|
1
|
Ahuja CS, Wilson JR, Nori S, Kotter MRN,
Druschel C, Curt A and Fehlings MG: Traumatic spinal cord injury.
Nat Rev Dis Primers. 3(17018)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Silva NA, Sousa N, Reis RL and Salgado AJ:
From basics to clinical: A comprehensive review on spinal cord
injury. Prog Neurobiol. 114:25–57. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
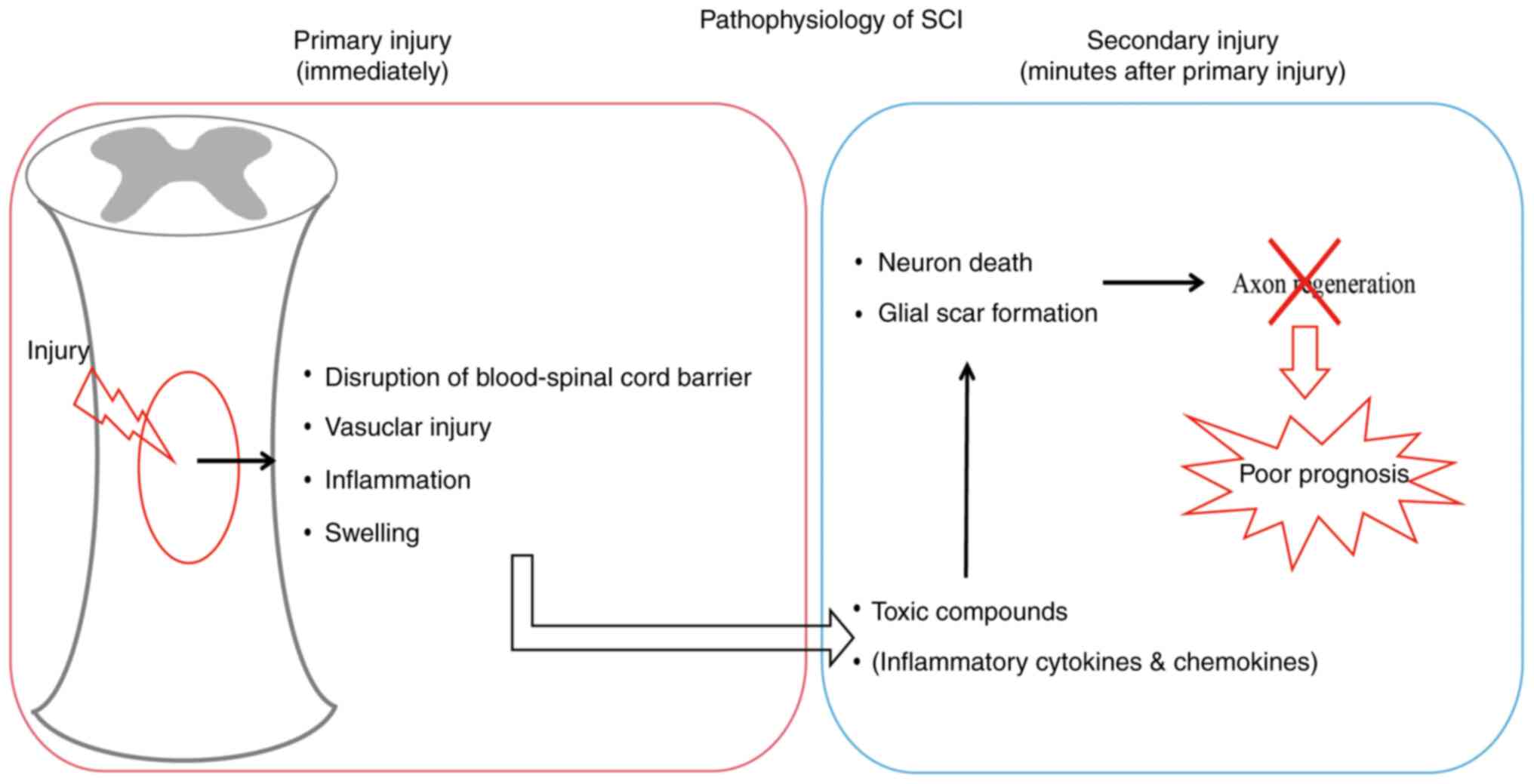
Vismara I, Papa S, Veneruso V, Mauri E,
Mariani A, De Paola M, Affatato R, Rossetti A, Sponchioni M,
Moscatelli D, et al: Selective modulation of A1 astrocytes by
drug-loaded nano-structured gel in spinal cord injury. ACS Nano.
14:360–371. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
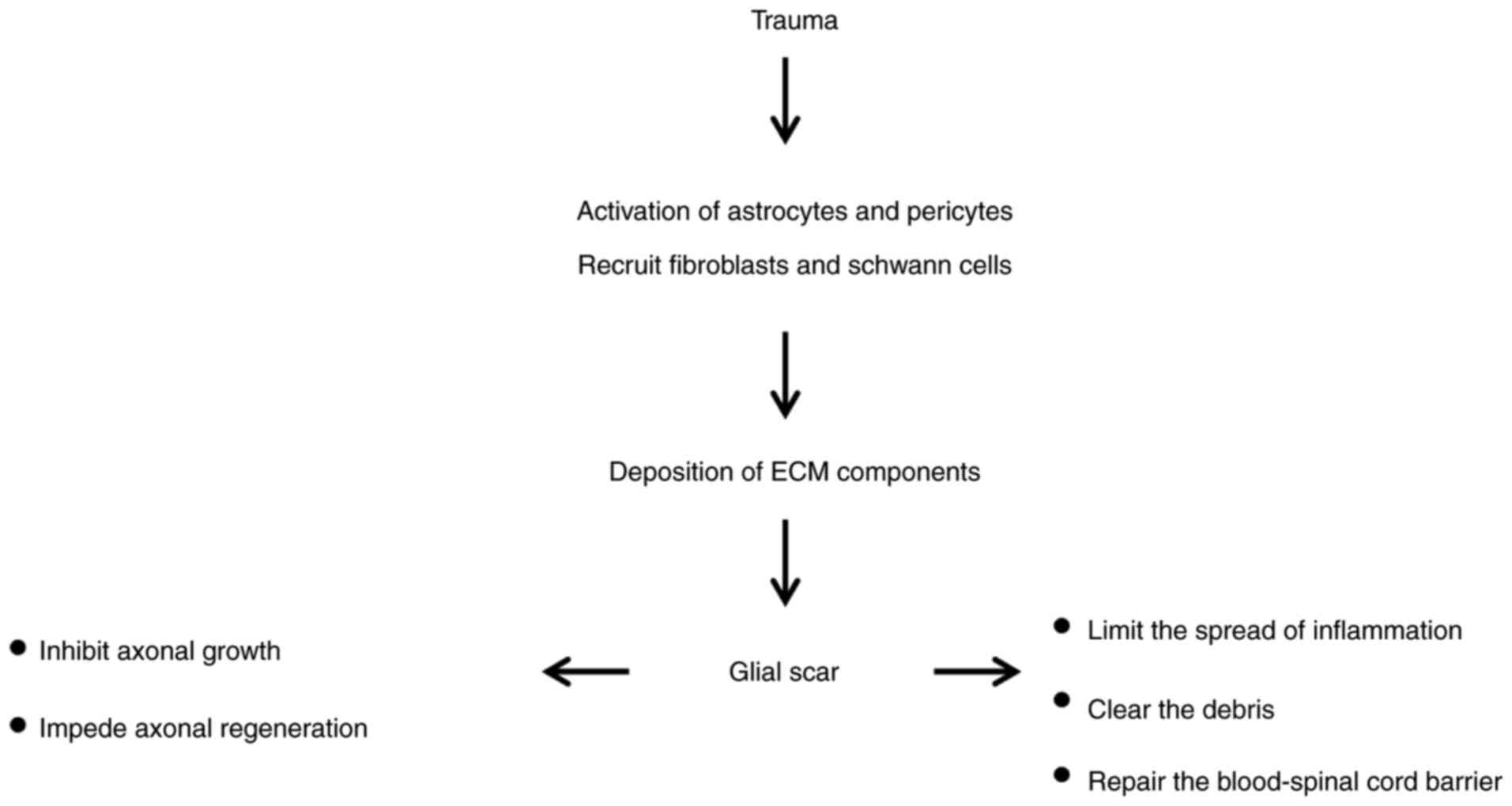
Huang X, Gu YK, Cheng XY and Su ZD:
Astrocytes as therapeutic targets after spinal cord injury. Sheng
Li Xue Bao. 69:794–804. 2017.PubMed/NCBI(In Chinese).
|
|
5
|
Erlich S, Alexandrovich A, Shohami E and
Pinkas-Kramarski R: Rapamycin is a neuroprotective treatment for
traumatic brain injury. Neurobiol Dis. 26:86–93. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wu Q, Li YL, Ning GZ, Feng SQ, Chu TC, Li
Y, Hao Y and Wu QL: Epidemiology of traumatic cervical spinal cord
injury in Tianjin, China. Spinal Cord. 50:740–744. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
McKinley WO, Seel RT and Hardman JT:
Nontraumatic spinal cord injury: Incidence, epidemiology, and
functional outcome. Arch Phys Med Rehabil. 80:619–623.
1999.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lu P, Wang Y, Graham L, McHale K, Gao M,
Wu D, Brock J, Blesch A, Rosenzweig ES, Havton LA, et al:
Long-distance growth and connectivity of neural stem cells after
severe spinal cord injury. Cell. 150:1264–1273. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mar FM, Simões AR, Rodrigo IS and Sousa
MM: Inhibitory injury signaling represses axon regeneration after
dorsal root injury. Mol Neurobiol. 53:4596–4605. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Prinz M and Priller J: The role of
peripheral immune cells in the CNS in steady state and disease. Nat
Neurosci. 20:136–144. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
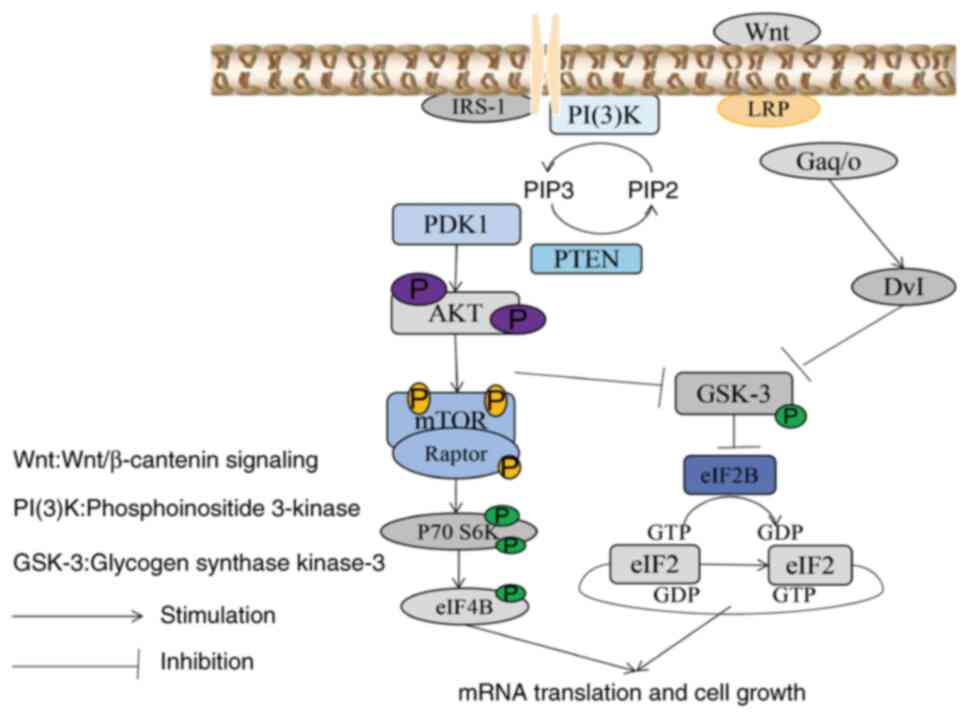
11
|
Kim YS, Choi J and Yoon BE: Neuron-glia
interactions in neurodevelopmental disorders. Cells.
9(2176)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pellerin L, Bouzier-Sore AK, Aubert A,
Serres S, Merle M, Costalat R and Magistretti PJ:
Activity-dependent regulation of energy metabolism by astrocytes:
An update. Glia. 55:1251–1262. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Taveggia C: Schwann cells-axon interaction
in myelination. Curr Opin Neurobiol. 39:24–29. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Casano AM and Peri F: Microglia:
Multitasking specialists of the brain. Dev Cell. 32:469–477.
2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Norenberg MD, Smith J and Marcillo A: The
pathology of human spinal cord injury: Defining the problems. J
Neurotrauma. 21:429–440. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sofroniew MV: Molecular dissection of
reactive astrogliosis and glial scar formation. Trends Neurosci.
32:638–647. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Alizadeh A, Dyck SM and Karimi-Abdolrezaee
S: Traumatic spinal cord injury: An overview of pathophysiology,
models and acute injury mechanisms. Front Neurol.
10(282)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wasner G, Naleschinski D and Baron R: A
role for peripheral afferents in the pathophysiology and treatment
of at-level neuropathic pain in spinal cord injury? A case report.
Pain. 131:219–225. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Anjum A, Yazid MD, Fauzi Daud M, Idris J,
Ng AMH, Selvi Naicker A, Ismail OHR, Athi Kumar RK and Lokanathan
Y: Spinal cord injury: Pathophysiology, multimolecular
interactions, and underlying recovery mechanisms. Int J Mol Sci.
21(7533)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nickel M and Gu C: Regulation of central
nervous system myelination in higher brain functions. Neural Plast.
2018(6436453)2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Schwartz G and Fehlings MG: Secondary
injury mechanisms of spinal cord trauma: A novel therapeutic
approach for the management of secondary pathophysiology with the
sodium channel blocker riluzole. Prog Brain Res. 137:177–190.
2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhang Y, Al Mamun A, Yuan Y, Lu Q, Xiong
J, Yang S, Wu C, Wu Y and Wang J: Acute spinal cord injury:
Pathophysiology and pharmacological intervention (Review). Mol Med
Rep. 23(417)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sharma HS, Patnaik R, Sharma A, Sjöquist
PO and Lafuente JV: Silicon dioxide nanoparticles (SiO2, 40-50 nm)
exacerbate pathophysiology of traumatic spinal cord injury and
deteriorate functional outcome in the rat. An experimental study
using pharmacological and morphological approaches. J Nanosci
Nanotechnol. 9:4970–4980. 2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Dimitrijevic MR, Danner SM and Mayr W:
Neurocontrol of movement in humans with spinal cord injury. Artif
Organs. 39:823–833. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhang JX, Wang R, Xi J, Shen L, Zhu AY, Qi
Q, Wang QY, Zhang LJ, Wang FC, Lü HZ and Hu JG: Morroniside
protects SK-N-SH human neuroblastoma cells against H2O2-induced
damage. Int J Mol Med. 39:603–612. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Leal-Filho MB: Spinal cord injury: From
inflammation to glial scar. Surg Neurol Int. 2(112)2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yang T, Xing L, Yu W, Cai Y, Cui S and
Chen G: Astrocytic reprogramming combined with rehabilitation
strategy improves recovery from spinal cord injury. FASEB J.
34:15504–15515. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lee-Liu D, Edwards-Faret G, Tapia VS and
Larraín J: Spinal cord regeneration: Lessons for mammals from
non-mammalian vertebrates. Genesis. 51:529–544. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Yılmaz T and Kaptanoğlu E: Current and
future medical therapeutic strategies for the functional repair of
spinal cord injury. World J Orthop. 6:42–55. 2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ahuja CS, Nori S, Tetreault L, Wilson J,
Kwon B, Harrop J, Choi D and Fehlings MG: Traumatic spinal cord
injury-repair and regeneration. Neurosurgery. 80 (3S):S9–S22.
2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sabapathy V, Tharion G and Kumar S: Cell
therapy augments functional recovery subsequent to spinal cord
injury under experimental conditions. Stem Cells Int.
2015(132172)2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yousefifard M, Rahimi-Movaghar V,
Nasirinezhad F, Baikpour M, Safari S, Saadat S, Moghadas Jafari A,
Asady H, Razavi Tousi SM and Hosseini M: Neural stem/progenitor
cell transplantation for spinal cord injury treatment; A systematic
review and meta-analysis. Neuroscience. 322:377–397.
2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ide C and Kanekiyo K: Points regarding
cell transplantation for the treatment of spinal cord injury.
Neural Regen Res. 11:1046–1049. 2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Lin XY, Lai BQ, Zeng X, Che MT, Ling EA,
Wu W and Zeng YS: Cell transplantation and neuroengineering
approach for spinal cord injury treatment: A summary of current
laboratory findings and review of literature. Cell Transplant.
25:1425–1438. 2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Dumont CM, Margul DJ and Shea LD: Tissue
engineering approaches to modulate the inflammatory milieu
following spinal cord injury. Cells Tissues Organs. 202:52–66.
2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Raspa A, Pugliese R, Maleki M and Gelain
F: Recent therapeutic approaches for spinal cord injury. Biotechnol
Bioeng. 113:253–259. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Gradišnik L, Bošnjak R, Maver T and Velnar
T: Advanced bio-based polymers for astrocyte cell models. Materials
(Basel). 14(3664)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Orr MB and Gensel JC: Spinal cord injury
scarring and inflammation: Therapies targeting glial and
inflammatory responses. Neurotherapeutics. 15:541–553.
2018.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Beck KD, Nguyen HX, Galvan MD, Salazar DL,
Woodruff TM and Anderson AJ: Quantitative analysis of cellular
inflammation after traumatic spinal cord injury: Evidence for a
multiphasic inflammatory response in the acute to chronic
environment. Brain. 133:433–447. 2010.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Buss A, Pech K, Kakulas BA, Martin D,
Schoenen J, Noth J and Brook GA: Growth-modulating molecules are
associated with invading Schwann cells and not astrocytes in human
traumatic spinal cord injury. Brain. 130:940–953. 2007.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zhang SX, Huang F, Gates M and Holmberg
EG: Role of endogenous Schwann cells in tissue repair after spinal
cord injury. Neural Regen Res. 8:177–185. 2013.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Tran AP, Warren PM and Silver J: The
biology of regeneration failure and success after spinal cord
injury. Physiol Rev. 98:881–917. 2018.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Adams KL and Gallo V: The diversity and
disparity of the glial scar. Nat Neurosci. 21:9–15. 2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Pang QM, Chen SY, Xu QJ, Fu SP, Yang YC,
Zou WH, Zhang M, Liu J, Wan WH, Peng JC and Zhang T:
Neuroinflammation and scarring after spinal cord injury:
Therapeutic roles of MSCs on inflammation and glial scar. Front
Immunol. 12(751021)2021.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Silver J and Miller JH: Regeneration
beyond the glial scar. Nat Rev Neurosci. 5:146–156. 2004.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Bradbury EJ, Moon LD, Popat RJ, King VR,
Bennett GS, Patel PN, Fawcett JW and McMahon SB: Chondroitinase ABC
promotes functional recovery after spinal cord injury. Nature.
416:636–640. 2002.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Diaz Quiroz JF and Echeverri K: Spinal
cord regeneration: Where fish, frogs and salamanders lead the way,
can we follow? Biochem J. 451:353–364. 2013.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Okada S, Nakamura M, Katoh H, Miyao T,
Shimazaki T, Ishii K, Yamane J, Yoshimura A, Iwamoto Y, Toyama Y
and Okano H: Conditional ablation of Stat3 or Socs3 discloses a
dual role for reactive astrocytes after spinal cord injury. Nat
Med. 12:829–834. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
49
|
Herrmann JE, Imura T, Song B, Qi J, Ao Y,
Nguyen TK, Korsak RA, Takeda K, Akira S and Sofroniew MV: STAT3 is
a critical regulator of astrogliosis and scar formation after
spinal cord injury. J Neurosci. 28:7231–7243. 2008.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Sofroniew MV: Astrocyte barriers to
neurotoxic inflammation. Nat Rev Neurosci. 16:249–263.
2015.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Yang T, Dai Y, Chen G and Cui S:
Dissecting the dual role of the glial scar and scar-forming
astrocytes in spinal cord injury. Front Cell Neurosci.
14(78)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Sofroniew MV: Dissecting spinal cord
regeneration. Nature. 557:343–350. 2018.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Wang L, Pei S, Han L, Guo B, Li Y, Duan R,
Yao Y, Xue B, Chen X and Jia Y: Mesenchymal stem cell-derived
exosomes reduce A1 astrocytes via downregulation of phosphorylated
NFκB P65 subunit in spinal cord injury. Cell Physiol Biochem.
50:1535–1559. 2018.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Alvarez-Buylla A and Lim DA: For the long
run: Maintaining germinal niches in the adult brain. Neuron.
41:683–686. 2004.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Ming GL and Song H: Adult neurogenesis in
the mammalian brain: Significant answers and significant questions.
Neuron. 70:687–702. 2011.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Horner PJ, Power AE, Kempermann G, Kuhn
HG, Palmer TD, Winkler J, Thal LJ and Gage FH: Proliferation and
differentiation of progenitor cells throughout the intact adult rat
spinal cord. J Neurosci. 20:2218–2228. 2000.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Borst K, Dumas AA and Prinz M: Microglia:
Immune and non-immune functions. Immunity. 54:2194–2208.
2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Park JH, Cho JH, Ahn JH, Choi SY, Lee TK,
Lee JC, Shin BN, Hong S, Jeon YH, Kim YM, et al: Neuronal loss and
gliosis in the rat striatum subjected to 15 and 30 min of middle
cerebral artery occlusion. Metab Brain Dis. 33:775–784.
2018.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Lee Y, Lee SR, Choi SS, Yeo HG, Chang KT
and Lee HJ: Therapeutically targeting neuroinflammation and
microglia after acute ischemic stroke. Biomed Res Int.
2014(297241)2014.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Wolf SA, Boddeke HWGM and Kettenmann H:
Microglia in physiology and disease. Annu Rev Physiol. 79:619–643.
2017.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Savage JC, Carrier M and Tremblay MÈ:
Morphology of microglia across contexts of health and disease.
Methods Mol Biol. 2034:13–26. 2019.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Brown GC: Neuronal loss after stroke due
to microglial phagocytosis of stressed neurons. Int J Mol Sci.
22(13442)2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Mothe AJ and Tator CH: Proliferation,
migration, and differentiation of endogenous ependymal region
stem/progenitor cells following minimal spinal cord injury in the
adult rat. Neuroscience. 131:177–187. 2005.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Park JH, Kim DY, Sung IY, Choi GH, Jeon
MH, Kim KK and Jeon SR: Long-term results of spinal cord injury
therapy using mesenchymal stem cells derived from bone marrow in
humans. Neurosurgery. 70:1238–1247. 2012.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Lima C, Escada P, Pratas-Vital J, Branco
C, Arcangeli CA, Lazzeri G, Maia CA, Capucho C, Hasse-Ferreira A
and Peduzzi JD: Olfactory mucosal autografts and rehabilitation for
chronic traumatic spinal cord injury. Neurorehabil Neural Repair.
24:10–22. 2010.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Saberi H, Firouzi M, Habibi Z, Moshayedi
P, Aghayan HR, Arjmand B, Hosseini K, Razavi HE and Yekaninejad MS:
Safety of intramedullary Schwann cell transplantation for
postrehabilitation spinal cord injuries: 2-Year follow-up of 33
cases. J Neurosurg Spine. 15:515–525. 2011.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Ronaghi M, Erceg S, Moreno-Manzano V and
Stojkovic M: Challenges of stem cell therapy for spinal cord
injury: Human embryonic stem cells, endogenous neural stem cells,
or induced pluripotent stem cells? Stem Cells. 28:93–99.
2010.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Osaka M, Honmou O, Murakami T, Nonaka T,
Houkin K, Hamada H and Kocsis JD: Intravenous administration of
mesenchymal stem cells derived from bone marrow after contusive
spinal cord injury improves functional outcome. Brain Res.
1343:226–235. 2010.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Chhabra HS, Lima C, Sachdeva S, Mittal A,
Nigam V, Chaturvedi D, Arora M, Aggarwal A, Kapur R and Khan TAH:
Autologous olfactory [corrected] mucosal transplant in chronic
spinal cord injury: An Indian pilot study. Spinal Cord. 47:887–895.
2009.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Liu C, Chen Z, Chen Z, Zhang T and Lu Y:
Multiple tumor types may originate from bone marrow-derived cells.
Neoplasia. 8:716–724. 2006.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Tolar J, Nauta AJ, Osborn MJ, Panoskaltsis
Mortari A, McElmurry RT, Bell S, Xia L, Zhou N, Riddle M, Schroeder
TM, et al: Sarcoma derived from cultured mesenchymal stem cells.
Stem Cells. 25:371–379. 2007.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Wu Z, Parry M, Hou XY, Liu MH, Wang H,
Cain R, Pei ZF, Chen YC, Guo ZY, Abhijeet S and Chen G: Gene
therapy conversion of striatal astrocytes into GABAergic neurons in
mouse models of Huntington's disease. Nat Commun.
11(1105)2020.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Chen YC, Ma NX, Pei ZF, Wu Z, Do-Monte FH,
Keefe S, Yellin E, Chen MS, Yin JC, Lee G, et al: A NeuroD1
AAV-based gene therapy for functional brain repair after ischemic
injury through in vivo astrocyte-to-neuron conversion. Mol Ther.
28:217–234. 2020.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Li H and Chen G: In vivo reprogramming for
CNS repair: Regenerating neurons from endogenous glial cells.
Neuron. 91:728–738. 2016.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Guo Z, Zhang L, Wu Z, Chen Y, Wang F and
Chen G: In vivo direct reprogramming of reactive glial cells into
functional neurons after brain injury and in an Alzheimer's disease
model. Cell Stem Cell. 14:188–202. 2014.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Hemmings BA, Yellowlees D, Kernohan JC and
Cohen P: Purification of glycogen synthase kinase 3 from rabbit
skeletal muscle. Copurification with the activating factor (FA) of
the (Mg-ATP) dependent protein phosphatase. Eur J Biochem.
119:443–451. 1981.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Jope RS: Lithium and GSK-3: One inhibitor,
two inhibitory actions, multiple outcomes. Trends Pharmacol Sci.
24:441–443. 2003.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Hur EM and Zhou FQ: GSK3 signalling in
neural development. Nat Rev Neurosci. 11:539–551. 2010.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Force T and Woodgett JR: Unique and
overlapping functions of GSK-3 isoforms in cell differentiation and
proliferation and cardiovascular development. J Biol Chem.
284:9643–9647. 2009.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Grimes CA and Jope RS: CREB DNA binding
activity is inhibited by glycogen synthase kinase-3 beta and
facilitated by lithium. J Neurochem. 78:1219–1232. 2001.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Neal JW and Clipstone NA: Glycogen
synthase kinase-3 inhibits the DNA binding activity of NFATc. J
Biol Chem. 276:3666–3673. 2001.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Ma YC, Song MR, Park JP, Henry Ho HY, Hu
L, Kurtev MV, Zieg J, Ma Q, Pfaff SL and Greenberg ME: Regulation
of motor neuron specification by phosphorylation of neurogenin 2.
Neuron. 58:65–77. 2008.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Fuentealba LC, Eivers E, Ikeda A, Hurtado
C, Kuroda H, Pera EM and De Robertis EM: Integrating patterning
signals: Wnt/GSK3 regulates the duration of the BMP/Smad1 signal.
Cell. 131:980–993. 2007.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Kazi A, Xiang S, Yang H, Delitto D,
Trevino J, Jiang RHY, Ayaz M, Lawrence HR, Kennedy P and Sebti SM:
GSK3 suppression upregulates β-catenin and c-Myc to abrogate
KRas-dependent tumors. Nat Commun. 9(5154)2018.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Linding R, Jensen LJ, Ostheimer GJ, van
Vugt MA, Jørgensen C, Miron IM, Diella F, Colwill K, Taylor L,
Elder K, et al: Systematic discovery of in vivo phosphorylation
networks. Cell. 129:1415–1426. 2007.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Beurel E, Grieco SF and Jope RS: Glycogen
synthase kinase-3 (GSK3): Regulation, actions, and diseases.
Pharmacol Ther. 148:114–131. 2015.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Mancinelli R, Carpino G, Petrungaro S,
Mammola CL, Tomaipitinca L, Filippini A, Facchiano A, Ziparo E and
Giampietri C: Multifaceted roles of GSK-3 in cancer and
autophagy-related diseases. Oxid Med Cell Longev.
2017(4629495)2017.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Jaworski T, Banach-Kasper E and Gralec K:
GSK-3 β at the intersection of neuronal plasticity and
neurodegeneration. Neural Plast. 2019(4209475)2019.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Hernandez F, Lucas JJ and Avila J: GSK3
and tau: Two convergence points in Alzheimer's disease. J
Alzheimers Dis. 33 (Suppl 1):S141–S144. 2013.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Albeely AM, Ryan SD and Perreault ML:
Pathogenic feed-forward mechanisms in Alzheimer's and Parkinson's
disease converge on GSK-3. Brain Plast. 4:151–167. 2018.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Manduca JD, Thériault RK and Perreault ML:
Glycogen synthase kinase-3: The missing link to aberrant circuit
function in disorders of cognitive dysfunction? Pharmacol Res.
157(104819)2020.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Wu YY, Wang X, Tan L, Liu D, Liu XH, Wang
Q, Wang JZ and Zhu LQ: Lithium attenuates scopolamine-induced
memory deficits with inhibition of GSK-3β and preservation of
postsynaptic components. J Alzheimers Dis. 37:515–527.
2013.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Kozlovsky N, Belmaker RH and Agam G: Low
GSK-3 activity in frontal cortex of schizophrenic patients.
Schizophr Res. 52:101–105. 2001.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Kozlovsky N, Shanon-Weickert C,
Tomaskovic-Crook E, Kleinman JE, Belmaker RH and Agam G: Reduced
GSK-3beta mRNA levels in postmortem dorsolateral prefrontal cortex
of schizophrenic patients. J Neural Transm (Vienna). 111:1583–1592.
2004.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Besing RC, Rogers CO, Paul JR, Hablitz LM,
Johnson RL, McMahon LL and Gamble KL: GSK3 activity regulates
rhythms in hippocampal clock gene expression and synaptic
plasticity. Hippocampus. 27:890–898. 2017.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Mao Y, Ge X, Frank CL, Madison JM, Koehler
AN, Doud MK, Tassa C, Berry EM, Soda T, Singh KK, et al: Disrupted
in schizophrenia 1 regulates neuronal progenitor proliferation via
modulation of GSK3beta/beta-catenin signaling. Cell. 136:1017–1031.
2009.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Morales-Garcia JA, Luna-Medina R,
Alonso-Gil S, Sanz-Sancristobal M, Palomo V, Gil C, Santos A,
Martinez A and Perez-Castillo A: Glycogen synthase kinase 3
inhibition promotes adult hippocampal neurogenesis in vitro and in
vivo. ACS Chem Neurosci. 3:963–971. 2012.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Lange C, Mix E, Frahm J, Glass A, Müller
J, Schmitt O, Schmöle AC, Klemm K, Ortinau S, Hübner R, et al:
Small molecule GSK-3 inhibitors increase neurogenesis of human
neural progenitor cells. Neurosci Lett. 488:36–40. 2011.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Lie DC, Colamarino SA, Song HJ, Désiré L,
Mira H, Consiglio A, Lein ES, Jessberger S, Lansford H, Dearie AR
and Gage FH: Wnt signalling regulates adult hippocampal
neurogenesis. Nature. 437:1370–1375. 2005.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Wexler EM, Geschwind DH and Palmer TD:
Lithium regulates adult hippocampal progenitor development through
canonical Wnt pathway activation. Mol Psychiatry. 13:285–292.
2008.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Kim WY, Wang X, Wu Y, Doble BW, Patel S,
Woodgett JR and Snider WD: GSK-3 is a master regulator of neural
progenitor homeostasis. Nat Neurosci. 12:1390–1397. 2009.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Rashvand M, Danyali S and Manaheji H: The
potential role of glycogen synthase kinase-3β in neuropathy-induced
apoptosis in spinal cord. Basic Clin Neurosci. 11:15–30.
2020.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Bareiss SK, Dugan E and Brewer KL: PI3K
mediated activation of GSK-3β reduces at-level primary afferent
growth responses associated with excitotoxic spinal cord injury
dysesthesias. Mol Pain. 11(35)2015.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Rodriguez-Jimenez FJ, Vilches A,
Perez-Arago MA, Clemente E, Roman R, Leal J, Castro AA, Fustero S,
Moreno-Manzano V, Jendelova P, et al: Activation of neurogenesis in
multipotent stem cells cultured in vitro and in the spinal cord
tissue after severe injury by inhibition of glycogen synthase
kinase-3. Neurotherapeutics. 18:515–533. 2021.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Lei F, He W, Tian X, Zhou Q, Zheng L, Kang
J, Song Y and Feng D: GSK-3 inhibitor promotes neuronal cell
regeneration and functional recovery in a rat model of spinal cord
injury. Biomed Res Int. 2019(9628065)2019.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Zhang G, Lei F, Zhou Q, Feng D and Bai Y:
Combined application of Rho-ROCKII and GSK-3β inhibitors exerts an
improved protective effect on axonal regeneration in rats with
spinal cord injury. Mol Med Rep. 14:5180–5188. 2016.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Burgess S, Geddes J, Hawton K, Townsend E,
Jamison K and Goodwin G: Lithium for maintenance treatment of mood
disorders. Cochrane Database Syst Rev. (CD003013)2001.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Young W: Review of lithium effects on
brain and blood. Cell Transplant. 18:951–975. 2009.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Li B, Ren J, Yang L, Li X, Sun G and Xia
M: Lithium inhibits GSK3β activity via two different signaling
pathways in neurons after spinal cord injury. Neurochem Res.
43:848–856. 2018.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Pan Z, Oh J, Huang L, Zeng Z, Duan P, Li
Z, Yun Y, Kim J, Ha Y and Cao K: The combination of forskolin and
VPA increases gene expression efficiency to the
hypoxia/neuron-specific system. Ann Transl Med.
8(933)2020.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Li Z, Wu F, Zhang X, Chai Y, Chen D, Yang
Y, Xu K, Yin J, Li R, Shi H, et al: Valproate attenuates
endoplasmic reticulum stress-induced apoptosis in SH-SY5Y cells via
the AKT/GSK3β signaling pathway. Int J Mol Sci.
18(315)2017.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Zhou Y, Wang Z, Li J, Li X and Xiao J:
Fibroblast growth factors in the management of spinal cord injury.
J Cell Mol Med. 22:25–37. 2018.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Rabchevsky AG, Fugaccia I, Turner AF,
Blades DA, Mattson MP and Scheff SW: Basic fibroblast growth factor
(bFGF) enhances functional recovery following severe spinal cord
injury to the rat. Exp Neurol. 164:280–291. 2000.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Rabchevsky AG, Fugaccia I, Fletcher-Turner
A, Blades DA, Mattson MP and Scheff SW: Basic fibroblast growth
factor (bFGF) enhances tissue sparing and functional recovery
following moderate spinal cord injury. J Neurotrauma. 16:817–830.
1999.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Sisakht M, Khoshdel Z, Mahmoodazdeh A,
Shafiee SM and Takhshid MA: Adrenomedullin increases cAMP
accumulation and BDNF expression in rat DRG and spinal motor
neurons. Iran J Basic Med Sci. 24:978–985. 2021.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Fu J, Sun H, Wei H, Dong M, Zhang Y, Xu W,
Fang Y and Zhao J: Astaxanthin alleviates spinal cord
ischemia-reperfusion injury via activation of PI3K/Akt/GSK-3β
pathway in rats. J Orthop Surg Res. 15(275)2020.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Ding Y, Xia S, Fang H, Niu B and Chen Q:
Loureirin B attenuates insulin resistance in HepG2 cells by
regulating gluconeogenesis signaling pathway. Eur J Pharmacol.
910(174481)2021.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Shi S, Zhao Q, Ke C, Long S, Zhang F,
Zhang X, Li Y, Liu X, Hu H and Yin S: Loureirin B exerts its
immunosuppressive effects by inhibiting STIM1/Orai1 and
KV1.3 channels. Front Pharmacol.
12(685092)2021.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Wang Q, Cai H, Hu Z, Wu Y, Guo X, Li J,
Wang H, Liu Y, Liu Y, Xie L, et al: Loureirin B promotes axon
regeneration by inhibiting endoplasmic reticulum stress: Induced
mitochondrial dysfunction and regulating the Akt/GSK-3β pathway
after spinal cord injury. J Neurotrauma. 36:1949–1964.
2019.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Yousefifard M, Nasirinezhad F, Shardi
Manaheji H, Janzadeh A, Hosseini M and Keshavarz M: Human bone
marrow-derived and umbilical cord-derived mesenchymal stem cells
for alleviating neuropathic pain in a spinal cord injury model.
Stem Cell Res Ther. 7(36)2016.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Schieweck R, Schöneweiss EC, Harner M,
Rieger D, Illig C, Saccà B, Popper B and Kiebler MA: Pumilio2
promotes growth of mature neurons. Int J Mol Sci.
22(8998)2021.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Huang F, Gao T, Wang W, Wang L, Xie Y, Tai
C, Liu S, Cui Y and Wang B: Engineered basic fibroblast growth
factor-overexpressing human umbilical cord-derived mesenchymal stem
cells improve the proliferation and neuronal differentiation of
endogenous neural stem cells and functional recovery of spinal cord
injury by activating the PI3K-Akt-GSK-3β signaling pathway. Stem
Cell Res Ther. 12(468)2021.PubMed/NCBI View Article : Google Scholar
|
|
123
|
New PW, Lim TC, Hill ST and Brown DJ: A
survey of pain during rehabilitation after acute spinal cord
injury. Spinal Cord. 35:658–663. 1997.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Störmer S, Gerner HJ, Grüninger W,
Metzmacher K, Föllinger S, Wienke C, Aldinger W, Walker N,
Zimmermann M and Paeslack V: Chronic pain/dysaesthesiae in spinal
cord injury patients: Results of a multicentre study. Spinal Cord.
35:446–455. 1997.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Peng Z, Zha L, Yang M, Li Y, Guo X and
Feng Z: Effects of ghrelin on pGSK-3β and β-catenin expression when
protects against neuropathic pain behavior in rats challenged with
chronic constriction injury. Sci Rep. 9(14664)2019.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Sarveazad A, Janzadeh A, Taheripak G,
Dameni S, Yousefifard M and Nasirinezhad F: Co-administration of
human adipose-derived stem cells and low-level laser to alleviate
neuropathic pain after experimental spinal cord injury. Stem Cell
Res Ther. 10(183)2019.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Parkitna JR, Obara I, Wawrzczak-Bargiela
A, Makuch W, Przewlocka B and Przewlocki R: Effects of glycogen
synthase kinase 3beta and cyclin-dependent kinase 5 inhibitors on
morphine-induced analgesia and tolerance in rats. J Pharmacol Exp
Ther. 319:832–839. 2006.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Wang X, Lin C, Jin S, Wang Y, Peng Y and
Wang X: Cannabidiol alleviates neuroinflammation and attenuates
neuropathic pain via targeting FKBP5. Brain Behav Immun.
111:365–375. 2023.PubMed/NCBI View Article : Google Scholar
|
|
129
|
Xu W, Zhu M, Yuan S and Yu W: Spinal CXCL5
contributes to nerve injury-induced neuropathic pain via modulating
GSK-3β phosphorylation and activity in rats. Neurosci Lett.
634:52–59. 2016.PubMed/NCBI View Article : Google Scholar
|
|
130
|
Chen JY, Chu LW, Cheng KI, Hsieh SL, Juan
YS and Wu BN: Valproate reduces neuroinflammation and neuronal
death in a rat chronic constriction injury model. Sci Rep.
8(16457)2018.PubMed/NCBI View Article : Google Scholar
|
|
131
|
Cheng H, Zhang L, Xia F, Jin L, Liu S, Ren
H, Zhu C, Ji Q and Tang J: Astrocytic NDRG2 is critical in the
maintenance of neuropathic pain. Brain Behav Immun. 89:300–313.
2020.PubMed/NCBI View Article : Google Scholar
|