Introduction
Lesions of the maxillary sinus span an
inflammatory-to-neoplastic spectrum that often looks deceptively
similar on clinical examination and imaging (1-3).
Chronic inflammatory disease may present as a well-circumscribed,
expansile radiolucency with bony remodeling, features that are
characteristic of benign tumors, while true neoplasms can remain
radiographically indistinct until late in their course. Such
overlap is a recognized diagnostic pitfall that can lead to
overtreatment when an aggressive surgical approach is chosen for a
problem that could be managed otherwise (2).
Among the neoplasms in the list of differential
diagnoses is pleomorphic adenoma, a benign salivary-gland tumor
that only rarely arises in ectopic sites such as the paranasal
sinuses (4,5). In a retrospective study conducted on
Asian populations, pleomorphic adenoma arising in the maxillary
sinus accounted for approximately 0.06% (6). Although uncommon, pleomorphic adenoma
is frequently cited because its sharply demarcated margins and
tendency to displace adjacent structures can mimic other benign
expansile processes on cone-beam computed tomography (CBCT) or
Magnetic Resonance Imaging (MRI) (7). However, inflammatory entities,
including mucoceles, postoperative maxillary cysts, fungal
sinusitis, and chronic bacterial sinusitis, can produce identical
radiologic hallmarks, especially when longstanding obstruction
leads to progressive sinus expansion and cortical thinning
(8-11).
Herein, we report a case of chronic maxillary
sinusitis masquerading as a neoplasm in a 53-year-old man whose
large, well-defined maxillary sinus lesion was initially
interpreted as pleomorphic adenoma on incisional biopsy. The case
highlights i) the importance of correlating histopathology with the
full clinical-radiologic picture, ii) the limitations of small
biopsies in heterogeneous sinus lesions, and iii) practical
strategies to avoid unnecessary radical surgery. By highlighting
these diagnostic challenges and their resolution, this report aims
to refine the clinician's approach to expansile maxillary sinus
lesions and to contribute to the growing literature on inflammatory
mimics of sinonasal tumors. This study was exempt from review by
the Institutional Review Board of Gangneung-Wonju National
University Dental Hospital (exemption no. GWNUDH-IRB2025-A007;
Gangneung, South Korea).
Case report
A 53-year-old man was referred to Gangneung-Wonju
National University Dental Hospital (Gangneung, Republic of Korea)
in November 2024 after a routine panoramic radiograph revealed a
large, well-circumscribed radiolucent lesion occupying the right
maxillary sinus. The lesion was clinically silent as the patient,
who reported having no prior sinus infection, denied experiencing
pain, nasal obstruction, epistaxis, or visual disturbance. His
medical history included chronic hepatitis B and a remote thoracic
operation for a benign chest tumor, but no maxillofacial trauma or
surgery. Three years earlier the first and second right maxillary
molars had been extracted without complication.
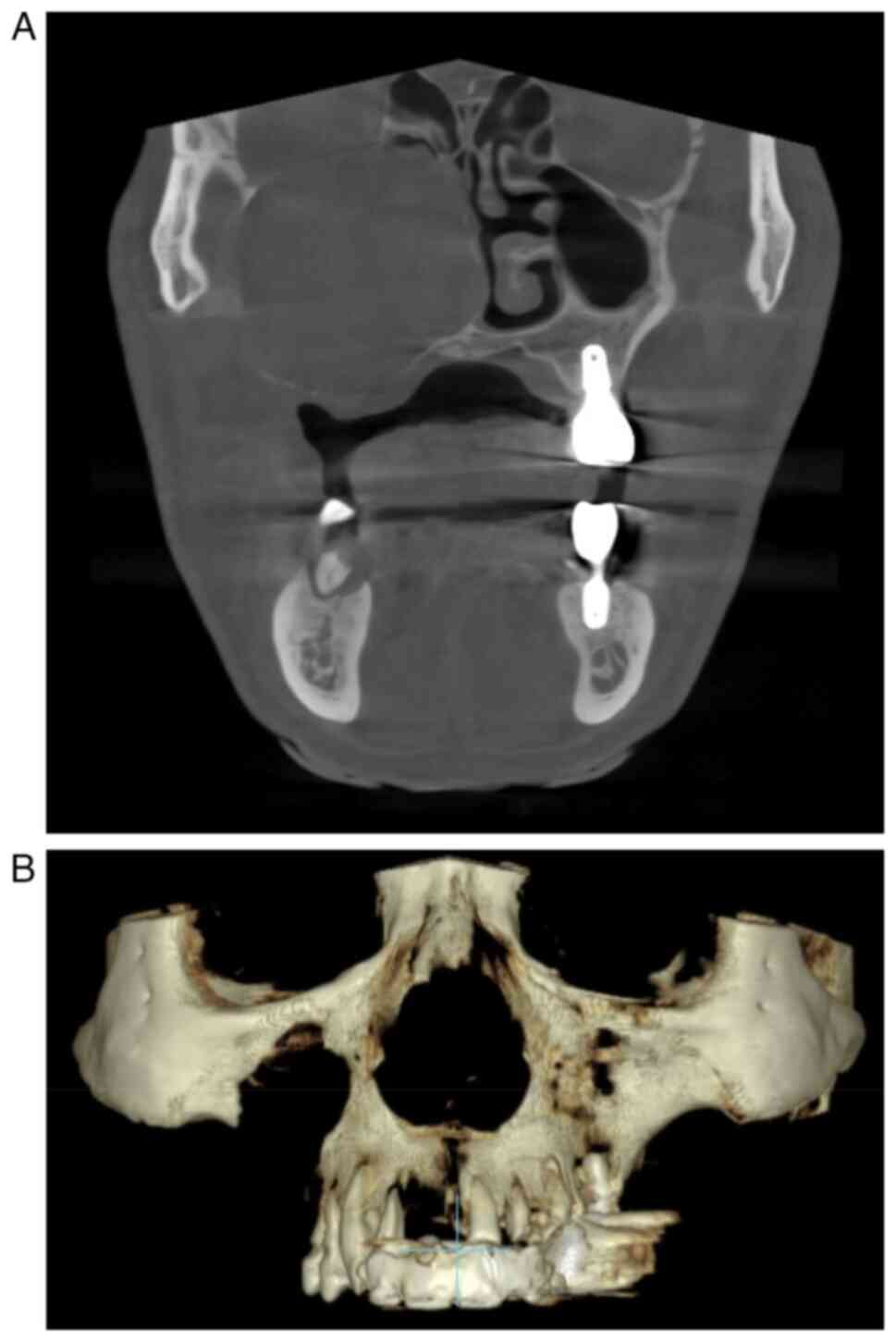
CBCT revealed an expansile mass measuring 53x43x49
mm with smooth cortical thinning, focal perforations of both buccal
and palatal plates, upward displacement of the orbital floor, and
mild deviation of the nasal septum (Fig. 1). The interior of the lesion was
homogeneously radiolucent, lacking calcifications or septa, and
demonstrated no mucosal thickening or fluid levels typical of
inflammatory sinus disease. These features indicated toward a
benign epithelial tumor-most plausibly a pleomorphic
adenoma-although the differential diagnoses included a mucocele,
postoperative maxillary cyst, and odontogenic lesion.
Intraoral incisional biopsy under local anesthesia
yielded scant, myxoid spindle-cell tissue interpreted as
‘pleomorphic adenoma like’. Because this histology did not fully
explain the degree of bony expansion, and because orbital support
might be jeopardized after tumor removal, we created a
patient-specific titanium implant (PSI) to reconstruct the orbital
floor if necessary. Since PSI placement required wide exposure, a
Weber-Ferguson approach was followed.
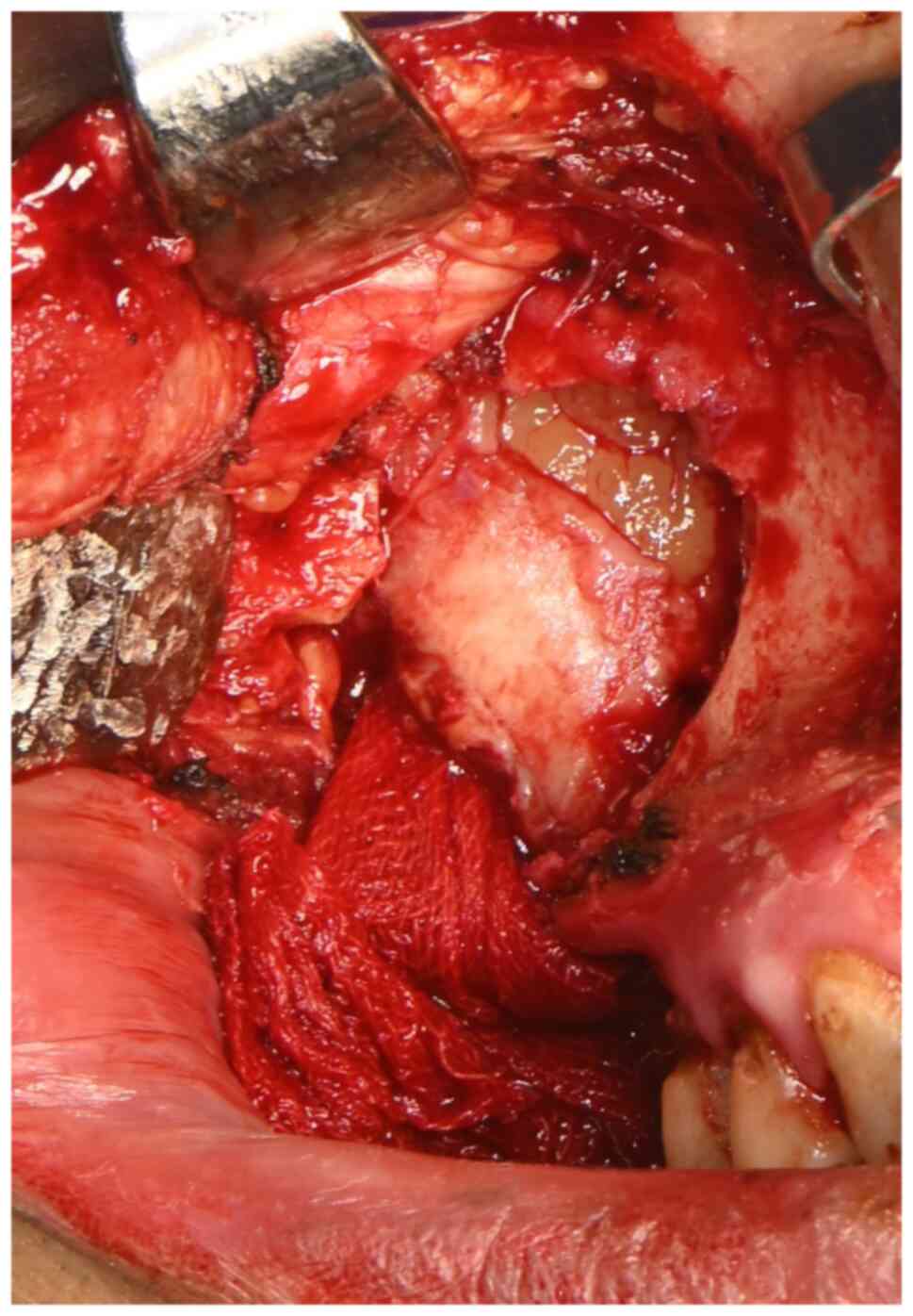
During surgery the mass was easily separated from
surrounding bone except at points of dense adhesions to the nasal
mucosa (Fig. 2). Once the mass was
removed, the underlying orbital floor was found to be just thinned
but not absent; the position of the globe was stable, and PSI
insertion was deferred. A small communication between the sinus and
the nasal cavity was closed, and Vaseline-gauze was packed for
hemostasis.
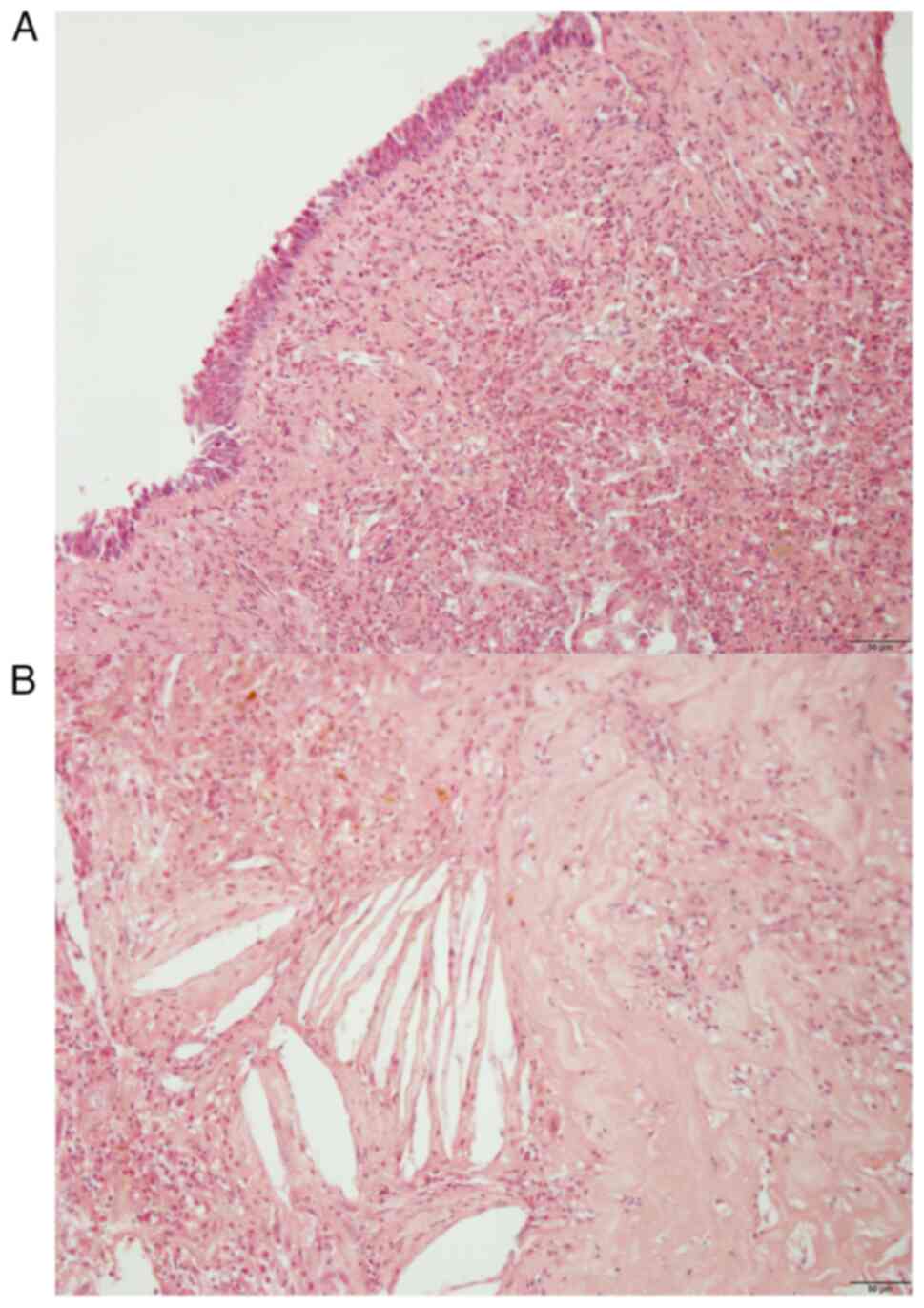
Definitive histopathology revealed a chronically
inflamed respiratory mucosa with granulation tissue, cholesterol
clefts, and fibrosis, but no salivary-gland or odontogenic tumor
elements, findings diagnostic of chronic maxillary sinusitis with
mucocele-like expansion (Fig. 3).
Postoperative CBCT performed 6 months later confirmed orbital
volume preservation, and the patient showed no clinical
manifestations of recurrence after six months of follow-up
(Fig. 4).
Discussion
Expansile, well-demarcated lesions of the maxillary
sinus are classically attributed to benign tumors or cysts
(12); however, chronic
inflammatory conditions, such as longstanding bacterial sinusitis,
fungal sinusitis, or obstructive mucoceles, may generate identical
imaging features when trapped secretions create sustained
hydrostatic pressure on the bony walls (13). In the present case, a 5-cm
radiolucency with cortical thinning, focal perforation, and orbital
floor elevation strongly suggested a salivary or odontogenic tumor.
However, definitive histology demonstrated only chronically
inflamed Schneiderian mucosa with fibrosis and cholesterol clefts,
confirming an inflammatory origin. Clinicians should therefore keep
‘tumor-like sinusitis’ in mind whenever an expansile maxillary mass
lacks the internal septations or heterogeneous enhancement typical
of true neoplasia (14).
Several entities were considered preoperatively.
First, pleomorphic adenoma was high on the list because the
lesion's smooth cortical expansion, orbital displacement, and
sharply defined borders resembled salivary-gland tumors reported in
the sinus. Despite a myxoid fragment from the first biopsy
strengthening this suspicion, the excised specimen ultimately
showed no salivary epithelial or myoepithelial elements, ruling the
diagnosis out. Sampling error is common because inflammatory sinus
cavities often contain reactive granulation tissue and metaplastic
epithelium that mimic neoplastic stroma (15). Reliance on a single limited sample
can misdirect treatment toward unnecessarily radical surgery. In
general diagnostic practice, the prevalence of misdiagnosis has
been reported to range from 5 to 15%, highlighting the importance
of coordinated clinicopathologic and radiologic evaluation to
ensure appropriate management (16,17).
Accurate diagnosis of maxillary sinus lesions requires close
collaboration among oral and maxillofacial surgeons, radiologists,
and pathologists. Whenever radiology, endoscopy, and the patient's
clinical presentation do not align with the results of an initial
biopsy, repeat or deeper sampling, or endoscopic sinus culture and
lavage, should be considered before definitive resection. A
mucocele or postoperative maxillary cyst was the next possibility;
both can produce a large, uniformly radiolucent cavity and remodel
surrounding bone when the ostium is chronically obstructed
(8,9,11).
In our patient, however, there was no prior sinus surgery, no
obstructive history, and no true cystic lining on histology;
findings more compatible with diffuse inflammatory change than with
a discrete cyst. Odontogenic lesions were also weighed. An
odontogenic keratocyst can scallop bone and expand the sinus from
below, whereas a myxoma often shows internal trabeculae or a
‘soap-bubble’ pattern (18). In
this case the epicenter lay within the sinus walls rather than in
the alveolar ridge, and neither keratin nor myxoid stroma was
identified microscopically, making these diagnoses unlikely.
Invasive fungal sinusitis can mimic neoplasm when it erodes bone,
especially in immunocompromised hosts, and scattered hyperdense
foci on CBCT sometimes betray fungal concretions (19). Finally, a cholesteatoma of the
maxillary sinus, which is rare but well documented, was
contemplated because it also causes bone erosion and may appear as
a soft-tissue mass (20).
Intraoperative inspection revealed none of the pearly keratin
debris typical of cholesteatoma, and the resected tissue lacked
keratinizing epithelium. By systematically excluding these
alternatives through clinical history, imaging features, and
definitive histopathology, we arrived at the final diagnosis of
chronic inflammatory sinusitis with mucocele-like expansion.
In conclusion, this case illustrates how, due to a
chronic inflammatory condition, the maxillary sinus can insidiously
become a large, expansile cavity that radiologically and
histologically mimics benign neoplasms. Thorough correlation of
clinical findings, cross-sectional imaging, and, crucially, the
pathology of the entire resected specimen was required to reach the
correct diagnosis and avoid unnecessary orbital reconstruction. Two
practical lessons emerge: i) An expansile, sharply marginated sinus
lesion should not automatically trigger oncologic surgery until
repeated or wide-field sampling confirms a tumor, and ii)
preoperative virtual planning with patient-specific implants is
prudent when orbital support appears threatened, but intraoperative
reassessment can spare patients foreign-body implantation when
residual bone proves adequate. Recognizing the inflammatory
masquerade of maxillary sinusitis can therefore reduce surgical
morbidity and guide more measured, evidence-based management of
similar lesions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
JHO contributed to the conception and design of the
report and drafted the initial manuscript. SYK collected clinical
data, organized the data, revised the manuscript and handled
correspondence with the journal. SGK contributed to the study
design and interpretation of clinical findings, supervised the
overall project, and provided critical revisions for important
intellectual content. JHO, SYK and SGK confirm the authenticity of
all the raw data. All the authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
This study was exempted from review by the
Institutional Review Board at Gangneung-Wonju National University
Dental Hospital (exemption no. GWNUDH-IRB2025-A007).
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and its accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Ji-Hyeon Oh: ORCID: 0000-0002-6050-7175 Seong-Gon
Kim: ORCID: 0000-0001-5088-2732 Su-Young Kim: ORCID:
0009-0000-6843-9608
References
|
1
|
Som PM, Brandwein MS, Maldjian C, Reino AJ
and Lawson W: Inflammatory pseudotumor of the maxillary sinus: CT
and MR findings in six cases. AJR Am J Roentgenol. 163:689–692.
1994.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Constantino Gde T, Sasaki F, Tavares RA,
Voegels RL and Butugan O: Inflammatory pseudotumors of the
paranasal sinuses. Braz J Otorhinolaryngol. 74:297–302.
2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kumar J, Daga R, Pradhan G and Meher R:
Sinonasal inflammation or neoplasm: Raise the red flagsǃ-A
pictorial review. Indian J Radiol Imaging. 33:522–531.
2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cai H, Zhang ZH, Zhou MZ, Wu YJ, Yue JX,
Zhou LQ, Chen GJ, Tian Y, Shen JX and Zhou T: A rare case of
sinonasal pleomorphic adenoma. Ear Nose Throat J. 104 (Suppl
2):412S–416S. 2025.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gana P and Masterson L: Pleomorphic
adenoma of the nasal septum: A case report. J Med Case Rep.
2(349)2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gao M, Hao Y, Huang MX, Ma DQ, Chen Y, Luo
HY, Gao Y, Cao ZQ, Peng X and Yu GY: Salivary gland tumours in a
northern Chinese population: A 50-year retrospective study of 7190
cases. Int J Oral Maxillofac Surg. 46:343–349. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kato H, Kawaguchi M, Ando T, Mizuta K,
Aoki M and Matsuo M: Pleomorphic adenoma of salivary glands: Common
and uncommon CT and MR imaging features. Jpn J Radiol. 36:463–471.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Alshoabi S and Gameraddin M: Giant frontal
mucocele presenting with displacement of the eye globe. Radiol Case
Rep. 13:627–630. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hwang SA, Kang BC, Yoon SJ, Liu L and Lee
JS: Bilateral postoperative maxillary cysts presenting as a
diagnostic challenge. Oral Biol Res. 42:168–173. 2018.
|
|
10
|
Reghunath A, Mittal MK, Thukral BB and
Sinha M: Approach to sinonasal masses: A comprehensive review. J
Head Neck Physicians Surg. 10:14–25. 2022.
|
|
11
|
Bahgat M, Bahgat Y and Bahgat A: Sphenoid
sinus mucocele. BMJ Case Rep. 2012(bcr2012007130)2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Han MH, Chang KH, Lee CH, Na DG, Yeon KM
and Han MC: Cystic expansile masses of the maxilla: Differential
diagnosis with CT and MR. AJNR Am J Neuroradiol. 16:333–338.
1995.PubMed/NCBI
|
|
13
|
Momeni AK, Roberts CC and Chew FS: Imaging
of chronic and exotic sinonasal disease: Review. AJR Am J
Roentgenol. 189 (Suppl 6):S35–S45. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Koeller KK: Radiologic features of
sinonasal tumors. Head Neck Pathol. 10:1–12. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tabaee A, Hsu AK and Kacker A:
Indications, technique, safety, and accuracy of office-based nasal
endoscopy with biopsy for sinonasal neoplasm. Int Forum Allergy
Rhinol. 1:225–228. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Newman-Toker DE, Peterson SM, Badihian S,
Hassoon A, Nassery N, Parizadeh D, Wilson LM, Jia Y, Omron R,
Tharmarajah S, Guerin L, et al: AHRQ comparative effectiveness
reviews. In: Diagnostic Errors in the Emergency Department: A
Systematic Review. Agency for Healthcare Research and Quality,
Rockville, MD, 2022.
|
|
17
|
Singh H, Meyer AN and Thomas EJ: The
frequency of diagnostic errors in outpatient care: Estimations from
three large observational studies involving US adult populations.
BMJ Qual Saf. 23:727–731. 2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Byun JH, Kang YH, Choi MJ and Park BW:
Expansile keratocystic odontogenic tumor in the maxilla:
Immunohistochemical studies and review of literature. J Korean
Assoc Oral Maxillofac Surg. 39:182–187. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ni Mhurchu E, Ospina J, Janjua AS,
Shewchuk JR and Vertinsky AT: Fungal Rhinosinusitis: A radiological
review with intraoperative correlation. Can Assoc Radiol J.
68:178–186. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Storper IS and Newman AN: Cholesteatoma of
the maxillary sinus. Arch Otolaryngol Head Neck Surg. 118:975–977.
1992.PubMed/NCBI View Article : Google Scholar
|