Introduction
Stroke, following coronary heart disease and cancer,
is the third most common cause of mortality in numerous countries
(1), and it has become an
enormous health issue globally (2). In China, stroke is one of the most
common causes of mortality and long-term disability in previous
years (3,4). More than 10 million Chinese
individuals are living with stroke, with 2.4 million novel cases
reported in 2013 (5). Acute
ischemic stroke is the most common type of stroke, which accounts
for 60-80% of all cases (6). To
date, antiplatelet agents and thrombolytic medications are the only
drug treatment options of ischemic strokes that are supported by
strong clinical evidence (7).
However, the applications of these two treatments are often limited
by the potential risk of cerebral bleeding and a narrow treatment
time window. The percentage of patients with ischemic stroke who
are receiving thrombolytic therapy is no more than 3.5% in the
United States (8) and only 1 to
3% in China (9). Overall, there
remains a very limited number of effective interventions for
ischemic stroke following decades of practice and investigation.
Therefore, it is necessary to further investigate feasible and
effective treatment options.
Hypoxia-inducible factor-1α (HIF-1α) serves an
important function in the cellular adaptation to hypoxia (10). HIF-1α is tightly regulated by
oxygen tension (11). Under
normoxia, HIF-1α is ubiquitinated and degraded by
prolyl-hydroxylases (12). Under
hypoxic conditions, HIF-1α is stabilized and translocated to the
nucleus where it dimerizes with HIF-1β, the other subunit of HIF-1,
and activates the transcription of its target genes involved in
survival in hypoxia (11). HIF-1
is able to induce the transcription of erythropoietin (EPO) and
vascular endothelial growth factor (VEGF) (13). These responses increase oxygen
supply to oxygen-deprived tissues by promoting erythropoiesis and
angiogenesis. A continuous supply of oxygen to the central nervous
system (CNS) is extremely important for maintaining normal brain
function. It is vital that neurons in the CNS are able to detect
and respond rapidly to brain hypoxia (13). It has been reported that hypoxic
preconditioning increases tolerance to hypoxic-ischemic-induced
brain injury and decreases apoptosis by upregulating the expression
of HIF-1α (14). Furthermore,
hypoxic preconditioning in transplanted bone marrow stromal cells
promoted their capability of regeneration and therapeutic potential
to treat rat ischemic stroke (15).
EPO, a target gene of HIF-1, is a glycoprotein
hormone that consists of a single polypeptide consisting of 166
amino acids folded into four α-helices (16). EPO production was revealed to be
induced by hypoxia in a murine brain, uterus and kidney (17). EPO administration protected
embryonic neurons and postnatal hippocampal neurons against cell
death induced by hypoxia (18).
In neonatal rats, delayed EPO administration stimulated
oligodendrogenesis and attenuated white matter damage in
hypoxic/ischemic brain injury (19). Furthermore, EPO attenuated
inflammatory response by decreasing cyclooxygenase 2 and inducible
nitric oxide synthase, suppressing microglial activation and
inhibiting autophagy activation in burn-induced motor neuron
neuroinflammation (20).
However, to the best of our knowledge, there are no
reports available concerning the effect of exogenous HIF-1α in
ischemic stroke models at present. Furthermore, there are also no
reports to the best of our knowledge concerning the effects of EPO
induced by exogenous HIF-1α on neuronal apoptosis following
cerebral ischemic stroke.
In the present study, a recombinant adenovirus
engineered to express HIF-1α (Ad-HIF-1α) was used to treat a
transient middle cerebral artery occlusion (tMCAO) rat model. The
aim of the present study was to investigate whether HIF-1α may
decrease neuronal apoptosis by inducing EPO.
Materials and methods
Ethics
The present study followed all guidelines stated in
Guide for the Care and Use of Laboratory Animals, prepared by the
Committee on Care and Use of Laboratory Animals of the Institute of
Laboratory Animal Resources Commission on Life Sciences (National
Research Council, China; 1996). The animal studies were ethically
approved by the local Animal Experimentation Ethics Committee
(Guizhou Provincial People's Hospital, Guizhou, China) for animal
experimentation. All efforts were made to minimize the number of
rats used and their suffering.
Transient focal cerebral ischemia rat
model
A rat model was produced as previously described
(21). A total of 32 male
Sprague-Dawley rats weighing 230-250 g purchased from Guizhou
Medical University were used in this study. Rats were housed
individually and had ad libitum access to food and water.
The temperature in the room was 25°C and the room was under the
condition of a 12-h light-dark cycle. Rats were initially
anesthetized with 0.05 mg/g ketamine followed by administration of
0.01 mg/g xylazine intraperitoneally. Oxygen was supplied through a
face mask during surgery. tMCAO was induced by following the method
of intraluminal vascular occlusion. Briefly, the right external
carotid artery (ECA), common carotid artery and internal carotid
artery (ICA) were isolated. A 4-0 nylon suture with a 3 cm length
and a slightly enlarged and rounded tip was inserted from the ECA
into the lumen of the ICA to block the origin of the MCA. The
distance was 18.5 to 19.5 mm from the tip of the suture to the
bifurcation of the common carotid artery. Following 60 min of MCAO,
reperfusion was performed by withdrawal of the suture until the tip
cleared the lumen of the ECA. In the sham group, the rats underwent
identical procedures without the insertion of the nylon
monofilament.
Treatments for rats
Rats were treated as previously described (22,23). A recombinant adenovirus carrying
the HIF-1α gene and the green fluorescent protein gene (Ad-HIF-1α)
was constructed using the AdEasy® System (American Type
Culture Collection). Previous studies have reported that the
recombinant adenovirus is able to stably express HIF-1α in neural
stem cells and differentiated derivatives (24,25).
At 1 h subsequent to MCAO, the rats were randomly
divided into four groups (n=8): Sham group, ischemia+Ad (Ad group),
ischemia+Ad-HIF-1α (Ad-HIF-1α group) and ischemia+Ad-HIF-1α+
erythropoietin mimetic peptide-9 (EMP-9) (Ad-HIF-1α+EMP-9 group).
Animals were anesthetized with equithesin (3 ml/kg administered
intraperitoneally) and transferred to a stereotaxic apparatus. A 2
to 5 mm incision was created in the scalp, 1.5 mm lateral to the
bregma, under an aseptic technique. By using a dental drill, a burr
hole was produced in the bone 3 mm lateral to bregma. Approximately
10 µl Ad, 10 µl Ad-HIF-1α or 10 µl Ad-HIF-1α
were slowly injected into the ischemic area at a depth of 2.0 mm
from the surface of the brain over 20 min. Prior to retraction, the
needle was maintained in the brain for an additional 5 min. To
inhibit EPO-receptor (-R) functions, rats in the Ad-HIF-1α+EMP-9
group received an intraperitoneal injection of EMP-9 (cat. no.
MBS8243539; MyBioSource, Inc.), a proven EPO-R antagonist, at 1.0
mg/time, four times at 1 h intervals per day from day 1 to day 7
following tMCAO. The EMP-9 was dissolved in 1X phosphate buffered
saline (PBS) at a final concentration of 1 mg/ml. Rats in the other
two groups (the Ad group and Ad-HIF-1α group) received equal volume
injections of PBS. Body temperature during surgery was controlled
with a thermostatically regulated heating pad at 37.0±0.5°C and was
monitored by a rectal thermometer. Rats were returned to their
cages on the warm pad and allowed to recover from anesthesia
following surgery. Agar chow instead of solid chow was used as the
rats experienced hemiplegia and hemidysesthesia following MCAO.
Humane endpoints of the study included major changes in body
weight, external physical appearance, behavior and physiological
measures (e.g., body temperature, hormonal fluctuations, clinical
pathology). A total of three rats were lost to intracerebral
hemorrhage four rats were lost to fever. Extra rat(s) were added to
the groups where necessary to ensure 8 rats/group.
Behavioral testing
A modified neurological severity score (NSS)
assessment was performed on days 0, 1, 3, 5 and 7 following tMCAO
by a well-trained researcher who was blinded to the study
conditions. The NSS assessment consisted of motor (muscle status
and abnormal movement), sensory (visual, tactile and
proprioceptive), reflex and balance tests as described previously
(26). Neurological function was
graded on a scale of 0 to 18 (normal score, 0; maximum deficit
score, 18). A higher score indicated a more severe injury.
Histological analysis
On day 7 following ischemia, four rats from each
group were sacrificed under deep anesthesia and transcardially
perfused using 1X PBS followed by 4% paraformaldehyde for
histological analysis. The injection site was located on the brain
and 3 mm of the frontal and dorsal sides of the injection site (6
mm thickness in total) were isolated. The isolated regions were
cryoprotected with 30% sucrose for 24 h following 24 h fixation at
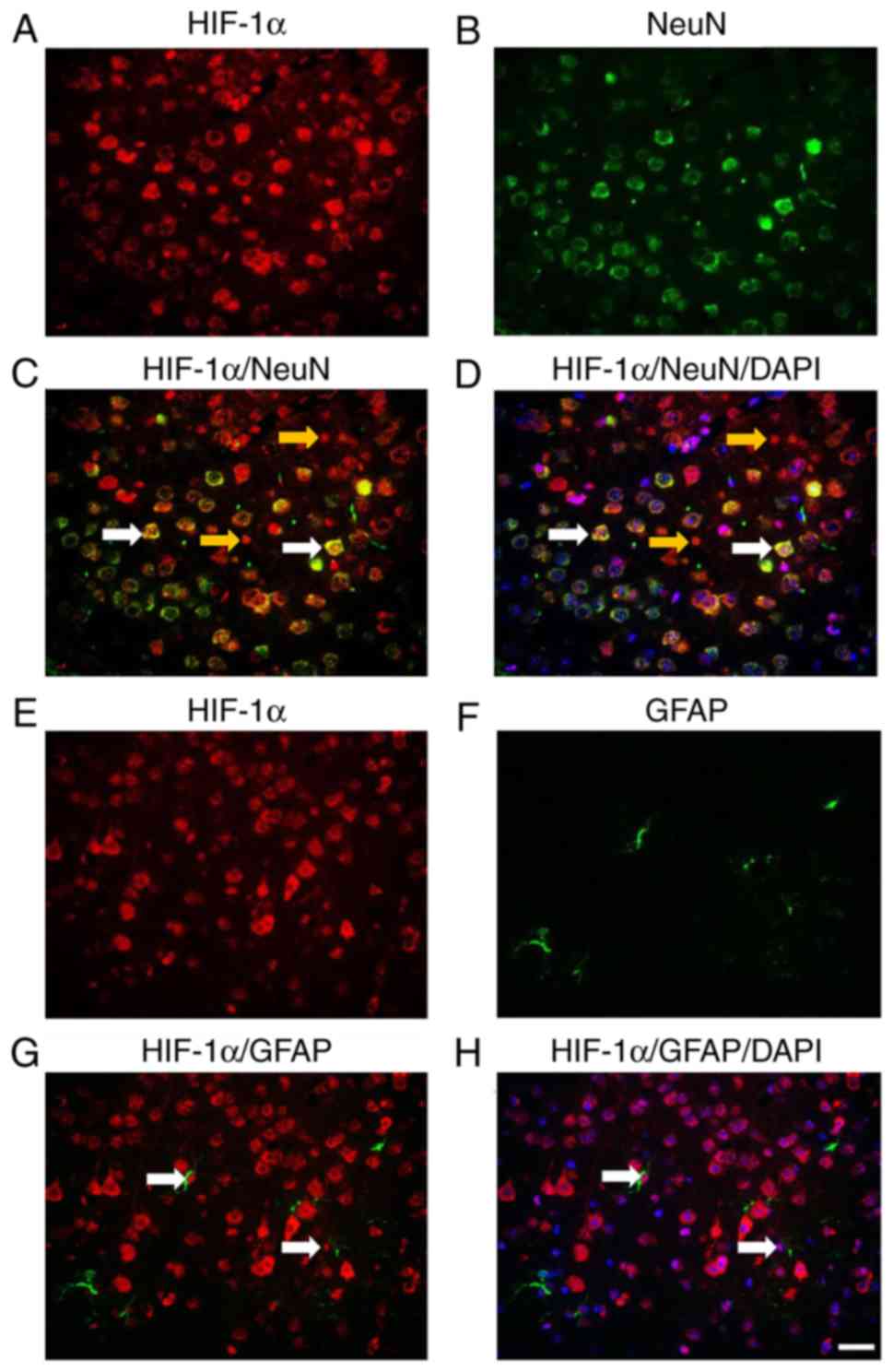
4°C in 4% paraformaldehyde. To evaluate HIF-1α expression, serial
10 µm-thick coronal sections were processed. Sections were
blocked by 3% BSA at room temperature for 30 min and stained with
mouse anti-HIF1α (1:200; cat. no. NB100-479; Novus Biologicals,
LLC), HIF-1α (1:200)/RNA binding fox-1 homolog 3 (NeuN; 1:500; cat.
no. ABN90; EMD Millipore) and HIF-1α (1:200)/glial fibrillary
acidic protein (GFAP; 1:500; cat. no. sc-33673; Santa Cruz
Biotechnology, Inc.) antibodies to identify whether neurons or
astrocytes expressing HIF-1α at 4°C for overnight.
Immunohistochemistry for activated caspase 3 was performed using an
anti-active caspase 3 antibody (1:100; cat. no. ab2302; Abcam) and
active caspase 3 (1:50)/NeuN (1:500; cat. no. ABN90; EMD Millipore)
at 4°C for overnight. The sections were incubated with goat
anti-rabbit biotin-conjugated secondary antibody (1:400; cat. no.
sc-2040; Santa Cruz Biotechnology, Inc.) or donkey anti-rabbit
Alexa Fluor 488 (1:400; A21206; Invitrogen; Thermo Fisher
Scientific, Inc.)/goat anti-mouse Alexa Fluor 594 (1:400; A11005;
Invitrogen; Thermo Fisher Scientific, Inc.) at room temperature for
1 h. Images were captured using an Olympus BX41 light microscope
(magnification, ×400; Olympus Corporation) for HIF-1α and active
caspase 3, and an Olympus BX51 Fluorescence microscope
(magnification, ×400; Olympus Corporation) for immunofluorescence
staining. ImageJ software 1.46 (National Institute of Health) was
used to quantitate the levels of immunoreactivity.
TUNEL assay
To determine the number of apoptotic cells, a TUNEL
assay was performed using an In Situ Cell Death Detection kit (cat.
no. 11684795910; fluorescein; Roche Diagnostics) according to the
manufacturer's protocol. Briefly, slides with brain tissue were
washed three times for 5 min with PBS and permeabilized with 0.5%
Triton X-100 in PBS for 10 min. Then, tissues were incubated in 100
µl TUNEL reaction mixture for 1 h at 37°C in a chamber with
a humidified atmosphere. As a positive control, tissues were
treated with RNase-free DNase I (400 U/ml; Qiagen, Inc.) at room
temperature for 15 min prior to incubation with the TUNEL reagent.
Tissues were incubated with the TUNEL reagent in the absence of
terminal deoxynucleotidyl transferase as a negative control for the
experiment. Subsequent to washing three times with PBS, the slides
were mounted with a mounting medium containing
4,6-diamidino-2-phenylindole (DAPI). Images were captured using an
Olympus BX51 Fluorescence Microscope (magnification, ×200). TUNEL
positive cells were calculated by counting the positively stained
cells in each of the five fields of vision.
Reverse transcription-quantitative PCR
(RT-qPCR)
On day 7 following MCAO, three rats from each group
were sacrificed to collect fresh samples. The penumbral cortex
(around the injection site, ~5 mm in diameter) on the ischemic side
was dissected and maintained in liquid nitrogen for RT-qPCR and
western blotting. Total RNA was extracted from penumbral cortex by
using the RNeasy kit (Invitrogen; Thermo Fisher Scientific, Inc.)
according to the manufacturer's protocol. Using a PrimeScript RT
Reagent kit (Takara Biotechnology Co., Ltd.), RNA samples were
subjected to reverse transcription at 37°C for 60 min. For each
rat, the reactions were run in triplicate in three independent
experiments. The FAM-labeled fluorophore was obtained from
TaqMan® (Thermo Fisher Scientific, Inc), and the qPCR
thermocycling conditions were as follows: 93°C for 3 min, followed
by 40 cycles of 93°C for 1 min, 55°C for 1 min and 72°C 1 min.
Rotor-Gene software v2.3 (Qiagen) accompanying the Applied
Biosystems™ 7500 Real-Time PCR System (Applied Biosystems; Thermo
Fisher Scientific, Inc.) was used to collect and analyze data. The
Cq values of each sample were normalized to the corresponding GAPDH
Cq values, and relative expression levels were calculated using the
ΔΔCq method (27). The primers
used were as follows: EPO forward, 5′-CAT CTG CGA CAG TCG AGT TCT
G-3′ and reverse, 5′-CAC AAC CCA TCG TGA CAT TTT C-3′; EPO-R
forward, 5′-ACA CGT CGA GTT TTG TGC CA-3′ and reverse, 5′-TGA TGA
TGC GGT GGT AGC-3′; GAPDH forward, 5′-CAT GGC CTT CCG TGT TCC TA3
and reverse, 5′-TAC TTG GCA GGT TTC TCC AGG3.
Western blot assay
Brain tissues were homogenized in RIPA lysis buffer
(Beijing BLKW Biotechnology Co., Ltd.), followed by centrifugation
at 10,000 × g for 10 min at 4°C. BCA method was used for
quantitative analysis the protein samples. Proteins (30 µg)
from brain tissues were separated by 10% SDS-PAGE under reducing
conditions. Subsequently, the proteins were transferred to
nitrocellulose membranes. A total of 3% milk in PBS with 0.05%
Tween-20 (PBST) was used to block the unspecific binding of
antibodies at room temperature for 1 h. Then, the blots were
incubated with the following primary antibodies: Mouse Anti-HIF1α
(1:10,000; cat. no. NB100-479; Novus Biologicals, LLC), anti-EPO
(1:1,000; cat. no. sc-5290; Santa Cruz Biotechnology, Inc.),
anti-EPO-R (1:1,000; cat. no. sc-365662; Santa Cruz Biotechnology,
Inc.) or mouse anti-β-actin antibody (AC-15; 1:3,000; cat. no.
sc-69879; Santa Cruz Biotechnology, Inc.) overnight at 4°C. Blots
were then incubated with a rabbit anti-goat IgG-HRP (1:3,000; cat.
no. sc-2922; Santa Cruz Biotechnology, Inc.) or goat anti-mouse
IgG-HRP (1:3,000; sc-2005; Santa Cruz Biotechnology, Inc.) for 1 h
at room temperature and washed three times with PBST. An enhanced
chemiluminescence (ECL) western blotting detection reagent (cat.
no. RPN2232; GE Healthcare) was used for visualization. An Odyssey
Infrared Imaging system and software (model 9120; LI-COR
Biosciences) were used to evaluate the specific signals and the
corresponding band intensities.
Statistical analysis
Data are presented as the mean ± standard deviation
and were analyzed using one-way analysis of variance followed by a
Bonferroni post hoc-test using SPSS 15.0 software (SPSS, Inc.).
P<0.05 was considered to indicate a statistically significant
difference.
Results
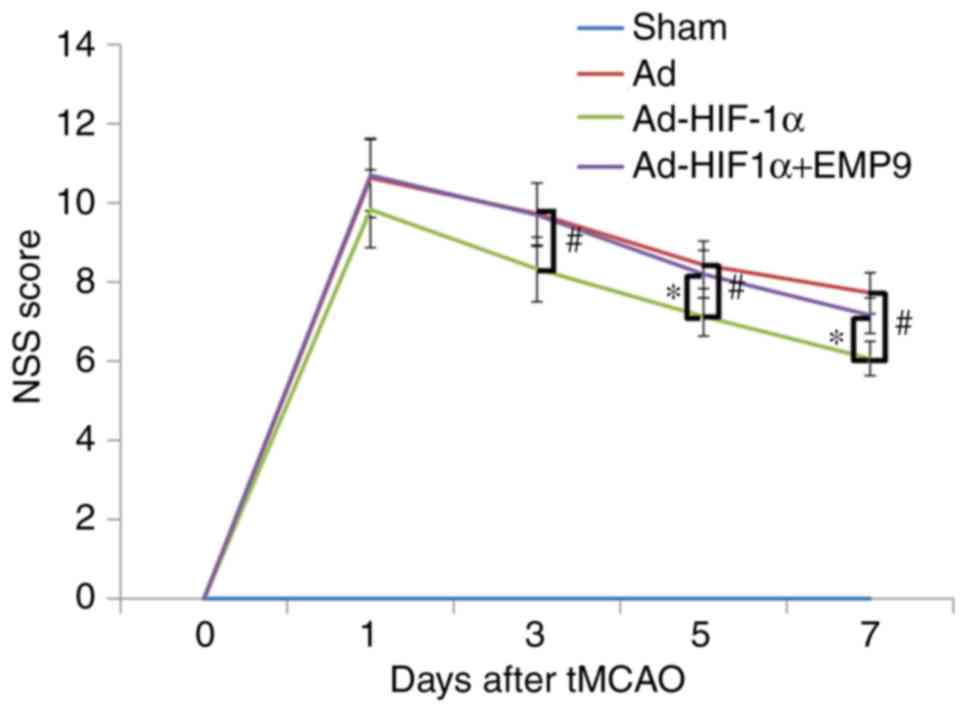
Ad-HIF-1α treatment promotes neurological
functional recovery in tMCAO rats
To investigate if treatment with Ad-HIF-1α may
improve sensorimotor deficit, the present study compared NSS
scores. The score of all rats in all groups was 0 prior to tMCAO
(day 0). No neurological functional deficits were revealed in the
Sham group. Following tMCAO on day 1, there were no significant
differences among the three groups in terms of NSS scores.
Neurological functional deficits evaluated by the NSS assessment
revealed a progressive recovery in each group from day 3 to 7
following tMCAO. Ad-HIF1-α treatment demonstrated a significantly
better improvement in NSS scores compared with the Ad group on
post-ischemia day 3, 5 and 7 (P<0.05; Fig. 1). EMP9 partially abolished the
benefits of Ad-HIF1-α treatment (Fig.
1). Body weights among the 4 groups were not significantly
different across the 7 days (data not shown).
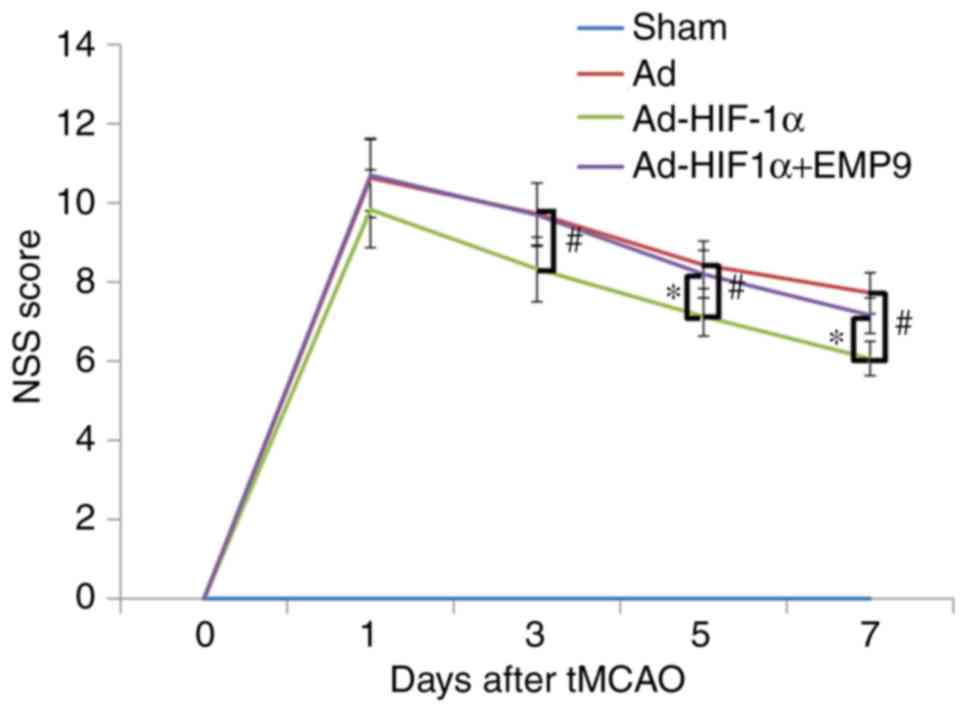 | Figure 1Ad-HIF-1α treatment promoted recovery
in rats with tMCAO. An NSS score was determined on day 0, 1, 3, 5
and 7 following treatment. No neurological deficit was observed in
the Sham group. Compared with the Ad-treated rats,
Ad-HIF-1α-treated rats had significantly fewer severe symptoms from
day 3 following treatment. #P<0.05 vs. Ad-treated
rats. Compared with Ad-HIF-1α +EMP9-treated rats, Ad-HIF-1α-treated
rats also exhibited significantly better recovery from day 3
onwards. *P<0.05 vs. Ad-HIF-1α +EMP9-treated rats.
Ad-HIF-1α +EMP9-treated rats did not recover better compared with
Ad-treated rats within 7 days. NSS, neurological severity score;
tMCAO, transient middle cerebral artery occlusion; Ad, adenovirus;
HIF-1α, hypoxia-inducible factor-1α; EMP9, erythropoietin mimetic
peptide-9. |
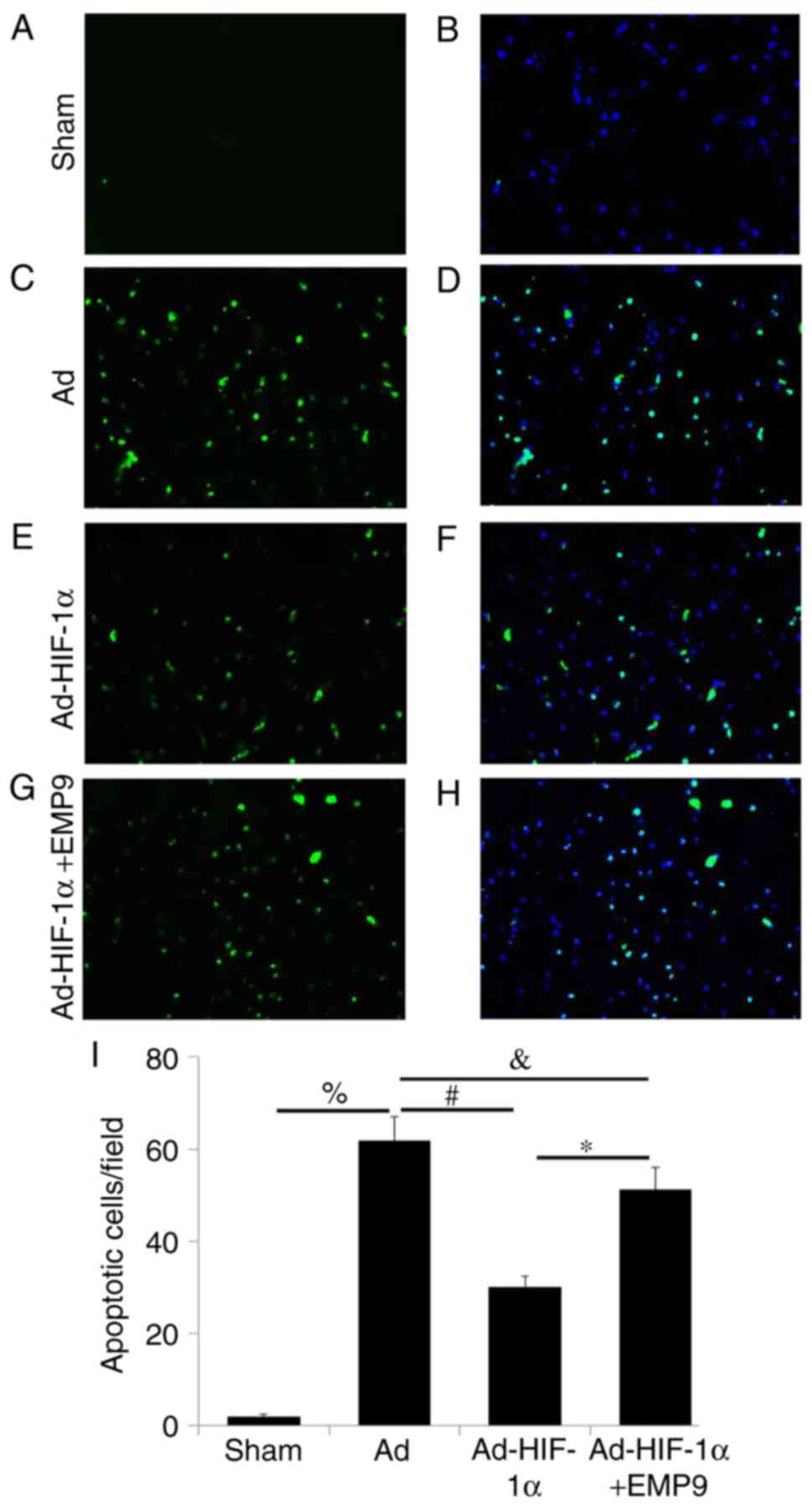
Ad-HIF-1α attenuates apoptosis in tMCAO
rats
To evaluate whether HIF-1α may decrease the number
of apoptotic cells in rats with tMCAO, the present study treated
rats 1 h following tMCAO with Ad, Ad-HIF-1α or Ad-HIF-1α and EMP9.
Very few TUNEL-positive apoptotic cells were detected (Fig. 2A), compared with the total number
of cells (Fig. 2B), as observed
through DAPI staining, in the Sham group. However, rats in the Ad
group had a substantially greater number of apoptotic cells in the
pre-ischemic area on day 7 following tMCAO (Fig. 2C and D). HIF-1α-treated rats had
substantially fewer apoptotic cells on day 7 compared with the
Ad-treated rats (Fig. 2E and F).
In the Ad-HIF1-α with EMP9-treated rats, the number of apoptotic
cells remained high (Fig. 2G and
H). Compared with rats treated with Ad and Ad-HIF1-α with EMP9,
Ad-HIF-1α significantly decreased the number of apoptotic cells
(P<0.05; Fig 2I).
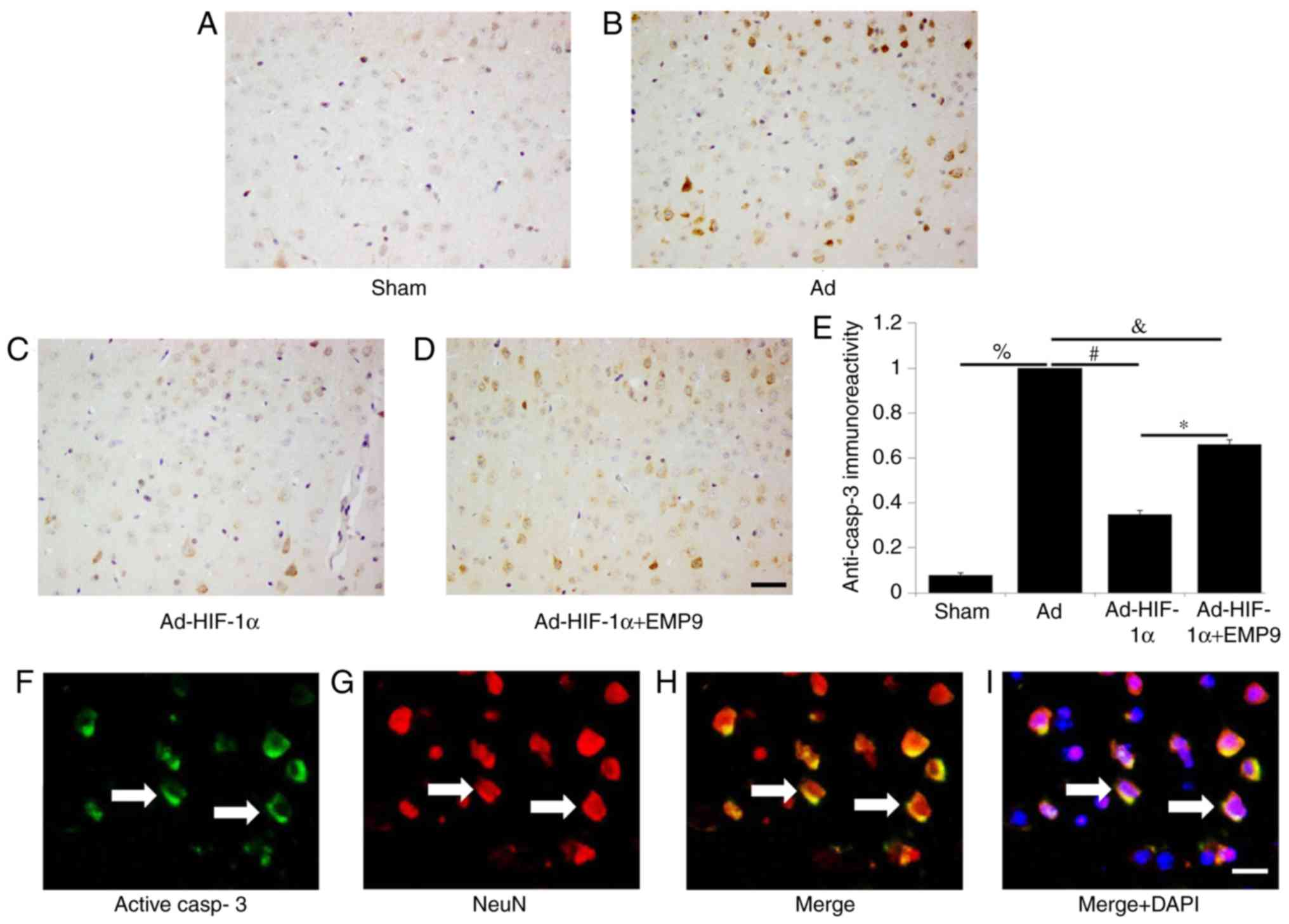
Ad-HIF-1α suppresses active caspase-3 in
neurons
Active caspase-3 is a cysteine protease involved in
the activation cascade of caspases responsible for apoptosis
execution (28). A very low
expression of active caspase 3 was revealed in the Sham group
(Fig. 3A). In comparison,
numerous active caspase 3-positive cells were observed in the brain
of rats treated with Ad (Fig.
3B). Active caspase 3 expression was downregulated by Ad-HIF-1α
treatment (Fig. 3C). EMP9
treatment did not change the active caspase-3 expression induced by
tMCAO (Fig. 3D). Statistical
analysis demonstrated that Ad-HIF-1α treatment significant
decreased active caspase 3 expression compared with the Ad group
(P<0.05; Fig. 3E). The present
study used double-labeled fluorescence staining to determine
whether active caspase-3 (Fig.
3F) was expressed in neurons (Fig. 3G). The results demonstrated that
active caspase-3 was expressed in neurons (Fig. 3H). Colocalization of active
caspase-3 (green), NeuN (red) and DAPI (blue) staining (Fig. 3I) further confirmed the
co-expression.
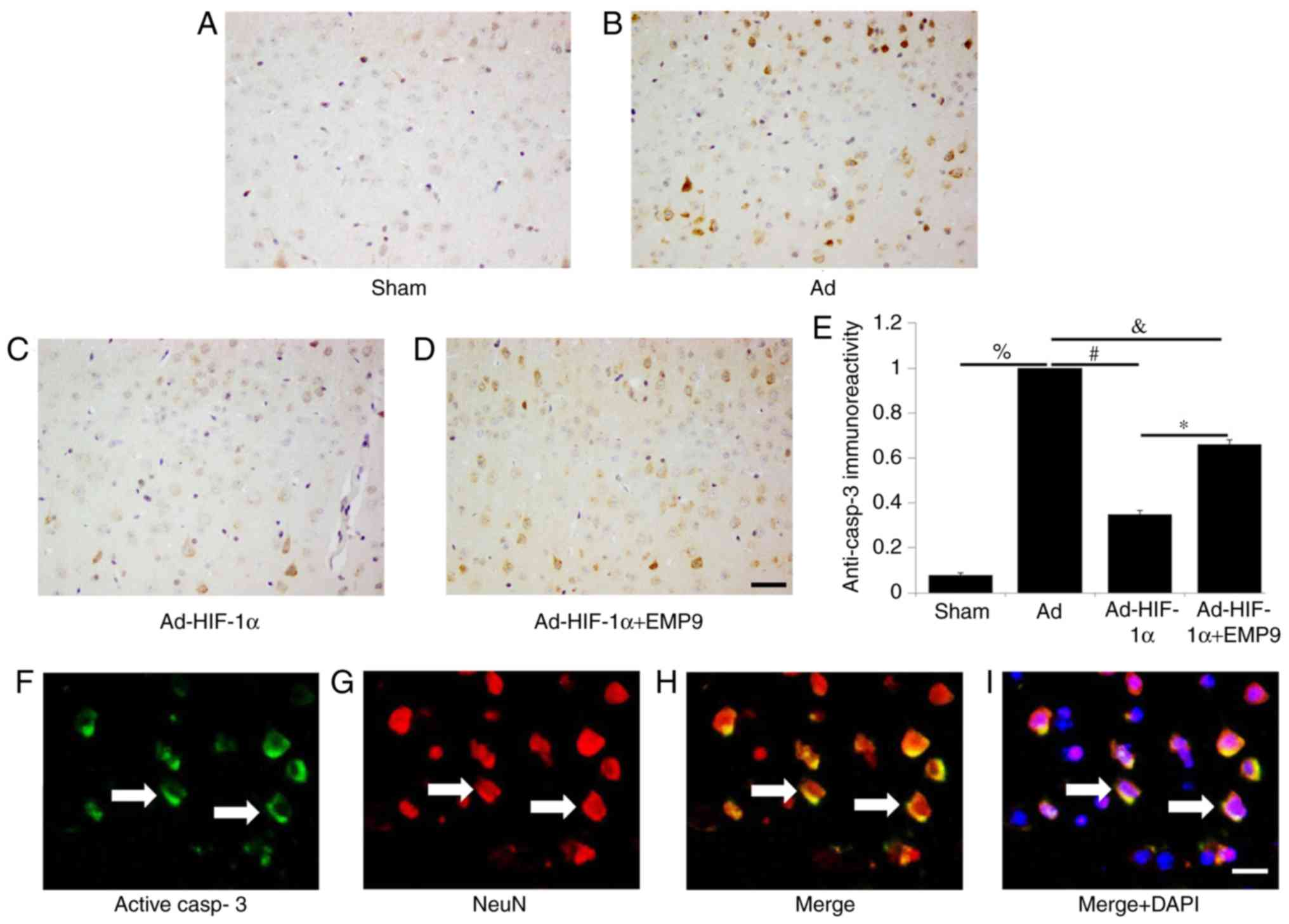 | Figure 3Ad-HIF-1α treatment suppressed active
caspase-3 expression in neurons. Active caspase-3 was detected in
(A) the Sham group, (B) the Ad group, (C) the Ad-HIF-1α and (D) the
Ad-HIF-1α +EMP9 group (scale bar, 50 µm), and then (E)
quantified. There were significantly more active caspase 3-positive
cells in the brains of rats treated with Ad compared with the Sham
group. %P<0.05, #P<0.05,
&P<0.05 and *P<0.05 with
comparisons shown by lines. (F) Active caspase 3 and (G) NeuN
double-labeled fluorescence staining in Ad-treated rat brains
(scale bar, 20 µm). (H) Colocalization of NeuN (red) and
active caspase 3 (green) (white arrows; scale bar, 20 µm).
(I) Colocalization of NeuN (red), and active casp3 (green) and DAPI
(blue) (white arrows; scale bar, 20 µm). Ad, adenovirus;
HIF-1α, hypoxia-inducible factor-1α; EMP9, erythropoietin mimetic
peptide-9; NeuN, RNA binding fox-1 homolog 3. |
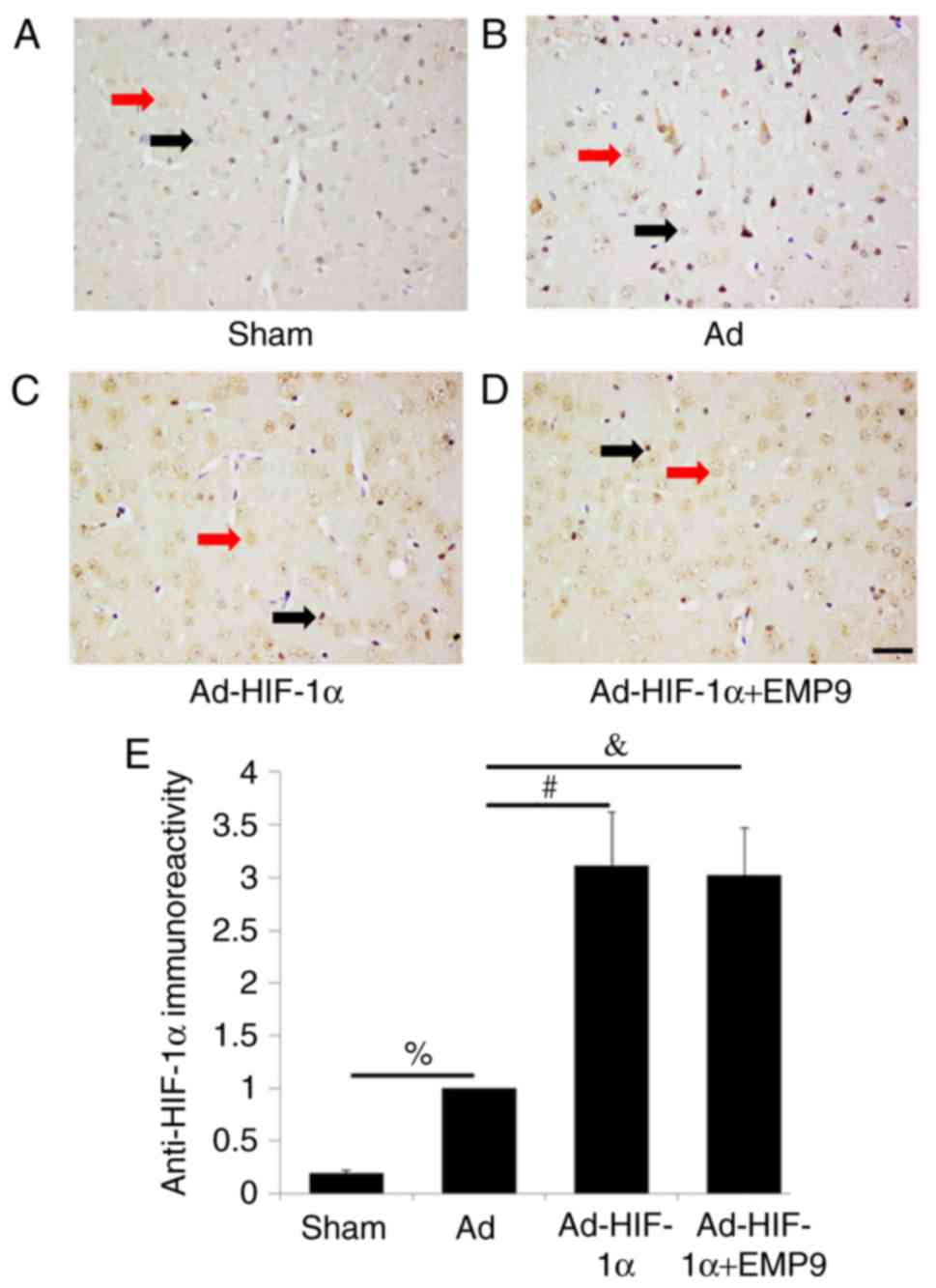
Ad-HIF-1α upregulated HIF-1α expression
following tMCAO
An extremely low expression of HIF-1α was observed
in the cytoplasm of neurons in the Sham group (Fig. 4A). In brain of rats treated with
Ad, HIF-1α nuclear positive cells demonstrated that tMCAO induces
HIF-1α activation (Fig. 4B).
HIF-1α was expressed in neurons and glia cells. HIF-1α expression
was upregulated by Ad-HIF-1α treatment (Fig. 4C) and EMP9 treatment did not
attenuate the effect (Fig. 4D).
Statistical analysis revealed that Ad-HIF-1α treatment
significantly increased HIF-1α expression compared with the
Ad-treated group (P<0.05; Fig.
4E). To further confirm that Ad-HIF-1α upregulated HIF-1α
expression, HIF-1α western blot analysis for Ad-treated rats and
Ad-HIF-1α-treated rats was performed. The results demonstrated that
compared with Ad treatment, HIF-1α was increased ~3.4 fold by
Ad-HIF-1α treatment (P<0.05; Fig.
S1).
The present study used double-labeled fluorescence
staining to determine whether HIF-1α (Fig. 5A) was expressed in neurons
(Fig. 5B). The results
demonstrated that activated HIF-1α was observed in neurons
(Fig. 5C). Colocalization of
active HIF-1α (red), NeuN (green) and DAPI (blue) staining
(Fig. 5D) further confirmed the
co-expression. The present study additionally used double-labeled
fluorescence staining to determine whether HIF-1α (Fig. 5E) was expressed in astrocytes
(Fig. 5F), which are
EPO-producing cells. Activated HIF-1α was observed in astrocytes
(Fig. 5G). It was further
confirmed by the colocalization of HIF-1α (red), GFAP (green) and
DAPI (blue) staining (Fig. 5H).
In a preliminary experiment, on day 3 rats treated by Ad-HIF-1α had
more activated GFAP-positive astrocytes compared with that in Ad
treated rats (data not shown). However on day 7, no significant
difference was observed either in the number or the morphology of
astrocytes (data not shown).
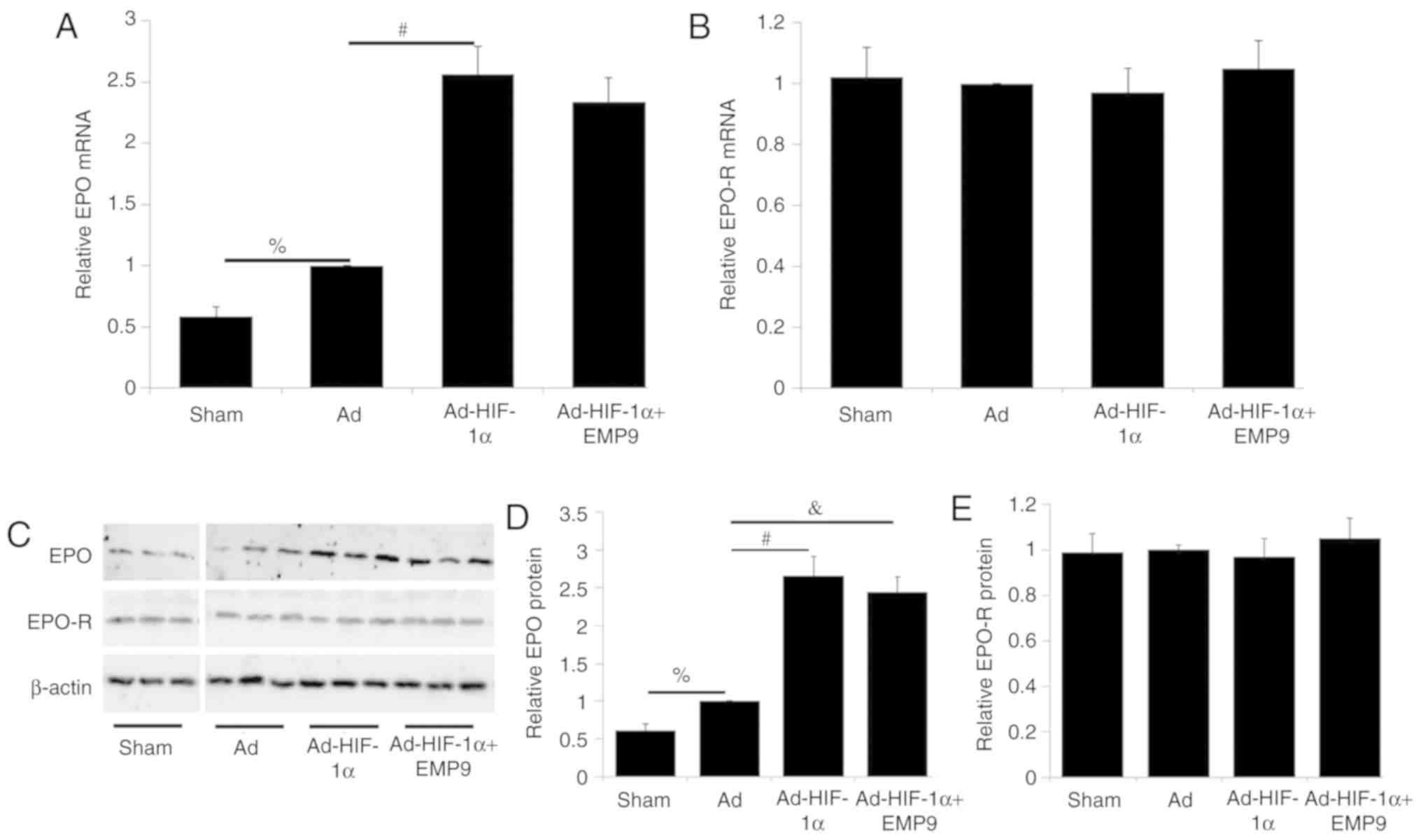
Ad-HIF-1α increased EPO expression
without changing the expression of EPO-R
To determine the effect of HIF-1α on the expression
of EPO and EPO-R, RT-qPCR and western blot analysis were performed.
EPO mRNA and protein levels in the Ad group were ~1.8 and ~1.7
fold, respectively, higher compared with that in the Sham group
(P<0.05; Fig. 6A and D).
Compared with Ad treatment, Ad-HIF-1α treatment increased EPO mRNA
levels ~2.6 fold (P<0.05; Fig.
6A). Ad-HIF-1α treatment did not significantly alter EPO-R mRNA
expression levels (Fig. 6B).
Compared with Ad treatment, Ad-HIF-1α treatment increased EPO
protein expression (Fig. 6C).
Quantitative analysis revealed that EPO protein levels were
upregulated ~2.7 folds (P<0.05; Fig. 6D). EMP9 treatment did not affect
EPO expression increased by HIF-1α at the protein level (Fig. 6C). Ad-HIF-1α treatment did not
change EPO-R protein expression (Fig.
6C). No significant difference was observed in EPO-R protein
expression levels between the different groups (Fig. 6E).
Discussion
The present study investigated whether HIF-1α
inhibits neuronal apoptosis through upregulating EPO in a rat model
of stroke. The results demonstrated that Ad-HIF-1α treatment
resulted in improved neurological functional recovery by decreasing
neuronal apoptosis. The results of the present study further proved
that the administration of Ad-HIF-1α upregulated HIF-1α expression
in neurons and astrocytes. Finally, the present study proved that
Ad-HIF-1α treatment upregulated EPO expression, which in turn
suppressed activated caspase-3 in neurons. The results presented
here provide novel insights into the function of HIF-1α for
treating ischemic stroke.
Stroke is one of the most common causes of adult
permanent disability globally, with ~90% of cases resulting from an
ischemic stroke, which is an acute reduction in cerebral blood
supply to the brain tissues (29). Reduced oxygen and nutrients
following focal ischemic stroke affect a small core of ischemic
tissues initially; however, the infarct expands over hours and
days, due to a loss of ion homeostasis, excitatory amino acid
release, edema and decreased pH, causing cell apoptosis in the
surrounding tissues of the brain parenchyma (30). These areas surrounding the
ischemic core are defined as the ischemic penumbra, a region where
selective neuronal death, hypoxia, protein denaturation and limited
diffusion happen at the same time. The penumbra region exists
between the normal cerebral blood flow region and infarct core
area, and the gene expression is different in various regions at
different time points (31). The
tissue of the ischemic penumbra is reversible through timely
treatment, so that for post-ischemic neuroprotective therapies the
strategy is to target the ischemic penumbra for preventing or
rescuing the spreading damage from the initial infarct (32). In the present study, it was
revealed that the administration of Ad-HIF-1α in the ischemic
penumbra subsequent to focal ischemia reduced neuronal apoptosis
and behavioral deficits associated with the upregulated expression
of HIF-1α and EPO, a HIF-1-regulated gene.
The ischemic penumbra remains the main target for
ischemic stroke treatment, as some tissue in the ischemic penumbra
is still salvageable surrounding the core of infarction (31,32). Neurons in the ischemic penumbra
are at a high risk for delayed apoptosis caused by the deleterious
metabolic processes propagated from the ischemic core, including
the loss of ion homeostasis, excitatory amino acid release,
inflammation, decreased pH and edema. Following stroke, the
surviving neurons in the ischemic penumbra directly contribute to
neurological function recovery (33). HIF-1α, pathologically stimulated
in the ischemic region, is of central importance in the response to
hypoxia/ischemia, and is crucial for the endogenous protection
against low oxygen. However, reports around the pharmacological or
genetic alteration of HIF activity to treat cerebral ischemia are
controversial. Studies have revealed that HIF-1α induction
decreased neuronal death in the ischemic penumbra (14,34-38). While neuron-specific HIF-1α
knockout increased tissue injury following an ischemic stroke
(39), in others, it improved
neuronal survival and sensorimotor function (40,41). In these two previous studies, the
function of HIF-1α knockout in the early acute stage (48 and 72 h)
was investigated. Furthermore, HIF-1α inhibition by
3-(5′-hydroxymethyl-2′-furyl)-1-benzylindazole (YC-1) has also been
revealed to promote brain damage following stroke while
simultaneously decreasing ischemia-induced vascular leakage
(42). In this previous study,
the results demonstrated that YC-1 not only inhibited
ischemia-induced HIF-1 but also downregulated the HIF-1 downstream
genes EPO, VEGF and glucose transporter in neurons and brain
endothelial cells. So, it was concluded that YC-1 lacks the
potential to function as a cerebral ischemic treatment. Thus,
further studies are required to clarify the exact function of HIF-1
and its target genes for stroke outcome and prevention. In the
present study, for the first time, an adenovirus was used to
overexpress HIF-1α in the ischemic penumbra. The adenovirus
themselves did not affect the HIF-1 downstream genes. The present
study demonstrated that Ad-HIF-1α administration increased HIF-1α
protein expression in neurons and astrocytes. Ad-HIF-1α treatment
also upregulated EPO expression without a significant change in
EPO-R expression in the ischemic penumbra. More importantly, the
neuroprotection exerted by Ad-HIF-1α was partially diminished by
EMP9, an erythropoietin receptor antagonist, proving that the
neuroprotective effect of HIF-1 is mediated by EPO upregulation.
Furthermore, the present study demonstrated that EMP9 failed to
alter the expression of EPO upregulated by Ad-HIF-1α, which
indicates that the HIF-1α neuroprotective effect depends on
upregulated EPO functionally binding to its receptor. Finally, the
present study demonstrated that Ad-HIF-1α treatment upregulated EPO
expression, which in turn suppresses activated caspase-3 in
neurons.
Caspases may be divided into two groups based on
their function in apoptosis (caspase-3, 6, 7, 8 and 9) and
inflammation (caspase-1, 4, 5 and 12) (43). Caspase-3, a major executioner
caspase in apoptosis, is cleaved and activated by caspase-8 and
caspase-9. The active caspase-3 enzyme is formed once caspase-3 is
cleaved at an aspartate residue to yield a p12 and a p17 subunit
(44). During apoptosis, active
caspase-3 degrades multiple cellular proteins and is responsible
for DNA fragmentation and morphological changes in cells (41). EPO has been reported to have an
anti-apoptosis function (45).
The EPO-R is dimerized once it binds to EPO that in turn activates
Janus kinase 2 (JAK2), a receptor-associated tyrosine kinase.
Activated JAK2 phosphorylates tyrosine residues on the cytosolic
domain of the EPO-R, which results in the recruitment of downstream
effectors, including growth factor receptor bound protein 2,
phosphoinositide-3 kinase (PI3K) and signal transducer and
activator of transcription family members (45,46). It has been revealed that EPO
prevents PC12 cell injuries by activating the PI3K⁄protein kinase B
pathway (47). EPO is also able
to enhance the antioxidant capacity by activating the reactive
oxygen species neutralizing enzymes, including superoxide
dismutase, glutathione peroxidase and catalase (48-50).
In the present study, the neuroprotection by
Ad-HIF-1α was not completely diminished by EMP9, indicating that
other HIF-1α-regulated pathways are involved in HIF-1α mediated
neuroprotection. HIF-1α is a universal molecular master switch,
controlling cellular survival, metabolic adaptation and glucose
metabolism and transport. More than 30 target genes are known for
HIF-1α, including but not limited to EPO, VEGF, insulin-like growth
factor 2, glycolytic enzymes and glucose transporter 1 (51,52). Among them, VEGF is the most
important angiogenetic factor in all steps of angiogenesis
(53). VEGF participates in
angiogenesis via recruiting endothelial cells into a hypoxic and
avascular area and stimulating their proliferation. Therefore, VEGF
induction, among other proangiogenic factors, in the ischemic area
causes an increase in the vascular density and a decrease in the
oxygen diffusion distances, resulting in neuronal apoptosis
inhibition (53). More studies
are required to investigate other mechanisms involved in
HIF-1α-mediated neuroprotection.
In the present study, TUNEL staining was used to
identify apoptotic cells. It is well known that TUNEL is unable to
distinguish apoptosis from necrosis. Furthermore apoptosis and
necrosis may coexist in the same tissue. However, in a tMCAO model,
necrosis mostly locates in the ischemic core and apoptosis more
frequently occurs in the ischemic penumbra (54). In the present study, ischemic
penumbra tissue was examined. Therefore, in combination with active
caspase-3 staining, the majority of TUNEL-positive signals
represent apoptotic cells.
In conclusion, the present study demonstrated that
HIF-1α attenuates neuronal apoptosis partially through upregulating
EPO, which in turn suppresses activated caspase-3 in neurons
following cerebral ischemia in rats. The data presented by the
present study provides novel insights into the function of HIF-1α
in the treatment of ischemic stroke. Thus, HIF-1α may be a
potential therapeutic target for ischemic stroke.
Supplementary Data
Funding
The present study was supported by the Health and
Family Planning Commission of Guizhou (grant nos. 2014-41 and
gzwjkj 2014-1-055), the Science and Technology Foundation of
Guizhou (grant no. 2007-2096) and the Special Governor's Fund for
Outstanding Technological and Educational Talents in Guizhou (grant
no. 2006-60).
Availability of data and materials
The data used and/or analyzed in this study are
available from the corresponding author with reasonable
request.
Authors' contributions
JL and TT wrote the manuscript, and contributed to
the acquisition, analysis and interpretation of the data. JX, ZL,
ZZ and MJ collected, analyzed and interpreted the data. JL, TT, JX
and ZL contributed to the conception and design of the present
study. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The animal studies were ethically approved by the
local Animal Experimentation Ethics Committee (Guizhou Provincial
People's Hospital, Guizhou, China) for animal experimentation.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Acknowledgments
The authors would like to thank Mr. Arvand Asghari
from the University of Houston (Houston, TX, USA) for carefully
editing the English of the manuscript.
References
|
1
|
Ng M, Fleming T, Robinson M, Thomson B,
Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF,
et al: Global, regional, and national prevalence of overweight and
obesity in children and adults during 1980-2013: A systematic
analysis for the Global Burden of Disease Study 2013. Lancet.
384:766–781. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
GBD 2016 Causes of Death Collaborators:
Global, regional, and national age-sex specific mortality for 264
causes of death, 1980-2016: A systematic analysis for the Global
Burden of Disease Study 2016. Lancet. 390:1151–210. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang G, Wang Y, Zeng Y, Gao GF, Liang X,
Zhou M, Wan X, Yu S, Jiang Y, Naghavi M, et al: Rapid health
transition in China, 1990-2010: Findings from the global burden of
disease study 2010. Lancet. 381:1987–2015. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu L, Wang D, Wong KS and Wang Y: Stroke
and stroke care in China: Huge burden, significant workload, and a
national priority. Stroke. 42:3651–3654. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang
L, Wang L, Jiang Y, Li Y, Wang Y, et al: Prevalence, incidence, and
mortality of stroke in China: Results from a nationwide
population-based survey of 480 687 adults. Circulation.
135:759–771. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang YJ, Zhang SM, Zhang L, Wang CX, Dong
Q, Gao S, Huang RX, Huang YN, Lv CZ, Liu M, et al: Chinese
guidelines for the secondary prevention of ischemic stroke and
transient ischemic attack 2010. CNS Neurosci Ther. 18:93–101. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hacke W, Kaste M, Bluhmki E, Brozman M,
Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, et
al: Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic
stroke. N Engl J Med. 359:1317–1329. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xydas T, Georgantopoulos C, Bethanis D and
Sarris M: Thrombolysis for acute ischemic stroke: A new paradigm.
Hosp Chron. 7:77–80. 2012.
|
|
9
|
National 'Ninth Five-Year Plan' Research
Group; Chen Q: Intravenous thrombolysis with urokinase for acute
cerebral infarctions. Chin J Neurol. 35:210–213. 2002.In
Chinese.
|
|
10
|
Semenza GL: Targeting HIF-1 for cancer
therapy. Nat Rev Cancer. 3:721–732. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Semenza GL: Hypoxia-inducible factor 1:
Oxygen homeostasis and disease pathophysiology. Trends Mol Med.
7:345–350. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ivan M, Kondo K, Yang H, Kim W, Valiando
J, Ohh M, Salic A, Asara JM, Lane WS and Kaelin WG Jr: HIFalpha
targeted for VHL-mediated destruction by proline hydroxylation:
Implications for O2 sensing. Science. 292:464–468. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Abe H, Semba H and Takeda N: The roles of
hypoxia signaling in the pathogenesis of cardiovascular diseases. J
Atheroscler Thromb. 24:884–894. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Feng Y and Bhatt AJ: Corticosteroid
responses following hypoxic preconditioning provide neuroprotection
against subsequent hypoxic-ischemic brain injury in the newborn
rats. Int J Dev Neurosci. 44:6–13. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen J, Yang Y, Shen L, Ding W, Chen X, Wu
E, Cai K and Wang G: Hypoxic preconditioning augments the
therapeutic efficacy of bone marrow stromal cells in a rat ischemic
stroke model. Cell Mol Neurobiol. 37:1115–1129. 2017. View Article : Google Scholar
|
|
16
|
Jacobs K, Shoemaker C, Rudersdorf R, Neill
SD, Kaufman RJ, Mufson A, Seehra J, Jones SS, Hewick R and Fritsch
EF: Isolation and characterization of genomic and cDNA clones of
human erythropoietin. Nature. 313:806–810. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chikuma M, Masuda S, Kobayashi T, Nagao M
and Sasaki R: Tissue-specific regulation of erythropoietin
production in the murine kidney, brain, and uterus. Am J Physiol
Endocrinol Metab. 279:E1242–E1248. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yu X, Shacka JJ, Eells JB, Suarez-Quian C,
Przygodzki RM, Beleslin-Cokic B, Lin CS, Nikodem VM, Hempstead B,
Flanders KC, et al: Erythropoietin receptor signalling is required
for normal brain development. Development. 129:505–516.
2002.PubMed/NCBI
|
|
19
|
Iwai M, Stetler RA, Xing J, Hu X, Gao Y,
Zhang W, Chen J and Cao G: Enhanced oligodendrogenesis and recovery
of neurological function by erythropoietin after neonatal
hypoxic/ischemic brain injury. Stroke. 41:1032–1037. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu SH, Lu IC, Lee SS, Kwan AL, Chai CY and
Huang SH: Erythropoietin attenuates motor neuron programmed cell
death in a burn animal model. PLoS One. 13:e01900392018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang P, Lu Y, Han D, Wang P, Ren L, Bi J
and Liang J: Neuroprotection by nicotinamide mononucleotide
adenylyltransferase 1 with involvement of autophagy in an aged rat
model of transient cerebral ischemia and reperfusion. Brain Res.
1723:1463912019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Saadoun S, Waters P, Bell BA, Vincent A,
Verkman AS and Papadopoulos MC: Intra-cerebral injection of
neuromyelitis optica immunoglobulin G and human complement produces
neuromyelitis optica lesions in mice. Brain. 133:349–361. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen T, Yu Y, Tang LJ, Kong L, Zhang CH,
Chu HY, Yin LW and Ma HY: Neural stem cells over-expressing
brain-derived neurotrophic factor promote neuronal survival and
cytoskeletal protein expression in traumatic brain injury sites.
Neural Regen Res. 12:433–439. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wu W, Chen X, Hu C, Li J, Yu Z and Cai W:
Transplantation of neural stem cells expressing hypoxia-inducible
factor-1alpha (HIF-1alpha) improves behavioral recovery in a rat
stroke model. J Clin Neurosci. 17:92–95. 2010. View Article : Google Scholar
|
|
25
|
Yang ML, Tao T, Xu J, Liu Z and Xu D:
Antiapoptotic effect of gene therapy with recombinant adenovirus
vector containing hypoxia-inducible factor-1α after cerebral
ischemia and reperfu-sion in rats. Chin Med J (Engl).
130:1700–1706. 2017. View Article : Google Scholar
|
|
26
|
Lin YW and Hsieh CL: Electroacupuncture at
Baihui acupoint (GV20) reverses behavior deficit and long-term
potentiation through N-methyl-d-aspartate and transient receptor
potential vanilloid subtype 1 receptors in middle cerebral artery
occlusion rats. J Integr Neurosci. 9:269–282. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
28
|
Snigdha S, Smith ED, Prieto GA and Cotman
CW: Caspase-3 activation as a bifurcation point between plasticity
and cell death. Neurosci Bull. 28:14–24. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Li Y, Huang L, Ma Q, Concepcion KR, Song
MA, Zhang P, Fu Y, Xiao D and Zhang L: Repression of the
glucocorticoid receptor aggravates acute ischemic brain injuries in
adult mice. Int J Mol Sci. 19:E24282018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Paciaroni M, Caso V and Agnelli G: The
concept of ischemic penumbra in acute stroke and therapeutic
opportunities. Eur Neurol. 61:321–330. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Rosso C and Samson Y: The ischemic
penumbra: The location rather than the volume of recovery
determines outcome. Curr Opin Neurol. 27:35–41. 2014. View Article : Google Scholar
|
|
32
|
Ran YC, Zhu M, Li SJ, Zhang ZX, Wang X,
Zhang Y and Cheng JL: Related research and recent progress of
ischemic penumbra. World Neurosurg. 116:5–13. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Murphy TH and Corbett D: Plasticity during
stroke recovery: From synapse to behaviour. Nat Rev Neurosci.
10:861–872. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Reischl S, Li L, Walkinshaw G, Flippin LA,
Marti HH and Kunze R: Inhibition of HIF prolyl-4-hydroxylases by
FG-4497 reduces brain tissue injury and edema formation during
ischemic stroke. PLoS One. 9:e847672014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ogle ME, Gu X, Espinera AR and Wei L:
Inhibition of prolyl hydroxylases by dimethyloxaloylglycine after
stroke reduces ischemic brain injury and requires hypoxia inducible
factor-1α. Neurobiol Dis. 45:733–742. 2012. View Article : Google Scholar
|
|
36
|
Li C, Zhang B, Zhu Y, Li Y, Liu P, Gao B,
Tian S, Du L and Bai Y: Post-stroke constraint-induced movement
therapy increases functional recovery, angiogenesis, and
neurogenesis with enhanced expression of HIF-1α and VEGF. Curr
Neurovasc Res. 14:368–377. 2017. View Article : Google Scholar
|
|
37
|
Wang H, Niu F, Fan W, Shi J, Zhang J and
Li B: Modulating effects of preconditioning exercise in the
expression of ET-1 and BNP via HIF-1α in ischemically injured
brain. Metab Brain Dis. 34:1299–1311. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Gao Y, Yin H, Zhang Y, Dong Y, Yang F, Wu
X and Liu H: Dexmedetomidine protects hippocampal neurons against
hypoxia/reoxygenation-induced apoptosis through activation
HIF-1α/p53 signaling. Life Sci. 232:1166112019. View Article : Google Scholar
|
|
39
|
Baranova O, Miranda LF, Pichiule P,
Dragatsis I, Johnson RS and Chavez JC: Neuron-specific inactivation
of the hypoxia inducible factor 1 alpha increases brain injury in a
mouse model of transient focal cerebral ischemia. J Neurosci.
27:6320–6332. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Barteczek P, Li L, Ernst AS, Böhler LI,
Marti HH and Kunze R: Neuronal HIF-1α and HIF-2α deficiency
improves neuronal survival and sensorimotor function in the early
acute phase after ischemic stroke. J Cereb Blood Flow Metab.
37:291–306. 2017. View Article : Google Scholar
|
|
41
|
Helton R, Cui J, Scheel JR, Ellison JA,
Ames C, Gibson C, Blouw B, Ouyang L, Dragatsis I, Zeitlin S, et al:
Brain-specific knock-out of hypoxia-inducible factor-1 alpha
reduces rather than increases hypoxic-ischemic damage. J Neurosci.
25:4099–4107. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Yan J, Zhou B, Taheri S and Shi H:
Differential effects of HIF-1 inhibition by YC-1 on the overall
outcome and blood-brain barrier damage in a rat model of ischemic
stroke. PLoS One. 6:e277982011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
McIlwain DR, Berger T and Mak TW: Caspase
functions in cell death and disease. Cold Spring Harb Perspect
Boil. 5:a0086562013.
|
|
44
|
O'Donovan N, Crown J, Stunell H, Hill AD,
McDermott E, O'Higgins N and Duffy MJ: Caspase 3 in breast cancer.
Clin Cancer Res. 9:738–742. 2003.PubMed/NCBI
|
|
45
|
Digicaylioglu M and Lipton SA:
Erythropoietin-mediated neuroprotection involves cross-talk between
Jak2 and NF-kappaB signalling cascades. Nature. 412:641–647. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bouscary D, Pene F, Claessens YE, Muller
O, Chrétien S, Fontenay-Roupie M, Gisselbrecht S, Mayeux P and
Lacombe C: Critical role for PI 3-kinase in the control of
erythropoietininduced erythroid progenitor proliferation. Blood.
101:3436–3443. 2003. View Article : Google Scholar
|
|
47
|
Haq R, Halupa A, Beattie BK, Mason JM,
Zanke BW and Barber DL: Regulation of erythropoietin-induced STAT
serine phosphorylation by distinct mitogen-activated protein
kinases. J Biol Chem. 277:17359–17366. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhi-Kun S, Hong-Qi Y, Zhi-Quan W, Jing P,
Zhen H and Sheng-Di C: Erythropoietin prevents PC12 cells from
beta-amyloid-induced apoptosis via PI3K⁄Akt pathway. Transl
Neurodegener. 1:72012. View Article : Google Scholar
|
|
49
|
Fan X, Heijnen CJ, van der KOOIJ MA,
Groenendaal F and van Bel F: Beneficial effect of erythropoietin on
sensorimotor function and white matter after hypoxia-ischemia in
neonatal mice. Pediatr Res. 69:56–61. 2011. View Article : Google Scholar
|
|
50
|
Wang Y, Zhang H, Liu Y, Li P, Cao Z and
Cao Y: Erythropoietin (EPO) protects against high glucose-induced
apoptosis in retinal ganglional cells. Cell Biochem Biophys.
71:749–755. 2015. View Article : Google Scholar
|
|
51
|
Cheng L, Yu H, Yan N, Lai K and Xiang M:
Hypoxia-inducible factor-1α target genes contribute to retinal
neuroprotection. Front Cell Neurosci. 11:202017. View Article : Google Scholar
|
|
52
|
Wang L, Zhao RP, Song XY and Wu WF:
Targeting ERβ in macrophage reduces crown-like structures in
adipose tissue by inhibiting osteopontin and HIF-1α. Sci Rep.
9:157622019. View Article : Google Scholar
|
|
53
|
Lee SH, Jeong D, Han YS and Baek MJ:
Pivotal role of vascular endothelial growth factor pathway in tumor
angiogenesis. Ann Surg Treat Res. 89:1–8. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Charriaut-Marlangue C, Margaill I, Represa
A, Popovici T, Plotkine M and Ben-Ari Y: Apoptosis and necrosis
after reversible focal ischemia: An in situ DNA fragmentation
analysis. J Cereb Blood Flow Metab. 16:186–194. 1996. View Article : Google Scholar : PubMed/NCBI
|