Introduction
Submucosal fecaliths are extremely rare, with most
previously reported cases occurring in the cecum or at the
appendiceal orifice (1), unrelated
to surgical treatment. In such cases, the formation of submucosal
fecaliths is thought to be associated with fecal material becoming
trapped at the appendiceal orifice and gradually migrating into the
submucosal layer over time (2). In
other words, submucosal mass formation due to fecalith results from
the presence of an appendiceal-like space that allows feces to
enter accompanied by chronic inflammation. Therefore, submucosal
fecalith formation in parts of the colon other than the cecum is
rare, and its occurrence at a surgical site is even more uncommon.
Furthermore, submucosal lesions are particularly difficult to
diagnose histologically via an endoscopic biopsy, making a
preoperative diagnosis challenging and often necessitating surgical
resection.
We herein report a rare case of a submucosal
fecalith mimicking a colonic submucosal tumor located at the small
intestine-transverse colon anastomosis site after right colectomy.
This report explores the potential mechanisms underlying the
formation of submucosal fecaliths at the surgical site, and
discusses the associated diagnostic challenges, comparisons with
previously reported cases, and considerations for appropriate
management.
Case report
A 70-year-old man had a history of multiple
abdominal surgeries performed in our department (Department of
Surgery, Saga University Faculty of Medicine, Saga, Japan) and had
been undergoing ongoing postoperative surveillance. He had
undergone open right colectomy for ascending colon cancer (1st
surgery, pT1bN0M0, pStage I) and laparoscopic-assisted transverse
colectomy with end-to-end ileo-transverse colon anastomosis for
transverse colon cancer located 3 cm distal to the previous
anastomosis site (2nd surgery, pT3N0M0, pStage IIa) at 51 and 58
years old, respectively.
At 68 years old, he underwent laparoscopic small
bowel resection for a submucosal tumor as his 3rd surgery and was
diagnosed with gastrointestinal stromal tumor (GIST) categorized as
low-risk based on the modified Fletcher classification. During the
examination of postoperative surveillance 12 months after the last
surgery (11 years after the 1st surgery), contrast-enhanced
computed tomography (CT) revealed a faint high-attenuation nodule
with calcification near the anastomotic site of the previous
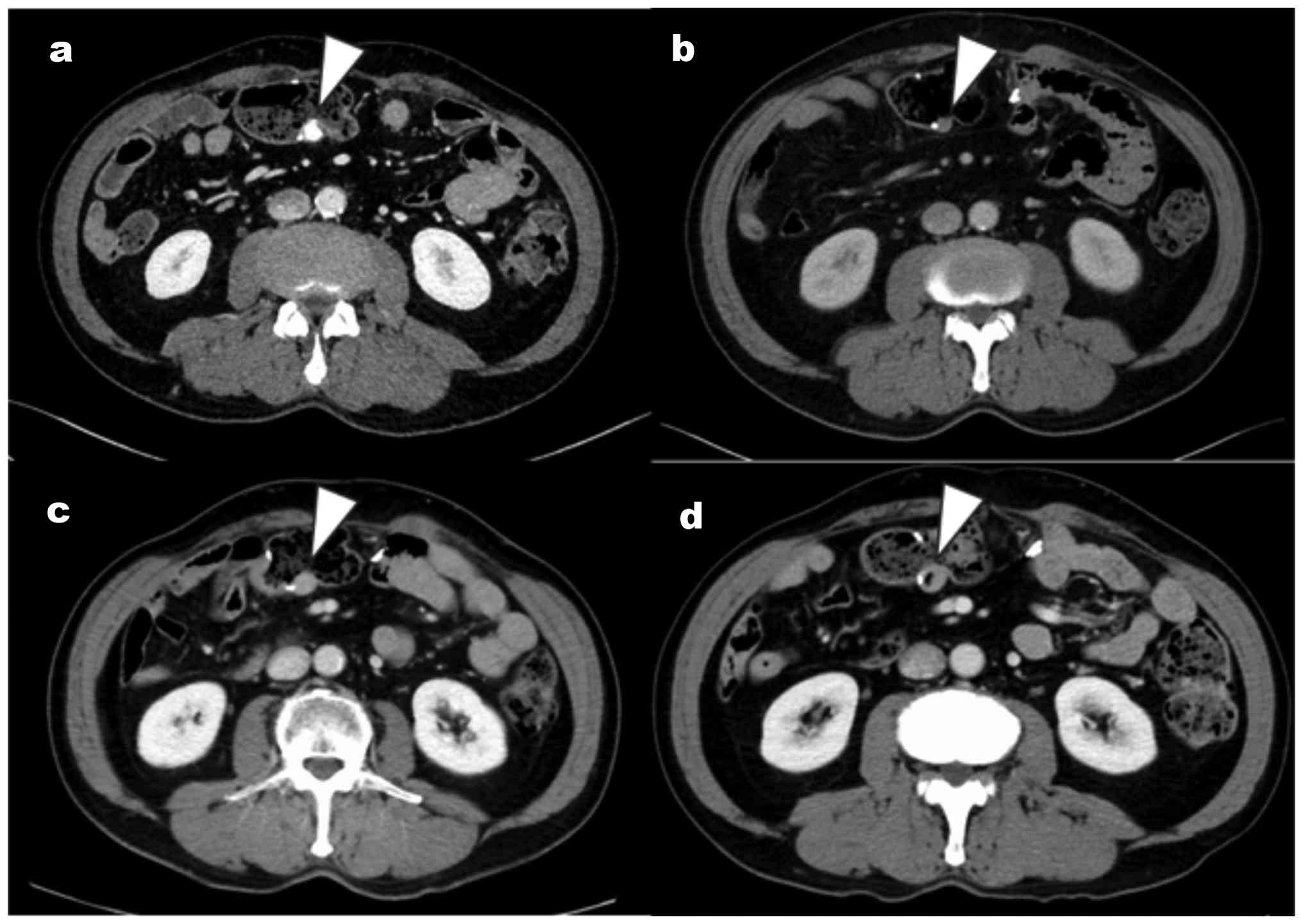
transverse colectomy (27x15x13 mm, Fig. 1A). A retrospective review of the CT
images revealed that the lesion could be identified as early as 10
years ago (1 year after the 1st surgery) (Fig. 1B) and showed a slow increase in
size over several years (Fig. 1C
and D). Blood examinations
revealed no elevation of carcinoembryonic antigen or carbohydrate
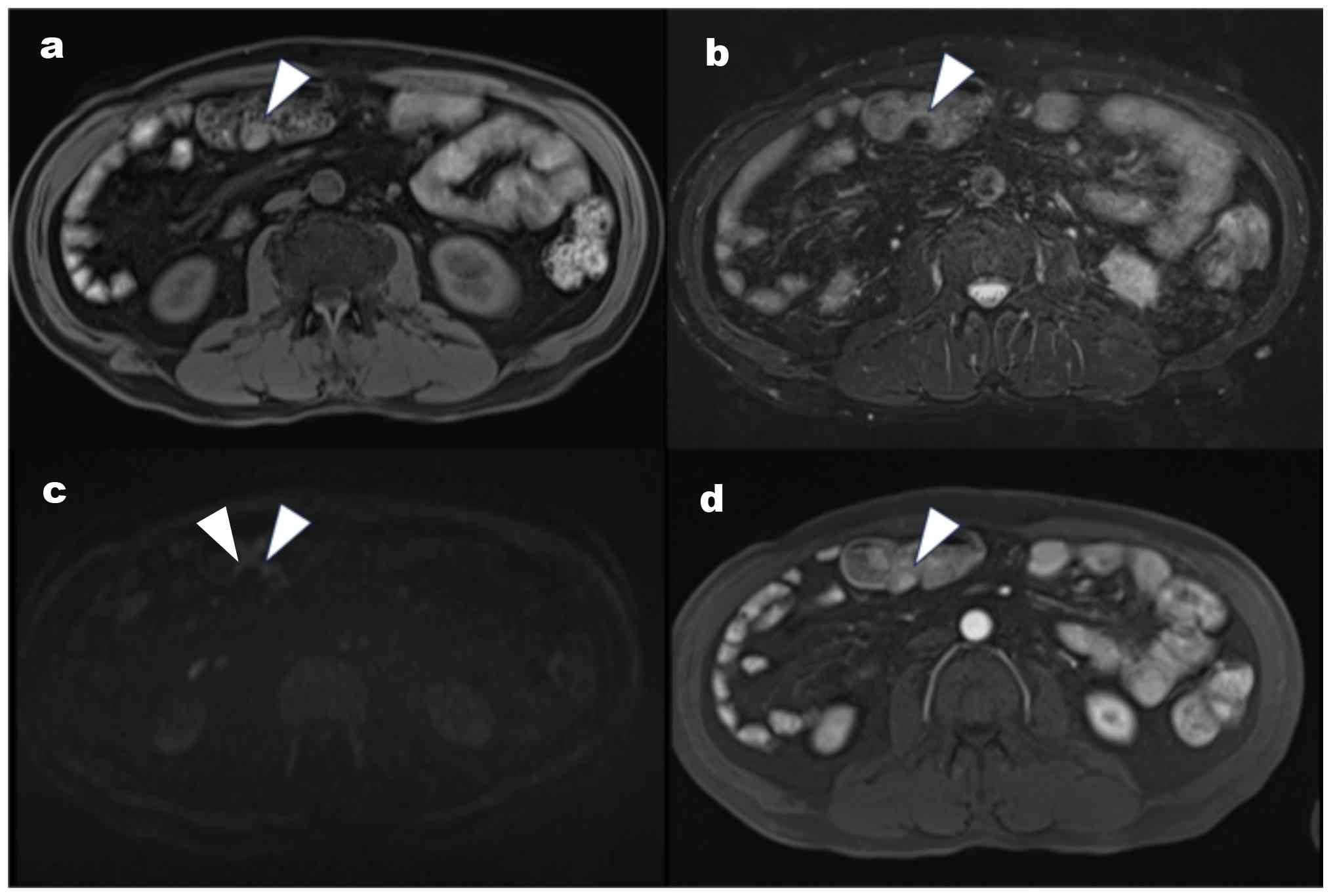
antigen. Magnetic resonance imaging (MRI) also detected a nodule at
the anastomosis site. However, the tumor showed no signal intensity
on T2-weighted imaging, without restricted diffusion on
diffusion-weighted imaging, or contrast enhancement on dynamic
imaging (Fig. 2). Furthermore,
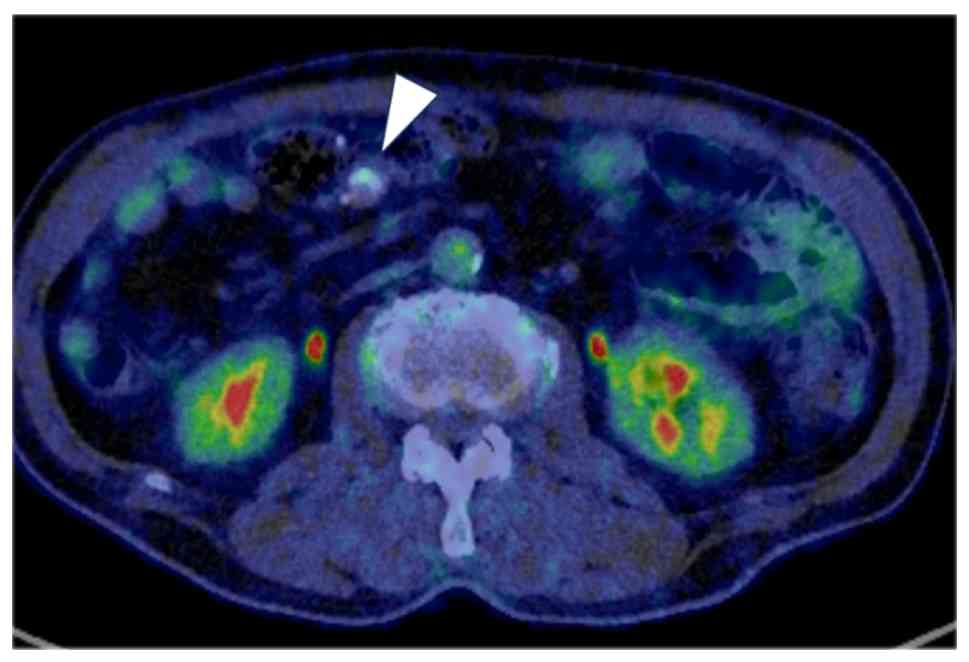
positron emission tomography (PET) demonstrated no significant
fluorodeoxyglucose uptake in the lesion (Fig. 3). Colonic endoscopy revealed no
tumors in the mucosal layer, and no tumors were detected in the
submucosal layer (Fig. 4).
Therefore, a histopathological diagnosis using endoscopic
ultrasound-guided fine needle aspiration could not be made.
Although the imaging findings suggested a low
possibility of a malignant tumor, the lesion showed gradual
enlargement with calcification and possibly mild enhancement on CT.
Thus, GIST with low-grade malignant potential was diagnosed.
Partial laparoscopic resection of the small intestine and
transverse colon including the previous anastomotic site was
performed for both diagnostic and therapeutic purposes as his 4th
surgery. During surgery, a tumorous lesion was identified at the
ileocolic anastomosis site. The lesion was dissected with the 5-cm
margin proximally and distantly, followed by reconstruction with
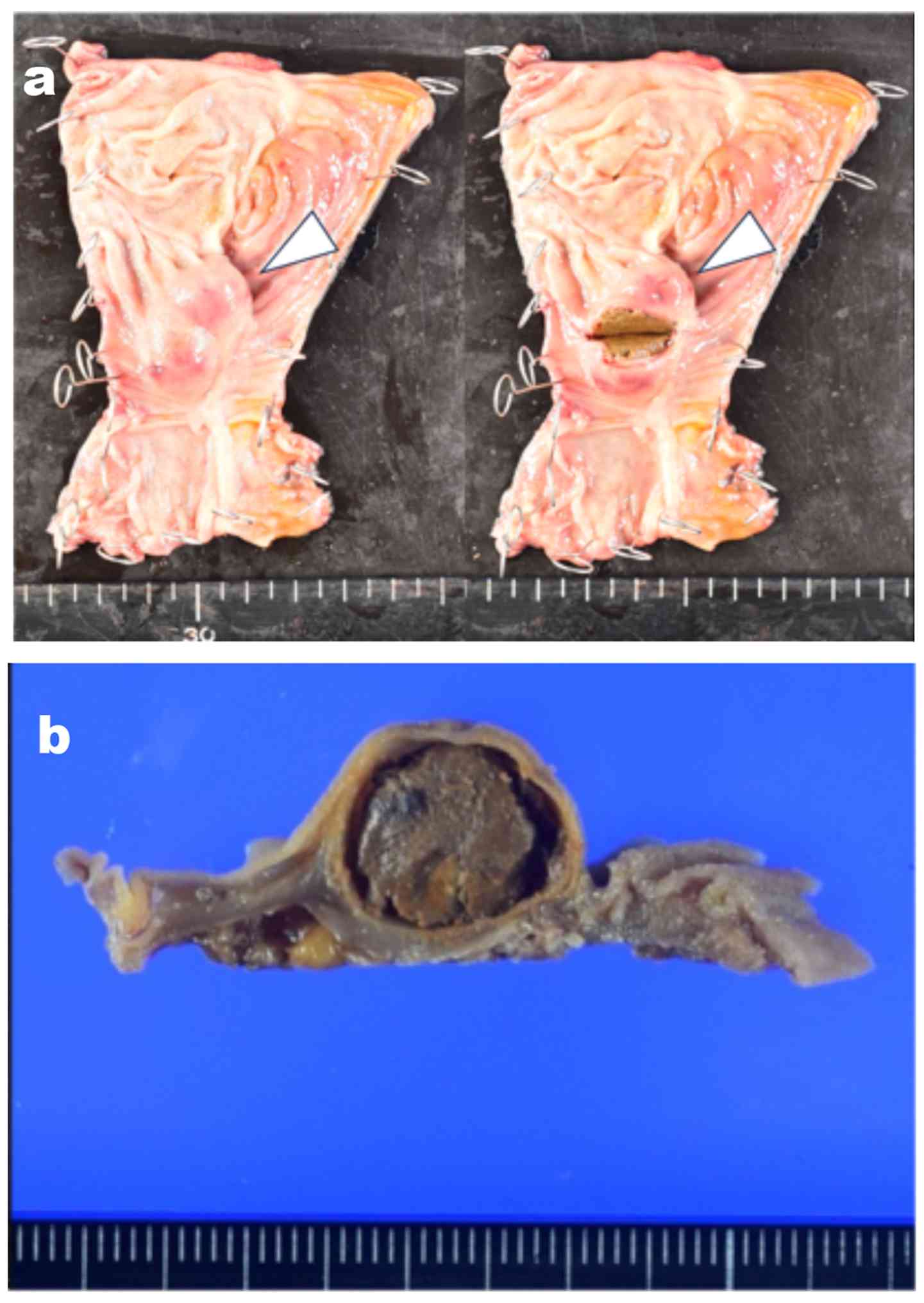
intracorporeal functional end-to-end anastomosis. Resected specimen
showed a submucosal tumor at the anastomotic site, which included
soft brownish structures inside (Fig.
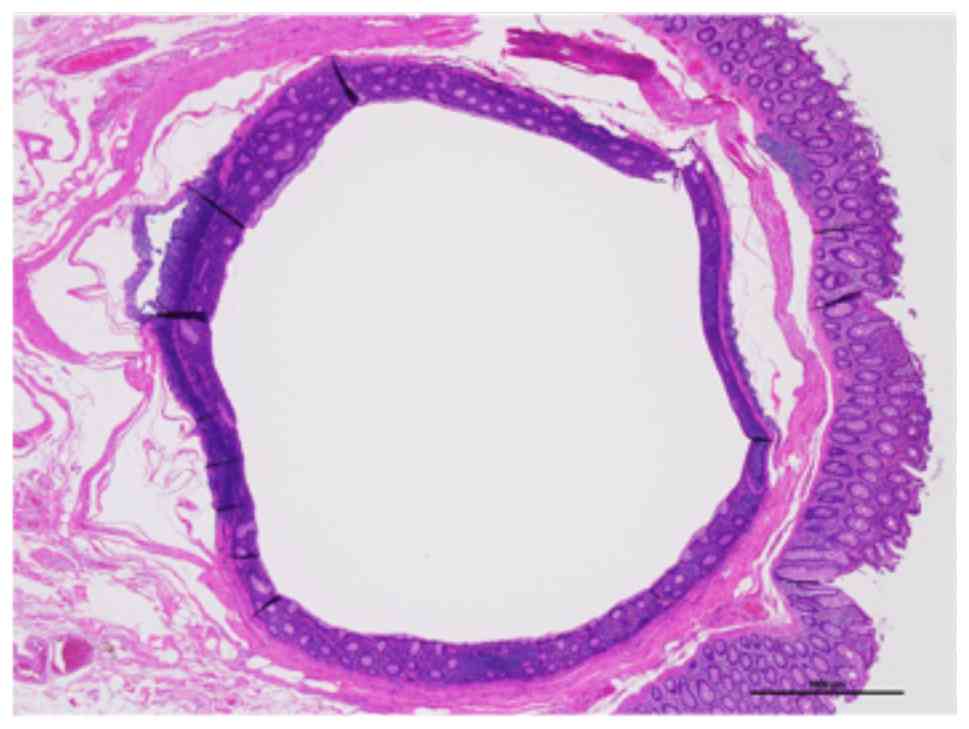
5). Tissues were fixed in 10% neutral buffered formalin at room
temperature for 48 h and sectioned at 4 µm. The tissue sections
were then stained with hematoxylin (at room temperature for 10 min)
to visualize cell nuclei, followed by counterstaining with eosin
(at room temperature for 2 min) to visualize the cytoplasm and
extracellular matrix. Observations were performed under a light
microscope. A histopathological examination revealed that the
lesion had a cystic structure filled with yellow-brown intestinal
content mixed with calcified deposits. The cystic structure was
primarily located in the submucosal layer of the colon, surrounded
by a thin layer of muscularis propria, and its lumen was lined by
non-neoplastic colonic mucosa. No clear communication was observed
between the cyst and colonic lumen (Fig. 6). Based on these findings, the
lesion was diagnosed as duplication of the bowel containing
fecaliths.
The patient was discharged from the hospital on
postoperative date eight days after surgery without any
complications. No recurrence was observed at eight months after the
last surgery.
Discussion
Submucosal fecaliths are most often reported in the
appendix or cecum, where fecal material enters an appendiceal-like
space and causes chronic inflammation that leads to fecalith
formation (1). However, their
occurrence at the surgical site after colectomy is extremely rare.
Since 2004, only five cases, including our case, have described a
fecalith presenting as a submucosal lesion at the surgical site
after colorectal surgery, as shown in Table I (3-6).
Azizi et al (3) reported a
submucosal fecal mass after the stapled hemorrhoidopexy and
speculated that it was due to the gradual penetration of the fecal
material through a non-healed staple-line. Bustamante et al
(4) reported a case of submucosal
fecalith at the cecum that was identified three years after an
appendectomy; however, the lesion was located in a mucosal fissure
near the appendiceal orifice, with no direct association with the
prior appendectomy procedure noted. Two cases were detected as
anastomotic diverticulum with a fecalith at the site of previous
colonic anastomosis (5,6). In our case, the submucosal fecalith
was located near the staple line without communication of the
intestinal lumen or existence of the mucosal fissure or
diverticular. Thus, this case was considered similar to the
Azizi s cases (3).
 | Table IReports of submucosal fecalith
presenting at the surgical site after colorectal surgery. |
Table I
Reports of submucosal fecalith
presenting at the surgical site after colorectal surgery.
| First author,
year | Age, years | Sex | Previous
operation | Initial detection
after the surgery | Maximum diameter,
mm | Location | Pre-treatment
diagnosis | Treatment | (Refs.) |
|---|
| Azizi, 2011 | 30 | F | Stapled
hemorrhoidopexy | 3 years | 40 | Rectum | N.D. | Excised | (3) |
| Bustamante, 2019 | 34 | M | Appendectomy | 3 years | 40 | Cecum | Malignancy
suspected | Right
hemicolectomy | (4) |
| Ma, 2022 | 65 | F | Partial rectal cancer
resection | 7 years | 20 | Rectum | Tumor recurrence | Endoscopic
removal | (5) |
| Li, 2024 | 45 | M | Sigmoidectomy | 3 years | N.D. | Colon | Anastomotic
diverticulum filled with fecalith | Endoscopic submucosal
resection | (6) |
| Present case | 70 | M | Transverse
colectomy | 1 year | 27 | Colon | GIST suspected | Partial resection of
the intestine | - |
However, the pathogenesis of submucosal fecalith
formation at the surgical site remains unclear. In the present
case, we speculated that a mucosal defect at the anastomotic site
during the transverse colectomy may have formed a diverticulum or
mucosal-strangled, leading to the continuous accumulation of feces
into the space of the submucosal layer. Initially, there may have
been communication between the diverticulum-like lesion and the
intestinal lumen, considering that a retrospective review of CT
scans revealed that the lesion had temporarily contained air
(Fig. 1D). However, the entrapped
feces may have been epithelialized over the long course of tissue
repair, ultimately forming a submucosal fecalith. Another
possibility is that this submucosal tumor developed because a
diverticulum located near the anastomosis site became a closed
space due to the anastomosis, and thereafter developed into a
cyst-like structure.
Regarding the treatment strategy in this case, the
tumor was reached 27 mm in diameter and showed a tendency to
increase in size. In addition, considering the patients age
and had a history of surgery for malignant abdominal diseases,
including GIST, relative surgical indications were considered. In
general, it is recommended that all stromal tumors of the large
intestine be surgically excised, regardless of their size or level
of suspicion for malignancy (7).
After obtaining sufficient informed consent, surgery was performed
for diagnosis and treatment. However, MRI and PET-CT could not
detect features suggestive of high-grade malignancy, and the
imaging pattern differed from that of the previous GIST.
Furthermore, a retrospective review of previous CT scans revealed
that the lesion had appeared shortly after transverse colectomy and
temporarily contained air. Considering these factors, if we had
been aware that a submucosal fecalith could develop at the surgical
site, then the operation might have been avoided. In addition, if a
submucosal tumor is detected, then endoscopic submucosal dissection
should also be considered in such cases. However, in this case, a
submucosal tumor was located at the anastomotic site and the
intestinal deformation likely caused by the anastomosis made
preoperative endoscopic confirmation difficult. Furthermore, only
four similar cases have so far been reported in the past (3-6),
as the result, it might be still difficult to make a diagnosis of a
submucosal colonic fecalith in such cases.
In conclusion, We encountered an extremely rare case
of a submucosal fecalith mimicking a submucosal tumor at the
anastomotic site after colon cancer. When a submucosal tumor is
suspected at the anastomotic site following colectomy, the
possibility of a submucosal fecalith should be considered.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data ana materials
The data generated in the present study may be
requested from the corresponding author.
Authors contribution
MY, MHi, ST, MHa, MN, YE, TM and HN contributed to
the diagnosis and treatment of the patient. MY, MHi and ST
contributed to the surgical treatment. MHa and MN were responsible
for the pathological diagnosis, YE contributed to the imaging
diagnosis. MY contributed to drafting the manuscript. MHi and TM
edited the manuscript. MY and MHi confirm the authenticity of all
the raw data. TM and HN supervised the patient s treatment.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for the treatment, as well
as for the publication of this case report and accompanying images,
were obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bekki T, Fukuda T, Moriuchi T, Namba Y,
Okimoto S, Mukai S, Saito Y, Oishi K, Nishida T and Ohdan H:
Appendicitis with submucosal fecalith mimicking a submucosal tumor:
A case report. Surg Case Rep. 27(105)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alhalabi SM, Alsaati G and Al-Kawas F:
Fecalith presenting as a submucosal cecal mass. Clin Gastroenterol
Hepatol. 11(A24)2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Azizi R, Sotoudehnia S, Heidari A and
Zahedi-Shoolami L: A submucosal fecal mass as the complication of
stapled hemorrhoidopexy: A case report. Int J Surg Case Rep.
2:109–110. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bustamante JP, Goñi HEB, Salas FP and
Mosco MD: Submucosal fecalith presenting as a submucosal cecal
mass. ACG Case Rep J. 6(e00182)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ma B, Wu J, Jiang L, Zhang H, Xu H and Shi
L: Anastomotic diverticulum with a fecalith after resection of
rectal cancer: A rare case. Am J Gastroenterol.
117(1735)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Li Q, Gong Z, Tang W and Hu D: An unusual
cause of protruding submucosal lesion in the colon (with video).
Gastrointest Endosc. 99:295–297. 2024.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Syllaios A, Schizas D, Davakis S, Koutras
A, Vailas M, Machairas N, Mpaili E and Felekouras E: GISTs of the
large intestine: Review of the literature. J BUON. 25:15–22.
2020.PubMed/NCBI
|