Introduction
Distal radius fractures (DRFs) are one of the most
common fractures, accounting for ~18% of fractures in older adult
patients (1). Surgical treatments
for DRFs often achieve good reduction, but the incidence of
reduction loss due to osteoporosis and comminution is as high as
30%, especially for radial height loss (RHL) (2). Currently, there is no consensus
regarding the prevention of RHL.
Previous studies have confirmed that the normal
distal radius of the wrist can withstand an axial load of up to 80%
(3). RHL often occurs due to
insufficient radial support against the axial load, especially in
non-surgical treatments. RHL may also be observed in patients
undergoing open reduction and internal fixation with a volar
locking plate for intra- and extra-articular DRF. Figl et al
(4) found the incidence of RHL was
25% with a mean radial shortening of 1.8 mm (range, 1-3 mm) 1 year
after surgery. As a result, the mean extension-flexion movement and
grip strength were reduced by 21 and 35%, respectively. As for risk
factors for RHL, LaMartina et al (5) suggested that these include advanced
age, poor bone quality, short distance between fracture site and
articular surface, and postoperative ulnar-positive deformity. An
external fixator combined with open reduction and volar plating can
effectively prevent the RHL in older patients with comminuted DRF
compared with volar plating alone, as reported by Han et al
(6). Furthermore, Ruch et
al (7) reported effective
maintenance of RHL using a cross-wrist supporting plate; however,
the disadvantages include creating a dorsal incision and breaking
the blood supply to the fractured end. Therefore, this technique is
used less than the conventional external fixation (8). As an alternative method to treat RHL,
Kulshrestha et al (9)
suggested the bridging external fixation (BEF) for 6 to 8 weeks;
this technique uses a bridging external fixator that spans the
wrist. However, this technique is insufficient in older patients
with comminuted DRF. Non-BEFs often yield instability as only one
or two screws capture the fragments. To reinforce the stability of
distal fragments, combined external fixation (CEF), combining both
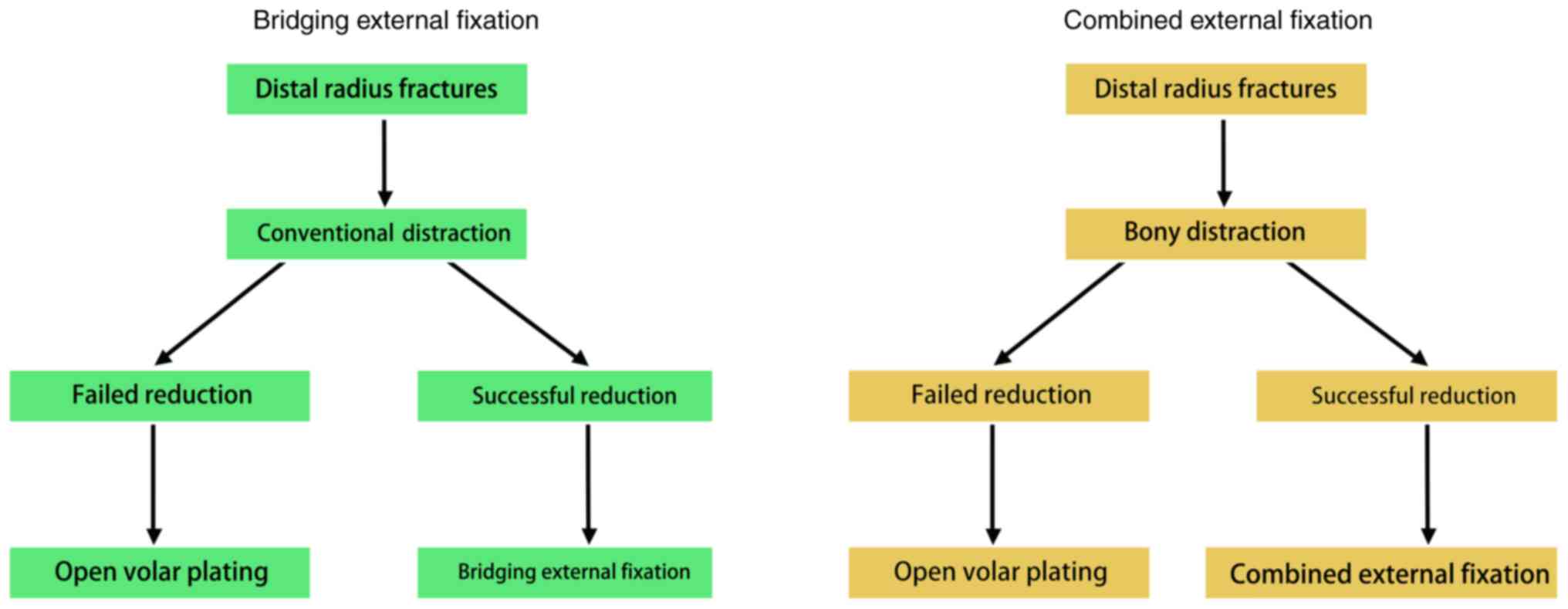
BEF and non-BEF, was used in the present study (Fig. 1).
The present prospective study aimed to compare the
efficacies of BEF and CEF in preventing RHL in older patients with
DRF.
Patients and methods
Patient selection
The research protocol was approved by the
Investigational Review Board of Jingxing County Hospital
(Shijiazhuang, China; approval no. 2017005), and written informed
consent was obtained from all participants prior to the study. The
patients involved in this study consented to the publication of
their images.
Between January 2018 and December 2022, 147
consecutive older patients (≥55 years) (10) with DRF were prospectively enrolled
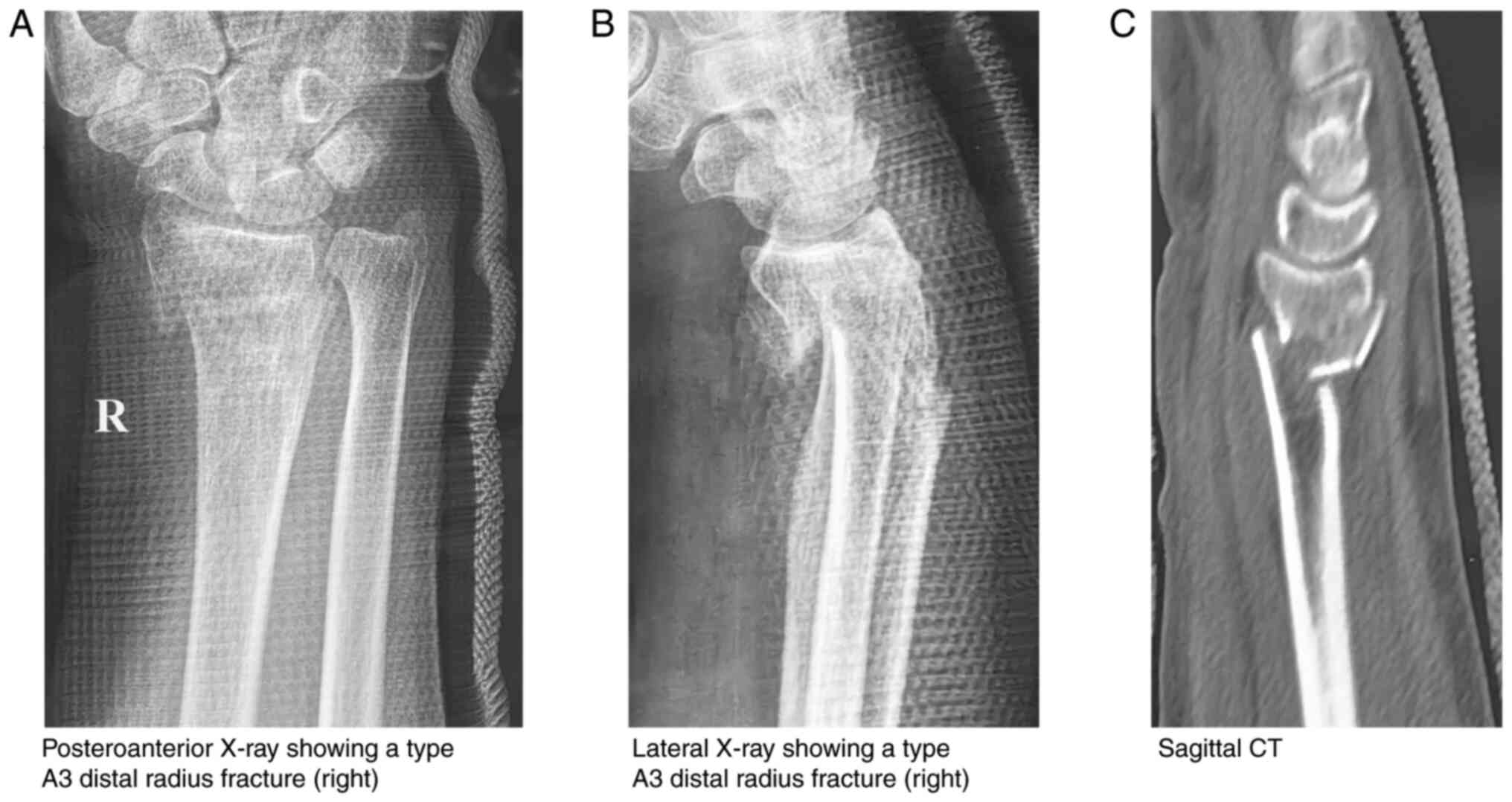
in the present study. Preoperatively, standard posteroanterior and
lateral wrist radiographs were obtained from all patients. Computed
tomography (CT) scans and three-dimensional reconstructions were
performed, as required (Fig. 2).
Magnetic resonance imaging was performed when a ligament tear was
suspected. Fracture diagnoses and types were determined by three
senior orthopaedic surgeons who were not involved in the
treatments.
The eligibility criteria for the study were as
follows: i) Patients aged between 55 and 70 years; ii) closed
distal radius fractures; iii) acute fractures within 14 days of
injury; iv) confirmed diagnoses of A2, A3, B1, B3, C1, C2 and C3
fractures based on the AO Foundation and Orthopaedic Trauma
Association (AO/OTA) Classification (11); and v) a normal opposite upper limb
for comparison. Patients meeting any of the following conditions
were excluded: i) Patients aged <55 years, as osteoporosis
rarely occurs (n=9); ii) patients aged >70 years, as malunion is
often tolerable (n=6); iii) open fractures (n=7); iv) type A1
fractures, as these do not involve the radius; v) type B2
fractures, as fixation with pins is difficult; vi) combined
ligament injuries (n=2); vii) fractures >14 days old, as
percutaneous reduction becomes difficult (n=3); viii) patients who
refused to undergo external fixation (n=1); and ix) patients who
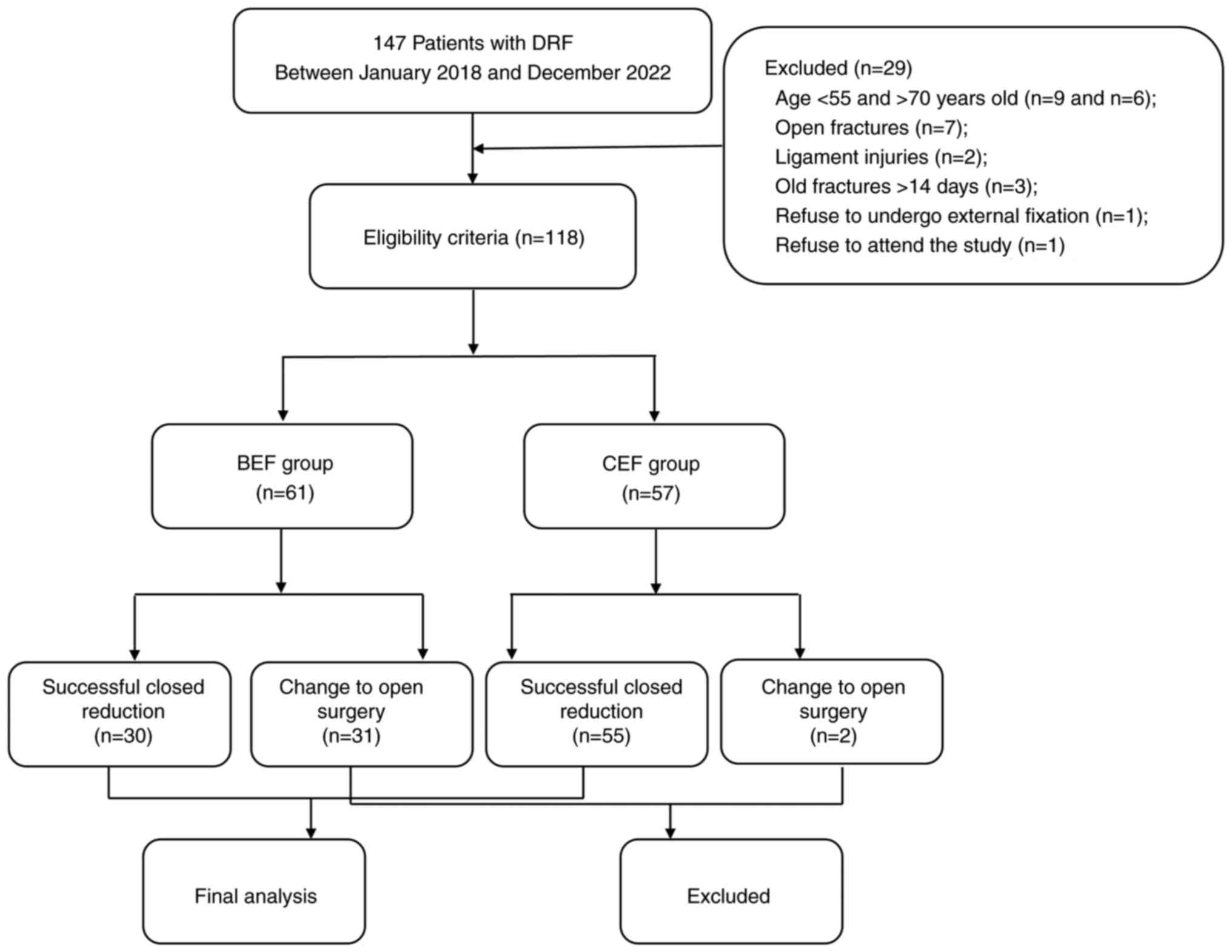
declined to participate in the study (n=1) (Fig. 3).
Patients were randomly and blindly allocated to the
BEF (n=61) and CEF (n=57) groups using a computational pseudorandom
number generator. Patients in the BEF group underwent BEF, whereas
those in the CEF group were subjected to CEF. All operations were
performed by the same senior surgeon.
Conventional distraction and BEF
Conventional distraction and BEF surgery were
performed under brachial plexus anesthesia without tourniquet
control. Fracture reduction was achieved using a distraction
manoeuvre, as described by Capo et al (12). Insertion of two 3.5-mm Schanz pins
(Hengshui Zengli Medical Instrument Co., Ltd.), into the second
metacarpal and proximal radius was performed, and a bridging
external fixator (Hengshui Zhengli Medical Instrument Company Ltd.)
was installed to maintain reduction. Several 2.5-mm Steinmann pins
(Hengshui Zengli Medical Instrument Co., Ltd.), were inserted to
secure small fragments, as needed. The reduction quality was
assessed using intraoperative X-rays.
Bony distraction and CEF
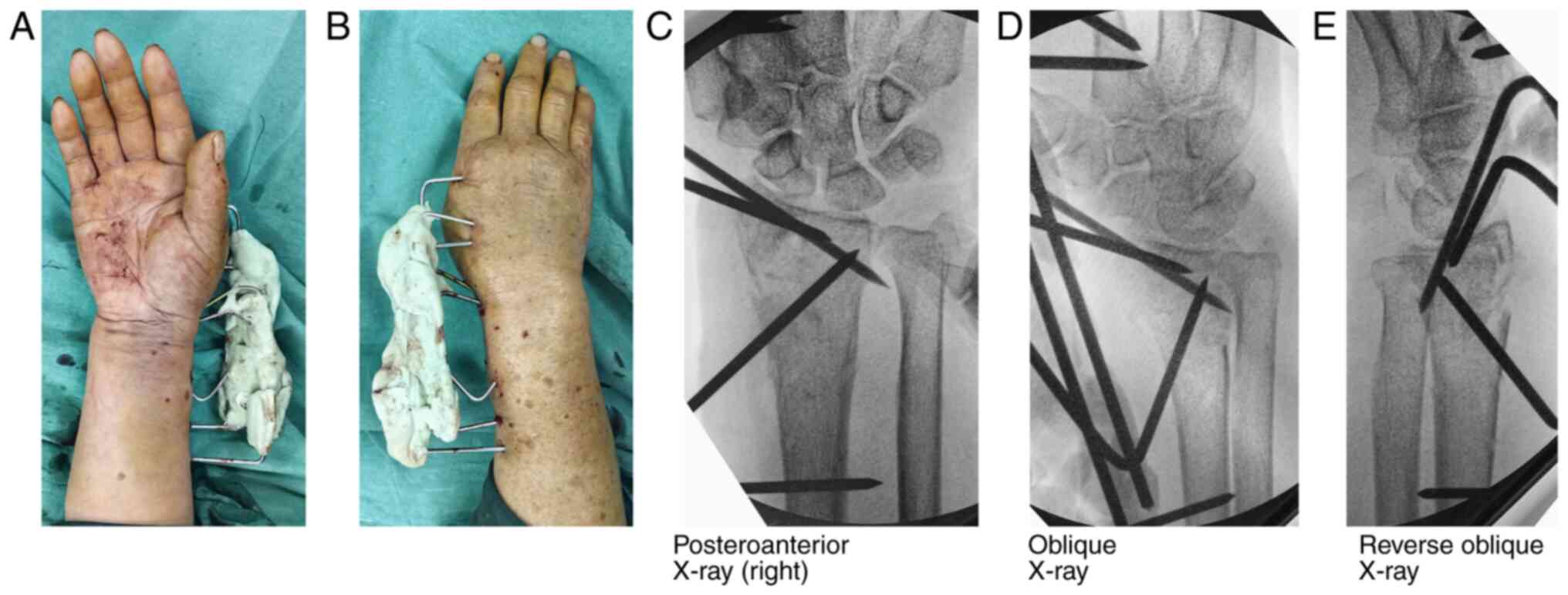
Bony distraction and CEF surgery were also performed
under brachial plexus anesthesia without tourniquet control. The
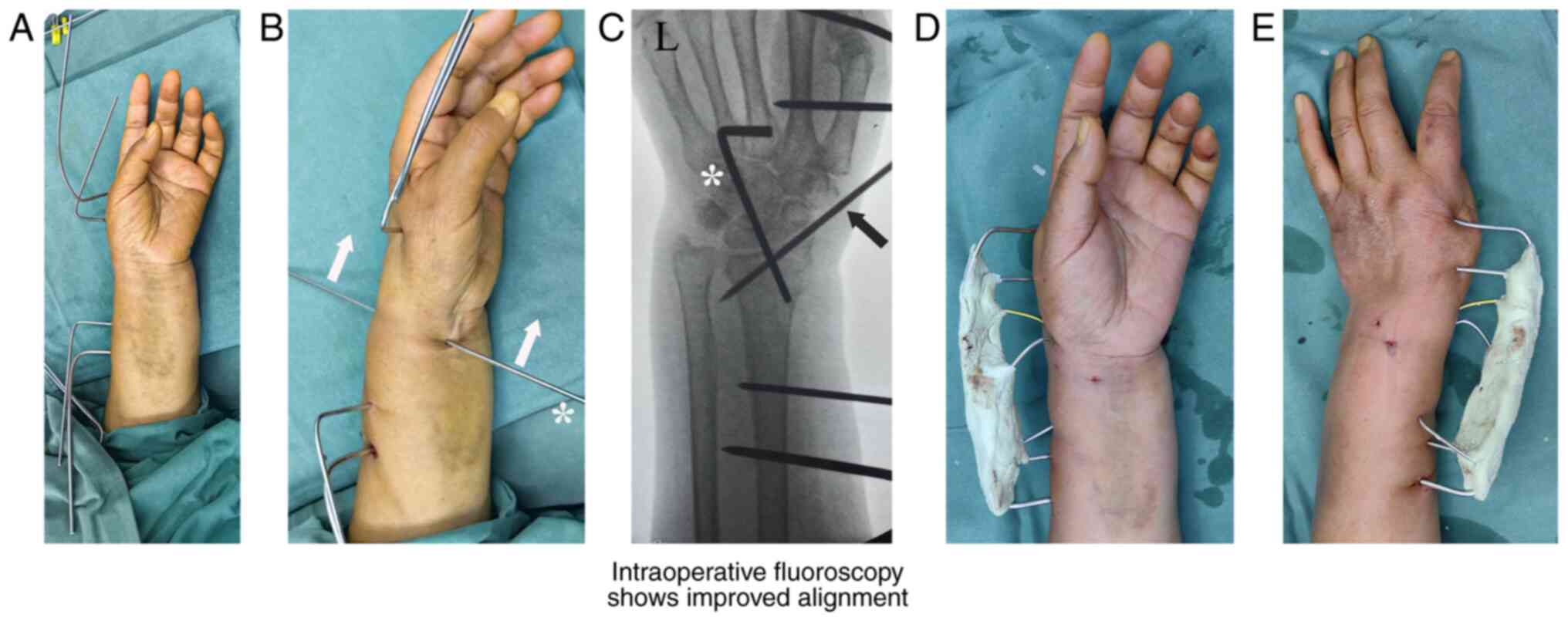
surgery involved the insertion of two to three 2.5-mm transverse
Steinmann pins into the second metacarpal and two to three pins
into the proximal radius, respectively (Fig. 4A). A 2.5-mm Steinmann pin was
manually placed across the fracture line from the anterior to the
posterior wrist. The insertion point was located 0.5 cm distal to
the fracture line that was identified on X-rays and 0.5 cm medial
to the radial artery that could be palpated easily. The attending
surgeon pulled both ends of the reduction pin distally to reduce
the fracture (Fig. 4B). The normal
volar tilt of the radius was restored by pulling the dorsal pin end
more distally and the volar pin end more proximally. The reduction
was maintained using several oblique pins inserted from the radial
styloid and proximal radius. Satisfactory reduction was confirmed
by fluoroscopy (Fig. 4C). All
K-wires were bent toward the fracture site, ~2 cm away from the
skin. The monomers (liquid) and polymers (powder) of the bone
cement (Palacos Bone Cements; Heraeus Medical GmbH) were mixed,
which changed the bone cement viscosity from a runny liquid to a
dough-like state. Subsequently, the mixture was applied to all bent
pin ends to allow it to harden into a solid material (Fig. 4D and E). Satisfactory reduction was confirmed
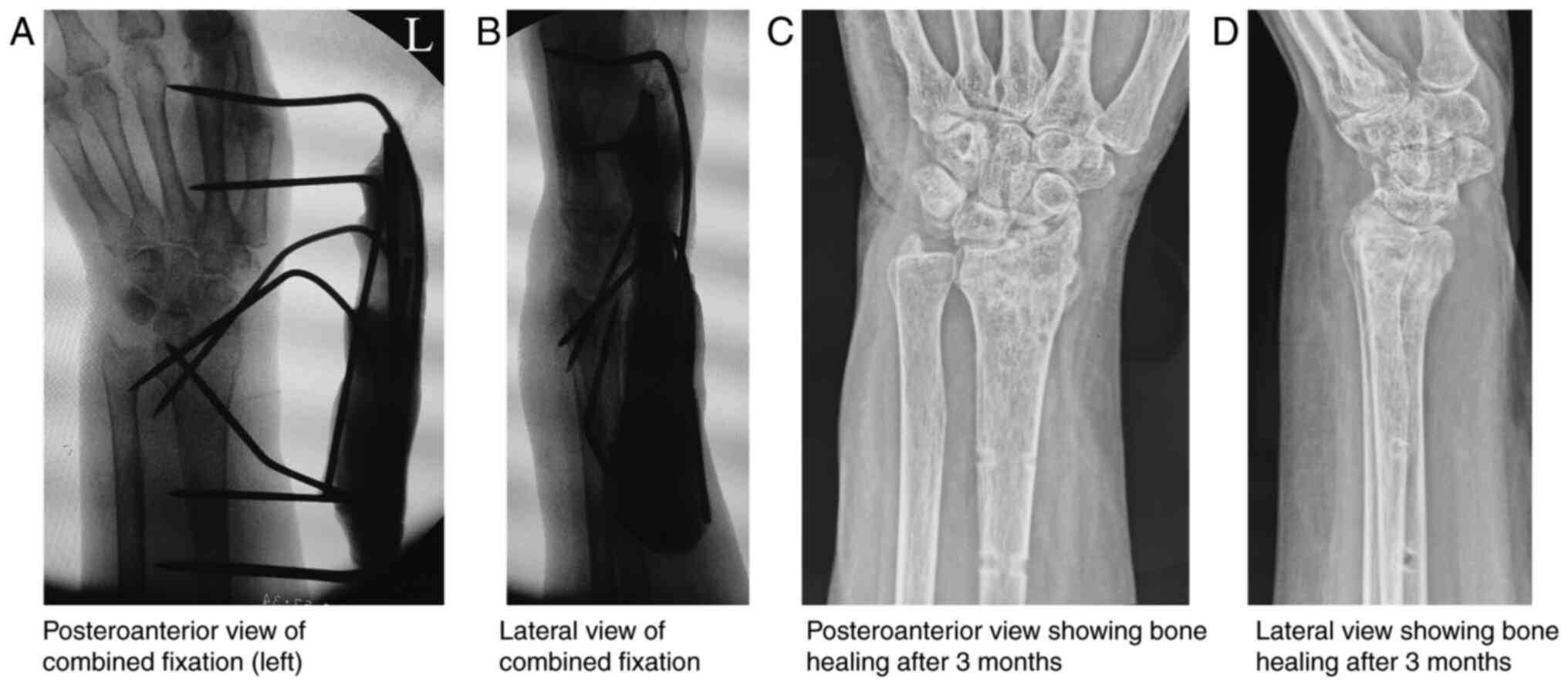
using intraoperative radiography (Fig.
5A and B).
Converting to open surgery
The patients with failed reduction (radial
inclination <15˚, radial shortening <5 mm, dorsal tilt
>15˚ and articular step-off >2 mm), irrespective of group,
were converted to open volar plating as described by Alter et
al (13).
Postoperative management
The injured wrist was protected using a dorsal
splint, which allowed for a range of motion (ROM) of the fingers
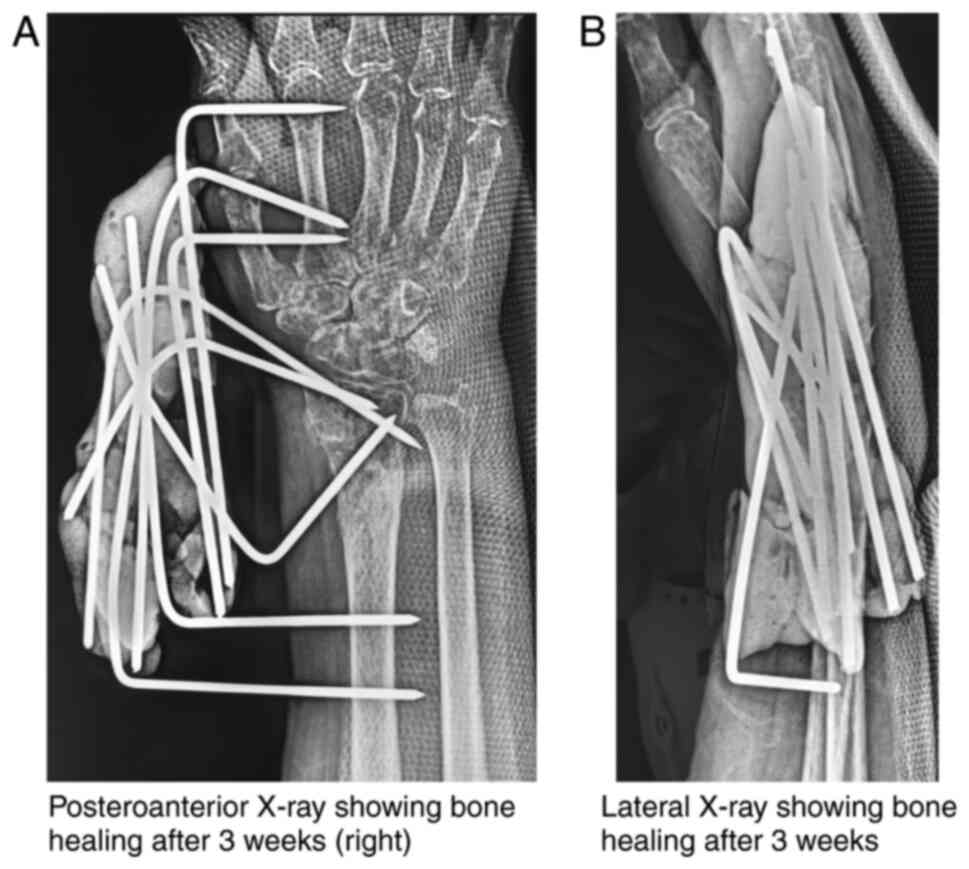
and thumb. The splint was removed after 4 weeks. Radiographs were
taken every 2 weeks until bone healing had occurred, and the
external fixators were removed (Fig.
5C and D). ROM exercises of
the wrist were performed thereafter.
Outcome evaluation
Radial height, palmar tilt, radial inclination,
ulnar variance and articular step-off were measured using standard
radiography. Fracture consolidation and Lidström classification
(14) was determined using
radiography. The wrist ROM was measured using a goniometer
(Fig. 6). Grip strength was
measured with a hand dynamometer (Jamar®; J.A. Preston
Corporation). Pronation torque of the wrist was assessed using the
McConkey method (15) at five
rotation positions (90˚ supination, 45˚ supination, neutral, 45˚
pronation and 80˚ pronation). All measurements were compared with
those on the opposite side. To eliminate the discrepancy between
dominant and non-dominant hand strength, the scores for analysis
were based on the premise that grip strength was 15% higher on the
dominant side than that on the non-dominant side, and no correction
was required for left-handed individuals, according to a previous
study (16). At the final
follow-up, the patients were asked to complete the following
questionnaires: The level of pain during specified activities based
on a numeric rating scale (NRS), a modified Mayo Wrist Score, a
Disabilities of the Arm Shoulder and Hand score, a Patient-Rated
Wrist Evaluation score and a patient satisfaction score
questionnaire (17-21).
To evaluate efficiency of the two external fixation techniques,
those patients undergoing open surgery were excluded.
Statistical analysis
All statistical analyses were performed using SPSS
version 21.0 (IBM Corp.). Continuous variables are expressed as the
mean ± SD. Pearson's χ2 test and Fisher's exact test
were used for qualitative data. An unpaired t-test was used for the
between-group analyses, while a paired t-test was used for the
within-group analyses. Pearson's χ2 test and Fisher's
exact test were used to compare the Lidström classification. An
unpaired t-test was used to compare the radiological parameters and
clinical outcomes between the BEF group and the CEF group.
P<0.05 was considered to indicate a statistically significant
difference.
Results
In the present study, 147 patients were reviewed,
with 118 patients (49 men and 69 women) eligible for the final
analysis (Table I). The BEF group
comprised 61 patients, with a mean age of 61.97±3.61 years (range,
56-68 years). According to the AO/OTA classification, the fracture
types in the BEF group were as follows: 3 cases of A2, 8 of A3, 7
of B1, 12 of B3, 17 of C1, 11 of C2 and 3 of C3. The mean follow-up
period was 29.70±3.47 months (range 24-36 months). The CEF group
included 57 patients, with a mean age of 61.51±4.00 years (range,
55-70 years). According to the AO/OTA classification, the CEF group
included 4 A2, 6 A3, 10 B1, 8 B3, 12 C1, 13 C2, and 4 C3 fractures.
The mean follow-up period was 28.53±2.76 months (range, 24-33
months). A successful closed reduction was achieved in 30 patients
(49.2%) in the BEF group and 55 patients (96.5%) in the CEF group.
Pin-site infection occurred in 1 patient (3.3%) in the BEF group
and 1 patient (1.8%) in the CEF group. Statistically significant
differences were observed in operative time (t=12.52; P<0.01),
successful closed reduction (χ2=32.74; P<0.01),
change to open surgery (χ2=32.74; P<0.01) and
treatment cost (t=4585.26; P<0.01). However, no statistically
significant differences were found in AO/OTA classification
(χ2=2.81; P=0.83), time between injury and operation
(t=1.17; =0.25), infection (χ2=0.19; P=0.67), bone
healing time (t=0.69; P=0.49) and follow-up duration (t=1.17;
P=0.09).
 | Table IPatient characteristics of the two
groups. |
Table I
Patient characteristics of the two
groups.
| Characteristics | BEF group (n=61) | CEF group (n=57) | Statistical
value | P-value |
|---|
| Mean age ± SD
(range), yearsa | 61.97±3.61
(56-68) | 61.51±4.00
(55-70) | 0.66 | 0.51 |
| Sex (m:f),
nb | 26:35 | 23:34 | 0.06 | 0.80 |
| Injured side (l:r),
nb | 22:39 | 19:38 | 0.10 | 0.76 |
| Dominance,
nb | 34 | 31 | 0.02 | 0.88 |
| Cause,
nc | | | 0.33 | 0.98 |
|
Fall | 27 | 25 | | |
|
Road traffic
accident | 19 | 17 | | |
|
Sports | 12 | 11 | | |
|
Others | 3 | 4 | | |
| AO/OTA,
nc | | | 2.92 | 0.84 |
|
A2 | 3 | 4 | | |
|
A3 | 8 | 6 | | |
|
B1 | 7 | 10 | | |
|
B3 | 12 | 8 | | |
|
C1 | 17 | 12 | | |
|
C2 | 11 | 13 | | |
|
C3 | 3 | 4 | | |
| Ulnar styloid
fracture, nb | 24 | 21 | 0.08 | 0.78 |
| Mean hospital stay
± SD (range), daysa | 6.69±1.78
(4-10) | 6.44±1.54
(3-9) | 0.82 | 0.42 |
| TBIO (range),
daysa | 4.75±1.29
(3-7) | 4.51±0.97
(3-6) | 1.17 | 0.25 |
| Mean operative time
± SD, mina | 52.61±7.03
(42-65) | 38.54±4.91
(30-47) | 12.52 | <0.01 |
| Successful closed
reduction, n (%)b | 30 (49.2) | 55 (96.5) | 32.74 | <0.01 |
| Change to open
surgery, n (%)b | 31 (50.8) | 2 (3.5) | 32.74 | <0.01 |
| Infection, n
(n/total n, %)c | 1
(3.3)d | 1
(1.8)e | - | 1.00 |
| Mean cost ± SD
(RMB)a | 8,023.35±5.53 | 563.73±7.91 | 4,585.26 | <0.01 |
| Mean bone healing
time ± SD (range), weeksa | 7.20±1.13
(6-9) | 7.05±0.80
(6-8) | 0.69 | 0.49 |
| Mean follow-up time
± SD (range), monthsa | 29.70±3.47
(24-36) | 28.53±2.76
(24-33) | 1.71 | 0.09 |
The radiological parameters of intraoperative closed
reduction, bone healing and final follow-up were compared between
the BEF group and the CEF group (Table II). The BEF group showed no
significant differences regarding radial height (t=0.16; P=0.88),
palmar tilt (t=0.40; P=0.69), radial inclination (t=0.46; P=0.65),
ulnar variance (t=0.02; P=0.98) and articular step-off (t=0.93;
P=0.36) between bone healing and the final follow-up. Similarly,
the CEF group also showed no significant differences in radial
height (t=0.69; P=0.49), palmar tilt (t=0.06; P=0.95), radial
inclination (t=0.14; P=0.89), ulnar variance (t=0.39; P=0.70) and
articular step-off (t=0.86; P=0.39) between bone healing and the
final follow-up. Bone healing showed no significant differences in
radial height (t=1.19; P=0.24), palmar tilt (t=0.41, P=0.69),
radial inclination (t=0.37; P=0.71), ulnar variance (t=0.30;
P=0.77) and articular step-off (t=0.92; P=0.36) between the BEF
group and CEF groups. Similarly, the final follow-up also showed no
significant differences in radial height (t=0.78; P=0.44), palmar
tilt (t=0.76; P=0.45), radial inclination (t=0.84; P=0.40), ulnar
variance (t=0.60; P=0.55) and articular step-off (t=0.60; P=0.55)
between the two groups. However, there were significant differences
in radial height (t=10.06; P<0.01), palmar tilt (t=8.77;
P<0.01), radial inclination (t=9.05; P<0.01), ulnar variance
(t=4.19; P<0.01), articular step-off (t=5.05; P<0.01) and
articular step-off ≥2 mm (t=23.45; P<0.01) during intraoperative
closed reduction between the two groups (Table II).
 | Table IIRadiological parameters measured at
the time of intraoperative closed reduction, bone healing and final
follow-up. |
Table II
Radiological parameters measured at
the time of intraoperative closed reduction, bone healing and final
follow-up.
| Parameter | BEF group
(n=61a;
n=30b) | CEF group
(n=57a;
n=55b) | t value | P-value |
|---|
| Radial height,
mm | | | | |
|
Intraoperative
closed reduction | 10.06±1.07 | 12.13±1.16 | 10.06 | <0.01 |
|
Bone
healing | 11.78±1.15 | 12.09±1.15 | 1.19 | 0.24 |
|
Final
follow-up | 11.73±1.14 | 11.94±1.18 | 0.78 | 0.44 |
|
t
valuec | 0.16 | 0.69 | | |
|
P-valuec | 0.88 | 0.49 | | |
| Palmar tilt, ˚ | | | | |
|
Intraoperative
closed reduction | 10.08±1.26 | 12.09±1.22 | 8.77 | <0.01 |
|
Bone
healing | 11.94±1.10 | 12.04±1.17 | 0.41 | 0.69 |
|
Final
follow-up | 11.82±1.09 | 12.03±1.24 | 0.76 | 0.45 |
|
t
valuec | 0.40 | 0.06 | | |
|
P-valuec | 0.69 | 0.95 | | |
| Radial inclination,
˚ | | | | |
|
Intraoperative
closed reduction | 20.14±1.65 | 22.84±1.59 | 9.05 | <0.01 |
|
Bone
healing | 22.69±1.89 | 22.84±1.58 | 0.37 | 0.71 |
|
Final
follow-up | 22.49±1.51 | 22.79±1.63 | 0.84 | 0.40 |
|
t
valuec | 0.46 | 0.14 | | |
|
P-valuec | 0.65 | 0.89 | | |
| Ulnar variance,
mm | | | | |
|
Intraoperative
closed reduction | 1.78±1.10 | 1.08±0.61 | 4.19 | <0.01 |
|
Bone
healing | 1.05±0.58 | 1.01±0.59 | 0.30 | 0.77 |
|
Final
follow-up | 1.04±0.56 | 0.96±0.60 | 0.60 | 0.55 |
|
t
valuec | 0.02 | 0.39 | | |
|
P-valuec | 0.98 | 0.70 | | |
| Articular stepoff,
mm | | | | |
|
Intraoperative
closed reduction | 1.58±0.91 | 0.87±0.57 | 5.05 | <0.01 |
|
Bone
healing | 0.85±0.39 | 0.76±0.46 | 0.92 | 0.36 |
|
Final
follow-up | 0.74±0.47 | 0.68±0.45 | 0.60 | 0.55 |
|
t
valuec | 0.93 | 0.86 | | |
|
P-valuec | 0.36 | 0.39 | | |
| Articular stepoff
≥2 mm, n | | | | - |
|
Intraoperative
closed reduction | 25 | 2 | 23.45 | <0.01 |
|
Bone
healing | 0 | 0 | | |
|
Final
follow-up | 0 | 0 | | |
Based on the Lidström classification, the BEF group
included 19 excellent and 11 good results at the time of bone
healing, and 27 excellent and 3 good results at the final
follow-up; the CEF group included 45 excellent and 10 good results
at the time of bone healing, and 54 excellent and 1 good result at
the final follow-up. Significant differences were observed between
bone healing and the final follow-up in the BEF group
(χ2=5.96; P<0.05) and in the CEF group
(χ2=8.18; P<0.01). However, there were no significant
differences between the BEF and CEF groups regarding bone healing
(χ2=3.57, P=0.06) or the final follow-up (P=0.12)
(Table III). The mean cost of
CEF was Renminbi (RMB) 563.73±7.91 (7 to 12 pins, each costing RMB
5.04; bone cement, RMB 517), while the mean cost of BEF was RMB
8,023.35±5.53 (3 to 6 pins, each costing RMB 5.04; external
fixator, RMB 8000) (t=4,585.26; P<0.01). The cost of CEF was ~7%
of that of BEF (Table I).
 | Table IIILidström classification at the time
of bone healing and the final follow-up. |
Table III
Lidström classification at the time
of bone healing and the final follow-up.
| | BEF group
(n=30) | CEF group
(n=55) | BEF vs. CEF for
bone healinga | BEF vs. CEF for
final follow-upb |
|---|
| Classification
(score) | Bone healing | Final
follow-up | Bone healing | Final
follow-up | Statistical
value | P-value | Statistical
value | P-value |
|---|
| Excellent
(90-100) | 19 | 27 | 45 | 54 | 3.57 | 0.06 | - | 0.12 |
| Good (80-90) | 11 | 3 | 10 | 1 | | | | |
| Fair (60-80) | 0 | 0 | 0 | 0 | | | | |
| Poor (<60) | 0 | 0 | 0 | 0 | | | | |
| Statistical
valuea | 5.96 | 8.18 | | | | |
| P-value | 0.015 | 0.004 | | | | |
At the final follow-up, there were no significant
differences between the two groups in terms of active ROM (flexion:
t=0.80, P=0.43; extension: t=1.48, P=0.14; radial deviation:
t=0.96, P=0.34; ulnar deviation: t=1.07, P=0.29; pronation: t=1.17,
P=0.25; and supination: t=0.82, P=0.41), grip strength (t=0.98,
P=0.33), supination torque (90˚ of supination: t=1.48, P=0.14; 45˚
of supination: t=1.55, P=0.13; neutral: t=0.62, P=0.54; 45˚ of
pronation: t=0.94, P=0.35; and 80˚ of pronation: t=0.80, P=0.43),
wrist pain (activities of daily living: t=1.33, P=0.19; and hard
work: t=1.75, P=0.09), modified Mayo Wrist score (t=0.86, P=0.39),
Disabilities of the Arm Shoulder and Hand score (t=0.78, P=0.44),
Patient-Rated Wrist Evaluation score (t=0.93, P=0.36), and patient
satisfaction (t=1.74, P=0.09) (Table
IV). Figs. 7, 8 and 9
show another representative case.
 | Table IVFunctional and clinical outcomes at
the final follow-up. |
Table IV
Functional and clinical outcomes at
the final follow-up.
| Outcome | BEF group
(n=30) | CEF group
(n=55) | Statistical
valuea | P-value |
|---|
| Active ROM, ˚ | | | | |
|
Flexion | 68.13±6.14 | 69.02±4.09 | 0.80 | 0.43 |
|
Extension | 52.43±3.39 | 53.36±2.37 | 1.48 | 0.14 |
|
Radial
deviation | 25.57±2.61 | 26.05±2.02 | 0.96 | 0.34 |
|
Ulnar
deviation | 29.60±3.20 | 30.40±3.33 | 1.07 | 0.29 |
|
Pronation | 83.30±5.86 | 84.75±5.19 | 1.17 | 0.25 |
|
Supination | 83.93±7.26 | 85.16±6.18 | 0.82 | 0.41 |
|
Grip
strength, % | 98.30±4.97 | 99.33±4.44 | 0.98 | 0.33 |
| Supination torque,
% | | | | |
|
90˚ of
supination | 80.93±4.17 | 91.18±3.47 | 1.48 | 0.14 |
|
45˚ of
supination | 94.53±1.81 | 95.02±1.08 | 1.55 | 0.13 |
|
Neutral | 89.23±5.65 | 88.42±5.92 | 0.62 | 0.54 |
|
45˚ of
pronation | 89.70±4.04 | 90.47±3.40 | 0.94 | 0.35 |
|
80˚ of
pronation | 95.50±4.28 | 96.13±2.93 | 0.80 | 0.43 |
| Wrist pain score
(NRS) | | | | |
|
Rest | 0 | 0 | - | - |
|
Activities
of daily living | 1.30±0.92 | 1.05±0.76 | 1.33 | 0.19 |
|
Hard
work | 1.83±1.29 | 1.40±0.97 | 1.75 | 0.09 |
| Modified Mayo Wrist
score | 92.23±4.22 | 93.13±4.75 | 0.86 | 0.39 |
| DASH score | 8.00±5.10 | 8.85±4.66 | 0.78 | 0.44 |
| PRWE score | 9.80±4.90 | 8.69±5.46 | 0.93 | 0.36 |
| Patient
satisfaction | 9.20±0.66 | 9.45±0.63 | 1.74 | 0.09 |
Discussion
The present study found that CEF may be as effective
as BEF in preventing RHL in older patients with DRF. Percutaneous
bony distraction may be more effective than conventional
distraction manoeuvres for achieving anatomical reduction with
minor morbidity. Both conventional and bony distraction manoeuvres
can produce similar functional outcomes and patient satisfaction
only if a good reduction has been achieved. The outcomes show that
there are no complications due to the percutaneous bony
distraction. The two techniques demonstrate a similar ability for
bone remodeling. Moreover, CEF is less expensive than BEF.
RHL is commonly observed in older patients due to
the axial load on the wrist (22).
RHL produces abnormal volar tilt, radial inclination and ulnar
variance (23). The abnormalities
further contribute to the development of ulnar impaction syndrome,
triangular fibrocartilage complex tears, distal radioulnar joint
instability, ulnar carpal arthritis, and rupture of the extensor
tendons of the little and ring fingers (24).
Various surgical techniques can be employed for
distal radius fractures in older patients. Non-surgical treatments
using a splint or cast are commonly used in minimally displaced or
reducible fractures, but RHL often occurs after 3 weeks due to
osteoporosis, comminution and absorbable collapse at the fracture
site (25,26). Open reduction and plating are
straightforward techniques that provide radial support; however, an
axial load can still be applied to the distal radius. RHL may also
occur postoperatively in patients with osteoporosis, comminution or
insufficient consideration. The use of a bridging external fixator
can effectively avoid axial load on the distal radius and wire
migration (27), but small
fragments of the distal radius cannot be maintained, even when
several spins are used. To reinforce fixation, CEF combining both
BEF and non-BEF has been developed.
Meng et al (28) reported a study in which 78 types of
A2, A3 and B1 distal radius fractures were treated using
percutaneous fixation using a cemented K-wire CEF. It was suggested
that this minimally invasive technique effectively prevented
redisplacement and wire migration, as the cement frame secured all
the pins together. Moreover, percutaneous bony distraction is also
more powerful and effective than conventional distraction in
restoring the radial height, resulting in a high-quality reduction.
This simplifies the preoperative plan, as all distal fragments can
be automatically reduced under powerful bony distraction. The
rationale is that the ligaments and tendons surrounding the wrist
(such as the rotator cuff of the shoulder) are tension-like
splints, pushing the fragments to be reduced. The present study
showed that BEF and CEF achieved similar radiological parameters
and functional outcomes. However, CEF had more advantages than BEF
in achieving a higher rate of successful closed reduction, shorter
operative time and lower treatment cost. The Lidström
classification categorises DRFs based on the fracture line,
direction of displacement, degree of displacement, articular
involvement and distal radioulnar joint involvement. The similar
changes observed between the time of bone healing and the final
follow-up in both techniques suggest a comparable ability for bone
remodeling.
The indication for CEF is AO/OTA classification type
A2, A3, B1, B3, C1, C2 and C3 distal radius fractures, especially
in older adult patients (≥55 years) with poor bone quality and
comminuted fractures, either open or closed fractures, and either
extra- or intraarticular fractures. Contraindications include minor
displacement, old fractures, infection statues and health issues.
The advantages of CEF are that it is easy to perform and has a high
success rate, especially if surgeons are familiar with the volar
wrist anatomy; inexperienced surgeons can identify structures using
ultrasonography or place the reduction pin via blunt dissection
through a small incision. Pin migration into the radiocarpal joint
due to articular fragmentation is rare; however, pin reduction may
also be achieved in this setting. Alternatively, adjustment of the
pin direction is preferred. Anatomical reduction with intact soft
tissues surrounding the wrist may lead to superior wrist function.
No complications due to over-distraction to the ligaments are
observed. However, the shortcomings of CEF include the risk of
iatrogenic injuries to the tendons, median nerve, superficial
branch of the radial nerve and radial artery (29). The present study confirmed that
minimally invasive CEF can achieve satisfactory fracture reduction
and strong external fixation with a short operative time and low
treatment cost.
Infection is a rare complication of minimally
invasive surgery following distal radius fracture. Pin-site
infection occurred in 1 patient (1/30, 3.3%) in the BEF group and
in 1 patient (1/55, 1.8%) in the CEF group, and both are lower than
the rate of pin-site infection (10.3%) reported in the literature
(30). Most pin-site infections
are relatively minor and resolve with disinfectant care, oral
antibiotic therapy and/or removal of the external fixator. Pin
loosening is associated with a high risk of pin-site infection,
which can be reduced by securing all the wire ends to a cemented
CEF (28). The surgeons should not
only pay attention to intraoperative sterilization but also to the
treatment of related underlying diseases, such as diabetes,
hypoimmunity, hypoproteinemia and infection of other body
parts.
The most common reason for distal radial malunion is
improper treatment, with an incidence rate of 33% (31). Malunion is defined as one of the
following: Radial inclination <15˚ on posteroanterior view;
radial length >5 mm shortening on posteroanterior view; radial
tilt >15˚ dorsally or 20˚ volar tilt on lateral view; or
articular incongruity >2 mm of step-off (30). When the DRF is less shortened, bone
grafting may not be necessary if the DRF is stable and some
anterior cortical contact remains. When intraoperative reduction
creates a large space with a loss of cortical contact, the risk of
malunion is greater, and bone grafting is required to avoid
postoperative fracture non-union. Allogeneic bone grafts, including
corticocancellous or cancellous bone, may be suitable candidates;
however, autogenous iliac grafts remain the optimal selection both
mechanically and biologically. During the postoperative follow-up,
high-resolution peripheral CT is feasible to further the evaluation
of bone healing in DRF (32). In
the present study, all patients in both groups showed satisfactory
bone healing, and no postoperative fracture non-union was
observed.
The present study had some limitations. First, the
treatments could not be performed in blinded manner due to the
nature of the study, which may have resulted in a selection bias.
Second, the manoeuvres and assessments were performed at different
time points, and the surgeons' experience improved with time,
thereby influencing the ascertainment of the effects of the
techniques. Third, the biomechanics of fixation were not assessed
and should be investigated in future studies and in randomised
controlled multicentre clinical trials to further determine the
efficacy of the treatments.
In conclusion, CEF may be as effective as BEF in
preventing RHL in older patients with DRF. Percutaneous bony
distraction may prove more effective than conventional distraction
manoeuvres in achieving anatomical reduction with minor morbidity.
The two techniques demonstrate a similar ability for bone
remodeling. Further studies are needed to explore the therapeutic
advantages of CEF over BEF, especially considering its lower cost
when compared with BEF.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JL and WD were involved in the study conception,
design, implementation, data analysis and interpretation, as well
as the writing of the paper. XZ and YPY contributed to the
collection, analysis and interpretation of data. DZ and YY
participated in implementation of the surgery and data collection.
RC was involved in the study conception and design. All listed
authors have made significant contributions to the development and
writing of this article. All authors have read and approved the
manuscript. JL and WD confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The research protocol was approved by the
Investigational Review Board of Jingxing County Hospital
(Shijiazhuang, China; approval no. 2017005), and written informed
consent was obtained from all participants prior to the study.
Patient consent for publication
The patients involved in this study consented to the
publication of their images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shapiro LM and Kamal RN: Management of
Distal Radius Fractures Work Group; Nonvoting Clinical Contributor;
Nonvoting Oversight Chairs; Staff of the American Academy of
Orthopaedic Surgeons and the American Society for Surgery of the
Hand. Distal Radius Fracture Clinical Practice Guidelines-Updates
and Clinical Implications. J Hand Surg Am. 46:807–811.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Meena S, Sharma P, Sambharia AK and Dawar
A: Fractures of distal radius: An overview. J Family Med Prim Care.
3:325–332. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Summers K, Mabrouk A and Fowles SM: Colles
Fracture, 2023 Jul 31. In: StatPearls [Internet]. Treasure Island
(FL), StatPearls Publishing, Jan, 2025.
|
|
4
|
Figl M, Weninger P, Liska M, Hofbauer M
and Leixnering M: Volar fixed-angle plate osteosynthesis of
unstable distal radius fractures: 12 months results. Arch Orthop
Trauma Surg. 129:661–669. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
LaMartina J, Jawa A, Stucken C, Merlin G
and Tornetta P III: Predicting alignment after closed reduction and
casting of distal radius fractures. J Hand Surg Am. 40:934–939.
2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Han LR, Jin CX, Yan J, Han SZ, He XB and
Yang XF: Effectiveness of external fixator combined with T-plate
internal fixation for the treatment of comminuted distal radius
fractures. Genet Mol Res. 14:2912–2919. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ruch DS, Ginn TA, Yang CC, Smith BP,
Rushing J and Hanel DP: Use of a distraction plate for distal
radial fractures with metaphyseal and diaphyseal comminution. J
Bone Joint Surg Am. 87:945–954. 2005.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kennedy SA and Hanel DP: Complex distal
radius fractures. Orthop Clin North Am. 44:81–92. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kulshrestha V, Roy T and Audige L: Dynamic
vs static external fixation of distal radial fractures: A
randomized study. Indian J Orthop. 45:527–534. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Synn AJ, Makhni EC, Makhni MC, Rozental TD
and Day CS: Distal radius fractures in older patients: Is anatomic
reduction necessary? Clin Orthop Relat Res. 467:1612–1620.
2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mehta SP, MacDermid JC, Richardson J,
MacIntyre NJ and Grewal R: A systematic review of the measurement
properties of the patient-rated wrist evaluation. J Orthop Sports
Phys Ther. 45:289–298. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Capo JT, Rossy W, Henry P, Maurer RJ,
Naidu S and Chen L: External fixation of distal radius fractures:
Effect of distraction and duration. J Hand Surg Am. 34:1605–1611.
2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Alter TH, Varghese BB, DelPrete CR, Katt
BM and Monica JT: Reduction techniques in volar locking plate
fixation of distal radius fractures. Tech Hand Up Extrem Surg.
26:168–177. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lidstrom A: Fractures of the distal end of
the radius: A clinical and statistical study of end results. Acta
Orthop Scand Suppl. 41:1–118. 1959.PubMed/NCBI
|
|
15
|
McConkey MO, Schwab TD, Travlos A, Oxland
TR and Goetz T: Quantification of pronator quadratus contribution
to isometric pronation torque of the forearm. J Hand Surg Am.
34:1612–1617. 2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Incel NA, Ceceli E, Durukan PB, Erdem HR
and Yorgancioglu ZR: Grip strength: Effect of hand dominance.
Singapore Med J. 43:234–237. 2002.PubMed/NCBI
|
|
17
|
Cantero-Téllez R, Algar LA, Cruz Gambero
L, Villafañe JH and Naughton N: Joint position sense testing at the
wrist and its correlations with kinesiophobia and pain intensity in
individuals who have sustained a distal radius fracture: A
cross-sectional study. J Hand Ther. 37:218–223. 2024.PubMed/NCBI View Article : Google Scholar
|
|
18
|
MacDermid JC, Turgeon T, Richards RS,
Beadle M and Roth JH: Patient rating of wrist pain and disability:
A reliable and valid measurement tool. J Orthop Trauma. 12:577–586.
1998.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wajngarten D, Campos JÁDB and Garcia PPNS:
The disabilities of the Arm, Shoulder and Hand scale in the
evaluation of disability-A literature review. Med Lav. 108:314–323.
2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mulders MAM, Kleipool SC, Dingemans SA,
van Eerten PV, Schepers T, Goslings JC and Schep NWL: Normative
data for the Patient-rated wrist evaluation questionnaire. J Hand
Ther. 31:287–294. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Green DP and O'Brien ET: Classification
and management of carpal dislocations. Clin Orthop Relat Res.
55–72. 1980.PubMed/NCBI
|
|
22
|
Zhang L, Jiang H, Zhou J and Jing J:
Comparison of modified K-wire fixation with open reduction and
internal fixation (ORIF) for unstable colles fracture in elderly
patients. Orthop Surg. 15:2621–2626. 2023.PubMed/NCBI View
Article : Google Scholar
|
|
23
|
Cheng MF, Chiang CC, Lin CC, Chang MC and
Wang CS: Loss of radial height in Extra-articular distal radial
fracture following volar locking plate fixation. Orthop Traumatol
Surg Res. 107(102842)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Im JH, Lee JW and Lee JY: Ulnar impaction
syndrome and TFCC injury: Their relationship and management. J
Wrist Surg. 14:14–26. 2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liddy N, Mohammed C, Kajitani SH, Prasad
N, Suresh SJ, Mathew P and LaPorte DM: Comparative outcomes of
surgical and nonsurgical treatments for scapholunate ligament
injuries with concomitant distal radius fractures: A systematic
review. Hand (N Y). 29(15589447251324533)2025.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Raittio L, Launonen AP, Hevonkorpi T,
Luokkala T, Kukkonen J, Reito A, Laitinen MK and Mattila VM: Two
casting methods compared in patients with Colles' fracture: A
pragmatic, randomized controlled trial. PLoS One.
15(e0232153)2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Biz C, Cerchiaro M, Belluzzi E, Bortolato
E, Rossin A, Berizzi A and Ruggieri P: Treatment of distal radius
fractures with bridging external fixator with optional percutaneous
K-Wires: What are the right indications for patient age, gender,
dominant limb and injury pattern? J Pers Med.
12(1532)2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Meng H, Xu B, Xu Y, Niu H, Liu N and Sun
D: Treatment of distal radius fractures using a cemented K-wire
frame. BMC Musculoskelet Disord. 23(591)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Gou Q, Xiong X, Cao D, He Y and Li X:
Volar locking plate versus external fixation for unstable distal
radius fractures: A systematic review and meta-analysis based on
randomized controlled trials. BMC Musculoskelet Disord.
22(433)2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Yuan ZZ, Yang Z, Liu Q and Liu YM:
Complications following open reduction and internal fixation versus
external fixation in treating unstable distal radius fractures:
Grading the evidence through a Meta-analysis. Orthop Traumatol Surg
Res. 104:95–103. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Cognet JM and Mares O: Distal radius
malunion in adults. Orthop Traumatol Surg Res.
107(102755)2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Van den Bergh JP, Szulc P, Cheung AM,
Bouxsein M, Engelke K and Chapurlat R: The clinical application of
high-resolution peripheral computed tomography (HR-pQCT) in adults:
State of the art and future directions. Osteoporos Int.
32:1465–1485. 2021.PubMed/NCBI View Article : Google Scholar
|