Introduction
The desire for breast-conserving surgery in patients
being treated for early breast cancer has modified the management
of these patients. With the recent widespread use of
breast-conserving surgery, assessing the extent of tumor spread has
become increasingly important (1–4). In
breast-conserving surgery, positive margins are closely related to
intramammary recurrence (5–8), but
methods of assessing resection stumps during breast-conserving
surgery have not been standardized. The present study investigated
the usefulness and pitfalls of intraoperative touch smear cytology
(touch cytology) in our department.
Patients and methods
From 2005 to 2008, a total of 420 patients underwent
breast cancer surgery. Subjects comprised 160 patients (1 man, 159
women; mean age 58.1 years; range 22–82 years) who underwent
breast-conserving surgery and touch smear cytology. Patient and
tumor characteristics are listed in Table I. Mean tumor histological size was
24.8 mm. Tumors included 7 non-invasive ductal carcinomas (4.4%),
79 papillotubular carcinomas (49.4%), 12 solid-tubular carcinomas
(7.5%), 35 scirrhous carcinomas (21.9%) and 27 special types
(16.9%). Moreover, the degree of atypia was mild [nuclear grade
(ng)1] in 70 cases (43.8%), moderate (ng2) in 50 cases (31.3%) and
severe (ng3) in 40 cases (25%).
 | Table I.Patient and tumor characteristics. |
Table I.
Patient and tumor characteristics.
| Gender | |
| Female | 159 |
| Male | 1 |
| Age (years) | |
| Range | 22–82 |
| Median | 58.1 |
| Tumor size (mm) | 24.8±7 |
| Histological type,
no. of cases (%) | |
| Non-invasive ductal
ca (1a) | 7 (4.4) |
| Papillotubular ca
(2a1) | 79 (49.4) |
| Solid-tubular ca
(2a2) | 12 (7.5) |
| Scirrhous ca
(2a3) | 35 (21.9) |
| Special type | 27 (16.9) |
| Nuclear grade, no. of
cases (%) | |
| Grade 1 | 70 (43.8) |
| Grade 2 | 50 (31.3) |
| Grade 3 | 40 (25.0) |
The method of touch cytology involved touching the
resected stump to the slide glass, then performing fixation as
promptly as possible using 95% ethanol with a prepared box.
Specimens were examined for the presence of cancer cells using
Papanicolaou stain. Additional resection was performed during the
operation, in principle, when the surgical cut end was positive. A
permanent tissue section was constructed, and the total
segmentation was cut at intervals of 5 mm. Results of touch smear
cytology were compared to those of the histological tissue
analysis. Cancer nests were defined as exposure in either direction
regardless of invasion or intraductal component with positive
margins in a permanent tissue section.
Results
Touch cytology displayed 70% sensitivity (14/20),
97.1% specificity (136/140) and a diagnostic accuracy of 93.8%
(150/160). Six false-negative cases and 4 false-positive cases were
identified (Table II). Residual
cancer cells were noted in touch cytology in 18 of the 160 cases
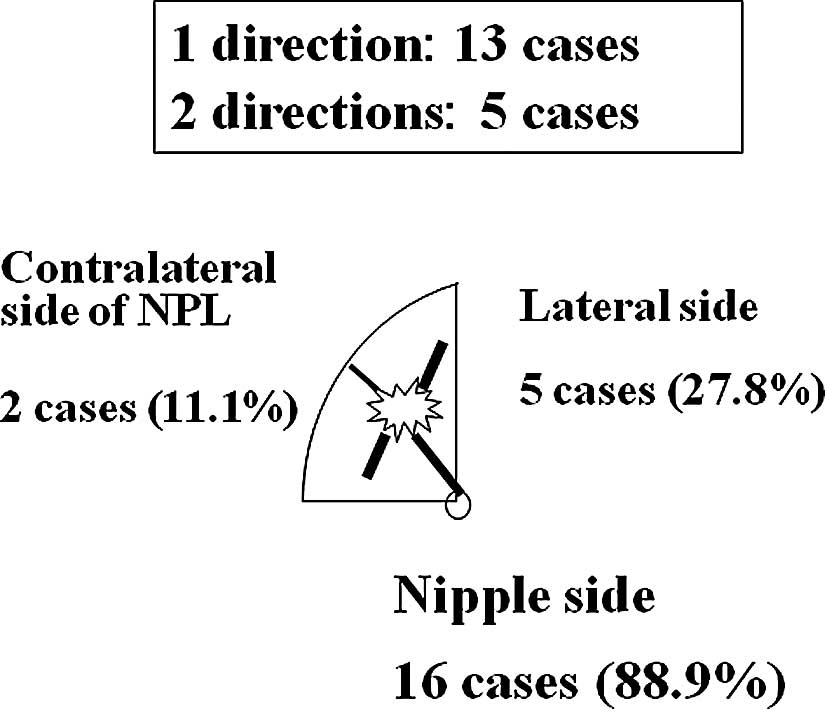
(Table III). The direction of
positive cytology was towards the nipple in 16 cases (88.9%), the
lateral tissue in 5 cases (27.8%) and the contralateral nipple in 2
cases (11.1%) (Fig. 1). Residual
cancer cells were noted in the stump in 18 cases, and additional
resection was performed on 16 cases, excluding 2 cases with few
cells showing low-level atypia.
 | Table II.Diagnostic accuracy of touch
cytology. |
Table II.
Diagnostic accuracy of touch
cytology.
| Resection stumps | Touch cytology
| Total (%) |
|---|
| Positive (%) | Negative (%) | |
|---|
| Tissue section
(permanent) |
| Positive | 14 (8.8) | 6 (3.8) | 20 (12.5) |
| Negative | 4 (2.5) | 136 (85.0) | 140 (87.5) |
| Total | 18 (11.3) | 142 (88.8) | 160 (100.0) |
 | Table III.Positive touch cytology cases
(n=18). |
Table III.
Positive touch cytology cases
(n=18).
| Case | Age (years) | Histological
type | Nuclear grade | Tumor size (mm) | Direction of positive
touch cytology | Intraoperative
treatment | Permanent
histological analysis (cancer cell + or −)
|
|---|
| (Before additional
resection) Stump | Additional resected
tissue |
|---|
| 1 | 67 | 2a3 | 2 | 26 | NPL | Additional
resection | + | − |
| 2 | 56 | 2a1 | 2 | 18 | NPL (++) | i) Additional
resection | | |
| | | | | | ii) Additional
resection | + | i) + ii) + |
| 3 | 47 | 2a1 | 2 | 11 | NPL | Additional
resection | − | − |
| 4 | 41 | 2a (mix) | 1 | 32 | NPL | Additional
resection | + | + |
| 5 | 37 | 2a1 | 2 | 0 | NPL (++) | i) Additional
resection | | |
| | | | | | ii) Additional
resection (on another day) | + | i) + ii) + |
| 6 | 51 | 2a1 | 2 | 42 | Lat | Additional
resection | − | − |
| 7 | 51 | 2a1 | 1 | 20 | NPL, Lat | Additional
resection | + | − |
| 8 | 41 | 2a1 | 2 | 15 | NPL | Additional
resection | + | − |
| 9 | 42 | 2a3 | 1 | 40 | NPL, Lat | Additional
resection | + | + |
| 10 | 35 | 2b1 | 1 | 23 | NPL, Lat | Additional
resection | + (lateral side) | − |
| 11 | 81 | 2a1 | 1 | 30 | NPL,
Contralateral | Additional
resection | + | − |
| 12 | 38 | 2b1 | 1 | 19 | NPL | Additional
resection | − | − |
| 13 | 58 | 2a1 | 1 | 16 | NPL | Additional
resection | + | + |
| 14 | 48 | 2a3 | 1 | 12 | NPL, Lat | Additional
resection | + | + |
| 15 | 71 | 2a1 | 1 | 13 | Contralateral | None | + | |
| 16 | 66 | 1a | 2 | 0 | NPL | Additional
resection | + | + |
| 17 | 59 | 2a3 | 2 | 18 | NPL | None | − | |
| 18 | 56 | 2a3 | 2 | 22 | NPL | Additional
resection | + | + |
In 4 of the 18 cases with touch cytology
margin-positive results (cases 3, 6, 12 and 17), cancer cells were
not observed in the resection stump before additional resection in
permanent tissue sections (false-positive cases). Assessing cancer
cells was very difficult, since very few cancer cells were
apparent. Cases 10 and 12 were mucinous carcinomas, and the mucin
outflow when stamping the specimen appeared to have caused the
false-positive results. The possibility of similar false-positives
must be considered even with intracystic tumors.
Cancer cells were identified histologically from 8
of the 16 cases (50%) with additionally resected tissue. In one
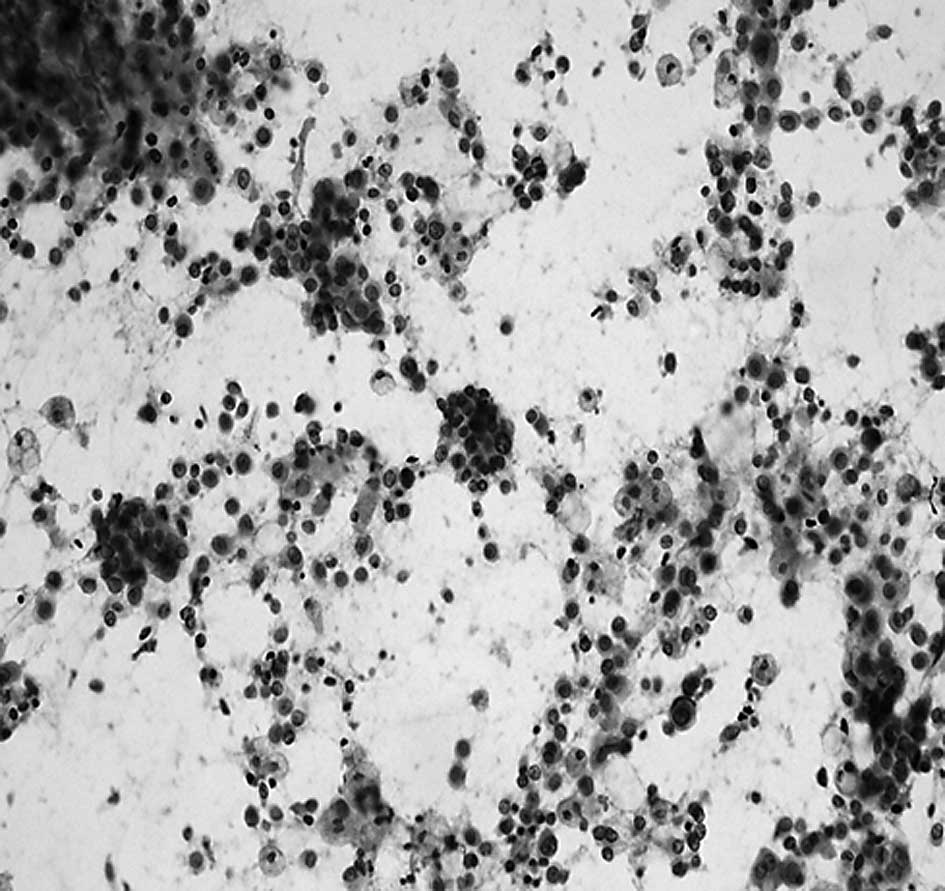
typical case, intraoperative additional resection was performed
(Table III, case 9).
Breast-conserving surgery was performed (right breast, internal
lower area). Intraoperative touch cytology towards the nipple and
lateral tissue sides was cut-end positive. Cancer cells were
observed both in the additional resection tissue and resection
stump before additional resection was performed in the permanent
tissue section. Greater cancer cell volume, as assessed by touch
smear cytology, tended to be associated with a higher frequency of
positive margins, as assessed by histological tissue analysis
(cases 2 and 5). Additional resection was performed twice in each
of these cases. A touch cytology specimen from case 2 is shown in
Fig. 3. Numerous cancer cells
showed dyshesion among cells and severe atypia in the background of
necrotic cells, and a positive margin was diagnosed. Given the
presence of a positive margin, additional resection was again
performed. In addition, the ng3 case was not included among the 18
cases with touch cytology-positive margins, suggesting that the
diagnosis of cancer by touch cytology may be possible even when a
low degree of nuclear atypia is identified.
On the other hand, 6 cases showed positive margins
in permanent tissue sections, despite no appearance of cancer cells
on touch cytology (false-negative cases). False-negative cases are
shown in Table IV.
 | Table IV.False-negative cases (n=6). |
Table IV.
False-negative cases (n=6).
| Case | Age (years) | Histological
type | Nuclear grade | Tumor size
(mm) | Direction of
positive margin, invasion or intraductal (no.) | Additional
therapy |
|---|
| 1 | 63 | 2a1 | 3 | 18 | Contralateral side
of NPL: invasion (1 piece) | Radiation |
| 2 | 39 | 2a1 | 1 | 26 | NPL side:
intraductal (1 piece) | Radiation |
| 3 | 51 | 2a1 | 3 | 11 | NPL side:
intraductal (2 pieces) | Radiation |
| 4 | 42 | 2a3 | 3 | 20 | Lateral side:
intraductal (2 pieces) | Radiation |
| | | | | Contralateral side
of NPL: intraductal (1 piece) | |
| 5 | 62 | 1a | 1 | 0 | NPL side:
intraductal (1 piece) | Radiation |
| | | | | Lateral side:
intraductal (1 piece) | |
| 6 | 60 | 2a1 | 3 | 17 | NPL side:
intraductal (1 piece) | Additional
resection + radiation |
| | | | | Lateral side:
intraductal (3 pieces) | |
Of the 6 false-negative cases, cancer cells were
noted in the ductal component in 5 cases, and the degree of cancer
cell atypia in the stump was low. Moreover, no cases with positive
margins showed lymphatic invasion.
Discussion
We previously reported that the direction of the
intraductal component was towards the nipple in 48.7%, lateral in
40.8% and towards the contralateral nipple in 28.9% (including
overlapping cases) of the cases (9). Importantly, care must be taken to
investigate, not only the nipple side, but also the lateral and
contralateral nipple sides. In the present study, the direction of
positive touch cytology was towards the nipple in 16 cases (88.9%),
lateral in 5 cases (27.8%) and towards the contralateral nipple in
2 cases (11.1%) (Fig. 1). As the
intraductal component towards the nipple side covered a long
distance, margins were considered to easily become positive in many
cases.
Histological tissue analysis and touch smear
cytology can be performed to assess resection stumps during
breast-conserving surgery. Histological tissue analysis is
accurate, but i) analyzing all areas of a large resection stump is
difficult; ii) preparing high-quality frozen sections is difficult
due to the high adipose content of breast tissue; iii) assessing
the malignancy of intraductal proliferating lesions is difficult;
and iv) regions of the tissue sample may be damaged. Touch smear
cytology is easily performed, offering a very useful technique
yielding comparable results to histological tissue analysis. In
contrast, touch smear cytology has some disadvantages. i)
Assessment is difficult in cases from which too few cells are
obtained; ii) assessing lesions showing low-grade atypia is
difficult; and iii) a special cytology screener and physician are
essential.
In many reports the result of cut end assessment
using touch cytology is identical to that of frozen tissue section,
and touch cytology offers the key advantage of providing an easy
technique (10–16).
Cut end assessment using frozen tissue sections
offers 77.3% sensitivity, 100% specificity and 95.5% accuracy
according to Cox et al (10); 68.3% sensitivity, 56% specificity
and 85.5% accuracy as reported by Morita et al (11); while 64.3% sensitivity, 100%
specificity and 92.8% accuracy were reported by Nagumo et al
(16). In the present study, the
results of cut end assessment using touch cytology showed 70–100%
sensitivity, 66.7–97.1% specificity and 86.8–97.3% accuracy
(Table V). Results for touch
cytology were equally accurate or more accurate than for frozen
tissue sections.
 | Table V.Comparison of the accuracy of
histology and cytology for assessing intraoperative resection
stumps. |
Table V.
Comparison of the accuracy of
histology and cytology for assessing intraoperative resection
stumps.
| n | No. of Stumps | Histological
analysis
| Touch cytology
|
|---|
| Sensitivity
(%) | Specificity
(%) | Accuracy (%) | Sensitivity
(%) | Specificity
(%) | Accuracy (%) |
|---|
| Cox et al
(10) | 114 | | 77.3 | 100 | 95.5 | 100 | 96.6 | 97.3 |
| Morita et al
(11) | 205 | 241 | 68.3 | 56.0 | 85.5 | | | |
| Morita et al
(11) | 58 | 66 | | | | 77.0 | 66.7 | 87.9 |
| Nagumo et al
(16) | 68 | 138 | 64.3 | 100 | 92.8 | 78.6 | 92.7 | 89.9 |
| Miyauchi et
al (12) | 114 | | | | | 87.2 | 86.6 | 86.8 |
| Kato et al
(13) | 33 | 132 | | | | 100 | 90.7 | 92.4 |
| Tohnosu et
al (14) | 50 | 200 | | | | 96.4 | 90.7 | 91.5 |
| Creager et
al (15) | 137 | 758 | | | | 75.0 | 95.5 | 94.5 |
Misdiagnosed lesions by touch cytology assessment
were reported to include i) papillary lesions, ii) lesions showing
low-grade atypia, iii) lesions showing few cells and iv) lesions
with ductal hyperplasia or ductal carcinoma in situ
(12,13).
In our examination, touch cytology assessment showed
97.1% specificity and 93.8% accuracy, representing excellent
results compared to other reports, although sensitivity was
slightly low at 70%. Causes of false-negative cases (n=6; Table IV) that contributed to the lower
sensitivity included the following. i) Sampling error:
investigation in only 1–2 directions may detect relatively few
cancer cells. ii) Staining: in cases using touch cytology specimens
stained by Papanicolaou stain after fixing in 95% ethanol,
sensitivity is slightly low and specificity is high (17). That is, cells flake off easily in
cases with fixation in ethanol. However, dry fixations, such as
other Diff-Quick methods and Giemsa staining, are unsuitable for
detailed observation of heavy cell populations and are a ready
cause of misdiagnosis. iii) Underestimation: in case 5 (Table IV) intraoperative touch cytology
assessment was cut end-negative since the few cells present showed
monotonous nuclei with little atypia.
The examination of cut ends requires the use of
information from touch cytology (cellularity and cell atypia) and
considering likely histological types, but without strict
intra-operative judgment of the cut end.
Some key points must be considered in touch cytology
examination (16). First, after
removing blood with gauze, the resection stumps must be touched
slightly onto the slide glass (when stumps are touched too firmly,
intraductal lesions may be pushed out, causing false-positive
results). Second, cytology specimens must be fixed in 95% ethanol
immediately, without allowing time for drying. Third, degenerative
cells must not be misdiagnosed. Fourth, when touch cytology
diagnosis (i.e., benign vs. malignant) is difficult to assess, a
comparison to a pre-operative aspiration cytology specimen is
useful. Finally, a cytologist must collaborate on the diagnosis
with a surgeon.
In our hospital, in all cases irradiation to the
remaining breast is performed in principle after breast-conserving
surgery. Ipsilateral breast recurrence was not identified in any of
the cases (160 samples), although surveillance was only continued
for a relatively short period. Takahashi et al reported that
when cancer cells include only an intraductal component or are
noted in only one direction or in only one specimen, the recurrence
rate is low in the ipsilateral breast without postoperative
irradiation (17). Only 1 case
with 4 slices showing cut end-positive results on permanent tissue
section required additional resection at a later date among the 6
false-negative cases. Strict follow-up is required.
Cut ends are often difficult to assess even in
permanent tissue sections since extreme intraductal component
atypia is low. Detailed cut end evaluation with a permanent tissue
section appears to allow accurate and efficient diagnosis after
initial intraoperative touch cytology to provide prompt, easy and
accurate diagnosis.
References
|
1.
|
Fisher B, Redmond C, Poisson R, et al:
Eight-year results of a randomized clinical trials comparing total
mastectomy and lumpectomy with and without radiation on the
treatment of breast cancer. N Engl J Med. 320:822–828. 1989.
|
|
2.
|
Polednak AP: Trends in breast-conserving
surgery in Connecticut: no effect of negative publicity. Conn Med.
60:527–530. 1996.PubMed/NCBI
|
|
3.
|
Kotwall CA, Covington DL, Rutledge R, et
al: Patient, hospital, and surgeon factors associated with breast
conservation surgery: a statewide analysis in North Carolina. Ann
Surg. 224:419–429. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Voogd AC, Nab HW, Crommelin MA, et al:
Comparison of breast-conserving therapy with mastectomy for the
treatment of early breast cancer in community hospitals. Eur J Surg
Oncol. 22:13–16. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Park CC, Mitsumori M, Nixon A, et al:
Outcome at 8 years after breast-conserving surgery and radiation
therapy for invasive breast cancer: influence of margin status and
systemic therapy on local recurrence. J Clin Oncol. 18:1668–1675.
2000.PubMed/NCBI
|
|
6.
|
Anscher MS, Jones P, Prosnitz LR, et al:
Local failure and margin status in early-stage carcinoma treated
with conservation surgery and radiation therapy. Ann Surg.
218:22–28. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Kurtz JM, Jacquemier J, Amalric R, et al:
Why are local recurrences after breast-conserving therapy more
frequent in younger patients? J Clin Oncol. 8:591–598.
1990.PubMed/NCBI
|
|
8.
|
Nixon AJ, Schnitt SJ, Gelman R, et al:
Relationship of tumor grade to other pathologic features and to
treatment outcome of patients with early stage breast carcinoma
treated with breast-conserving therapy. Cancer. 78:1426–1431. 1996.
View Article : Google Scholar
|
|
9.
|
Sumiyoshi K, Kani H, Nohara T, et al: A
comparison study between multidetector-row CT and histopathological
findings in terms of the extension diagnosis of breast cancer. J
Jpn Surg Assoc. 67:1463–1472. 2006. View Article : Google Scholar
|
|
10.
|
Cox CE, Ku NN, Reintgen DS, Greenberg HM,
Nicosia SV and Wangensteen S: Touch preparation cytology of breast
lumpectomy margins with histologic correlation. Arch Surg.
126:490–493. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Morita T, Shin E, Takatsuka Y, et al:
Significance of intraoperative pathologic consultation in
breast-conserving surgery. Jap J Breast Cancer. 12:673–678.
1997.
|
|
12.
|
Miyauchi M, Yamamoto N, Fujita Y, et al:
Clinical significance of rapid imprint cytology to ensure the
cancer free margin in breast conservative surgery. Jpn J Breast
Cancer. 9:1293–1297. 1994.
|
|
13.
|
Kato T, Takahashi H, Ando T, et al:
Intraoperative rapid imprint cytologic examination of surgical
margin in breast cancer conserving surgery. J Jpn Soc Clin Cytol.
36:119–123. 1997. View Article : Google Scholar
|
|
14.
|
Tohnosu N, Nabeya Y, Matsuda M, et al:
Rapid intraoperative scrape cytology assessment of surgical margins
in breast conservation surgery. Breast Cancer. 5:165–169. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Creager AJ, Shaw JA, Young PR and
Geisinger KR: Intraoperative evaluation of lumpectomy margins by
imprint cytology with histologic correlation: a community hospital
experience. Arch Pathol Lab Med. 126:846–848. 2002.
|
|
16.
|
Nagumo S, Motomura K, Kasugai T, Inaji H
and Koyama H: Intraoperative cytological examination: diagnosis of
surgical margins and sentinel nodes in breast cancer. Jpn J Breast
Cancer. 18:16–23. 2003.
|
|
17.
|
Takahashi K, Akiyama F, Yamashita T and
Sakamoto G: Role of radiation therapy in breast conserving therapy
in relation to the surgical margin status. Jpn J Breast Cancer.
21:435–441. 2006.
|