate of 92.11% in the
splenectomy group, which was statistically significant (P<0.05).
Cox proportional hazard model prediction before and after weighting
indicated that, compared with that in the non-splenectomy group,
splenectomy decreased risk of death by 71% [before adjustment,
hazard ratio (HR)=0.296; 95% CI, 0.1725-0.5061; after adjustment,
HR=0.295; 95% CI, 0.1872-0.4635] and the results were relatively
stable and statistically significant (P<0.001). Kaplan-Meier
curve predicted by the Cox proportional hazard model after
adjusting the baseline data is shown in Fig. 8. Due to crossover of survival
curves at a later stage, the data were analysed using landmark
analysis. Splenectomy decreased the death rate by 84% within 10
years (HR=0.158; 95% Cl, 0.0198-1.2545; P<0.05) compared with
that in the non-splenectomy group, but there was no significant
difference between the two groups after 10 years (HR=0.445; 95% Cl,
0.2463-0.8022; P>0.05; Fig.
9).
Discussion
All cases in the present study came from the First
Affiliated Hospital of Anhui University of Traditional Chinese
Medicine. Since 1973, the aforementioned hospital has taken the
lead in conducting experimental and clinical research on WD for
>40 years in China. Through in-depth research and exploration of
the aetiology and pathology, diagnostic typing, treatment and
efficacy evaluation of WD, a suitable diagnosis and treatment
system for WD have gradually been formed. As a leading WD diagnosis
and treatment centre, the aforementioned hospital has gathered
patients globally and receives thousands of outpatients and
inpatients with WD every year. Therefore, the present study has a
sufficient and reliable source of cases.
The present retrospective cohort study assessed the
effect of splenectomy on PLT, liver function, psychoneurological
symptoms and survival prognosis in patients with hypersplenism of
WD using the inverse probability weighting method of propensity
score. Splenectomy significantly improved the PLT and liver
function levels but did not affect the psychoneurological symptoms.
In addition, the mean survival time and 10-year survival rate of
non-splenectomy group were lower than those of splenectomy group.
After adjusting for confounding factors, the risk of death in the
surgical group was reduced by 71% compared with that in the
non-surgical group. Splenectomy decreased death rate by 84%
compared with that in the non-splenectomy group within 10 years but
there was no significant difference after 10 years.
Splenectomy, as an effective method to improve
hypersplenism, is now widely used in diseases such as liver
cirrhosis caused by viral hepatitis and liver cancer following
hematopoietic stem cell transplantation and liver transplantation
(24-26).
As an important immune organ, the spleen is involved in the
immediate immune response to blood-derived antigens. However, for
patients with severe liver disease, portal vein blood circulation
disorder causes deposition of splenic blood flow, resulting in
splenomegaly and hypersplenism, which further leads to
complications, such as haemopenia, aggravated coagulation
dysfunction, bleeding and infection (27).
Although there are few studies on the mechanism
changes in liver function in patients with hypersplenism of WD,
research has shown that splenectomy significantly improves blood
cell count and liver function in patients with liver cancer, viral
hepatitis and liver cirrhosis (28-30).
Studies have also shown that splenectomy in the early stage of
liver fibrosis blocks rapid deployment of monocytes to the liver,
thus reducing the inflammatory response and delaying the
progression of early liver fibrosis in mice (31,32).
In addition, splenectomy enhances the mitotic cycle of hepatocytes
by reducing the release of anti-hepatocyte proliferation factor
TGF-β1 from the spleen, thus promoting proliferation of hepatocytes
(33). Therefore, improvement in
liver function in patients with hypersplenism following splenectomy
may be related to the reduction in the inflammatory response,
promotion of hepatocyte proliferation, antifibrosis (34,35)
and improvement in haemodynamics (36). Splenectomy can significantly
increase the PLT count of patients (8,9),
even when preoperative PLT levels are ≤30x109/l, without
affecting the operation and postoperative functional recovery of
the patient (10). The liver
function is also significantly improved after splenectomy
(including aspartate transaminase, alanine aminotransferase, total
bilirubin, albumin, prothrombin time), while prothrombin time is
shorter compared with that before the procedure (11). Even for children with hypersplenism
of WD or patients with moderate to severe hypersplenism, a
splenectomy yields improved curative effects and safety with
sufficient perioperative treatment (12,13).
The results of the present study also suggested that splenectomy
improves the levels of PLT and liver function in patients with
hypersplenism of WD.
Improvement of neurological function in patients
undergoing splenectomy is controversial. An early study reported
that splenectomy to treat WD can aggravate neurological dysfunction
(6). By contrast, another study
suggested that splenectomy would improve the neurological function
of patients following surgery (8).
However, to the best of our knowledge, there are few studies on the
neurological function of patients with WD after splenectomy. The
current study found that the overall neurological function scores
in both the splenectomy and non-splenectomy groups decreased but
this was not associated with whether the operation was performed or
not. The decline in overall neurological function score may be
associated with long-term standardized intravenous or oral
anti-copper treatment before and after the operation.
A topical literature review has reported that
splenectomy may increase the risk of complications such as
bleeding, infection, splenic portal vein thrombosis, pulmonary
embolism and disseminated intravascular coagulation and may be
associated with a postoperative hypercoagulable state, PLT
activation, endothelial dysfunction and activation and lipid mass
spectrum changes (37). In the
present study, two patients died in the splenectomy group, whereas
six patients died in the non-splenectomy group. The causes of death
in the operation group included liver coma induced by surgical
anaesthetics and aggravation of postoperative infection. Patients
in the non-splenectomy group died due to the progression of the
disease, including upper gastrointestinal bleeding caused by
oesophageal and gastric varices, spontaneous cerebral haemorrhage
caused by further deterioration of coagulation function,
hepatorenal syndrome and hepatic encephalopathy caused by further
deterioration of liver function. Patients with hypersplenism of WD
often have a decrease in blood cells, aggravation of liver
fibrosis, and cirrhosis with the progression of the disease,
accompanied by abnormalities in transaminase and protein and
coagulation factor synthesis disorders (38). The long-term use of anti-copper
drugs further aggravates abnormalities in clinical markers
(39,40). In this regard, splenectomy not only
decreases the mortality of patients with haemopenia and mild to
moderate abnormal liver function but also ensures long-term copper
excretion treatment (7).
Therefore, combined with the results of the present study,
splenectomy improves the survival of patients by decreasing portal
vein pressure in the short term, alleviating the negative effects
of hypersplenism and thus improving PLT count and liver function.
However, with the further progression of WD cirrhosis, the increase
of long-term venous reflux pressure causes vascular rupture and
bleeding. In addition, the continuous deterioration of liver
function can cause liver failure, hepatic encephalopathy and coma.
This may be the reason splenectomy cannot reverse the poor
prognosis of the disease in the long term.
As a retrospective clinical study, the present
sample size was small due to doubtful diagnosis, lack of data and
insufficient follow-up. In addition, due to the limited clinical
data, the method of assessing the efficacy of was based on few
clinical data, such as serological indicators and scale scores, and
more objective alternative biomarkers should be evaluated.
Therefore, a larger sample size should be included and an improved
experimental design should be used when designing future
prospective studies to improve reliability.
The present research suggested that splenectomy can
improve the survival and prognosis of patients with WD However, a
longer follow-up time and a larger sample size are still needed to
evaluate the clinical value of splenectomy in the treatment of
hypersplenism in patients with WD.
Acknowledgements
The authors would like to thank Dr Qingsheng Yu (The
First Affiliated Hospital of Anhui University of Traditional
Chinese Medicine, China) for performing splenectomy.
Funding
Funding: The present study was supported by the National Natural
Science Foundation of China (grant no. 82274493).
Availability of data and materials
The datasets generated and/or analysed during the
current study are available from the corresponding author on
reasonable request.
Authors' contributions
HC and XW wrote the manuscript. HC and JZ conceived
the research. HC and XW obtained the data and analyzed them. JZ
revised the manuscript for intellectual content and obtained
funding. JZ and DX provided general supervision. DX participated in
data analysis and manuscript revision. HC and XW confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The protocol of this clinical study is in full
compliance with the ethical principles of the Declaration of
Helsinki, as well as good clinical practice guidelines and
applicable local regulatory requirements. This study was approved
by The Institutional Review Committee of The First Affiliated
Hospital of Anhui University of Traditional Chinese Medicine
(approval no. 2022AH-25; Date of Approval, 12/03/2022).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Compston A: Progressive lenticular
degeneration: A familial nervous disease associated with cirrhosis
of the liver, by S. A. Kinnier Wilson, (from the national hospital,
and the laboratory of the national hospital, queen square, London)
brain 1912: 34; 295-509. Brain. 132:1997–2001. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Strickland GT, Chang NK and Beckner WM:
Hypersplenism in Wilson's disease. Gut. 13:220–224. 1972.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Poujois A and Woimant F: Wilson's disease:
A 2017 update. Clin Res Hepatol Gastroenterol. 42:512–520.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zeng DB, Di L, Zhang RC, Guo QL, Duan BW,
Jia CY, Chen F, Lin DD, Zang YJ and Lu SC: The effect of
splenectomy on the reversal of cirrhosis: A prospective study.
Gastroenterol Res Pract. 2019(5459427)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rabiner AM, et al: Hepatolenticular
degeneration following splenectomy, interrelationship of the
reticuloendothlial system and central nervous system. Arch Int Med,
1941.
|
|
6
|
Sternlieb I, Scheinberg IH and Walshe JM:
Bleeding oesophageal varices in patients with Wilson's disease.
Lancet. 1:638–641. 1970.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cai YL, Yang XT and Yang RM: Discussion on
splenectomy in hepatolenticular degeneration (with 42 cases
report). J Clin Neurol. 6:131–133. 1993.(In Chinese).
|
|
8
|
Li LY, Yang WM, Chen HZ, Wu YH, Fang X,
Zhang J, Wang Z, Han YS and Wang Y: Successful splenectomy for
hypersplenism in Wilson's disease: A single center experience from
China. PLoS One. 10(e0124569)2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Guo BB, Yu QS, Sheng Y, et al: Platelet
changes and its clinical significance in patients with
hepatolenticular degeneration complicated with hypersplenism before
and after splenectomy. J Liaoning Univ Tradit Chin Med. 21:134–137.
2019.(In Chinese).
|
|
10
|
Yang W, Yu QS and Pan JF: Effect of
platelet level on operation and prognosis in patients with
hepatolenticular degeneration and hypersplenism undergoing
splenectomy. Shaanxi Med J. 49:1403–1407. 2020.(In Chinese).
|
|
11
|
Wei FS, Yu QS, Pan JF, Shen Y, Zhang Q,
Wang Z and Hunag L: Effect of splenectomy on liver function in
patients with hepatolenticular degeneration and hypersplenism.
Guangxi Med. 42:2475–2491. 2020.(In Chinese).
|
|
12
|
Wang XM, Zhang FZ, Yu QS, et al:
Plenectomy in the treatment of hepatolenticular degeneration with
hypersplenism in children. J Hepatobiliary Pancreat Surg.
19:217–219. 2007.(In Chinese).
|
|
13
|
Qian Y, Pan JF, Huang L, Wang Z, Jing W
and Yu Q: Hepatolenticular degeneration with moderate to severe
hypersplenism Analysis of related factors of complications after
splenectomy. Shandong Med J. 62:63–66. 2022.(In Chinese).
|
|
14
|
Carry PM, Vanderlinden LA, Dong F, Buckner
T, Litkowski E, Vigers T, Norris JM and Kechris K: Inverse
probability weighting is an effective method to address selection
bias during the analysis of high dimensional data. Genet Epidemiol.
45:593–603. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yang RM: Hepatolenticular degeneration.
9th Edition. People's Health Publishing House, Beijing, 2015.
|
|
16
|
Rosencrantz R and Schilsky M: Wilson
disease: Pathogenesis and clinical considerations in diagnosis and
treatment. Semin Liver Dis. 31:245–259. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ferenci P, Caca K, Loudianos G,
Mieli-Vergani G, Tanner S, Sternlieb I, Schilsky M, Cox D and Berr
F: Diagnosis and phenotypic classification of Wilson disease. Liver
Int. 23:139–142. 2003.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hou Y and Sun GX: Diagnostic
classification criteria and clinical significance of hypersplenism
in portal hypertension. J Mod Integr Tradit Chin West Med.
18(3603)2009.(In Chinese).
|
|
19
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649.
1973.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zhou XX, Qin HL, He RX, Chen DB, Wu C,
Feng L, Li XH and Liang XL: Clinical characteristics of patients
with delayed hepatolenticular degeneration. Zhonghua Nei Ke Za Zhi.
58:501–507. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
21
|
Mansournia MA and Altman DG: Inverse
probability weighting. BMJ. 352(i189)2016.PubMed/NCBI View
Article : Google Scholar
|
|
22
|
Rubin DB: Estimating causal effects from
large data sets using propensity scores. Ann Intern Med.
127:757–763. 1997.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Liu L, Nevo D, Nishihara R, Cao Y, Song M,
Twombly TS, Chan AT, Giovannucci EL, VanderWeele TJ, Wang M and
Ogino S: Utility of inverse probability weighting in molecular
pathological epidemiology. Eur J Epidemiol. 33:381–392.
2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yoshizumi T, Itoh S, Shimokawa M, Inokuchi
S, Harada N, Takeishi K, Mano Y, Yoshiya S, Kurihara T, Nagao Y, et
al: Simultaneous splenectomy improves outcomes after adult living
donor liver transplantation. J Hepatol. 74:372–379. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Brauer DL, Rapoport AP, Yanovich S and
Akpek G: Splenectomy as a measure to treat prolonged
post-transplant cytopenia associated with hypersplenism. Bone
Marrow Transplant. 49:717–719. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Inagaki Y, Sugimoto K, Shiraki K, Tameda
M, Kusagawa S, Nojiri K, Ogura S, Yamamoto N, Takei Y, Ito M, et
al: The long-term effects of splenectomy and subsequent interferon
therapy in patients with HCV-related liver cirrhosis. Mol Med Rep.
9:487–492. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
McKenzie CV, Colonne CK, Yeo JH and Fraser
ST: Splenomegaly: Pathophysiological bases and therapeutic options.
Int J Biochem Cell Biol. 94:40–43. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Schwabl P, Seeland BA, Riedl F, Schubert
TL, Königshofer P, Brusilovskaya K, Petrenko O, Hofer B, Schiefer
AI, Trauner M, et al: Splenectomy ameliorates portal pressure and
anemia in animal models of cirrhotic and non-cirrhotic portal
hypertension. Adv Med Sci. 67:154–162. 2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Yamamoto N, Okano K, Oshima M, Akamoto S,
Fujiwara M, Tani J, Miyoshi H, Yoneyama H, Masaki T and Suzuki Y:
Laparoscopic splenectomy for patients with liver cirrhosis:
Improvement of liver function in patients with Child-Pugh class B.
Surgery. 158:1538–1544. 2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Shi XB, Feng JK, Wang JH and Jiang XQ:
Does splenectomy significantly improve the prognosis of
hepatocellular carcinoma patients with hypersplenism? A systematic
review and meta-analysis. Ann Transl Med. 9(641)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Wang MJ, Ling WW, Wang H, Meng LW, Cai H
and Peng B: Non-invasive evaluation of liver stiffness after
splenectomy in rabbits with CCl4-induced liver fibrosis.
World J Gastroenterol. 22:10166–10179. 2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Wang Y, Guo X, Jiao G, Luo L, Zhou L,
Zhang J and Wang B: Splenectomy promotes macrophage polarization in
a mouse model of concanavalin A-(ConA-) Induced liver fibrosis.
Biomed Res Int. 2019(5756189)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Elchaninov AV, Fatkhudinov TK, Vishnyakova
PA, Nikitina MP, Lokhonina AV, Makarov AV, Arutyunyan IV,
Kananykhina EY, Poltavets AS, Butov KR, et al: Molecular mechanisms
of splenectomy-induced hepatocyte proliferation. PLoS One.
15(e0233767)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Liang QS, Xie JG, Yu C, Feng Z, Ma J,
Zhang Y, Wang D, Lu J, Zhuang R and Yin J: Splenectomy improves
liver fibrosis via tumor necrosis factor superfamily 14 (LIGHT)
through the JNK/TGF-β1 signaling pathway. Exp Mol Med. 53:393–406.
2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zheng Z, Wang H, Li L, Zhang S, Zhang C,
Zhang H, Ji F, Liu X, Zhu K, Kong G and Li Z: Splenectomy enhances
the Ly6Clow phenotype in hepatic macrophages by
activating the ERK1/2 pathway during liver fibrosis. Int
Immunopharmacol. 86(106762)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Zeng DB, Di L, Guo QL, Ding J, Zhao XF and
Lu SC: Splenectomy with portoazygous disconnection for correction
of systemic hemodynamic disorders in hepatic cirrhosis patients
with portal hypertension: A prospective single-center cohort study.
Can J Gastroenterol Hepatol. 2020(8893119)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Weledji EP: Benefits and risks of
splenectomy. Int J Surg. 12:113–119. 2014.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Członkowska A, Litwin T, Dusek P, Ferenci
P, Lutsenko S, Medici V, Rybakowski JK, Weiss KH and Schilsky ML:
Wilson disease. Nat Rev Dis Primers. 4(21)2018.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Grasedyck K: D-penicillamine-side effects,
pathogenesis and decreasing the risks. Z Rheumatol. 47 (Suppl
1):S17–S19. 1988.PubMed/NCBI(In German).
|
|
40
|
Langan MN and Thomas P:
Penicillamine-induced liver disease. Am J Gastroenterol.
82:1318–1319. 1987.PubMed/NCBI
|