Introduction
Elderly and postmenopausal middle-aged women are
prone to osteoporosis, with a large amount of bone loss occurring
due to a decline in body function and bone microenvironment changes
(1). One of the hallmarks of the
disease is a loss of bone strength, which can lead to fractures
(2). Osteoporotic vertebral
compression fractures (OVCFs) are the most serious result of
osteoporosis (3,4). While most OVCFs are benign, some can
lead to serious morbidity and socioeconomic costs, as well as a
reduced quality of life and productivity in the growing elderly
population (5). Conservative
management (the patient should rest in bed and apply appropriate
medication to relieve pain; after the fracture has healed
initially, the patient should wear a brace and start to get out of
bed) and vertebral cemented augmentation (a technique for
strengthening a diseased vertebra by injecting bone cement into it)
are the two most common treatments for OVCF. In vertebral cement
augmentation, there are two mainstream minimally invasive surgical
procedures: Percutaneous vertebroplasty (PVP) (after the puncture,
bone cement was injected directly into the diseased vertebra) and
percutaneous kyphoplasty (PKP) (after the puncture was completed,
the bone cement was injected by balloon dilation) (6,7).
Following technological improvements and developments, PKP has been
recommended as an advanced method for treating OVCF (7). It has been demonstrated that PKP has
a potential advantage over PVP in restoring compressed vertebral
and spinal deformities without increasing the cement leakage rate
and fracture risk of adjacent segments (8). PKP involves two different surgical
approaches with either a unilateral or bilateral puncture. Certain
studies suggest that bilateral puncture PKP can make the sides of
the diseased vertebra symmetrical and evenly distribute the bone
cement in the compressed vertebral body by avoiding unevenly
applied force, thus it is more effective for the recovery of the
compressed vertebral body (9,10).
However, Steinmann et al (11) reported no significant differences
in the vertebral strength, stiffness or height recovery between
patients treated with unilateral or bilateral PKP. The present
study collected a large amount of retrospective research data and
evaluated the safety and efficacy of the two types of PKP for the
treatment of vertebral fractures caused by osteoporosis to guide
the selection of clinical surgical methods.
Materials and methods
Literature inclusion and exclusion
criteria
The literature inclusion criteria were as follows:
i) Study object: Patients with OVCFs; ii) intervention measures:
Unilateral approach; iii) control: Bilateral approach; iv) outcome
indicators: Operative time, cement injection, visual analog score
(VAS), Oswestry disability index (ODI), post-kyphotic angle (KPA),
height restoration rate and incidence of cement leakage; and v)
study design: Randomized controlled trials (RCTs) or non-RCTs. Only
studies published in English were included in the analysis. The
exclusion criteria were duplicate published studies, incomplete
studies, studies with incomplete or unavailable data, animal
testing, reviews and systematic reviews.
Search strategy
In the present meta-analysis, PubMed (https://pubmed.ncbi.nlm.nih.gov/), Embase
(https://www.embase.com/) and the Cochrane Library
(http://www.cochranelibrary.com) were
searched from the establishment of the databases to March 2023. In
addition, additional records were identified through other sources
(Reference lists of relevant studies). The search terms used were
as follows: [osteoporotic vertebral compression fracture
(Title/Abstract)] and [percutaneous kyphoplasty
(Title/Abstract)].
Literature screening and data
extraction
The literature searches, data screening and data
extraction were conducted by two researchers. Any questions or
disputes were addressed after consultation with a third party. The
extracted study contents included the author, publication year,
country, study design, sample size, sex, age, post-KPA status, mean
follow-up duration and outcome indicators.
Literature quality assessment
The quality of the studies was independently
assessed by two researchers (QZ and ZZ). The Cochrane
Collaboration's Risk of Bias Tool was used to assess literature
quality for RCTs (12), whereas
the Newcastle-Ottawa Scale (NOS) was used to evaluate cohort
studies (13). Disagreements were
addressed through consultation or deliberation by a third party
(GL). The meta-analysis was performed according to the reported and
relevant items in the meta-analysis checklist (the PRISMA
checklist), which are preferred for systematic evaluations
(14).
Data synthesis and statistical
analysis
All data were processed with the statistical
analysis software, STATA 15.1 (StataCorp LP) (15). Standardized mean difference (SMD)
with 95% confidence interval (CI) were used to analyze continuous
variables and odds ratio (OR) with 95% CI was used to analyze
categorical variables. A heterogeneity result of P>0.1 and
I2<50% indicated that all studies were homogeneous.
P<0.1 and I2>50% indicated that the studies
differed and a difference sensitivity analysis (conducted by
excluding each trial individually and then hen performing a
combined analysis of the remaining trials) was performed to
identify the sources of the difference. Subsequently, a
random-effects model was applied or a descriptive analysis was
conducted instead of a pooled analysis. Funnel plots and Egger's
test were used to investigate publication bias. P<0.05 was
considered to indicate a statistically significant difference.
Results
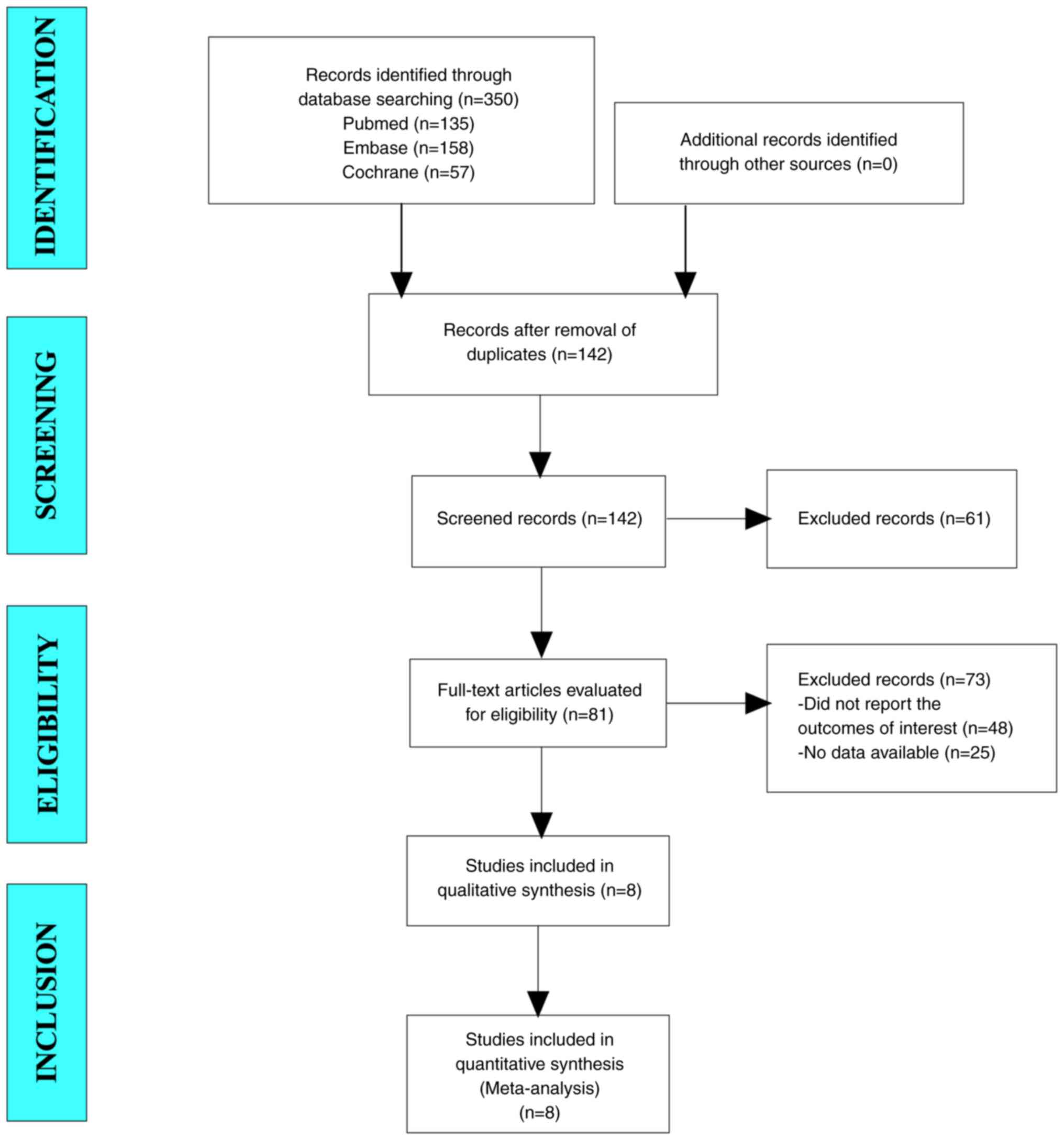
Literature search results
A total of 350 articles were collected for the
present study. After excluding duplicate studies, 142 articles
remained. From this pool, 81 articles were identified following
eligibility screening of titles and abstracts. After reading the
full text, 48 studies that didn't report the outcomes of interest
and 23 studies with no data available were excluded. Finally, eight
studies were included in the present meta-analysis (Fig. 1).
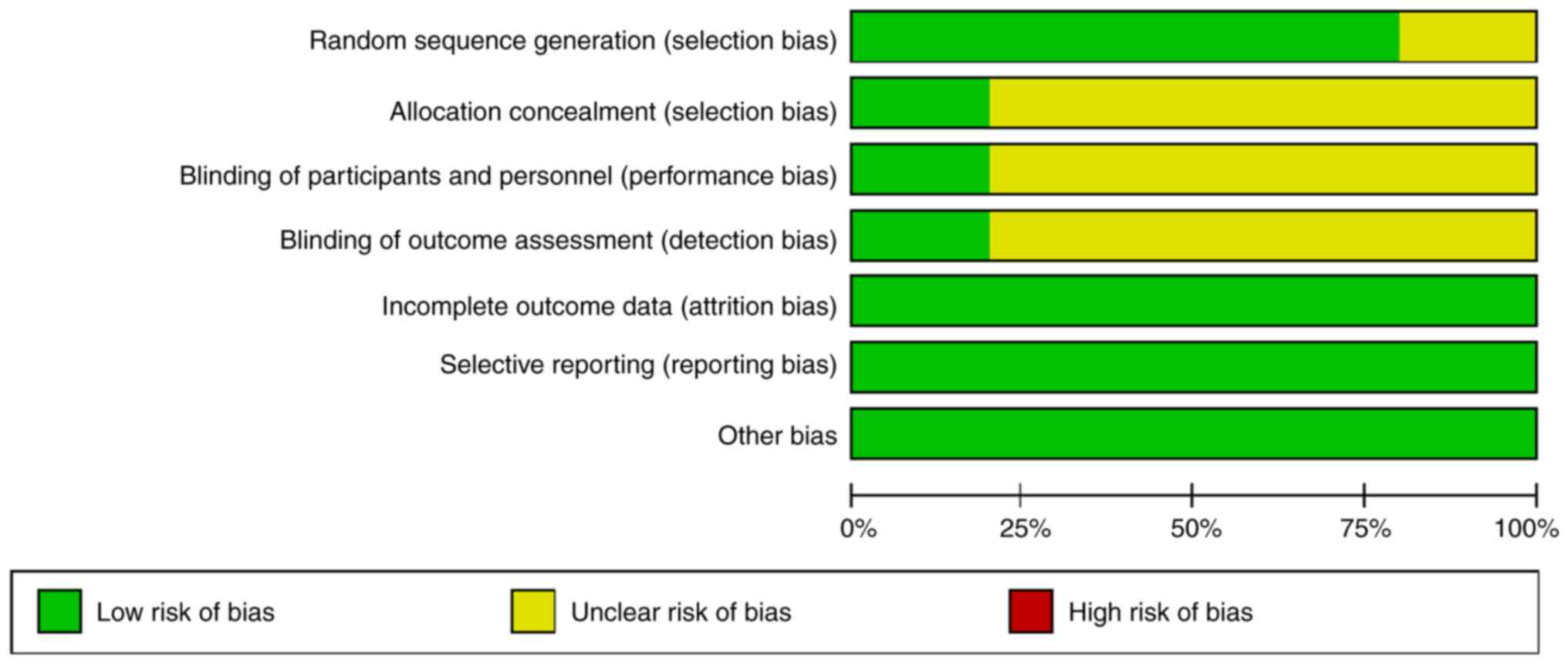
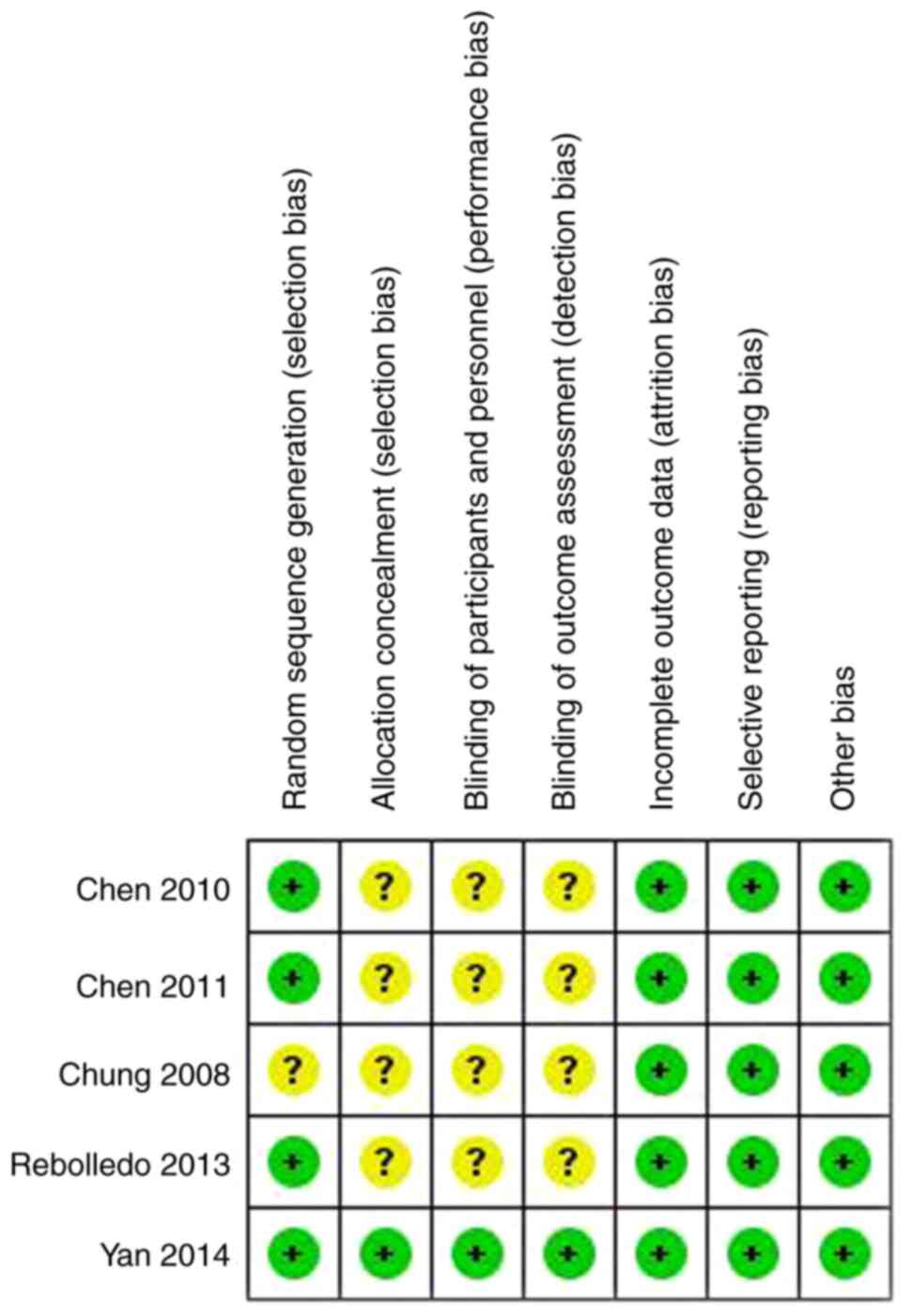
Baseline characteristics and quality
assessment of the included studies
A total of eight studies (five RCTs and three cohort
studies) were included in the present meta-analysis (16-23).
The patient sample size ranged from 44 to 309, with a total of 717
patients, including 356 in the unilateral group and 361 in the
bilateral group. A single study included patients from the USA and
all other studies included patients from Asia. The age range of
patients was 52-91 years, all of whom were aged. The NOS scores
(used for quality assessment) of the three cohort studies were all
>7 and met the quality requirements (Table I). The quality assessment results
of the five RCTs are shown in Figs.
2 and 3. The results indicated
that four studies included in the present review utilized random
sequences for patient group allocation and only one conducted
double-blinding (Figs. 2 and
3).
 | Table IBaseline characteristics and quality
assessment of the included studies. |
Table I
Baseline characteristics and quality
assessment of the included studies.
| | Sample size, n | Sex, no. of
male/female | Age, years [median
(range) or mean ± standard deviation] | Post-KPA (°) | Mean follow-up,
months | |
|---|
| First author,
year | Country | Study design | U | B | U | B | U | B | U | B | U | B | NOS score | (Refs.) |
|---|
| Chung et al,
2008 | South Korea | RCT | 24 | 28 | 2/22 | 1/27 | 66.8 (57-80) | 68.9 (57-83) | 17.6 (13-25) | 18.5 (12-27) | 17.8 | 16.6 | - | (16) |
| Chen et al,
2010 | China | RCT | 33 | 25 | - | - | 67.7±7.1 | 68.5±7.3 | - | - | - | - | - | (17) |
| Chen et al,
2011 | China | RCT | 24 | 25 | 4/20 | 4/21 | 70.4 (52-91) | 72.4 (54-87) | 24.3±13.7 | 27.3±12.1 | 31.8 | 35.2 | - | (18) |
| Wang et al,
2012 | China | Cohort | 31 | 31 | 13/18 | 17/14 | 68.3 (59-78) | 69.2 (62-79) | - | - | 16.7 | 15.9 | 7 | (19) |
| Rebolledo et
al, 2013 | USA | RCT | 23 | 21 | 4/19 | 2/19 | 78.7±7.8 | 79.3±6.5 | 26.5±10.3 | 24.0±9.9 | 12 | 12 | - | (20) |
| Yan et al,
2014 | China | RCT | 158 | 151 | 46/112 | 43/108 | 71.9±4.2 | 71.1±3.7 | 18.83±8.22 | 17.98±7.18 | 12 | 12 | - | (21) |
| Zhang et al,
2022 | China | Cohort | 29 | 38 | 10/19 | 12/26 | 73.6±5.7 | 74.1±4.9 | - | - | 17.1 | | 8 | (22) |
| Zhu et al,
2022 | China | Cohort | 34 | 42 | 5/29 | 8/34 | 70.1±6.8 | 71.4±8.7 | - | - | 16.6 | | 8 | (23) |
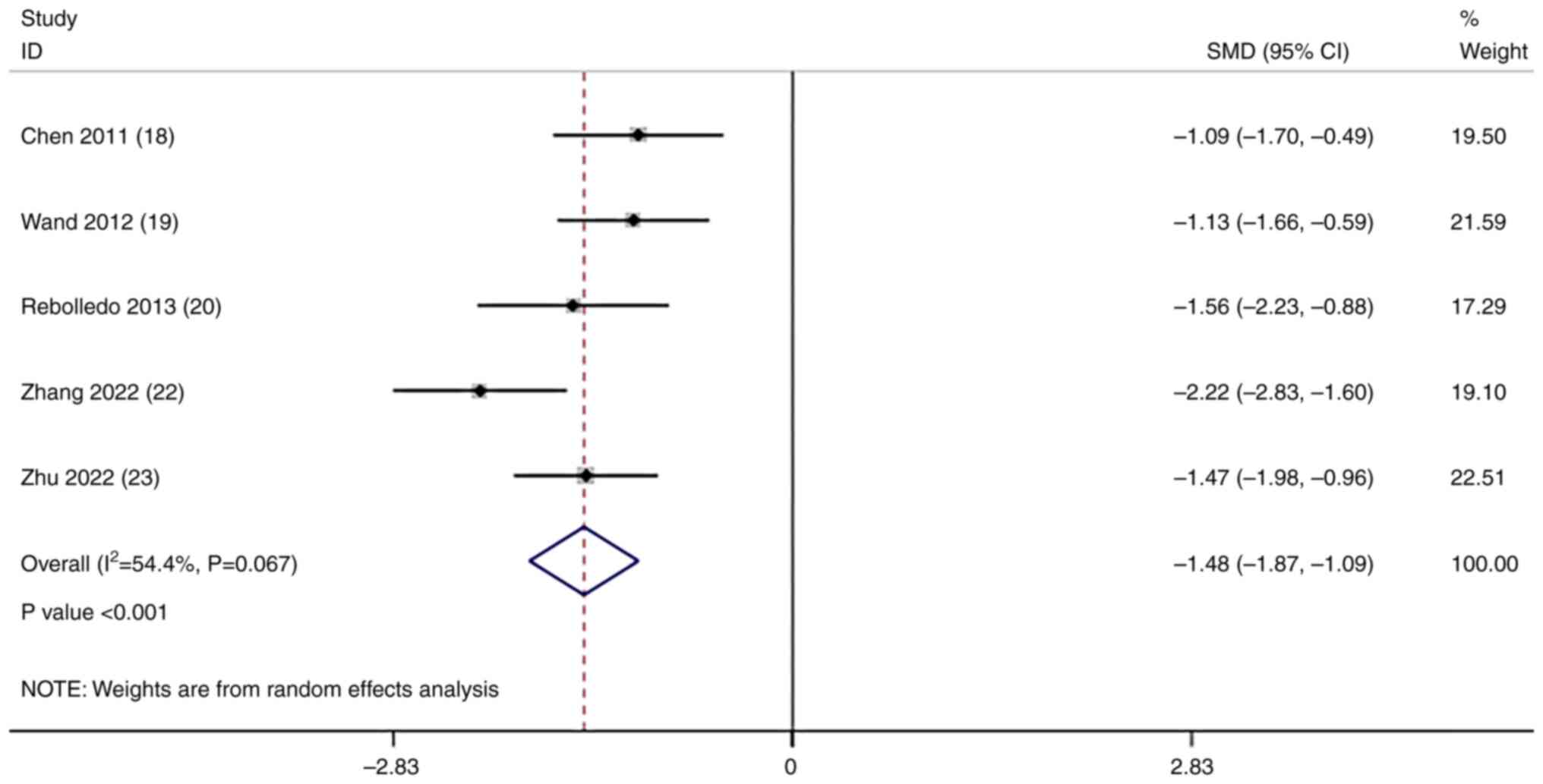
Analysis of the operative time
A total of six studies compared the operative time
in the unilateral and bilateral surgical approaches. Owing to
significant heterogeneity (I2=80.8%; P<0.001;
Fig. S1), sensitivity analyses
were performed, and it was found that the study by Yan et al
(21) had a significant impact on
the results (Fig. S2). After
excluding this article, a noTable reduction in heterogeneity was
found (I2=54.4%; P=0.067; Fig. 4) and the effect sizes were pooled
using a random-effects model. The pooled results demonstrated that
the operative time of the unilateral approach was significantly
reduced compared with the bilateral approach (SMD=-1.48; 95% CI,
-1.87 to -1.09; P<0.001; Fig.
4).
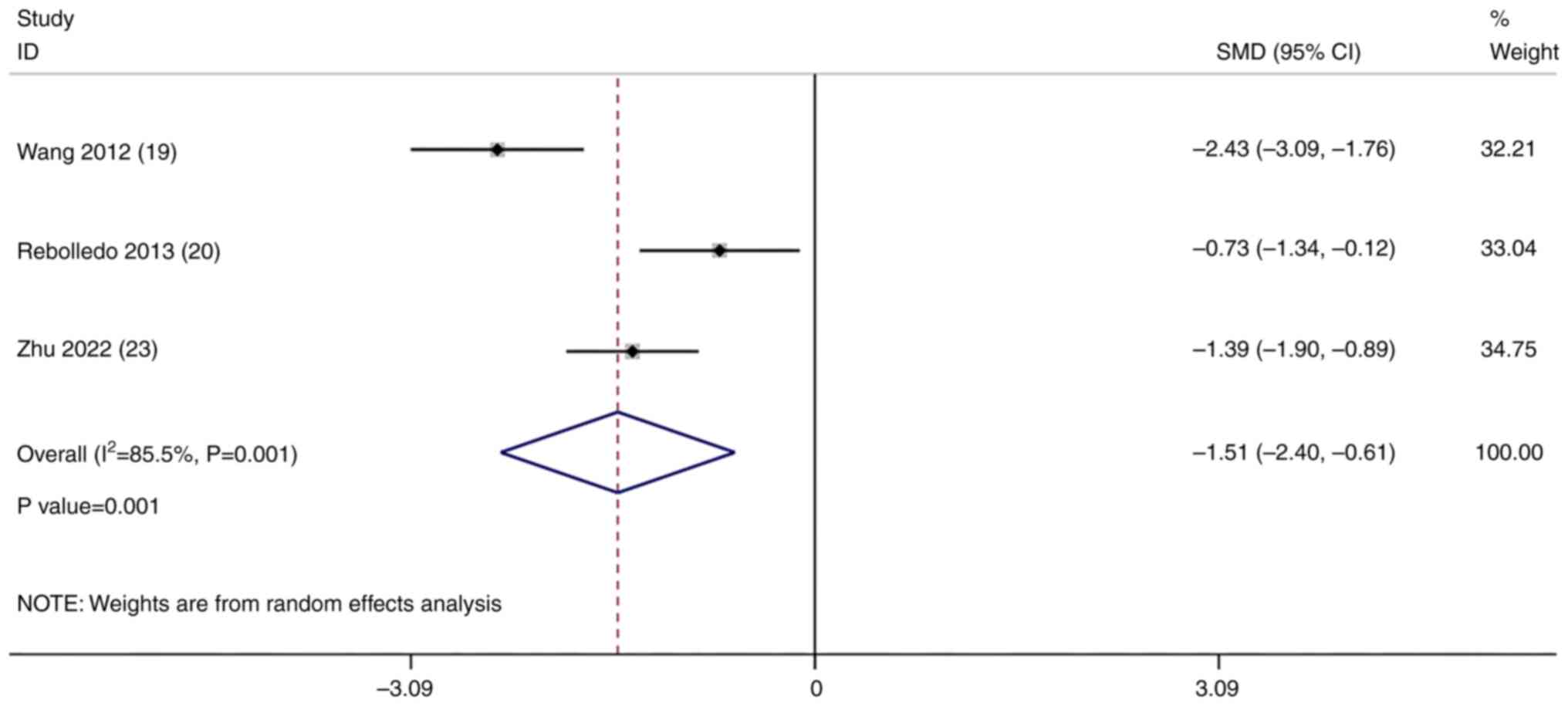
Analysis of cement injection
volume
A total of five studies compared the cement
injection volume in the unilateral and bilateral surgical
approaches. Owing to significant heterogeneity
(I2=96.6%; P<0.001; Fig. S3), sensitivity analyses were
performed, and it was found that the study by Yan et al
(21) and Zhang et al (22)
had significant impact on the results. After excluding the two
studies, a noTable reduction in heterogeneity was found
(I2=85.5%; P=0.001; Fig.
5) and the effect sizes were pooled using a random-effects
model. The pooled results demonstrated that the cement injection
volume of the unilateral approach was significantly reduced
compared with the bilateral approach (SMD=-1.51; 95% CI, -2.40 to
-0.61; P=0.001; Fig. 5).
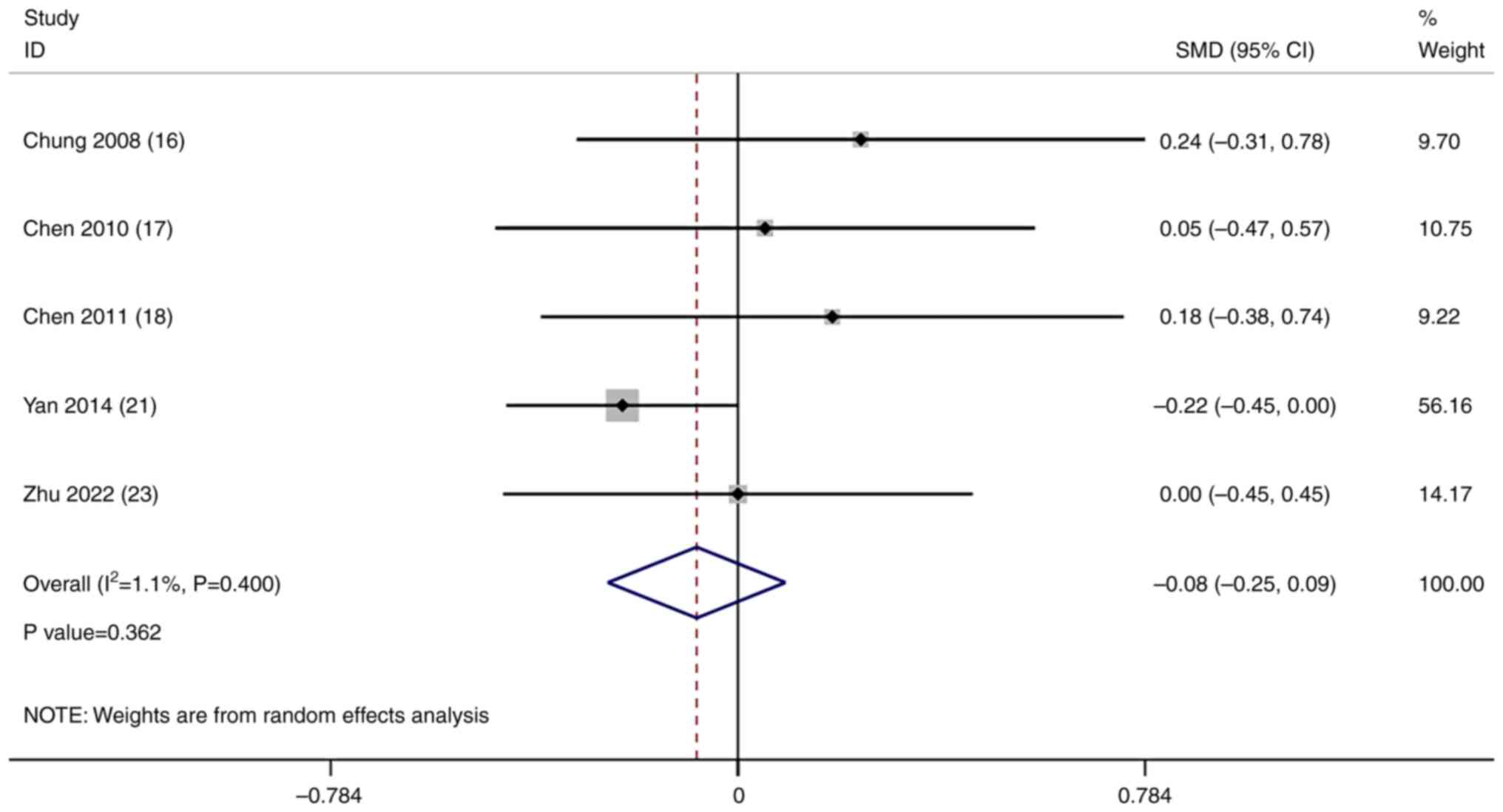
Analysis of the VAS
A total of five studies compared the VAS (a scale
used to evaluate pain) in the unilateral and bilateral surgical
approaches. A meta-analysis of the results of these studies was
conducted using a random-effects model. The pooled results
demonstrated that there was no significant difference in the VAS
between the unilateral and bilateral surgical approaches
(SMD=-0.08; 95% CI, -0.25-0.09; P=0.362; Fig. 6).
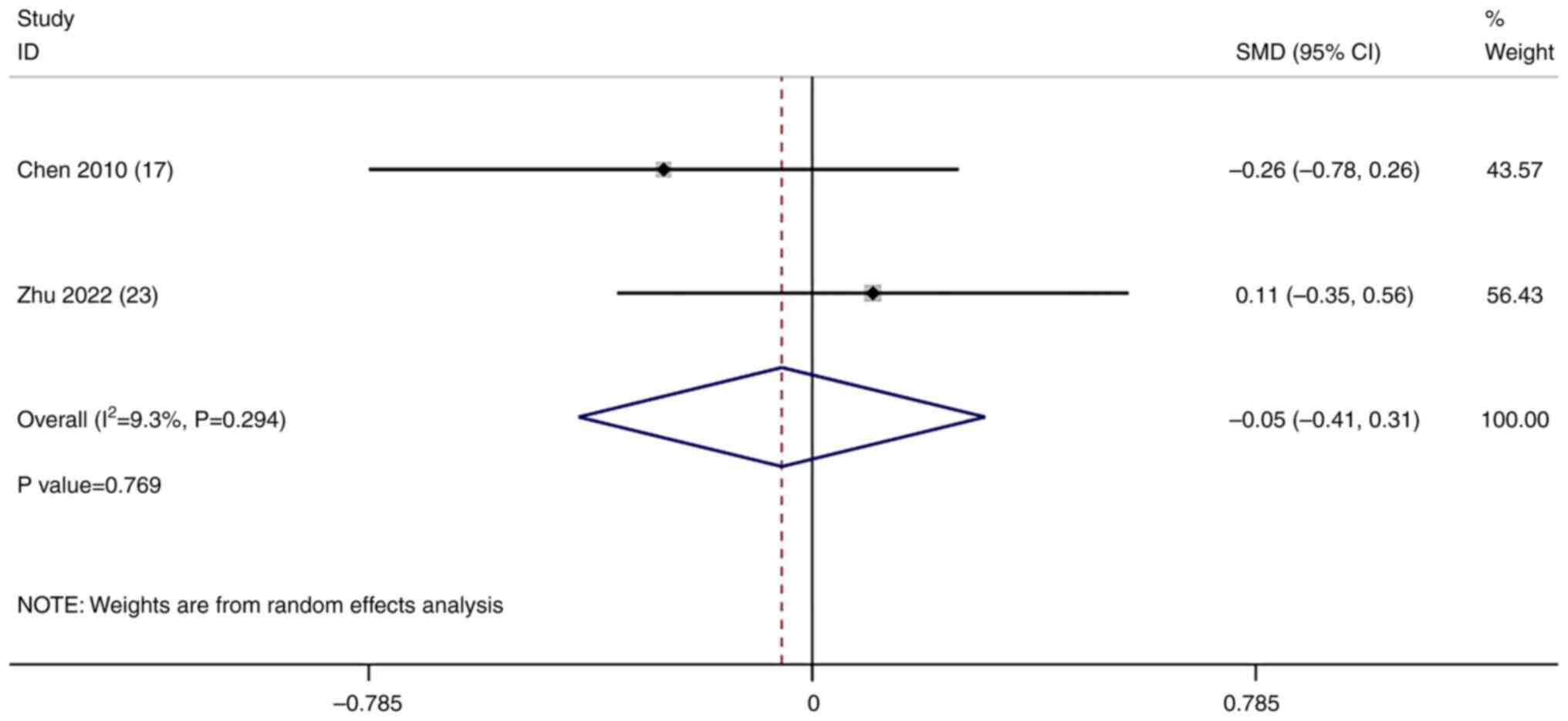
Analysis of the ODI
A total of two studies compared the ODI (one of the
principal condition-specific outcome measures used in the
management of spinal disorders) in the unilateral and bilateral
surgical approaches. A meta-analysis of the results of these
studies was conducted using a random-effects model. The pooled
results demonstrated no significant difference in the ODI between
the unilateral and bilateral surgical approaches (SMD=-0.05; 95%
CI, -0.41-0.31; P=0.769; Fig.
7).
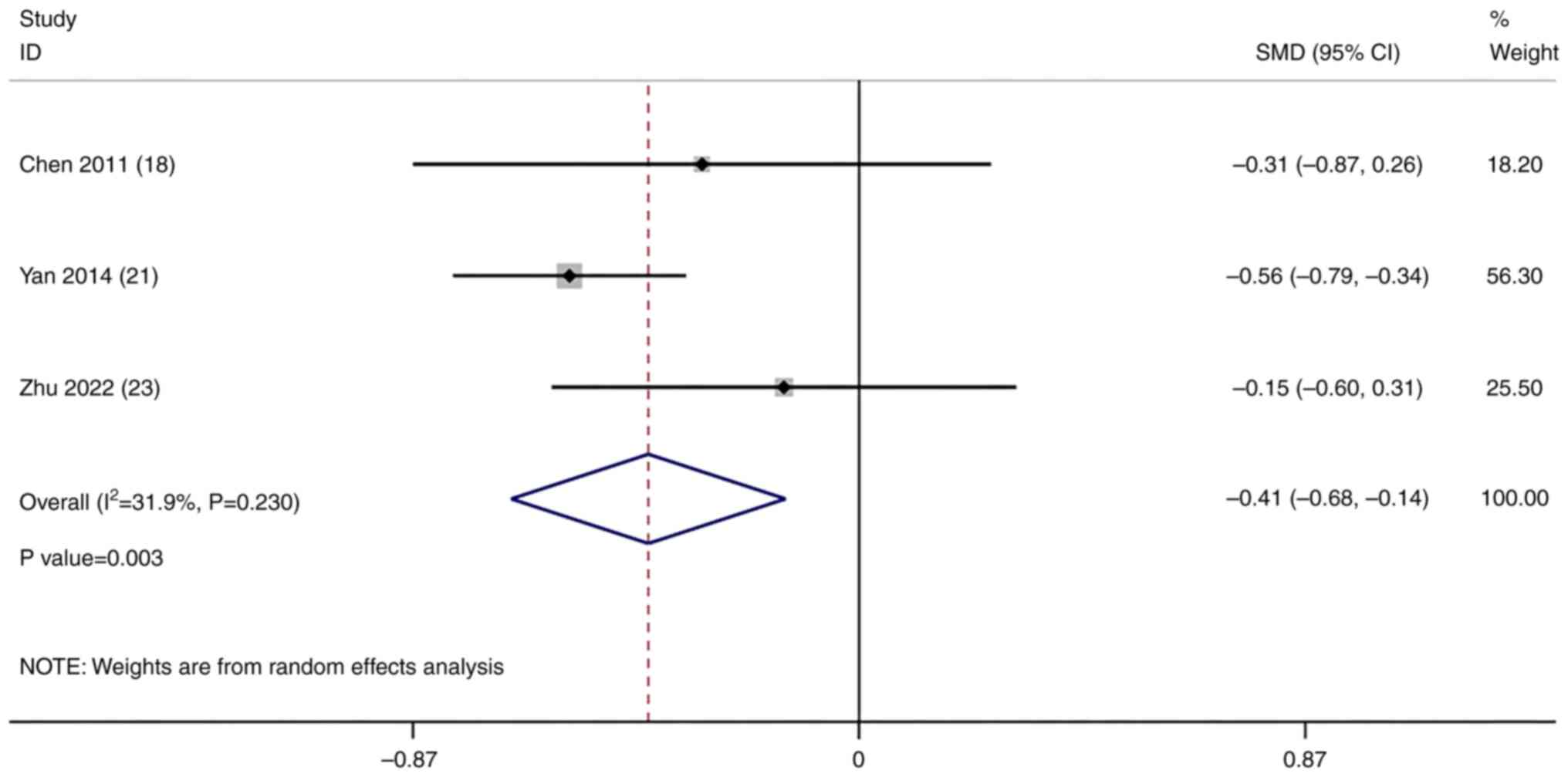
Analysis of the post-KPA
A total of three studies compared the post-KPA in
the unilateral and bilateral surgical approaches. A meta-analysis
of the results of these studies was conducted using a
random-effects model. The pooled results demonstrated that the
post-KPA of the unilateral approach was significantly lower than
that of the bilateral approach (SMD=-0.41; 95% CI, -0.68 to -0.14;
P=0.003; Fig. 8).
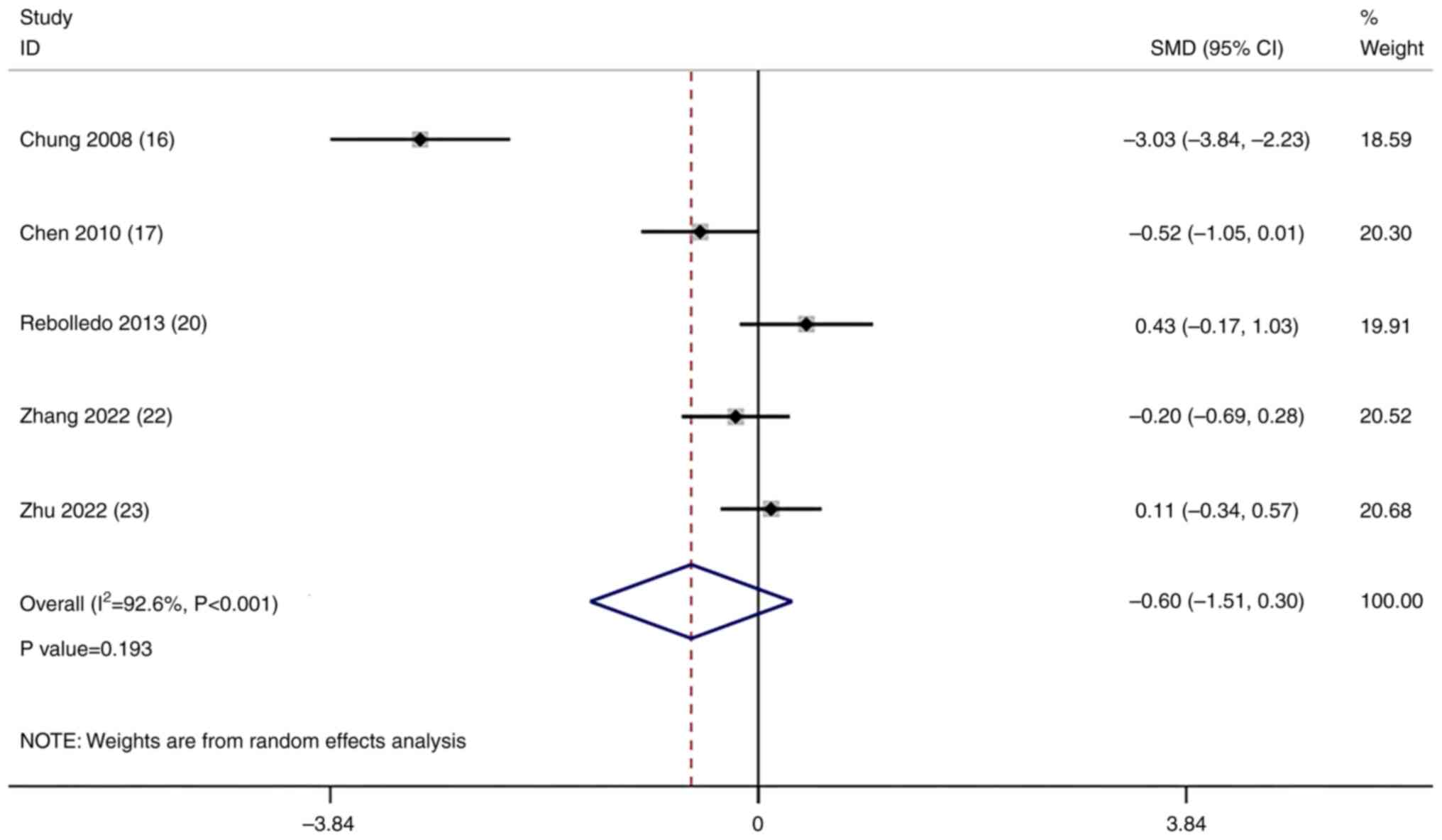
Analysis of the height restoration
rate
A total of five studies compared the height
restoration rate in the unilateral and bilateral surgical
approaches. A meta-analysis of the results of these studies was
conducted using a random-effects model. The pooled results
demonstrated that there was no significant difference in the height
restoration rate between the unilateral and bilateral surgical
approaches (SMD=-0.60; 95% CI, -1.51-0.30; P=0.193; Fig. 9).
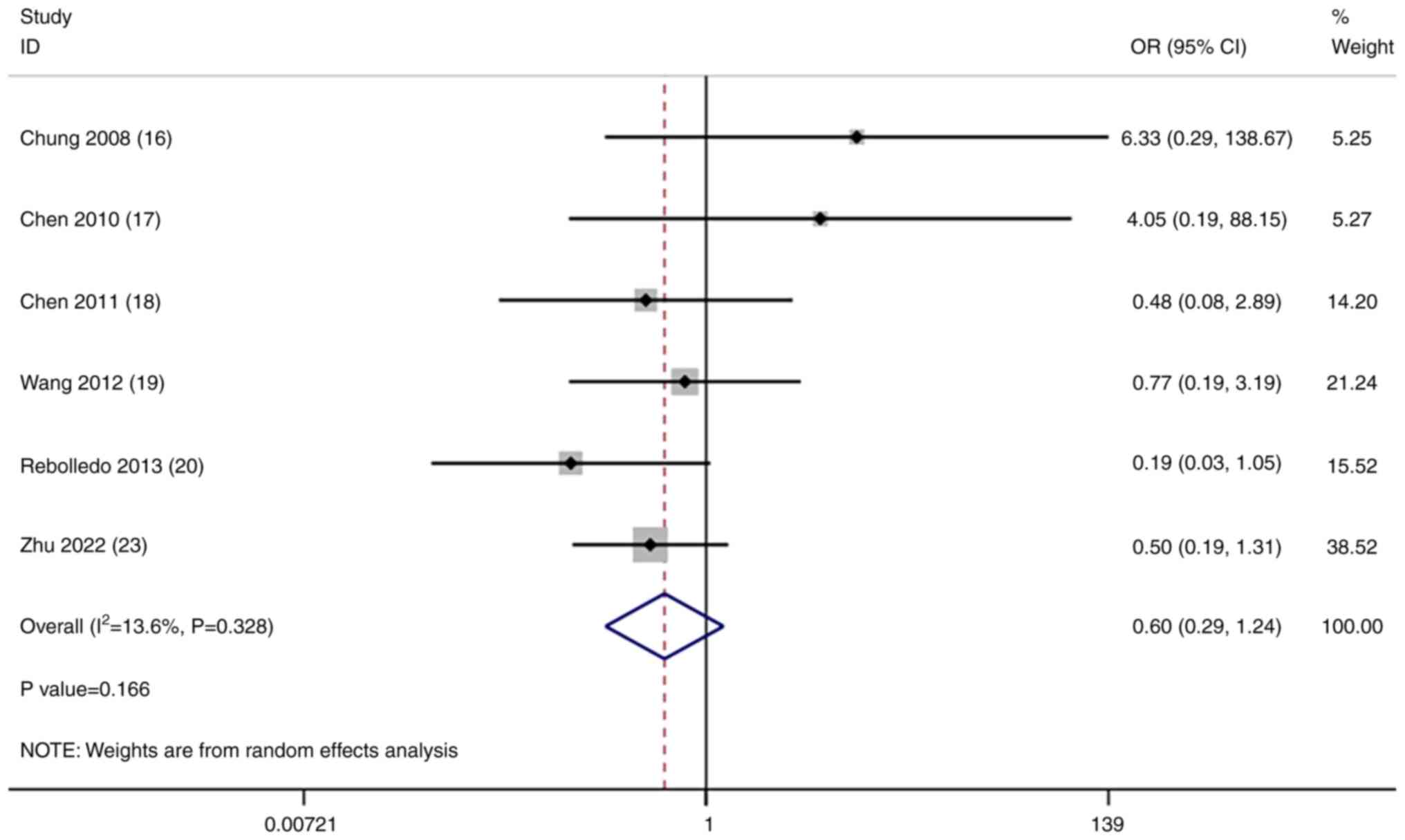
Analysis of cement leakage
incidence
A total of six studies compared the incidence of
cement leakage in the unilateral and bilateral surgical approaches.
A meta-analysis of the results of these studies was conducted using
a random-effects model. The pooled results demonstrated that there
was no significant difference in the incidence of cement leakage
between the unilateral and bilateral surgical approaches [odds
ratio (OR)=0.60; 95% CI, 0.29-1.24; P=0.166; Fig. 10].
Sensitivity analysis
A sensitivity analysis was performed to exclude each
trial individually and then a combined analysis of the remaining
trials was performed. Following the subsequent meta-analyses, it
was found that the study by Yan et al (21) had a large impact on the results of
the surgery time; Yan et al (21) and Zhang et al (22) had a large impact on the results of
the cement injection volume analyses; no other articles
significantly impacted the results of the other outcomes (Fig. S3, Fig. S4, Fig. S5, Fig. S6, Fig. S7 and Fig. S8).
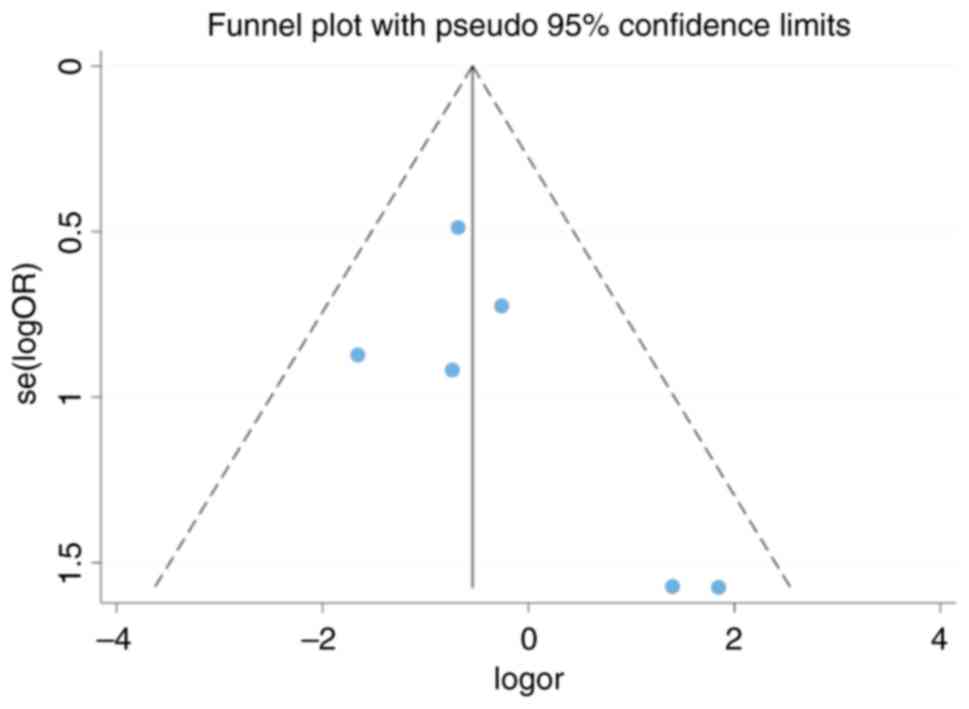
Publication bias
Fig. 11 presents
the publication bias funnel plot. The funnel plot was symmetrical
and the result of the Egger's tests was P=0.205, which indicated
that there was no significant publication bias in the studies
analyzed in the present study.
Discussion
Osteoporosis often leads to vertebral fractures that
seriously affect the health and quality of life of the elderly
(24). Symptom relief is mainly
achieved through conservative or surgical treatment (25). PKP is a minimally invasive
procedure and an effective treatment for OVCF that is divided into
two surgical approaches: Unilateral or bilateral pedicle puncture
(26). Previous studies have
suggested that the latter should be the mainstay treatment for OVCF
(27,28). However, with advances in
technology, previous studies have shown that a unilateral pedicle
puncture can produce the same clinical and radiological
improvements (20,29). The present meta-analysis included
eight studies involving 717 patients and evaluated the safety and
efficacy of the two types of PKP in the treatment of vertebral
fractures caused by osteoporosis to guide the selection of clinical
surgical methods.
In the present study, the VAS and ODI results were
used for the assessment of clinical effectiveness. The pooled
results demonstrated that there were no significant differences in
the VAS and ODI scores between the unilateral and bilateral
surgical approaches, which was consistent with the results of the
included studies. Findings of present study showed that once a
certain amount of properly distributed cement was reached, no
matter the puncture approach used, pain was alleviated and the
functional status was promoted. Of note, the present study
demonstrated that the post-KPA of the unilateral surgical approach
was significantly lower than that of the bilateral approach.
Although the findings of the present study indicated that there was
no clear difference between the two surgical approaches for
improving vertebral height, the improved KPA observed with the
unilateral approach could aid decision making amongst clinicians.
In addition, the pooled results demonstrated that the operative
time and cement injection volume using the unilateral approach were
significantly lower compared with the bilateral approach. The short
operation time may be due to the simplicity of the unilateral
approach.
To evaluate safety, the occurrences of cement
leakage were analyzed. The pooled results demonstrated no
significant difference in the incidence of cement leakage between
the unilateral and bilateral surgical approaches. However, an OR
value of 0.62 indicated that the unilateral approach may be
potentially safer than the bilateral approach, but this conclusion
requires further validation in the future.
The present meta-analysis had certain limitations.
First, the included studies had small sample sizes. Therefore, the
objectivity of the meta-analysis results may be reduced despite
data pooling and further studies are required. Second, although the
aggregated data contained greater statistical power, the included
prospective randomized studies had various types of biases, such as
selection, performance and detection bias, which lowered the
quality of the evidence.
In conclusion, there were no significant differences
in the VAS and ODI between the unilateral and bilateral surgical
approaches. However, the pooled results indicated that the
unilateral method had a more significant effect on improving KPA
and required less operative time and a lower cement injection
volume. This approach may therefore be safer for elderly patients,
who are more likely to suffer from a greater number of underlying
diseases.
Supplementary Material
Comparison of the differences in the
operative times between the unilateral and bilateral surgical
approaches in different studies (before sensitivity analysis). SMD,
standardized mean difference; CI, confidence interval.
Sensitivity analysis of the comparison
of the differences in the operative time between the unilateral and
bilateral surgical approaches in different studies. The red point
indicates an excluded study.
Comparison of the differences in the
cement injection volume between the unilateral and bilateral
surgical approaches in different studies (before sensitivity
analysis). SMD, standardized mean difference; CI, confidence
interval.
Sensitivity analysis of the comparison
of the differences in the cement injection volume between the
unilateral and bilateral surgical approaches in different studies.
The red point indicates an excluded study.
Sensitivity analysis of the comparison
of the differences in the VASs between the unilateral and bilateral
surgical approaches in different studies. VAS, visual analogue
scale score.
Sensitivity analysis of the comparison
of the differences in the post-KPAs between the unilateral and
bilateral surgical approaches in different studies. KPA, kyphotic
angle.
Sensitivity analysis of the comparison
of the differences in the height restoration rates between the
unilateral and bilateral surgical approaches in different
studies.
Sensitivity analysis of the comparison
of the differences in the incidence of cement leakage between the
unilateral and bilateral surgical approaches in different studies.
CI, confidence interval.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by The Medical Health Science
and Technology Project of The Zhejiang Provincial Health Commission
(grant no. 2023KY1232).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ and GL conceived the study. ZZ and QZ analyzed
data and wrote the manuscript. ZZ and GL participated in literature
review and figure drawing. JZ participated in the revision of the
article. JZ and GL checked and confirm the authenticity of all the
raw data. All authors have read and approved the final manuscript.
ZZ and GL agreement to be accountable for all aspects of the work
in ensuring that questions related to the accuracy or integrity of
any part of the work are appropriately investigated and
resolved.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sindel D: Osteoporosis: Spotlight on
current approaches to pharmacological treatment. Turk J Phys Med
Rehabil. 69:140–152. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lucas TS and Einhorn TA: Osteoporosis: The
role of the orthopaedist. J Am Acad Orthop Surg. 1:48–56.
1993.PubMed/NCBI View Article : Google Scholar
|
|
3
|
McCarthy J and Davis A: Diagnosis and
management of vertebral compression fractures. Am Fam Physician.
94:44–50. 2016.PubMed/NCBI
|
|
4
|
Li HM, Zhang RJ, Gao H, Jia CY, Zhang JX,
Dong FL and Shen CL: New vertebral fractures after osteoporotic
vertebral compression fracture between balloon kyphoplasty and
nonsurgical treatment PRISMA. Medicine (Baltimore).
97(e12666)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kim DH and Vaccaro AR: Osteoporotic
compression fractures of the spine; current options and
considerations for treatment. Spine J. 6:479–487. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhou X, Meng X, Zhu H, Zhu Y and Yuan W:
Early versus late percutaneous kyphoplasty for treating
osteoporotic vertebral compression fracture: A retrospective study.
Clin Neurol Neurosurg. 180:101–105. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhang Y, Liu H, He F, Chen A, Yang H and
Pi B: Safety and efficacy of percutaneous kyphoplasty assisted with
O-arm navigation for the treatment of osteoporotic vertebral
compression fractures at T6 to T9 vertebrae. Int Orthop.
44:349–355. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang F, Wang LF, Miao DC, Dong Z and Shen
Y: Which one is more effective for the treatment of very severe
osteoporotic vertebral compression fractures: PVP or PKP? J Pain
Res. 11:2625–2631. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chen B, Li Y, Xie D, Yang X and Zheng Z:
Comparison of unipedicular and bipedicular kyphoplasty on the
stiffness and biomechanical balance of compression fractured
vertebrae. Eur Spine J. 20:1272–1280. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Li LH, Sun TS, Liu Z, Zhang JZ, Zhang Y,
Cai YH and Wang H: Comparison of unipedicular and bipedicular
percutaneous kyphoplasty for treating osteoporotic vertebral
compression fractures: A meta-analysis. Chin Med J (Engl).
126:3956–3961. 2013.PubMed/NCBI
|
|
11
|
Steinmann J, Tingey CT, Cruz G and Dai Q:
Biomechanical comparison of unipedicular versus bipedicular
kyphoplasty. Spine (Phila Pa 1976). 30:201–205. 2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et
al: The cochrane collaboration's tool for assessing risk of bias in
randomised trials. BMJ. 343(d5928)2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cook DA and Reed DA: Appraising the
quality of medical education research methods: The medical
education research study quality instrument and the
newcastle-ottawa scale-education. Acad Med. 90:1067–1076.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Chaimani A, Mavridis D and Salanti G: A
hands-on practical tutorial on performing meta-analysis with Stata.
Evid Based Ment Health. 17:111–116. 2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chung HJ, Chung KJ, Yoon HS and Kwon IH:
Comparative study of balloon kyphoplasty with unilateral versus
bilateral approach in osteoporotic vertebral compression fractures.
Int Orthop. 32:817–820. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chen C, Chen L, Gu Y, Xu Y, Liu Y, Bai X,
Zhu X and Yang H: Kyphoplasty for chronic painful osteoporotic
vertebral compression fractures via unipedicular versus bipedicular
approachment: A comparative study in early stage. Injury.
41:356–359. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chen L, Yang H and Tang T: Unilateral
versus bilateral balloon kyphoplasty for multilevel osteoporotic
vertebral compression fractures: A prospective study. Spine (Phila
Pa 1976). 36:534–540. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang Z, Wang G and Yang H: Comparison of
unilateral versus bilateral balloon kyphoplasty for the treatment
of osteoporotic vertebral compression fractures. J Clin Neurosci.
19:723–726. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rebolledo BJ, Gladnick BP, Unnanuntana A,
Nguyen JT, Kepler CK and Lane JM: Comparison of unipedicular and
bipedicular balloon kyphoplasty for the treatment of osteoporotic
vertebral compression fractures: A prospective randomised study.
Bone Joint J. 95-B:401–406. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yan L, Jiang R, He B, Liu T and Hao D: A
comparison between unilateral transverse process-pedicle and
bilateral puncture techniques in percutaneous kyphoplasty. Spine
(Phila Pa 1976). 39(26 Spec No.):B19–B26. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhang Y, Chen X, Ji J, Xu Z, Sun H, Dong L
and Hao D: Comparison of unilateral and bilateral percutaneous
kyphoplasty for bone cement distribution and clinical efficacy: An
analysis using three-dimensional computed tomography images. Pain
Physician. 25:E805–E813. 2022.PubMed/NCBI
|
|
23
|
Zhu D, Hu J, Wang L, Zhu J, Ma S and Liu
B: A comparison between modified unilateral extrapedicular and
bilateral transpedicular percutaneous kyphoplasty in the treatment
of lumbar osteoporotic vertebral compression fracture. World
Neurosurg. 166:e99–e108. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Landham PR, Baker-Rand HL, Gilbert SJ,
Pollintine P, Annesley-Williams DJ, Adams MA and Dolan P: Is
kyphoplasty better than vertebroplasty at restoring form and
function after severe vertebral wedge fractures? Spine J.
15:721–732. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Lyritis GP, Mayasis B, Tsakalakos N,
Lambropoulos A, Gazi S, Karachalios T, Tsekoura M and Yiatzides A:
The natural history of the osteoporotic vertebral fracture. Clin
Rheumatol. 8(Suppl 2):66–69. 1989.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wardlaw D, Cummings SR, Van Meirhaeghe J,
Bastian L, Tillman JB, Ranstam J, Eastell R, Shabe P, Talmadge K
and Boonen S: Efficacy and safety of balloon kyphoplasty compared
with non-surgical care for vertebral compression fracture (FREE): A
randomised controlled trial. Lancet. 373:1016–1024. 2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Nevitt MC, Ettinger B, Black DM, Stone K,
Jamal SA, Ensrud K, Segal M, Genant HK and Cummings SR: The
association of radiographically detected vertebral fractures with
back pain and function: A prospective study. Ann Intern Med.
128:793–800. 1998.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yan L, He B, Guo H, Liu T and Hao D: The
prospective self-controlled study of unilateral transverse
process-pedicle and bilateral puncture techniques in percutaneous
kyphoplasty. Osteoporos Int. 27:1849–1855. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Li Y, Wang H, Cui W, Zhou P, Li C, Xiao W,
Hu B and Li F: Clinical study of percutaneous vertebroplasty
through extreme extrapedicular approach in the treatment of
osteoporotic vertebral compression fracture. Zhongguo Xiu Fu Chong
Jian Wai Ke Za Zhi. 33:612–617. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|