Introduction
In clinical practice, patients who present with
cough as the sole or primary symptom lasting >8 weeks and
exhibit no marked abnormalities on chest radiographs are often
diagnosed with chronic cough (1,2).
Chronic cough affects ~10% of the general population and accounts
for over one-third of visits to respiratory outpatient clinics in
China (3). Epidemiological studies
of the Chinese population report a prevalence of chronic cough
ranging from 2.0 to 28.3% (3),
with the majority of cases occurring in individuals aged 30-40
years and a nearly equal sex distribution (4).
Chronic cough has diverse etiologies, with common
causes including cough variant asthma (CVA), upper airway cough
syndrome (UACS), eosinophilic bronchitis (EB), gastroesophageal
reflux cough (GERC) and atopic cough. These conditions account for
70-95% of cases, with multicenter data identifying CVA as the most
prevalent, responsible for 32.6% of cases in China (5,6). The
prevalence of GERC is rising, likely due to changes in diet and
lifestyle. Despite thorough evaluation, 8.4% of chronic cough cases
remain unexplained (7). Reported
risk factors for chronic cough include air pollution, seasonal
changes, dietary triggers, occupational exposure, allergens,
smoking, female sex, advanced age, obesity and certain medications
(8).
CVA typically responds well to anti-asthmatic
therapy, including inhaled corticosteroids (ICSs) and leukotriene
receptor antagonists. Early diagnosis and treatment are crucial, as
untreated CVA may progress to classic asthma. Diagnosis relies on
objective evidence of airway hyperresponsiveness (AHR), such as
that obtained by bronchial provocation testing (9). Gastroesophageal reflux disease (GERD)
and CVA frequently coexist and may exacerbate each other: Reflux
can aggravate AHR, while persistent coughing may increase
intra-abdominal pressure, promoting reflux (10,11).
This bidirectional relationship is supported by studies showing
that gastric contents can induce bronchoconstriction via
vagally-mediated reflexes and microaspiration, thereby contributing
to airway inflammation and hyperresponsiveness (12,13).
Conversely, coughing in CVA may increase the frequency of transient
lower esophageal sphincter relaxations, facilitating reflux
episodes and establishing a cycle of mutual exacerbation (14). This interrelationship highlights
the importance of a combined therapeutic approach. In clinical
practice, the management of GERC typically involves lifestyle
modifications, acid suppression and prokinetic therapy, with
surgical intervention considered in refractory cases (10).
Given the multifactorial nature of chronic cough and
its often prolonged course, effective management requires accurate
diagnosis and individualized treatment plans (15,16).
However, misdiagnosis and inadequate treatment remain common in
primary care, largely due to limited diagnostic tools and clinical
experience. The present report describes a case of CVA complicated
by GERC, manifesting as persistent dry cough. The case underscores
the importance of the flexible application of clinical guidelines
in primary care and highlights that timely referral to specialized
centers is necessary when patients have an unclear diagnosis or
poor response to empirical therapy. Enhancing diagnostic and
therapeutic capacity in primary care is essential for improving
outcomes in patients with chronic cough.
Case report
Case presentation
A 30-year-old married woman with a college
education, who worked as a manual laborer, presented to the
Department of General Medicine, Shenzhen Longhua District Central
Hospital (Shenzhen, China) in June 2021, with a history of chronic,
non-productive cough lasting >1 year. The cough was
predominantly nocturnal and irritating, without identifiable
triggers. Associated symptoms included throat itchiness, a foreign
body sensation, and mild postprandial acid reflux. The patient
denied heartburn, recurrent sore throat, nasal congestion,
rhinorrhea, postnasal drip, chest pain, hemoptysis, palpitations,
shortness of breath, fever, night sweats, dizziness or headache.
Prior treatments with anti-infectives and antitussives at a
community clinic were ineffective, prompting referral for further
evaluation. Despite sleep disturbances due to nocturnal coughing
episodes, the general condition, appetite and weight of the patient
remained stable.
Medical and personal history
The patient reported no history of chronic
respiratory, cardiovascular, metabolic or gastrointestinal
diseases, and had no prior history of major infections, surgeries
or blood transfusions. Allergies included seafood and eggs, which
caused cutaneous reactions, but no drug allergies were reported.
The patient also had no history of angiotensin-converting enzyme
inhibitor use, did not smoke, consume alcohol, or report exposure
to occupational or environmental irritants. Her menstrual and
obstetric history were unremarkable, and her psychosocial
background was stable.
Physical examinations
On admission, vital signs were within normal limits:
Temperature 36.6˚C, pulse 78 bpm, respiratory rate 20 breaths/min,
blood pressure 102/67 mmHg and BMI 19.53 kg/m². Throat examination
revealed no congestion or tonsillar enlargement, and there was no
tenderness over the sinus regions. Chest examination revealed
slightly coarse breath sounds bilaterally, without rales or
wheezes. Cardiovascular, abdominal and neurologic examinations
detected no abnormalities. No peripheral edema was observed.
Laboratory and imaging analyses
Routine laboratory tests were largely unremarkable,
with a mildly reduced hemoglobin level of 111 g/l, white blood cell
count of 4.4x109/l, platelet count of
170x109/l, neutrophil level of 63.9% and eosinophil
count of 0.1x109/l. A positive Mycoplasma
pneumoniae IgM titer of 1:80 suggested recent or past
infection. Fractional exhaled nitric oxide (FeNO) testing revealed
elevated levels, with FeNO measured at a flow rate of 50 ml/sec
yielding a value of 50 parts per billion, suggestive of
eosinophilic airway inflammation.
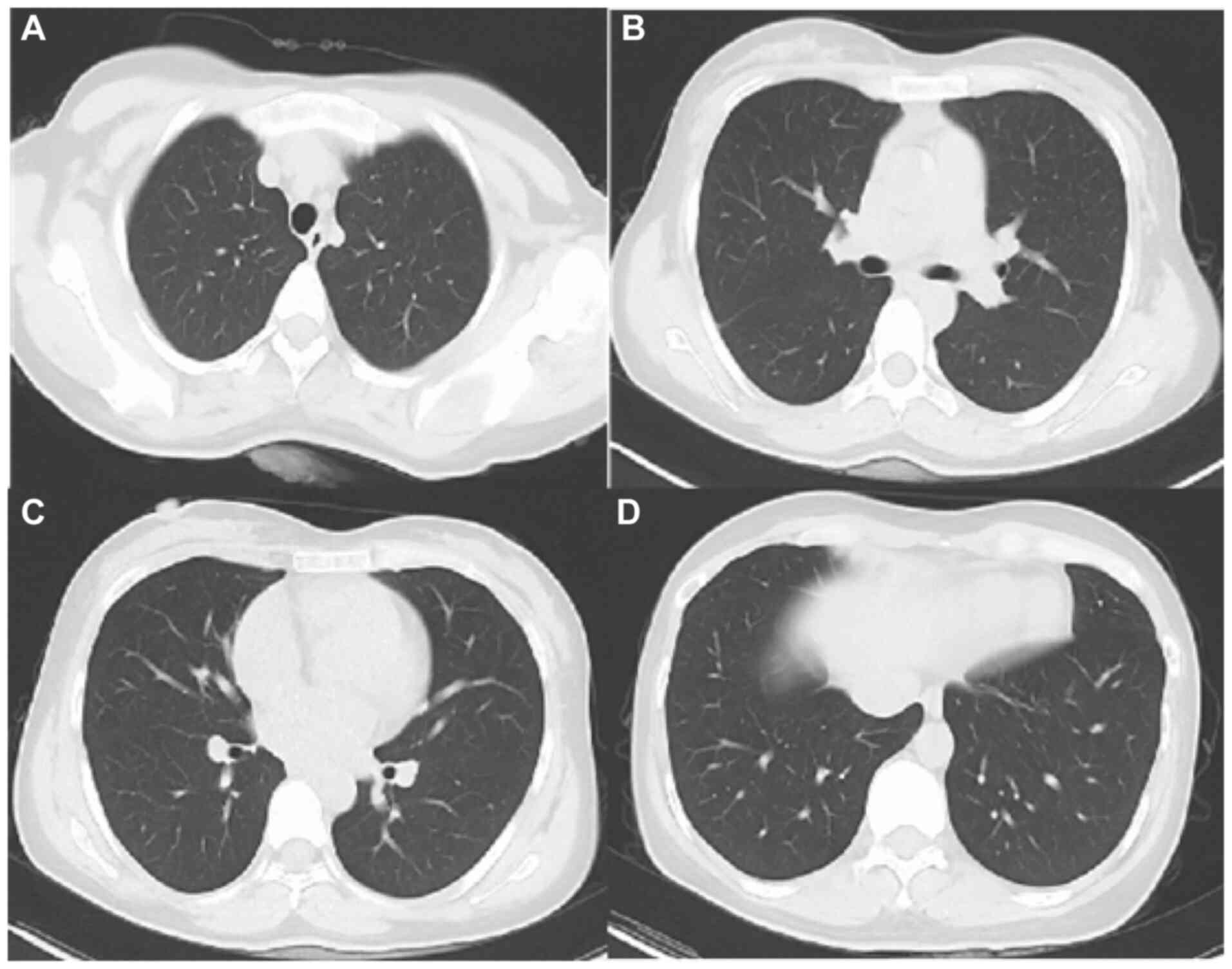
Chest computed tomography (Fig. 1) revealed no evidence of pulmonary
infiltrates, nodules or structural abnormalities. Pulmonary
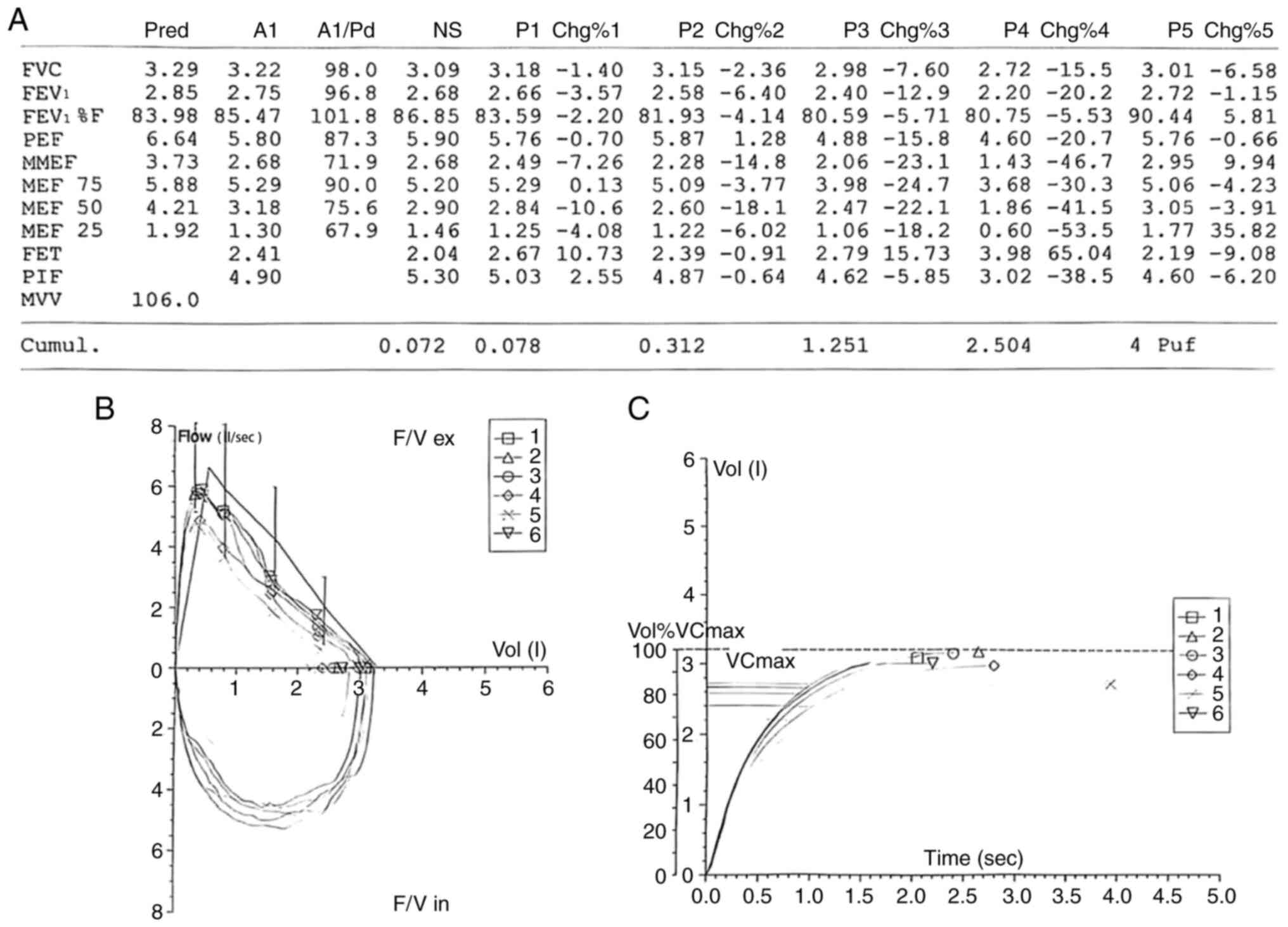
function testing (Fig. 2)
demonstrated normal baseline spirometry but a positive bronchial
provocation response; the forced expiratory volume in 1 sec
(FEV1) declined by >20% after a cumulative
acetylmethacholine dose of 2.504 mg, which is indicative of
AHR.
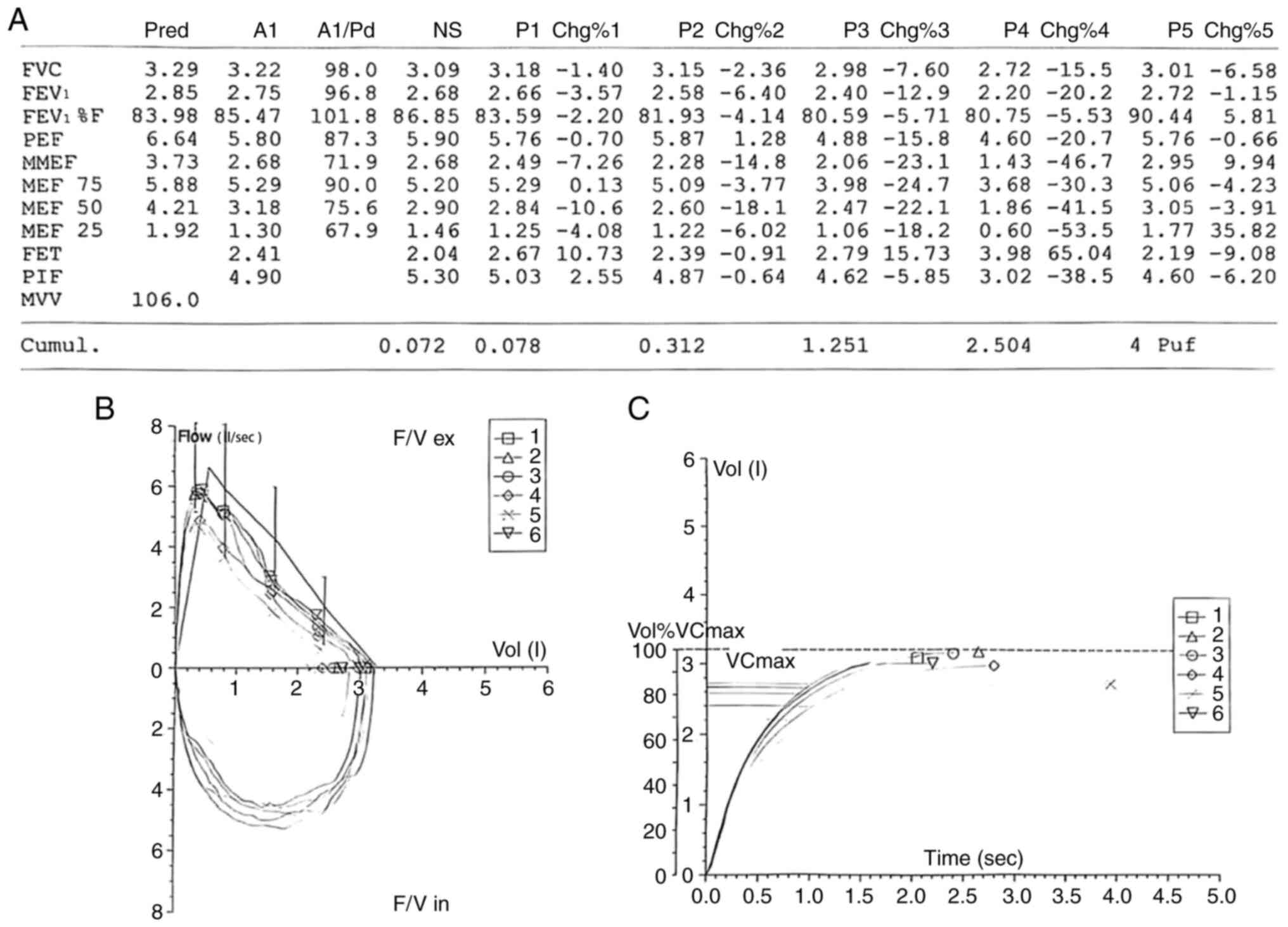 | Figure 2Pulmonary function test with
acetylmethacholine bronchial provocation. Baseline spirometry
demonstrated normal ventilatory function with a normal
FEV1. However, during the acetylmethacholine challenge,
progressive airway hyperresponsiveness was observed. A ≥20% decline
in FEV1 occurred at a cumulative acetylmethacholine dose
of 2.504 mg, confirming a positive bronchial provocation result
consistent with cough-variant asthma. The provocative dose causing
a 20% reduction in FEV1 is indicative of heightened
bronchial sensitivity. (A) Table summarizing spirometric
measurements across multiple test repetitions. (B) Flow-volume loop
graph; curves labeled 1-6 correspond to repeated test attempts. (C)
Volume-time curve; curves labeled 1-6 correspond to repeated test
attempts. FEV1, forced expiratory volume in 1 sec; FVC,
forced vital capacity; FEV1%F, FEV1/FVC ratio, the
percentage of the forced vital capacity that is exhaled in the
first second; PEF, peak expiratory flow; MMEF, maximal
mid-expiratory flow; MEF 75/50/25, maximum expiratory flow at
75/50/25% of FVC; FET, forced expiratory time; PIF, peak
inspiratory flow; MVV, maximum voluntary ventilation; Cumul.,
cumulative; F/V ex, flow/volume during exhalation; F/V in,
flow/volume during inhalation; Vol, volume; VCmax, maximum vital
capacity; Vol%VCmax, volume as a percentage of VCmax. Pred,
predicted value; A1, measured value at baseline; A1/Pred, measured
value as a percentage of predicted; P1-P5, values obtained during
different test phases, including post-bronchial provocation and
post-bronchodilator administration; Chg%1-5, percentage change in
measured values compared to baseline, reflecting response over
successive test repetitions. |
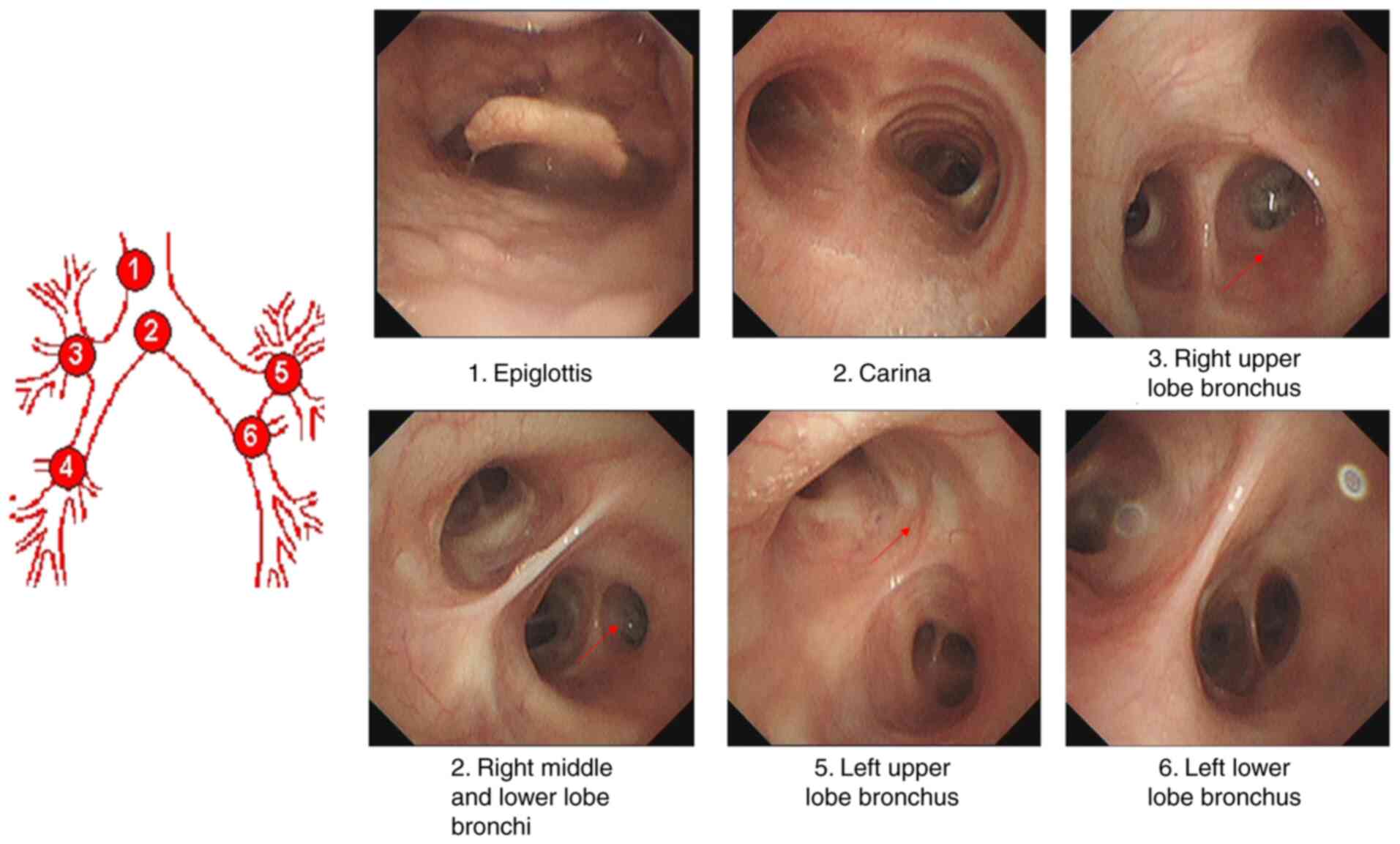
Esophagogastroduodenoscopy revealed chronic
non-atrophic gastritis. Fiberoptic bronchoscopy (Fig. 3) revealed hyperemia and edema of
the mucosa in the right and left main bronchi and their branches,
with no evidence of tuberculosis, neoplasia or fungal infection.
Bronchoalveolar lavage cultures were negative. Fiberoptic
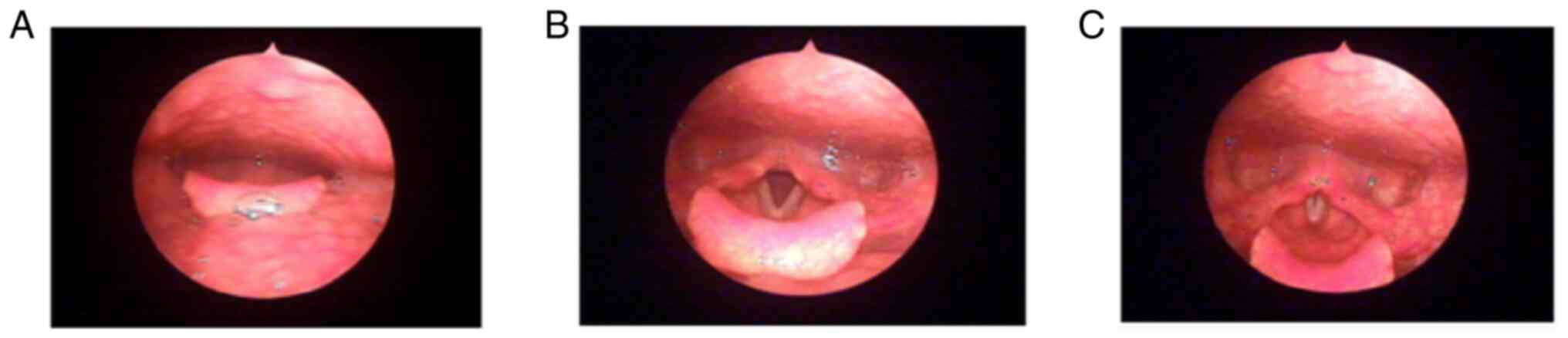
laryngoscopy (Fig. 4) showed
chronic mucosal edema and erythema in the interarytenoid region and
vocal cords, consistent with reflux laryngitis.
Diagnosis
Based on clinical presentation and objective
findings, the patient was diagnosed with CVA and GERC. The
diagnosis of CVA was supported by characteristic features,
including chronic nocturnal dry cough, the absence of wheezing or
dyspnea, elevated FeNO levels, and a positive bronchial provocation
test. Structural lung diseases and infections were excluded by
imaging and bronchoscopy. GERC was diagnosed based on postprandial
acid reflux and throat irritation, along with laryngoscopic
evidence of reflux laryngitis. Although the patient denied typical
GERD symptoms such as heartburn, the presence of extra-esophageal
manifestations supported this diagnosis.
Differential diagnosis
UACS was considered due to the persistent dry,
irritative cough. However, the absence of recurrent nasal
congestion, rhinorrhea or postnasal drip made this diagnosis less
likely. EB was also evaluated given the chronic dry cough and
absence of abnormal lung CT findings. However, the presence of
airway hyperresponsiveness on bronchial provocation testing
rendered EB an unlikely diagnosis, since it is typically
characterized by normal airway responsiveness.
Treatment and management
The treatment plan integrated both
non-pharmacological and pharmacological approaches, aiming to
alleviate symptoms, address underlying causes and promote long-term
disease control. The patient was advised to avoid environmental
irritants such as secondhand smoke, harmful gases and known
allergens, and to modify her daily habits by not lying down
immediately after meals to help manage reflux symptoms. In
addition, regular physical activity was encouraged to improve
overall health and strengthen immunity, with the aim of preventing
respiratory infections. Psychological support was provided to ease
anxiety associated with her chronic symptoms and disrupted sleep,
contributing to overall symptom relief and quality of life. To
ensure continuity of care, the patient was advised to establish a
family doctor contract with a community health center for regular
follow-up and monitoring.
During hospitalization, pharmacological treatment
primarily targeted CVA. On the second day of admission, after
completion of the bronchial provocation test, the patient was
started on terbutaline (5 mg) and budesonide (1 mg) via
nebulization every 8 h, along with oral montelukast (10 mg) once
nightly. For symptomatic relief, dextromethorphan hydrobromide and
guaifenesin syrup (15 ml) was administered three times daily. On
the fourth day of hospitalization, treatment for GERD was
initiated, consisting of omeprazole (20 mg) twice daily and
domperidone (10 mg) three times daily to suppress gastric acid and
enhance gastrointestinal motility.
After a 13-day hospitalization, the patient was
discharged. At discharge, the treatment regimen was adjusted to
ensure long-term control of the two conditions. The patient was
transitioned to budesonide-formoterol inhalation powder twice daily
for asthma maintenance, and the montelukast therapy was continued.
GERD management with omeprazole and domperidone was also
maintained. Comprehensive instructions on inhaler use, medication
adherence and potential side effects were provided to optimize
therapeutic effectiveness and safety.
Follow-up
By the time of discharge, the patient reported a
marked improvement in cough severity. Follow-up through telephone
and app-based messages confirmed high compliance with the treatment
regimen. At the 6-month follow-up, the patient reported complete
resolution of the chronic cough, defined as the absence of daytime
and nighttime coughing episodes for at >4 consecutive weeks. In
addition, the patient experienced improved sleep quality and no
recurrence of gastrointestinal symptoms.
Discussion
The present case report describes a young female
patient with a chronic, non-productive cough and an allergic
predisposition, ultimately diagnosed with CVA complicated by
subclinical GERD. The patient initially presented with features
typical of CVA, including a persistent, dry, irritating cough, and
no evident radiographic or ventilatory abnormalities. Elevated FeNO
levels and a positive bronchial provocation test supported the CVA
diagnosis, while fiberoptic bronchoscopy ruled out other possible
etiologies such as bronchial tuberculosis, foreign bodies or airway
tumors.
Despite the initiation of standard CVA treatment,
including an ICS, a leukotriene receptor antagonist and a cough
suppressant, the patient's response was limited. Notably, she also
reported symptoms suggestive of gastroesophageal reflux, and the
laryngoscopy findings were consistent with reflux laryngitis. These
observations prompted a shift in diagnostic focus, highlighting
GERD as a potential exacerbating factor. Following a 10-day course
of anti-reflux therapy with omeprazole and domperidone, her
symptoms significantly improved, suggesting an important role of
GERD in the clinical presentation.
The delayed recognition of GERD was attributable to
the absence of classic symptoms such as heartburn or regurgitation.
The initial therapy was focused solely on CVA; however,
GERD-induced airway hypersensitivity and inflammation likely
compromised asthma control. Additionally, the typically delayed
onset of extra-esophageal symptom relief with the proton pump
inhibitor (PPI) omeprazole may have masked the early benefits of
anti-reflux therapy. Ultimately, a combined pathophysiology-based
approach targeting both CVA and GERD was necessary to achieve
symptom resolution.
The present case exemplifies the diagnostic
complexity of overlapping CVA and GERD, particularly when reflux
presents atypically. While the initial focus on CVA was reasonable
given the patient's allergic history and positive bronchial
challenge test, the limited response prompted a broader evaluation.
Gastroenterology consultation was prompted by the laryngoscopic
findings and clinical suspicion, and confirmed subclinical GERD.
Interdisciplinary collaboration subsequently enabled a refined
diagnostic approach and the initiation of tailored anti-reflux
therapy which, in combination with asthma-directed treatment, led
to progressive and ultimately sustained symptom relief.
The roles of the respiratory and gastroenterology
departments were clearly delineated throughout the care of the
patient. The respiratory team conducted the initial assessment,
pulmonary function testing, FeNO measurement and bronchial
provocation testing. Following limited response to initial
treatment, the gastroenterology team was consulted to assess
potential reflux pathology, interpret laryngoscopy results, and
initiate acid-suppressive and prokinetic therapy. Although no
formal joint consultations were conducted, close communication
between the two departments ensured coordinated management and
appropriate follow-up planning.
Importantly, the present case highlights that GERD
should be considered in patients with chronic cough who are
unresponsive to conventional asthma therapies, even in the absence
of typical gastrointestinal symptoms. While GERD and CVA are each
well-established causes of chronic cough, their coexistence is
relatively common and clinically relevant. However, atypical
presentations, such as chronic cough in young female patients
without heartburn or regurgitation (17,18),
may delay diagnosis and treatment, particularly in primary care
settings. Extra-esophageal manifestations such as chronic cough
occur in up to 30-40% of patients with GERD and are frequently
underdiagnosed (18). Unlike most
reports that address CVA and GERD separately, the present case
demonstrates the diagnostic value of recognizing their overlap and
the therapeutic efficacy of a sequential, physiology-guided dual
treatment strategy.
Another important aspect is the role of
multidisciplinary collaboration. Coordinated care between
respiratory and gastrointestinal specialists enabled a tailored
treatment strategy in the present case, with monitoring for
potential long-term effects, such as bone loss associated with ICS
and PPI use. This underscores the value of integrated,
patient-centered care in managing complex overlapping
conditions.
The successful use of telemedicine played a crucial
role in the follow-up of the patient. Remote monitoring through
structured questionnaires and video consultations facilitated
continuity of care, reinforced adherence and enabled timely
interventions, which are particularly beneficial in settings with
limited access to in-person services.
The present case also highlights the importance of
clinical reasoning and flexible diagnostic strategies in
resource-limited environments. While advanced diagnostic tools such
as 24-h pH monitoring or induced sputum eosinophil counts were
unavailable, clinical assessment, FeNO measurements and
laryngoscopic findings effectively guided the diagnosis. The
achievement of a favorable response further validated this
pragmatic approach.
However, several limitations must be acknowledged. A
major constraint was the lack of objective pre- and post-treatment
comparison data, including follow-up FeNO levels, spirometry
parameters (e.g., FEV1) and standardized cough scores.
This was primarily due to the patient's early discharge, which was
prompted by significant symptom relief, as well as a need to return
to work in another city. As a result, follow-up was conducted
remotely via telephone, limiting the ability of the medical team to
quantify the treatment response using physiological measures.
Additionally, although initial laboratory tests, such as eosinophil
counts and Mycoplasma pneumoniae antibody titers, supported
the diagnostic process, serial monitoring of these indicators was
not conducted, which restricts the ability to associate treatment
effects with biomarker trends. These limitations reflect the
challenges of conducting detailed longitudinal assessments in
resource-limited or remote follow-up settings.
However, the present case highlights several
important considerations for clinical practice. For primary care
physicians, it emphasizes the importance of considering GERD as a
potential contributor to chronic cough, even in the absence of
classical gastrointestinal symptoms, particularly when patients do
not respond to standard asthma treatments. For pulmonologists, the
case supports the adoption of a pathophysiology-based diagnostic
and therapeutic approach for the management of complex or
refractory cases of chronic cough. For multidisciplinary teams, it
illustrates the practical benefits of shared decision-making and
role-specific expertise. Furthermore, at the healthcare system
level, it underscores the value of integrating telemedicine into
the follow-up and fostering multidisciplinary collaboration to
improve the diagnosis, treatment and long-term management of
overlapping chronic conditions.
In conclusion, while CVA and GERD are each common
conditions individually, the novelty of the present case lies in
their atypical concurrent presentation in a young female with no
classic reflux symptoms. In addition, the case highlights the
dynamic diagnostic shift and effective cross-specialty
collaboration that led to symptom resolution without invasive
testing. This reinforces the importance of a systematic,
individualized approach when evaluating chronic cough, which is a
frequently encountered but diagnostically challenging condition in
clinical practice.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the Key Laboratory of
Personalized Precision Treatment for Elderly Coronary Heart Disease
[grant no. Shen Long Hua Ke Chuang Ke Ji Zi (2024) No. 2] and by
the Key Disciplines Program of Shenzhen Longhua District Central
Hospital.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FY and WG were responsible for clinical data
collection, patient assessment and data analysis. XQ assisted with
clinical evaluations and manuscript preparation. XC and LN
supervised the clinical management of the patient, contributed to
manuscript drafting and provided critical revisions. FY and WG
confirm the authenticity of all the raw data. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
This case report was reviewed and approved by Ethics
Committee of Shenzhen Longhua District Central Hospital (Shenzhen,
China; approval no. 2024-096-01).
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and the accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Irwin RS, French CL, Chang AB and Altman
KW: CHEST Expert Cough Panel*. Classification of cough as a symptom
in adults and management algorithms. Chest. 153:196–209.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lai K, Chen R, Lin J, Huang K, Shen H,
Kong L, Zhou X, Luo Z, Yang L, Wen F and Zhong N: A prospective,
multicenter survey on causes of chronic cough in China. Chest.
143:613–620. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Liang H, Ye W, Wang Z, Liang J, Yi F,
Jiang M and Lai K: Prevalence of chronic cough in China: A
systematic review and meta-analysis. BMC Pulm Med.
22(62)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Long L and Lai K: Characteristics of
Chinese chronic cough patients. Pulm Pharmacol Ther.
57(101811)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Katz PO, Dunbar KB, Schnoll-Sussman FH,
Greer KB, Yadlapati R and Spechler SJ: ACG clinical guideline for
the diagnosis and management of gastroesophageal reflux disease. Am
J Gastroenterol. 117:27–56. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Iwakiri K, Fujiwara Y, Manabe N, Ihara E,
Kuribayashi S, Akiyama J, Kondo T, Yamashita H, Ishimura N,
Kitasako Y, et al: Evidence-based clinical practice guidelines for
gastroesophageal reflux disease 2021. J Gastroenterol. 57:267–285.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lai K, Tang J, Zhan W, Li H, Yi F, Long L,
Zhou J, Chen X, Huang L, Sun Z, et al: The spectrum, clinical
features and diagnosis of chronic cough due to rare causes. J
Thorac Dis. 13:2575–2582. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang J, Perret JL, Chang AB, Idrose NS,
Bui DS, Lowe AJ, Abramson MJ, Walters EH, Lodge CJ and Dharmage SC:
Risk factors for chronic cough in adults: A systematic review and
meta-analysis. Respirology. 27:36–47. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Brannan JD and Lougheed MD: Airway
hyperresponsiveness in asthma: Mechanisms, clinical significance,
and treatment. Front Physiol. 3(460)2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Niimi A: Cough associated with
gastro-oesophageal reflux disease (GORD): Japanese experience. Pulm
Pharmacol Ther. 47:59–65. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wu J, Ma Y and Chen Y: GERD-related
chronic cough: Possible mechanism, diagnosis and treatment. Front
Physiol. 13(1005404)2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Morice AH, Millqvist E, Bieksiene K,
Birring SS, Dicpinigaitis P, Domingo Ribas C, Hilton Boon M, Kantar
A, Lai K, McGarvey L, et al: ERS guidelines on the diagnosis and
treatment of chronic cough in adults and children. Eur Respir J.
55(1901136)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kahrilas PJ, Altman KW, Chang AB, Field
SK, Harding SM, Lane AP, Lim K, McGarvey L, Smith J and Irwin RS:
CHEST Expert Cough Panel. Chronic cough due to gastroesophageal
reflux in adults. Chest. 150:1341–1360. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sontag SJ: Why do the published data fail
to clarify the relationship between gastroesophageal reflux and
asthma? Am J Med. 108 (Suppl 4a):159S–169S. 2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Smith JA: The therapeutic landscape in
chronic cough. Lung. 202:5–16. 2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Arinze JT, Van Der Veer T, Bos D, Stricker
B, Verhamme KMC and Brusselle G: Epidemiology of unexplained
chronic cough in adults: A population-based study. ERJ Open Res.
9:00739–02022. 2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hránková V, Balner T, Gubová P, Staníková
L, Zeleník K and Komínek P: Narrative review of relationship
between chronic cough and laryngopharyngeal reflux. Front Med
(Lausanne). 11(1348985)2024.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Durazzo M, Lupi G, Cicerchia F, Ferro A,
Barutta F, Beccuti G, Gruden G and Pellicano R: Extra-esophageal
presentation of gastroesophageal reflux disease: 2020 update. J
Clin Med. 9(2559)2020.PubMed/NCBI View Article : Google Scholar
|