Introduction
Osteoporosis, a metabolic disease affecting millions
of older adults globally, is represented by the deterioration of
bone mass and microarchitecture, leading to fragility fracture
(1). Dual-energy X-ray
absorptiometry (DXA) is the gold-standard method for diagnosing
osteoporosis. It quantifies bone mineral density (BMD) as a
surrogate of bone strength. However, DXA is not portable and emits
ionising radiation. Therefore, it is unsuitable for deployment in
mass bone health screening. These limitations can be overcome with
quantitative ultrasonometry (QUS), which provides alternative
measures of bone health (2).
Previous studies have established that QUS indices predict
osteoporosis/osteopenia (3,4) and
fracture risk (5) and may reflect
microarchitecture (6).
Apart from being female and menopausal, being
underweight is a major risk factor for osteoporosis (7,8). A
low body weight negatively impacts bone health by acting as a
surrogate for malnutrition or exerting low mechanical loading on
bone (9). Mechanical loading is
important to stimulate bone repair and maintain bone health
(10). Previous studies have
firmly established body weight and the body mass index (BMI) as
positive predictors of bone health status (11). Obesity, defined by BMI, is found to
decrease the odds of osteoporosis by 70.1% (11). The BMI is reflective of body size
but may not reflect adiposity status correctly (12). It underestimates the degree of
adiposity in patients with sarcopenia but overestimates that in
athletes (12). The relationship
between adiposity and bone health remains controversial even after
the delineation of the effects of the BMI (13).
Adiposity may be a double-edged sword for bone
health. On the positive side, it exerts mechanical loading on bone;
such loading stimulates bone mass accrual to support a person's
weight (14). Adipose tissue also
synthesises oestrogens, which are beneficial for bone health
(15). Furthermore, the
hyperinsulinaemia that is often associated with obesity can
increase bone mass because of the anabolic action of insulin
(16).
On the negative side, adiposity is associated with
chronic inflammation, a state known to cause bone loss. Adipokines
secreted by adipocytes, such as adiponectin and resistin, can
actively promote bone loss (17,18).
Meanwhile, leptin's role is complex: It can be either pro- or
antiosteogenic depending on whether it regulates bone health
through central or peripheral pathways (19). Therefore, the net effect of
adiposity on bone health remains debatable.
Other indices have been developed as alternatives in
consideration of the limitations of the BMI in reflecting
adiposity. Waist circumference (WC) (20), waist-to-hip ratio (WHR) (21), waist-to-height ratio (WtHR)
(22), a body shape index (ABSI)
(23), body roundness index (BRI)
(24) and conicity index (CI)
(25), derived from body
anthropometric measurements, can predict cardiometabolic risks
well. The relationship between these alternative adiposity indices
and bone health has been explored. However, most studies that
investigated these relationships are derived from the databases of
the National Health and Nutrition Examination Survey on the United
States population (26-32),
whereas those from other geographical regions are sparse (33-37).
Heterogenous findings, whereby negative and positive relationships
between adiposity indicated by the above indices and bone health
have been observed, have been obtained. These gaps suggest that
additional studies on diverse populations should be
implemented.
The present study attempts to address the above
research gaps by comparing the associations between various
adiposity indices and bone health measured via calcaneal QUS
amongst Malaysians. It will help clarify the effect of adiposity on
bone health. Its findings are particularly important for Malaysians
at two levels. Firstly, Malaysia is rapidly advancing to an ageing
society, with 15% of the overall population projected to be aged 60
years or above by 2030(38).
Secondly, Malaysians have a combined obesity and overweight
prevalence of 54.4% (39). The
compounded effects of ageing and obesity could have an influence on
the prevalence of osteoporosis in Malaysia. Therefore, the present
study offers insight into adiposity as an interventional target in
osteoporosis.
Patients and methods
Ethical considerations
The study protocol was reviewed and approved by the
Universiti Kebangsaan Malaysia Ethics Committee (Kuala Lumpur,
Malaysia; approval code: JEP-2024-739). Subjects were briefed on
the details of the study and provided written informed consent
before participating.
Subject recruitment
This cross-sectional study was conducted from
October 2024 to November 2024 in conjunction with the institutional
Osteoporosis Month programme. Subjects were recruited through
purposive sampling, in which all individuals who met the selection
criteria were invited to participate in the study. The purposive
sampling strategy was adopted because of the nature of the health
screening event. The screening site was the lobby of Hospital
Canselor Tuanku Muhriz, affiliated with Universiti Kebangsaan
Malaysia (Kuala Lumpur, Malaysia). The researchers were aware of
the biases carried by the recruitment strategy. These biases are
discussed amongst the limitations of the study.
The subjects included were adult Malaysians aged 20
years and above. They were excluded if they declared having medical
conditions affecting bone health (such as Paget's disease,
osteogenesis imperfecta, osteomalacia, rickets,
hyper/hypothyroidism, hyper/hypoparathyroidism and chronic kidney
diseases) or taking medication that affects bone health [such as
glucocorticoids, sex hormones, aromatase inhibitors, androgen
deprivation therapy, anticoagulants (heparin and warfarin), loop
diuretics, chemotherapeutics, anticonvulsants, antidepressants,
thiazolidinediones and antiretrovirals].
Sample size calculation
Sample size was calculated by using G*Power version
3.1.97 (Heinrich-Heine-Universität) with input effect size=0.15
(moderate effect size by convention), alpha error=0.05, power=0.8
and number of predictors (variables of interest and
confounders)=16. The calculated minimum sample was 143.
Confounder measurements
The subjects answered a demographic, lifestyle and
medical history questionnaire that has been used in previous bone
health studies (40). Their date
of birth and citizenship were identified from their national
registration identity card. Their biological sex, ethnicity,
household income, pre-existing medical conditions and medical use
were self-declared. The lifestyle questionnaire explores the
subjects' habits in smoking cigarettes and consuming alcohol, dairy
products, tea and coffee. Female subjects answered additional
questions on menstrual status.
Anthropometric measurements
The subjects' waist circumference at the midpoint
between the lowest point of the ribcage and highest point of the
iliac crest was determined by using a measuring tape. Hip
circumference was measured at the widest part of the gluteal
muscle. The subjects' height without shoes was measured with a
stadiometer. These three measurements were recorded to the nearest
1 cm. The subjects' body weight while wearing light clothing
without shoes was recorded by using a scale (BC353; Accunic) to the
nearest 0.1 kg.
Calculation of adiposity indices
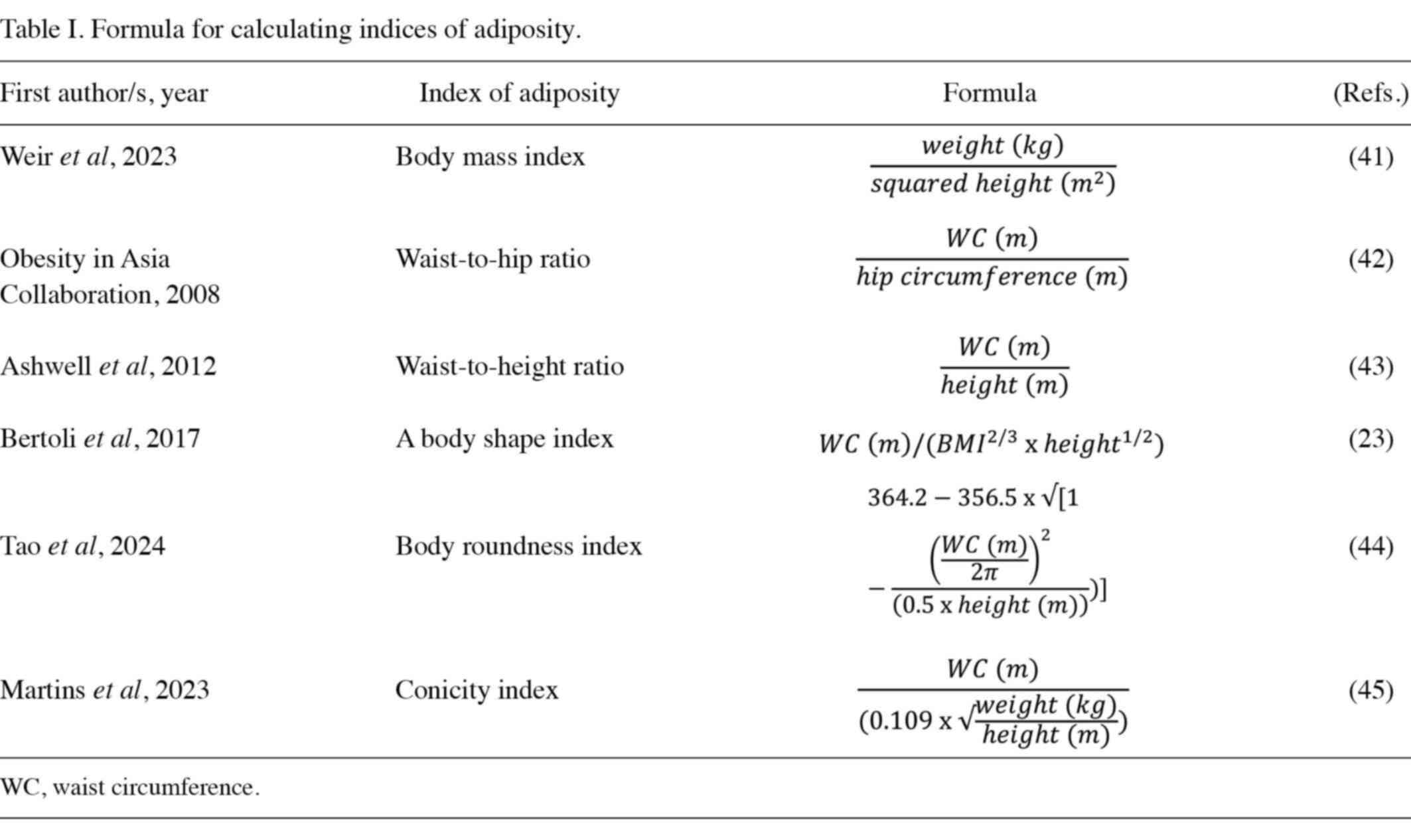
The adiposity indices BMI (41), WHR (42), WtHR (43), ABSI (23), BRI (44) and CI (45) were calculated on the basis of the
formulas shown in Table I.
Bone health measurements
The bone health of the subjects was quantified by
using a calcaneal bone sonometer (OSTEOKJ3000; Kejin) and recorded
as speed of sound (SOS) and broadband ultrasound attenuation (BUA).
The osteoporosis index (OI) was calculated automatically by using
the formula OI=0.106 x SOS + 0.5 x BUA-127.4, as preset by the
manufacturer. The subject inserted their nondominant foot into the
holder. Two oil-filled balloon transducers were inflated to touch
the lateral sides of the calcaneus, which had been cleaned with
alcohol and covered with ultrasonic gel. Ultrasound was transmitted
through the calcaneal bone and the device interpreted signals. Each
subject was measured two times and a third reading was taken when
the previous two readings were inconsistent. The categorisation of
subjects based on T-score or Z-score was not performed in the
present study because the World Health Organisation's cut-offs
apply only to DXA. Therefore, raw OI values were used to reflect
the bone health of the subject, in which a high value indicates
good bone health.
Statistical analysis
The Kolmogorov-Smirnov test was used to test for
data normality. The subjects' characteristics were compared between
men and women by using an independent-samples t-test for normally
distributed parameters and the Mann-Whitney U-test for skewed data.
Comparison between categorical variables was conducted by employing
the Chi-squared test or Fisher's exact test. Multiple linear
regression was used to investigate the association between OI and
bone health, with adjustment for potential confounders, such as
age, sex, ethnicity, status of smoking (yes or former/no), status
of alcohol use (yes or former/no), status of regular
milk/tea/coffee consumption (yes/no), calcium supplements (yes/no),
self-reported fracture (yes/no), self-reported parental fracture
(yes/no), self-reported height reduction (yes/no), use of
medication (yes/no) and presence of comorbidities (yes/no). Cook's
distance was employed to identify multivariate outliers, which were
subsequently removed to ensure the generalisability of the models.
Associations were reported in the form of B and β values.
Statistical analysis was performed by utilising SPSS version 26
(IBM, Corp.). The data were expressed as mean standard ± deviation
and n (%). P<0.05 was considered to indicate a statistically
significant difference.
Results
Subject characteristics
The present study recruited 320 subjects (231 women
and 89 men) within the study period. The mean age of the subjects
was 50.1±16.7 years. The height, weight, waist circumference, WHR,
WtHR, CI, BRI, ABSI, skeletal muscle mass, visceral fat area, BUA
and OI of men were significantly higher compared with women
(P>0.05). The body fat percentage of women was significantly
higher compared with men (P>0.05; Table II). Significantly more men were
regular cigarette smokers and alcohol consumers (P<0.05).
Significantly more women were regular coffee and calcium supplement
consumers (P<0.05). The distributions of ethnicity, regular milk
and tea consumption, self-reported fracture history, parental
fracture history and height reduction were not significantly
different between sexes (P>0.05; Table III).
 | Table IISubject's age, body composition and
calcaneal quantitative ultrasonometry data. |
Table II
Subject's age, body composition and
calcaneal quantitative ultrasonometry data.
| Parameter | Total (n=320) | Women (n=231) | Men (n=89) | P-value |
|---|
| Age, years | 50.1±16.7 | 50.0±16.0 | 50.5±18.5 | 0.802 |
| Height, cm | 159.8±8.4 | 156.1±5.2 | 169.4±7.5 | <0.001 |
| Weight, kg | 66.8±16.4 | 63.4±14.2 | 75.6±18.5 |
<0.001a |
| Body weight index,
kg/m2 | 26.1±5.6 | 26.0±5.7 | 26.2±5.5 | 0.770a |
| Waist
circumference, cm | 85.1±12.0 | 82.1±10.1 | 92.7±13.2 | <0.001 |
| Waist-to-hip
ratio | 0.89±0.09 | 0.87±0.07 | 0.94±0.12 | 0.009b |
| Waist-to-height
ratio | 0.53±0.07 | 0.53±0.07 | 0.55±0.07 | 0.017 |
| Conicity index | 1.21±0.06 | 1.19±0.03 | 1.28±0.06 | <0.001 |
| Body roundness
index | 4.08±1.46 | 3.96±1.39 | 4.39±1.61 | 0.024a |
| A body shape
index | 0.077±0.004 | 0.075±0.002 | 0.081±0.003 |
<0.001b |
| Skeletal muscle
mass, kg | 24.9±5.4 | 22.6±3.3 | 30.8±5.4 |
<0.001c |
| Fat mass, kg | 21.6±8.9 | 22.2±8.5 | 20.1±9.7 | 0.060 |
| Body fat
percentage, % | 31.5±7.2 | 33.8±5.9 | 25.3±6.9 | <0.001 |
| Visceral fat area,
cm2 | 99.1±52.0 | 90.7±47.2 | 120.9±57.8 |
<0.001a |
| Speed of sound,
m/sec | 1,530.3±26.5 | 1,528.9±24.1 | 1,533.9±31.9 | 0.183 |
| Broadband
attenuation of sound, dB/MHz | 25.1±6.1 | 24.1±5.7 | 27.5±6.5 | <0.001 |
| Osteoporosis
index | 47.0±5.4 | 46.4±4.9 | 48.6±6.2 | 0.003 |
 | Table IIISubject characteristics. |
Table III
Subject characteristics.
| Item | Total (n=320) | Women (n=231) | Men (n=89) | P-value |
|---|
| Ethnicity | | | | 0.145 |
|
Malay | 180 (56.3) | 137 (59.3) | 43 (48.3) | |
|
Chinese | 113 (35.3) | 79 (34.2) | 34 (38.2) | |
|
Indian | 18 (5.6) | 10 (4.3) | 8(9) | |
|
Others | 9 (2.8) | 5 (2.2) | 4 (4.5) | |
| Menstrual
status | | | | NR |
|
Regular | 105 (45.5) | 105 (45.5) | NR | |
|
Irregular | 16 (6.9) | 16 (6.9) | NR | |
|
Menopausal | 110 (47.6) | 110 (47.6) | NR | |
| Regular
smokinga | | | | <0.001 |
|
No | 303 (94.7) | 227 (98.3) | 76 (85.4) | |
|
Yes | 17 (5.3) | 4 (1.7) | 13 (14.6) | |
| Regular alcohol
drinking | | | | 0.009 |
|
No | 304(95) | 224(97) | 80 (89.9) | |
|
Yes | 16(5) | 7(3) | 9 (10.1) | |
| Regular milk
consumption | | | | 0.845 |
|
No | 195 (60.9) | 140 (60.6) | 55 (61.8) | |
|
Yes | 125 (39.1) | 91 (39.4) | 34 (38.2) | |
| Regular coffee
drinking | | | | 0.021 |
|
No | 161 (50.3) | 107 (46.3) | 54 (60.7) | |
|
Yes | 159 (49.7) | 124 (53.7) | 35 (39.3) | |
| Regular tea
drinking | | | | 0.289 |
|
No | 177 (55.3) | 132 (57.1) | 45 (50.6) | |
|
Yes | 143 (44.7) | 99 (42.9) | 44 (49.4) | |
| Regular calcium
supplement | | | | 0.018 |
|
No | 228 (71.3) | 156 (67.5) | 72 (80.9) | |
|
Yes | 92 (28.7) | 75 (32.5) | 17 (19.1) | |
| Self-reported
fracture history | | | | 0.962 |
|
No | 280 (87.5) | 202 (87.4) | 78 (87.6) | |
|
Yes | 40 (12.5) | 29 (12.6) | 11 (12.4) | |
| Self-reported
parental fracture | | | | 0.151 |
|
No | 273 (85.3) | 193 (83.5) | 80 (89.9) | |
|
Yes | 47 (14.7) | 38 (16.5) | 9 (10.1) | |
| Self-reported
height reduction | | | | 0.238 |
|
No | 280 (87.5) | 199 (86.1) | 81(91) | |
|
Yes | 40 (12.5) | 32 (13.9) | 8(9) | |
Association between bone health and
adiposity indices
Linear regression revealed a positive association
between OI and BMI (β=0.212, P<0.001), waist circumference
(β=0.268, P<0.001), WtHR (β=0.190, P=0.001), CI (β=0.151,
P=0.007) and BRI (β=0.203, P<0.001) before adjustment for
confounders (Table IV, Model 1).
After adjustment for confounders (Table IV, Model 2), a significant
positive association was found between OI and BMI (β=0.172,
P<0.001), waist circumference (β=0.184, P=0.001), WHR (β=0.124,
P=0.025), WtHR (β=0.160, P=0.002) and BRI (β=0.165, P=0.001). A
significant negative association was found between OI and ABSI
(β=-0.183, P=0.008). The changes in the regression coefficient with
the increment of confounders are presented in Table SI. The associations between OI and
adiposity indices were consistent in each model, showing their
robustness.
 | Table IVAssociation between bone health
(osteoporosis index) and adiposity indices. |
Table IV
Association between bone health
(osteoporosis index) and adiposity indices.
| | | Model 1 | Model 2 |
|---|
| Parameter | na | B | SE | β | P-value | B | SE | β | P-value |
|---|
| Body mass
index | 300 | 0.189 | 0.05 | 0.212 | <0.001 | 0.152 | 0.043 | 0.172 | <0.001 |
| Waist
circumference | 300 | 0.105 | 0.022 | 0.268 | <0.001 | 0.072 | 0.021 | 0.184 | 0.001 |
| Waist-to-hip
ratio | 302 | 1.182 | 3.024 | 0.022 | 0.700 | 6.485 | 2.874 | 0.124 | 0.025 |
| Waist-to-height
ratio | 302 | 13.756 | 4.111 | 0.190 | 0.001 | 11.581 | 3.625 | 0.16 | 0.002 |
| Conicity index | 302 | 14.647 | 5.367 | 0.151 | 0.007 | 7.106 | 7.078 | 0.073 | 0.316 |
| Body roundness
index | 302 | 0.695 | 0.194 | 0.203 | <0.001 | 0.566 | 0.171 | 0.165 | 0.001 |
| A body shape
index | 298 | 5.529 | 79.668 | 0.004 | 0.945 | -251.311 | 94.264 | -0.183 | 0.008 |
Discussion
The present cross-sectional study found a positive
association between bone health and BMI, waist circumference, WHR,
WtHR, CI and BRI and a negative association between bone health and
ABSI amongst Malaysians. It found no significant association
between bone health and CI.
In the present study, the BMI was found to be
positively associated with bone health. This observation agrees
with the authors' previous findings on Malaysian men aged >20
years that revealed a positive relationship between BMI and bone
health, as indicated by QUS (46).
As mentioned earlier, underweight is well recognised as a strong
risk factor for osteoporosis (7,8). A
Mendelian randomisation study demonstrated a causal relationship
between BMI and BMD; however, this relationship is site-specific
(47). A high BMI was found to
causally increase the BMD at the lumbar spine and calcaneus but
exerts no effects on forearm and femoral neck BMD (47). This association is likely driven by
mechanical loading (11). However,
the relationship between the BMI and bone health is highly complex.
A meta-analysis reported a low risk of vertebral fracture with a
high BMI in men, whereas the inverse was observed in women after
adjustment for BMD (48). Another
meta-analysis found that an increased BMI was associated with
trabecular microarchitecture deterioration (49). Therefore, an increased BMI
associated with BMD does not always translate into improved bone
quality.
In this work, bone health was positively associated
with the waist circumference, WHR, WtHR and BRI. Given that these
indices were not adjusted for the BMI, they could act as surrogate
measures for body size, reflecting the relationship between
mechanical loading and bone health. This observation was supported
by other studies that indicated a positive association between the
above indices and BMD (37) or a
negative association between the above indices and osteoporosis
risk (29,31,50).
Nevertheless, other studies reported contradictory results
(32,34,51).
These controversies may be explained by a nonlinear relationship
between these indices and bone health (U-shape) and sex differences
in this relationship (52). As a
result of the limited number of male subjects, a sex-based
subanalysis was not performed in the present study.
CI was positively associated with bone health in the
adjusted model. However, this association weakened after adjustment
for potential confounders. CI primarily reflects central adiposity
and, indirectly, the effects of body size and mechanical loading on
bone, thereby explaining the above positive association.
Nevertheless, this association is weak and not independent of the
covariates studied. While CI is a useful cardiometabolic risk
marker, it may not effectively predict bone health. Another study
comparing the association between various anthropometric indices
and osteoporosis risk found that CI did not perform as well as BRI
and WtHR (53).
In this research, bone health was negatively
associated with ABSI. Similar findings were obtained by previous
studies (27,28,30,34-36,54),
which reported low BMD and high osteoporosis risk. Given that the
calculation of ABSI accounts for BMI, ABSI may accurately reflect
the adiposity status independent of body size. It has been shown to
correlate with visceral adiposity without being influenced by body
weight (55). Visceral fat has a
more significant association with systemic inflammation and
metabolic dysregulation than subcutaneous fat (56). These underlying mechanisms could
explain the negative association between ABSI and bone health
observed in the present study. However, given that inflammatory
cytokine and adipokine levels were not determined in the subjects
of this research, this mechanistic explanation remains
speculative.
Several limitations should be noted before
generalising the results of the present study. The cross-sectional
nature of this work prevents causal inference between adiposity and
bone health. The subjects' recruitment from a health screening
programme is prone to suffering from selection and volunteer
biases. Therefore, the characteristics of these subjects might
differ from those of the general population. For example, the
subjects who volunteered for the present study may be more
health-conscious than the general population. Conversely, they may
have specific health concerns that motivated them to participate in
the research. The nonrandomised sampling approach also prevented
the authors from comparing the baseline characteristics of the
subjects with those of a national representative cohort, such as
the cohort included in the National Health and Morbidity Survey of
Malaysia, to verify the extent of sampling bias. The small sizes of
subgroups (based on sex, ethnicity and BMI status) also prevented
the authors from investigating the relationship between variables
in different contexts. Certain studies have demonstrated that the
association between the adiposity index and bone health can be
influenced by sex and diabetes status (28,52),
and most have revealed consistent associations (26,31,32).
A study found that the connection between adiposity and bone health
differs by sex in older adults (52). For postmenopausal women, the
relationship is U-shaped: Both very low and very high adiposity
levels are associated with poor bone health. This may be because
low body fat limits their postmenopausal oestrogen production
(57), which supports bone health,
while high body fat promotes chronic inflammation that damages
bones. For older men, the relationship is linear, meaning bone
health simply declines as adiposity increases, likely due to the
damaging effects of chronic inflammation.
Regarding the bone health assessment tool, QUS is
not the gold standard for diagnosing osteoporosis despite its
portability and safety features. Its T- and Z-scores cannot be used
interchangeably with the values generated by DXA because of
differences in reference values and technology. In the present
study, the physical activity levels of the subjects were excluded
from the analysis because the subjects had difficulty in accurately
recalling their physical activities. Bone health biochemical
markers, such as circulating vitamin D, calcium and phosphorus
levels, were not determined in this research because blood
collection was not performed in the health screening session.
Nevertheless, this work provides novel insights into the
relationship between adiposity and bone health and affirms that
ABSI could be considered as a risk factor for osteoporosis in the
general population.
In conclusion, amongst Malaysians, adiposity indices
unadjusted for body size, such as the BMI, waist circumference,
WHR, WtHR, CI and BRI, are positively associated with the bone
health index measured by QUS. By contrast, ABSI, which accounts for
body size, shows a negative association with the bone health index.
The findings of this work suggest that ABSI may be a useful marker
for identifying individuals at risk of poor bone health in the
Malaysian population. However, its critical value and clinical
effectiveness still require further substantial validation before
it can be reliably used as a routine risk assessment tool.
Supplementary Material
Changes in association between bone
health (osteoporosis index) and adiposity indices with increasing
adjustments.
Acknowledgements
The authors thank Associate Professor Bo Ma
(Department of Traditional Chinese Medicine, The First People's
Hospital of Sishui County, Jining, China) for lending the QUS bone
ultrasonometer. The authors also thank Ms. Tianru Ruan, Nanjing
Kejing Industrial Co., Ltd. (Nanjing, Jiangsu, China) for technical
support in data retrieval of QUS. The authors also thank Ms Goh Li
Lian (School of Medicine, IMU University, Bukit Jalil, Selangor,
Malaysia) for assistance in the literature search.
Funding
Funding: Universiti Kebangsaan Malaysia funded the study via the
Fundamental Research Grant (grant no. FF-2024-403).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
KYC, NM, SKW, TRJ and SA were involved in the
conceptualisation of the study and acquired funding. KYC, WjZ, YW,
XJ and YG performed data curation. KYC performed formal analysis,
project administration and supervision. WjZ, WzZ, KYC, XM, HSTS,
SOE, YW, XJ and YG performed investigations. KYC, NM, SKW, TRJ and
SA were responsible for methodology. WjZ, WzZ and XM provided
resources. WjZ, WzZ and KYC wrote the original draft. NM, SKW, TRJ
and SA reviewed and edited the manuscript. KYC and WjZ confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The Universiti Kebangsaan Malaysia Ethics Committee
approved the present study (Kuala Lumpur, Malaysia; approval no:
JEP-2024-739) and participants provided informed consent prior to
participation.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools [ChatGPT 3.0 (OpenAI)] were used to improve the
readability and language of the manuscript, and subsequently, the
authors revised and edited the content produced by the artificial
intelligence tools as necessary, taking full responsibility for the
ultimate content of the present manuscript.
References
|
1
|
Chin KY, Ng BN, Rostam MKI, Muhammad
Fadzil NFD, Raman V, Mohamed Yunus F, Syed Hashim SA and Ekeuku SO:
A mini review on osteoporosis: From biology to pharmacological
management of bone loss. J Clin Med. 11(6434)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chin KY and Ima-Nirwana S: Calcaneal
quantitative ultrasound as a determinant of bone health status:
What properties of bone does it reflect? Int J Med Sci.
10:1778–1783. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jiang Y, Wu H, Yang D, Wang W, Chu J, Tang
J and Yao X: Diagnostic value of quantitative ultrasound for
osteoporosis in elderly women: A meta-analysis. Altern Ther Health
Med. 30:226–231. 2024.PubMed/NCBI
|
|
4
|
Subramaniam S, Chan CY, Soelaiman IN,
Mohamed N, Muhammad N, Ahmad F, Ng PY, Jamil NA, Aziz NA and Chin
KY: The performance of a calcaneal quantitative ultrasound device,
CM-200, in stratifying osteoporosis risk among malaysian population
aged 40 years and above. Diagnostics (Basel).
10(178)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fu Y, Li C, Luo W, Chen Z, Liu Z and Ding
Y: Fragility fracture discriminative ability of radius quantitative
ultrasound: A systematic review and meta-analysis. Osteoporos Int.
32:23–38. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Olmos JM, Hernández JL, Pariente E,
Martínez J, Valero C and González-Macías J: Trabecular bone score
and bone quantitative ultrasound in Spanish postmenopausal women.
The Camargo Cohort Study. Maturitas. 132:24–29. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Liu Y, Huang X, Tang K, Wu J, Zhou J, Bai
H, Zhou L, Shan S, Luo Z, Cao J, et al: Prevalence of osteoporosis
and associated factors among Chinese adults: A systematic review
and modelling study. J Glob Health. 15(04009)2025.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tong X, Cui S, Shen H and Yao XI:
Developing and validating a nomogram prediction model for
osteoporosis risk in the UK biobank: A national prospective cohort.
BMC Public Health. 25(1263)2025.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Park SM, Park J, Han S, Jang HD, Hong JY,
Han K, Kim HJ and Yeom JS: Underweight and risk of fractures in
adults over 40 years using the nationwide claims database. Sci Rep.
13(8013)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ma Q, Miri Z, Haugen HJ, Moghanian A and
Loca D: Significance of mechanical loading in bone fracture
healing, bone regeneration, and vascularization. J Tissue Eng.
14(20417314231172573)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu Y, Liu Y, Huang Y, Le S, Jiang H, Ruan
B, Ao X, Shi X, Fu X and Wang S: The effect of overweight or
obesity on osteoporosis: A systematic review and meta-analysis.
Clin Nutr. 42:2457–2467. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sweatt K, Garvey WT and Martins C:
Strengths and limitations of BMI in the diagnosis of obesity: What
is the path forward? Curr Obes Rep. 13:584–595. 2024.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hou J, He C, He W, Yang M, Luo X and Li C:
Obesity and bone health: A complex link. Front Cell Dev Biol.
8(600181)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gkastaris K, Goulis DG, Potoupnis M,
Anastasilakis AD and Kapetanos G: Obesity, osteoporosis and bone
metabolism. J Musculoskelet Neuronal Interact. 20:372–381.
2020.PubMed/NCBI
|
|
15
|
Steiner BM and Berry DC: The regulation of
adipose tissue health by estrogens. Front Endocrinol (Lausanne).
13(889923)2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ravindran S, Wong SK, Mohamad NV and Chin
KY: A review of the relationship between insulin and bone health.
Biomedicines. 13(1504)2025.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Shu L, Fu Y and Sun H: The association
between common serum adipokines levels and postmenopausal
osteoporosis: A meta-analysis. J Cell Mol Med. 26:4333–4342.
2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tariq S, Tariq S, Khaliq S and Lone KP:
Serum resistin levels and related genetic variants are associated
with bone mineral density in postmenopausal women. Front Endocrinol
(Lausanne). 13(868120)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Cosme D and Gomes AC: Leptin levels and
bone mineral density: A friend or a foe for bone loss? A systematic
review of the association between leptin levels and low bone
mineral density. Int J Mol Sci. 26(2066)2025.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nevill AM, Duncan MJ and Myers T: BMI is
dead; long live waist-circumference indices: But which index should
we choose to predict cardio-metabolic risk? Nutr Metab Cardiovasc
Dis. 32:1642–1650. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cheng CH, Ho CC, Yang CF, Huang YC, Lai CH
and Liaw YP: Waist-to-hip ratio is a better anthropometric index
than body mass index for predicting the risk of type 2 diabetes in
Taiwanese population. Nutr Res. 30:585–593. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tewari A, Kumar G, Maheshwari A, Tewari V
and Tewari J: Comparative evaluation of waist-to-height ratio and
BMI in predicting adverse cardiovascular outcome in people with
diabetes: A systematic review. Cureus. 15(e38801)2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Bertoli S, Leone A, Krakauer NY, Bedogni
G, Vanzulli A, Redaelli VI, De Amicis R, Vignati L, Krakauer JC and
Battezzati A: Association of Body Shape Index (ABSI) with
cardio-metabolic risk factors: A cross-sectional study of 6081
Caucasian adults. PLoS One. 12(e0185013)2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Xu J, Zhang L, Wu Q, Zhou Y, Jin Z, Li Z
and Zhu Y: Body roundness index is a superior indicator to
associate with the cardio-metabolic risk: Evidence from a
cross-sectional study with 17,000 Eastern-China adults. BMC
Cardiovasc Disord. 21(97)2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kheirouri S and Alizadeh M: Contribution
of body adiposity index and conicity index in prediction of
metabolic syndrome risk and components. Human Nutrition &
Metabolism. 38(200290)2024.
|
|
26
|
Wu J and Wu G: Association between a body
shape index and bone mineral density in US adults based on NHANES
data. Sci Rep. 15(2817)2025.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wu M, Lu B, Wang Y, Zhang A, Zhou X, Zeng
X, Zhu Y, Chen S and Lin R: The association between A in body shape
index and total bone mineral density adults aged 20 to 59 NHANES
2011 to 2018. Medicine (Baltimore). 104(e42652)2025.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhang M, Hou Y, Ren X, Cai Y, Wang J and
Chen O: Association of a body shape index with femur bone mineral
density among older adults: NHANES 2007-2018. Arch Osteoporos.
19(63)2024.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Li H, Qiu J, Gao Z, Li C and Chu J:
Association between waist-to-height ratio and osteoporosis in the
National health and nutrition examination survey: A cross-sectional
study. Front Med (Lausanne). 11(1486611)2024.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Niu HG, Hu GK, Li T, Guo Z, Hu Y, Gong YK,
Ye GQ, Chen DJ, An JL and Gao WS: Association of a body shape index
with bone mineral density and osteoporosis among U.S. adults:
Evidence from NHANES. Calcif Tissue Int. 116(76)2025.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Zhang X, Liang J, Luo H, Zhang H, Xiang J,
Guo L and Zhu X: The association between body roundness index and
osteoporosis in American adults: Analysis from NHANES dataset.
Front Nutr. 11(1461540)2024.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ding Z, Zhuang Z, Tang R, Qu X, Huang Z,
Sun M and Yuan F: Negative association between body roundness index
and bone mineral density: Insights from NHANES. Front Nutr.
11(1448938)2024.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Deng G, Yin L, Li K, Hu B, Cheng X, Wang
L, Zhang Y, Xu L, Xu S, Zhu L, et al: Relationships between
anthropometric adiposity indexes and bone mineral density in a
cross-sectional Chinese study. Spine J. 21:332–342. 2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Zhao X, Sun J, Xin S and Zhang X:
Association between new anthropometric indices and osteoporosis in
Chinese postmenopausal women-retrospective study based on
hospitalized patients in China. Front Endocrinol (Lausanne).
16(1535540)2025.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Xiong MF, He P, Chen YH, Cao RR and Lei
SF: The effect of a body shape index (ABSI) and its interaction
with low estimated glomerular filtration rate (eGFR) on
osteoporosis in elderly Chinese. J Orthop Sci. 29:262–267.
2024.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kim B, Kim GM, Kim E, Park J, Isobe T,
Mori Y and Oh S: The anthropometric measure ‘a body shape index’
may predict the risk of osteoporosis in middle-aged and older
Korean people. Int J Environ Res Public Health.
19(4926)2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Murat S, Dogruoz Karatekin B, Demirdag F
and Kolbasi EN: Anthropometric and body composition measurements
related to osteoporosis in geriatric population. Medeni Med J.
36:294–301. 2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Abdullah JM, Ismail A and Yusoff MSB:
Healthy ageing in Malaysia by 2030: Needs, challenges and future
directions. Malays J Med Sci. 31:1–13. 2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Tee ES and Voon SH: Combating obesity in
Southeast Asia countries: Current status and the way forward. J
Glob' Health. 8:147–151. 2024.
|
|
40
|
Chan CY, Subramaniam S, Mohamed N,
Ima-Nirwana S, Muhammad N, Fairus A, Ng PY, Jamil NA, Abd Aziz N
and Chin KY: Determinants of bone health status in a multi-ethnic
population in klang valley, Malaysia. Int J Environ Res Public
Health. 17(384)2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Weir CB and Jan A: BMI Classification
Percentile And Cut Off Points. Journal 2023.
|
|
42
|
Obesity in Asia Collaboration. Is central
obesity a better discriminator of the risk of hypertension than
body mass index in ethnically diverse populations? J Hypertens.
26:169–177. 2008.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Ashwell M, Gunn P and Gibson S:
Waist-to-height ratio is a better screening tool than waist
circumference and BMI for adult cardiometabolic risk factors:
Systematic review and meta-analysis. Obes Rev. 13:275–286.
2012.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Tao L, Miao L, Guo YJ, Liu YL, Xiao LH and
Yang ZJ: Associations of body roundness index with cardiovascular
and all-cause mortality: NHANES 2001-2018. J Hum Hypertens.
38:120–127. 2024.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Martins CA, do Prado CB, Santos Ferreira
JR, Cattafesta M, Dos Santos Neto ET, Haraguchi FK, Marques-Rocha
JL and Salaroli LB: Conicity index as an indicator of abdominal
obesity in individuals with chronic kidney disease on hemodialysis.
PLoS One. 18(e0284059)2023.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Chin KY, Soelaiman IN, Mohamed IN, Ibrahim
S and Wan Ngah WZ: The effects of age, physical activity level, and
body anthropometry on calcaneal speed of sound value in men. Arch
Osteoporos. 7:135–145. 2012.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Song J, Zhang R, Lv L, Liang J, Wang W,
Liu R and Dang X: The relationship between body mass index and bone
mineral density: A mendelian randomization study. Calcif Tissue
Int. 107:440–445. 2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Kaze AD, Rosen HN and Paik JM: A
meta-analysis of the association between body mass index and risk
of vertebral fracture. Osteoporos Int. 29:31–39. 2018.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Kusuman K, Wiryadana KA, Setiawan IMB and
Rante SDT: Body mass index inversely associated with bone
microarchitecture quality: A systematic review and meta-analysis.
IJBS. 16:28–33. 2022.
|
|
50
|
Chen R, Zhao W, Cai P, Peng C and Liu H:
The association between body roundness index and risk of
osteoporosis in patients with type 2 diabetes mellitus: A
cross-sectional study based on NHANES database. J Orthop Surg (Hong
Kong). 33(10225536251356804)2025.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Tian N, Chen S, Han H, Jin J and Li Z:
Association between triglyceride glucose index and total bone
mineral density: A cross-sectional study from NHANES 2011-2018. Sci
Rep. 14(4208)2024.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Chen PJ, Lu YC, Lu SN, Liang FW and Chuang
HY: Association between osteoporosis and adiposity index reveals
nonlinearity among postmenopausal women and linearity among men
aged over 50 years. J Epidemiol Glob Health. 14:1202–1218.
2024.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Zhang J, Wang Y, Guo J, Liu H, Lei Z,
Cheng S and Cao H: The association between ten anthropometric
measures and osteoporosis and osteopenia among postmenopausal
women. Sci Rep. 15(10994)2025.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Zhao Z, Ji H, Liu W, Wang Z, Ren S, Liu C,
Wu C, Wang J and Ding X: The saturation effect of a body shape
index on lumbar bone mineral density in US adults: Findings from a
nationwide survey. PLoS One. 20(e0324160)2025.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Ryotaro B, Masahiro A, Norihiko O, Nakano
Y, Takeuchi T, Murakami M, Sasahara Y, Numasawa M, Minami I,
Izumiyama H, et al: Indirect measure of visceral adiposity ‘A Body
Shape Index’ (ABSI) is associated with arterial stiffness in
patients with type 2 diabetes. BMJ Open Diabetes Res Care.
4(e000188)2016.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Yu JY, Choi WJ, Lee HS and Lee JW:
Relationship between inflammatory markers and visceral obesity in
obese and overweight Korean adults: An observational study.
Medicine (Baltimore). 98(e14740)2019.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Hetemäki N, Savolainen-Peltonen H,
Tikkanen MJ, Wang F, Paatela H, Hämäläinen E, Turpeinen U, Haanpää
M, Vihma V and Mikkola TS: Estrogen metabolism in abdominal
subcutaneous and visceral adipose tissue in postmenopausal women. J
Clin Endocrinol Metab. 102:4588–4595. 2017.PubMed/NCBI View Article : Google Scholar
|