|
1
|
Tazuma S, Unno M, Igarashi Y, Inui K,
Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, et
al: Evidence-based clinical practice guidelines for cholelithiasis
2016. J Gastroenterol. 52:276–300. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Unalp-Arida A and Ruhl CE: Burden of
gallstone disease in the United States population: Prepandemic
rates and trends. World J Gastrointest Surg. 16:1130–1148.
2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Li S, Guizzetti L, Ma C, Shaheen AA, Dixon
E, Ball C, Wani S and Forbes N: Epidemiology and outcomes of
choledocholithiasis and cholangitis in the United States: Trends
and Urban-rural variations. BMC Gastroenterol.
23(254)2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Molvar C and Glaenzer B:
Choledocholithiasis: Evaluation, treatment, and outcomes. Semin
Intervent Radiol. 33:268–276. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Morales SJ, Sampath K and Gardner TB: A
review of prevention of Post-ERCP pancreatitis. Gastroenterol
Hepatol (N Y). 14:286–292. 2018.PubMed/NCBI
|
|
6
|
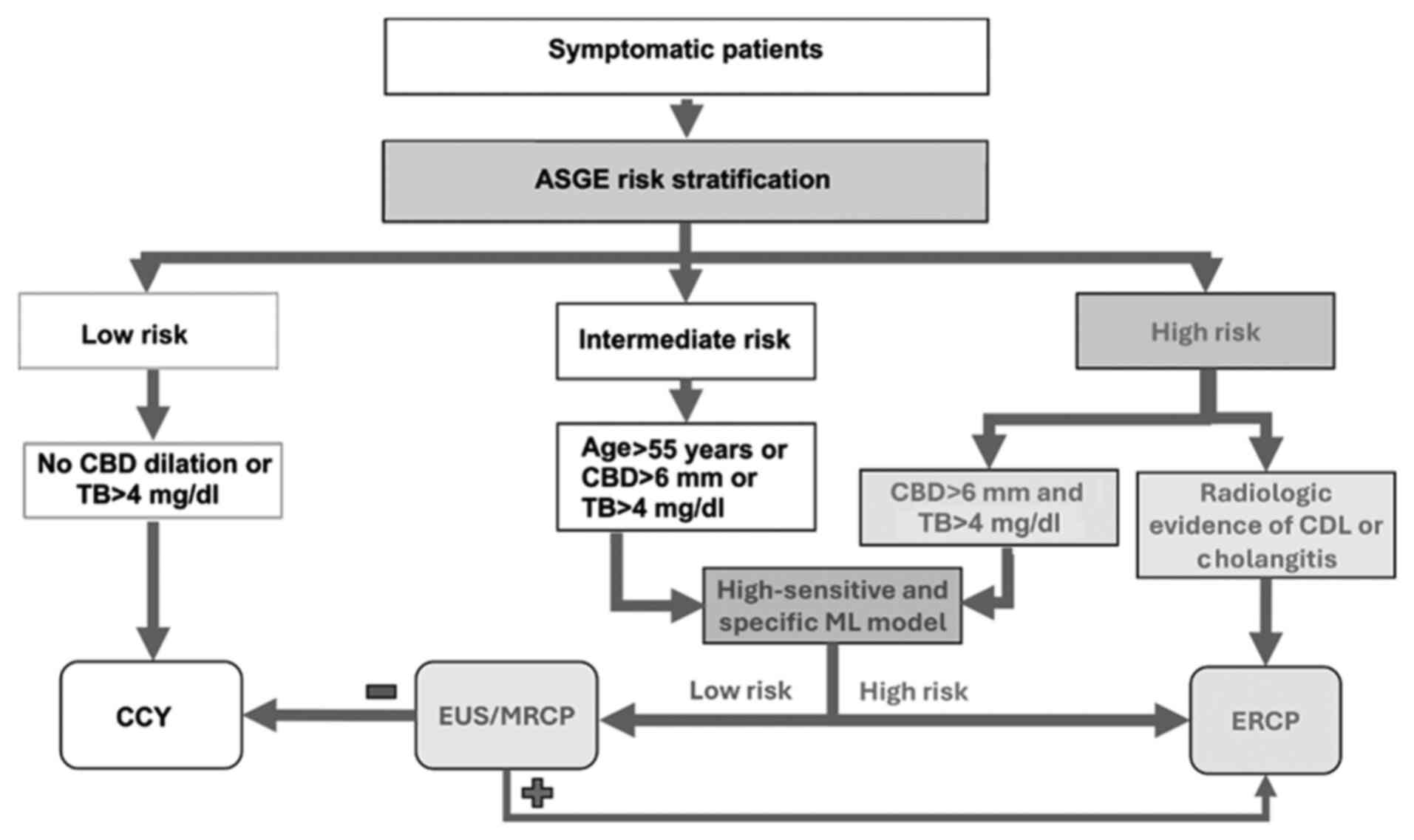
ASGE Standards of Practice Committee.
Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ,
Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, et al: ASGE
guideline on the role of endoscopy in the evaluation and management
of choledocholithiasis. Gastrointest Endosc. 89:1075–1105.e15.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
ASGE Standards of Practice Committee.
Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S,
Cash BD, Fisher L, Harrison ME, Fanelli RD, et al: The role of
endoscopy in the evaluation of suspected choledocholithiasis.
Gastrointest Endosc. 71:1–9. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tunruttanakul S, Chareonsil B, Verasmith
K, Patumanond J and Mingmalairak C: Evaluation of the American
society of gastrointestinal endoscopy 2019 and the european society
of gastrointestinal endoscopy guidelines' performances for
choledocholithiasis prediction in clinically suspected patients: A
retrospective cohort study. JGH Open. 6:434–440. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Rajpurkar P, Chen E, Banerjee O and Topol
EJ: AI in health and medicine. Nat Med. 28:31–38. 2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kröner PT, Engels MM, Glicksberg BS,
Johnson KW, Mzaik O, van Hooft JE, Wallace MB, El-Serag HB and
Krittanawong C: Artificial intelligence in gastroenterology: A
state-of-the-art review. World J Gastroenterol. 27:6794–824.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Byrne MF, Chapados N, Soudan F, Oertel C,
Linares Pérez M, Kelly R, Iqbal N, Chandelier F and Rex DK:
Real-time differentiation of adenomatous and hyperplastic
diminutive colorectal polyps during analysis of unaltered videos of
standard colonoscopy using a deep learning model. Gut. 68:94–100.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Korbar B, Olofson AM, Miraflor AP, Nicka
CM, Suriawinata MA, Torresani L, Suriawinata AA and Hassanpour S:
Deep learning for classification of colorectal polyps on
Whole-slide images. J Pathol Inform. 8(30)2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
An Q, Rahman S, Zhou J and Kang JJ: A
comprehensive review on machine learning in healthcare industry:
Classification, restrictions, opportunities and challenges. Sensors
(Basel). 23(4178)2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Trezza A, Visibelli A, Roncaglia B, Spiga
O and Santucci A: Unsupervised learning in precision medicine:
Unlocking personalized healthcare through AI. Appl Sci.
14(9305)2024.
|
|
15
|
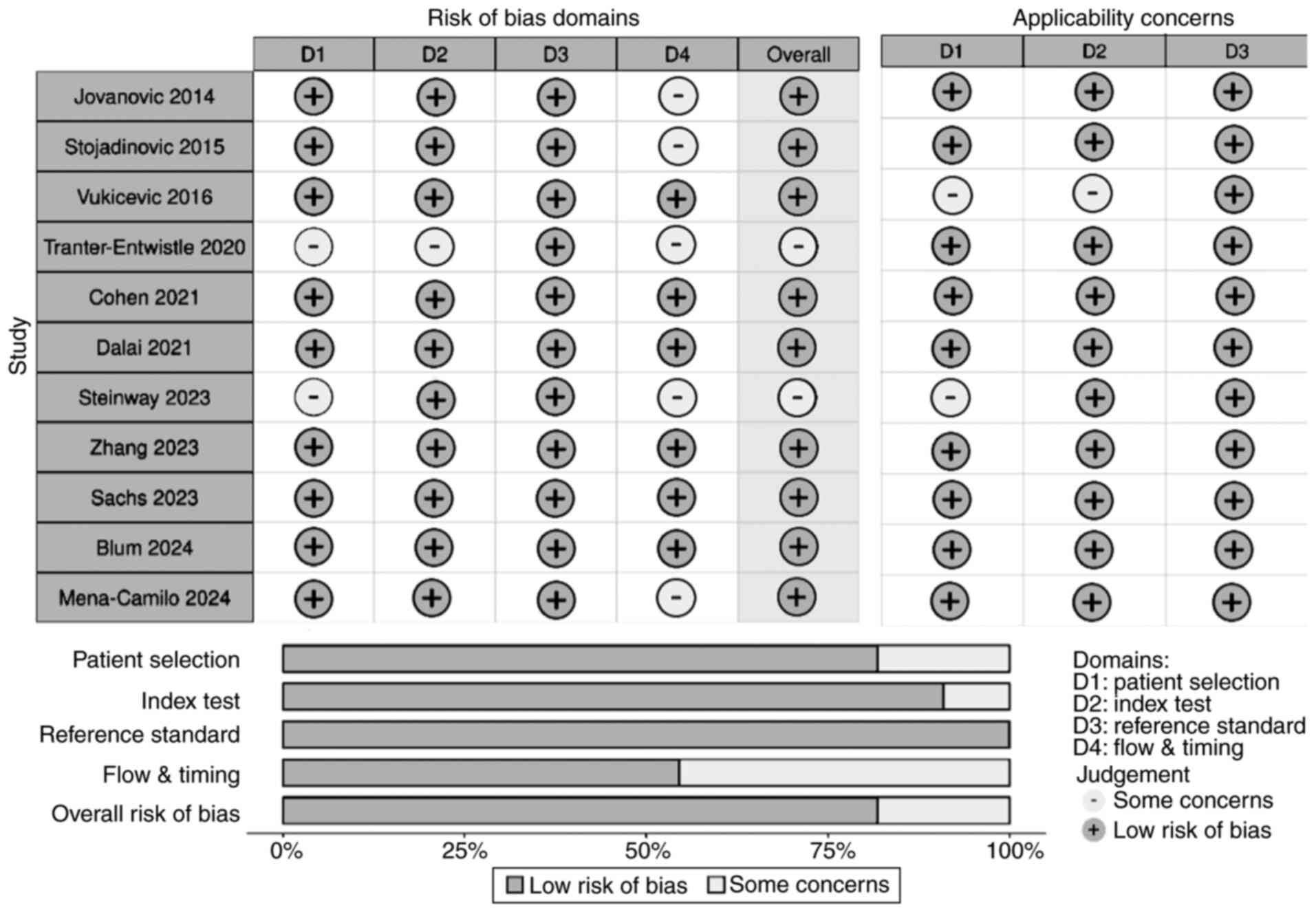
Blum J, Hunn S, Smith J, Chan FY and
Turner R: Using artificial intelligence to predict
choledocholithiasis: Can machine learning models abate the use of
MRCP in patients with biliary dysfunction? ANZ J Surg.
94:1260–1265. 2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cohen RZ, Tian H, Sauer CG, Willingham FF,
Santore MT, Mei Y and Freeman AJ: Creation of a pediatric
choledocholithiasis prediction model. J Pediatr Gastroenterol Nutr.
73:636–641. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Dalai C, Azizian J, Trieu H, Rajan A, Chen
F, Dong T, Beaven S and Tabibian JH: Machine learning models
compared to existing criteria for noninvasive prediction of
endoscopic retrograde cholangiopancreatography-confirmed
choledocholithiasis. Liver Res. 5:224–231. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Jovanovic P, Salkic NN and Zerem E:
Artificial neural network predicts the need for therapeutic ERCP in
patients with suspected choledocholithiasis. Gastrointest Endosc.
80:260–268. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mena-Camilo E, Salazar-Colores S,
Aceves-Fernández MA, Lozada-Hernández EE and Ramos-Arreguín JM:
Non-invasive prediction of choledocholithiasis using 1D
convolutional neural networks and clinical data. Diagnostics.
14(1278)2024.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Floan Sachs G, Ourshalimian S, Jensen AR,
Kelley-Quon LI, Padilla BE, Shew SB, Lofberg KM, Smith CA, Roach
JP, Pandya SR, et al: Machine learning to predict pediatric
choledocholithiasis: A western pediatric surgery research
consortium retrospective study. Surgery. 174:934–939.
2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Steinway SN, Tang B, Telezing J, Ashok A,
Kamal A, Yu CY, Jagtap N, Buxbaum JL, Elmunzer J, Wani SB, et al: A
machine learning-based choledocholithiasis prediction tool to
improve ERCP decision making: A proof-of-concept study. Endoscopy.
56:165–171. 2024.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Stojadinovic MM and Pejovic T: Regression
tree for choledocholithiasis prediction. Eur J Gastroenterol
Hepatol. 27:607–613. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tranter-Entwistle I, Wang H, Daly K,
Maxwell S and Connor S: The challenges of implementing artificial
intelligence into surgical practice. World J Surg. 45:420–428.
2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Vukicevic AM, Stojadinovic M, Radovic M,
Djordjevic M, Cirkovic BA, Pejovic T, Jovicic G and Filipovic N:
Automated development of artificial neural networks for clinical
purposes: Application for predicting the outcome of
choledocholithiasis surgery. Comput Biol Med. 75:80–89.
2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhang H, Gao J, Sun Z, Zhang Q, Qi B,
Jiang X, Li S and Shang D: Diagnostic accuracy of updated risk
assessment criteria and development of novel computational
prediction models for patients with suspected choledocholithiasis.
Surg Endosc. 37:7348–7357. 2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhou Y and Dendukuri N: Statistics for
quantifying heterogeneity in univariate and bivariate meta-analyses
of binary data: The case of Meta-analyses of diagnostic accuracy.
Stat Med. 33:2701–2717. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Huerta-Reyna R, Guevara-Torres L,
Martínez-Jiménez MA, Armas-Zarate F, Aguilar-García J,
Waldo-Hernández LI and Martínez-Martínez MU: Development and
validation of a predictive model for choledocholithiasis. World J
Surg. 48:1730–1738. 2024.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shi Y, Lin J, Zhu J, Gao J, Liu L, Yin M,
Yu C, Liu X, Wang Y and Xu C: Predicting the recurrence of common
bile duct stones after ERCP treatment with automated machine
learning algorithms. Dig Dis Sci. 68:2866–2877. 2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Huang L, Lu X, Huang X, Zou X, Wu L, Zhou
Z, Wu D, Tang D, Chen D, Wan X, et al: Intelligent difficulty
scoring and assistance system for endoscopic extraction of common
bile duct stones based on deep learning: Multicenter study.
Endoscopy. 53:491–498. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wang Z, Yuan H, Lin K, Zhang Y, Xue Y, Liu
P, Chen Z and Wu M: Artificial intelligence-empowered assessment of
bile duct stone removal challenges. Expert Systems Applications.
258(125146)2024.
|
|
31
|
Li D, Du B, Shen Y and Ge L: Artificial
Intelligence-assisted visual sensing technology under duodenoscopy
of gallbladder stones. J Sensors. 2021(5158577)2021.
|
|
32
|
Akabane S, Iwagami M, Bell-Allen N,
Navadgi S, Kawahara T and Bhandari M: Machine learning-based
prediction for incidence of endoscopic retrograde
cholangiopancreatography after emergency laparoscopic
cholecystectomy: A retrospective, multicenter cohort study. Surg
Endosc. 39:1770–1777. 2025.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Hou JU, Park SW, Park SM, Park DH, Park CH
and Min S: Efficacy of an artificial neural network algorithm based
on Thick-slab magnetic resonance cholangiopancreatography images
for the automated diagnosis of common bile duct stones. J
Gastroenterol Hepatol. 36:3532–3540. 2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sun K, Li M, Shi Y, He H, Li Y, Sun L,
Wang H, Jin C, Chen M and Li L: Convolutional neural network for
identifying common bile duct stones based on magnetic resonance
cholangiopancreatography. Clin Radiol. 79:553–558. 2024.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Singhvi G, Ampara R, Baum J and Gumaste V:
ASGE guidelines result in Cost-saving in the management of
choledocholithiasis. Ann Gastroenterol. 29:85–90. 2016.PubMed/NCBI
|
|
36
|
Kang J, Paik KH, Lee JC, Kim HW, Lee J,
Hwang JH and Kim J: The efficacy of clinical predictors for
patients with intermediate risk of choledocholithiasis. Digestion.
94:100–105. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
He H, Tan C, Wu J, Dai N, Hu W, Zhang Y,
Laine L, Scheiman J and Kim JJ: Accuracy of ASGE high-risk criteria
in evaluation of patients with suspected common bile duct stones.
Gastrointest Endosc. 86:525–532. 2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Jacob JS, Lee ME, Chew EY, Thrift AP and
Sealock RJ: Evaluating the revised american society for
gastrointestinal endoscopy guidelines for common bile duct stone
diagnosis. Clin Endosc. 54:269–274. 2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Lee H, Song T, Park DH, Lee SS, Seo DW,
Lee SK, Kim MH, Jun JH, Moon JE and Song YH: Diagnostic performance
of the current Risk-stratified approach with computed tomography
for suspected choledocholithiasis and its options when negative
finding. Hepatobiliary Pancreat Dis Int. 18:366–372.
2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Anand G, Yeh HC, Khashab M, Kim KJ, Lennon
AM, Shin EJ, Canto M, Okolo PI, Kalloo AN and Singh VK: Mo1582
Patterns of MRCP Utilization prior to ERCP among patients at high
risk for choledocholithiasis. Gastrointestinal Endoscopy.
73:AB393–AB394. 2011.
|
|
41
|
Tuna Kirsaclioglu C, Çuhacı Çakır B,
Bayram G, Akbıyık F, Işık P and Tunç B: Risk factors, complications
and outcome of cholelithiasis in children: A retrospective,
single-centre review. J Paediatr Child Health. 52:944–949.
2016.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Frybova B, Drabek J, Lochmannova J, Douda
L, Hlava S, Zemkova D, Mixa V, Kyncl M, Zeman L, Rygl M and Keil R:
Cholelithiasis and choledocholithiasis in children; risk factors
for development. PLoS One. 13(e0196475)2018.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Murphy PB, Vogt KN, Winick-Ng J, McClure
JA, Welk B and Jones SA: The increasing incidence of gallbladder
disease in children: A 20year perspective. J Pediatr Surg.
51:748–752. 2016.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Lascia AD, Tartaglia N, Pavone G, Pacilli
M, Ambrosi A, Buccino RV, Petruzzelli F, Menga MR, Fersini A and
Maddalena F: One-step versus two-step procedure for management
procedures for management of concurrent gallbladder and common bile
duct stones. Outcomes and cost analysis. Ann Ital Chir. 92:260–207.
2021.PubMed/NCBI
|
|
45
|
Jones M, Johnson M, Samourjian E, Slauch K
and Ozobia N: ERCP and laparoscopic cholecystectomy in a combined
(one-step) procedure: A random comparison to the standard
(two-step) procedure. Surg Endosc. 27:1907–1912. 2013.PubMed/NCBI View Article : Google Scholar
|
|
46
|
de Medeiros KS, Aragão Fernandes AC, Fulco
Gonçalves G, Villarim CVO, Costa E Silva LC, de Sousa VMC, Meneses
Rêgo AC and Araújo-Filho I: Cholecystectomy before, simultaneously,
or after ERCP in patients with acute cholecystitis: A protocol for
systematic review and/or meta analysis. Medicine (Baltimore).
101(e30772)2022.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Ebigbo A, Messmann H and Lee SH:
Artificial intelligence applications in Image-based diagnosis of
early esophageal and gastric neoplasms. Gastroenterology.
169:396–415.e2. 2025.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Sharma P and Hassan C: Artificial
intelligence and deep learning for upper gastrointestinal
neoplasia. Gastroenterology. 162:1056–1066. 2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Alhejaily AG: Artificial intelligence in
healthcare (review). Biomed Rep. 22(11)2024.PubMed/NCBI View Article : Google Scholar
|