Introduction
Allergic rhinitis (AR), a non-infectious disease of
the nasal mucosa, is primarily mediated by immunoglobulin E (IgE)
following contact with allergens (1). The self-reported prevalence of AR in
11 cities across Mainland China had wide variations in 2005,
ranging between <10 and >20% (2); in 2011, the standardized prevalence
of adult AR in the 18 major cities was 17.6%, with the highest
prevalence of 23% in Shanghai and the lowest prevalence of 9.8% in
Chengdu (3). The number of
patients with AR in China has increased by 100 million between 2005
and 2011 (4). AR has
traditionally been considered to originate from a T helper
(Th)1/Th2 immune response imbalance, leading to allergic
inflammation dominated by the Th2 immune response within the nasal
mucosa (5). Following further
study, the pathogenesis of AR has been extended from the Thl/Th2
model to a Thl/Th2/Thl7 and T regulatory cell (Treg) model
(6). However, as AR is a
multi-factor disease induced by gene-environment interactions, its
exact pathogenesis has not been elucidated.
Lysine acetylation is a reversible
post-transcriptional modification that regulates changes in gene
expression profiles (7). Two
opposing enzymes function intracellularly to determine protein
acetylation levels; specifically, histone acetyltransferase (HAT)
catalyzes the addition of an acetyl group to lysine residues,
whereas histone deacetylase (HDAC) catalyzes the removal of an
acetyl group from lysine residues (7). The HAT/HDAC balance maintains
histone acetylation levels and regulates gene transcription
(8). Redox signaling, which is
mediated by HAT-induced inactivation of histone acetylation,
decisively contributes to the activation phase of the inflammatory
cascade (9). Targeting HAT Tip60
inhibits intestinal allergies in a mouse model (10). The expression of HDAC1, HDAC5,
HDAC6 and HDAC8 increases in asthmatic mice (11); HDAC11 (12) and HDAC1 (13) expression levels are increased in
patients with AR, and HDAC1 also participates in the pathogenesis
of childhood asthma (14).
Sodium butyrate (NaB) is an aliphatic acid and a
nonspecific HDAC inhibitor (15).
The results of our previous study indicated that NaB nasal drops
decreased the expression of HDAC1 and HDAC3 and increased histone
H3 acetylation at lysine 9 (H3-AcK9) (16). Butyrate is the final product of
the anaerobic fermentation of dietary fiber by intestinal
microorganisms (17), and
butyrate levels in stool samples from patients with atopic
dermatitis have been demonstrated to be decreased (18). Oral NaB may modulate brain
metabolism (19) and attenuate
experimental murine colitis in an IL-10 independent manner
(20).
The objective of the present study was to
investigate the preventive effect of NaB on AR by adding it to the
diet of newly weaned mice at 3 weeks of age and to determine the
changes in lncRNA and mRNA expression profiles in the nasal mucosa
following NaB treatment.
Materials and methods
Animals and trials
BALB/C mice (3 weeks old; 6-8 g) were purchased from
the Air Force Military Medical University (Xi'an, China). Mice were
maintained in a pathogen-free environment under a 12/12-h
light/dark cycle at 22°C with free access to food and water. All
animal experiments were conducted in accordance with the National
Institutes of Health guidelines and approved by the Committee on
Animal Research of the Air Force Military Medical University
(approval no. KJ-2016-XJB5436).
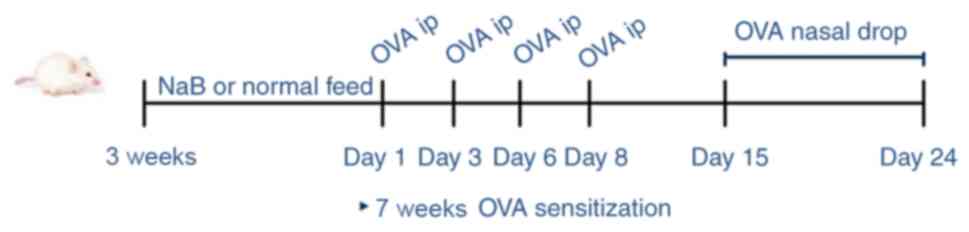
Mice were randomly divided into three groups (n=30
mice/group) as follows: i) Control (C) group (no treatment); ii) AR
group [treated with ovalbumin (OVA)]; and iii) NaB + AR group
(treated with OVA and NaB). Mice began to feed after weaning at 3
weeks of age. The mouse feed was premixed, 30 g/kg NaB
(Sigma-Aldrich; Merck KGaA) was added, and granules were produced.
Normal feed and NaB feed were provided by the Animal Center of the
Air Force Medical University. Each mouse in the NaB + AR group
consumed an average of 5 g feed/day, which contained 0.15 g NaB.
The other 2 groups were provided with normal feed throughout the
study period. At 7 weeks of age, mice in the AR and NaB + AR groups
received intraperitoneal injections of mixed OVA solution (20 mg)
and aluminum (2 mg) in 0.5 ml PBS on days 1, 3, 6 and 8, whereas
the control mice received injections of aluminum (2 mg) in 0.5 ml
PBS under the same schedule. Mice in the AR and NaB + AR groups
were also treated with 10% OVA (20 µl) via intranasal
instillation once daily between days 15 and 24. Mice in the control
group were treated with 20 µl PBS via intranasal
instillation once daily during the same period. Fig. 1 demonstrates the experimental
design. One hour after the last challenge, mice were anesthetized
(4% chloral hydrate, 400 mg/kg) and venous blood was obtained for
use in ELISA [mouse ELISA kits: IL-2 (cat. no. 223588), IL-4 (cat.
no. 221833), IL-5 (cat. no. 204523), IL-17 (cat. no. 100702),
interferon γ (IFN-γ; cat. no. 46107) and transforming growth
factor-β1 (TGF-β1; cat. no. 119557); all from Abcam]. Following
blood sample collection, the mice were sacrificed by cervical
dislocation, and the nasal mucosa was preserved in liquid nitrogen
for further analysis.
Behavioral assessment
Allergy symptoms were assessed using the following
scoring criteria: 1 point for sneezing 1-3 times during a 30-min
observation, clear nasal flow to the anterior nostril and
occasional scratching of the nose with a single front limb; 2
points for sneezing 4-10 times, clear nasal flow beyond the nostril
and scratching of the nose with both front limbs; and 3 points for
sneezing >10 times, clear nasal flow to the face and continuous
scratching. After the last stimulation, each animal was observed
for 30 min, and the three parameters were recorded and quantified.
A total score >5 points indicated that the model was
successfully established (21).
Histological observation
The muscle tissue of the nose was removed, and the
nasal cavity was fixed in 4% formaldehyde for 24 h at 37°C.
Following 10% EDTA decalcification for 24 h at 37°C, the nose was
embedded in paraffin, and 4-µm sections were cut. The
sections (4-µm) were dewaxed, stained with hematoxylin (cat.
no. 245880; Abcam) for 10 min, differentiated with 1% hydrochloric
acid ethanol for 1 min, stained with eosin for 1 min, dehydrated
with a series of ethanol concentrations (70, 80, 90 and 100%)
ethanol for 10 sec, incubated with xylene for 1 min and sealed. In
addition, other sections were dewaxed, soaked with 3% acetic acid
for 3 min, stained with 1% Alcian blue (cat. no. 150680; Abcam) for
30 min, soaked with 3% acetic acid for 3 min, washed with water,
oxidized with 0.5% periodate for 10 min, soaked in Schiff's
solution for 20 min and sealed.
Western blotting
Proteins were obtained from the nasal mucosa tissues
of each mouse 1 h after the final intranasal administration of OVA
or PBS. Proteins were extracted using a Protein Extraction kit
(Applygen Technologies, Inc.), and total protein concentrations
were measured using the Bio-Rad protein assay kit (Bio-Rad
Laboratories, Inc.). A total of 20 µg protein/lane was
isolated by 12.5% sodium dodecyl sulfate-polyacrylamide gel
electrophoresis and transferred to a nitrocellulose membrane
(Bio-Rad Laboratories, Inc.). The membranes were blocked with 2.5%
nonfat milk at 37°C for 1 h and incubated with anti-HDAC1 (mouse;
1:1,000; cat. no. 5356), anti-H3 (rabbit; 1:1,000; cat. no. 4499),
anti-H3-AcK9 (rabbit; 1:1,000; cat. no. 9649S; all from Cell
Signaling Technology, Inc.), anti-HDAC8 (rabbit; 1:1,000; cat. no.
187139; Abcam) and anti-GAPDH (mouse; 1:1,000; cat. no. 686613;
R&D Systems, Inc.) antibodies overnight at 4°C. Following
exposure to horseradish peroxidase-conjugated anti-mouse and
anti-rabbit IgG secondary antibodies (1:200; Sigma-Aldrich; Merck
KGaA) for 1 h at 37°C, immunoreactive bands were detected using an
enhanced chemiluminescence western blotting system (Thermo Fisher
Scientific, Inc.).
RNA microarray
The CapitalBio Technology Mouse LncRNA Array v1 was
designed with four identical arrays per slide (4X180K format), with
each array containing probes for 58,809 mouse lncRNAs and 39,027
mouse mRNAs. The lncRNA and mRNA target sequences were obtained by
merging the results from multiple databases, including NCBI RefSeq
(https://www.ncbi.nlm.nih.gov/), Ensembl
(http://asia.ensembl.org/index.html),
UCSC (http://www.genome.ucsc.edu/), FANTOM
(https://fantom.org/), LncRNAdb (http://live.dbpedia.org/page/LncRNAdb/),
NO NCODE V4.0 (http://www.noncode.org/), UCR (https://www.ucr.edu/), LncRNA Disease (http://www.cuilab.cn/lncrnadisease) and
LncRNA.org (https://lncipedia.org/). Each RNA was detected by
probes based on ≥2 replicates. The array also contained 4,974
Agilent control probes.
RNA extraction, amplification, labeling
and hybridization
The microarray assay was performed by Capital
Biotech Corporation (Beijing, China) with the Agilent mouse lncRNA
+ mRNA Array V4.0 (4X180K) (Agilent Technologies, Inc.) according
to the manufacturer's instructions. Total RNA was extracted using
TRIzol® reagent (Invitrogen; Thermo Fisher Scientific,
Inc.) according to the manufacturer's instructions. Briefly, 200 ng
purified RNA from each sample was amplified and reverse-transcribed
into cDNA. The cDNAs were transcribed into cRNAs at 70°C for 5 min,
25°C for 5 min and 4°C for 2 min, and the cRNAs were transcribed
into cDNAs using the WT Expression Kit (cat. no. 4411973; Thermo
Fisher Scientific, Inc.) at 70°C for 5 min, 25°C for 5 min and 4°C
for 2 min, labeled with a fluorescent dye (Cy3-dCTP, Agilent
Technologies, Inc.), denatured at 95°C for 3 min and incubated in
an ice bath for 5 min. Labeled cDNAs were hybridized onto a Crystal
core human lncRNA chip V4.0. The microarray data analyzed in the
present study have been deposited in the NCBI GEO database under
the accession number GSE140454.
Microarray imaging and data analysis
The lncRNA and mRNA array data were analyzed for
data summarization, normalization and quality control using Gene
Spring software V12.0 (Agilent Technologies, Inc.). To identify the
differentially expressed genes, the threshold values of fold-change
≥2 and ≤−2 and a Benjamini-Hochberg corrected P-value <0.05 were
used. The data were log2-transformed and median-centered
on genes using the 'Adjust Data' function of CLUSTER 3.0 software
(Michiel de Hoon, University of Tokyo, Human Genome Center) prior
to further analysis via hierarchical clustering with average
linkage. Tree visualization was performed using Java Treeview 3.0
(Stanford University School of Medicine).
RNA isolation and reverse
transcription-quantitative PCR (RT-qPCR)
Total RNA was extracted using TRIzol®
reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to
the manufacturer's instructions. The concentration, quality and
purity of RNA were assessed using the RNA 6000 Nano assay on the
Agilent 2100 Bioanalyzer (Agilent Technologies, Inc.). No samples
exhibited RNA degradation (ratio of 28S:18S ribosomal RNA ≥2) or
contamination with DNA. For reverse transcription, samples were
incubated in an Eppendorf PCR system at 42°C for 30 min, 90°C for 5
min and 5°C for 5 min. The samples were subjected to qPCR with
specific primers (Table SI).
qPCR was performed in a 10 µl total volume containing 1
µl cDNA, 5 µl SYBR® Green Real-time PCR
Master Mix (Toyobo Life Science) and 1 µl of each primer
under the following conditions: 95°C for 10 sec at; 40 cycles of
60°C for 5 sec and 72°C for 10 sec; and 65°C for 30 sec. Melting
analysis of PCR products was conducted to validate the
amplification of a specific product, and the relative fold-change
was calculated using the 2−∆∆Cq method normalized to
GAPDH (22).
LncRNA-mRNA co-expression and
construction of the coding-non-coding gene co-expression
network
Differentially expressed mRNAs were used to
construct a co-expression network to explore specific lncRNAs
involved in the pathogenesis of AR. Pearson correlation
coefficients (PCCs) were calculated between selected mRNAs and all
differentially expressed lncRNAs. A PCC ≥0.99 indicated that the
selected lncRNA and mRNA formed a significantly correlated
pair.
The coding-non-coding gene co-expression network was
constructed based on the correlation analysis between
differentially expressed lncRNAs and mRNAs. Significantly
correlated pairs (based on PCC) were selected to construct the
network. LncRNAs and mRNAs with PCCs ≥0.99 were selected to draw
the network using the open-source bioinformatics software Cytoscape
3.7.2 (https://cytoscape.org/). For network
analysis, a degree of centrality was defined as the number of links
that one node had to others.
Prediction of cis-acting and trans-acting
lncRNA
The prediction of cis-acting lncRNA was performed
based on a strong correlation between the lncRNA and a group of
expressed protein-coding genes (PCC ≥0.99). The lncRNAs were only
selected if they resided at the genomic loci where a protein-coding
gene and an lncRNA gene were within 10 kb of each other along the
genome; 'cis' therefore refers to the same locus (not necessarily
the same allele) regulatory mechanism, which included the
antisense-mediated regulation of protein-coding genes by lncRNAs
that in the same locus.
The trans-prediction was conducted using a
Standalone BLAT v. 35 × 1 fast sequence search command line tool
(http://hgdownload.cse.ucsc.edu/admin/exe/) to compare
the full sequence of the lncRNA to the 3′-untranslated region of
its co-expressed mRNAs using default parameter settings.
Analysis of Gene Ontology (GO) and
PANTHER pathways
The functions of biological processes differentially
expressed geneswere identified by GO analysis (http://geneontology.org/). The differentially
expressed mRNAs were analyzed using PANTHER analysis (http://pantherdb.org/).
Statistical analysis
Data are presented as the means ± SD. Analyses were
performed using SPSS version 13.0 (SPSS, Inc.). Unpaired Student's
t-test was used to identify differences between two groups. One-way
ANOVA followed by the least significant difference test was used to
compare multiple groups. Analysis of mRNA, lncRNA and RT-qPCR
fold-change data were performed by Student's t-test using Microsoft
Excel 15.17 (Microsoft Corporation). P<0.05 was considered to
indicate a statistically significant difference.
Results
Oral NaB decreases the AR-related
behavioral score and improves nasal mucosal morphology
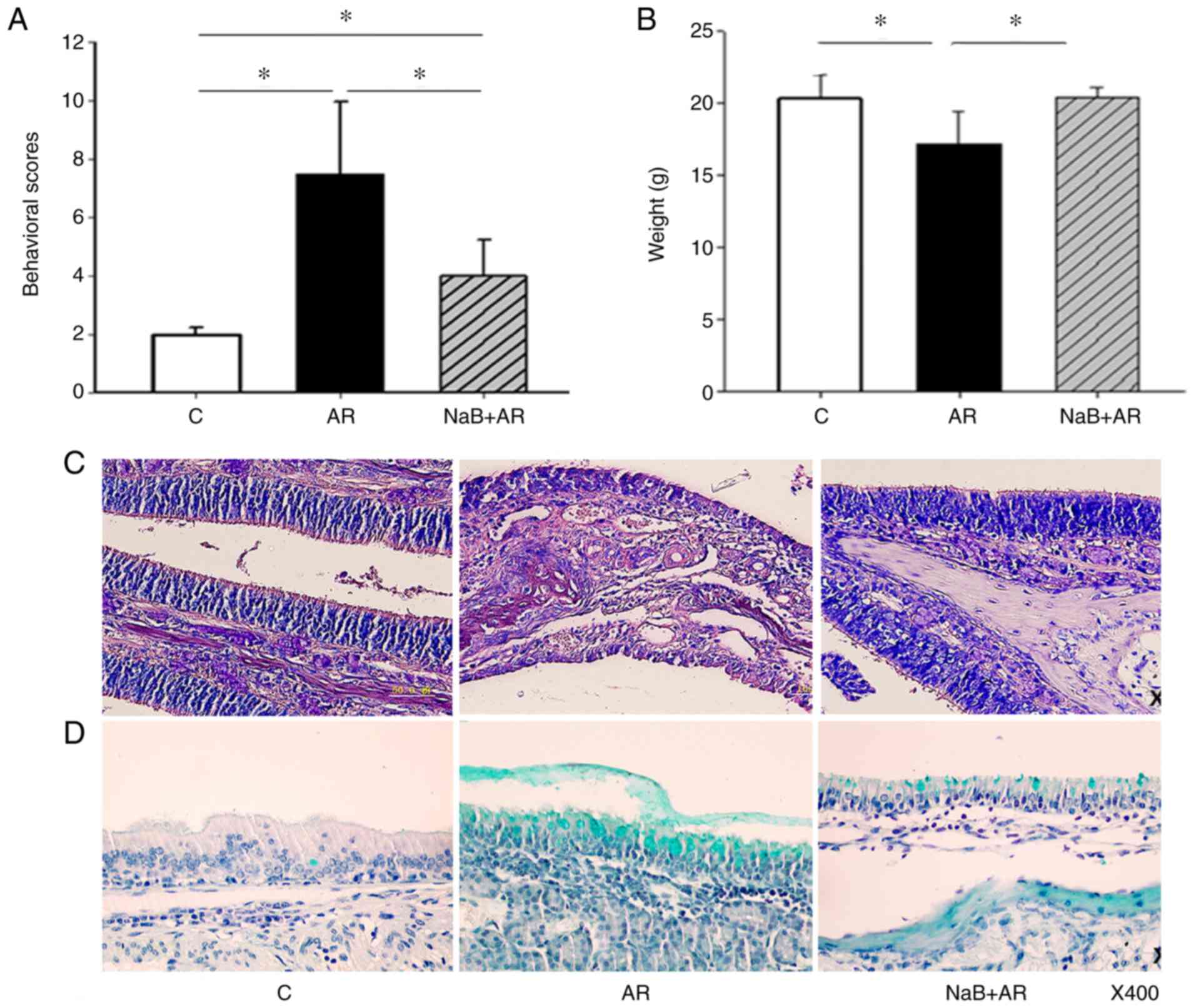
NaB treatment decreased the behavioral scores of
mice with AR (Fig. 2A). In
addition, mice fed NaB for 7 weeks did not experience diarrhea or
other adverse effects and gained weight normally (Fig. 2B). Epithelial cells of the nasal
mucosa in the AR group exhibited loss of cilia, edema of the
sub-mucosal tissue, small vessel proliferation, infiltration of
eosinophils (Fig. 2C) and
exuberant secretion of goblet cells (Fig. 2D). NaB treatment reduced nasal
mucosal inflammation in AR mice (Fig.
2C and D). These results indicated that NaB could prevent AR,
and that 7 weeks of NaB feeding did not affect mouse growth.
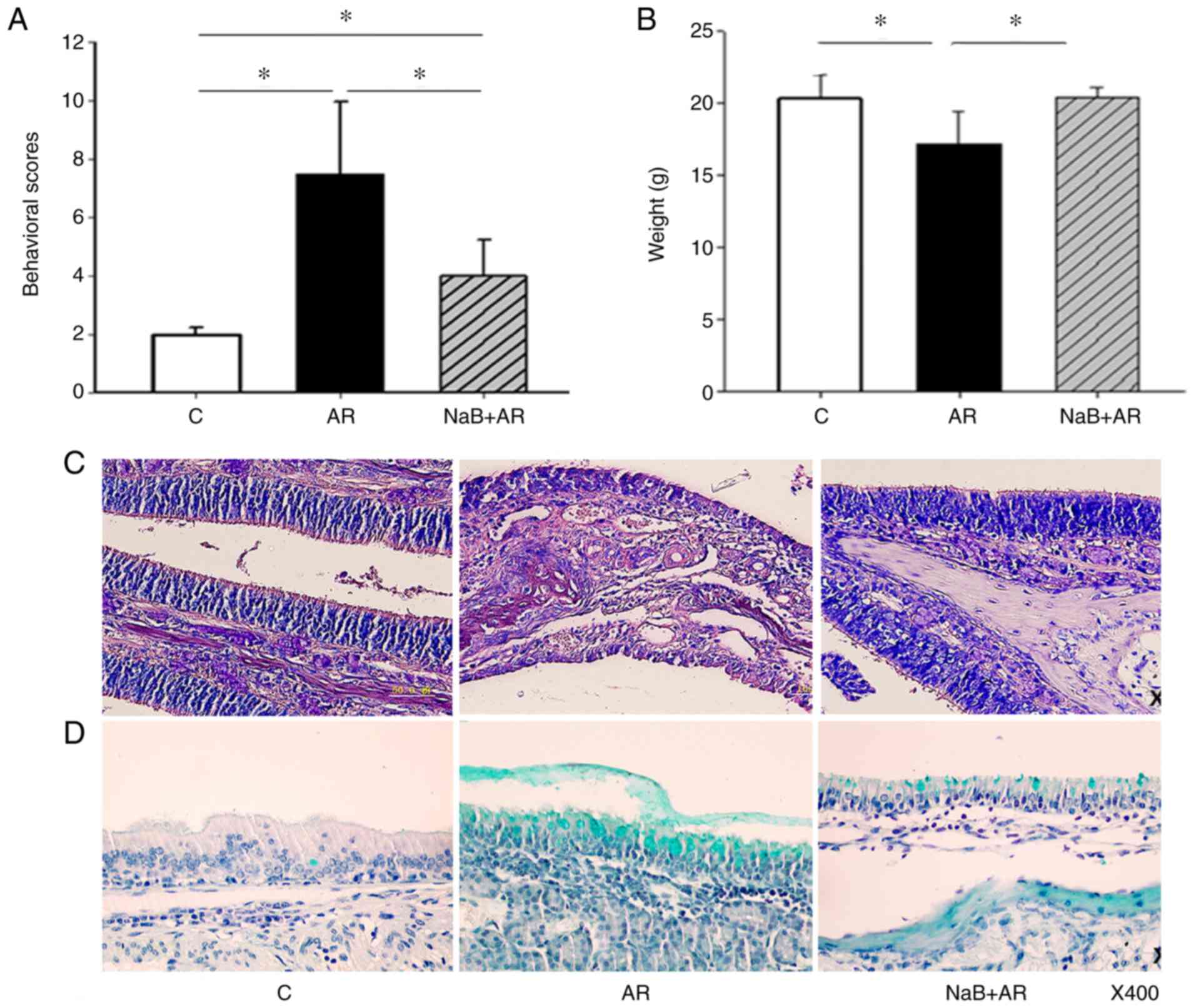 | Figure 2NaB improves symptoms of allergic
rhinitis in a mouse model. (A) In the AR group, the behavioral
scores were higher compared with the C group. NaB treatment
decreased the behavioral scores in the NaB + AR group compared with
those in the AR group, although significant differences in
behavioral scores were present between the C and NaB + AR groups.
(B) The average bodyweight in the AR group was significantly lower
compared with the C and NaB + AR groups. No significant differences
were observed between the bodyweights in the C and NaB + AR groups.
(C) Hematoxylin and eosin staining of epithelial cells of the nasal
mucosa in the AR group revealed loss of cilia, edema of sub-mucosal
tissue, proliferation of small vessels and infiltration of
eosinophils. (D) Alcian blue staining demonstrated exuberant
secretion by goblet cells. The NaB + AR group exhibited less cilia
loss, edema of sub-mucosal tissue, proliferation of small vessels,
infiltration of eosinophils and secretion of goblet cells compared
with the AR group. Data are presented as the mean ± SD. *P<0.05.
NaB, sodium butyrate; C, control group; AR, rats treated with
ovalbumin; NaB + AR, rats treated with NaB and ovalbumin. |
NaB rebalances Th1/Th2/Thl7 and Treg
ratios in AR mouse mucosa
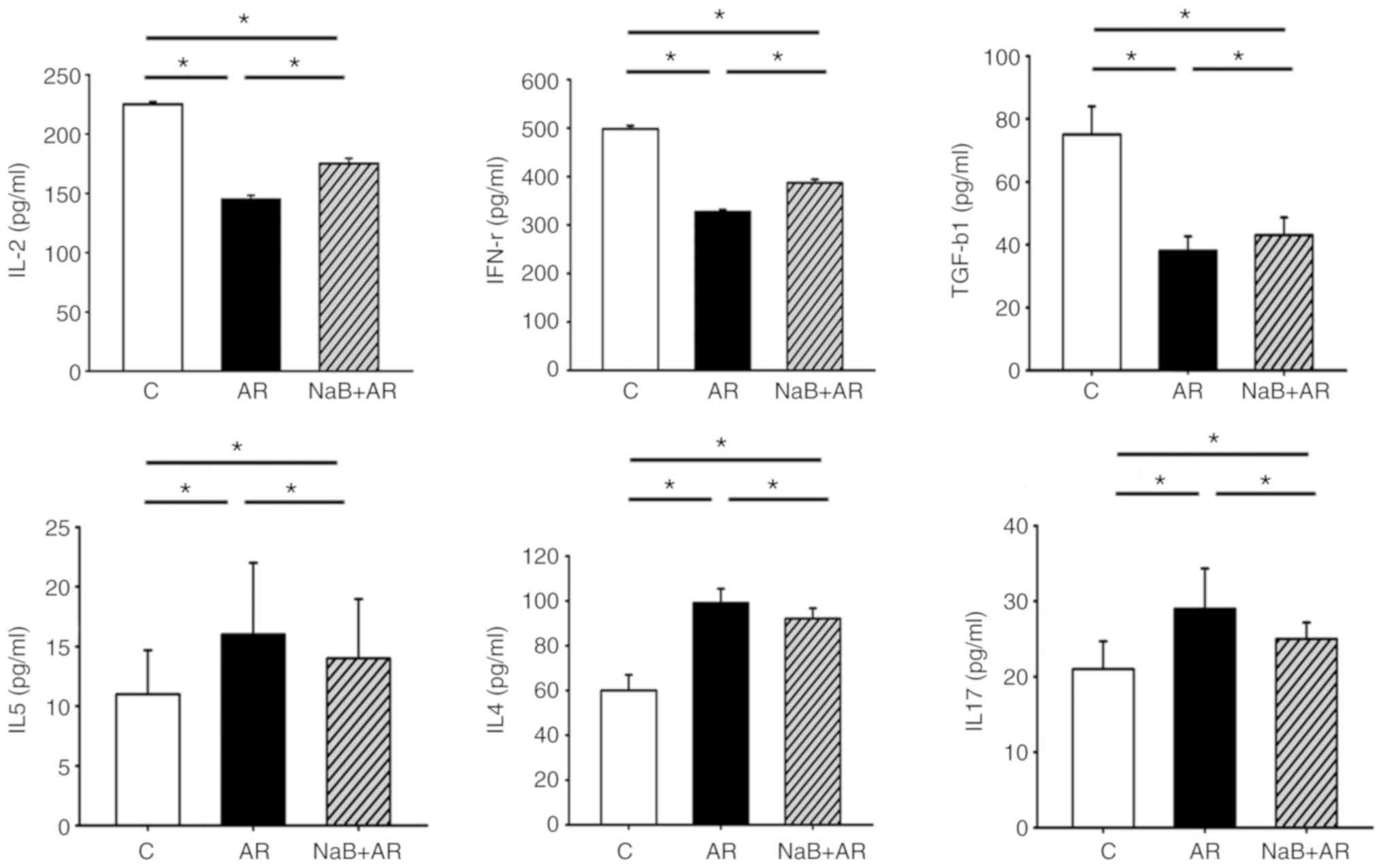
Following treatment of AR mice with NaB, serum ELISA
demonstrated that the expression of IL-2 (a marker of Th1), IFN-γ
(a marker of Th1) and TGF-β1 (a marker of Treg) was higher, whereas
the levels of IL-4 (a marker of Th2), IL-5 (a marker of Th2) and
IL-17 (a marker of Th17) were lower in the NaB + AR group compared
with that in the AR group. These results indicated that NaB could
restore Thl/Th2/Thl7 and Treg balance in AR mice (Fig. 3).
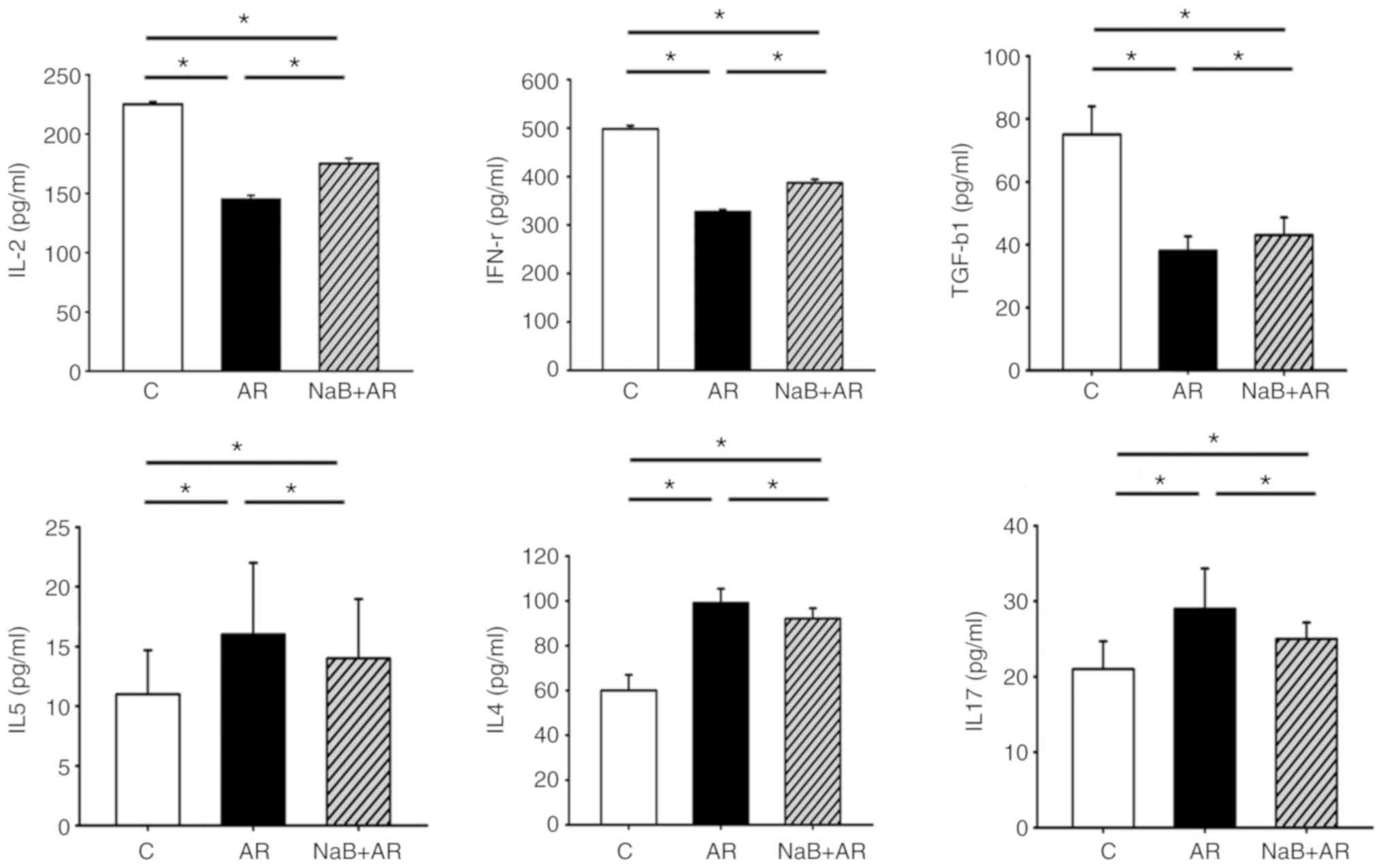 | Figure 3Serum ELISA results of IL-2, IFN-γ,
TGF-β1, IL-4, IL-5 and IL-17. The expression levels of IL-2, IFN-γ
and TGF-β1 were lower, whereas those of IL-4, IL-5 and IL-17 were
higher in the AR group compared with the C group. NaB treatment
increased the expression of IL-2, IFN-γ and TGF-β1 and decreased
the expression of IL-4, IL-5 and IL-17 compared with the AR group,
although significant differences in ELISA results were present
between the C and NaB + AR groups. Data are presented as the mean ±
SD. *P<0.05. IL, interleukin; INF-γ, interferon γ;
TGF-β1, transforming growth factor β1; NaB, sodium butyrate; C,
control group; AR, rats treated with ovalbumin; NaB + AR, rats
treated with NaB and ovalbumin. |
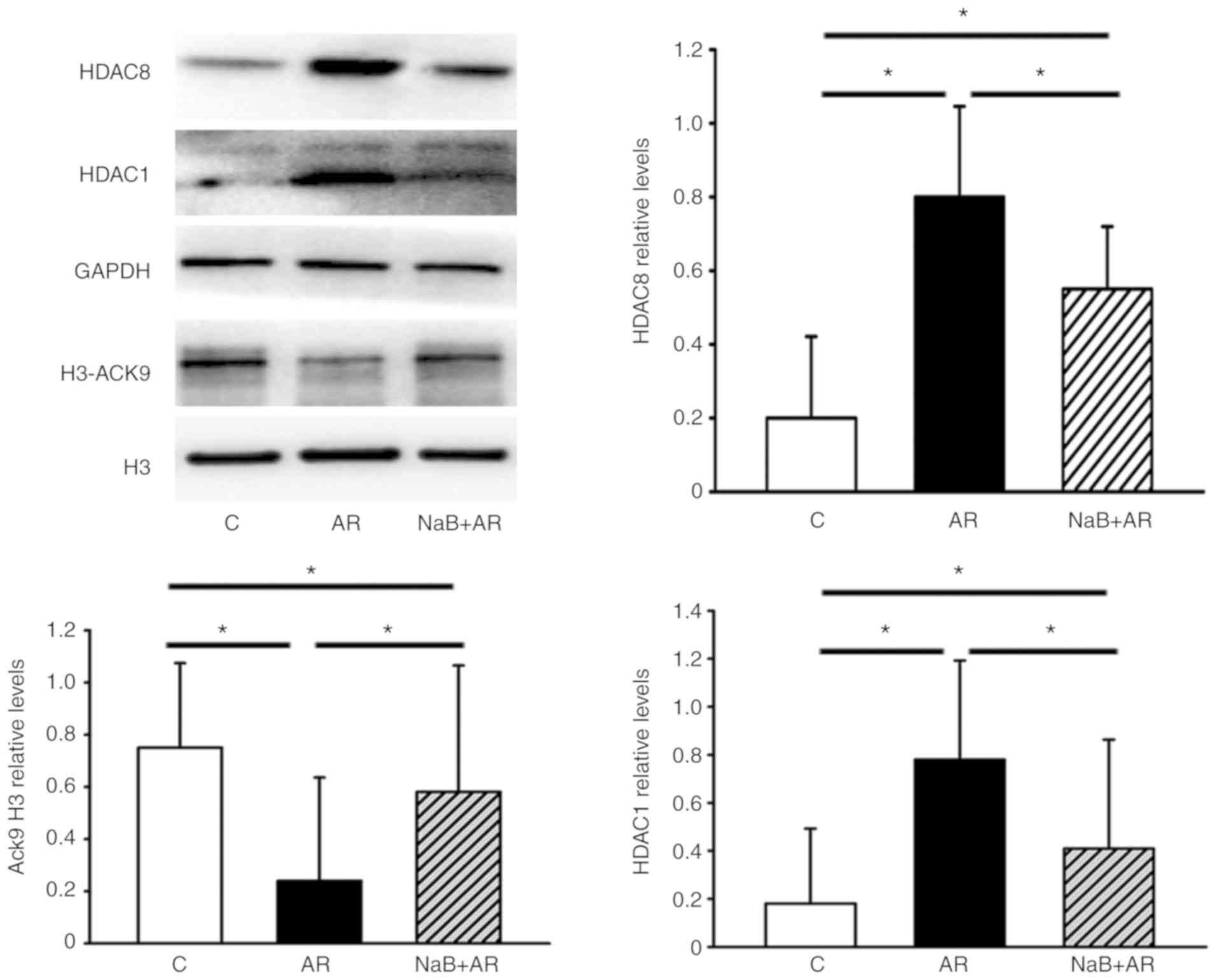
NaB normalizes the AR-induced
downregulation of H3-AcK9 and upregulation of HDAC1 and HDAC8
expression in mouse mucosa
NaB partially reversed the downregulation of H3-AcK9
and upregulation of HDAC1 and HDAC8 expression induced by AR in the
nasal mucosa of mice (Fig. 4).
These results suggested that NaB could restore the HDAC/HAT
balance.
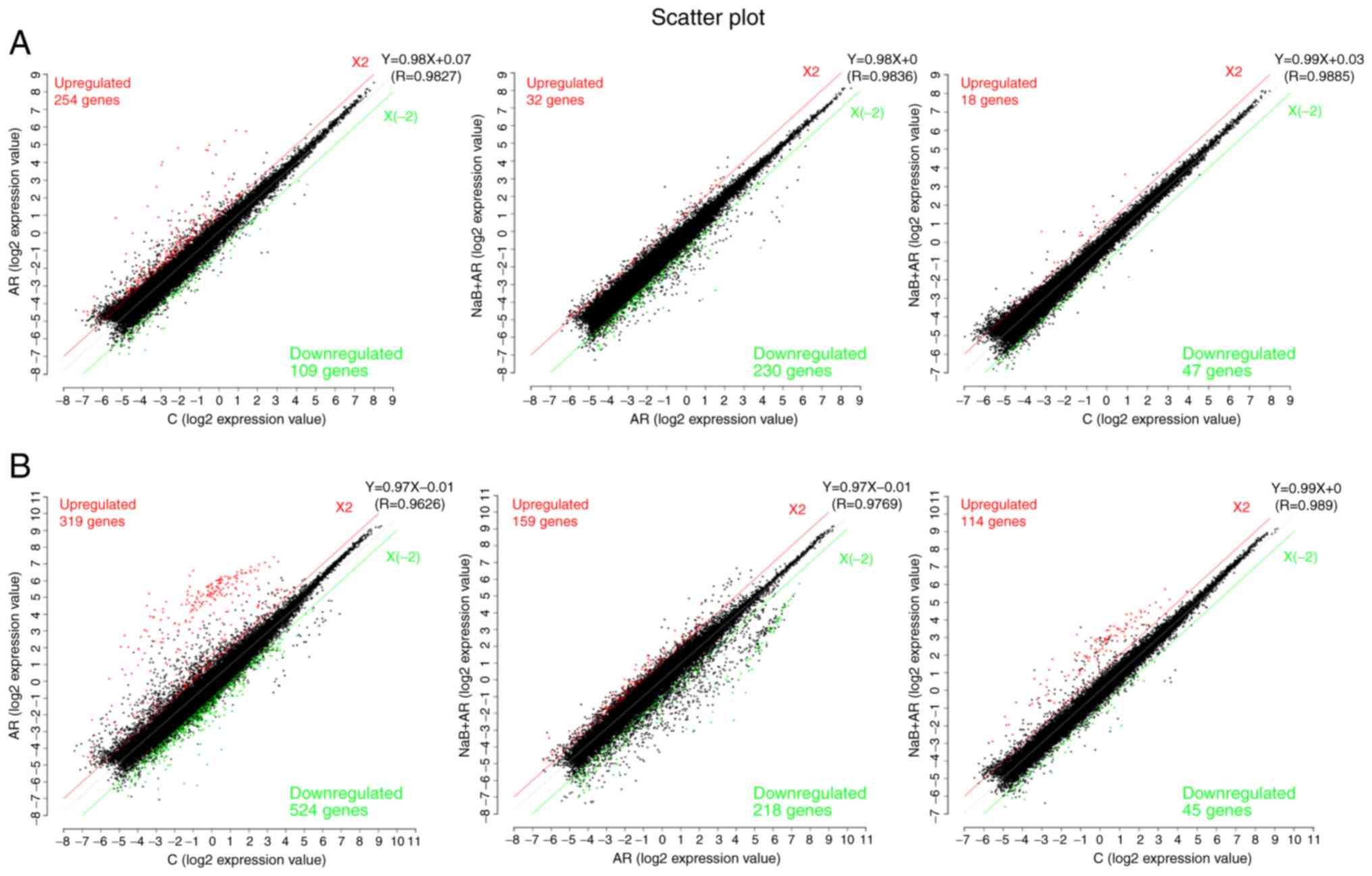
Differences in lncRNA and mRNA expression
profiles in the nasal mucosa among the three groups
A scatter function was used to identify the
differences in lncRNA and mRNA expression (log2
expression value) among the three groups. LncRNA analysis
demonstrated that compared with the expression levels in the C
group, 254 genes were upregulated and 109 were downregulated in the
AR group, and 18 genes were upregulated and 47 were downregulated
in the NaB + AR group. Compared with the AR group, 32 genes were
upregulated and 230 were downregulated in the NaB + AR group
(Fig. 5A). mRNA analysis revealed
that compared with the expression levels in the C group, 319 genes
were upregulated and 524 were downregulated in the AR group, and
159 genes were upregulated and 218 were downregulated in the NaB +
AR group. Compared with the AR group, 114 genes were upregulated
and 45 were downregulated in the NaB + AR group (Fig. 5B).
LncRNA (NONMMUT057309), lncRNA (NONMMUT016103)
(Table I) and 33 mRNAs (Table II) were identified to be
co-expressed, and expression trends for these markers were
consistent among the C, AR and NaB + AR groups. The 33 mRNAs
encoded immunoglobulins, suggesting that lncRNA may regulate the
expression of immunoglobulins during AR inflammation.
 | Table ILncRNA (NONMMUT057309) and lncRNA
(NONMMUT016103) expression trends among the C, AR, and NaB + AR
groups. |
Table I
LncRNA (NONMMUT057309) and lncRNA
(NONMMUT016103) expression trends among the C, AR, and NaB + AR
groups.
| LncRNA | Chr | Gene ID | NaB + AR vs. C
| NaB + AR vs. AR
| C vs. AR
|
|---|
| P-value | |FC| | Regulation | P-value | |FC| | Regulation | P-value | |FC| | Regulation |
|---|
| NONMMUT016103 | 12 | NONMMUG0
10108.2 | 0.04 | 3.8545 | Up | 0.04 | 11.5375 | Down | 0.01 | 44.4719 | Up |
| NONMMUT057309 | 6 | NONMMUG0
35579.2 | 0.03 | 2.4944 | Up | 0.04 | 4.9847 | Down | 0.01 | 12.4342 | Up |
 | Table IICo-expressed mRNAs encoding
immunoglobulins (n=33) among the C, AR, and NaB + AR groups. |
Table II
Co-expressed mRNAs encoding
immunoglobulins (n=33) among the C, AR, and NaB + AR groups.
| mRNA | Description | ID |
|---|
| A_52_P382676 | Immunoglobulin
heavy variable 6-6 [Source:MGI Symbol;Acc:MGI:4439619] |
ENSMUST00000103489 |
| A_55_P2001269 | Immunoglobulin
heavy variable 1-52 [Source:MGI Symbol;Acc:MGI:4439752] |
ENSMUST00000103522 |
| A_55_P2046653 | Immunoglobulin
heavy variable 2-9 [Source:MGI Symbol;Acc:MGI:4439624] |
ENSMUST00000103451 |
| A_55_P2060897 | Immunoglobulin
kappa constant [Source:MGI Symbol;Acc:MGI:96495] |
ENSMUST00000103410 |
| A_66_P114582 | Immunoglobulin
heavy variable V1-54 [Source:MGI Symbol;Acc:MGI:3647133] |
ENSMUST00000103525 |
| A_55_P2001274 | Immunoglobulin
heavy variable 1-62-3 [Source:MGI Symbol;Acc:MGI:3648544] |
ENSMUST00000103532 |
| A_55_P2130497 | Immunoglobulin
heavy variable V1-67 [Source:MGI Symbol;Acc:MGI:3645228] |
ENSMUST00000103538 |
| A_55_P2030299 | Immunoglobulin
heavy variable V14-3 [Source:MGI Symbol;Acc:MGI:4439764] |
ENSMUST00000103469 |
| A_55_P1993001 | Immunoglobulin
heavy variable 1-55 [Source:MGI Symbol;Acc:MGI:4439716] |
ENSMUST00000103526 |
| A_55_P2058621 | Mus musculus clone
J558.2 immunoglobulin heavy chain variable region mRNA, partial
cds | AF303833 |
| A_52_P15966 | Immunoglobulin
heavy variable 1-84 [Source:MGI Symbol;Acc:MGI:3644235] |
ENSMUST00000103551 |
| A_65_P07626 | Immunoglobulin
kappa variable 3-2 [Source:MGI Symbol;Acc:MGI:1330850] |
ENSMUST00000103403 |
| A_55_P2187234 | Immunoglobulin
heavy variable 2-2 [Source:MGI Symbol;Acc:MGI:4439894] |
ENSMUST00000103443 |
| A_55_P2052913 | Immunoglobulin
heavy variable 5-9 [Source:MGI Symbol;Acc:MGI:4439873] |
ENSMUST00000103448 |
| A_55_P1979364 | Immunoglobulin
heavy variable 1-83 [Source:MGI Symbol;Acc:MGI:3648939] |
ENSMUST00000103550 |
| A_55_P2159911 | Immunoglobulin
heavy variable 2-3 [Source:MGI Symbol;Acc:MGI:4439872] |
ENSMUST00000178229 |
| A_52_P320761 | Immunoglobulin
heavy variable 1-31 [Source:MGI Symbol;Acc:MGI:4439889] |
ENSMUST00000103511 |
| A_55_P2026268 | Immunoglobulin
kappa chain variable 5-43 [Source:MGI Symbol;Acc: MGI:4943320] |
ENSMUST00000103368 |
| A_52_P213483 | Immunoglobulin
heavy variable 1-77 [Source:MGI Symbol;Acc:MGI:4439670] |
ENSMUST00000170551 |
| A_55_P1969901 | Immunoglobulin
heavy variable 1-80 [Source:MGI Symbol;Acc:MGI:4439738] |
ENSMUST00000103547 |
| A_52_P502849 | Immunoglobulin
kappa variable 3-4 [Source:MGI Symbol;Acc:MGI:1330855] |
ENSMUST00000103401 |
| A_51_P461067 | Immunoglobulin
heavy constant gamma 1 [Source:MGI Symbol;Acc: MGI:96446] |
ENSMUST00000103420 |
| A_55_P1970464 | Immunoglobulin
heavy variable 1-22 [Source:MGI Symbol;Acc:MGI:4439784] |
ENSMUST00000103507 |
| A_55_P2155560 | Immunoglobulin
heavy variable V1-5 [Source:MGI Symbol;Acc:MGI:3704121] |
ENSMUST00000103494 |
| A_55_P2134277 | Immunoglobulin
heavy variable V1-18 [Source:MGI Symbol;Acc:MGI:4439780] |
ENSMUST00000103504 |
| A_66_P103232 | Immunoglobulin
kappa chain variable 5-45 [Source:MGI Symbol;Acc: MGI:4439774] |
ENSMUST00000103366 |
| A_55_P2065506 | Immunoglobulin
heavy variable 1-36 [Source:MGI Symbol;Acc:MGI:4439639] |
ENSMUST00000103513 |
| A_55_P2129334 | Mus musculus clone
L2MZB-13.3 immunoglobulin heavy chain variable region mRNA, partial
cds | AY171990 |
| A_55_P2138627 | Immunoglobulin
heavy variable 6-3 [Source:MGI Symbol;Acc:MGI:4439854] |
ENSMUST00000103486 |
| A_55_P2164784 | Immunoglobulin
heavy variable 2-5 [Source:MGI Symbol;-Acc:MGI:4439517] |
ENSMUST00000103449 |
| A_66_P104923 | Immunoglobulin
heavy variable 1-81 [Source:MGI Symbol;Acc:MGI:4439635] |
ENSMUST00000103548 |
| A_51_P390937 | Immunoglobulin
kappa variable 14-111 [Source:MGI Symbol;Acc:MGI:4439863] |
ENSMUST00000103320 |
| A_55_P2187235 | Immunoglobulin
heavy variable 2-2 [Source:MGI Symbol;Acc:MGI:4439894] |
ENSMUST00000103443 |
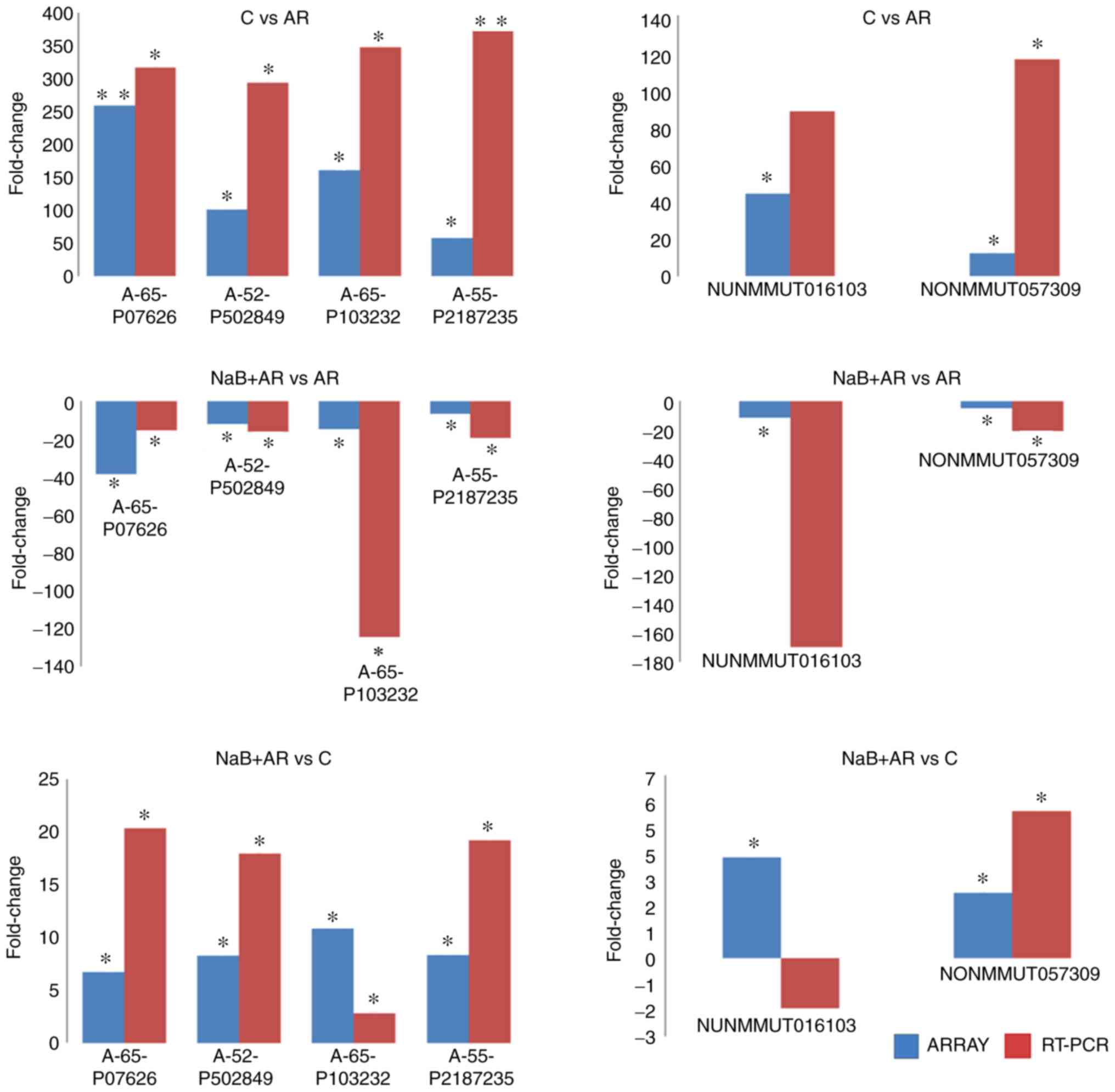
RT-qPCR validation of microarray
data
Statistically significant differences were
identified at four mRNA (A-65-P07626, A-52-P50284, A-66-P10323 and
A-55-P21872) and two lncRNA (NONMMUT016103 and NONMMUT057309) loci
between C vs. AR, NaB + AR vs. AR and NaB + AR vs. C groups in the
microarray results. RT-qPCR validation results in the three groups
were consistent with the micro-array analysis results, with the
exception of the lncRNA (NUNMMUT016103) locus (Fig. 6).
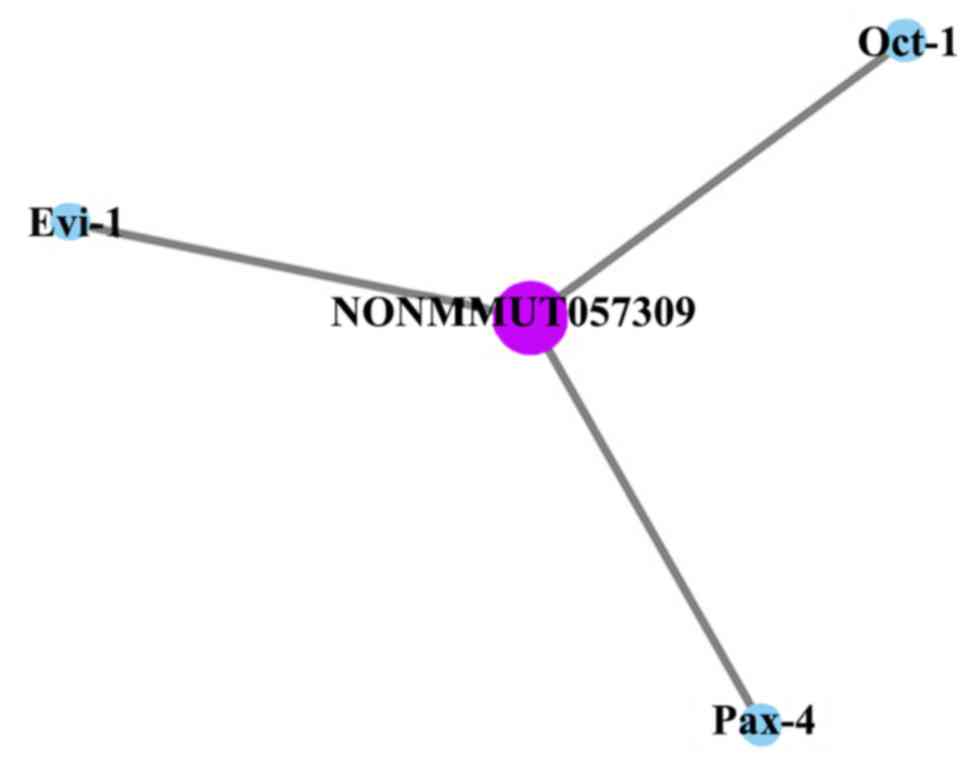
LncRNA (NONMMUT057309)-mRNA co-expression
analysis
LncRNA (NONMMUT057309) co-expression analysis of
mRNA (data not shown) and target gene prediction (Fig. 7) revealed that only three target
genes of lncRNA (NONMMUT057309) [octamer-binding transcription
factor 1 (Oct-1), ecotropic viral integration site 1 (Evi-1) and
paired box 4 (Pax-4)] were predicted between NaB + AR vs. AR, NaB +
AR vs. C and AR vs. C groups.
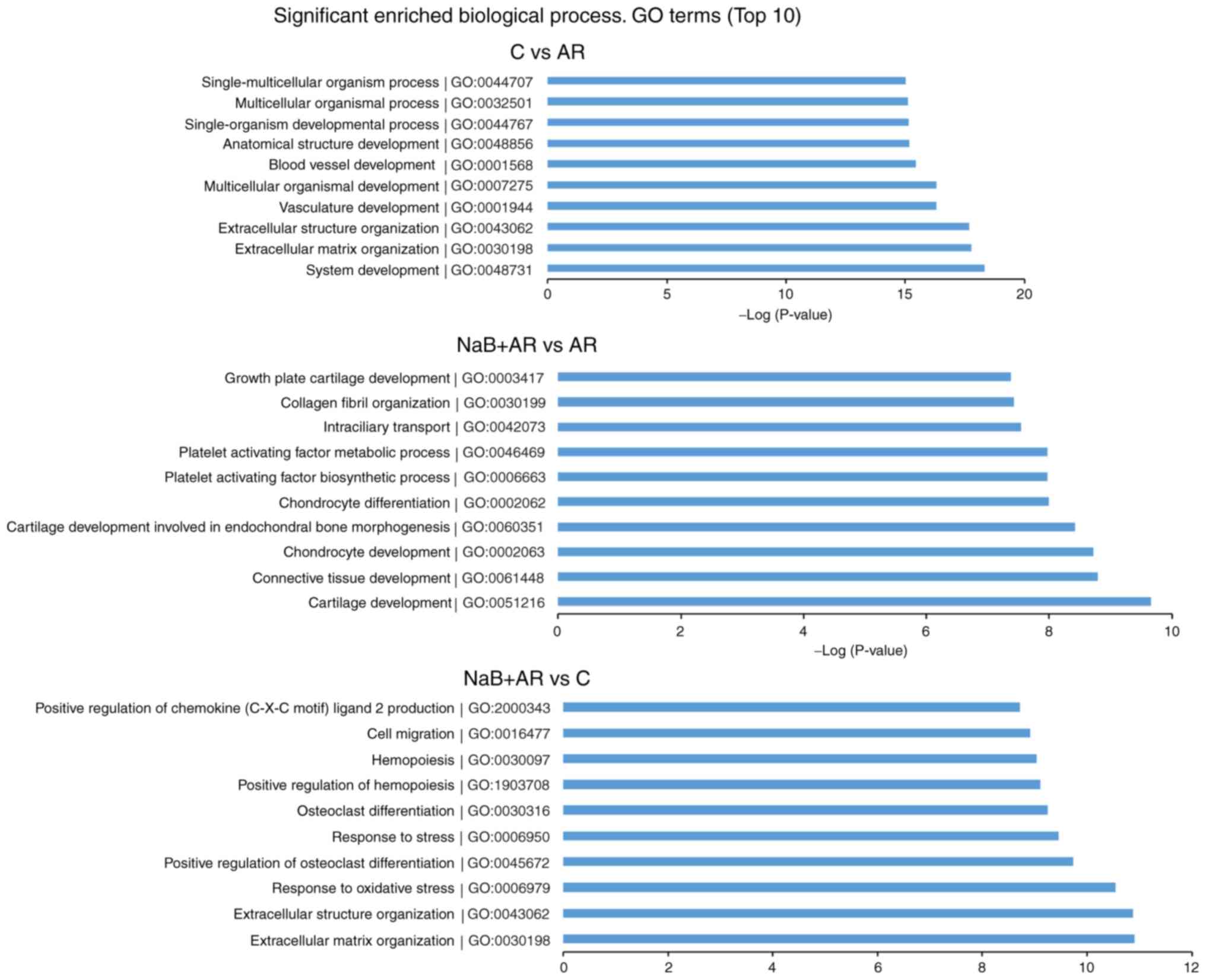
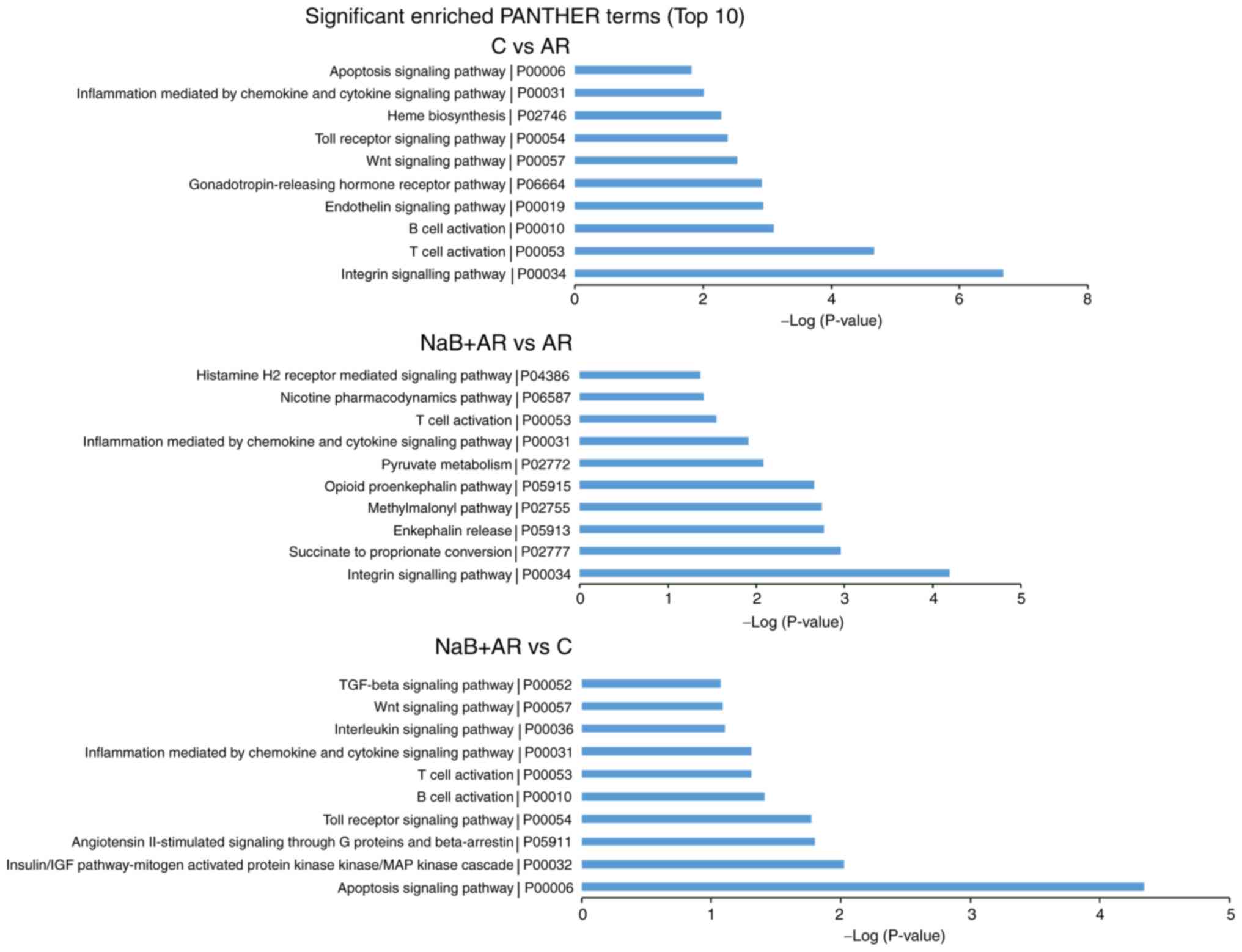
GO and PANTHER pathway analyses
GO analysis was conducted to determine the
enrichment of the differentially expressed mRNAs between the
different groups in the categories of biological processes. The top
10 significantly enriched GO terms between each pair of groups are
presented in Fig. 8.
Pathway analysis was conducted to determine the
biological pathways represented by the significantly differentially
expressed mRNAs between the groups. The top 10 significantly
enriched PANTHER pathway terms among the three groups are presented
in Fig. 9. Based on these
results, inflammation mediated by chemokine and cytokine signaling
pathways and T-cell activation were suggested to be involved in AR
pathogenesis.
Discussion
HDAC inhibitors can be divided into four categories,
including hydroxamates, cyclic peptides, aliphatic acids and
benzamides. Suberoylanilide hydroxamic acid (SAHA) has been
approved by the US Food and Drug Administration for the treatment
of cutaneous T-cell lymphoma (7).
HDAC inhibitors have also been demonstrated to exhibit therapeutic
effects in cancer, arthritis, hearing loss and asthma (23-27). Since epigenetic modifications,
which contribute to disease development, are neither permanent nor
transient, identifying disease-specific epigenetic alterations may
help identify novel therapeutic interventions (28,29). NaB can be dissolved without
dimethyl sulfoxide, which is a solvent that also inhibits HDAC,
thus enabling the sole evaluation of NaB and its effects (30,31). The results of our previous study
demonstrated that NaB exhibited a therapeutic effect in an
OVA-induced murine AR model when administered intranasally
(16). The present study
demonstrated that oral NaB for 7 weeks did not result in any
adverse effects, and animals gained weight normally. In addition, a
previous study revealed that NaB enhanced intestinal integrity in
weaned pigs (32). Adding NaB
increased the food intake of lactating sows and improved the growth
of piglets (33). In the present
study, NaB prophylactically reduced AR-related behavioral scores,
improved nasal mucosal morphology and restored Th1/Th2/Thl7 and
Treg cell balance. Thus, NaB may exhibit a preventive effect on AR.
The present study demonstrated that NaB increased H3-AcK9
expression and decreased of HDAC1 and HDAC8 expression in mice with
AR. Accordingly, high HDAC1 and HDAC8 expression levels have been
observed in OVA-sensitized asthmatic mice (11). In addition, an HDAC8-specific
inhibitor was demonstrated to reduce the eosinophil-mediated
inflammatory response and reduce the sensitivity of the airway in
an asthma model (34). Therefore,
blocking HDAC activity may be a novel therapeutic target in
patients with AR (7).
LncRNA regulates gene expression at the
transcriptional, RNA processing and translational levels (35). In addition, lncRNA dysregulation
underlies certain human diseases caused by chromosome deletion and
translocation (36). LncRNAs are
also involved in the development, plasticity, disease and evolution
of the mammalian nervous system (37). LncRNAs can promote the
differentiation and activation of dendritic cells, B lymphocytes
and T lymphocytes (38).
Accordingly, a number of specific lncRNAs have been identified in
Th1 and Th2 cells (39-42) and in the nasal mucosa of mice with
AR (3). The results of the
present study confirmed the differential expression of lncRNAs and
mRNAs in the nasal mucosa of AR mice treated with NaB. A degree is
the simplest and most important measure of gene centrality within a
network that determines the relative importance of that gene
(43). LncRNA (NONMMUT057309),
which is 306 nt long and located on chromosome 6, is mainly
expressed in the hippo-campus, liver, and lung (44); however, to the best of our
knowledge, no published studies on the mechanism associated with
its function are currently available.
NaB, a pan-HDAC inhibitor, not only decreased the
expression of HDAC1 and HDAC8, but also downregulated the
expression of lncRNA (NONMMUT057309) and altered the expression of
immunoglobulins in the present study. Previous studies have
demonstrated that HDAC and lnc-H19 could be bidirectionally
regulated (45), and the pan-HDAC
inhibitors panobinostat and SAHA upregulated lnc-GAS5 expression in
non-small cell lung cancer (46).
Thus, it may be speculated that NaB could influence the nasal
mucosa allergic response through lncRNA (NONMMUT057309) expression.
LncRNA (NONMMUT057309) may act on its target genes to regulate the
expression of immunoglobulin in the nasal mucosa to prevent AR.
Three target genes (Oct-1, Evi-1 and Pax-4) were
predicted for lncRNA (NONMMUT057309). Oct-1 can co-regulate Th2
cytokine gene expression through Rhs-related transmembrane protein
(47) and regulate the expression
of IL-17 (48). Evi-1
participates in the pathogenesis of colorectal cancer through TGF-β
signaling (49). The duodenum of
functional dyspepsia rats displayed increased expressions of PAX4
(50).
Among the top 10 significantly enriched GO terms in
C vs. AR groups, 'extracellular matrix organization' has been
determined to exert effects on airway epithelial cells and
fibroblast structure (51). The
regulation of the immune system in early life by the microbiota may
be associated with allergy development (52). The pathology of bronchial asthma
demonstrates a multicellular process (53). AR rats exhibit microvascular
remodeling of the nasal mucosa (54). In the top 10 significantly
enriched GO terms in NaB + AR vs. AR groups, salmon cartilage
proteoglycan attenuates allergic responses in mice (55). Inhibiting platelet activating
factor can treat AR (56). Among
top 10 significantly enriched GO terms in NaB+AR vs. C groups,
immunoglobulin E (lgε) receptor on lymphocyte γ chain can mediate
the receptor activator for NF-κB ligand, which is the primary
cytokine required for osteoclastogenesis (57). ROS likely originates from
inflammatory cells (eosinophils, neutrophils and macrophages), and
their deleterious activity can result in oxidative DNA damage
(58). Maternal exposure to any
type of stressor is associated with an increased risk of an atopic
offspring (59). There are
important connections between hemopoiesis and allergy/asthma
(60). Immunotherapy decreases
antigen-induced eosinophil cell migration into the nasal cavity
(61). In patients with asthma,
serum endotoxin concentrations significantly correlate with sputum
chemokine motif ligand 2 concentrations (62).
The present study also determined the top 10 PANTHER
pathways represented by the differentially expressed genes. 'T-cell
activation', 'B cell activation', 'Interleukin signaling pathway',
'Inflammation mediated by chemokine and cytokine signaling pathway'
and 'Histamine H2 receptor mediated signaling pathway' participate
in allergic inflammation (4,63-64). 'Apoptosis signaling pathway'
(65) and 'Toll receptor
signaling pathway' (66) are also
involved in the pathology of AR. The expression of endotherin 2 is
increased in cigarette-exposed asthmatic mice (67). Heme oxygenase-1 protects airway
epithelium against apoptosis by targeting the proinflammatory
NLRP3-RXR axis in asthma (68).
Fibroblast-specific integrin-α V differentially regulates type 17
and type 2 driven inflammation and fibrosis (69). The p38 MAP-kinase pathway is
involved in the production of chloride voltage-gated channel 3 in
nasal epithelial AR cells induced by IL-4 (70). The Wnt signaling pathway has also
been demonstrated to be differentially regulated in patients with
AR (71). TGF-β/Smad signaling is
involved in allergic diseases (72-74). At present, to the best of our
knowledge, no reports are available on the gonadotropin-releasing
hormone receptor, succinate to proportionate conversion or
angiotensin H-stimulated signaling through G proteins and
β-arrestin involvement in allergic inflammation pathogenesis, which
is worth further study.
Together, previous findings along with the results
of the present study may provide new options for the treatment of
AR. However, in the present study, the gene sample was small, and
further in vitro experiments are needed to further verify
the role of lncRNA (NONMMUT057309), as well as the target genes
(Oct-1, Evi-1, Pax-4) and signaling pathways, in the prevention of
AR in the nasal mucosa of NaB-treated mice.
Supplementary Data
Funding
This study was supported by the National Natural
Science Foundation of China (grant nos. 81670925 and 81271069),
Shaanxi Health Research Fund (grant no. 2018D006), Xi'an Health and
Family Planning Commission Fund (grant no. J201902034) and Shaanxi
Natural Science Foundation (grant no. 2019JQ-434).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JW produced the animal model and was a major
contributor in writing the manuscript. CM analyzed the gene data.
SF performed the histological examination and western blotting. FC
and JQ helped with the design, implementation, and revision of
important contents of the experiments. The corresponding authors
contributed equally to this work. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
All animal experiments were conducted in accordance
with the National Institutes of Health guidelines and approved by
the Committee on Animal Research of the Air Force Military Medical
University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Acknowledgments
Not applicable.
References
|
1
|
Seidman MD, Gurgel RK, Lin SY, Schwartz
SR, Baroody FM, Bonner JR, Dawson DE, Dykewicz MS, Hackell JM, Han
JK, et al: Clinical practice guideline: Allergic rhinitis executive
summary. Otolarygol Head Neck Surg. 152:197–206. 2015. View Article : Google Scholar
|
|
2
|
Zhang L, Han D, Huang D, Wu Y, Dong Z, Xu
G, Kong W and Bachert C: Prevalence of self-reported allergic
rhinitis in eleven major cities in china. Int Arch Allergy Immunol.
149:47–57. 2009. View Article : Google Scholar
|
|
3
|
Wang XD, Zheng M, Lou HF, Wang CS, Zhang
Y, Bo MY, Ge SQ, Zhang N, Zhang L and Bachert C: An increased
prevalence of self-reported allergic rhinitis in major Chinese
cities from 2005 to 2011. Allergy. 71:1170–1180. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cheng L, Chen J, Fu Q, He S, Li H, Liu Z,
Tan G, Tao Z, Wang D, Wen W, et al: Chinese Society of Allergy
guidelines for diagnosis and treatment of allergic rhinitis.
Allergy Asthma Immunol Res. 10:300–353. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eifan AO and Durham SR: Pathogenesis of
rhinitis. Clin Exp Allergy. 46:1139–1151. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Milner JD: IL-17 producing cells in host
defense and atopy. Curr Opin Immunol. 23:784–788. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Steelant B, Wawrzyniak P, Martens K,
Jonckheere AC, Pugin B, Schrijvers R, Bullens DM, Vanoirbeek JA,
Krawczyk K, Dreher A, et al: Blocking histone deacetylase activity
as a novel target for epithelial barrier defects in patients with
allergic rhinitis. J Allergy Clin Immunol. 144:1242.e7–1253.e7.
2019. View Article : Google Scholar
|
|
8
|
Liu J, Livingston MJ, Dong G, Tang C, Su
Y, Wu G, Yin XM and Dong Z: Histone deacetylase inhibitors protect
against cisplatin-induced acute kidney injury by activating
autophagy in proximal tubular cells. Cell Death Dis. 9:3222018.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Escobar J, Pereda J, Arduini A, Sandoval
J, Sabater L, Aparisi L, Vento M, López-Rodas G and Sastre J: Role
of redox signaling, protein phosphatases and histone acetylation in
the inflammatory cascade in acute pancreatitis. Therapeutic
implications Inflamm Allergy Drug Targets. 9:97–108. 2010.
View Article : Google Scholar
|
|
10
|
Yang G, Cheng BH, Yang SB, Liu ZQ, Qiu SQ,
Yang LT, Xie RD, Geng XR, Li MG, Gao L, et al: Targeting
histone-acetyltransferase Tat-interactive protein 60 inhibits
intestinal allergy. Allergy. 73:387–394. 2018. View Article : Google Scholar
|
|
11
|
Su XM, Ren Y, Li ML, Zhao X, Kong LF and
Kang J: Performance evaluation of histone deacetylases in lungs of
mice exposed to ovalbumin aerosols. J Physiol Pharmacol.
69:2018.
|
|
12
|
Shao JB, Luo XQ, Wu YJ, Li MG, Hong JY, Mo
LH, Liu ZG, Li HB, Liu DB and Yang PC: Histone deacetylase 11
inhibits interleukin 10 in B cells of subjects with allergic
rhinitis. Int Forum Allergy Rhinol. 8:1274–1283. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jiang J, Liu JQ, Li J, Li M, Chen HB, Yan
H, Mo LH, Qiu SQ, Liu ZG and Yang PC: Trek1 contributes to
maintaining nasal epithelial barrier integrity. Sci Rep.
5:91912015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang C, Li H, Cao L and Wang G:
Identification of differentially expressed genes associated with
asthma in children based on the bioanalysis of the regulatory
network. Mol Med Rep. 18:2153–2163. 2018.PubMed/NCBI
|
|
15
|
Wang J, Wang Y, Chen X, Zhang PZ, Shi ZT,
Wen LT, Qiu JH and Chen FQ: Histone deacetylase inhibitor sodium
butyrate attenuates gentamicin-induced hearing loss in vivo. Am J
Otolaryngol. 36:242–248. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang J, Wen L, Wang Y and Chen F:
Therapeutic effect of histone deacetylase inhibitor, sodium
butyrate, on allergic rhinitis in vivo. DNA Cell Biol. 35:203–208.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cerf-Bensussan N and Gaboriau-Routhiau V:
The immune system and the gut microbiota: Friends or foes? Nat Rev
Immunol. 10:735–744. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Song H, Yoo Y, Hwang J, Na YC and Kim HS:
Faecalibacterium prausnitzii subspecies-level dysbiosis in the
human gut micro-biome underlying atopic dermatitis. J Allergy Clin
Immunol. 137:852–860. 2016. View Article : Google Scholar
|
|
19
|
Val-Laillet D, Guérin S, Coquery N, Nogret
I, Formal M, Romé V, Le Normand L, Meurice P, Randuineau G,
Guilloteau P, et al: Oral sodium butyrate impacts brain metabolism
and hippocampal neurogenesis, with limited effects on gut anatomy
and function in pigs. FASEB J. 32:2160–2171. 2018. View Article : Google Scholar
|
|
20
|
Lee C, Kim BG, Kim JH, Chun J, Im JP and
Kim JS: Sodium butyrate inhibits the NF-kappa B signaling pathway
and histone deacetylation, and attenuates experimental colitis in
an IL-10 independent manner. Int Immunopharmacol. 51:47–56. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang W, Zhu Z, Zhu B and Ma Z: Peroxisome
proliferator-activated receptor-gamma agonist induces regulatory T
cells in a murine model of allergic rhinitis. Otolaryngol Head Neck
Surg. 144:506–513. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li L, Wang L, Li H, Han X, Chen S, Yang B,
Hu Z, Zhu H, Cai C, Chen J, et al: Characterization of LncRNA
expression profile and identification of novel LncRNA biomarkers to
diagnose coronary artery disease. Atherosclerosis. 275:359–367.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bian X, Liang Z, Feng A, Salgado E and
Shim H: HDAC inhibitor suppresses proliferation and invasion of
breast cancer cells through regulation of miR-200c targeting CRKL.
Biochem Pharmacol. 147:30–37. 2018. View Article : Google Scholar
|
|
24
|
Licciardi PV, Ververis K, Tang ML, El-Osta
A and Karagiannis TC: Immunomodulatory effects of histone
deacetylase inhibitors. Curr Mol Med. 13:640–647. 2013. View Article : Google Scholar
|
|
25
|
Yang DH, Xie J, Liu K, Peng Z, Guo JY, Yu
SK, Wang GP and Gong SS: The histone deacetylase inhibitor sodium
butyrate protects against noise-induced hearing loss in Guinea
pigs. Neurosci Lett. 660:140–146. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Toki S, Goleniewska K, Reiss S, Zhou W,
Newcomb DC, Bloodworth MH, Stier MT, Boyd KL, Polosukhin VV,
Subramaniam S and Peebles RS Jr: The histone deacetylase inhibitor
trichostatin A suppresses murine innate allergic inflammation by
blocking group 2 innate lymphoid cell (ILC2) activation. Thorax.
71:633–645. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wawrzyniak P, Wawrzyniak M, Wanke K,
Sokolowska M, Bendelja K, Rückert B, Globinska A, Jakiela B, Kast
JI, Idzko M, et al: Regulation of bronchial epithelial barrier
integrity by type 2 cytokines and histone deacetylases in asthmatic
patients. J Allergy Clin Immunol. 139:93–103. 2017. View Article : Google Scholar
|
|
28
|
Comer BS, Ba M, Singer CA and Gerthoffer
WT: Epigenetic targets for novel therapies of lung diseases.
Pharmacol Ther. 147:91–110. 2015. View Article : Google Scholar
|
|
29
|
Wouters BJ and Delwel R: Epigenetics and
approaches to targeted epigenetic therapy in acute myeloid
leukemia. Blood. 127:42–52. 2016. View Article : Google Scholar
|
|
30
|
Marks PA and Breslow R: Dimethyl sulfoxide
to vorinostat: Development of this histone deacetylase inhibitor as
an anticancer drug. Nat Biotechnol. 25:84–90. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Thaler R, Spitzer S, Karlic H, Klaushofer
K and Varga F: DMSO is a strong inducer of DNA hydroxymethylation
in preosteo-blastic MC3T3-E1 cells. Epigenetics. 7:635–651. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang CC, Wu H, Lin FH, Gong R, Xie F, Peng
Y, Feng J and Hu CH: Sodium butyrate enhances intestinal integrity,
inhibits mast cell activation, inflammatory mediator production and
JNK signaling pathway in weaned pigs. Innate Immun. 24:40–46. 2018.
View Article : Google Scholar
|
|
33
|
Wang J, Yang M, Xu S, Lin Y, Che L, Fang Z
and Wu D: Comparative effects of sodium butyrate and flavors on
feed intake of lactating sows and growth performance of piglets.
Anim Sci J. 85:683–689. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ren Y, Su X, Kong L, Li M, Zhao X, Yu N
and Kang J: Therapeutic effects of histone deacetylase inhibitors
in a murine asthma model. Inflamm Res. 65:995–1008. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Cech TR and Steitz JA: The noncoding RNA
revolution-trashing old rules to forge new ones. Cell. 157:77–94.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Batista PJ and Chang HY: Long noncoding
RNAs: Cellular address codes in development and disease. Cell.
152:1298–1307. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Briggs JA, Wolvetang EJ, Mattick JS, Rinn
JL and Barry G: Mechanisms of long non-coding RNAs in mammalian
nervous system development, plasticity, disease, and evolution.
Neuron. 88:861–877. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Aune TM and Spurlock CF III: Long
non-coding RNAs in innate and adaptive immunity. Virus Res.
212:146–160. 2016. View Article : Google Scholar :
|
|
39
|
Collier SP, Collins PL, Williams CL,
Boothby MR and Aune TM: Cutting edge: Influence of Tmevpg1, a long
intergenic noncoding RNA, on the expression of Ifng by Th1 cells. J
Immunol. 189:2084–2088. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Gomez JA, Wapinski OL, Yang YW, Bureau JF,
Gopinath S, Monack DM, Chang HY, Brahic M and Kirkegaard K: The
NeST long ncRNA controls microbial susceptibility and epigenetic
activation of the interferon-γ locus. Cell. 152:743–754. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Spurlock CF III, Tossberg JT, Guo Y,
Collier SP, Crooke PS III and Aune TM: Expression and functions of
long noncoding RNAs during human T helper cell differentiation. Nat
Commun. 6:69322015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhang H, Nestor CE, Zhao S, Lentini A,
Bohle B, Benson M and Wang H: Profiling of human CD4+ T-cell
subsets identifies the TH2-specific noncoding RNA GATA3-AS1. J
Allergy Clin Immunol. 132:1005–1008. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hohmann S: UNICELLSYS-Understanding the
cell's functional organization. J Biotechnol. 150:S5452010.
View Article : Google Scholar
|
|
44
|
Bu D, Luo H, Jiao F, Fang S, Tan C, Liu Z
and Zhao Y: Evolutionary annotation of conserved long non-coding
RNAs in major mammalian species. Sci China Life Sci. 58:787–798.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Huang Y, Zhang Y, Jin C, Li X, Jia L and
Li W: Long non-coding RNA H19 inhibits adipocyte differentiation of
bone marrow mesenchymal stem cells through epigenetic modulation of
histone deacetylases. Sci Rep. 6:288972016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Keenan CR, Schuliga MJ and Stewart AG:
Pro-inflammatory mediators increase levels of the noncoding RNA
GAS5 in airway smooth muscle and epithelial cells. Can J Physiol
Pharmacol. 93:203–207. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kim K, Kim N and Lee GR: Transcription
factors Oct-1 and GATA-3 cooperatively regulate Th2 cytokine gene
expression via the RHS5 within the Th2 locus control region. PLoS
One. 11:e01485762016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kim LK, Esplugues E, Zorca CE, Parisi F,
Kluger Y, Kim TH, Galjart NJ and Flavell RA: Oct-1 regulates IL-17
expression by directing interchromosomal associations in
conjunction with CTCF in T cells. Mol Cell. 54:56–66. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Deng X, Cao Y, Liu Y, Li F, Sambandam K,
Rajaraman S, Perkins AS, Fields AP, Hellmich MR, Townsend CM Jr, et
al: Overexpression of Evi-1 oncoprotein represses TGF-β signaling
in colorectal cancer. Mol Carcinog. 52:255–264. 2013. View Article : Google Scholar
|
|
50
|
Zhao J, Zhao L, Zhang S and Zhu C:
Modified Liu-Jun-Zi decoction alleviates visceral hypersensitivity
in functional dyspepsia by regulating EC cell-5HT3r signaling in
duodenum. J Ethnopharmacol. 250:1124682020. View Article : Google Scholar
|
|
51
|
Royce SG, Tan L, Koek AA and Tang ML:
Effect of extracellular matrix composition on airway epithelial
cell and fibroblast structure: Implications for airway remodeling
in asthma. Ann Allergy Asthma Immunol. 102:238–246. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Gensollen T and Blumberg RS: Correlation
between early-life regulation of the immune system by microbiota
and allergy development. J Allergy Clin Immunol. 139:1084–1091.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Sharma N, Akkoyunlu M and Rabin RL:
Macrophages-common culprit in obesity and asthma. Allergy.
73:1196–1205. 2018. View Article : Google Scholar
|
|
54
|
Liu JG, Wang MQ, Zhu XH, Liu YH and Cai
JY: Microvascular remodeling of nasal mucosa in allergic rhinitis
induced by an allergen in Sprague-Dawley rats. Genet Mol Res.
14:11624–11630. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ono HK, Yoshimura S, Hirose S, Narita K,
Tsuboi M, Asano K and Nakane A: Salmon cartilage proteoglycan
attenuates allergic responses in mouse model of papain-induced
respiratory inflammation. Mol Med Rep. 18:4058–4064.
2018.PubMed/NCBI
|
|
56
|
Muñoz-Cano RM, Casas-Saucedo R, Valero
Santiago A, Bobolea I, Ribó P and Mullol J: Platelet-activating
factor (PAF) in allergic rhinitis: Clinical and therapeutic
implications. J Clin Med. 8:2019. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Humphrey MB and Nakamura MC: A
comprehensive review of immunoreceptor regulation of osteoclasts.
Clin Rev Allergy Immunol. 51:48–58. 2016. View Article : Google Scholar :
|
|
58
|
de Groot LES, Sabogal Piñeros YS, Bal SM,
van de Pol MA, Hamann J, Sterk PJ, Kulik W and Lutter R: Do
eosinophils contribute to oxidative stress in mild asthma? Clin Exp
Allergy. 49:929–931. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Flanigan C, Sheikh A, DunnGalvin A, Brew
BK, Almqvist C and Nwaru BI: Prenatal maternal psychosocial stress
and offspring's asthma and allergic disease: A systematic review
and meta-analysis. Clin Exp Allergy. 48:403–414. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Elsas P: Hemopoiesis and allergy, an
introduction to the special issue. Curr Drug Targets Inflamm
Allergy. 2:267–270. 2003. View Article : Google Scholar
|
|
61
|
Furin MJ, Norman PS, Creticos PS, Proud D,
Kagey-Sobotka A, Lichtenstein LM and Naclerio RM: Immunotherapy
decreases antigen-induced eosinophil cell migration into the nasal
cavity. J Allergy Clin Immunol. 88:27–32. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
McSharry C, Spears M, Chaudhuri R, Cameron
EJ, Husi H and Thomson NC: Increased sputum endotoxin levels are
associated with an impaired lung function response to oral steroids
in asthmatic patients. J Allergy Clin Immunol. 134:1068–1075. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Bui TT, Piao CH, Hyeon E, Fan Y, Choi DW,
Jung SY, Jang BH, Shin HS, Song CH and Chai OH: Preventive effect
of Bupleurum chinense on nasal inflammation via suppressing T
helper type 2, Eosinophil and mast cell activation. Am J Chin Med.
47:405–421. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Chen Q, Ba YP, Zhou MH, Li SD and Zhang
PW: CD23 on B cells determines Breg-facilitated IL-10 secretion as
well as activation of T cells. Lin Chung Er Bi Yan Hou Tou Jing Wai
Ke Za Zhi. 32:931–937. 2018.In Chinese. PubMed/NCBI
|
|
65
|
Ciebiada M, Kasztalska K, Gorska-Ciebiada
M and Górski P: Histamine type 2 receptor expression on peripheral
blood regulatory lymphocytes in patients with allergic rhinitis
treated with specific immunotherapy. Am J Rhinol Allergy.
28:e130-e1352014. View Article : Google Scholar
|
|
66
|
Wang Z and Tan F: The blockade of
PD-1/PD-L1 pathway promotes the apoptosis of CD19+
CD25+ Bregs and suppresses the secretion of IL-10 in
patients with allergic rhinitis. Scand J Immunol.
91:e128362020.
|
|
67
|
Golshiri-Isfahani A, Amizadeh M and
Arababadi MK: The roles of toll like receptor 3, 7 and 8 in
allergic rhinitis pathogenesis. Allergol Immunopathol (Madr).
46:503–507. 2018. View Article : Google Scholar
|
|
68
|
Han F, Zhu S, Chen B and Li J: Elevated
expression of endothelin 2 in lung tissues of asthmatic rats after
exposed to cigarette smoke and its mechanism. Xi Bao Yu Fen Zi Mian
Yi Xue Za Zhi. 33:1030–1034. 2017.In Chinese. PubMed/NCBI
|
|
69
|
Lv J, Su W, Yu Q, Zhang M, Di C, Lin X, Wu
M and Xia Z: Heme oxygenase-1 protects airway epithelium against
apoptosis by targeting the proinflammatory NLRP3-RXR axis in
asthma. J Biol Chem. 293:18454–18465. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Sciurba JC, Gieseck RL, Jiwrajka N, White
SD, Karmele EP, Redes J, Vannella KM, Henderson NC, Wynn TA and
Hart KM: Fibroblast-specific integrin-alpha V differentially
regulates type 17 and type 2 driven inflammation and fibrosis. J
Pathol. 248:16–29. 2019. View Article : Google Scholar
|
|
71
|
Han D, Zhou B, Cheng L, Oh Y and Li H: P38
MAP-kinase pathway is involved in the production of CLC-3 in nasal
epithelial cells with allergic rhinitis induced by interleukin-4.
Laryngoscope. 116:1973–1977. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Tirado-Rodriguez B, Ortega E,
Segura-Medina P and Huerta-Yepez S: TGF-β: An important mediator of
allergic disease and a molecule with dual activity in cancer
development. J Immunol Res. 2014:3184812014. View Article : Google Scholar
|
|
73
|
Gregory LG, Mathie SA, Walker SA, Pegorier
S, Jones CP and Lloyd CM: Overexpression of Smad2 drives house dust
mite-mediated airway remodeling and airway hyperresponsiveness via
activin and IL-25. Am J Respir Crit Care Med. 182:143–154. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Luo X, Ding Q, Wang M, Li Z, Mao K, Sun B,
Pan Y, Wang Z, Zang YQ and Chen Y: In vivo disruption of TGF-beta
signaling by Smad7 in airway epithelium alleviates allergic asthma
but aggravates lung carcinogenesis in mouse. PLoS One.
5:e101492010. View Article : Google Scholar : PubMed/NCBI
|