Introduction
Femtosecond laser, as an infrared laser, has the
advantages of a short action time, high instantaneous power and a
small thermal effect area. Thus, it can achieve high-precision
incisions (1). Small-incision
lenticule extraction (SMILE) uses a femtosecond laser to perform
three-dimensional scanning of the corneal stroma to form a
lenticule. The lenticule was then removed from the corneal stroma
through a small (2-4 mm) incision to correct myopia. The SMILE
procedure is safe, effective and highly predictable. Studies have
shown that it has better corneal biomechanics compared to
traditional surgery (2). Owing to
its significant clinical advantages, SMILE is being increasingly
adopted by experts. The corneal stromal lenticule is a biological
material that can be used to correct hyperopia (3,4) and
treat corneal ulcers, perforations (5,6) and
keratoconus (7-9).
Conical cornea is a common, progressive,
non-inflammatory corneal degeneration disease that typically
develops in adolescents (10).
Early refractive correction involves the use of frames and rigid
gas-permeable (RGP) lenses, whereas disease progression is
controlled by corneal collagen cross-linking. Corneal collagen
cross-linking uses chemical principles to increase the connections
between collagen fibres, thereby enhancing the biomechanics of the
cornea and controlling keratoconus progression (11,12).
High-energy UV irradiation can damage the corneal endothelium and
lenticule. Therefore, the cornea must be 400 µm or greater in
thickness before the cross-linking procedure to minimise damage to
the corneal endothelium and lenticule (13). Consequently, patients with advanced
keratoconus and thin corneas face significant treatment
limitations. Treatment options for this group of patients include
corneal transplantation or lenticule implantation, depending on the
degree of scarring (14).
Femtosecond laser-assisted lenticule transplantation
is used to treat keratoconus by implanting a surgically acquired
stromal lenticule into the recipient's stromal capsular bag through
a small 2-4 mm incision (15).
This surgical procedure is flapless, minimally invasive,
single-step and does not require postoperative sutures. Therefore,
suture scarring can be avoided. The increased thickness of the
cornea postoperatively also enhances its biomechanical strength to
a certain extent. Corneal stromal lenticule implantation for
keratoconus has several advantages and limitations. SMILE-derived
lenticules, used in myopia correction, are convex, with a thick
centre and thin edges (15). In
comparison, patients with keratoconus are characterised by a
central anterior protrusion and an increase in curvature (16). Therefore, the curvature does not
improve or even become increasingly steep despite an increase in
the thickness. This phenomenon may result in intolerance to
postoperative framed lenticules. It may also cause a poor RGP fit,
difficulty in refractive reconstruction and poor patient
satisfaction (7,8). The excimer laser can cut corneal
tissues with high precision without affecting tissues outside the
cutting area, making it highly safe (17). In the present study, excimer laser
cutting of the corneal stromal lenticule was performed. Thus, a
corneal stromal lenticule is produced, which is either parallel or
concave. Consequently, the thickness of the corneal cone can be
increased while avoiding excessive curvature during the
postoperative period. This outcome is conducive to refractive
reconstruction.
Patients and methods
Study objective and grouping
A total of 75 patients (111 eyes) who underwent
SMILE surgery at Jinan Mingshui Eye Hospital (Jinan, China) between
September 2023 and April 2024 were selected for this study. All
patients voluntarily came to Jinan Mingshui Eye Hospital for
refractive surgery, and none had received any treatment for an eye
condition. A complete ophthalmological examination was performed
before the surgery. The surgically designed spherical equivalent
lenticule was -6.75 [interquartile range (IQR): -7.00, -6.38;
range: -8.13, -5.00] D. Astigmatism in each eye did not exceed 1.00
D. A complete preoperative ophthalmological examination was
conducted. The lenticules were randomly divided into three groups
at a ratio of 1:1:1 using a random number table. Each group
consisted of 37 lenticules. Group I was cut using a 1:1 ratio
according to the equivalent spherical mirror of the lenticule
itself (diopters of the excimer laser cutting=equivalent spherical
power of the lenticule). Group II was cut using a 1:1.5 ratio
(excimer laser cutting diopter=1.5 times the equivalent spherical
lenticule). Group III was cut at a 1:2 ratio (diopters of excimer
laser cutting=2 times the equivalent spherical power of the
lenticule). After cutting, the thickness measurements of the centre
of the corneal stromal lenticule were repeated at distances of 1.5,
2 and 2.5 mm from the centre. The interval between pre- and
post-cutting measurements was recorded as the time T. The research
protocol complied with the principles of the Declaration of
Helsinki and was approved by the Medical Ethics Committee of Jinan
Mingshui Eye Hospital (Ref. Ethics/2024/004). Informed consent was
obtained from all adult participants and the guardians of juvenile
participants. A pre-experiment was conducted before the main
experiment, in which the degree of expansion of the corneal stromal
lenticule in the balanced salt solution was measured. Based on
this, the ratios were designed as a reference.
Corneal stromal lenticule acquisition
process
All patients underwent a detailed ophthalmological
examination before surgery and the same experienced physician
performed all of the surgeries. Levofloxacin eye drops
(levofloxacin bromofenac sodium; Ruilin Medicince) were routinely
administered for 1 day before surgery, with a total dosage of 5 ml.
Furthermore, local anaesthetic proparacaine hydrochloride eye drops
were applied for surface anaesthesia after rinsing the conjunctival
sac and routinely disinfecting the periocular area during
preoperative preparations, with two applications, each containing
one drop (~0.1 ml in total; concentration, 0.5%). Femtosecond laser
lenticule production and small-incision parameters included the
following: Visumax 500 kHz femtosecond Laser System (Carl Zeiss
AG); laser pulse frequency, 500 kHz; energy, 130 nJ; lenticule
cutting diameter, 6.5 mm; corneal cap thickness, 120 µm; and
small-incision length, 2 mm (18).
The removed stromal lenticules were placed on a flat surface of a
Petri dish. Subsequently, one to two drops of balanced salt
solution were added to flatten the stromal lenticules.
Measurement of corneal stromal
lenticules
Measurements were taken using an optical coherence
tomography (OCT) scanner (RTVue100-2; Kelin Instrument Co., Ltd.).
Preparations and measurements were conducted at the same suitable
temperature (temperature, 20±0.5˚C; humidity, 42±2%). The excess
liquid on the surface and sides of the lenticule was absorbed using
a surgical sponge. The preparation process was completed in 1 min.
The Petri dish was then fixed to the homemade fixation device made
from foam, which was positioned in front of the OCT. The thickness
of the corneal stromal lenticule was measured at the centre and
1.5, 2 and 2.5 mm from the centre. Immediately after the
measurement, the flat dish was placed on an Amax excimer machine
for excimer cutting and the optical zone of the cutting was set to
4 mm.
Data processing
The change in central thickness was represented by
the central thickness change (ctc). The thickness changes at 1.5,
2.0 and 2.5 mm from the centre were denoted as 1.5tc, 2tc and
2.5tc, respectively. Lenticule concavity was expressed as the
difference between the central thickness and thickness at 2 mm from
the centre (ct-2t). ct-2t values #x003C;-3 µm indicate a concave
lens, values between -3 and 3 µm indicate a parallel lens and
values >3 µm indicate a convex lens.
Statistical analysis
All data were analysed using SPSS version 27.0 (IBM
Corp.). The Shapiro-Wilk test was used to assess the normal
distribution of data. If the normal distribution and χ2
criteria were met, a one-way ANOVA was used with the Least
Significant Difference post hoc test. If the assumptions were not
met, the data were analysed using the Kruskal-Wallis test and the
Dunn's test was employed as the post hoc test. The χ2
test was used for sex in Table I.
P#x003C;0.05 was considered to indicate a statistically significant
difference.
 | Table IBasic information statistics of
patients before the operation. |
Table I
Basic information statistics of
patients before the operation.
| Parameter | Total (n=111) | Group I (n=37) | Group II (n=37) | Group III (n=37) | H-value | P-value |
|---|
| Age, years | 22 (19, 25) | 22 (21, 23) | 20 (18, 23) | 20 (20.5, 27.5) | 5.342 | 0.069 |
| Sex | | | | | 1.510 | 0.470 |
|
Male | 60 (54.1) | 18 (48.6) | 19 (51.4) | 23 (62.2) | | |
|
Female | 51 (45.9) | 19 (51.4) | 18 (48.6) | 14 (37.8) | | |
| Diopters | -6.75 (-7.00,
-6.38) | -6.88 (-7.25,
-6.57) | -6.75 (-7.00,
-6.44) | -6.5 (-7.00,
-6.07) | 5.265 | 0.072 |
| Spherical
diopters | -6.5 (-6.75,
-6.00) | -6.75 (-7.00,
-6.25) | -6.37 (-6.75,
-6.06) | -6.25 (-6.75,
-5.75) | 5.595 | 0.061 |
| Cylindrical
diopters | -0.5 (-0.75,
-0.25) | -0.50 (-0.75,
-0.25) | -0.50 (-0.75,
-0.25) | -0.50 (-0.75,
-0.25) | 2.075 | 0.354 |
Results
Basic information statistics of
patients
Participants were aged 17-35 years (23.15±4.982
years). The surgically designed equivalent spherical lenticule was
-6.75 (-7.00, -6.38) (range, -8.13 - -5.00 D). Astigmatism in each
eye did not exceed 1.00 D. Basic information statistics showed no
statistically significant differences in age, sex or diopters among
the three groups (Table I).
Comparison of pre-plastic thickness in
the three groups
No statistically significant differences were found
among the three groups in the plastic anterior centre, thickness at
distances of 1.5, 2 and 2.5 mm from the centre, or ct-2t (Table II).
 | Table IIComparison of pre-shaping thickness
among the three groups and between two groups. |
Table II
Comparison of pre-shaping thickness
among the three groups and between two groups.
| Parameter | Group I, µm | Group II, µm | Group III, µm | F/H value | P-value |
|---|
| Center [M
(P25, P75)] | 247 (225.5, 257) | 236 (216, 245) | 243 (223.5,
253.5) | 4.832 | 0.890 |
| 1.5 mm [M
(P25, P75)] | 205 (184, 220) | 189 (180, 203) | 197 (184.5,
213.5) | 5.054 | 0.080 |
| 2 mm (x̄ ± SD) | 173.162±23.367 | 162.054±18.824 | 165.622±16.914 | 3.009 | 0.053 |
| 2.5 mm [M
(P25, P75)] | 128 (118, 142) | 120 (112, 130) | 120 (111, 134) | 5.086 | 0.079 |
| ct-2t [M
(P25, P75)] | 72 (60, 80.5) | 69 (61.5, 80.5) | 72 (62, 83) | 0.663 | 0.718 |
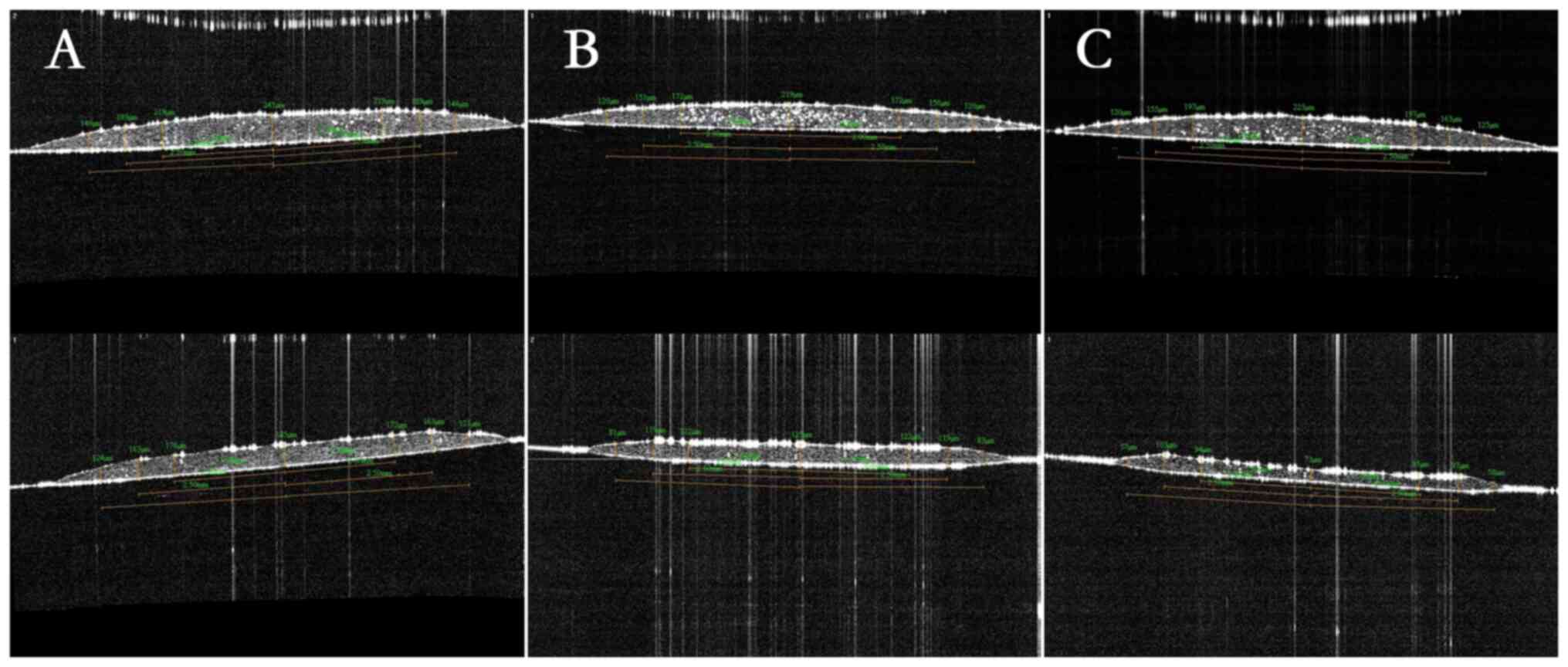
Comparison of the three groups
The cuttings of the three groups are shown in
Fig. 1. The difference between the
two measurement intervals (T) in the three groups was not
statistically significant (Table
III). The difference in ctc and 1.5tc of the three groups was
statistically significant. No statistically significant differences
were observed in the 2tc or 2.5tc values of the three groups. The
difference in ct-2t after laser plasticity was statistically
significant among the three groups (Table III).
 | Table IIIComparison of post-shaping thickness
among the three groups and between two groups. |
Table III
Comparison of post-shaping thickness
among the three groups and between two groups.
| Considerations | Group I | Group II | Group III | F/H value | P-value | a | b | c |
|---|
| ctc, µm [M
(P25, P75)] | 75 (66, 84) | 111 (100, 124) | 138 (128, 147) | 82.082 | #x003C;0.001 | #x003C;0.001 | #x003C;0.001 | #x003C;0.001 |
| 1.5tc, µm [M
(P25, P75)] | 54 (47.5,
63.5) | 73 (62, 86) | 88 (81, 94.5) | 51.623 | #x003C;0.001 | #x003C;0.001 | #x003C;0.001 | #x003C;0.001 |
| 2tc, µm (x̄ ±
SD) | 48.351±18.662 | 46.784±14.675 | 53.162±12.518 | 1.702 | 0.187 | | | |
| 2.5tc, µm [M
(P25, P75)] | 36 (32, 42) | 41 (35.5,
53.5) | 39 (34, 50) | 5.147 | 0.076 | | | |
| ct-2t, µm [M
(P25, P75)] | 38 (28, 53.5) | 6 (-3, 15.5) | -10 (-16.5,
-5) | 87.169 | #x003C;0.001 | #x003C;0.001 | #x003C;0.001 | #x003C;0.001 |
| T, min [M
(P25, P75)] | 3.27 (2.67,
4.75) | 4.1 (2.94,
4.5) | 3.69 (2.51,
4.35) | 3.071 | 0.215 | | | |
Postplasticisation ct-1/4t
After laser plasticity, Group I had a ct-2t of 38
(IQR, 28, 53.5) µm, Group II had a ct-2t of 6 (IQR, -3, 15.5) µm
and Group III had a ct-2t of -10 (IQR, -16.5, -5) µm (Table III).
Discussion
Femtosecond laser-assisted corneal lenticule
transplantation has achieved good results in the treatment of
conical corneas. Zhao et al (7), Wang et al (8) and Sun et al (9) used surface lenticule transplantation
combined with corneal collagen cross-linking to treat patients with
advanced keratoconus and thin corneas. The postoperative surface
lenticules were well-adhered, with increased corneal thickness, and
a significant reduction of irregular astigmatism. Furthermore, the
mean keratometry (K) value, steep K value and maximal postoperative
surface height value stabilised from the third month. Li et
al (19) reported a case of
corneal dilatation after laser-assisted in situ
keratomileusis (LASIK). SMILE allogeneic lenticule lamellar
transplantation was performed first, followed by corneal collagen
cross-linking surgery 4 months postoperatively. Follow-up was
maintained for 30 months. Therefore, the corneal thickness
increased and the corneal morphology stabilised. Previous studies
have collectively demonstrated the safety and efficacy of corneal
stromal lenticule implantation combined with corneal collagen
cross-linking for the treatment of keratoconus.
However, the process of effectively controlling the
further development of keratoconus can lead to a further increase
in corneal curvature in patients with the disease, thereby
resulting in difficulty in postoperative refractive reconstruction.
For instance, Zhao et al (7) used surface lenticule implantation
combined with corneal collagen cross-linking to treat a patient
with advanced keratoconus who could not tolerate an RGP contact
lens. Preoperatively, the steep K was 62.7 D and the average K was
55.4 D. At three years postoperatively, the steep K was 63.8 D,
with an average K value of 61.9 D. Wang et al (8) reported that surface lenticule
implantation combined with cross-linking for thin corneal cone
treatment resulted in a corneal curvature that was significantly
higher than that at 1 and 3 months after surgery. Li et al
(19) reported that in patients
with corneal dilatation after LASIK, the preoperative flat
keratometry (K1), steep keratometry (K2) and
maximum keratometry (Kmax) values were 57.5, 67.2 and 74.9 D,
respectively. Simultaneously, the postoperative K1,
K2 and Kmax values were 59.7, 71.7 and 82.7 D,
respectively. Sun et al (9)
reported that preoperative K1 was 55.26 D, K2
was 64.80 D and the mean K value was 59.65 D. One year after
surgery, the K1, K2 and mean K values were
62.44, 64.04 and 63.23 D, respectively. These values were
significantly higher than the preoperative values. In a recent
domestic study, Gao et al (20) used parallel lenticule row corneal
transplantation to avoid these problems. Furthermore, a
statistically significant decrease in anterior central corneal
elevation and an increase in central corneal thickness were
observed in the postoperative period. However, the scarcity of
corneal sources and shortage of donor sources for corneal
transplantation have not changed for a long time (21). The corneal stromal lenticule is an
anterior layer of tissue in the central region of the corneal
stroma. It is composed of collagen fibres arranged in an orderly
fashion, and its normal anatomical structure and physiological
functions are essential for maintaining corneal transparency and
biomechanics. The excimer laser can cut corneal tissue with high
precision without affecting tissues outside the cut area.
Therefore, this approach is considered safe (22). In the present study, an excimer
laser was used to cut the corneal stromal lenticule, which was
either parallel or concave.
In the present study, an excimer laser was used to
cut three groups of lenticules at ratios of 1:1, 1:1.5 and 1:2. The
optical zone was 4 mm, and the thickness at 1.5 mm from the centre
was within the cutting range. Furthermore, a thickness of 2 mm from
the centre represents the boundary of the cutting zone, with the
lenticule's centre at the centre of cutting. When the three groups
were compared, the differences between the ctc and 1.5 tc among the
three groups were caused by the different cutting ratios. No
differences were observed in the 2tc and 2.5 tc of the three
groups. This finding indicates that thicknesses of 2 and 2.5 mm
were probably not affected by cutting. Because all other conditions
of the three groups were consistent except for the different
cutting ratios, 2tc and 2.5tc were probably only caused by
dehydration. No difference in ct-2t was observed before laser
plastination in the three groups because ct-2t was affected by the
diopters. No differences were observed in the refraction of the
lenticules incorporated into any of the three groups. However, a
significant difference in ct-2t was observed after laser
plastination. One group had a ct-2t of 38 (IQR: 28, 53.5) µm after
laser plasticity, with a distinct convex lenticule at the centre.
The second group had a ct-2t of 6 (IQR, -3, 15.5) µm after laser
plasticity, which was still a convex lenticule in the centre but
was already very close to a parallel lenticule compared with the
two other groups. The third group had a ct-2t of -10 (IQR: -16.5,
-5) µm after laser plasticity, with a distinct concave lenticule at
the centre. This may be because the amount of tissue ablation is
affected by the corneal stromal lenticule, which swells because of
in vitro water absorption (23). This finding shows that excimer
cutting changed the morphology of the centre of the stromal
lenticule. Given the water-absorbing swelling of the stromal
lenticule in vitro, a 1:1.5 ratio of excimer cutting can be
used to obtain a stromal lenticule with a centre close to a
parallel lenticule. Similarly, a 1:2 excimer cutting ratio can be
used to obtain a stromal lenticule with a concave lenticule at the
centre. We hypothesize that this technology can also customize the
corneal stromal lenticule according to the different needs of
patients and then reuse it, thus transforming the traditional
corneal laser surgery from the ‘subtraction’ mode of ‘thinning and
weakening’ to the ‘addition’ mode of ‘thickening and
strengthening’. Additionally, we hypothesize that this
transformation not only provides a new treatment approach for
patients with thin corneal refractive errors, but also opens up new
possibilities for the treatment of corneal diseases. Our
experimental results indicated that the use of excimer
laser-plasticised corneal stromal lenticules for keratoconus
treatment is highly conducive to refractive reconstruction because
it avoids excessive postoperative curvature while adding thickness
to the conical cornea.
However, this study still has certain limitations.
The current research is only confined to in vitro
experiments of corneal stromal lenticules and has not yet conducted
in-depth exploration of the series of changes after their
implantation into the recipient's capsular bag. Whether the corneal
stromal lenticules, after being shaped by excimer laser, can
achieve the ideal refractive correction effect, effectively
increase the biomechanical strength of the cornea and their
long-term stability and biocompatibility in the body all need to be
evaluated through more clinical experiments and long-term
follow-ups. Future research can further study the refractive effect
and biomechanical changes of corneal stromal lenticules after
implantation through animal models or clinical trials; optimize the
cutting parameters by comparing the effects of different cutting
ratios on the microstructure and biomechanical properties of
corneal stromal lenticule; and conduct a comprehensive assessment
of the long-term performance of corneal stromal lenticules in the
body by combining advanced imaging techniques and biomechanical
analysis methods to ensure their safety and effectiveness. These
studies are expected to further improve the corneal stromal
lenticule implantation technique and provide more reliable and
efficient treatment options for refractive and corneal
diseases.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YL contributed to the study conception and design.
JH, SL, SY, XL and XW acquired and interpreted study data. XW
conducted the statistical analysis and drafted the manuscript. YL
and JH provided critical manuscript revisions and administrative,
technical support. YL supervised the study. XW and YL checked and
confirmed the authenticity of the raw data. All authors have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
The study protocol conformed to the tenets of
Declaration of Helsinki and was approved by the Human Ethics
Committee of Jinan Mingshui Eye Hospital (approval no. Ref.
Ethics/2024/004). Informed consent was obtained in writing from all
adult participants and the guardians of juvenile participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Akimoto K, Tsuichihara S, Takamatsu T,
Soga K, Yokota H, Ito M, Gotoda N and Takemura H: Evaluation of
laser-induced plasma ablation focusing on the difference in pulse
duration. Conf Proc IEEE Eng Med Biol Soc. 2019:6987–6990.
2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Reinstein DZ, Archer TJ and Randleman JB:
Mathematical model to compare the relative tensile strength of the
cornea after PRK,LASIK, and small incision lenticule extraction. J
Refract Surg. 29:454–460. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sun L, Yao P, Li M, Shen Y, Zhao J and
Zhou X: The safety and predictability of implanting autologous
lenticule obtained by SMILE for hyperopia. J Refract Surg.
31:374–379. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Dong Y, Hou J, Zhang J, Lei Y, Yang X and
Sun F: Epithelial thickness remodeling after small incision
lenticule intrastromal keratoplasty in correcting hyperopia
measured by RTVue OCT. BMC Ophthalmol. 24(13)2024.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wu F, Jin X, Xu Y and Yang Y: Treatment of
corneal perforation with lenticules from small incision lenticule
extraction surgery: A preliminary study of 6 patients. Cornea.
34:658–663. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Jiang Y, Li Y, Liu XW and Xu J: A novel
tectonic keratoplasty with femtosecond laser intrastromal lenticule
for corneal ulcer and perforation. Chin Med J (Engl).
129:1817–1821. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhao J, Shang J, Zhao Y, Fu D, Zhang X,
Zeng L, Xu H and Zhou X: Epikeratophakia using small-incision
lenticule extraction lenticule addition combined with corneal
crosslinking for keratoconus. J Cataract Refract Surg.
45:1191–1194. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang KN, Fu MJ, Zhao JJ, Wang YC, Wang JH,
Zhang HR and Wang R: Corneal surface mirror (stromal lens)
implantation combined with corneal collagen cross-linking for the
treatment of keratoconus: A case report. J Clin Ophthalmol.
30:552–553. 2022.
|
|
9
|
Sun X, Shen D, Cai J, Zhang CN and Wei W:
A case of keratoconus treated by femtosecond laser assisted
implantation of corneal allogenic matrix lens combined with corneal
collagen crosslinking. Chin J Optom Ophthalmol Vis Sci. 24:472–474.
2022.
|
|
10
|
Ferrari G and Rama P: The keratoconus
enigma: A review with emphasis on pathogenesis. Ocul Surf.
18:363–373. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wollensak G, Spoerl E and Seiler T:
Riboflavin/ultraviolet-a-induced collagen crosslinking for the
treatment of keratoconus. Am J Ophthalmol. 135:620–627.
2003.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Padmanabhan P and lsheikh A: Keratoconus:
A biomechanical perspective. Curr Eye Res. 48:121–129.
2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wollensak G, Spörl E, Reber F, Pillunat L
and Funk R: Corneal endothelial cytotoxicity of riboflavin/UVA
treatment in vitro. Ophthalmic Res. 35:324–328. 2003.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Matthyssen S, Van den Bogerd B,
Dhubhghaill SN, Kompen C and Zakaria N: Corneal regeneration: A
review of stromal replacements. Acta Biomater. 69:31–41.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fasolo A, Galzignato A, Pedrotti E,
Chierego C, Cozzini T, Bonacci E and Marchini G: Femtosecond
laser-assisted implantation of corneal stroma lenticule for
keratoconus. Int Ophthalmol. 41:1949–1957. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sun X, Zhang H, Shan M, Dong Y, Zhang L,
Chen L and Wang Y: Comprehensive transcriptome analysis of patients
with keratoconus highlights the regulation of immune responses and
inflammatory processes. Front Genet. 13(782709)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Shah SU and Gritz DC: Application of the
femtosecond laser LASIK microkeratome in eye banking. Curr Opin
Ophthalmol. 23:257–263. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Reinstein DZ, Archer TJ and Gobbe M: Small
incision lenticule extraction (SMILE) history, fundamentals of a
new refractive surgery technique and clinical outcomes. Eye Vis
(Lond). 1(3)2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Li M, Yang D, Zhao F, Han T, Li M, Zhou X
and Ni K: Thirty-month results after the treatment of post-LASIK
ectasia with allogenic lenticule addition and corneal
cross-linking: A case report. BMC Ophthalmol.
18(294)2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Gao H, Liu M, Li N, Chen T, Qi X, Xie L
and Shi W: Femtosecond laser-assisted minimally invasive lamellar
keratoplasty for the treatment of advanced keratoconus. Clin Exp
Ophthalmol. 50:294–302. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gain P, Jullienne R, He Z, Aldossary M,
Acquart S, Cognasse F and Thuret G: Global survey of corneal
transplantation and eye banking. JAMA Ophthalmol. 134:167–173.
2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Laurent JM, Schallhorn SC, Spigelmire JR
and Tanzer DJ: Stability of the laser in situ keratomileusis
corneal flap in rabbit eyes. J Cataract Refract Surg. 32:1046–1051.
2006.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wang Q, Rao J, Zhang M, Zhou L, Chen X, Ma
Y, Guo H, Gu J, Wang Y and Zhou Q: SMILE-derived corneal stromal
lenticule: Experimental study as a corneal repair material and drug
carrier. Cornea: Jan 21, 2025 (Epub ahead of print).
|