|
1
|
Richter L, Black M, Britto P, Daelmans B,
Desmond C, Devercelli A, Dua T, Fink G, Heymann J, Lombardi J, et
al: Early childhood development: An imperative for action and
measurement at scale. BMJ Global Health. 4 (Suppl
4)(e001302)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ferrante G, Fasola S, Cilluffo G,
Piacentini G, Viegi G and La Grutta S: Addressing Exposome: An
innovative approach to environmental determinants in pediatric
respiratory health. Front Public Health. 10(871140)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fenga C: Gut microbiota modulation: A
tailored approach for the prevention of chronic diseases. Biomed
Rep. 16(23)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Abeysinghe P, Turner N, Morean Garcia I,
Mosaad E, Peiris HN and Mitchell MD: The role of exosomal
epigenetic modifiers in cell communication and fertility of dairy
cows. Int J Mol Sci. 21(9106)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhang B, Zhao J, Jiang M, Peng D, Dou X,
Song Y and Shi J: The potential role of gut microbial-derived
exosomes in metabolic-associated fatty liver disease: Implications
for treatment. Front Immunol. 13(893617)2022.PubMed/NCBI View Article : Google Scholar
|
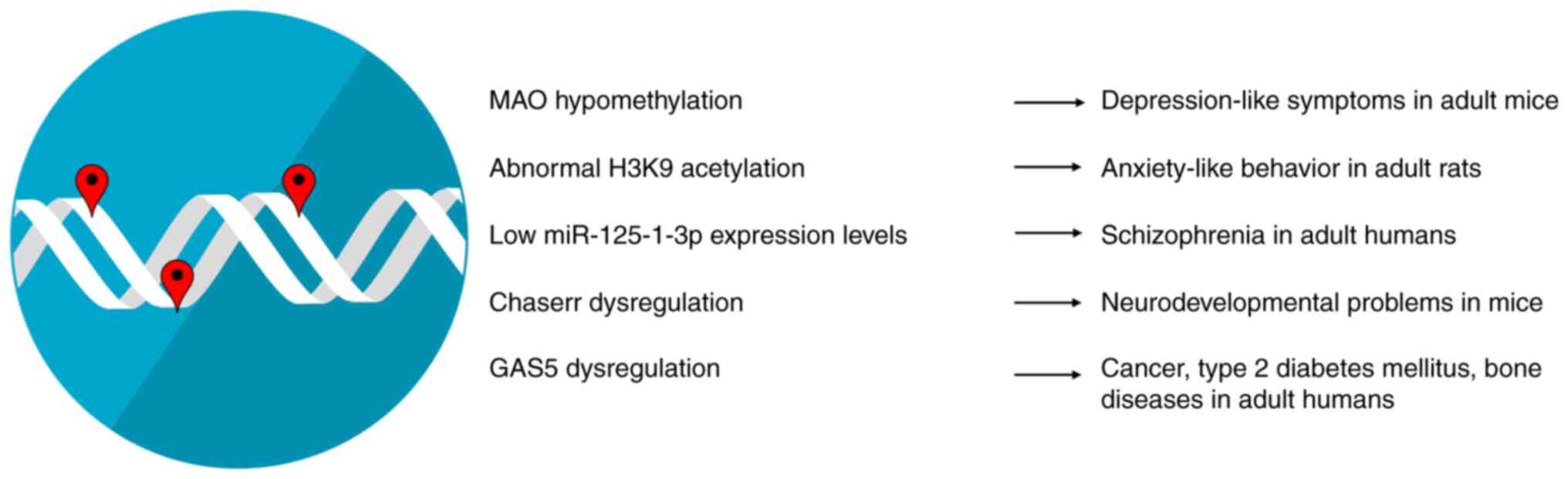
|
6
|
Galley JD and Besner GE: The therapeutic
potential of breast milk-derived extracellular vesicles. Nutrients.
12(745)2020.PubMed/NCBI View Article : Google Scholar
|
|
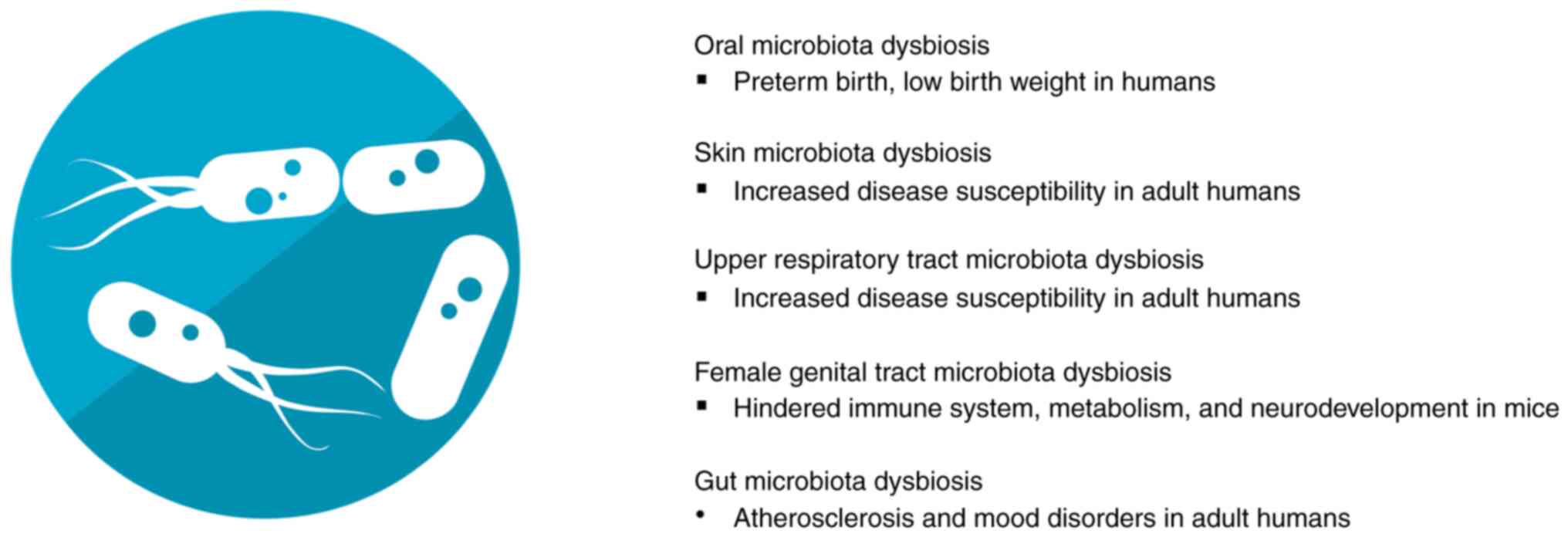
7
|
Wang DR and Pan J: Extracellular vesicles:
Emerged as a promising strategy for regenerative medicine. World J
Stem Cells. 15:165–181. 2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Doyle LM and Wang MZ: Overview of
extracellular vesicles, their origin, composition, purpose, and
methods for exosome isolation and analysis. Cells.
8(727)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kumar MA, Baba SK, Sadida HQ, Marzooqi SA,
Jerobin J, Altemani FH, Algehainy N, Alanazi MA, Abou-Samra AB,
Kumar R, et al: Extracellular vesicles as tools and targets in
therapy for diseases. Signal Transduct Target Ther.
9(27)2024.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mobarak H, Javid F, Narmi MT, Mardi N,
Sadeghsoltani F, Khanicheragh P, Narimani S, Mahdipour M, Sokullu
E, Valioglu F and Rahbarghazi R: Prokaryotic microvesicles Ortholog
of eukaryotic extracellular vesicles in biomedical fields. Cell
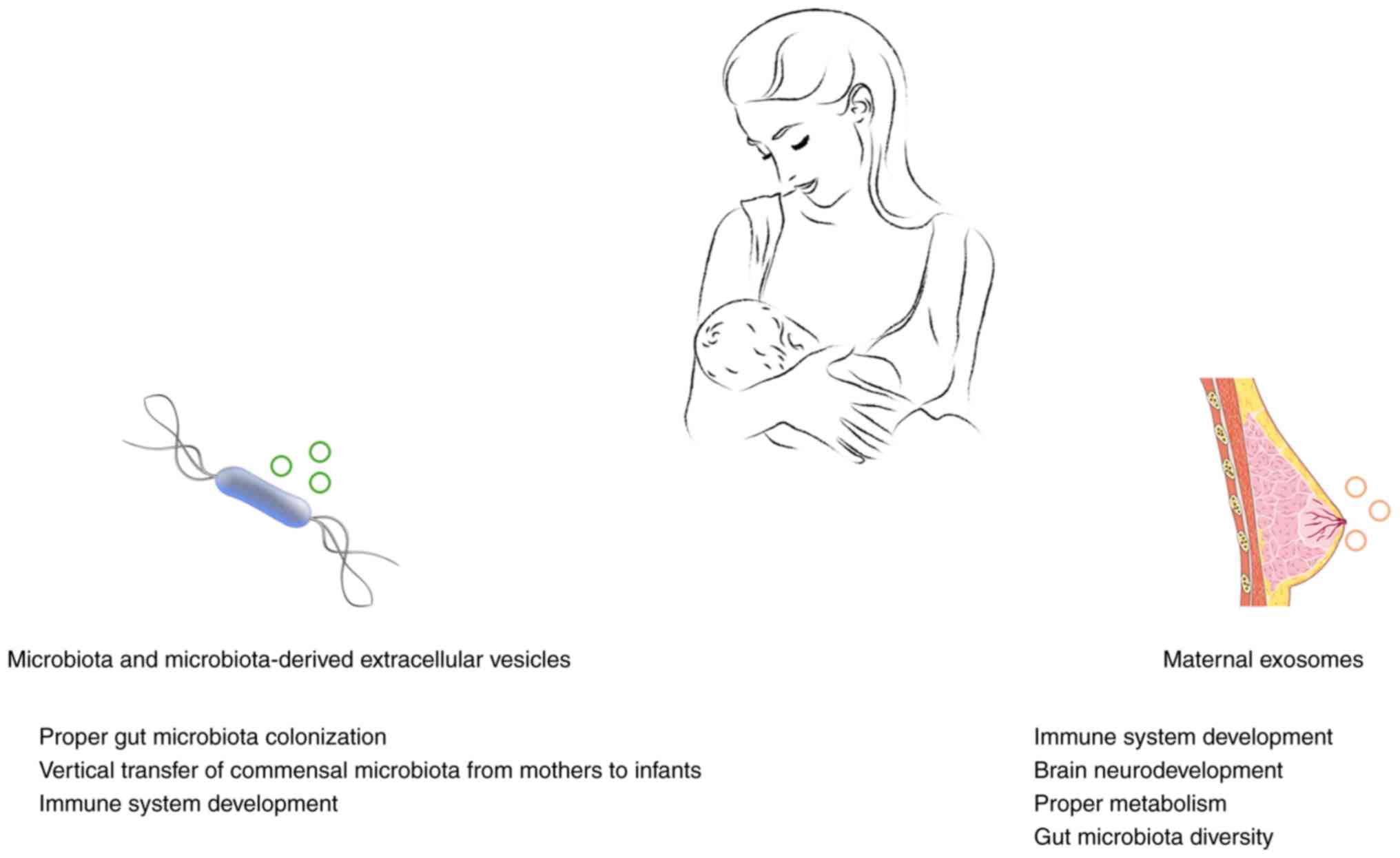
Commun Signal. 22(80)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liu J, Cvirkaite-Krupovic V, Commere PH,
Yang Y, Zhou F, Forterre P, Shen Y and Krupovic M: Archaeal
extracellular vesicles are produced in an ESCRT-dependent manner
and promote gene transfer and nutrient cycling in extreme
environments. ISME J. 15:2892–2905. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sheta M, Taha EA, Lu Y and Eguchi T:
Extracellular vesicles: New classification and tumor
immunosuppression. Biology (Basel). 12(110)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhang Y, Bi J, Huang J, Tang Y, Du S and
Li P: Exosome: A review of its classification, isolation
techniques, storage, diagnostic and targeted therapy applications.
Int J Nanomedicine. 15:6917–6934. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Duréndez-Sáez E, Calabuig-Fariñas S,
Torres-Martínez S, Moreno-Manuel A, Herreros-Pomares A, Escorihuela
E, Mosqueda M, Gallach S, Guijarro R, Serna E, et al: Analysis of
exosomal cargo provides accurate clinical, histologic and
mutational information in non-small cell lung cancer. Cancers
(Basel). 14(3216)2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dimik M, Abeysinghe P, Logan J and
Mitchell M: The exosome: A review of current therapeutic roles and
capabilities in human reproduction. Drug Deliv Transl Res.
13:473–502. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Dilsiz N: Hallmarks of exosomes. Future
Sci OA. 8(FSO764)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhang Y, Dou Y, Liu Y, Di M, Bian H, Sun X
and Yang Q: Advances in therapeutic applications of extracellular
vesicles. Int J Nanomedicine. 18:3285–3307. 2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Schiller EA, Cohen K, Lin X, El-Khawam R
and Hanna N: Extracellular Vesicle-microRNAs as diagnostic
biomarkers in preterm neonates. Int J Mol Sci.
24(2622)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lak NSM, van der Kooi EJ, Enciso-Martinez
A, Lozano-Andrés E, Otto C, Wauben MHM and Tytgat GAM:
Extracellular vesicles: A new source of biomarkers in pediatric
solid tumors? A systematic review. Front Oncol.
12(887210)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Galardi A, Colletti M, Di Paolo V, Vitullo
P, Antonetti L, Russo I and Di Giannatale A: Exosomal MiRNAs in
pediatric cancers. Int J Mol Sci. 20(4600)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chaubey S, Thueson S, Ponnalagu D, Alam
MA, Gheorghe CP, Aghai Z, Singh H and Bhandari V: Early gestational
mesenchymal stem cell secretome attenuates experimental
bronchopulmonary dysplasia in part via exosome-associated factor
TSG-6. Stem Cell Res Ther. 9(173)2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Braun RK, Chetty C, Balasubramaniam V,
Centanni R, Haraldsdottir K, Hematti P and Eldridge MW:
Intraperitoneal injection of MSC-derived exosomes prevent
experimental bronchopulmonary dysplasia. Biochem Biophys Res
Commun. 503:2653–2658. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cavalli G and Heard E: Advances in
epigenetics link genetics to the environment and disease. Nature.
571:489–499. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bertogliat MJ, Morris-Blanco KC and
Vemuganti R: Epigenetic mechanisms of neurodegenerative diseases
and acute brain injury. Neurochem Int. 133(104642)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liang M: Epigenetic mechanisms and
hypertension. Hypertension. 72:1244–1254. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Nasrullah Hussain A, Ahmed S, Rasool M and
Shah AJ: DNA methylation across the tree of life, from micro to
macro-organism. Bioengineered. 13:1666–1685. 2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Shi J, Xu J, Chen YE, Li JS, Cui Y, Shen
L, Li JJ and Li W: The concurrence of DNA methylation and
demethylation is associated with transcription regulation. Nat
Commun. 12(5285)2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Uddin MG and Fandy TE: DNA methylation
inhibitors: Retrospective and perspective view. Adv Cancer Res.
152:205–223. 2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sallustio F, Gesualdo L and Gallone A: New
findings showing how DNA methylation influences diseases. World J
Biol Chem. 10:1–6. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Tompkins JD: Discovering DNA methylation,
the history and future of the writing on DNA. J Hist Biol.
55:865–887. 2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Alaskhar Alhamwe B, Khalaila R, Wolf J,
von Bülow V, Harb H, Alhamdan F, Hii CS, Prescott SL, Ferrante A,
Renz H, et al: Histone modifications and their role in epigenetics
of atopy and allergic diseases. Allergy Asthma Clin Immunol.
14(39)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Lee HT, Oh S, Ro DH, Yoo H and Kwon YW:
The Key Role of DNA Methylation and histone acetylation in
epigenetics of atherosclerosis. J Lipid Atheroscler. 9:419–434.
2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Liu R, Wu J, Guo H, Yao W, Li S, Lu Y, Jia
Y, Liang X, Tang J and Zhang H: Post-translational modifications of
histones: Mechanisms, biological functions, and therapeutic
targets. MedComm (2020). 4(e292)2023.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Zhang SF, Gao J and Liu CM: The role of
non-coding RNAs in neurodevelopmental disorders. Front Genet.
10(1033)2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Ratti M, Lampis A, Ghidini M, Salati M,
Mirchev MB, Valeri N and Hahne JC: MicroRNAs (miRNAs) and Long
Non-Coding RNAs (lncRNAs) as new tools for cancer therapy: First
steps from bench to bedside. Target Oncol. 15:261–278.
2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Jorge AL, Pereira ER, Oliveira CS,
Ferreira EDS, Menon ETN, Diniz SN and Pezuk JA: MicroRNAs:
Understanding their role in gene expression and cancer. Einstein
(Sao Paulo). 19(eRB5996)2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Borkiewicz L, Kalafut J, Dudziak K,
Przybyszewska-Podstawka A and Telejko I: Decoding LncRNAs. Cancers
(Basel). 13(2643)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Li S, Ye Z, Mather KA, Nguyen TL, Dite GS,
Armstrong NJ, Wong EM, Thalamuthu A, Giles GG, Craig JM, et al:
Early life affects late-life health through determining DNA
methylation across the lifespan: A twin study. EBioMedicine.
77(103927)2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Schrott R, Song A and Ladd-Acosta C:
Epigenetics as a biomarker for early-life environmental exposure.
Curr Environ Health Rep. 9:604–624. 2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Xu Q, Jiang M, Gu S, Wang F and Yuan B:
Early life stress induced DNA methylation of monoamine oxidases
leads to depressive-like behavior. Front Cell Dev Biol.
8(582247)2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Park J, Lee K, Kim K and Yi SJ: The role
of histone modifications: From neurodevelopment to neurodiseases.
Signal Transduct Target Ther. 7(217)2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Guan L, Shi X, Tang Y, Yan Y, Chen L, Chen
Y, Gao G, Lin C and Chen A: Contribution of amygdala histone
acetylation in early life stress-induced visceral hypersensitivity
and emotional comorbidity. Front Neurosci.
16(843396)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Allen L and Dwivedi Y: MicroRNA mediators
of early life stress vulnerability to depression and suicidal
behavior. Mol Psychiatry. 25:308–320. 2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Tsagakis I, Douka K, Birds I and Aspden
JL: Long non-coding RNAs in development and disease: Conservation
to mechanisms. J Pathol. 250:480–495. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Rom A, Melamed L, Gil N, Goldrich MJ,
Kadir R, Golan M, Biton I, Perry RB and Ulitsky I: Regulation of
CHD2 expression by the Chaserr long noncoding RNA gene is essential
for viability. Nat Commun. 10(5092)2019.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Caldwell KK, Hafez A, Solomon E,
Cunningham M and Allan AM: Arsenic exposure during embryonic
development alters the expression of the long noncoding RNA growth
arrest specific-5 (Gas5) in a sex-dependent manner. Neurotoxicol
Teratol. 66:102–112. 2018.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Zhou Z, Chen J, Huang Y, Liu D, Chen S and
Qin S: Long Noncoding RNA GAS5: A new factor involved in bone
diseases. Front Cell Dev Biol. 9(807419)2022.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Hou K, Wu ZX, Chen XY, Wang JQ, Zhang D,
Xiao C, Zhu D, Koya JB, Wei L, Li J and Chen ZS: Microbiota in
health and diseases. Signal Transduct Target Ther.
7(135)2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Afzaal M, Saeed F, Shah YA, Hussain M,
Rabail R, Socol CT, Hassoun A, Pateiro M, Lorenzo JM, Rusu AV and
Aadil RM: Human gut microbiota in health and disease: Unveiling the
relationship. Front Microbiol. 13(999001)2022.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Peng X, Cheng L, You Y, Tang C, Ren B, Li
Y, Xu X and Zhou X: Oral microbiota in human systematic diseases.
Int J Oral Sci. 14(14)2022.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Skowron K, Bauza-Kaszewska J, Kraszewska
Z, Wiktorczyk-Kapischke N, Grudlewska-Buda K, Kwiecińska-Piróg J,
Wałecka-Zacharska E, Radtke L and Gospodarek-Komkowska E: Human
skin microbiome: Impact of intrinsic and extrinsic factors on skin
microbiota. Microorganisms. 9(543)2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Man WH, de Steenhuijsen Piters WA and
Bogaert D: The microbiota of the respiratory tract: Gatekeeper to
respiratory health. Nat Rev Microbiol. 15:259–270. 2017.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Cocomazzi G, De Stefani S, Del Pup L,
Palini S, Buccheri M, Primiterra M, Sciannamè N, Faioli R, Maglione
A, Baldini GM, et al: The impact of the female genital microbiota
on the outcome of assisted reproduction treatments. Microorganisms.
11(1443)2023.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Al Bander Z, Nitert MD, Mousa A and
Naderpoor N: The gut microbiota and inflammation: An overview. Int
J Environ Res Public Health. 17(7618)2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Ferraris C, Elli M and Tagliabue A: Gut
microbiota for health: How can diet maintain a healthy Gut
Microbiota? Nutrients. 12(3596)2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Chen Y, Zhou J and Wang L: Role and
mechanism of gut microbiota in human disease. Front Cell Infect
Microbiol. 11(625913)2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Russo M, Calevo MG, D'Alessandro G,
Tantari M, Migliorati M, Piccardo I, Perucchin PP and Arioni C:
Influence of maternal oral microbiome on newborn oral microbiome in
healthy pregnancies. Ital J Pediatr. 49(140)2023.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Dhariwala MO and Scharschmidt TC: Baby's
skin bacteria: First impressions are long-lasting. Trends Immunol.
42:1088–1099. 2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Jašarević E, Hill EM, Kane PJ, Rutt L,
Gyles T, Folts L, Rock KD, Howard CD, Morrison KE, Ravel J and Bale
TL: The composition of human vaginal microbiota transferred at
birth affects offspring health in a mouse model. Nat Commun.
12(6289)2021.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Zhuang L, Chen H, Zhang S, Zhuang J, Li Q
and Feng Z: Intestinal microbiota in early life and its
implications on childhood health. Genomics Proteomics
Bioinformatics. 17:13–25. 2019.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Niu J, Xu L, Qian Y, Sun Z, Yu D, Huang J,
Zhou X, Wang Y, Zhang T, Ren R, et al: Evolution of the gut
microbiome in early childhood: A cross-sectional study of Chinese
children. Front Microbiol. 11(439)2020.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Sarkar A, Yoo JY, Valeria Ozorio Dutra S,
Morgan KH and Groer M: The Association between early-life gut
microbiota and long-term health and diseases. J Clin Med.
10(459)2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Coley EJL, Mayer EA, Osadchiy V, Chen Z,
Subramanyam V, Zhang Y, Hsiao EY, Gao K, Bhatt R, Dong T, et al:
Early life adversity predicts brain-gut alterations associated with
increased stress and mood. Neurobiol Stress.
15(100348)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Erabi H, Okada G, Shibasaki C, Setoyama D,
Kang D, Takamura M, Yoshino A, Fuchikami M, Kurata A, Kato TA, et
al: Kynurenic acid is a potential overlapped biomarker between
diagnosis and treatment response for depression from metabolome
analysis. Sci Rep. 10(16822)2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Li B, Guo K, Zeng L, Zeng B, Huo R, Luo Y,
Wang H, Dong M, Zheng P, Zhou C, et al: Metabolite identification
in fecal microbiota transplantation mouse livers and combined
proteomics with chronic unpredictive mild stress mouse livers.
Transl Psychiatry. 8(34)2018.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Behr C, Kamp H, Fabian E, Krennrich G,
Mellert W, Peter E, Strauss V, Walk T, Rietjens IMCM and van
Ravenzwaay B: Gut microbiome-related metabolic changes in plasma of
antibiotic-treated rats. Arch Toxicol. 91:3439–3454.
2017.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Padmasekar M, Savai R, Seeger W and
Pullamsetti SS: Exposomes to exosomes: Exosomes as tools to study
epigenetic adaptive mechanisms in high-altitude humans. Int J
Environ Res Public Health. 18(8280)2021.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Fischer J, Koch L, Emmerling C, Vierkotten
J, Peters T, Brüning JC and Rüther U: Inactivation of the Fto gene
protects from obesity. Nature. 458:894–898. 2009.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Sachse G, Church C, Stewart M, Cater H,
Teboul L, Cox RD and Ashcroft FM: FTO demethylase activity is
essential for normal bone growth and bone mineralization in mice.
Biochim Biophys Acta Mol Basis Dis. 1864:843–850. 2018.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Melnik BC and Schmitz G: Milk's role as an
epigenetic regulator in health and disease. Diseases.
5(12)2017.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Zhang L, Lin TV, Yuan Q, Sadoul R, Lam TT
and Bordey A: Small extracellular vesicles control dendritic spine
development through regulation of HDAC2 signaling. J Neurosci.
41:3799–3807. 2021.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Schwarzenbach H and Gahan PB: MicroRNA
shuttle from cell-to-cell by exosomes and its impact in cancer.
Noncoding RNA. 5(28)2019.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Shirazi S, Huang CC, Kang M, Lu Y,
Ravindran S and Cooper LF: The importance of cellular and exosomal
miRNAs in mesenchymal stem cell osteoblastic differentiation. Sci
Rep. 11(5953)2021.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Li C, Zhou T, Chen J, Li R, Chen H, Luo S,
Chen D, Cai C and Li W: The role of Exosomal miRNAs in cancer. J
Transl Med. 20(6)2022.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Wang Y, Zhang M and Zhou F: Biological
functions and clinical applications of exosomal long non-coding
RNAs in cancer. J Cell Mol Med. 24:11656–11666. 2020.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Zhang W, Yan Y, Peng J, Thakur A, Bai N,
Yang K and Xu Z: Decoding roles of exosomal lncRNAs in tumor-immune
regulation and therapeutic potential. Cancers (Basel).
15(286)2022.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Yang Q, Diamond MP and Al-Hendy A: Early
life adverse environmental exposures increase the risk of uterine
fibroid development: role of epigenetic regulation. Front
Pharmacol. 7(40)2016.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Díez-Sainz E, Milagro FI, Riezu-Boj JI and
Lorente-Cebrián S: Effects of gut microbiota-derived extracellular
vesicles on obesity and diabetes and their potential modulation
through diet. J Physiol Biochem. 78:485–499. 2022.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Liang X, Dai N, Sheng K, Lu H, Wang J,
Chen L and Wang Y: Gut bacterial extracellular vesicles: Important
players in regulating intestinal microenvironment. Gut Microbes.
14(2134689)2022.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Macia L, Nanan R, Hosseini-Beheshti E and
Grau GE: Host- and Microbiota-derived extracellular vesicles,
immune function, and disease development. Int J Mol Sci.
21(107)2019.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Martínez-Ruiz S, Sáez-Fuertes L,
Casanova-Crespo S, Rodríguez-Lagunas MJ, Pérez-Cano FJ, Badia J and
Baldoma L: Microbiota-Derived extracellular vesicles promote
immunity and intestinal maturation in suckling rats. Nutrients.
15(4701)2023.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Liu H, Zhang Q, Wang S, Weng W, Jing Y and
Su J: Bacterial extracellular vesicles as bioactive nanocarriers
for drug delivery: Advances and perspectives. Bioact Mater.
14:169–181. 2021.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Liu JH, Chen CY, Liu ZZ, Luo ZW, Rao SS,
Jin L, Wan TF, Yue T, Tan YJ, Yin H, et al: Extracellular vesicles
from child gut microbiota enter into bone to preserve bone mass and
strength. Adv Sci (Weinh). 8(2004831)2021.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Kaisanlahti A, Turunen J, Byts N,
Samoylenko A, Bart G, Virtanen N, Tejesvi MV, Zhyvolozhnyi A,
Sarfraz S and Kumpula S: , et al: Maternal microbiota
communicates with the fetus through microbiota-derived
extracellular vesicles. Microbiome. 11(249)2023.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Du X, Ley R and Buck AH: MicroRNAs and
extracellular vesicles in the gut: New host modulators of the
microbiome? Microlife. 2(uqab010)2021.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Feng X, Chen X, Zheng X, Zhu H, Qi Q, Liu
S, Zhang H and Che J: Latest trend of milk derived exosomes:
Cargos, functions, and applications. Front Nutr.
8(747294)2021.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Lyons KE, Ryan CA, Dempsey EM, Ross RP and
Stanton C: Breast milk, a source of beneficial microbes and
associated benefits for infant health. Nutrients.
12(1039)2020.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Duale A, Singh P and Al Khodor S: Breast
milk: A meal worth having. Front Nutr. 8(800927)2022.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Yi DY and Kim SY: Human breast milk
composition and function in human health: From nutritional
components to microbiome and MicroRNAs. Nutrients.
13(3094)2021.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Banić M, Butorac K, Čuljak N, Leboš Pavunc
A, Novak J, Bellich B, Kazazić S, Kazazić S, Cescutti P, Šušković
J, et al: The human milk microbiota produces potential therapeutic
biomolecules and shapes the intestinal microbiota of infants. Int J
Mol Sci. 23(14382)2022.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Notarbartolo V, Giuffrè M, Montante C,
Corsello G and Carta M: Composition of human breast milk microbiota
and its role in children's health. Pediatr Gastroenterol Hepatol
Nutr. 25:194–210. 2022.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Kim KU, Kim WH, Jeong CH, Yi DY and Min H:
More than Nutrition: Therapeutic potential of breast milk-derived
exosomes in cancer. Int J Mol Sci. 21(7327)2020.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Shah J, Sims B and Martin C: Therapeutic
potential of human breast milk derived exosomes. J Nanopart Res.
24(260)2022.
|
|
94
|
Admyre C, Johansson SM, Qazi KR, Filén
JJ, Lahesmaa R, Norman M, Neve EP, Scheynius A and Gabrielsson S:
Exosomes with immune modulatory features are present in human
breast milk1. J Immunol. 179:1969–1978. 2007.PubMed/NCBI View Article : Google Scholar
|
|
95
|
de la Torre Gomez C, Goreham RV, Bech
Serra JJ, Nann T and Kussmann M: ‘Exosomics’-A review of
biophysics, biology and biochemistry of exosomes with a focus on
human breast milk. Front Genet. 9(92)2018.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Mirza AH, Kaur S, Nielsen LB, Størling J,
Yarani R, Roursgaard M, Mathiesen ER, Damm P, Svare J, Mortensen HB
and Pociot F: Breast milk-derived extracellular vesicles enriched
in exosomes from mothers with type 1 diabetes contain aberrant
levels of microRNAs. Front Immunol. 10(2543)2019.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Kim KU, Han K, Kim J, Kwon DH, Ji YW, Yi
DY and Min H: The protective role of exosome-derived MicroRNAs and
proteins from human breast milk against infectious agents.
Metabolites. 13(635)2023.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Chiurazzi M, Cozzolino M, Reinelt T,
Nguyen TD, Elke Chie S, Natalucci G and Miletta MC: Human milk and
brain development in infants. Reprod Med. 2:107–117. 2021.
|
|
99
|
Guo MM, Zhang K and Zhang JH: Human breast
milk-derived exosomal miR-148a-3p protects against necrotizing
enterocolitis by regulating p53 and Sirtuin 1. Inflammation.
45:1254–1268. 2022.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Gialeli G, Panagopoulou O, Liosis G and
Siahanidou T: Potential epigenetic effects of human milk on
infants' neurodevelopment. Nutrients. 15(3614)2023.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Cintio M, Polacchini G, Scarsella E,
Montanari T, Stefanon B and Colitti M: MicroRNA Milk Exosomes: From
cellular regulator to genomic marker. Animals (Basel).
10(1126)2020.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Melnik BC, Stremmel W, Weiskirchen R, John
SM and Schmitz G: Exosome-Derived MicroRNAs of human milk and their
effects on infant health and development. Biomolecules.
11(851)2021.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Zhou F, Paz HA, Sadri M, Cui J, Kachman
SD, Fernando SC and Zempleni J: Dietary bovine milk exosomes elicit
changes in bacterial communities in C57BL/6 mice. Am J Physiol
Gastrointest Liver Physiol. 317:G618–G624. 2019.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Turunen J, Tejesvi MV, Suokas M, Virtanen
N, Paalanne N, Kaisanlahti A, Reunanen J and Tapiainen T: Bacterial
extracellular vesicles in the microbiome of first-pass meconium in
newborn infants. Pediatr Res. 93:887–896. 2023.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Holzhausen EA, Kupsco A, Chalifour BN,
Patterson WB, Schmidt KA, Mokhtari P, Baccarelli AA, Goran MI and
Alderete TL: Influence of technical and maternal-infant factors on
the measurement and expression of extracellular miRNA in human
milk. Front Immunol. 14(1151870)2023.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Shah KB, Chernausek SD, Garman LD, Pezant
NP, Plows JF, Kharoud HK, Demerath EW and Fields DA: Human milk
exosomal MicroRNA: Associations with maternal overweight/obesity
and infant body composition at 1 month of life. Nutrients.
13(1091)2021.PubMed/NCBI View Article : Google Scholar
|