|
1
|
Chobanian AV, Bakris GL, Black HR, et al:
The Seventh Report of the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood Pressure: the
JNC 7 report. JAMA. 289:2560–2572. 2003. View Article : Google Scholar
|
|
2
|
Chobanian AV, Bakris GL, Black HR, et al:
Seventh report of the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood Pressure.
Hypertension. 42:1206–1252. 2003. View Article : Google Scholar
|
|
3
|
Sun Z, Zheng L, Detrano R, et al: Risk of
progression to hypertension in a rural Chinese women population
with prehypertension and normal blood pressure. Am J Hypertens.
23:627–632. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vasan RS, Larson MG, Leip EP, Kannel WB
and Levy D: Assessment of frequency of progression to hypertension
in non-hypertensive participants in the Framingham Heart Study: a
cohort study. Lancet. 358:1682–1686. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Greenlund KJ, Croft JB and Mensah GA:
Prevalence of heart disease and stroke risk factors in persons with
prehypertension in the United States, 1999–2000. Arch Intern Med.
164:2113–2118. 2004.PubMed/NCBI
|
|
6
|
Mainous AG III, Everett CJ, Liszka H, King
DE and Egan BM: Prehypertension and mortality in a nationally
representative cohort. Am J Cardiol. 94:1496–1500. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Maillard P, Seshadri S, Beiser A, et al:
Effects of systolic blood pressure on white-matter integrity in
young adults in the Framingham Heart Study: a cross-sectional
study. Lancet Neurol. 11:1039–1047. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Julius S, Nesbitt SD, Egan BM, et al:
Feasibility of treating prehypertension with an
angiotensin-receptor blocker. N Engl J Med. 354:1685–1697. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yambe M, Tomiyama H, Yamada J, et al:
Arterial stiffness and progression to hypertension in Japanese male
subjects with high normal blood pressure. J Hypertens. 25:87–93.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Baumann M, Janssen BJ, Hermans JJ, et al:
Transient AT1 receptor-inhibition in prehypertensive spontaneously
hypertensive rats results in maintained cardiac protection until
advanced age. J Hypertens. 25:207–215. 2007. View Article : Google Scholar
|
|
11
|
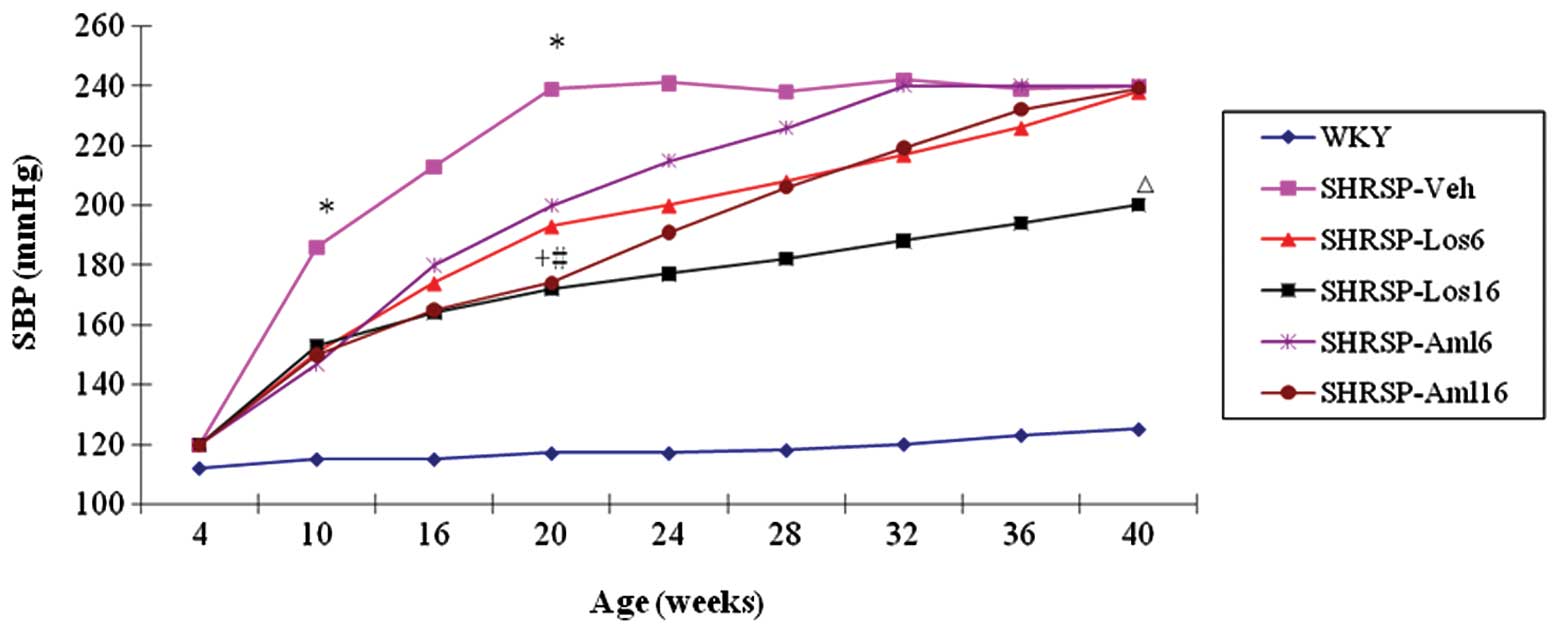
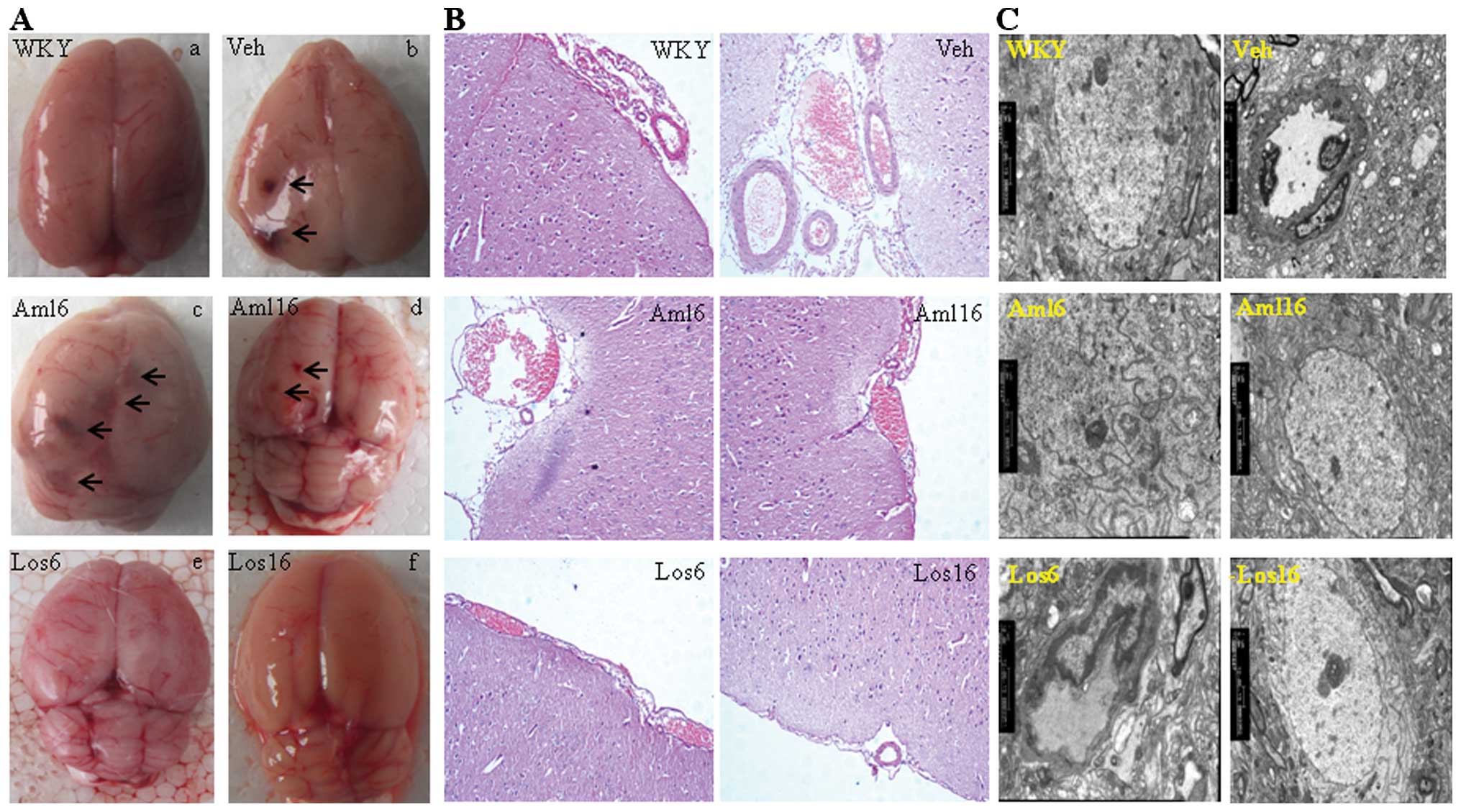
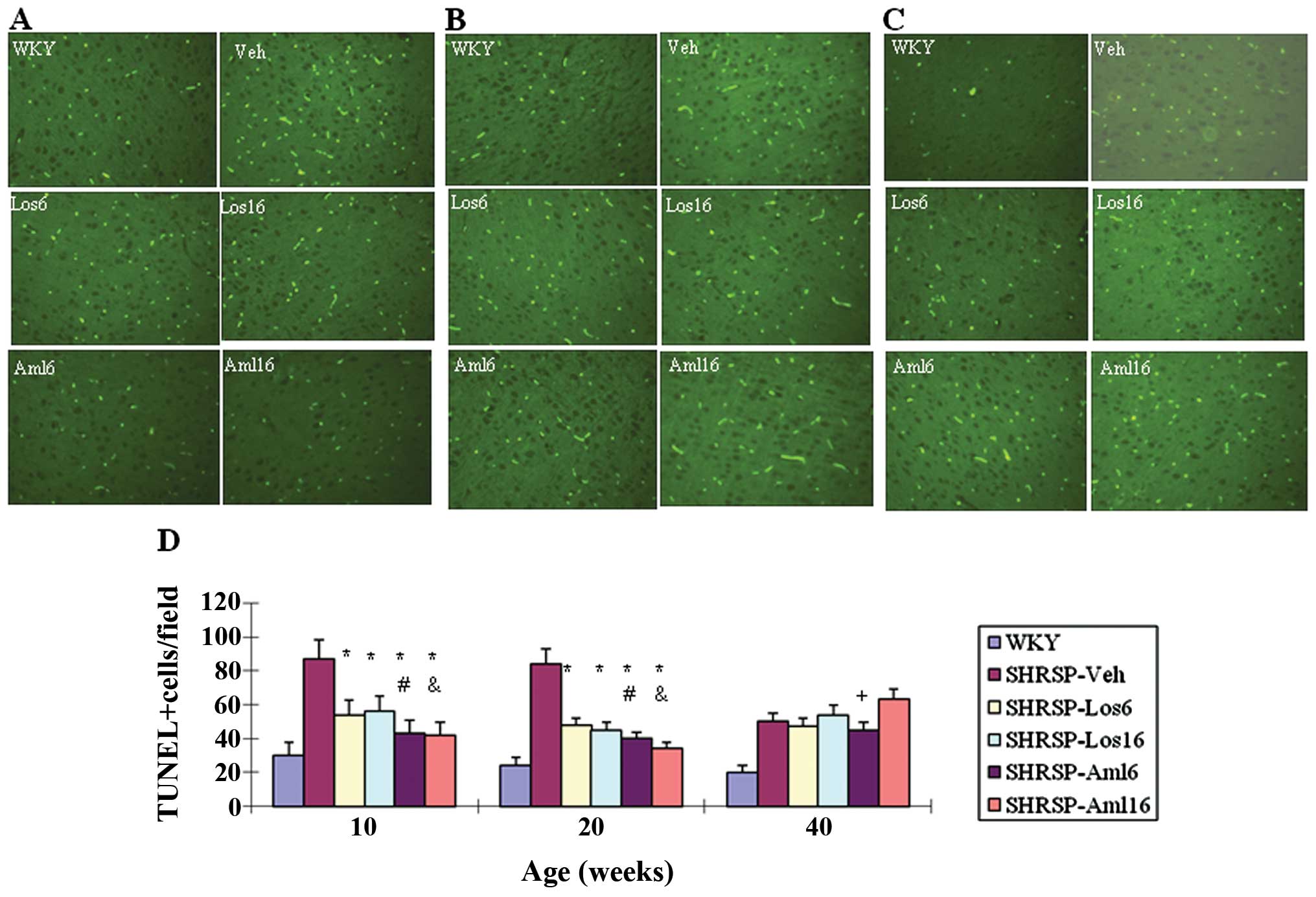
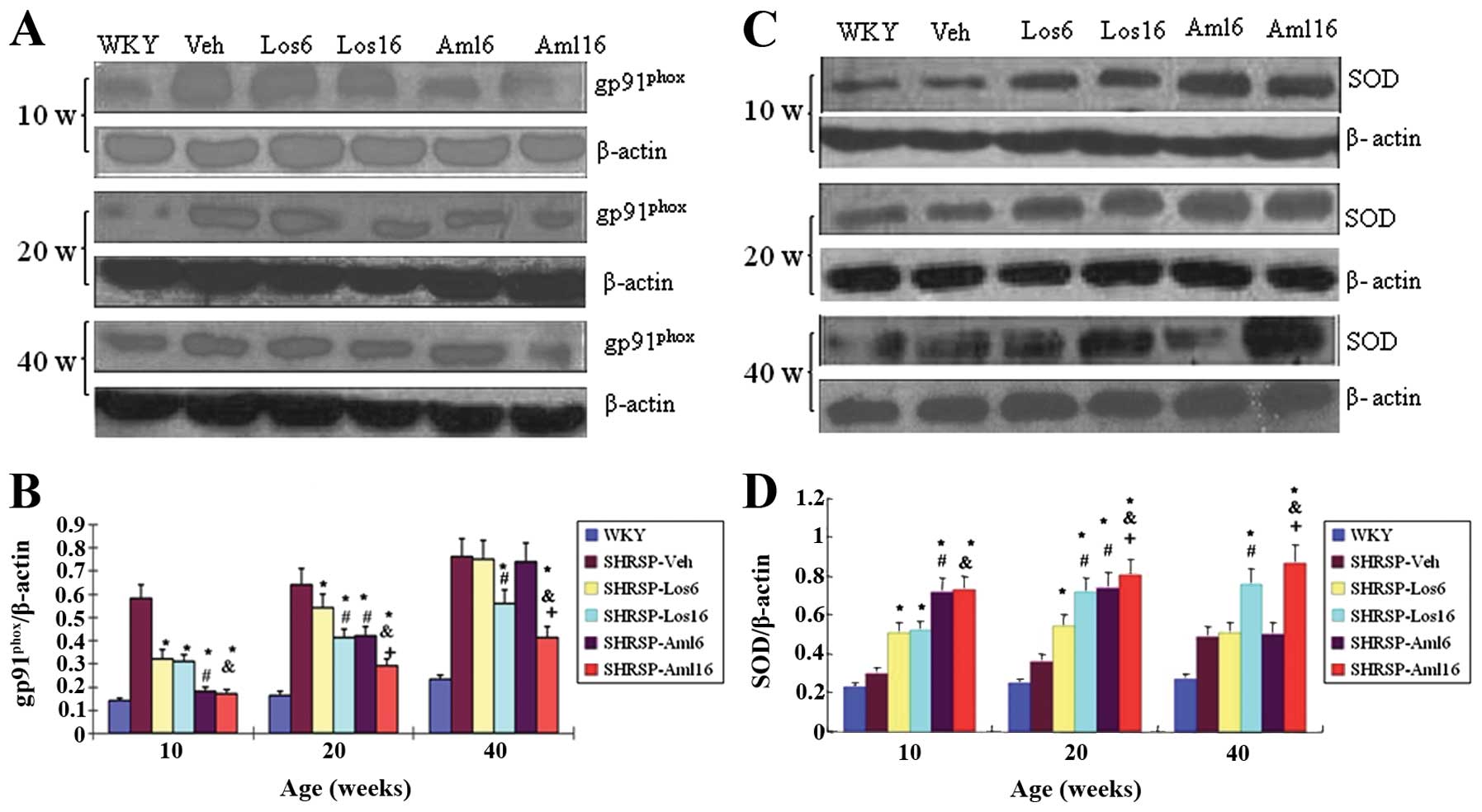
Peng F, Lin J, Lin L and Tang H: Transient
prehypertensive treatment in spontaneously hypertensive rats: A
comparison of losartan and amlodipine regarding long-term blood
pressure, cardiac and renal protection. Int J Mol Med.
30:1376–1386. 2012.
|
|
12
|
Vacher E, Richer C and Giudicelli JF:
Effects of losartan on cerebral arteries in stroke-prone
spontaneously hypertensive rats. J Hypertens. 14:1341–1348. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamori Y, Horie R, Akiguchi I, Kihara M,
Nara Y and Lovenberg W: Symptomatological classification in the
development of stroke in stroke-prone spontaneously hypertensive
rats. Jpn Circ J. 46:274–283. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu Y and Song W: Regulation of RCAN1
translation and its role in oxidative stress-induced apoptosis.
FASEB J. 27:208–221. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kishi T, Hirooka Y, Kimura Y, Ito K,
Shimokawa H and Takeshita A: Increased reactive oxygen species in
rostral ventrolateral medulla contribute to neural mechanisms of
hypertension in stroke-prone spontaneously hypertensive rats.
Circulation. 109:2357–2362. 2004. View Article : Google Scholar
|
|
16
|
Ito H, Torii M and Suzuki T: A comparative
study on lipid peroxidation in cerebral cortex of stroke-prone
spontaneously hypertensive and normotensive rats. Int J Biochem.
25:1801–1805. 1993.PubMed/NCBI
|
|
17
|
Yu L, Quinn MT, Cross AR and Dinauer MC:
Gp91(phox) is the heme binding subunit of the superoxide-generating
NADPH oxidase. Proc Natl Acad Sci USA. 95:7993–7998. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tang J, Liu J, Zhou C, et al: Role of
NADPH oxidase in the brain injury of intracerebral hemorrhage. J
Neurochem. 94:1342–1350. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fujii J and Taniguchi N: Down regulation
of superoxide dismutases and glutathione peroxidase by reactive
oxygen and nitrogen species. Free Radic Res. 31:301–308. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Phillips MI and de Oliveira EM: Brain
renin angiotensin in disease. J Mol Med (Berl). 86:715–722. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wright JW and Harding JW: The brain
renin-angiotensin system: a diversity of functions and implications
for CNS diseases. Pflugers Arch. 465:133–151. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gao L, Wang WZ, Wang W and Zucker IH:
Imbalance of angiotensin type 1 receptor and angiotensin II type 2
receptor in the rostral ventrolateral medulla: potential mechanism
for sympathetic overactivity in heart failure. Hypertension.
52:708–714. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takeda-Matsubara Y, Matsubara K, Ochi H,
Ito M, Iwai M and Horiuchi M: Expression of endothelial angiotensin
II receptor mRNA in pregnancy-induced hypertension. Am J Hypertens.
16:993–999. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ganten D, Marquez-Julio A, Granger P, et
al: Renin in dog brain. Am J Physiol. 221:1733–1737.
1971.PubMed/NCBI
|
|
25
|
Fischer-Ferraro C, Nahmod VE, Goldstein DJ
and Finkielman S: Angiotensin and renin in rat and dog brain. J Exp
Med. 133:353–361. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hamaguchi R, Takemori K, Inoue T, Masuno K
and Ito H: Short-term treatment of stroke-prone spontaneously
hypertensive rats with an AT1 receptor blocker protects against
hypertensive end-organ damage by prolonged inhibition of the
renin-angiotensin system. Clin Exp Pharmacol Physiol. 35:1151–1155.
2008. View Article : Google Scholar
|
|
27
|
Takemori K, Ishida H and Ito H: Continuous
inhibition of the renin-angiotensin system and protection from
hypertensive end-organ damage by brief treatment with angiotensin
II type 1 receptor blocker in stroke-prone spontaneously
hypertensive rats. Life Sci. 77:2233–2245. 2005. View Article : Google Scholar
|
|
28
|
Ichiki T: Regulation of angiotensin II
receptor expression. Curr Pharm Des. 19:3013–3021. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mogi M and Horiuchi M: Effect of
angiotensin II type 2 receptor on stroke, cognitive impairment and
neurodegenerative diseases. Geriatr Gerontol Int. 13:13–18. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Steckelings UM, Paulis L, Namsolleck P and
Unger T: AT2 receptor agonists: hypertension and beyond. Curr Opin
Nephrol Hypertens. 21:142–146. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Muradian K and Schachtschabel DO: The role
of apoptosis in aging and age-related disease: update. Z Gerontol
Geriatr. 34:441–446. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mattson MP: Apoptosis in neurodegenerative
disorders. Nat Rev Mol Cell Biol. 1:120–129. 2000. View Article : Google Scholar
|
|
33
|
Hamet P, Richard L, Dam TV, et al:
Apoptosis in target organs of hypertension. Hypertension.
26:642–648. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kannan K and Jain SK: Oxidative stress and
apoptosis. Pathophysiology. 7:153–163. 2000. View Article : Google Scholar
|