Introduction
Since the start of the 21st century, vitamin D has
received increasing attention from the health and biomedical
scientific community, more so than any other micronutrient
(1). Vitamin D is a crucial
nutrient as it promotes calcium absorption from the intestines,
prevents calcium excretion via renal reabsorption, bone development
and metabolism, and prevent the development of rickets during
childhood (2). Over the past few
decades, evidence regarding the extra-skeletal functions of vitamin
D has been increasing, such as in the muscular, reproductive,
immune and integumentary systems. Such evidence indicates that an
improved vitamin D status leads to improved overall health
(3,4). Vitamin D is primarily obtained
through exposure to the sun and, to a lesser extent, through dairy
products and vitamin D supplements (5). Failure to acquire the necessary
amounts of vitamin D has been linked to an increased risk of a wide
range of conditions, including osteoporosis, diabetes,
cardiovascular diseases, cancer, musculoskeletal conditions and
hypertension (6). Serum
25-hydroxyvitamin D[25(OH)D] is a highly reliable biomarker that
has been recommended for use to assess the vitamin D status
(7). Currently, there is
controversy as regards the optimum serum levels of 25(OH)D, as
there is considerable variation between the normal values of
different populations (4,8). A wide range of minimum values have
been proposed, ranging from 12 to 40 ng/ml. Despite the
disagreements, a serum 25(OH)D level of <20 ng/ml is the most
commonly used value among studies to indicate vitamin D deficiency
(6). Globally, vitamin D
deficiency is highly prevalent, to the extent that it is considered
a pandemic and a major global health issue (1,7). The
worldwide prevalence of vitamin D deficiency varies from 30 to 93%
(8). It has been observed that
41.6% of adults in the USA are vitamin D-deficient (9). Similarly, according to the study by
Cashman et al (10),
>40% of the European population suffers from vitamin D
deficiency (<20 ng/ml). Even though the Middle Eastern
populations have ample exposure to sunlight, vitamin D deficiency
is even more prevalent (8).
However, to date, at least to the best of our knowledge, no study
has been performed to evaluate the prevalence of vitamin D
deficiency among the general population of Iraq or the Kurdistan
region.
Therefore, the present study aimed to examine the
vitamin D status among the healthy population of the Kurdistan
region in northern Iraq.
Subjects and methods
Study design and setting
The present study was a community-based
cross-sectional study carried out from June, 2021 to January, 2022
at the Kurdistan region of Iraq. In total, 991 apparently healthy
individuals (582 males and 409 females) of various ages were
randomly recruited from various public areas after obtaining
ethical permission. Both written and informed consent were obtained
from each participant. The study was approved by the Sulaimani
University Ethics Committee.
Inclusion and exclusion criteria
In the present study, only healthy individuals
currently residing in the Kurdistan region were enrolled. The
exclusion criteria were as follows: Individuals with any medical or
chronic condition (apart from obesity, so as to determine any
possible link between obesity and vitamin D levels), pregnant
women, or those taking vitamin D supplements or other potentially
interfering medications were not enrolled.
Data collection
Each participant completed a questionnaire to
provide socio-demographic characteristics (age, marital status,
smoking status, alcohol consumption and occupation), medical
history, and medications. For children, consent was acquired from
the parents. Bodyweight and height were measured for the
participants for the calculation of body mass index (BMI).
Clinical measures
Trained health workers performed the data collection
and obtained blood samples from the individuals who consented to
participate. All the blood samples were obtained during the day and
were collected in gel tubes (Greiner Bio-One). On the same day of
sample collection, the samples were immediately sent to the Smart
Laboratory (at Smart Health Tower in Sulaimani, Iraq) for sera
separation by centrifugation (5,000 rpm, 10 min, at 25˚C) and
storage in a -70˚C environment for later use in the evaluation of
vitamin D status.
Vitamin D assessment
Chemiluminescence immunoassay was performed via
Cobas E411 using the Vitamin D total Elecsys Cobas E100 kit (Lot
no. 56154801; Roche Diagnostics) to analyze the serum 25(OH)D
concentrations of the samples, as it is the most utilized form of
vitamin D and accounts for the majority of the circulating 25(OH)D.
In the present study, the vitamin D status was categorized into
three major cut-offs based on serum 25(OH)D concentrations: <20
ng/ml for deficiency, 20-29.9 ng/ml for insufficiency and 30-60
ng/ml for optimality. Levels >60 ng/ml were considered toxic
(11).
Statistical analysis
The acquired data were analyzed using SPSS software
24.0 (IBM Corp.). Quantitative variables were analyzed using an
independent samples t-test (comparisons between means of more than
two groups were performed using one-way ANOVA), and the data are
presented in the form of the mean ± standard deviation. In the case
of significant results from ANOVA, Hochberg's GT2 post hoc test was
used (due to unequal sample size of the groups) to determine which
groups led to the significant differences. Qualitative data are
presented as proportions and percentages. A P-value <0.05 was
considered to indicate a statistically significant difference.
Results
Demographics and characteristics of
the participants
Of the total number of healthy subjects enrolled in
the present study (n=991), 582 (58.7%) were male, and 409 (41.3%)
were female. The subjects had a mean age of 30.6±12.2 years (range,
2-80 years), with the majority of the subjects (60.5%) being
between 18-39 years of age. The mean BMI of the participants was
25.07±4.7 (13-50). The difference between the mean age of the male
and female participants was insignificant (P=0.265). The majority
of the subjects were non-smokers (88.3%). Further characteristics
of the enrolled participants are presented in Table I.
 | Table ICharacteristics of the participants
enrolled in the present study. |
Table I
Characteristics of the participants
enrolled in the present study.
| Characteristic | Frequency/mean | Percentage |
|---|
| Sex | | |
|
Male | 582 | 58.7 |
|
Female | 409 | 41.3 |
| Age, years | 30.6 | |
|
<18 | 161 | 16.2 |
|
18-39 | 599 | 60.5 |
|
40-60 | 221 | 22.3 |
|
>60 | 10 | 1 |
| Marital status | | |
|
Married | 573 | 57.8 |
|
Single | 418 | 42.2 |
| BMI | 25.07 | |
|
<18.5 | 74 | 7.5 |
|
18.5-24.9 | 377 | 38 |
|
25-29.9 | 379 | 38.2 |
|
≥30 | 161 | 16.3 |
| Smoking status | | |
|
Ever
smoker | 116 | 11.7 |
|
Non-smoker | 875 | 88.3 |
| Alcohol
consumption | | |
|
Yes | 18 | 1.8 |
|
No | 973 | 98.2 |
| Occupation
category | | |
|
Indoor
workers (barber, cleaner, clerk, receptionist, government
employee) | 298 | 30.1 |
|
Health care
professionals (Pharmacist, nurse, laboratorian, physician,
radiologist) | 67 | 6.8 |
|
Unemployed
(housewife, retired) | 131 | 13.2 |
|
Student | 214 | 21.6 |
|
Teaching
professionals | 52 | 5.2 |
|
Outdoor
workers (engineer, driver, construction worker, farmer) | 154 | 15.5 |
|
Security and
military | 75 | 7.6 |
| Blood group | | |
|
A+ | 263 | 26.5 |
|
A- | 23 | 2.3 |
|
B+ | 188 | 19 |
|
B- | 16 | 1.6 |
|
AB+ | 65 | 6.6 |
|
AB- | 6 | 0.6 |
|
O+ | 409 | 41.3 |
|
O- | 21 | 2.1 |
Prevalence of vitamin D deficiency and
insufficiency
In the present study population, the prevalence of
vitamin D deficiency (<20 ng/ml) was markedly high (74.3%), with
another large proportion of the study population (21.1%) having
insufficient levels of vitamin D (20-29.9 ng/ml). Only 4.5% of the
subjects had serum 25(OH)D levels within the optimal range (30-60
ng/ml), and one individual (0.1%) had a toxic level of 25(OH)D
(>60 ng/ml) (Table II).
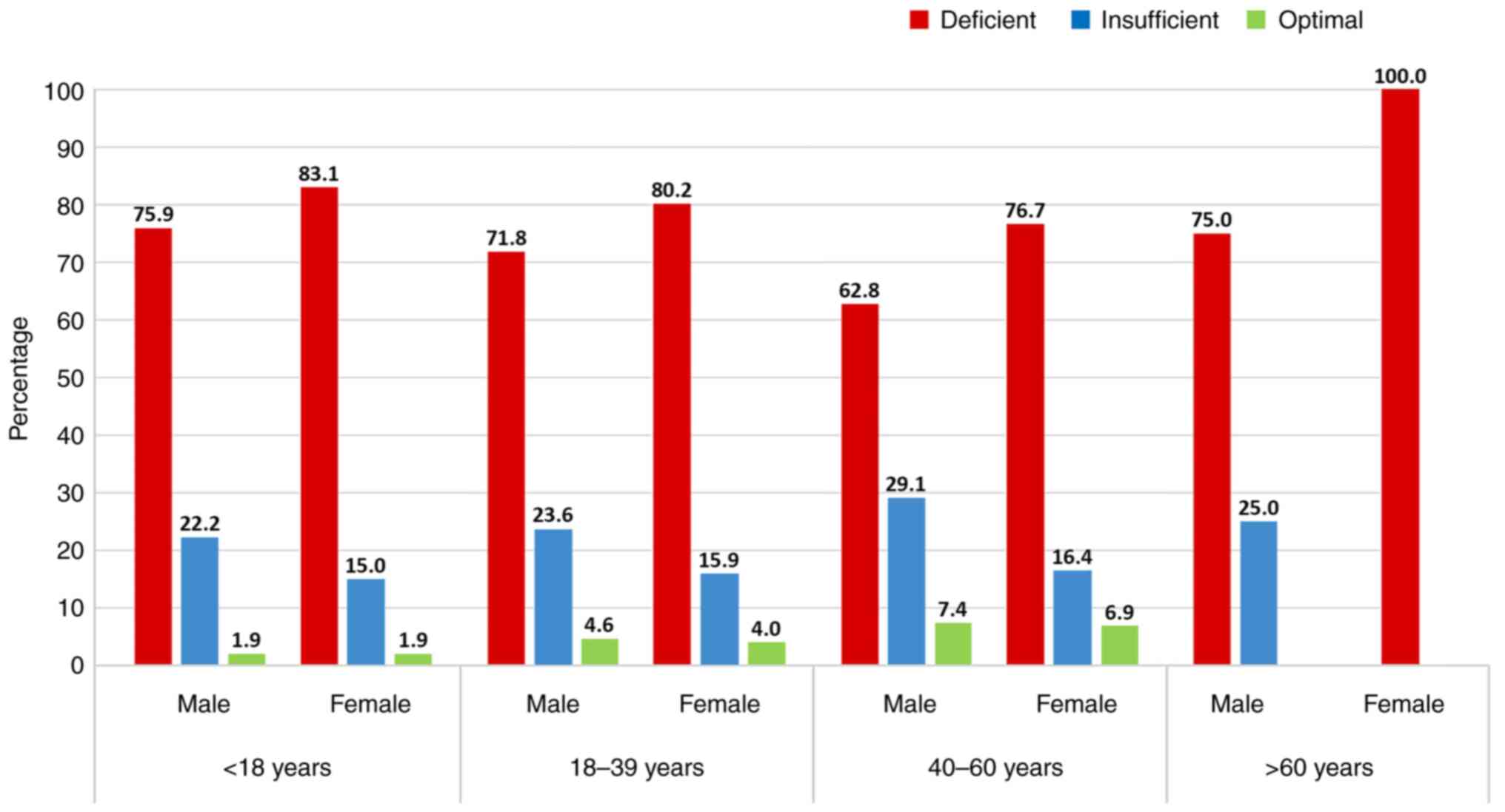
Vitamin D deficiency was more prevalent among the females of all
age groups (80.4%) compared to the males (69.9%) in the population
studied. Additionally, the highest prevalence of vitamin D
deficiency was found in participants aged <18 years and in those
>60 years. The vitamin D status in both sexes according to age
groups is illustrated in Fig.
1.
 | Table IIVitamin D status in the studied
population according to the serum 25(OH)D level. |
Table II
Vitamin D status in the studied
population according to the serum 25(OH)D level.
| Parameter | Frequency | Percentage |
|---|
| Deficient | 736 | 74.3 |
| Insufficient | 209 | 21.1 |
| Optimal | 45 | 4.5 |
| Toxic | 1 | 0.1 |
Predictors for lower serum 25(OH)D
concentrations
The mean serum 25(OH)D concentration of the study
population was 16.29±7.1 ng/ml (3.78-62.16 ng/ml). No significant
difference in 25(OH)D levels was noted as regards the BMI, smoking
status, or alcohol consumption. Despite the high prevalence of
vitamin D deficiency, the mean 25(OH)D level was significantly
lower in females (14.05±7.55 ng/ml) than in males (17.87±6.46
ng/ml) (P<0.001) (Table III).
Despite an overall noticeable difference in the mean 25(OH)D
concentration among the different age groups, which revealed lower
serum 25(OH)D levels in participants <40 years, significant age
group differences were only found in males (P=0.028) and not in
females (P=0.259) (Table IV).
 | Table IIIMean serum 25(OH)D levels according
to different characteristics. |
Table III
Mean serum 25(OH)D levels according
to different characteristics.
| Characteristic | Mean 25(OH)D | P-value |
|---|
| Sex | | <0.001 |
|
Male |
17.8671±6.45803 | |
|
Female |
14.0544±7.55038 | |
| Age, years | | <0.001 |
|
<18 |
14.8242±6.70206 | |
|
18-39 |
16.0220±7.03543 | |
|
40-60 |
18.0099±7.67882 | |
|
>60 |
18.2860±3.96385 | |
| Marital status | | 0.534 |
|
Married |
17.0817±7.14544 | |
|
Single |
15.2131±7.08522 | |
| BMI | | 0.366 |
|
<18.5 |
15.5951±6.76480 | |
|
18.5-24.9 |
15.9714±7.41235 | |
|
25-29.9 |
16.7744±7.14961 | |
|
≥30 |
16.2371±6.84541 | |
| Smoking status | | 0.817 |
|
Ever
smoker |
19.1954±7.19120 | |
|
Non-smoker |
15.9088±7.08957 | |
| Alcohol
consumption | | 0.185 |
|
Yes |
20.2956±7.79813 | |
|
No |
16.2195±7.14740 | |
| Blood group | | 0.335 |
|
A+ |
16.5320±6.96608 | |
|
A- |
13.4663±7.83233 | |
|
B+ |
15.9848±6.67549 | |
|
B- |
13.0046±7.35624 | |
|
AB+ |
17.3835±7.35428 | |
|
AB- |
14.0320±7.21451 | |
|
O+ |
16.3114±7.28488 | |
|
O- |
18.0722±12.92086 | |
 | Table IVComparison of the mean serum 25(OH)D
levels between different sexes and age groups. |
Table IV
Comparison of the mean serum 25(OH)D
levels between different sexes and age groups.
| | Serum 25(OH)D
levels (ng/ml) |
|---|
| Sex | Age group | Frequency | Mean | SD | P-value |
|---|
| Male | <18 years | 54 | 17.4096 | 5.45653 | 0.028 | <0.001 |
| | 18-39 years | 372 | 17.3783 | 6.23975 | | |
| | 40-60 years | 148 | 19.2297 | 7.23821 | | |
| | >60 years | 8 | 18.4775 | 4.29270 | | |
| | Total | 582 | 17.8671 | 6.45803 | | |
| Female | <18 years | 107 | 13.5193 | 6.91299 | 0.259 | |
| | 18-39 years | 227 | 13.7994 | 7.68548 | | |
| | 40-60 years | 73 | 15.5367 | 7.99638 | | |
| | >60 years | 2 | 17.5200 | 3.30926 | | |
| | Total | 409 | 14.0544 | 7.55038 | | |
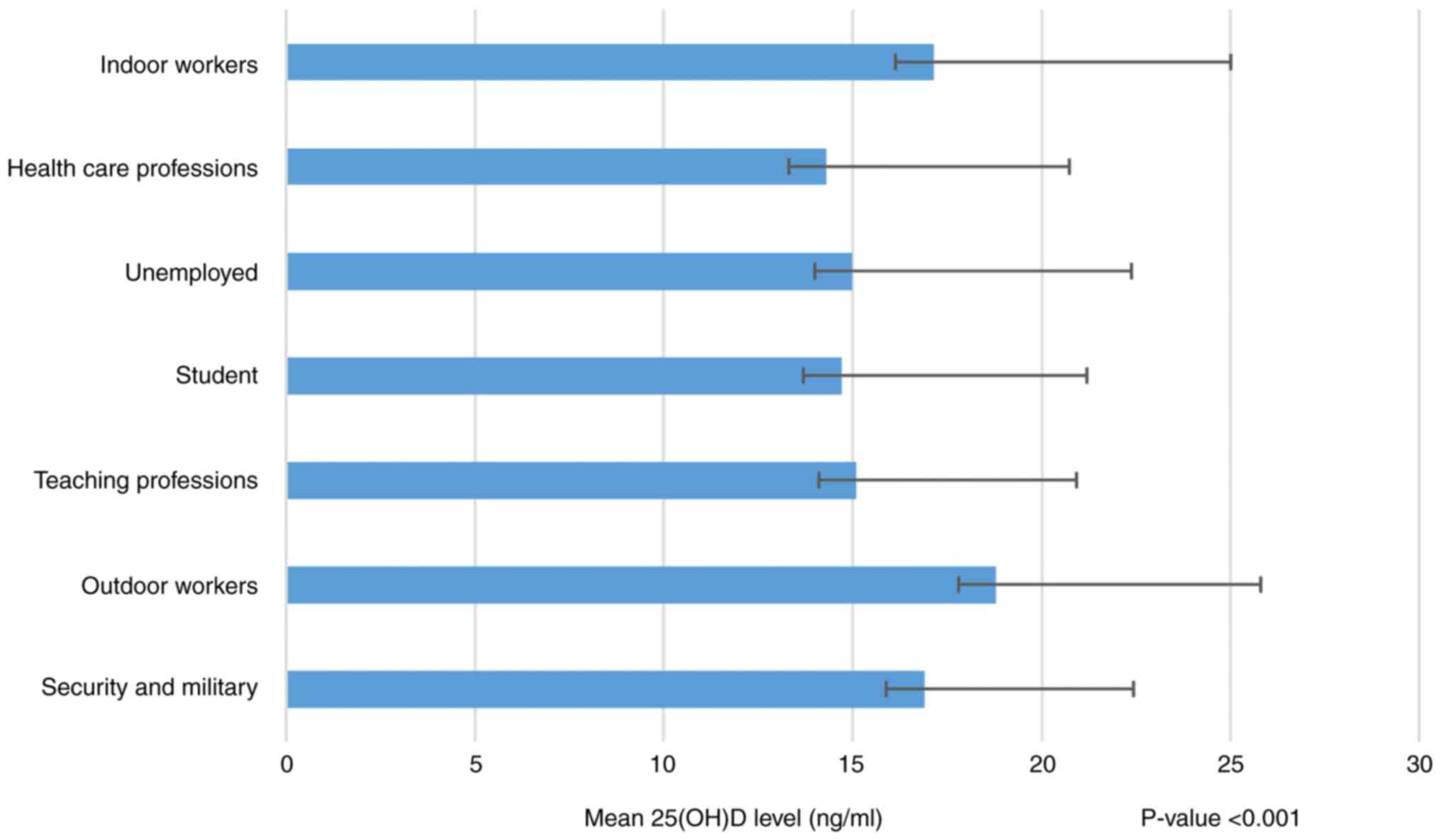
The type of occupation appeared to have some
influence on the serum 25(OH)D levels. However, despite a small
difference, the mean value of 25(OH)D levels in all occupational
categories was still within the vitamin D deficiency threshold.
Thus, of note, the prevalence of vitamin D deficiency was still
high, not regarding the occupations of the participants (Fig. 2).
Discussion
The Kurdistan region in the northern part of Iraq
has a semi-arid climate. The days in this area are often sunny and
provide a sufficient amount of sunlight for the inhabitants. Hence,
in the present population, the vitamin D status was expected to be
mostly within the normal range. However, according to the findings,
this expectation was far from true, with the majority of the
population either having deficient or insufficient values of
vitamin D (74.3 and 21.1%, respectively).
Vitamin D is a micronutrient that is primarily
acquired from sunlight; hence, avoiding the sun can lead to various
complications (12). Moreover, it
has been reported that almost all body tissues have vitamin D
receptors, and the majority even possess the hydroxylase enzyme
required for the conversion of 25(OH)D to the active form,
indicating their importance for the proper functioning of the body
(1).
Currently, there is some controversy regarding the
optimum levels of serum 25(OH)D (4). A wide range of minimum values have
been proposed, ranging from 12 to 40 ng/ml, primarily depending on
whether that value can suppress the parathyroid hormone to its
minimum. The Endocrine Society Clinical Practice Guidelines
consider a serum 25(OH)D level of >30 ng/ml to be sufficient for
the body. By contrast, the National Academy of Medicine recommends
a level of >20 ng/ml to be sufficient (11). Despite the disagreements however, a
serum 25(OH)D level <20 ng/ml is the most commonly used value
among studies to indicate vitamin D deficiency, and it is the value
that was regarded to indicate deficiency throughout the present
study (6). When measuring vitamin
D levels, the time of the year can influence the concentration of
serum 25(OH)D levels. In this regard, summer is considered an ideal
season for the measurement of vitamin D levels (13). The present study was conducted
during the summer and autumn seasons.
The worldwide prevalence of vitamin D deficiency
varies largely, ranging from 30 to 93% (8). It has been observed that 41.6% of
adults in the USA are vitamin D-deficient (9). Other community-based studies have
reported that vitamin D deficiency ranges between 45-52% in New
Zealand, 25% in Canada, 47-65% in Korea and 45% in Portugal
(7,14-16).
In Europe, vitamin D deficiency has been observed to range between
30-60% of Western, Southern, and Eastern European populations and
>20% of populations in Northern Europe (17).
Although sunlight is abundant in developing
countries, particularly in the Middle East, vitamin D deficiency
appears to be a much more prevalent, with only a minority of these
populations having adequate vitamin D levels (1,8). In
China, Ning et al (18)
reported that 87.1% of the Beijing population were vitamin
D-deficient, and only 2.9% of the participants achieved optimal
levels. In Pakistan, the prevalence of vitamin D deficiency and
insufficiency were reported to be 70 and 21.1%, respectively
(8). A study conducted in Qatar
revealed a prevalence of 64% (6).
A meta-analysis on the prevalence of vitamin D deficiency in Saudi
Arabia also revealed that 81% of the population were deficient
(1). In Kuwait, the prevalence of
deficiency was found to be 83% (19). Bachhel and colleagues found that
90% of the Indian population were vitamin D insufficient (<30
ng/ml) (20). In Iran, vitamin D
deficiency prevalence was found to be around 85.2% (21). Notably, the study by Öztürk et
al (22) in southeast Turkey,
in which the inhabitants have the same cultural and ethnic
background as the Kurdistan region in northern Iraq, revealed very
similar findings to those of the present study, with a mean serum
level of 25(OH)D of 16.61±6.90 ng/ml, with the prevalence of
vitamin D deficiency and insufficiency being 75.54 and 19.38%,
respectively (22). In a recent
study performed in the Dohuk Governorate, Kurdistan Region, Iraq by
Abdulrahman et al (23),
only 24% of the participants had a normal level of total 25(OH)D,
which is higher than that observed in the present study
population.
The present study demonstrated that vitamin D
deficiency was more prevalent in females than in males (80.4 vs.
69.9%), and sex was associated with a lower mean serum 25(OH)D
concentration (14.05 vs. 17.87 ng/ml). However, the findings in the
literature are conflicting regarding this aspect. Some studies have
indicated a higher prevalence among females due to less sun
exposure, which may be explained by the frequent use of sunscreens,
fewer outdoor activities and the Islamic culture of covering the
body from head to toe (24-27).
However, other studies have demonstrated lower 25OHD levels and a
higher prevalence of vitamin D deficiency among males, probably due
to the more common use of vitamin D supplements among the females
of these populations (6,28).
In the present study, the levels of 25(OH)D differed
considerably between the age groups, with subjects <40 years of
age having the lowest levels of 25(OH)D, particularly among
females. This is in agreement with other studies conducted in
developing countries (22,23,29,30).
This finding may be explained by the fact that elders may have more
frequent exposure to sunlight and may consume more healthy foods
than younger individuals. However, an inverse association of age
with the 25(OH)D level has also been reported, with higher serum
concentrations of 25(OH)D found among younger subjects (12). As regards the association between
obesity and vitamin D deficiency, previous studies have indicated a
positive association between the two (6,31),
with only a few studies reporting no association (32,33).
In the present study, no significant difference in 25(OH)D levels
was found with regards to BMI.
Similar findings between the mentioned studies
regarding the prevalence of vitamin D deficiency can somewhat be
explained by the shared geographical location of the stated
populations, in which high temperatures and the intensity of
sunlight during the summer prevent individuals from exposing their
skin. Additionally, dressing culture and the lack of awareness
regarding the importance of consuming healthy foods that contain
vitamin D and exposure to sunlight may also play a role in the high
prevalence of deficiency (30).
The international recommendation for the correction
of vitamin D deficiency is vitamin D supplementation and increased
sunlight exposure. However, current international guidelines may
not apply to the local communities of Middle Eastern countries as
these guidelines have been specifically tailored for North American
or European communities, which are vastly different (genetically,
geographically, economically and culturally) from Middle Eastern
countries (1). Additionally, the
optimal level of vitamin D may differ from one nation to another.
Hence, it is highly recommended that further research is conducted
to accurately determine the amounts of vitamin D required by these
populations.
The ministry of health of the Kurdistan region of
Iraq needs to develop a public health policy to raise community
awareness on this matter by promoting healthy exposure to sunlight
and the consumption of vitamin D-containing foods. The ministry
should possibly also take the necessary measures for vitamin D
fortification of food and dairy products to correct the high
vitamin D deficiency prevalence found in this population.
Although a point of strength of the present study is
the fact that it was a community-based study, it also has multiple
limitations, as information regarding diet, the amount of sun
exposure, and dressing habits was not acquired from the
participants. In addition, the concentrations of serum calcium and
parathyroid hormone were not measured for the participants.
In conclusion, vitamin D deficiency is highly
prevalent among the population of the Kurdistan region in Iraq,
particularly among females and the younger age group. Efforts are
thus required to raise public awareness regarding this health
concern. The vitamin D fortification of foods and dairy products is
strongly recommended as a first-line measure to correct vitamin D
deficiency. Further studies are warranted to determine other
potential factors that contribute to the high prevalence of vitamin
D deficiency among these populations.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
FHK was involved in the literature selection, in the
conception and design of the study, and in the writing of the first
draft of the manuscript. GSA was involved in data interpretation
and in the writing of the first draft of the manuscript. DAH, SHM,
ROS, SEH, SSH, AKH, CMR, WAH, BAA, SFA, KMS, RQS, AMS and BJHA were
involved in obtaining patient data, and in the final reading and
approval of the manuscript. BAA and GSA confirm the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Sulaimani
University Ethics Committee. Written informed consent was obtained
from all participants or the parents in the case that the
participants were underage.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Al-Daghri NM: Vitamin D in Saudi Arabia:
Prevalence, distribution and disease associations. J Steroid
Biochem Mol Biol. 175:102–107. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gordon CM, DePeter KC, Feldman HA, Grace E
and Emans SJ: Prevalence of vitamin D deficiency among healthy
adolescents. Arch Pediatr Adolesc Med. 158:531–537. 2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Holick MF: High prevalence of vitamin D
inadequacy and implications for health. In: Mayo Clinic
Proceedings. Vol 81. Elsevier, Amsterdam, pp353-373, 2006.
|
|
4
|
Cashman KD: Vitamin D deficiency:
Defining, prevalence, causes, and strategies of addressing. Calcif
Tissue Int. 106:14–29. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tabrizi R, Moosazadeh M, Akbari M,
Dabbaghmanesh MH, Mohamadkhani M, Asemi Z, Heydari ST, Akbari M and
Lankarani KB: High prevalence of vitamin D deficiency among Iranian
population: A systematic review and meta-analysis. Iran J Med Sci.
43:125–139. 2018.PubMed/NCBI
|
|
6
|
Al-Dabhani K, Tsilidis KK, Murphy N, Ward
HA, Elliott P, Riboli E, Gunter M and Tzoulaki I: Prevalence of
vitamin D deficiency and association with metabolic syndrome in a
Qatari population. Nutr Diabetes. 7(e263)2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Duarte C, Carvalheiro H, Rodrigues AM,
Dias SS, Marques A, Santiago T, Canhão H, Branco JC and da Silva
JAP: Prevalence of vitamin D deficiency and its predictors in the
Portuguese population: A nationwide population-based study. Arch
Osteoporos. 15(36)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mansoor S, Habib A, Ghani F, Fatmi Z,
Badruddin S, Mansoor S, Siddiqui I and Jabbar A: Prevalence and
significance of vitamin D deficiency and insufficiency among
apparently healthy adults. Clin Biochem. 43:1431–1435.
2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Forrest KY and Stuhldreher WL: Prevalence
and correlates of vitamin D deficiency in US adults. Nutr Res.
31:48–54. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Cashman KD, Dowling KG, Škrabáková Z,
Gonzalez-Gross M, Valtueña J, De Henauw S, Moreno L, Damsgaard CT,
Michaelsen KF, Mølgaard C, et al: Vitamin D deficiency in Europe:
Pandemic? Am J Clin Nutr. 103:1033–1044. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Holick MF, Binkley NC, Bischoff-Ferrari
HA, Gordon CM, Hanley DA, Heaney RP, Murad MH and Weaver CM:
Endocrine Society. Evaluation, treatment, and prevention of vitamin
D deficiency: An Endocrine society clinical practice guideline. J
Clin Endocrinol Metab. 96:1911–1930. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Badawi A, Arora P, Sadoun E, Al-Thani AA
and Al Thani MH: Prevalence of vitamin d insufficiency in Qatar: A
systematic review. J Public Health Res. 1:229–235. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bolland MJ, Chiu WW, Davidson JS, Grey A,
Bacon C, Gamble GD and Reid IR: The effects of seasonal variation
of 25-hydroxyvitamin D on diagnosis of vitamin D insufficiency. N Z
Med J. 121:63–74. 2008.PubMed/NCBI
|
|
14
|
Rockell JEP, Skeaff CM, Williams SM and
Green TJ: Serum 25-hydroxyvitamin D concentrations of New
Zealanders aged 15 years and older. Osteoporos Int. 17:1382–1389.
2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Langlois K, Green-Finestone L, Little J,
Hidiroglou N and Whiting S: Vitamin D status of Canadians as
measured in the 2007 to 2009 Canadian health measures survey.
Health Rep. 21:47–55. 2010.PubMed/NCBI
|
|
16
|
Choi HS, Oh HJ, Choi H, Choi WH, Kim JG,
Kim KM, Kim KJ, Rhee Y and Lim SK: Vitamin D insufficiency in
Korea-a greater threat to younger generation: The Korea national
health and nutrition examination survey (KNHANES) 2008. J Clin
Endocrinol Metab. 96:643–651. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lips P, Cashman KD, Lamberg-Allardt C,
Bischoff-Ferrari HA, Obermayer-Pietsch B, Bianchi ML, Stepan J,
El-Hajj Fuleihan G and Bouillon R: Current vitamin D status in
European and Middle East countries and strategies to prevent
vitamin D deficiency: A position statement of the European
calcified tissue society. Eur J Endocrinol. 180:P23–P54.
2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ning Z, Song S, Miao L, Zhang P, Wang X,
Liu J, Hu Y, Xu Y, Zhao T, Liang Y, et al: High prevalence of
vitamin D deficiency in urban health checkup population. Clin Nutr.
35:859–863. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zhang FF, Al Hooti S, Al Zenki S, Alomirah
H, Jamil KM, Rao A, Al Jahmah N, Saltzman E and Ausman LM: Vitamin
D deficiency is associated with high prevalence of diabetes in
Kuwaiti adults: Results from a national survey. BMC Public Health.
16(100)2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bachhel R, Singh NR and Sidhu JS:
Prevalence of vitamin D deficiency in north-west Punjab population:
A cross-sectional study. Int J Appl Basic Med Res. 5:7–11.
2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kaykhaei MA, Hashemi M, Narouie B,
Shikhzadeh A, Rashidi H, Moulaei N and Ghavami S: High prevalence
of vitamin D deficiency in Zahedan, southeast Iran. Ann Nutr Metab.
58:37–41. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Öztürk ZA, Gol M and Türkbeyler İH:
Prevalence of vitamin D deficiency in otherwise healthy individuals
between the ages of 18 and 90 years in southeast Turkey. Wien Klin
Wochenschr. 129:854–855. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Abdulrahman MA, Alkass SY and Mohammed NI:
Total and free vitamin D status among apparently healthy adults
living in Duhok Governorate. Sci Rep. 12(1778)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zargar AH, Ahmad S, Masoodi SR, Wani AI,
Bashir MI, Laway BA and Shah ZA: Vitamin D status in apparently
healthy adults in Kashmir Valley of Indian subcontinent. Postgrad
Med J. 83:713–716. 2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Atli T, Gullu S, Uysal AR and Erdogan G:
The prevalence of vitamin D deficiency and effects of ultraviolet
light on vitamin D levels in elderly Turkish population. Arch
Gerontol Geriatr. 40:53–60. 2005.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Goswami R, Kochupillai N, Gupta N, Goswami
D, Singh N and Dudha A: Presence of 25(OH) D deficiency in a rural
North Indian village despite abundant sunshine. J Assoc Physicians
India. 56:755–757. 2008.PubMed/NCBI
|
|
27
|
Hussain AN, Alkhenizan AH, El Shaker M,
Raef H and Gabr A: Increasing trends and significance of
hypovitaminosis D: A population-based study in the Kingdom of Saudi
Arabia. Arch Osteoporos. 9(190)2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hagenau T, Vest R, Gissel TN, Poulsen CS,
Erlandsen M, Mosekilde L and Vestergaard P: Global vitamin D levels
in relation to age, gender, skin pigmentation and latitude: An
ecologic meta-regression analysis. Osteoporos Int. 20:133–140.
2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Khan AH, Iqbal R, Naureen G, Dar FJ and
Ahmed FN: Prevalence of vitamin D deficiency and its correlates:
Results of a community-based study conducted in Karachi, Pakistan.
Arch Osteoporos. 7:275–282. 2012.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Al-Daghri NM, Hussain SD, Ansari MGA,
Khattak MNK, Aljohani N, Al-Saleh Y, Al-Harbi MY, Sabico S and
Alokail MS: Decreasing prevalence of vitamin D deficiency in the
central region of Saudi Arabia (2008-2017). J Steroid Biochem Mol
Biol. 212(105920)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sadiya A, Ahmed SM, Skaria S and Abusnana
S: Vitamin D status and its relationship with metabolic markers in
persons with obesity and type 2 diabetes in the UAE: A
cross-sectional study. J Diabetes Res. 2014(869307)2014.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Majumdar V, Nagaraja D and Christopher R:
Vitamin D status and metabolic syndrome in Asian Indians. Int J
Obes (Lond). 35:1131–1134. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Oosterwerff MM, Eekhoff EM, Heymans MW,
Lips P and van Schoor NM: Serum 25-hydroxyvitamin D levels and the
metabolic syndrome in older persons: A population-based study. Clin
Endocrinol (Oxf). 75:608–613. 2011.PubMed/NCBI View Article : Google Scholar
|