Introduction
Head and neck cancer (HNC) ranks as the 6th most
common type of cancer worldwide, with the vast majority being head
and neck squamous cell carcinomas (HNSCC) (1). Despite advances in diagnostic and
treatment methods over the past two decades, the overall survival
rate of HNSCC remains poor (5-year survival rate of ~50%) (2). Surgical resection is a commonly used
treatment for patients with HNSCC (3). However, tumor metastasis often
occurs after HNSCC surgery, and is the leading cause of death in
HNSCC patients (4). During cancer
resection, a number of factors may affect the risk of metastatic
recurrence. These factors include combinations of the surgery
per se, anesthetic drugs or techniques, acute pain and
opioid analgesia (5), suggesting
that anesthetic management may have the potential to minimize
cancer recurrence.
Balanced anesthesia (inhalational combined with
intravenous anesthesia) is the most widely used type of anesthesia
in head and neck tumor surgery (6). Compared with total intravenous
anesthesia, balanced anesthesia enables a better haemodynamic
stability during surgery and a faster and safer recovery of
consciousness after surgery (7),
which is particularly beneficial for elderly HNSCC patients
(8). However, the risks during
the surgery are often overlooked. Sevoflurane, a volatile
anesthetic agent that is widely used during HNSCC surgery. The
duration of oral cancer surgery is often >6 h for complete
resection of the primary tumor (9,10)
and flap reconstruction (11,12), which means that sevoflurane may
interact with the HNSCC cells for a considerable length of time.
However, the effect of sevoflurane on HNSCC cells remains unclear.
Therefore, the focus of the present study was the potential
interaction between HNSCC cells and the common inhalational
anaesthetic sevoflurane.
The effects of sevoflurane on HNSCC cell
proliferation, apoptosis and invasion were investigated using two
different types of HNSCC cells in an in vitro model, in
order to elucidate the molecular mechanism underlying the effects
of sevoflurane on HNSCC cells.
Materials and methods
Cell culture
The CAL-27 and FaDu HNSCC cell lines were obtained
from the Institutes of Biomedical Sciences, Fudan University
(Shanghai, China). The HNSCC cells were grown in Dulbecco's
modified Eagle's medium (DMEM) supplemented with 10% fetal bovine
serum (FBS) in a humidified atmosphere of 95% air and 5%
CO2 at 37°C. All experiments were performed with cells
in the logarithmic phase of growth.
Drugs
Sevoflurane was purchased from Maruishi
Pharmaceutical Co., Ltd. (Osaka, Japan). The hypoxia-inducible
factor-1α (HIF-1α) inhibitor YC-1 was purchased from Cayman
Chemical Co. (Ann Arbor, MI, USA). For in vitro studies,
YC-1 was dissolved in dimethyl sulfoxide (Sigma-Aldrich; Merck
KGaA, St. Louis, MO, USA) at the indicated concentrations.
Sevoflurane exposure
FaDu and CAL-27 cells were exposed to sevoflurane
in vitro according to the experimental protocol previously
described (13,14). Cell culture plates were placed in
an air-tight glass chamber with inflow and outflow connectors. The
chamber atmosphere was maintained continuously saturated with water
at 37°C. The entrance port of the chamber was connected to an
anesthetic machine (Cicero-EM 8060; Dräger, Lübeck, germany).
Sevoflurane was delivered into the chamber by a sevoflurane
vaporizer (Sevoflurane®; Abbott Laboratories, Abott
Park, IL, USA) attached to the anesthesia machine. A Datex infrared
gas analyser (Puritan-Bennett, Tewksbury, MA, USA) was used to
continuously monitor the delivered CO2, O2
and sevoflurane concentrations.
Cell survival analysis
The viability of CAL-27 and FaDu cells was evaluated
using the Cell Counting Kit-8 (CCK-8) assay. In brief, the cells
(5×103) were plated in 96-well cell culture plates in
DMEM with 10% FBS in a final volume of 0.1 ml. At 60% confluence,
the cells were treated with 2 and 4% sevoflurane for 2, 4, 6 and 8
h, then placed in a CO2 incubator for an additional 24-h
culture. Cell survival was assessed by addition of 10 µl
CCK-8 solution to 100 µl of medium for another 3 h in 37°C
prior to reading the absorbance at 450 nm using a Bio-Rad
microplate reader (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Three independent experiments were performed.
Apoptosis analysis by Annexin V/propidium
iodide (PI) flow cytometry
FaDu and CAL-27 cells were cultured in 6-well plates
(1×106 cells/well). After treatment with 2 and 4%
sevoflurane for 2, 4, 6 and 8 h, the cells were placed in a
CO2 incubator for an additional 24-h culture.
Thereafter, the apoptotic percentage of cells was measured by flow
cytometry analysis using an Annexin V-fluorescein isothiocyanate
(FITC) Apoptosis kit (Becton-Dickinson, Franklin Lakes, NJ, USA).
The cells were washed twice with cold phosphate-buffered saline
(PBS), and resuspended in 400 µl with 1X binding buffer at a
concentration of 1×106 cells/ml. This binding buffer was
supplemented with 5 µl of Annexin V-FITC and incubated at
room temperature in the dark for 15 min. PI (10 µl) was then
added and incubated at 4°C in the dark for 5 min. The cells were
then immediately analyzed with a flow cytometer (BD FACSCanto II;
BD Biosciences, Franklin Lakes, NJ, USA). All assays were repeated
at least three times.
Transwell invasion assay
FaDu cells were seeded in 24-well plates
(2×105 cells/well). After being exposed to different
concentrations of sevoflurane for 2, 4, 6 and 8 h, the cells were
placed in a CO2 incubator for an additional 24 h of
culture. Thereafter, the Transwell chambers, which incorporated a
polycarbonate filter membrane (diameter 6.5 mm, pore size 8
µm; Corning Costar, Corning, NY, USA), were used to evaluate
cell invasiveness. The polycarbonate filters at the bottom of the
Transwell chamber were coated with 100 µl Matrigel (BD
Biosciences) and air-dried in a laminar hood overnight. The cells
were harvested and then inoculated into the upper compartment of
the Transwell chambers (2×105 cells/well). DMEM with FBS
was added into the lower compartment (600 µl/well). The
cells were cultured at 37°C in 5% CO2 atmosphere for 24
h. Cells that did not penetrate the polycarbonate membrane at the
bottom of the chamber were gently wiped off using a cotton swab.
The membrane was then removed, fixed with 4% paraformaldehyde for
15 min and stained with 0.5% crystal violet. Five fields of vision
were randomly selected under a microscope (olympus IX51; olympus,
Tokyo, Japan), and the number of cells that penetrated the membrane
was counted.
Western blotting
FaDu cells were cultured in 6-well plate
(1×106 cells/well). After treatment with 2 and 4%
sevoflurane for 2, 4 and 8 h, the cells were placed in a
CO2 incubator for an additional 24-h culture.
Thereafter, the cell lysates were collected. The proteins were
quantified using a bicinchoninic acid assay kit (Pierce, Rockford,
IL, USA). The proteins (20 µg) were separated with 10%
SDS-PAGE gels and transferred onto polyvinylidene fluoride
membranes (EMD Millipore, Billerica, MA, USA). The membranes were
blocked with 5% skimmed milk and incubated overnight at 4°C with
primary antibodies: Anti-GAPDH (rabbit; 1:1,000; ab37168), HIF-1α
(mouse; 1:500; ab113642) and Bcl-2 (rabbit; 1:500; ab194583) were
all purchased from Abcam (Cambridge, UK); the Fas, anti-phospho-Akt
(Ser473; rabbit; 1:1,000; cat. no. 9271) and anti-Akt (rabbit;
1:1,000; cat. no. 9272) antibodies were all obtained from Cell
Signaling Technology, Inc. (Danvers, MA, USA). The immune complexes
were detected through incubation of the membrane with horseradish
peroxidase-conjugated goat anti-rabbit antibody (1:200; cat. no.
111-035-003) or goat anti-mouse antibody (1:200; cat. no.
115-035-003) (both from Jackson ImmunoResearch Laboratories, Inc.,
West Grove, PA, USA) for 1 h at room temperature and subsequent
exposure of the membrane to enhanced chemiluminescence reagents
(EMD Millipore).
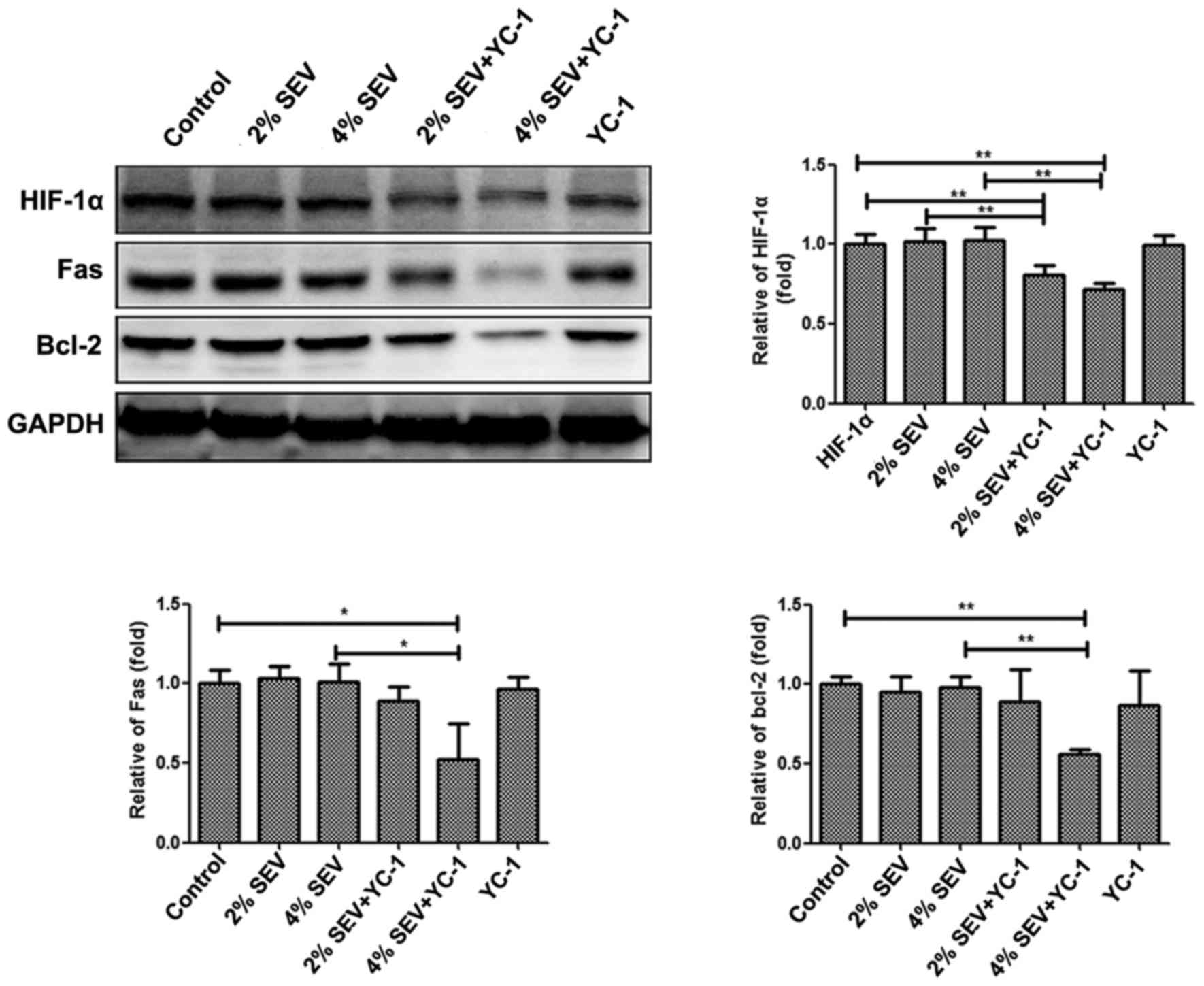
HIF-1α inhibitor treatment
To investigate the effect of YC-1 (HIF-1α inhibitor)
on sevoflurane-mediated apoptosis, FaDu cells were pretreated with
100 µM YC-1 for 8 h prior to exposing the cells to 2 and 4%
sevoflurane for 4 h. The protein expression levels of HIF-1α, Fas
and Bcl-2 were detected at 24 h post-sevoflurane treatment by
western blotting.
Statistical analysis
All data are presented as the mean ± standard error
of the mean. Data were examined using an analysis of variance and
the least significant differences method for multi-sample
comparisons. P<0.05 was considered to indicate statistically
significant differences.
Results
Sevoflurane inhibits HNSCC cell
survival
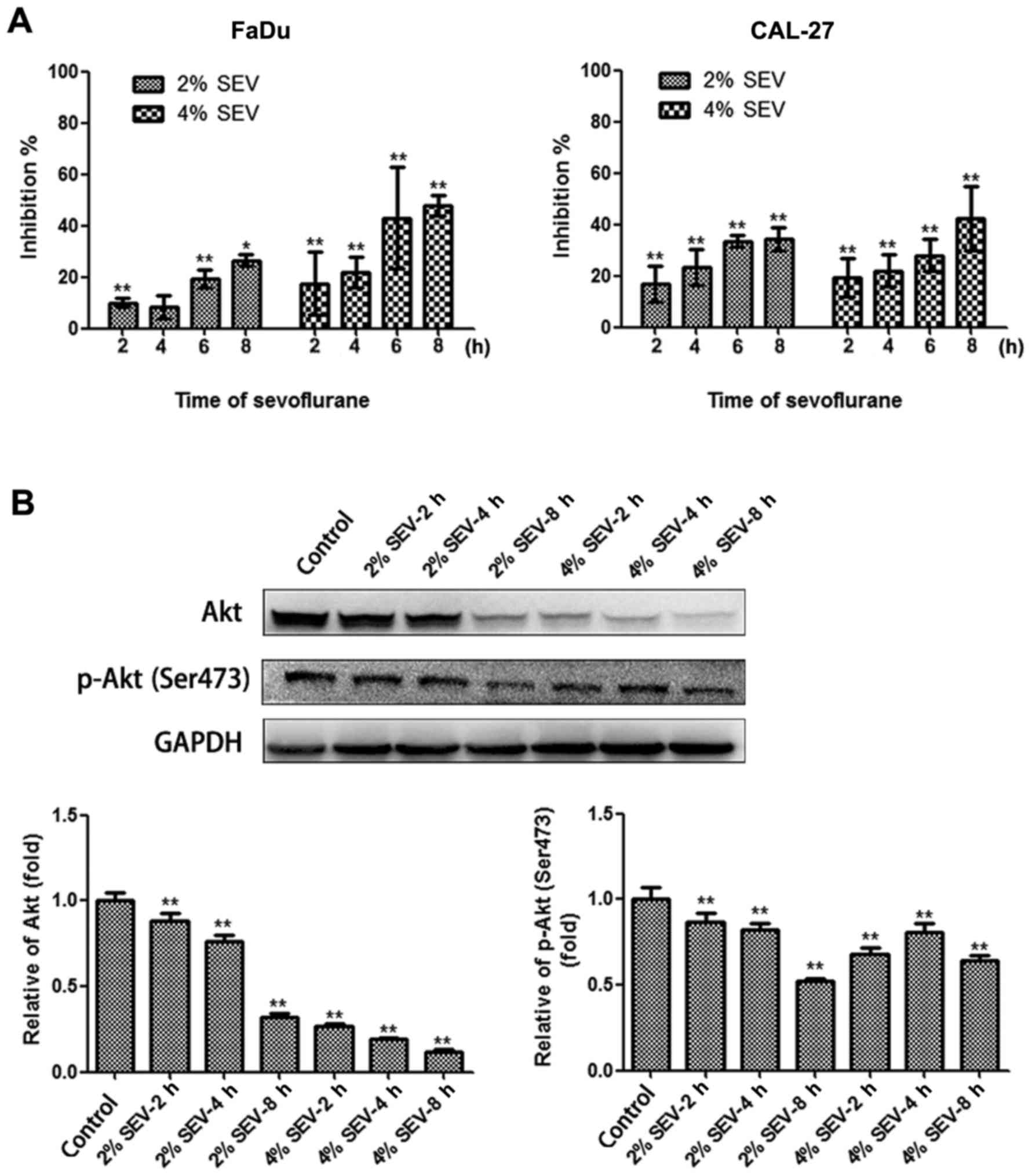
In order to determine the antiproliferative potency
of single exposure of human HNSCC cells to sevoflurane, the CCK-8
assay was performed. Both the FaDu and CAL-27 cell lines exhibited
growth alterations following a single exposure to 2 and 4%
sevoflurane. Our data demonstrated that the incubation of FaDu and
CAL-27 cells with sevoflurane resulted in a time- and
concentration-dependent elevation of cell inhibition (Fig. 1A).
Subsequently, the mechanisms underlying the
reduction in cell proliferation caused by sevoflurane were
investigated. It was previously suggested that the p-Akt levels
were increased in response to isoflurane, which was associated with
enhanced renal cancer growth and malignant potential (15). Therefore, the total and p-Akt
levels in FaDu cells treated with various concentrations and action
times of sevoflurane were evaluated by western blotting. A marked
downregulation of both total and p-Akt levels was observed in FaDu
cells (Fig. 1B).
Sevoflurane induces apoptosis of HNSCC
cells
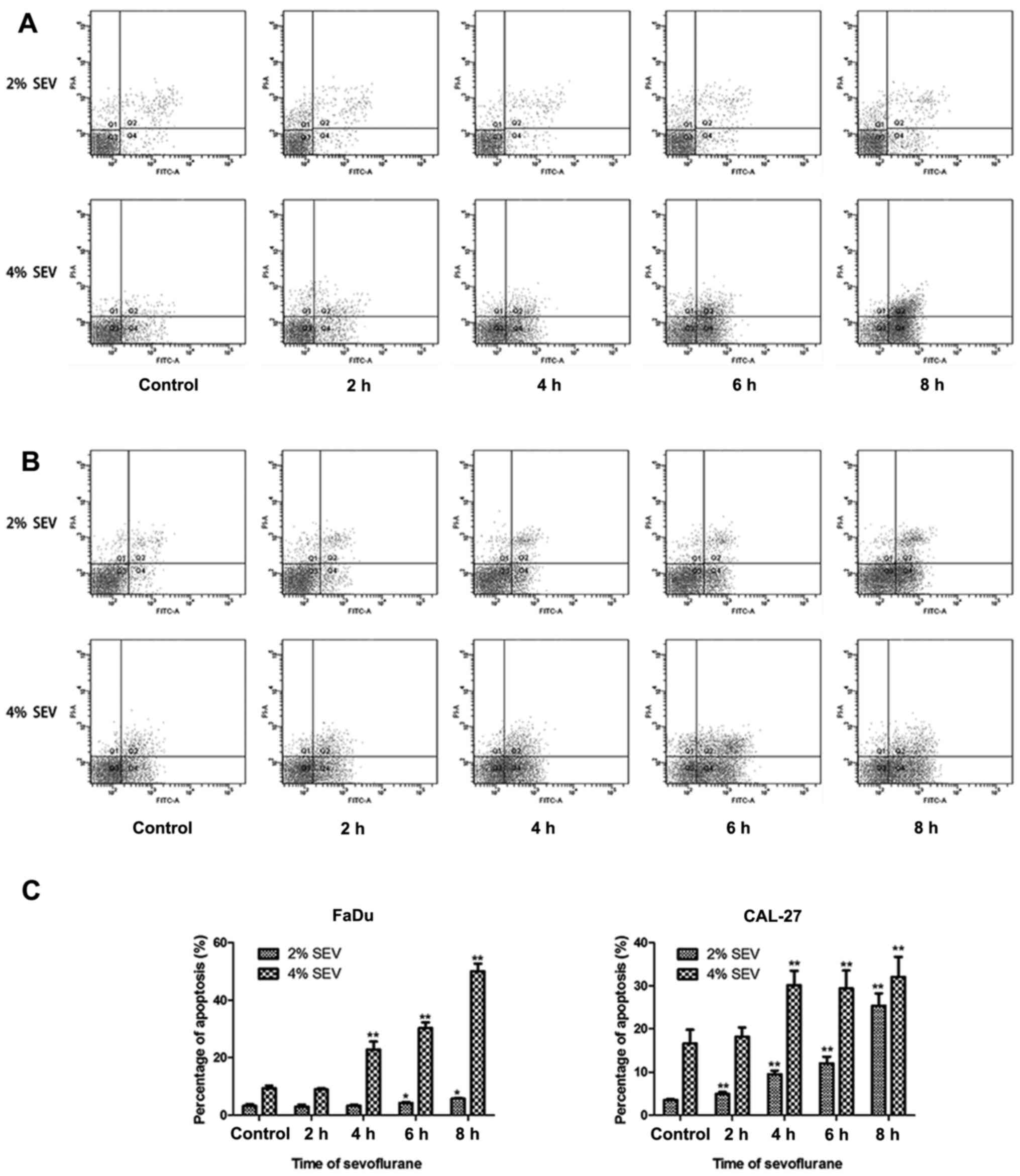
To investigate the apoptosis percentage, the cells
were treated with 2 and 4% sevoflurane for 2, 4, 6 and 8 h, and the
percentage of apoptotic cells was measured by flow cytometry. As
shown in Fig. 2, the ratio of
early apoptosis was 3.2% in the non-treated control FaDu cells and
3.5% in the non-treated control CAL-27 cells. Following sevoflurane
treatment, the ratio of apoptotic cells increased in both cell
lines (Fig. 2A and B). The effect
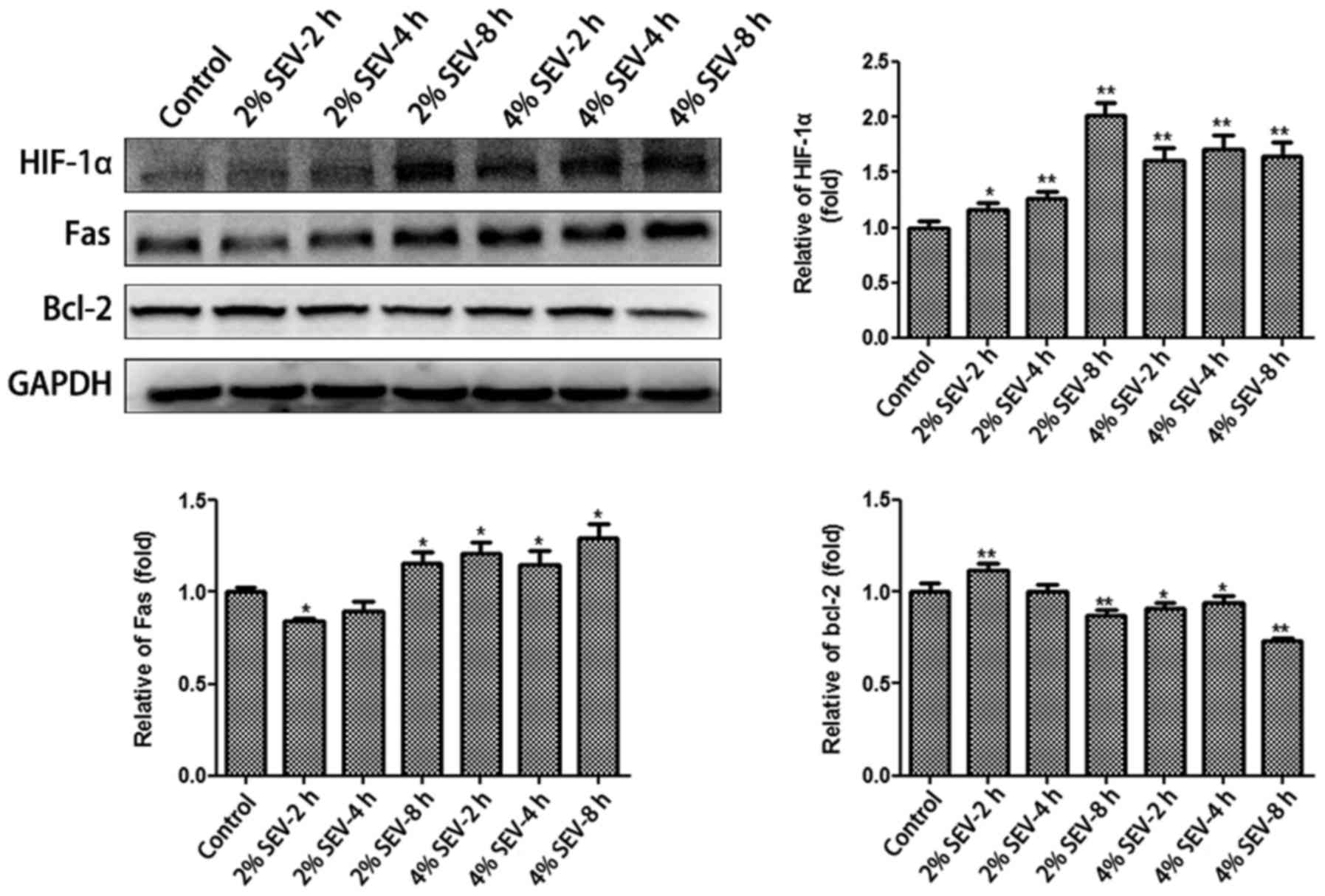
of sevoflurane-induced FaDu and CAL-27 cell apoptosis was
concentration- and time-dependent. Moreover, the results were
further confirmed by detection of the protein levels of Fas and
Bcl-2 in FaDu cells. As shown in Fig.
4, western blotting revealed that the expression of Fas was
significantly increased following sevoflurane treatment,
particularly with 2 or 4% sevoflurane for 8 h. Furthermore, the
expression of Bcl-2 was downregulated when the cells were exposed
to 2 and 4% sevoflurane for 8 h (Fig.
4).
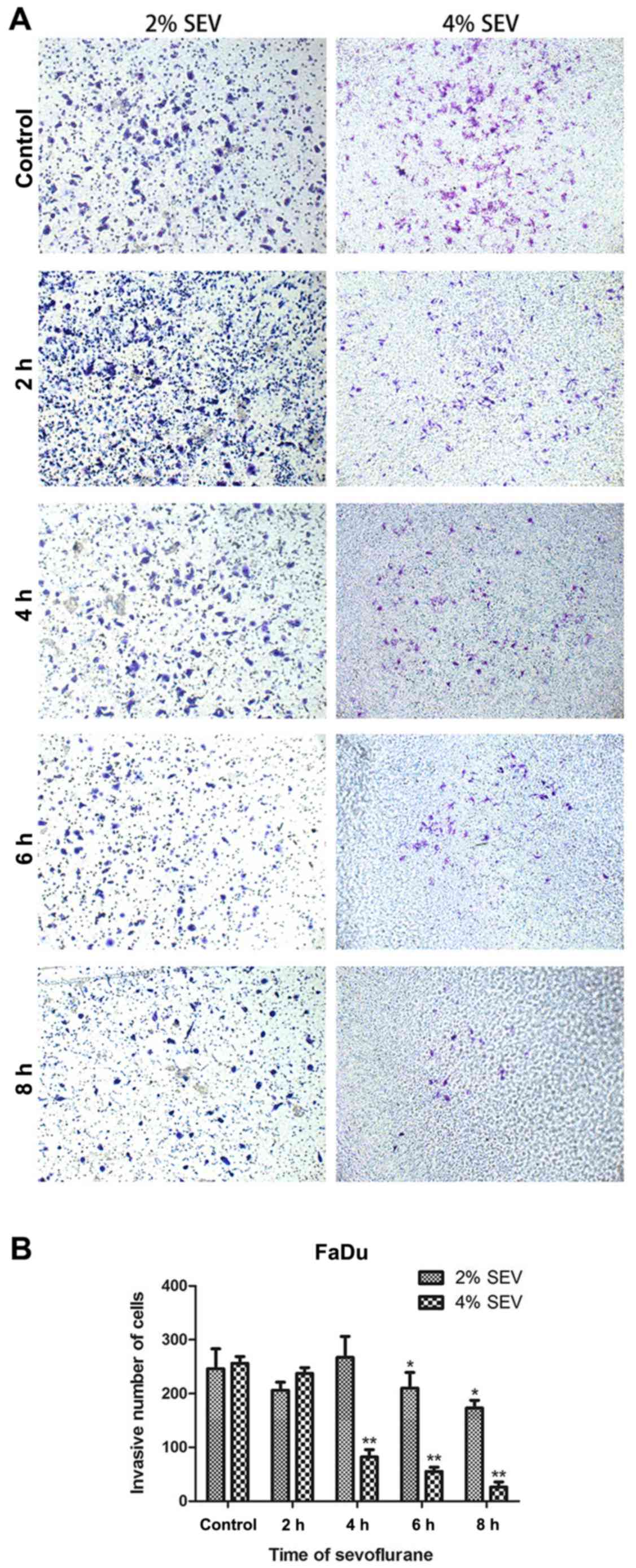
Sevoflurane inhibits FaDu cell
invasion
To investigate the effect of sevoflurane on the
invasion of FaDu cells, the effect of sevoflurane on the invasive
ability of cancer cells was evaluated by an invasion assay using a
BioCoat Matrigel Invasion Chamber kit in vitro. The number
of invading FaDu cells was significantly decreased at 6 and 8 h in
the groups treated with 2% sevoflurane compared with that in the
control group (number of invading cells: 246±37 in controls,
210±29.3 with 2% sevoflurane for 6 h and 173±14.6 with 2%
sevoflurane for 8 h) (Fig. 3A and
B). There was a significant difference at 4 h between the
groups treated with 4% sevoflurane and the control group (number of
invading cells: 256±12.8 in controls, 82±13.8 with 4% sevoflurane
for 4 h, 55±8.2 with 4% sevoflurane for 6 h and 26±9.8 with 4%
sevoflurane for 8 h) (Fig. 3A and
B). These results demonstrated that sevoflurane decreased cell
invasion in the FaDu cell line.
Sevoflurane induces HIF-1α expression in
a time- and concentration-dependent manner
To evaluate the effect of sevoflurane on HIF-1α
protein expression, FaDu cells were exposed to 2 and 4% sevoflurane
for 2, 4 and 8 h, and were then harvested for immunoblotting after
24 h of incubation. Immunoblotting data revealed a significant
increase in HIF-1α protein levels in a time- and
concentration-dependent manner when cells were exposed to 2 and 4%
sevoflurane (Fig. 4).
Effect of the HIF-1α inhibitor YC-1 on
the sevoflurane-induced apoptosis signaling pathway
To further explore whether the sevoflurane
upregulation of Fas expression occurred via activating the HIF-1α
signaling pathway, FaDu cells were pretreated with the HIF-1α
inhibitor YC-1 (100 µM) for 8 h prior to exposing the cells
to 2 and 4% sevoflurane for 4 h. The western blotting results
revealed that the combination treatment of YC-1 with 2 and 4%
sevoflurane was able to downregulate the level of HIF-1α and
inhibit the expression of Fas more effectively compared with
sevoflurane treatment or YC-1 treatment alone; however, there was
no obvious effect of YC-1 on Bcl-2 (Fig. 5). The results suggested that
increased Fas expression was partly associated with activation of
the HIF-1α pathway.
Discussion
Whether the anesthetic procedures affect the outcome
after cancer surgery has been a research focus. Retrospective data
have demonstrated that the choice of anaesthesia technique for
cancer surgery may affect the risk of cancer recurrence and
metastasis (4,16-18). Sevoflurane as an inhalational
anesthetic that is extensively used during HNSCC surgery as
anesthesia maintenance or induction. However, the risks during the
operative period are often overlooked. The duration of oral cancer
surgery is often >6 h, and during this time the effect of
sevoflurane on tumor cells is unknown. It has been reported that
sevoflurane may induce T-lymphocyte (19), H4 human neuroglioma cell (20) and Jurkat T cell (21) apoptosis. Moreover, the anticancer
effect of sevoflurane has been previously reported. In vitro
studies demonstrated that sevoflurane exerted an inhibitory effect
on growth and promoted apoptosis of SW620 colon cancer (22), Caco-2 laryngeal cancer (23) and A549 lung adenocarcinoma cells
(24). However, the effect of
sevoflurane on the proliferation, apoptosis, cell cycle, migration
and invasion of HNSCC cells remains unclear, and the underlying
molecular mechanisms require further elucidation.
In the present study, the effect of clinically
relevant concentrations of sevoflurane on HNSCC cells was examined.
FaDu and CAL-27 are two widely used HNSCC cell lines. Sevoflurane
obviously affected the viability of FaDu and CAL-27 cells in
vitro (Fig. 1A). Upon
investigating the mechanisms underlying the reduction in cell
proliferation caused by sevoflurane, it was observed that Akt and
p-Akt (Ser473) were inhibited by sevoflurane treatment. Thus, it
was hypothesized that sevoflurane exerts its the antitumor effect
partially through the PI3K̸Akt pathway.
The molecular mechanism of apoptosis induction in
HNSCC cells after a single exposure to sevoflurane in clinically
useful concentrations was also investigated. Under our experimental
conditions, the ratio of apoptotic cells significantly increased in
both the FaDu and CAL-27 cell lines. Fas and its ligand, FasL, are
cell surface receptors that belong to the tumor necrosis factor
receptor family. Interaction of the Fas receptor on cells with FasL
results in ligand-mediated cell death (25-28). Fas-mediated cell death has also
been implicated in the regulation of tumor development, growth and
progression. Downregulation of Fas or impaired Fas signaling have
been correlated with tumor progression (27,29-32). Bcl-2 is an anti-apoptotic member
of the Bcl-2 family, which prevents apoptosis by inhibiting the
release of mitochondrial apoptogenic factors into the cytoplasm
(33). In the present study, the
data demonstrated that sevoflurane upregulated the levels of Fas
and downregulated the levels of Bcl-2 in FaDu cells. In addition,
it was observed that HIF-1α was noticeably increased when the cells
were exposed to sevoflurane. HIF-1α is a dimeric transcription
factor that mediates various cellular responses to hypoxia and may
be upregulated by sevoflurane and isoflurane (34-37). Furthermore, the increase in the
level of Fas was abolished when cells were pretreated with the
HIF-1α inhibitor YC-1 (Fig. 5).
There was no change in Bcl-2 when YC-1 was used. These findings
suggest that sevoflurane-mediated cell apoptosis was associated
with activation of the Fas/FasL signaling pathway, which may be
regulated by HIF-1α.
The development of cancer invasion is a complex
cascade of events involving tumor dissemination from the primary
site to distant organs. During this process, the degradation of
extracellular matrix, which poses a biochemical and mechanical
barrier to cell movement, has been shown to be an important
biological process in the metastasis of cancer cells (38,39). Recent research reported that
sevoflurane may attenuate the migration and invasion in U87MG
glioma cells (40) and Lovo colon
cancer cells (41) in
vitro. In the present study, exposure to sevoflurane at
clinically relevant concentrations significantly inhibited the
invasion of FaDu cells (Fig. 3).
However, cancer metastasis is not only regulated by the direct
effects of the general anesthetic on the tumor cells, but is also
affected by the effects of the anesthetic on immune cells (42).
In conclusion, the results of the present study
demonstrated that sevoflurane inhibited proliferation, invasion and
migration, and induced apoptosis in HNSCC cells. Moreover, the
results of the study indicated that the antiproliferative effect of
sevoflurane was associated with downregulating the expression of
p-Akt (Ser473), and that the resulting cell apoptosis was
associated with activation of the Fas/FasL signaling pathway, which
may be regulated by HIF-1α. Finally, some potential limitations of
the present study should be mentioned: In vivo research
should also be conducted to veify the findings of the present
study, as it more accurately simulates the tumor environment and
provides more objective results of tumor growth; the molecular
mechanism of the effect sevoflurane on HNSCC should also be fully
elucidated to reach definitive conclusions.
Acknowledgments
The present study is supported by the '2016 Shanghai
Outstanding Academic Leaders Plan of the Shanghai Science and
Technology Committee' (grant no. 16XD1401800).
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fuller CD, Wang SJ, Thomas CR Jr, Hoffman
HT, Weber RS and Rosenthal DI: Conditional survival in head and
neck squamous cell carcinoma: results from the SEER dataset
1973-1998. Cancer. 109:1331–1343. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kalavrezos N and Bhandari R: Current
trends and future perspectives in the surgical management of oral
cancer. Oral oncol. 46:429–432. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Niwa H, Rowbotham DJ, Lambert DG and Buggy
DJ: Can anesthetic techniques or drugs affect cancer recurrence in
patients undergoing cancer surgery? J Anesth. 27:731–741. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Snyder GL and Greenberg S: Effect of
anaesthetic technique and other perioperative factors on cancer
recurrence. Br J Anaesth. 105:106–115. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
López Correa T, Sánchez Hernández MV, Briz
Sánchez E and Estévez Amores FI: Anesthesia in head and neck
paragangliomas. Acta Otorrinolaringol Esp. 60(Suppl 1): 76–79.
2009.In Spanish.
|
|
7
|
Juckenhöfel S, Feisel C, Schmitt HJ and
Biedler A: TIVA with propofol-remifentanil or balanced anesthesia
with sevoflurane-fentanyl in laparoscopic operations. Hemodynamics,
awakening and adverse effects. Anaesthesist. 48:807–812. 1999.In
German. View Article : Google Scholar
|
|
8
|
Jun R, Gui-he Z, Xing-xing S, Hui Z and
Li-xian X: Isoflurane enhances malignancy of head and neck squamous
cell carcinoma cell lines: a preliminary study in vitro. Oral
Oncol. 47:329–333. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saunders MI and Rojas AM: Management of
cancer of the head and neck - a cocktail with your PORT? N Engl J
Med. 350:1997–1999. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vartanian JG, Carvalho AL, Carvalho SM,
Mizobe L, Magrin J and Kowalski LP: Pectoralis major and other
myofascial/myocutaneous flaps in head and neck cancer
reconstruction: experience with 437 cases at a single institution.
Head Neck. 26:1018–1023. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Spriano G, Pellini R and Roselli R:
Pectoralis major myocutaneous flap for hypopharyngeal
reconstruction. Plast Reconstr Surg. 110:1408–1413. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Engroff SL: Fibula flap reconstruction of
the condyle in disarticulation resections of the mandible: a case
report and review of the technique. Oral Surg oral Med Oral Pathol
Oral Radiol Endod. 100:661–665. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang L, Zhang J, Yang L, Dong Y, Zhang Y
and Xie Z: Isoflurane and sevoflurane increase interleukin-6 levels
through the nuclear factor-kappa B pathway in neuroglioma cells. Br
J Anaesth. 110(Suppl 1): i82–i91. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sun Y, Li QF, Zhang Y, Hu R and Jiang H:
Isoflurane preconditioning increases survival of rat skin
random-pattern flaps by induction of HIF-1α expression. Cell
Physiol Biochem. 31:579–591. 2013. View Article : Google Scholar
|
|
15
|
Benzonana LL, Perry NJ, Watts HR, Yang B,
Perry IA, Coombes C, Takata M and Ma D: Isoflurane, a commonly used
volatile anesthetic, enhances renal cancer growth and malignant
potential via the hypoxia-inducible factor cellular signaling
pathway in vitro. Anesthesiology. 119:593–605. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Heaney A and Buggy DJ: Can anaesthetic and
analgesic techniques affect cancer recurrence or metastasis? Br J
Anaesth. 109(Suppl 1): i17–i28. 2012. View Article : Google Scholar
|
|
17
|
Exadaktylos AK, Buggy DJ, Moriarty DC,
Mascha E and Sessler DI: Can anesthetic technique for primary
breast cancer surgery affect recurrence or metastasis?
Anesthesiology. 105:660–664. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Biki B, Mascha E, Moriarty DC, Fitzpatrick
JM, Sessler DI and Buggy DJ: Anesthetic technique for radical
prostatectomy surgery affects cancer recurrence: a retrospective
analysis. Anesthesiology. 109:180–187. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Loop T, Scheiermann P, Doviakue D,
Musshoff F, Humar M, Roesslein M, Hoetzel A, Schmidt R, Madea B,
Geiger KK, et al: Sevoflurane inhibits
phorbol-myristate-acetate-induced activator protein-1 activation in
human T lymphocytes in vitro: potential role of the p38-stress
kinase pathway. Anesthesiology. 101:710–721. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dong Y, Zhang G, Zhang B, Moir RD, Xia W,
Marcantonio ER, Culley DJ, Crosby G, Tanzi RE and Xie Z: The common
inhalational anesthetic sevoflurane induces apoptosis and increases
beta-amyloid protein levels. Arch Neurol. 66:620–631. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Roesslein M, Frick M, Auwaerter V, Humar
M, Goebel U, Schwer C, Geiger KK, Pahl HL, Pannen BH and Loop T:
Sevoflurane-mediated activation of p38-mitogen-activated stress
kinase is independent of apoptosis in Jurkat T-cells. Anesth Analg.
106:1150–1160. 2008. View Article : Google Scholar
|
|
22
|
Kvolik S, Glavas-Obrovac L, Bares V and
Karner I: Effects of inhalation anesthetics halothane, sevoflurane,
and isoflurane on human cell lines. Life Sci. 77:2369–2383. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kvolik S, Dobrosevic B, Marczi S, Prlic L
and Glavas-Obrovac L: Different apoptosis ratios and gene
expressions in two human cell lines after sevoflurane anaesthesia.
Acta Anaesthesiol Scand. 53:1192–1199. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liang H, Gu MN, Yang CX, Wang HB, Wen XJ
and Zhou QL: Sevoflurane inhibits proliferation, induces apoptosis,
and blocks cell cycle progression of lung carcinoma cells. Asian
Pac J Cancer Prev. 12:3415–3420. 2011.PubMed/NCBI
|
|
25
|
Owen-Schaub L, Chan H, Cusack JC, Roth J
and Hill LL: Fas and Fas ligand interactions in malignant disease.
Int J oncol. 17:5–12. 2000.PubMed/NCBI
|
|
26
|
Nagata S: Apoptosis by death factor. Cell.
88:355–365. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Owen-Schaub LB, van Golen KL, Hill LL and
Price JE: Fas and Fas ligand interactions suppress melanoma lung
metastasis. J Exp Med. 188:1717–1723. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Algeciras-Schimnich A, Shen L, Barnhart
BC, Murmann AE, Burkhardt JK and Peter ME: Molecular ordering of
the initial signaling events of CD95. Mol Cell Biol. 22:207–220.
2002. View Article : Google Scholar
|
|
29
|
Möller P, Koretz K, Leithäuser F,
Brüderlein S, Henne C, Quentmeier A and Krammer PH: Expression of
APo-1 (CD95), a member of the NGF/TNF receptor superfamily, in
normal and neoplastic colon epithelium. Int J Cancer. 57:371–377.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hill LL, Ouhtit A, Loughlin SM, Kripke ML,
Ananthaswamy HN and Owen-Schaub LB: Fas ligand: a sensor for DNA
damage critical in skin cancer etiology. Science. 285:898–900.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zörnig M, Grzeschiczek A, Kowalski MB,
Hartmann KU and Möröy T: Loss of Fas/Apo-1 receptor accelerates
lymphomagenesis in E mu L-MYC transgenic mice but not in animals
infected with MoMuLV. Oncogene. 10:2397–2401. 1995.PubMed/NCBI
|
|
32
|
Gordon N and Kleinerman ES: The role of
Fas/FasL in the metastatic potential of osteosarcoma and targeting
this pathway for the treatment of osteosarcoma lung metastases.
Cancer Treat Res. 152:497–508. 2009. View Article : Google Scholar
|
|
33
|
Leber B, Geng F, Kale J and Andrews DW:
Drugs targeting Bcl-2 family members as an emerging strategy in
cancer. Expert Rev Mol Med. 12:e282010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gong JS, Yao YT, Fang NX and Li LH:
Sevoflurane postconditioning attenuates reperfusion-induced
ventricular arrhythmias in isolated rat hearts exposed to
ischemia/reperfusion injury. Mol Biol Rep. 39:6417–6425. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wang JK, Yu LN, Zhang FJ, Yang MJ, Yu J,
Yan M and Chen G: Postconditioning with sevoflurane protects
against focal cerebral ischemia and reperfusion injury via PI3K/Akt
pathway. Brain Res. 1357:142–151. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li QF, Zhu YS and Jiang H: Isoflurane
preconditioning activates HIF-1alpha, iNOS and Erk1/2 and protects
against oxygen-glucose deprivation neuronal injury. Brain Res.
1245:26–35. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li QF, Wang XR, Yang YW and Su DS:
Up-regulation of hypoxia inducible factor 1alpha by isoflurane in
Hep3B cells. Anesthesiology. 105:1211–1219. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
McCawley LJ and Matrisian LM: Matrix
metalloproteinases: multifunctional contributors to tumor
progression. Mol Med Today. 6:149–156. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sternlicht MD and Werb Z: How matrix
metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol.
17:463–516. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hurmath FK, Mittal M, Ramaswamy P,
Umamaheswara Rao QS and Dalavaikodihalli Nanjaiah N: Sevoflurane
and thiopental preconditioning attenuates the migration and
activity of MMP-2 in U87MG glioma cells. Neurochem Int. 94:32–38.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Xu YJ, Li SY, Cheng Q, Chen WK, Wang SL,
Ren Y and Miao CH: Effects of anaesthesia on proliferation,
invasion and apoptosis of Lovo colon cancer cells in vitro.
Anaesthesia. 71:147–154. 2016. View Article : Google Scholar
|
|
42
|
Gottschalk A, Sharma S, Ford J, Durieux ME
and Tiouririne M: The role of the perioperative period in
recurrence after cancer surgery (Review). Anesth Analg.
110:1636–1643. 2010. View Article : Google Scholar : PubMed/NCBI
|