1. Introduction
The coccyx is located at the lowermost part of the
spine, where it forms a pelvic tripod with the sciatic tuberosities
to support sitting. The majority of coccyx fracture-dislocations
are caused by direct trauma, such as falling vertically and landing
on the buttocks, where the coccyx impacts a hard surface with
sufficient force to create a fracture (1-3).
Difficult labor and multiple deliveries are also important causes
of coccyx fracture-dislocation (3,4).
Coccyx fracture-dislocations are typically treated
conservatively, with most recommendations including the use of
circular cushions and the adoption of a side-lying position to
avoid placing weight on the injury site. This is often followed by
oral anti-inflammatory analgesics, topical medications, local
injections, radiofrequency therapy and other therapies with the
ability to reduce pain in the sacrococcygeal region. In general,
90% of coccyx fracture-dislocations heal successfully with
conservative treatment (5,6). However, if symptoms are not
alleviated after 6 months of conservative treatment, surgical
treatment may be considered. Surgical options include
coccygeoplasty, coccygectomy and internal fixation of the coccygeal
fracture by incision and reduction (7). Due to the continuous development of
treatment methods for coccyx fracture-dislocation, the success rate
of the management of this condition has gradually improved over
time.
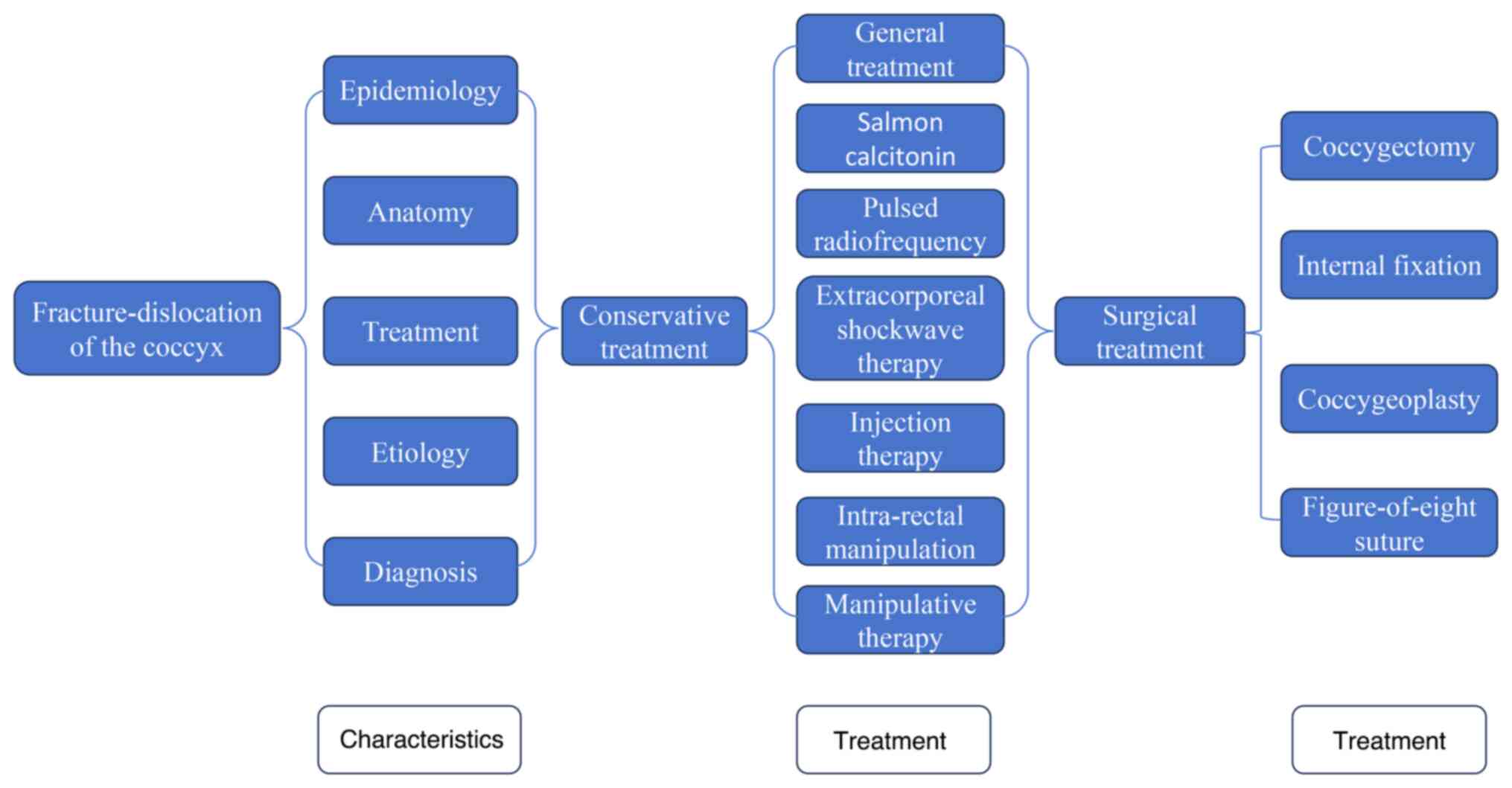
The present review summarizes the treatment methods
of coccyx fracture-dislocation, aiming to serve as a reference for
the treatment of patients with coccyx fracture-dislocation. In
particular, it summarizes the characteristics and treatment methods
of coccyx fracture-dislocation (Fig.
1).
2. Epidemiology
A study of data published by the Korean Health
Insurance Review and Assessment Service revealed that a total of
26,545 coccyx fractures occurred in South Korea between 2010 and
2018, with a male-to-female ratio of 1:2.6. The annual incidence
rate of coccyx fracture was 119.75 per 100,000 individuals overall,
with a rate of 33.44 per 100,000 in male patients and 86.30 per
100,000 in female patients. Furthermore, the incidence rate was
highest among males during puberty (age, 10-14 years) and among
females during menopause (age, 50-54 years). The study also found
that coccyx fractures occur more frequently during the winter and
less frequently in the summer (8).
The higher incidence of coccyx fractures in women, with the highest
incidence in menopause, suggests that coccyx fractures may be
associated with osteoporosis (9).
Another reason may be related to the morphological differences in
the coccyx. Compared with men, women have a straighter coccyx and
are more likely to have coccyx fractures after falling backward
(10,11). The high incidence in adolescence
can be explained by two factors: i) In contrast to the rapid growth
of bone, mineralization of bone is relatively delayed, leading to
increased bone fragility; and ii) intense physical activity in this
age group (12). A study
investigating hip, distal radius, proximal humerus and ankle
fractures in individuals aged ≥65 years revealed that incidence
rates peaked during winter months and reached their lowest levels
in summer, suggesting that colder temperatures may increase
fracture susceptibility (13).
3. Anatomy
The word coccyx is derived from the ancient Greek
word for cuckoo, as its shape is similar to that of the cuckoo's
curved beak (14). The coccyx is
approximately triangular in shape and formed from 3-5 fused coccyx
vertebrae, The first coccygeal vertebra which forms the base of the
triangle is the largest and is connected to the sacrum. The lower
point of the upwardly extending coccygeal angle is formed by the
superior articular process of the first coccygeal vertebra, which
articulates with the sacrum. On either side of the coccygeal angle,
a pair of outwardly projecting bony structures, or cusps, form the
transverse processes of the coccyx. The transverse processes of the
second coccygeal vertebra are relatively small, while the third and
fourth vertebrae are even smaller, degenerating into small nodular
bony masses. Woon et al (10) report that the first coccyx (Co1) is
fused to the fifth sacral vertebra (S5) in 57% of normal
individuals. As a result, the lower part of the sacrum is referred
to as Co1 and the first free vertebra is known as Co2(10). On the anterior surface of the
sacrum, there are three transverse grooves that correspond to the
lines of fusion between the segments. On either side of the
posterior surface are the coccygeal angles, which meet the sacral
angles to form the posterior foramen of the sacrum, where the
posterior division of the fifth sacral nerve is situated. In
addition, the flattened lateral edge of the first coccygeal segment
meets the edge of the last sacral vertebra, forming the anterior
foramen of S5, which houses the anterior branch of the fifth sacral
nerve. The wafer-thin lateral edge of the coccyx serves as an
attachment point for the sacrococcygeal ligament, as well as for
the fibers of the coccygeal muscle anterior to the ligament and the
gluteus maximus muscle posterior to it. By contrast, the
sacrococcygeal tendon attaches to the tip of the coccyx, providing
protection to the rectum and supporting it through the coccyx
(15).
There are two current classifications of coccyx
morphology, which categorize structural differences of the coccyx
into specific types. The Postacchini classification (16) defines these types as follows: i)
Type I is a slightly forward-curved coccyx; ii) type II has a more
pronounced curvature, with the coccyx pointing forward; iii) type
III is an anteriorly pointed angulation; and iv) type IV manifests
as a semi-dislocation of the sacrococcygeal joint or the
intercoccygeal joint. An alternative classification of coccyx
morphology describes the following three types of coccyges: i) Type
I shows a forward curvature of >25°; ii) type II has
a displaced or posteriorly subluxated coccyx; and iii) type III
comprises an immobile coccyx with spiculae. Spiculae are defined as
morphological abnormalities in the form of small bony excrescences
on the dorsal aspect of the tip of the coccyx (17).
4. Etiology
The coccyx is positioned at the extreme tail end of
the spine and, in a sitting position, is the lowest point of the
body. If an individual accidentally slips and lands directly on the
buttocks, the impact of direct contact with the ground can fracture
the coccyx. Additionally, in an automobile accident, sudden
backward and forward impact can also lead to a coccyx fracture
(18). The type of coccyx
fracture-dislocation is dependent on the morphology of the coccyx;
vertical varieties are more susceptible to damage from external
forces due to their immediate proximity to the skin (19). By contrast, a curved or hooked
tailbone provides protection against external damage. Direct impact
has been documented as the main cause of coccyx fracture and
dislocation, while childbirth is the second most frequent cause,
with a ratio of 9:1 for these two causes (1,8).
During childbirth, the coccyx, as part of the birth
canal, can move backward due to fetal compression to provide more
space for the fetus to pass through. However, excessive compression
by a large fetus or other factors can lead to coccyx fracture or
dislocation. Childbirth-related fractures of the coccyx are rare
and often overlooked, as its symptoms primarily manifest as
localized pain when sitting on a hard surface, which can be
relieved by standing or lying on the side (20-22).
Maigne et al (4) analyzed
57 patients with postpartum coccydynia and found that coccygeal
dislocation occurred in 17.0% of cases, whilst coccygeal fracture
was observed in 5.3% of cases (4).
5. Diagnosis
Fracture-dislocations of the coccyx, like those in
other parts of the body, typically result from physical trauma.
However, in women, the presence of the vagina anterior to the
coccyx introduces an additional risk during labor, as fetus-induced
pressure on the coccyx from the inside out can lead to a coccyx
fracture (5). On external
palpation or intrarectal palpation of a fractured coccyx, increased
mobility may be detected, and pain elicited at the site of the
dislocation or fracture (23). A
definitive diagnosis of coccyx fracture-dislocation is typically
made using standard X-ray procedures or computed tomographs scans,
with motion pictures being particularly useful for the assessment
of trauma-induced coccyx fracture-dislocations (23,24).
In addition, magnetic resonance imaging (MRI) scans are preferred
for the diagnosis of coccyx fracture-dislocations in pregnant women
and other patients for whom radiation exposure is contraindicated
(25). MRI can also help to
identify other organic abnormalities around the dislocated segment
of the coccyx fracture, as well as bone marrow edema and effusion
in the dislocated segment of the fracture.
Coccyx fractures can be categorized into types I-III
based on pathogenesis, namely flexion, compression and extension
(25). Type I, a flexion fracture,
occurs due to a fall or direct impact on the sacrococcygeal
junction, typically resulting in a compression fracture of the
lower sacral or upper coccygeal segments. Type II, a compression
fracture, involves vertical fracture lines affecting the separate
coccygeal vertebrae, namely Co2 or Co1, where they are compressed
without fusion to S5. Type III, extension fractures, primarily
occur as obstetric fractures with involvement of the lower coccyx,
likely caused by forced extension of the coccyx during labor and
delivery (25).
6. Treatment options
The treatment principles of fracture-dislocation
involve reduction, immobilization and rehabilitation (26). Since the coccyx does not serve a
primary motor or supportive function, a fracture-dislocation of the
coccyx typically does not markedly impede the daily life of a
patient, and anatomical or functional repositioning of the affected
coccyx is not typically required. Located at the most distal end of
the spine, the coccyx forms a pelvic tripod with the sciatic
tuberosities to support the sitting posture. Following a fracture,
the fractured end is subjected to downwards compression during
sitting movements. In addition, due to its location relative to the
rectum, the coccyx is subjected to backward pressure during
defecation. These forces can destabilize the fracture site,
potentially prolonging healing time. The treatment of coccyx
fracture-dislocation is mainly focused on restoring the shape of
the coccyx promptly after diagnosis, reducing pressure on the
coccyx, restricting movement of the fracture site, minimizing pain
and promoting healing. Management strategies are generally
categorized into conservative and surgical treatments.
Conservative treatment
Conservative treatment of coccyx
fracture-dislocation mainly entails non-surgical treatment to
reduce the pressure on the sacrococcygeal region. This often
includes the use of medication to promote fracture healing and
relieve pain. It has been reported that 90% of coccyx
fracture-dislocations recover fully following conservative
treatment (6,15).
General treatment. The most common treatment
approach involves the reduction of pressure on the fracture site,
which mainly comprises advising the patient to lie on their side,
sit on a hollow cushion and regulate their diet. These measures
help to reduce the pressure of body weight and rectal defecation on
the fracture site, reduce the mobility of the coccyx and provide
optimal conditions for the fracture to heal (6). For localized pain due to trauma, oral
medications are commonly used. Various medications, such as
nonsteroidal anti-inflammatory drugs and opioid analgesics, can
alleviate pain associated with fracture-dislocation of the coccyx
(6).
Salmon calcitonin (SCT). SCT has been
approved by the US Food and Drug Administration for the treatment
of postmenopausal osteoporosis and has been shown to be effective
in alleviating the pain resulting from various neurological and
musculoskeletal disorders in numerous studies (27). In a rat model, fracture healing was
found to be improved in rats treated with intramuscular calcitonin
compared with that in the placebo-treated controls (28). In addition, in a study of patients
who underwent the internal fixation of acute hip fractures,
intranasal calcitonin was reported to promote fracture healing
compared with that in patients treated with a placebo (29). Furthermore, Foye et al
(30) found that intranasal SCT
significantly reduced pain in patients with acute coccyx fractures.
However, as the study was a case series and no control group was
included, further studies are necessary to determine the role of
intranasal SCT in the treatment of acute coccyx fractures (30).
Pulsed radiofrequency (PRF) therapy. PRF
therapy is a neuromodulation technique that has been widely used
for the treatment of neuropathic pain, sensory injury pain and
cancer-related pain, without causing permanent nerve damage. In PRF
therapy, a discontinuous, pulsed electric current is generated that
creates a field around neural tissues to achieve an analgesic
effect. It is commonly used in the treatment of chronic pain
associated with nerves, joints, intervertebral discs and soft
tissues (31). Although PRF
therapy has been suggested for the treatment of sacrococcygeal
pain, information on its use specifically for this condition is
limited (32). However, Adas et
al (33) treated a total of 41
cases of chronic intractable coccydynia between January 1, 2010,
and December 31, 2012, and an evaluation performed after 6 months
of treatment revealed treatment success in 90.2% of the patients
and failure in the remaining 9.8%.
Shockwave therapy. A shockwave is an acoustic
wave that generates energy through high-speed mechanical
vibrations, leading to rapid compression and the concentration of
energy in the medium it passes through (34). Extracorporeal shockwave therapy
(ESWT) was first reported for the treatment of kidney stones by
Chaussy et al (35) in
1980. Since then, the scope of application of ESWT has gradually
broadened and it is now applied for the treatment of chronic soft
tissue pain, muscle spasms, osteoarthritis, and acute and chronic
skin injuries (31,36). While the mechanism of action of
ESWT remains to be fully elucidated, it has been reported to have a
wide range of therapeutic effects on musculoskeletal conditions,
including the promotion of tissue regeneration, wound healing,
angiogenesis and bone remodeling, and the inhibition of
inflammation (37). Notably, Ahadi
et al (38) found that ESWT
provided stronger and longer-lasting relief of coccygeal pain
compared with steroidal injection therapy in a randomized
controlled trial (38).
Injection therapy. Local anesthesia combined
with glucocorticoid injections have been reported to be effective
in 60% of patients with sacrococcygeal pain (39). Local anesthetics are a class of
drugs that reversibly block the initiation and transmission of
sensory nerve impulses at the local level, leading to a reversible
loss of nociception in the affected tissue (40). Glucocorticoids act by increasing
vascular tone, reducing congestion, decreasing capillary
permeability and minimizing exudation and edema. They achieve this
by inhibiting the aggregation of inflammatory cells at the site of
inflammation, thereby preventing complement activation in the
inflammatory response. In addition, glucocorticoids block the
synthesis and release of chemical mediators of inflammation, which
relieves symptoms such as redness, swelling, heat and pain
(41,42). The combination of local anesthetics
and glucocorticosteroids effectively alleviates the inflammation
and pain associated with coccyx fracture-dislocation. The injection
is typically administered around the fracture-dislocation site and
can be performed under fluoroscopic or ultrasound guidance for
precise injection (41,43,44).
Wray et al (39) conducted
a study in which local injections of methylprednisolone acetate (40
mg) in combination with bupivacaine (10 ml) were administered to 50
patients with coccygeal pain. All patients were followed up for ≥1
year, with a mean follow-up of 2 years and 9 months. This treatment
was found to be successful in 60% of the patients.
Intra-rectal manipulation. For patients with
obvious displacement of a coccyx fracture-dislocation, intra-rectal
manipulation can be used to restore the anatomical alignment of the
coccyx. This technique helps to reset the fracture-dislocation,
reduce the occurrence of deformity during healing and facilitate
the healing of the fracture. During the operation, the patient is
placed in the left lateral decubitus position with hip and knee
flexion as far as possible, and the operator wears sterile gloves
and stands behind the patient. The patient is asked to breathe
deeply to relax the muscles around the anus. The operator then
slowly inserts their right-hand index finger into the rectum to
access the fracture site, where the patient is likely to feel pain
upon contact. The right thumb of the operator is placed behind the
coccyx, at the back of the buttocks, and the coccyx is gently
pinched between the thumb and index finger. The index finger is
then pressed against the displaced coccyx and a backward push is
performed, being careful not to apply excessive force to avoid
damage to the rectum. If the reset is successful, the operator
feels a sliding or popping sensation, indicating proper
realignment. The index finger is then moved along the coccyx in the
anal canal to restore the physiological curvature of the coccyx
(45,46). If the displacement is corrected,
the pain typically disappears immediately (47). Fang et al (47) treated 29 patients with caudal
fracture-dislocations using endorectal manipulative repositioning,
and 20 patients were considered cured, 4 reported ‘remarkable’
effects, 4 reported being ‘better’ and 1 reported an ineffective
outcome (47). Intra-rectal
manipulative reduction is one of the more frequently used methods
of treating coccyx fracture-dislocation in China, as it can restore
the anatomical structure of the coccyx and aligns with the
treatment principles of fracture-dislocation (26). The simple endorectal reduction of
dislocated coccyx fractures restores the anatomical structure of
the fracture site, which promotes the healing of fresh fractures.
However, in older fractures, closure of the marrow cavity and
sclerosis at the fracture ends create a mechanically unfavorable
environment that substantially impairs new bone formation and
connectivity (48).
Manipulative therapy. Manipulative therapy
uses manual manipulation to relax the sacrococcygeal muscles and
adjust the position of a stiff coccyx. Common manipulation
techniques include the following: i) Massage of the levator ani,
coccygeus and pectineus muscles; ii) repetitive joint mobilization
around the coccyx; and iii) mobilization of the coccyx in a
stretched position with vigorous stretching of the levator ani
muscles (44,49). A randomized controlled study
performed by Maigne et al (49) reported a success rate for coccyx
manipulation in the treatment of coccydynia of only ~25%.
Recent-onset traumatic coccyx pain with a stable coccyx and no
interfering psychosocial factors are proposed to serve as
indications for coccyx manipulation. The effectiveness of
manipulation may be improved by the concurrent administration of
steroid injections (50).
Surgical treatment
In certain patients undergoing conservative
treatment, the fracture site does not heal, resulting in recurrent
pain in the sacrococcygeal area. In such cases, surgery may be
performed to relieve the pain. The surgical treatment of coccyx
fracture-dislocation can be divided into four main methods:
Polymethyl methacrylate (PMMA) coccygeoplasty, resection of the
fractured segments or coccyx, internal fixation of the
fracture-dislocation by incision and reduction, and modified
figure-of-eight minimally invasive suture. Among surgical treatment
options, surgical resection of the coccyx for refractory
sacrococcygeal pain has the highest improvement rate of 79%
(51). There have been few studies
on the surgical treatment of coccygeal fracture and dislocation as
it is restricted to the sacrococcygeal region and does not affect
patient survival. Previous studies on the surgical treatment of
coccygeal fracture and dislocation have primarily focused on the
impact of surgery, with a few reports of surgical complications,
the main complication being surgical site infection, with an
incidence of 2.6-26% (51-53).
Coccygectomy. In 1937, Key (54) first described a surgical procedure
to remove the mobile fractured portion of the coccyx. The extent of
resection remains a controversial issue, as evidence suggests that
total resection of the coccyx and partial resection of the distal
fracture achieve similar results (23,55,56).
Despite this, total removal of the coccyx is generally regarded as
the optimal surgical option (57,58).
The inclusion criteria for this procedure are as follows: i)
Confirmed history of trauma with imaging evidence of coccyx
fracture-dislocation; ii) persistent or intractable sacrococcygeal
pain, paroxysmal or persistent perianal discomfort, or dyspareunia;
and iii) failure of non-surgical treatment for ≥6 months (23,53).
The surgical method begins with a preoperative enema
and urinary catheterization. The patient is placed in knee-chest
position, with a soft pillow for abdominal cushioning. Saddle or
local anesthesia is then applied, after which a posterior median
incision is made to expose the sacrococcygeal joints. The joint
capsule is incised, and scarf pincers are used to clamp the upper
end of the coccyx and pull it backwards. A sharp knife is then
employed to cut through muscles attached to the coccyx, including
the anus-lift and coccygeal muscles, and the surrounding ligaments.
If the coccyx is heavily displaced forward or there is overlap
between dislocated coccygeal joints, an assistant can insert an
index finger into the anus and press the coccyx backward to
facilitate the surgery. Care must be taken to avoid injury to the
middle sacral, sacral lumbar and subsacral arterial branches and
the sacrococcygeal nerve joint branch during dissection. The
sacrococcygeal intervertebral discs and coccygeal ligaments are
then separated and the coccyx resected from the proximal to the
distal end. The residual ligament is then closed with sutures.
Postoperatively, laxatives are prescribed for 5 days to avoid
constipation, as this could exacerbate pain at the surgical site
(44,53).
Mouhsine et al (23) performed coccygectomy in 15 patients
with post-traumatic coccyx instability, which yielded ‘excellent’
outcomes in 11 cases, ‘good’ in 3 and ‘fair’ in 1. They also
reported significant improvements in another 14 patients who
underwent partial coccygectomy. In another study, Ramieri et
al (54) performed resection
of the coccyx fracture-dislocation site in 28 cases of coccyx
fracture-dislocation and followed up the patients for 24-70 months.
Visual analog scale (VAS) scores were 0-1 at the end of follow-up.
In addition, 21 patients were satisfied with the outcome of the
procedure, 4 were dissatisfied with the outcome, and 3 had missing
follow-up data (54). In another
study, Perna et al (44)
performed caudal osteotomy on 21 patients with chronic pain in the
coccyx, which was due to trauma in 10 cases. The numerical rating
scores decreased from 9.4±3.1 preoperatively to 5.2±2.3 at 1 month
after surgery and 1.8±1.1 at 1 year after surgery. All patients
with chronic pain in the coccyx who were treated with coccygectomy
exhibited a significant improvement (44). In another study, with a follow-up
time of up to 29 years after coccygectomy, Hochgatterer et
al (53) concluded that
coccygectomy is a safe therapeutic option for patients with
coccygeal pain and yields favorable long-term outcomes. In
addition, the study recommended coccygectomy if a patient fails to
respond to conservative treatment for 6 months. Kalstad et
al (59) found that
coccygectomy is a generally acceptable to patients, with outpatient
and inpatient surgeries resulting in the same level of patient
satisfaction (59).
Incision and internal fixation of coccyx
fracture-dislocation. Restoration of the anatomical structure
of the coccyx through surgical incision, repositioning and internal
fixation is another procedure for the treatment of coccyx
fracture-dislocation. Internal fixation promotes healing of the
fracture while preserving the structure of the coccyx and the
muscles and tendons attached to it. However, this procedure is more
complex and costly compared with coccygectomy, and the recovery
time is longer. The surgical approach involves preoperative bowel
preparation, followed by the creation of an S-shaped incision in
the sacrococcygeal region, where the skin, subcutaneous tissue and
fascia are incised sequentially. The dorsal sacrococcygeal
ligament, coccygeal muscle and part of the sacrospinous ligament
are then incised to reveal the coccyx. Subsequently, cartilage and
blood clots between the sacrum and coccyx are removed using a small
spatula, and the anococcygeal ligament and part of the sacral
muscular ligament are peeled off under the periosteum for
anatomical repositioning. Based on the diameter of the coccyx
measured by preoperative imaging, a depth limiter is used, and a
small T-shaped plate is applied for internal fixation. Bone is then
taken from the posterior superior iliac spine for bone grafting
between the fracture-dislocations and both sides of the coccyx.
After satisfactory restoration, the dorsal sacrococcygeal ligaments
are tightly closed, followed by internal fixation under fluoroscopy
using a C-arm machine (47). Fang
et al (47) treated 27
patients with coccyx fracture-dislocations using an internal
fixation procedure with microplates. Of these, 26 patients healed
and 1 patient showed a significant improvement (47). A coccygectomy clearly affects the
stability of the muscles, ligaments and musculature attached to the
coccyx. In addition, the coccyx serves as one of the pelvic
tripods, along with the sciatic tuberosity, which provides
weight-bearing support for sitting. To the best of our knowledge,
the clinical issues associated with coccygectomy have not been
studied in detail, and sufficiently robust clinical trials are
lacking. However, coccygectomy is a simpler procedure than the open
reduction and internal fixation of coccygeal fractures and is
preferred by both physicians and patients (59). Therefore, additional clinical data
are required to demonstrate the efficacy of the two procedures and
provide a valid reference for treatment.
PMMA coccygeoplasty. Coccygeoplasty is a
treatment for coccyx fracture-dislocation that does not require
incisional exposure and, in comparison with coccygeal fracture
incision and internal fixation, is less invasive with a shorter
recovery time. In this procedure, the patient typically adopts a
prone position on the operating table and is anesthetized and
sedated. The pelvis and abdomen are supported with rolls and pads.
With the assistance of C-arm fluoroscopy, the point of entry is
determined based on orthostasis and laterality. Then, 2.5-3 ml PMMA
is administered by injection (60). Postoperatively, patients are
allowed to move on the day of the procedure, and do not require any
analgesia (60). Manfre et
al (61) performed
coccygeoplasty in 12 patients with coccyx subluxation, and found
that VAS scores decreased significantly in 75% of the patients
during 3- and 12-month follow-ups. In addition, various case
reports have indicated that coccygeoplasty is superior compared
with other surgical treatments in terms of surgical difficulty,
cost, length of hospitalization and patient satisfaction (62). However, due to the small number of
reported cases of coccygeoplasty, it is challenging to evaluate the
indications, contraindications and long-term efficacy of this
treatment, although it remains viable as a treatment option.
Modified figure-of-eight minimally invasive
suture. For coccyx fracture-dislocations with small distal
coccyx fragments, a figure-of-eight suture can be used to fix the
broken ends. A small local incision is made to expose the fracture
site and non-absorbable sutures are used to fix the mobile
fragments (45). Deviandri et
al (45) treated a patient
with a distal coccyx fracture conservatively for 1 month. As the
pain associated with the fracture persisted, immobilization of the
fracture was performed via a small incision with a figure-of-eight
suture. The Oswestry Disability Index score of the patient, which
was initially 16, decreased to 3 after 6 months of follow-up, and
the sacrococcygeal pain caused by fracture-dislocation of the
coccyx was significantly alleviated (47).
7. Conclusion
The diagnosis of coccyx fracture-dislocation is
relatively straightforward and can be confirmed by medical history
and imaging. However, the treatment of this injury varies as it is
often considered to be self-healing through conservative treatment.
The function of the coccyx is frequently overlooked, leading to the
treatment of patients with coccyx fractures and dislocations being
influenced by factors such as economic status, cognitive level, the
treatment approach of the physician and the overall medical
condition of the patient. Andersen et al (6) performed a systematic review of the
therapeutic effects of different treatment measures on coccyx pain,
which included a total of 1,980 patients from 64 studies, including
5 randomized controlled trials, 1 experimental study, 1
quasi-experimental study, 11 prospective observational studies, 45
retrospective studies and unpublished data from the DaneSpine
registry. In patients receiving radiofrequency therapy, the mean
VAS was decreased by 5.11 points, which was the greatest
improvement in pain among all the treatments tested. By contrast,
the VAS decreased by 5.06 points in patients receiving ESWT, 4.86
points in patients treated with coccygectomy, 4.22 points in
patients treated with injectable therapies, 2.19 points in patients
receiving manipulative therapies and 1.69 points in patients
treated with conservative therapy (6). In China, the treatment of coccyx
fracture-dislocation is typically applied in a combined and gradual
manner. Oral medication or injection therapy is used alongside
conservative treatment. As the treatment time extends, the VAS pain
score tends to gradually decrease, although this can be influenced
by the uneven distribution of medical resources, with
radiofrequency treatment or suitable surgical conditions being
unavailable in certain areas. Therefore, these treatment strategies
should be considered as a reference and applied in a personalized
manner.
Coccyx fracture-dislocation is a common condition in
trauma surgery due to the anatomical location of the coccyx. In
addition, its limited physiological function in the body often
results in insufficient medical care, leading to delayed healing,
deformities and bone non-union, which may further result in
complications such as old fractures, pseudo joints and
osteoarthritis. Compression of the rectum can also lead to
difficulties with defecation, blood in the stool and other
symptoms, causing further pain to the patient. As some patients
with coccyx fracture-dislocation experience localized chronic
intractable pain, which can seriously affect their quality of life,
coccygeal fracture and dislocation warrants further research
attention (63).
The treatment of coccyx fracture-dislocation aims to
relieve pain, promote the healing of the fracture and ultimately
improve the quality of life of the patient. Treatment methods can
include the following: i) Reducing the pressure on the site of the
coccyx fracture, restricting its movement and promoting healing;
ii) local administration of anti-inflammatory agents with analgesic
or local anesthetic drugs to relieve pain; iii) physical therapy to
relieve the pain of the fracture and promote healing; iv)
endorectal manipulation and restoration to restore the anatomical
structure of the coccyx; v) resection of the dislocated end of the
coccyx, coccydotomy and incision of the coccyx for internal
fixation; and vi) coccyoplasty to restore the structure of the
coccyx. The treatment of coccyx fracture should follow a step-wise
approach as 90% of patients can be successfully treated by
conservative treatment. However, surgical treatment may be
recommended for patients with persistent sacrococcygeal pain that
is not significantly relieved by >6 months of conservative
treatment or in cases of recurrent episodes. Patients undergoing
conservative treatment are frequently required to restrict certain
physically intensive activities for long periods of time, which may
be inconvenient. If the patient is unable to accept the
restrictions of conservative treatment, then early surgical
treatment can be considered. The clinical management of coccyx
fracture-dislocation should follow the principle of individualized
treatment, taking into account several multidimensional factors,
including differences in pathogenic mechanisms, disease course
characteristics, healthcare resources, the pain tolerance of the
patient and their quality of life. Notably, the choice of treatment
strategy should be dynamic and adaptive, rather than limited to a
single approach. Instead, treatment is often characterized by the
synergistic effect of two or more interventions. Typical treatment
protocols may include the use of a hollow decompression cushion
combined with a baseline oral analgesic regimen. Local injections
may be applied to enhance efficacy, with surgical intervention as
the final treatment option in cases with marked displacement or
nerve compression. Such a stepwise treatment model can effectively
improve clinical outcomes through the combined effects of different
mechanisms of action.
In general, the number of studies on the treatment
of coccygeal fracture and dislocation, particularly surgical
treatment, is insufficient and further research is necessary. In
addition, it is recommended that education on coccyx fracture and
dislocation should be improved to help patients and medical staff
fully understand this injury, and ultimately improve the quality of
life of patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
YZ and GG established the background of the study,
analyzed and interpreted the literature, and drafted, wrote,
substantially revised and critically reviewed the manuscript. Both
authors read and approved the final version of the manuscript. Data
authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Maigne JY, Doursounian L and Chatellier G:
Causes and mechanisms of common coccydynia: Role of body mass index
and coccygeal trauma. Spine (Phila Pa 1976). 25:3072–3079.
2000.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Schapiro S: Low back and rectal pain from
an orthopedic and proctologic viewpoint; with a review of 180
cases. Am J Surg. 79:117–128. 1950.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Karadimas EJ, Trypsiannis G and Giannoudis
PV: Surgical treatment of coccygodynia: An analytic review of the
literature. Eur Spine J. 20:698–705. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Maigne JY, Rusakiewicz F and Diouf M:
Postpartum coccydynia: A case series study of 57 women. Eur J Phys
Rehab Med. 48:387–392. 2012.PubMed/NCBI
|
|
5
|
Lirette LS, Chaiban G, Tolba R and Eissa
H: Coccydynia: An overview of the anatomy, etiology, and treatment
of coccyx pain. Ochsner J. 14:84–87. 2014.PubMed/NCBI
|
|
6
|
Andersen GØ, Milosevic S, Jensen MM,
Andersen MØ, Simony A, Rasmussen MM and Carreon L: Coccydynia-the
efficacy of available treatment options: A systematic review.
Global Spine J. 12:1611–1623. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lin CH, Wu SY, Hu WL, Hung CH, Hung YC and
Aurea Kuo CE: Laser acupuncture for refractory coccydynia after
traumatic coccyx fracture: A case report. Medicine (Baltimore).
99(e18860)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Won H, Moon SY, Park JH, Kim JK, Kim HS,
Baek SH, Kim SY, Lee YK and Koo KH: Epidemiology and risk factors
of coccyx fracture: A study using national claim database in South
Korea. Injury. 51:2278–2282. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Perez MO, Pedro PPDA, Lyrio AM, Grizzo F
and Loures MAADR: Osteoporosis and fracture risk assessment:
Improving outcomes in postmenopausal women. Rev Assoc Med Bras
ff992). 69 (Suppl 1)(e2023S130)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Woon JT, Perumal V, Maigne JY and Stringer
MD: CT morphology and morphometry of the normal adult coccyx. Eur
Spine J. 22:863–870. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yoon MG, Moon MS, Park BK, Lee H and Kim
DH: Analysis of sacrococcygeal morphology in Koreans using computed
tomography. Clin Orthop Surg. 8:412–419. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Parfitt AM: The two faces of growth:
Benefits and risks to bone integrity. Osteoporosis Int. 4:382–398.
1994.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bischoff-Ferrari HA, Orav JE, Barrett JA
and Baron JA: Effect of seasonality and weather on fracture risk in
individuals 65 years and older. Osteoporosis Int. 18:1225–1233.
2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sugar O: Coccyx. The bone named for a
bird. Spine (Phila Pa 1976). 20:379–383. 1995.PubMed/NCBI
|
|
15
|
Nathan ST, Fisher BE and Roberts CS:
Coccydynia: A review of pathoanatomy, aetiology, treatment and
outcome. J Bone Joint Surg Br. 92:1622–1627. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Bijur PE, Silver W and Gallagher EJ:
Reliability of the visual analog scale for measurement of acute
pain. Acad Emerg Med. 8:1153–1157. 2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Maigne JY, Guedj S and Fautrel B:
Coccygodynia: Value of dynamic lateral x-ray films in sitting
position. Rev Rhum Mal Osteoartic. 59:728–731. 1992.PubMed/NCBI(In French).
|
|
18
|
Sukun A, Cankurtaran T, Agildere M and
Weber MA: Imaging findings and treatment in coccydynia-update of
the recent study findings. Rofo. 196:560–572. 2024.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kim NH and Suk KS: Clinical and
radiological differences between traumatic and idiopathic
coccygodynia. Yonsei Med J. 40:215–220. 1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Guo F, Yang Z, Tang L, Ming F, Guo Y and
Zhu Y: An intrapartum coccygeal fracture: An easily missed buttock
pain. Eur J Obstet Gynecol Reprod Biol. 236:259–260.
2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kaushal R, Bhanot A, Luthra S, Gupta PN
and Sharma RB: Intrapartum coccygeal fracture, a cause for
postpartum coccydynia: A case report. J Surg Orthop Adv.
14:136–137. 2005.PubMed/NCBI
|
|
22
|
Jones ME, Shoaib A and Bircher MD: A case
of coccygodynia due to coccygeal fracture secondary to parturition.
Injury. 28:549–550. 1997.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mouhsine E, Garofalo R, Chevalley F,
Moretti B, Theumann N, Borens O, Maffulli N, Schizas C and
Wettstein M: Posttraumatic coccygeal instability. Spine J.
6:544–549. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Maigne JY, Guedj S and Straus C:
Idiopathic coccygodynia. Lateral roentgenograms in the sitting
position and coccygeal discography. Spine (Phila Pa 1976).
19:930–934. 1994.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Maigne JY, Doursounian L and Jacquot F:
Classification of fractures of the coccyx from a series of 104
patients. Eur Spine J. 29:2534–2542. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Bose KS: Principles of closed fracture
treatment. J Indian Med Assoc. 30:254–256. 1958.PubMed/NCBI
|
|
27
|
Chesnut CH III, Azria M, Silverman S,
Engelhardt M, Olson M and Mindeholm L: Salmon calcitonin: A review
of current and future therapeutic indications. Osteoporosis Int.
19:479–491. 2008.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Bulbul M, Esenyel CZ, Esenyel M, Ayanoglu
S, Bilgic B and Gulmez T: Effects of calcitonin on the
biomechanics, histopathology, and radiography of callus formation
in rats. J Orthop Sci. 13:136–144. 2008.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Huusko TM, Karppi P, Kautiainen H,
Suominen H, Avikainen V and Sulkava R: Randomized, double-blind,
clinically controlled trial of intranasal calcitonin treatment in
patients with hip fracture. Calcif Tissue Int. 71:478–484.
2002.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Foye PM, Shupper P and Wendel I: Coccyx
fractures treated with intranasal calcitonin. Pain Physician.
17:E229–E233. 2014.PubMed/NCBI
|
|
31
|
Rhim HC, Shin J, Kang J, Dyrek P, Crockett
Z, Galido P, Wade C, Hollander K, Borg-Stein J, Sampson S and
Tenforde AS: Use of extracorporeal shockwave therapies for athletes
and physically active individuals: A systematic review. Br J Sports
Med. 58:154–163. 2024.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Atim A, Ergin A, Bilgiç S, Deniz S and
Kurt E: Pulsed radiofrequency in the treatment of coccygodynia.
Agri. 23:1–6. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Adas C, Ozdemir U, Toman H, Luleci N,
Luleci E and Adas H: Transsacrococcygeal approach to ganglion
impar: Radiofrequency application for the treatment of chronic
intractable coccydynia. J Pain Res. 9:1173–1177. 2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Simplicio CL, Purita J, Murrell W, Santos
GS, Dos Santos RG and Lana JFSD: Extracorporeal shock wave therapy
mechanisms in musculoskeletal regenerative medicine. J Clin Orthop
Trauma. 11 (Suppl 3):S309–S318. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chaussy C, Brendel W and Schmiedt E:
Extracorporeally induced destruction of kidney stones by shock
waves. Lancet. 2:1265–1268. 1980.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Alvarez L: Extracorporeal shockwave
therapy for musculoskeletal pathologies. Vet Clin North Am Small
Anim Pract. 52:1033–1042. 2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Cheng JH and Wang CJ: Biological mechanism
of shockwave in bone. Int J Surg. 24:143–146. 2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Ahadi T, Hosseinverdi S, Raissi G, Sajadi
S and Forogh B: Comparison of extracorporeal shockwave therapy and
blind steroid injection in patients with coccydynia: A randomized
clinical trial. Am J Phys Med Rehabil. 101:417–422. 2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Wray CC, Easom S and Hoskinson J:
Coccydynia. Aetiology and treatment. J Bone Joint Surg Br.
73:335–338. 1991.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Shah J, Votta-Velis EG and Borgeat A: New
local anesthetics. Best Pract Res Clin Anaesthesiol. 32:179–185.
2018.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Can E, Yildiz G, Akkaya ÖT, Perdecioğlu
GRG and Yürük D: Ultrasound-guided coccygeal nerve radiofrequency
ablation and steroid injection: Combination therapy for coccydynia.
J Ultrasound Med. 43:57–64. 2024.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Oppong E and Cato AC: Effects of
glucocorticoids in the immune system. Adv Exp Med Biol.
872:217–233. 2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Lee SH, Yang M, Won HS and Kim YD:
Coccydynia: Anatomic origin and considerations regarding the
effectiveness of injections for pain management. Korean J Pain.
36:272–280. 2023.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Perna A, Franchini A, Macchiarola L,
Maruccia F, Barletta F, Bosco F, Rovere G and Gorgoglione FL:
Coccygectomy for refractory coccydynia, old-fashioned but effective
procedure: A retrospective analysis. Int Orthop. 48:2251–2258.
2024.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Deviandri R, Pribadi BPP and Wiranata M:
The mini-open procedure with a modified figure of eight for
managing sacrococcygeal fracture-dislocation: A case report and
literature review. Int J Surg Case Rep. 119(109769)2024.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Kanabur P, Gowd A, Bulkeley JA, Behrend CJ
and Carmouche JJ: Symptomatic sacrococcygeal joint dislocation
treated using closed manual reduction: A case report with 36-month
follow-up and review of literature. Trauma Case Rep. 12:11–15.
2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Fang HB, Xu HH, Fang HL, Zhang YL, Liu ZZ,
Wang FX and Zou QY: Open reduction and mini-plate internal fixation
for the treatment of fracture and dislocation of coccyx. Zhongguo
Gu Shang. 26:549–552. 2013.PubMed/NCBI(In Chinese).
|
|
48
|
Panteli M, Vun JSH, Pountos I, J HA, Jones
E and Giannoudis PV: Biological and molecular profile of fracture
non-union tissue: A systematic review and an update on current
insights. J Cell Mol Med. 26:601–623. 2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Maigne JY, Chatellier G, Faou ML and
Archambeau M: The treatment of chronic coccydynia with intrarectal
manipulation: A randomized controlled study. Spine (Phila Pa 1976).
31:E621–E627. 2006.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Seker A, Sarikaya IA, Korkmaz O, Yalcin S,
Malkoc M and Bulbul AM: Management of persistent coccydynia with
transrectal manipulation: Results of a combined procedure. Eur
Spine J. 27:1166–1171. 2018.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Kleimeyer JP, Wood KB, Lønne G, Herzog T,
Ju K, Beyer L and Park C: Surgery for refractory coccygodynia:
Operative versus nonoperative treatment. Spine (Phila Pa 1976).
42:1214–1219. 2017.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Izci EK and Keskin F: Coccygectomy for
coccygodynia: A single-center experience. Medicine (Baltimore).
102(e33606)2023.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Hochgatterer R, Gahleitner M, Allerstorfer
J, Maier J, Luger M, Großbötzl G, Gotterbarm T and Pisecky L:
Coccygectomy for coccygodynia: A cohort study with a long-term
follow-up of up to 29 years. Eur Spine J. 30:1072–1076.
2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Ramieri A, Domenicucci M, Cellocco P,
Miscusi M and Costanzo G: Acute traumatic instability of the
coccyx: Results in 28 consecutive coccygectomies. Eur Spine J. 22
(Suppl 6):S939–S944. 2013.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Maigne JY, Lagauche D and Doursounian L:
Instability of the coccyx in coccydynia. J Bone Joint Surg Br.
82:1038–1041. 2000.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Postacchini F and Massobrio M: Idiopathic
coccygodynia. Analysis of fifty-one operative cases and a
radiographic study of the normal coccyx. J Bone Joint Surg Am.
65:1116–1124. 1983.PubMed/NCBI
|
|
57
|
Sehirlioglu A, Ozturk C, Oguz E, Emre T,
Bek D and Altinmakas M: Coccygectomy in the surgical treatment of
traumatic coccygodynia. Injury. 38:182–187. 2007.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Hellberg S and Strange-Vognsen HH:
Coccygodynia treated by resection of the coccyx. Acta Orthop Scand.
61:463–465. 1990.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Kalstad AM, Knobloch RG and Finsen V:
Resection of the coccyx as an outpatient procedure. Orthop Rev
(Pavia). 12(8813)2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Akar E, Koban O, Öğrenci A, Yilmaz M and
Dalbayrak S: Polymethylmetacrylate cement augmentation of the
coccyx (coccygeoplasty) for fracture: A case report. Balkan Med J.
37:348–350. 2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Manfre L, Gil I, Baptista T, Calvão Pires
P, de Vivo AE, Masala S, Chandra RV, D'Anna G and Hirsch JA:
Coccygeoplasty: Preliminary experience with this new alternative
treatment of refractory coccydynia in patients with coccyx
hypermobility. J Neurointerv Surg. 15:82–85. 2023.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Kushchayev SV, Wiener PC, Teytelboym OM,
Arrington JA, Khan M and Preul MC: Percutaneous vertebroplasty: A
history of procedure, technology, culture, specialty, and
economics. Neuroimag Clin N Am. 29:481–494. 2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Cawley DT, Power F and Murphy M:
Cerebrospinal fluid leak after coccyx fracture. Spine J.
16:e735–e736. 2016.PubMed/NCBI View Article : Google Scholar
|