Background
Orbital cavernous venous malformation (CVM),
previously referred to as ‘orbital cavernous hemangioma’, is one of
the most common primary orbital lesion in adults (1). Typically, the CVM condition causes a
series of concerning effects on the patient's vision and
appearance, such as visual deterioration and exophthalmos due to
pushing the eyeball (2,3). The pathological CVM condition is
often characterized by a single mass with a capsule. However, it
should be noted that, in certain instances, it is highly
challenging to distinguish between schwannoma and pleomorphic
adenoma conditions (4). In recent
times, the application potential of contrast-enhanced ultrasound
(CEUS) imaging technology has been recognized by numerous
researchers. However, there are still few studies on orbital CVM
(5-7).
Motivated by these considerations, the present study
aimed to analyze the characteristics of CEUS in orbital CVM to
improve its diagnostic accuracy. Considering the reported
literature, this work may provide valuable insights into the
potential of CEUS for preoperative diagnosis. In this light, the
present findings may facilitate and improve the differentiation of
CVM from other orbital lesions, addressing important diagnostic
challenges and potentiating its applicability (8).
Patients and methods
Patients
In the present study, patients (n=56) diagnosed with
orbital CVM admitted to Sichuan Provincial People's Hospital
(Chengdu, China) from January 2018 to September 2023 were analyzed
retrospectively. These patients (22 males and 34 females) were in
the age range of 23 to 73 years, with an average age of 47.6
(47.6±14.1) years. Notably, the orbital CVM condition of all
subjects was confirmed by postoperative pathological observations.
Conventional ultrasound and CEUS were performed prior to surgery.
Written informed consent for the publication of imaging and
clinical data was obtained from each subject recruited for the
study. Furthermore, the study protocol was designed to conform to
the ethical guidelines of the 1975 Declaration of Helsinki, as
reflected in a priori approval by the Ethics Committee of Sichuan
Provincial People's Hospital (Chengdu, China).
The inclusion criteria were set as follows: i)
Patients who had a confirmed diagnosis of orbital CVM based on
postoperative pathology; ii) patients who underwent both
conventional ultrasound and CEUS before surgery; iii) patients who
had provided written informed consent for participating in the
study.
The exclusion criteria were set as follows: i)
Patients with incomplete imaging data or poor-quality ultrasound
images; ii) patients with previous orbital surgery or a history of
other orbital pathologies that could affect the imaging results;
iii) patients who disagree with the use of ultrasound contrast
agents.
Methods
The study protocol was approved by the Medical
Ethics Committee of Sichuan Provincial People's Hospital (Chengdu,
China; approval no. 2017-642). The ultrasound procedure was
performed using the method as stated. The ultrasound examinations
were performed using MyLab 90 and Logic E9 from GE Healthcare
equipped with a 7-12 MHz linear-array transducer. Initially,
patients were directed to rest on the table on their backs with
their eyes closed. Conventional ultrasound was then performed to
observe various characteristics of the lesions, including the
location, size, shape, internal echo, calcification, liquefaction
and blood flow. Blood flow signals were further assessed using
Color Doppler Flow Imaging (CDFI). The examination was performed
using a 7-12 MHz linear-array transducer, with the color Doppler
parameters set to a pulse repetition frequency of 0.7-1.2 kHz and a
wall filter of 50-100 Hz, depending on the lesion depth and size.
Blood flow signals were classified according to the Alder
classification: Grade 0 (no flow), Grade 1 (minimal flow), Grade 2
(moderate flow) and Grade 3 (abundant flow). Further, the CEUS
examination was performed in the vein on the section with rich
blood flow or the largest section of the lesion. Subsequently, a
suspension was prepared by mixing 25 mg of a contrast agent
(SonoVue; Bracco) with 5 ml of normal saline using manual
oscillation for injection. Then, 1.0 ml of suspension was injected
through the antecubital vein, which was quickly followed by 5 ml of
normal saline. Further, the CEUS dynamic images in the whole
process (~1 min) were recorded. Finally, the focus was completely
fan-scanned, displaying the blood perfusion in the mass and the
infiltration of surrounding tissues.
Evaluation
The recorded images were reviewed and analyzed by
two senior radiologists. Accordingly, the location, size, boundary,
morphology, echo and blood flow signals (based on the Alder
classification) of the lesions were analyzed by conventional
ultrasound (9).
Furthermore, the characteristics of CEUS were
observed, including the enhancement features of CVM in the early
phase (enhancement of lesions earlier/simultaneously/later) and the
enhancement features of CVM in the late phase (lesions washout
earlier/simultaneously/later) compared to surrounding tissues, as
well as the enhancement patterns of CVM (diffuse
enhancement/progressive enhancement) and the peak enhancement of
CVM
(hyperenhancement/isoenhancement/hypoenhancement/non-enhancement).
Notably, the results were evaluated without considering the
enhancement pattern (homogeneous or inhomogeneous) or lesion
enlargement (present or absent).
Statistical analysis
Data were analyzed in SPSS 19.0 (IBM Corp.). Data
are presented as the mean ± standard deviation for continuous
variables and as n (%) for categorical variables, unless otherwise
specified. Descriptive statistics were used to summarize the
characteristics of the study population and the imaging findings.
No statistical hypothesis testing was conducted in this study.
Results
Population characteristics
In the present study, the ultrasound examination of
all patients (n=56) with 56 lesions showed single, round and
space-occupying lesions in the unilateral orbit. The cohort
included 30 male patients (53.6%) and 26 female patients (46.4%),
with a mean age of 45±12.3 years. The lesions were located in
different orbital regions: 20 cases (35.7%) in the orbital floor,
10 cases (17.9%) in the orbital roof, 15 cases (26.8%) in the
medial wall, and 11 cases (19.6%) in the lateral wall. The diameter
of the lesions was 18±6.3 mm, with a minimum diameter of ~8 mm and
a maximum diameter of 36 mm (Table
I).
 | Table IPopulation characteristics (n=56). |
Table I
Population characteristics (n=56).
| Characteristic | Value |
|---|
| Sex | |
|
Male | 30 (53.6) |
|
Female | 26 (46.4) |
| Age, years | 45±12.3 |
| Lesion location | |
|
Orbital
floor | 20 (35.7) |
|
Orbital
roof | 10 (17.9) |
|
Medial
wall | 15 (26.8) |
|
Lateral
wall | 11 (19.6) |
Conventional two-dimensional (2D)
ultrasound findings
Considering the echo of 2D ultrasound, these lesions
were classified into hyperechoic, isoechoic and hypoechoic types in
accordance with the surrounding soft tissues at the same level.
Accordingly, the conventional 2D ultrasound findings revealed 36
hypoechoic lesions (64.2%), 15 isoechoic lesions (26.8%) and 5
hyperechoic lesions (8.9%). All of these lesions (100%) were
quasi-circular in shape and most of the lesions (55/56, 98.2%)
showed clear boundaries. The CDFI results showed weak or absent
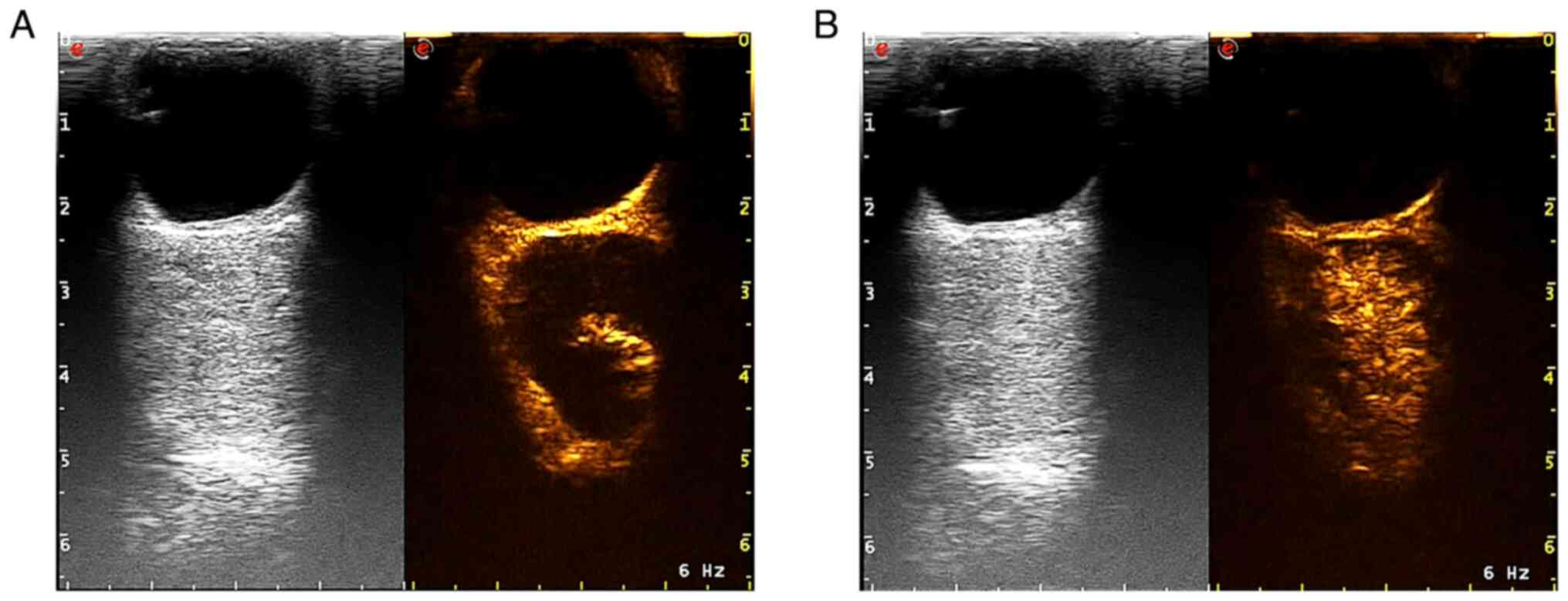
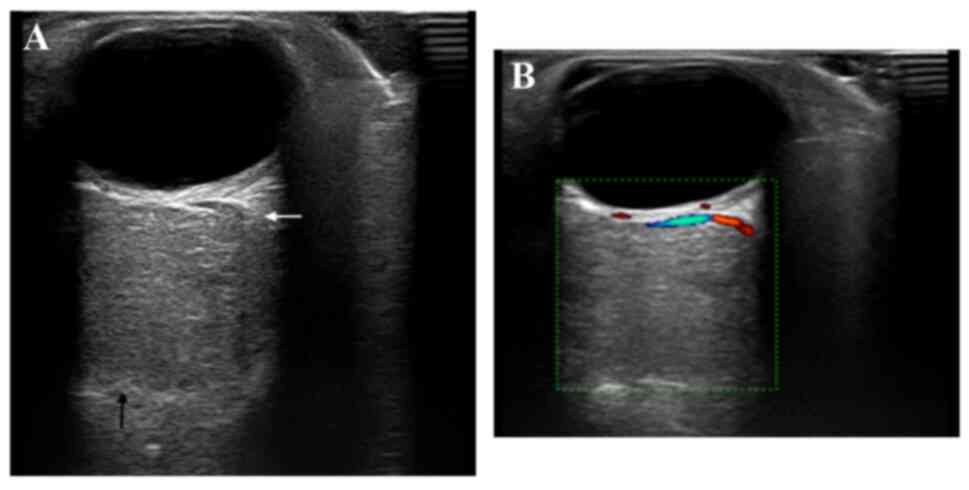
blood flow signals in 50 cases (89.3%) (Figs. 1A and 2B), with only 6 cases (10.7%) showing
weak blood flow. The characteristics are summarized in Table II.
 | Table IISummary of the conventional ultrasound
findings of orbital cavernous venous malformation in patients
(n=56). |
Table II
Summary of the conventional ultrasound
findings of orbital cavernous venous malformation in patients
(n=56).
| | | Location | Boundary | Calcification | Fluid sonolucent
area | Blood flow
signal |
|---|
| Category | n | Left | Right | Clear | Unclear | No | Yes | Yes | No | 0 | I | II |
|---|
| Low echo | 36 | 19 | 17 | 36 | 0 | 35 | 1 | 12 | 24 | 18 | 15 | 3 |
| Equal echo | 12 | 6 | 6 | 11 | 1 | 12 | 0 | 0 | 12 | 7 | 3 | 2 |
| High echo | 8 | 6 | 2 | 8 | 0 | 8 | 0 | 2 | 6 | 4 | 3 | 1 |
CEUS enhancement patterns and washout
characteristics
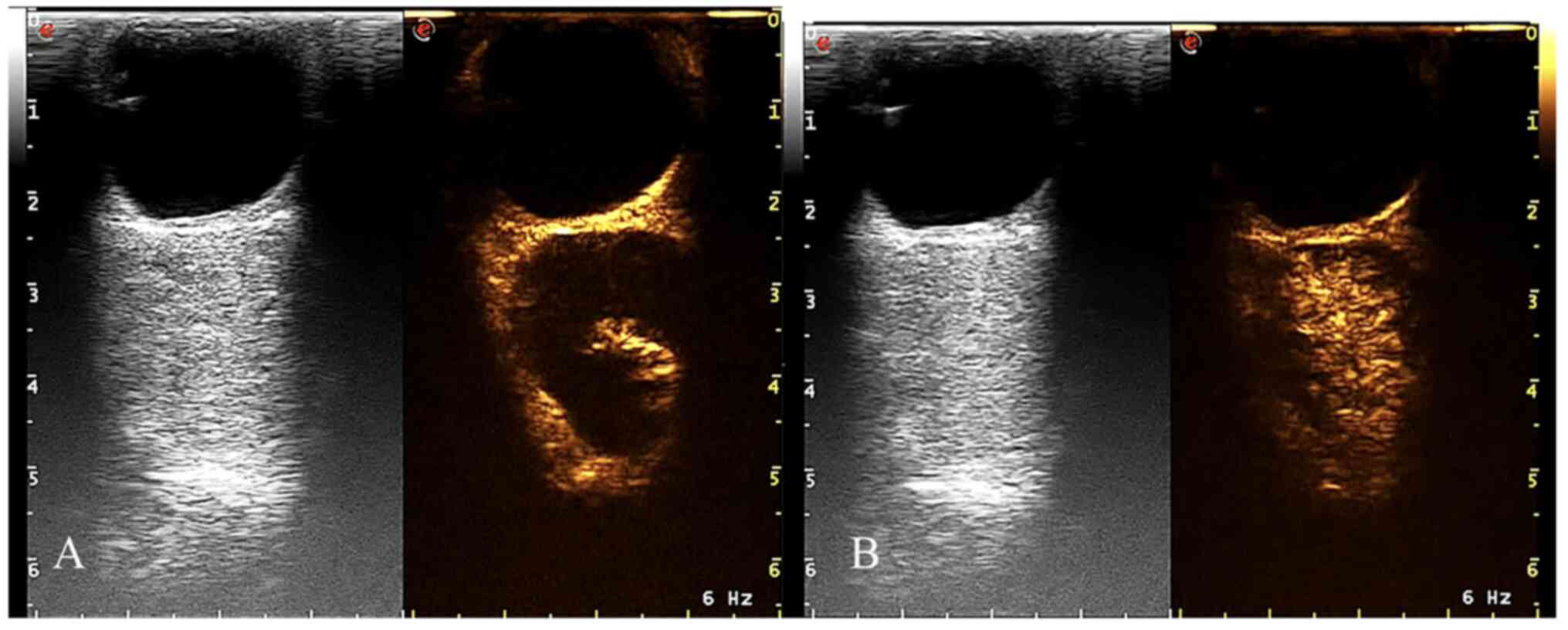
The CEUS characteristics showed a gradual
enhancement pattern of the progressive enhancement pattern of focal
nodules (94.6%), which was slightly synchronized with the
surrounding soft tissues. Among the selected lesions, several
lesions (n=50, 89.2%) showed simultaneous enhancement or slightly
later than the surrounding tissues. Certain lesions (n=3, 5.4%)
displayed a diffuse enhancement pattern without the progressive
fill-in pattern that was observed in most of the lesions. Several
lesions (54/56, 96.4%) displayed inhomogeneous enhancement at the
peak time, with incomplete filling of the contrast agent, while
only 2 lesions (3.6%) showed complete fill-in. All lesions showed
synchronous washout with surrounding tissues after 90 sec of
enhancement (Table III). Despite
the changes, the lesions eventually showed complete or incomplete
fill-in (Fig. 2A and B), which were not observed in the CEUS of
other orbital space-occupying lesions. The other 3 lesions showed
diffused enhancement without a progressive enhancement pattern
(Fig. 3A and B). After the examination, all patients
rested in the lounge for 30 min and were carefully asked for any
visual or other abnormal sensations. No positive findings were
found. The patients reported no visual changes or other abnormal
sensations. Therefore, these findings suggested that no obvious
changes were observed in the vision of all subjects before and
after the examination.
 | Table IIISummary of the contrast-enhanced
ultrasound findings of orbital cavernous venous malformation in
patients (n=56). |
Table III
Summary of the contrast-enhanced
ultrasound findings of orbital cavernous venous malformation in
patients (n=56).
| | | Early enhancement
phase | Enhancement
patterns | Peak
enhancement | Homogeneous |
Enlargeda |
|---|
| Category | n | Later |
Synchronization | Earlier | Diffuse | Progressive | Hypo- | Iso- | Hyper- | Yes | No | Yes | No |
|---|
| Low echo | 36 | 15 | 16 | 5 | 3 | 33 | 2 | 7 | 27 | 2 | 34 | 0 | 36 |
| Equal echo | 12 | 7 | 5 | 0 | 0 | 12 | 3 | 2 | 7 | 0 | 12 | 0 | 12 |
| High echo | 8 | 2 | 4 | 2 | 0 | 8 | 1 | 0 | 7 | 0 | 8 | 0 | 8 |
Discussion
Orbital CVM has emerged as one of the most common
space-occupying lesions in adults, posing a challenge regarding its
differentiation from other similar orbital lesions. Despite the
useful insights, the applicability of conventional imaging
techniques, such as magnetic resonance imaging (MRI) and
traditional 2D ultrasound, is limited due to their diagnostic
specificity. Although CEUS has been well-established in the
diagnosis of hepatic and subcutaneous cavernous venous
malformations (10), the
application of this technique in orbital CVM is relatively novel.
Previous studies on orbital masses relied heavily on MRI and
conventional 2D ultrasound (11,12).
However, these exceptional techniques suffer from major limitations
in differentiating CVM from other lesions. The present study
intended to demonstrate the potential of CEUS to offer superior
diagnostic specificity in a non-invasive manner. The CEUS imaging
of orbital CVM showed a typical progressive enhancement pattern
with inhomogeneous enhancement, which could serve as a distinct
feature for preoperative diagnosis. The resultant patterns may
provide additional diagnostic clarity, distinguishing CVM from
other orbital lesions, such as fibromas, schwannomas or lymphomas,
and lacking these specific CEUS characteristics.
Typically, CVM is one of the most common types of
non-dilated venous malformations (13-16).
Although there were related case reports of infants, no obvious
clinical symptoms were evident before adulthood. In the present
study, adults were selected as patients with a broad age range of
23 to 73 years, with an average age of 47.6 years. As evident from
the previous studies, most cases occurred between 40 and 60 years
of age (12). Accordingly, no
substantial age-related variations in CEUS characteristics or
lesion presentation were observed. Previous findings suggested that
orbital CVM followed a relatively consistent imaging pattern across
different age groups (17,18). However, the predilection for
middle-aged adults, particularly women, indicated a possible
hormonal influence, as reported previously (6,7). In
the current study, the majority of cases (34/56, 61%) were females,
which was consistent with the previous report showing in several
long-term follow-up studies the enlargement or decrease of the
lesions may be related to the level of progesterone (17). Contrarily, the lesions in the
estrogen supplementation group showed no signs of enlargement
(8,19).
Previous reports suggested that the most common
clinical symptoms of orbital CVM were axial exophthalmos, resulting
in the worsening of varied degrees of vision (20,21).
In addition, certain patients presented with ocular movement
impairment, strabismus and rare localized pain (17). The orbital CVM tended to occur in
the preorbital area and orbital muscle cones. Compared with lesions
that occurred in other tissues, these lesions generally showed an
intact envelope (18). Therefore,
the orbital CVM often appeared as a solitary mass with a clear
boundary on imaging examination. Considering the fulfillment of
orbital CVM with stagnant blood in a resting state, the
reflectivity was normally medium to high, with no signs of internal
vascularization. Therefore, the conventional 2D ultrasound images
of orbital CVM mostly appeared as isoechoic or slightly hyperechoic
masses with clear boundaries and regular shapes. The CDFI results
showed a small amount or no signs of internal blood flow. In
addition, the relationship between the lesion and the eyeball wall
and optic nerve could be observed during the dynamic scanning to
observe the location of the eyeball wall and optic nerve.
Considering its real-time imaging capabilities, CEUS
can offer valuable insights during preoperative evaluation,
allowing for accurate differentiation between CVM and other orbital
lesions, such as schwannomas and lymphomas (22-24).
Accordingly, CEUS offers substantial utility for the diagnosis of
orbital masses. For instance, surgeons may improve their approach
with a more definitive preoperative diagnosis, potentially reducing
surgical risks and complications (25). An accurate preoperative diagnosis
plays an important role in clinicians' selection of appropriate
treatment options. CVM lesions are often benign, requiring precise
surgical intervention based on their location and relationship with
surrounding tissues. In terms of clinical implications, the study
demonstrated that CEUS could provide exceptional diagnostic
specificity by identifying the characteristic progressive
enhancement pattern and inhomogeneous enhancement of orbital CVM.
The unique imaging features could distinguish CVM from other
orbital space-occupying lesions that may present with similar
characteristics on conventional 2D ultrasound, such as fibromas,
schwannomas or lymphomas. The ability of CEUS to reveal these
distinct patterns may highlight its potential in terms of reducing
diagnostic uncertainty, making it a valuable tool for clinical
decision-making. In several cases where conventional ultrasound
failed to provide sufficient detail, CEUS could provide critical
vascular information that may aid in the precise diagnosis and
treatment planning for orbital CVM.
Despite the advantages, several features of CEUS
must be considered for its replacement of other diagnostic
modalities, such as MRI, or serve as a complementary tool (25). Although CEUS offers real-time
dynamic imaging and excellent visualization of vascular structures,
MRI remains the gold standard for detailed anatomical resolution
and assessment of soft tissue involvement. MRI provides superior
visualization of the relationship between the lesion and critical
structures, such as the optic nerve, orbital walls and adjacent
tissues, which is vital for complex surgical planning. Considering
these attributes, CEUS remains a complementary tool to MRI rather
than a replacement. However, the combined use of CEUS and MRI may
enhance the accuracy of orbital CVM diagnosis and management
(26). Coupled with detailed
anatomical information by MRI, the real-time imaging ability of
CEUS provides a comprehensive diagnostic approach to assess blood
flow dynamics. The combination of CEUS and MRI could result in a
more accurate preoperative assessment. Thus, this approach could
improve treatment outcomes by guiding clinicians to choose the most
appropriate surgical approach based on the specific characteristics
of lesions.
Several reports demonstrated that CEUS applied to
the orbit may result in certain adverse effects on the retina or
vision. In the present study, the parameter settings of CEUS were
set, including the mechanical index (MI; 0.06-0.08) and thermal
index (TI; <0.01), which were lower than the guidelines for the
safe use of diagnostic ultrasound equipment adopted by the European
Federation of Societies for ultrasound in Medicine and Biology
(EFSUMB). The recommended values by EFSUMB were MI of <0.7 and
TI of <1(8) to avoid the
occurrence of cavitation effects. Although the clinical application
of ocular CEUS has been carried out for >10 years, no related
reports on visual impairment appear to exist (6,10,14,27,28).
Furthermore, no precise enhancement staging of the arterial phase,
portal-venous phase and delayed phase was developed due to the
difference in the blood supply between the eye and liver. During
CEUS, the onset of enhancement time of the lesions was observed
compared with surrounding tissues. The results showed that 50
(89.2%) lesions enhanced simultaneously with or later than
surrounding tissues. Among the selected 56 orbital CVMs, 53 (94.6%)
lesions showed a progressive enhancement pattern that was similar
to the CEUS of hepatic cavernous hemangioma (29). The periphery or center of the
lesions was enhanced in the early phase with progressive fill-in
and gradual enlargement of the extent of nodular enhancement.
Despite the changes, the lesions eventually showed complete or
incomplete fill-in, which were not observed in the CEUS of other
orbital space-occupying lesions. The other 3 lesions showed
diffused enhancement without a progressive enhancement pattern. It
could be speculated that the changes may be related to the larger
sinus cavity inside of the venous malformation in pathology, which
should be a high-flow type. In the present study, 54 (96.4%)
lesions eventually showed incomplete enhancement, namely
inhomogeneity enhancement. Consistent with the report by Rootman
and Rootman, orbital CVMs were more prone to intraluminal
thrombosis (30).
In conclusion, the conventional ultrasound
manifestations of orbital CVM may be similar to those of other
orbital space-occupying lesions. The CEUS of orbital CVM showed a
typical progressive enhancement pattern with an inhomogeneous
enhancement at the peak time. The combination of the two image
features could be highly characteristic, showing great value in the
preoperative qualitative diagnosis. However, one of the limitations
of the present study is the lack of statistical analysis. This was
primarily due to the different characteristics of two diagnostic
methods employed. Conventional ultrasound and CEUS differ
significantly in their approaches and observational parameters.
Conventional ultrasound focuses on the detection of the lesion's
size, morphology, echogenicity and blood flow, whereas CEUS
involves the administration of contrast agents to evaluate the
lesion's perfusion characteristics after enhancement. As the two
methods observe entirely different parameters, a direct statistical
comparison between them was not feasible. While descriptive data
and imaging characteristics were systematically analyzed, the
absence of statistical testing precluded definitive conclusions
about associations or differences between specific subgroups.
Future studies with larger cohorts should incorporate rigorous
statistical analysis to validate the findings and assess the
diagnostic accuracy of CEUS in comparison to other modalities.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
XL, LF, QZ and HW mainly participated in the
literature search, study design, writing and critical revision, and
prepared Fig. 1, Fig. 2 and Fig. 3. QZ, HW, JC, QCC and QC mainly
participated in data collection, data analysis and data
interpretation, and prepared Tables
I and II. XL and LF checked
and confirmed the authenticity of the raw data. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
The study protocol conforms to the ethical
guidelines of the 1975 Declaration of Helsinki, as reflected in its
prior approval by the Ethics Committee of Sichuan Provincial
People's Hospital (Chengdu, China; approval no. 2017-642).
Patient consent for publication
Informed consent for the publication of imaging and
clinical data was obtained from all individual participants
included in the study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zyck S and Gould GC: Cavernous venous
malformation. [Updated 2023 Mar 27]. In. StatPearls [Internet,
Treasure Island (FL): StatPearls Publishing, 2024.
|
|
2
|
Austria QM, Tran AQ, Tooley AA, Kazim M
and Godfrey KJ: Orbital cavernous venous malformation with partial
bone encasement. Orbit. 42:352–353. 2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Snellings DA, Hong CC, Ren AA,
Lopez-Ramirez MA, Girard R, Srinath A, Marchuk DA, Ginsberg MH,
Awad IA and Kahn ML: Cerebral cavernous malformation: from
mechanism to therapy. Circ Res. 129:195–215. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Taconet S, Gorphe P and Handra-Luca A:
Adult sublingual schwannoma with angioma-like features and foam
cell vascular change. Folia Neuropathol. 52:298–302.
2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abushamat F, Dietrich CF, Clevert DA,
Piscaglia F, Fetzer DT, Meloni MF, Shiehmorteza M and Kono Y:
Contrast-enhanced ultrasound (CEUS) in the evaluation of
hemoperitoneum in patients with cirrhosis. J Ultrasound Med.
42:247–253. 2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bartolotta TV, Terranova MC, Gagliardo C
and Taibbi A: CEUS LI-RADS: A pictorial review. Insights Imaging.
11(9)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cozzi D, Agostini S, Bertelli E, Galluzzo
M, Papa E, Scevola G, Trinci M and Miele V: Contrast-enhanced
ultrasound (CEUS) in non-traumatic abdominal emergencies.
Ultrasound Int Open. 6:E76–E86. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rootman DB, Rootman J, Gregory S, Feldman
KA and Ma R: Stereotactic fractionated radiotherapy for cavernous
venous malformations (hemangioma) of the orbit. Ophthalmic Plast
Reconstr Surg. 28:96–102. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Adler DD, Carson PL, Rubin JM and
Quinn-Reid D: Doppler ultrasound color flow imaging in the study of
breast cancer: Preliminary findings. Ultrasound Med Biol.
16:553–559. 1990.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Blohm KO, Hittmair KM, Tichy A and Nell B:
Quantitative, noninvasive assessment of intra- and extraocular
perfusion by contrast-enhanced ultrasonography and its clinical
applicability in healthy dogs. Vet Ophthalmol. 22:767–777.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mu X, Wang H, Li Y, Hao Y, Wu C and Ma L:
Magnetic resonance imaging and DWI features of orbital
rhabdomyosarcoma. Eye Sci. 29:6–11. 2014.PubMed/NCBI
|
|
12
|
Wang X and Yan J: Multiple cavernous
hemangiomas of the orbit. Eye Sci. 26:48–51. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ahlawat S, Fayad LM, Durand DJ, Puttgen K
and Tekes A: International society for the study of vascular
anomalies classification of soft tissue vascular anomalies:
Survey-based assessment of musculoskeletal radiologists' use in
clinical practice. Curr Probl Diagn Radiol. 48:10–16.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bertolotto M, Serafini G, Sconfienza LM,
Lacelli F, Cavallaro M, Coslovich A, Tognetto D and Cova MA: The
use of CEUS in the diagnosis of retinal/choroidal detachment and
associated intraocular masses-preliminary investigation in patients
with equivocal findings at conventional ultrasound. Ultraschall
Med. 35:173–180. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Calandriello L, Grimaldi G, Petrone G,
Rigante M, Petroni S, Riso M and Savino G: Cavernous venous
malformation (cavernous hemangioma) of the orbit: Current concepts
and a review of the literature. Surv Ophthalmol. 62:393–403.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sadick M, Müller-Wille R, Wildgruber M and
Wohlgemuth WA: Vascular anomalies (part I): Classification and
diagnostics of vascular anomalies. Rofo. 190:825–835.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jayaram A, Lissner GS, Cohen LM and
Karagianis AG: Potential correlation between menopausal status and
the clinical course of orbital cavernous hemangiomas. Ophthalmic
Plast Reconstr Surg. 31:187–190. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yan J and Wu Z: Cavernous hemangioma of
the orbit: Analysis of 214 cases. Orbit. 23:33–40. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rootman DB, Heran MKS, Rootman J, White
VA, Luemsamran P and Yucel YH: Cavernous venous malformations of
the orbit (so-called cavernous haemangioma): A comprehensive
evaluation of their clinical, imaging and histologic nature. Br J
Ophthalmol. 98:880–888. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bonavolontà P, Fossataro F, Attanasi F,
Clemente L, Iuliano A and Bonavolontà G: Epidemiological analysis
of venous malformation of the orbit. J Craniofac Surg. 31:759–761.
2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chirapapaisan N, Ngamsombat C, Tanboon J,
Cheunsuchon P and Koohasawad S: A cavernous venous malformation of
the orbit mimicking an idiopathic orbital inflammation. Asian J
Neurosurg. 15:750–752. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Jiang W, Xue H, Wang Q, Zhang X, Wang Z
and Zhao C: Value of contrast-enhanced ultrasound and PET/CT in
assessment of extramedullary lymphoma. Eur J Radiol. 99:88–93.
2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ota Y, Aso K, Watanabe K, Einama T, Imai
K, Karasaki H, Sudo R, Tamaki Y, Okada M, Tokusashi Y, et al:
Hepatic schwannoma: Imaging findings on CT, MRI and
contrast-enhanced ultrasonography. World J Gastroenterol.
18:4967–4972. 2012.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Trenker C, Kunsch S, Michl P, Wissniowski
TT, Goerg K and Goerg C: Contrast-enhanced ultrasound (CEUS) in
hepatic lymphoma: retrospective evaluation in 38 cases. Ultraschall
Med. 35:142–148. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liu YX, Liu Y, Xu JM, Chen Q and Xiong W:
Color Doppler ultrasound and contrast-enhanced ultrasound in the
diagnosis of lacrimal apparatus tumors. Oncol Lett. 16:2215–2220.
2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhou Y, Ding J, Qin Z, Long L, Zhang X,
Wang F, Chen C, Wang Y, Zhou H and Jing X: Combination of CT/MRI
LI-RADS with CEUS can improve the diagnostic performance for HCCs.
Eur J Radiol. 149(110199)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Blohm KO, Tichy A and Nell B: Clinical
utility, dose determination, and safety of ocular contrast-enhanced
ultrasonography in horses: A pilot study. Vet Ophthalmol.
23:331–340. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Labruyere JJ, Hartley C and Holloway A:
Contrast-enhanced ultrasonography in the differentiation of retinal
detachment and vitreous membrane in dogs and cats. J Small Anim
Pract. 52:522–530. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Dietrich CF, Nolsøe CP, Barr RG,
Berzigotti A, Burns PN, Cantisani V, Chammas MC, Chaubal N, Choi
BI, Clevert DA, et al: Guidelines and good clinical practice
recommendations for contrast-enhanced ultrasound (CEUS) in the
liver-update 2020 WFUMB in cooperation with EFSUMB, AFSUMB, AIUM,
and FLAUS. Ultrasound Med Biol. 46:2579–2604. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Rootman DB, Rootman J and White VA:
Comparative histology of orbital, hepatic and subcutaneous
cavernous venous malformations. Br J Ophthalmol. 99:138–140.
2015.PubMed/NCBI View Article : Google Scholar
|