Introduction
Acute respiratory distress syndrome (ARDS) is one of
the major critical diseases encountered in intensive care units
(1). The main symptom of ARDS is
refractory hypoxemia. Low tidal volume ventilation is routinely
applied in clinical practice to correct hypoxemia, which aims to
reduce the risk of ventilator-induced lung injury (2). However, this ventilation strategy
inevitably leads to hypercapnia, which is referred to as
'permissive' hypercapnia (3).
Permissive hypercapnia may contribute to an improved outcome in
terms of pulmonary function (4,5),
but its effects on cerebral function, such as cognitive function,
have not been extensively investigated. Indeed, our previous study
demonstrated that permissive hypercapnia aggravated cognitive
impairment in hypoxemic rats (6);
however, the underlying mechanism remains unclear.
It has been reported that there is a close
association between disruption of the blood-brain barrier (BBB) and
cognitive impairment (7-10). BBB disruption, particularly in the
region of the hippocampus, may lead to cognitive dysfunction
(11,12). A recent study demonstrated that
BBB breakdown played a predictive role in human cognitive
disorders, particularly at the early stages (13). Moreover, Wang et al
reported that hyper-permeability of the BBB resulted in cognitive
impairment in a rat model of splenectomy (14). However, it remains unknown whether
hypercapnia exerts any effects on BBB disruption in hypoxemic
rats.
Tight junctions between cerebrovascular endothelial
cells play a key role in maintaining the integrity of the BBB.
Tight junctional proteins, including zonula occludens (ZO)-1,
occludin and claudin-5, are involved in the determination of BBB
permeability (15-17). Additionally, previous studies
suggested that peripheral inflammation is crucial in the process of
BBB disruption (18,19). Interleukin (IL)-1β, one of the
major pro‑inflammatory factors, may also be involved in the
disruption of the BBB. Wang et al revealed that IL-1β
induced BBB breakdown through suppressing sonic hedgehog expression
in astrocytes. They also observed that IL-1β promoted the
expression of other inflammatory factors, thereby augmenting
inflammation and aggravating BBB disruption (20). It remains to be determined whether
hypercapnia would further increase BBB permeability through
upregulating IL-1β expression in the blood of hypoxemic rats.
The aim of the present study was to determine
whether hypercapnia can exacerbate BBB disruption through inducing
IL-1β overproduction in the blood of hypoxemic adult rats, and
whether this effect is mediated by triggering the expression of
IL-1 receptor 1 (IL-1R1) in cerebrovascular endothelial cells,
decreasing the expression of tight junctional proteins, and
ultimately increasing BBB permeability.
Materials and methods
Animals and treatment
Male adult Sprague-Dawley rats (n=144), aged ~3
months and weighing 220-250 g, were included in present study. All
efforts were made to mini-mize the number of animals used in the
experiments. The rats were fed standard chow and water, and were
housed under standard experimental conditions (temperature,
20-25°C; humidity, 50-70%) under a 12-h light/dark cycle. All rats
were fasted with access to water overnight prior to the
experiments. The rat model of hypercapnia/hypoxemia was established
as described in our previous study (6). To minimize suffering and distress,
the rats were anesthetized with 2% pentobarbital sodium (30 mg/kg
by intraperitoneal injection) followed by mechanical ventilation.
The tidal volume (9 ml/kg body weight), respiratory rate (45
breaths/min), and inspiratory:expiratory ratio (1:1) were fixed.
The rats were randomly divided into four groups according to
different concentrations of O2 and CO2 as
follows: Sham group (exposed to air), hypercapnia group (exposed to
5% CO2), hypoxemia group (exposed to 16% O2),
and hypercapnia + hypoxemia group (HH group; exposed to 16%
O2 mixed with 5% CO2). These concentrations
(16% O2 and 5% CO2) were used to maintain the
PO2 of arterial blood at ~60 mmHg and the pH at
7.20-7.25. The right femoral artery was cannulated to collect
arterial blood samples. The PO2, PCO2 and pH
of the arterial blood samples were immediately measured by a Blood
Gas/Electrolyte Analyzer (Model 5700; Werfen Corporation).
The rats that were used for western blotting and
immu-nofluorescence staining were not subjected to invasive
manipulation apart from ventilation. All animals were ventilated
for 3 h, after which time they were euthanized by intraperitoneal
injection of pentobarbital sodium (150 mg/kg).
Assessment of BBB permeability
At 3 h after ventilation, 2% Evans blue (EB)
solution (4 ml/kg) was injected through the caudal vein. After 1 h,
the rats were perfused transcardially with normal saline to remove
the intravascular dye, and 4% paraformaldehyde was used to perfuse
the brain. The brains were harvested and incubated in formamide (1
ml/100 mg) at 60°C for 24 h. The supernatant was separated after
centrifugation at 12,000 x g at 4°C for 20 min. The optical density
(OD) values were measured at 620 nm using a spectrophotometer
(Multiskan FC IVD; Thermo Fisher Scientific, Inc.).
Human whole‑blood cultures and ethics
statement
Whole blood was donated by 4 healthy male volunteers
(mean age ± standard deviation, 35±9.4 years). None of the
volunteers had a history of cancer, hematological disorders,
infections, autoimmune diseases, transplantation, or use of
immunosuppressive drugs. The whole blood was cultured as reported
previously (21). Briefly, 2 ml
of whole blood were collected from each volunteer. Subsequently,
the whole-blood samples were mixed with 18 ml RPMI-1640 medium
(Invitrogen; Thermo Fisher Scientific, Inc., cat. no. 8118329),
which was supplemented with 10% human serum (Gemini Bio-Products;
cat. no. H91S001) and 1% penicillin-streptomycin solution (Aladdin
Biochemical Technology Co., Ltd.; cat. no. P113150). The blood
samples were randomly divided into four groups as follows: Control,
high concentration of CO2 (HC), hypoxia, and hypoxia + +
HC groups. The control group was exposed to 5% CO2 + 20%
O2. The HC group was exposed to 10% CO2 + 20%
O2. The hypoxia group was exposed to 5% CO2 +
0.2% O2. The hypoxia + HC group was exposed to 10%
CO2 + 0.2% O2. These concentrations (0.2%
O2 and 10% CO2) were used to maintain the
PO2 of the medium at ~60 mmHg and the pH at 7.20-7.25.
The PO2, PCO2 and pH of the medium were
measured by a Blood Gas/Electrolyte Analyzer (Model 5700; Werfen
Corporation).
IL‑1β evaluation by ELISA in vitro and in
vivo
The levels of IL-1β were evaluated using ELISA kits
(applied to human blood cultures, cat. no. ab100562; applied to rat
blood, cat. no. ab100768; Abcam) following the manufacturers'
instructions. Briefly, the samples and standards were added to the
plate wells coated by IL-1β antibodies labeled with horseradish
peroxidase (HRP). Subsequently, a TMB substrate solution was
pipetted to the wells. Then, stop buffer was added, and the OD was
measured spectrophotometrically at a wavelength of 450 nm. The
concentration of IL-1β in the samples was determined by comparing
the OD of the samples to the standard curve.
Primary cultures of rat brain capillary
endothelial cells (RBECs)
Primary cultures of RBECs were prepared as
previously described (22–24).
Briefly, the gray matter was isolated from the brain of 3-week-old
Sprague-Dawley rats. The gray matter was minced into tiny
particles, digested with DMEM containing collagenase type 2 (1
mg/ml), gentamycin (50 μg/ml), and 300 μl DNase (15
μg/ml) at 37°C for 1.5 h, then neutralized with bovine serum
albumin (Calbiochem-Novabiochem Corp.), and finally centrifuged at
1,000 x g at 4°C for 20 min. The cells were further digested in
DMEM containing collagenase-dispase (1 mg/ml) and DNase (6.7
μg/ml) for 1 h at 37°C. Microvessel endothelial cell
clusters were separated on a 33% continuous Percoll gradient, then
collected and washed twice with DMEM before plating into collagen
type IV‑ and fibronectin‑coated dishes. RBECs were cultured in
DMEM/F12 supplemented with 10% plasma-derived serum, heparin (100
μg/ml), basic fibroblast growth factor (1.5 ng/ml),
transferrin (5 μg/ml), insulin (5 μg/ml), sodium
selenite (5 ng/ml), puromycin (4 μg/ml) and gentamycin (50
μg/ml) (RBEC medium I) at 37°C in a humidified incubator
with 5% CO2/95% air for 2 days. On the following day,
RBECs were cultured in RBEC medium II (RBEC medium I without
puromycin). The medium was changed every other day from the 4th day
onwards. The RBECs were randomly divided into four groups as
follows: Control, IL-1β, IL-1β + IL-1 receptor antagonist (IL-1Ra),
and IL-1Ra groups. The control group was treated with 0.01 M PBS.
The IL-1β group was treated with IL-1β (40 ng/ml; MedChemExpress;
cat. no. HY-P7028). The IL-1β + IL-1Ra group was treated with IL-1β
(40 ng/ml) and IL-1Ra (40 ng/ml; MedChemExpress; cat. no.
HY-P7029). The IL-1Ra group was treated with IL-1Ra (40 ng/ml)
(25).
Western blotting
Total proteins from the hippocampal tissue samples
and RBECs (n=4 for each group) were extracted using a Total Protein
Extraction kit (BestBio; cat. no. BB-3101-100T). Equal amounts (40
μg) of proteins from each sample were separated in a 10%
SDS-PAGE gel and transferred to PVDF membranes (EMD Millipore),
which were then blocked with 5% non-fat milk for 1 h at room
temperature. Subsequently, the membranes were incubated overnight
at 4°C with primary antibodies against the following target
proteins: IL-1R1 (1:1,000, Abcam; cat. no. ab106278), ZO-1
(1:1,000; Invitrogen; Thermo Fisher Scientific, Inc.; cat. no.
SL258826), occludin (1:1,000; Abcam; cat. no. Ab216327), claudin-5
(1:1,000; Abbkine Scientific Co., Ltd.; cat. no. Abp50990),
t‑IRAK‑1 (1:1,000; Abcam; cat. no. ab238) and p-IRAK-1 (1:1,000;
Abcam; cat. no. ab218130). On the following day, HRP-labeled goat
anti-rabbit antibody (1:3,000; Cell Signaling Technology, Inc.;
cat. no. 7074S) was added and the membranes were incubated for 2 h
at 4°C. The immunoblots were visualized using a chemiluminescence
kit (Bioworld Technology, Inc.; cat. no. AC36131), and detected by
an imaging densitometer (ImageQuant LAS 500, GE Healthcare
Bio-Sciences AB). The gray value was quantified using FluorChem
8900 software (version 4.0.1, Alpha Innotech Corporation). β-actin
was used as the control. The relative density was calculated
through dividing the gray value of β-actin by that of the target
protein. Both the target protein and β-actin were from the same
lane of the same membrane.
Double immunofluorescence labeling
In vivo, the rats were anesthetized with 2%
pentobarbital sodium (30 mg/kg by intraperitoneal injection) and
transcardially perfused with saline and 4% paraformaldehyde at 3 h
after ventilation. The brains were harvested and post‑fixed
overnight at 4°C in 4% paraformaldehyde. Subsequently, the tissue
samples were dehydrated in graded sucrose and cut into 10-μm
sections. The sections were blocked in 5% normal donkey serum
(Abbkine Co., Ltd. cat. no. BMS0140) for 0.5 h at room temperature.
In vitro, the coverslips with adherent RBECs were fixed with
4% paraformaldehyde for 20 min at room temperature at 24 h after
treatment. The coverslips were blocked in 5% normal donkey serum
for 0.5 h at room temperature sequentially.
Subsequently, the sections/coverslips were incubated
overnight at 4°C with the following primary antibodies: IL‑1R1
(1:100, Abcam; cat. no. ab106278), ZO-1 (1:100; Invitrogen; Thermo
Fisher Scientific Inc.; cat. no. SL258826), occludin (1:100; Abcam;
cat. no. Ab216327), claudin-5 (1:100; Abbkine Scientific Co., Ltd.;
cat. no. Abp50990), and CD31 (1:100; Abcam; cat. no. Ab24590). The
sections/coverslips were washed on the following day, the secondary
antibodies Alexa Fluor® 549 goat anti-rabbit IgG (H + L)
(1:100; Invitrogen; Thermo Fisher Scientific Inc.; cat. no.
ATRJN1301) and Alexa Fluor® 488 goat anti-mouse IgG
(1:100; Invitrogen; Thermo Fisher Scientific Inc.; cat. no.
ATRMR2301) were added, and the sections/coverslips were incubated
for 1 h at room temperature. Finally, the sections/coverslips were
mounted using fluorescent mounting medium with DAPI (Sigma-Aldrich;
Merck KGaA; cat. no. SLBW4468) and examined using a fluorescence
microscope (DP73, Olympus Corporation). At a magnification of x400.
Four fields of view per section/coverslip were examined in each
group.
Statistical analysis
The statistical analysis was performed using SPSS
v.19.0 (IBM Corp.). All values are expressed as mean ± standard
deviation. Student's t-test was used to analyze the data of
two-group univariate-factor measurements. One-way analysis of
variance (ANOVA) was used to analyze the data of 3 or more group
univariate-factor measurements followed by Tukey's post hoc test.
Repeated measures ANOVA was used to analyze the repeated
measurement data. Factorial ANOVA was used for the interaction
effects. When an interaction was examined, simple effects analyses
were evaluated. P<0.05 was considered to indicate statistically
significant differences.
Results
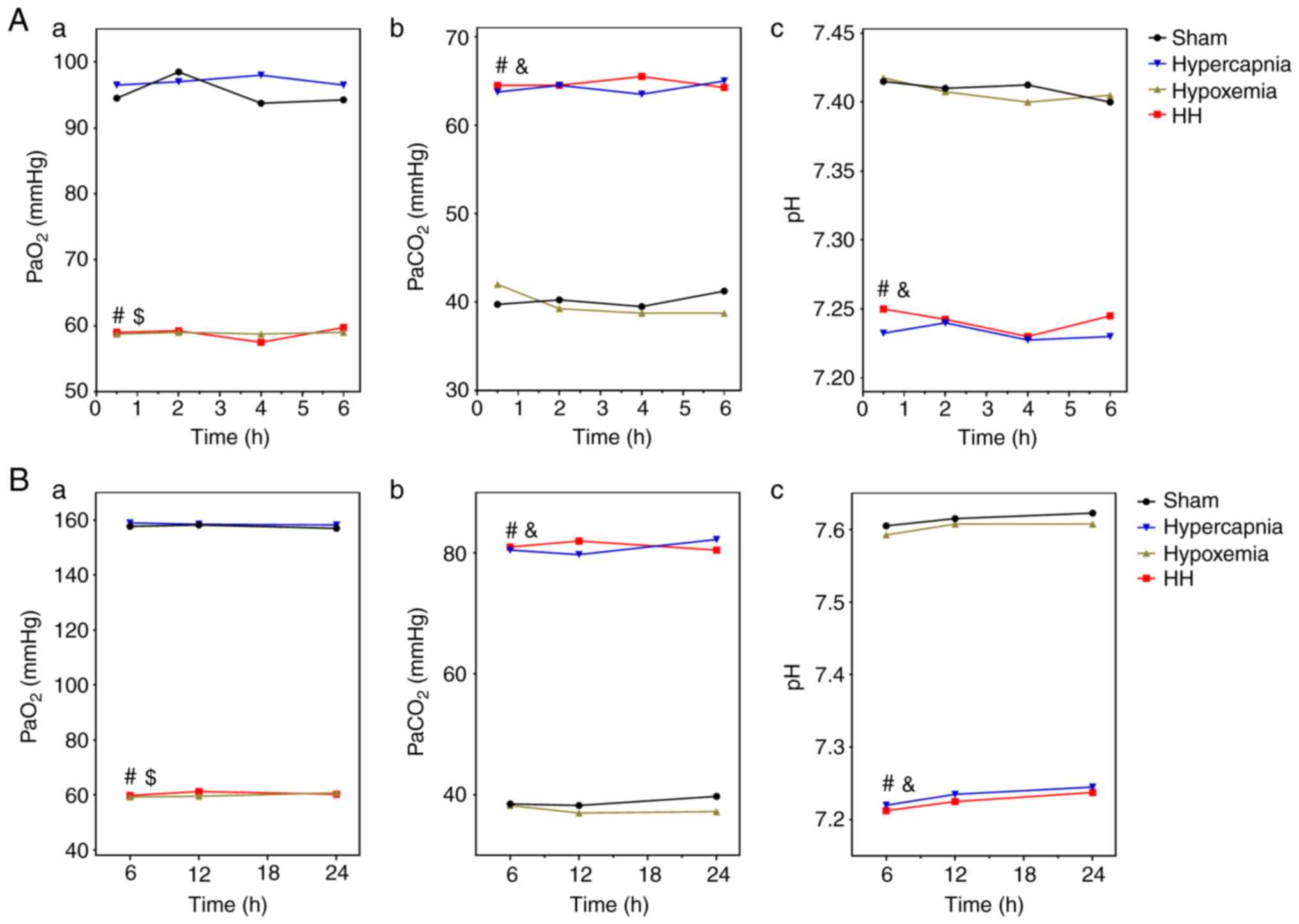
PO2, PCO2 and pH
levels in the arterial blood of the rats
The PO2 levels in the arterial blood were
maintained at ~60 mmHg in the HH and hypoxemia groups, and were
significantly decreased compared with those in the Sham group (HH
vs. Sham: P<0.01; hypoxemia vs. Sham: P<0.01) and the
hypercapnia group (HH vs. hypercapnia: P<0.01; hypoxemia vs.
hypercapnia: P<0.01). The PO2 levels of the HH group
were not significantly different when compared with those of the
hypoxemia group (P>0.05; Fig.
1A-a). The PCO2 levels in the arterial blood were
maintained at 60-70 mmHg in the HH and hypercapnia groups, and were
significantly higher compared with those in the Sham group (HH vs.
Sham: P<0.01; hypercapnia vs. Sham: P<0.01) and the hypoxemia
group (HH vs. hypoxemia: P<0.01; hypercapnia vs. hypoxemia:
P<0.01). There was no significant difference between the HH and
hypercapnia groups in the PCO2 levels (P>0.05;
Fig. 1A-b). The pH of the
arterial blood was maintained at 7.20-7.25 in the HH and
hypercapnia groups, and was significantly lower compared with that
in the Sham group (HH vs. Sham: P<0.01; hypercapnia vs. Sham:
P<0.01) and the hypoxemia group (HH vs. hypoxemia: P<0.01;
hypercapnia vs. hypoxemia: P<0.01). There was no significant
difference in the pH levels between the HH and hypercapnia groups
(P>0.05; Fig. 1A-c).
PO2, PCO2 and pH
levels in the whole‑blood culture medium
The PO2 levels were maintained at ~60
mmHg in the hypoxia + HC and hypoxia groups, and were significantly
decreased compared with those in the control group (hypoxia + HC
vs. control: P<0.01; hypoxia vs. control: P<0.01) and the HC
group (hypoxia + HC vs. HC: P<0.01; hypoxia vs. HC: P<0.01).
The PO2 levels of the hypoxia + HC group were not
significantly different when compared with those of the hypoxia
group (P>0.05; Fig. 1B-a). The
PCO2 levels were maintained at ~80 mmHg in the hypoxia +
HC and HC groups, and were significantly higher compared with those
in the control group (hypoxia + HC vs. control: P<0.01; HC vs.
control: P<0.01) and the hypoxia group (hypoxia + HC vs.
hypoxia: P<0.01; HC vs. hypoxia: P<0.01). There was no
significant difference in the PCO2 levels between the
hypoxia + HC and HC groups (P>0.05; Fig. 1B-b). The pH was maintained at
7.20-7.25 in the hypoxia + HC and HC groups, and was significantly
decreased compared with that in the control group (hypoxia + HC vs.
control: P<0.01; HC vs. control: P<0.01) and the hypoxia
group (hypoxia + HC vs. hypoxia: P<0.01; HC vs. hypoxia:
P<0.01). There was no significant difference in the pH levels
between the hypoxia + HC and HC groups (P>0.05; Fig. 1B-c).
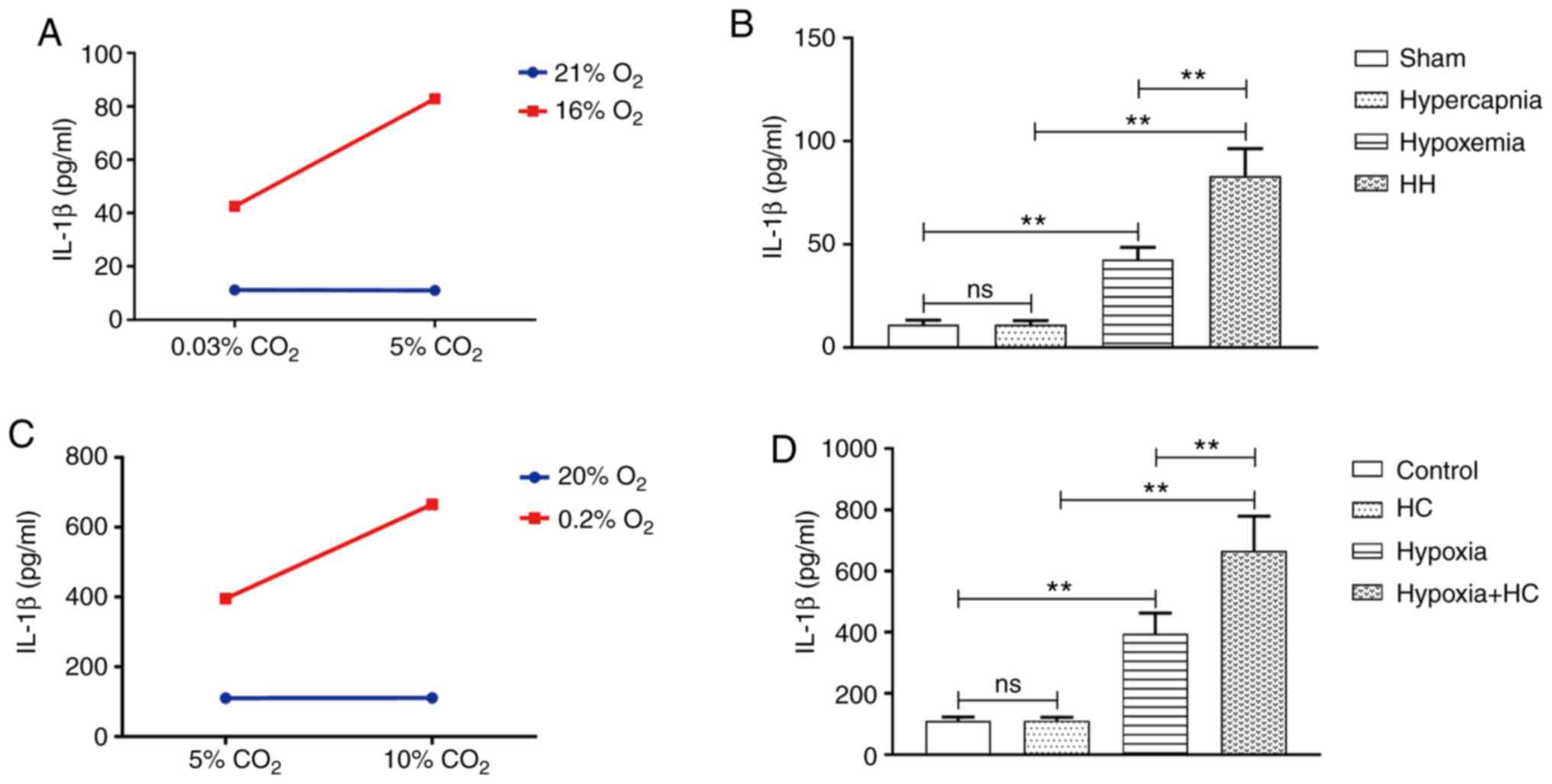
Hypercapnia increases IL‑1β expression in
the blood of hypoxemic rats
An interaction effect was observed between hypoxia
treatment and hypercapnia treatment (P<0.01; Fig. 2A). Simple effects analyses found
increased IL-1β expression in the hypoxemia group (P<0.01), but
not in the hypercapnia group (P>0.05) compared with the Sham
group. The HH group exhibited the highest expression levels of
IL-1β when compared with the hypoxemia group (P<0.01) and the
hypercapnia group (P<0.01; Fig. 2B).
Treatment with 10% CO2
increases IL‑1β expression in hypoxic whole‑blood cultures
An interaction effect was observed between 10%
CO2 treatment and 0.2% O2 treatment
(P<0.01; Fig. 2C). Simple
effects analyses found increased IL-1β expression in the hypoxia
group (P<0.01), but not in the HC group (P>0.05) compared
with the control group. The hypoxia + HC group exhibited the
highest expression levels of IL-1β compared with the hypoxia group
(P<0.01) and the HC group (P<0.01; Fig. 2D).
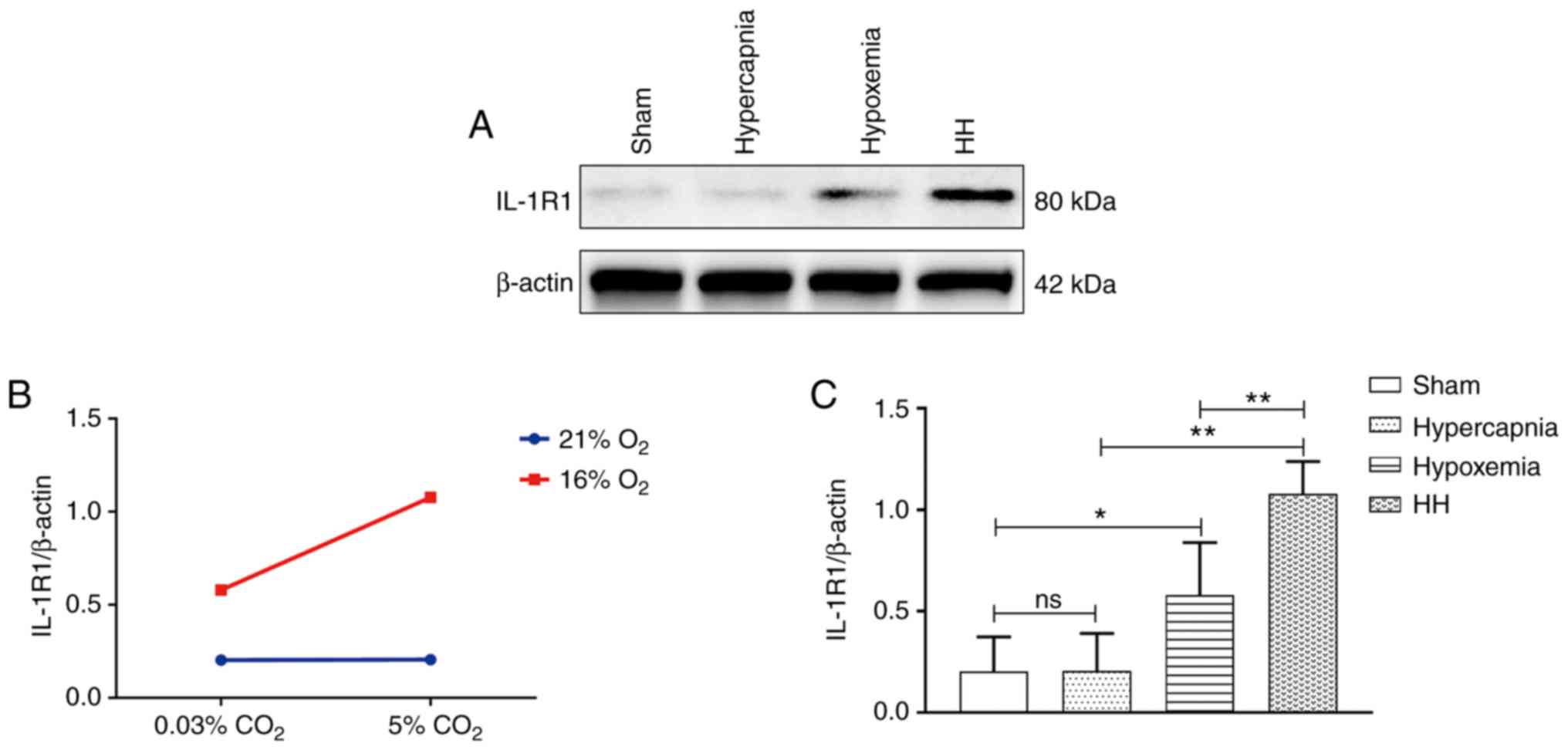
Hypercapnia increases IL‑1R1 expression
in the cerebrovascular endothelial cells of hypoxemic rats
An interaction effect was observed between hypoxia
treatment and hypercapnia treatment (P<0.05; Fig. 3B). Simple effects analyses found
increased IL-1R1 expression in the hypoxemia group (P<0.05), but
not in the hypercapnia group (P>0.05) when compared with the
Sham group. The expression levels of IL-1R1 were the highest in the
HH group compared with those in the hypoxemia group (P<0.01) and
the hypercapnia group (P<0.01; Fig. 3C). Double immunofluorescence was
used to examine IL-1R1 expression in cerebrovascular endothelial
cells. Enhanced IL‑1R1 immunofluorescence was observed in the
hypoxemia group, but not in the hypercapnia group compared with the
Sham group. The HH group exhibited the most intense IL-1R1
fluorescence compared with the hypoxemia and hypercapnia groups
(Fig. 3D).
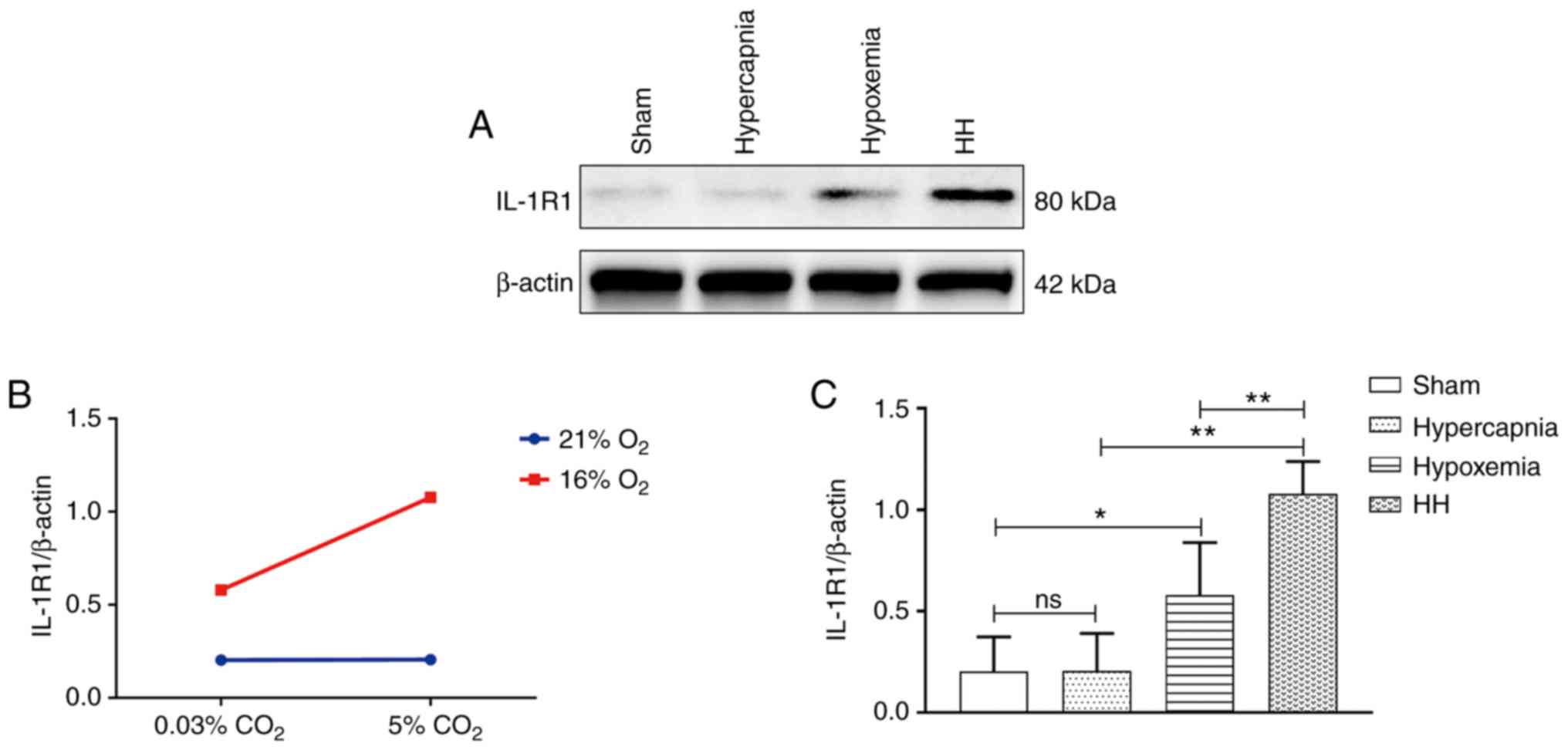 | Figure 3Hypercapnia increased IL-1R1
expression in the cerebrovascular endothelial cells of hypoxemic
rats (n=4). (A) Immunoreactive bands of IL-1R1 (80 kDa) and β-actin
(42 kDa). (B) There was an interaction effect between hypoxia
treatment and hypercapnia treatment (P<0.05). (C) Simple effects
analyses revealed increased IL-1R1 expression in the hypoxemia
group (*P<0.05), but not in the hypercapnia group
(P>0.05) compared with the Sham group. The HH group exhibited
the highest expression levels of IL-1R1 when compared with the
hypoxemia group (**P<0.01) and the hypercapnia group
(**P<0.01). (D) Immunofluorescence images showing the
expression of CD31+ cerebrovascular endothelial cells
(a, d, g and j, green), IL-1R1 (b, e, h and k, red), and the
co‑localization of IL‑1R1 and cerebrovascular endothelial cells (c,
f, i and l). Of note, enhanced IL‑1R1 immunofluorescence was
evident in the hypoxemia group, but not in the hypercapnia group,
compared with the Sham group. The HH group emitted the strongest
IL‑1R1 fluorescence as compared with the hypoxemia and hypercapnia
groups. Scale bars (a-l): 50 μm. The concentrations of
O2 and CO2 in the air were 21 and 0.03%,
respectively. IL-1R, interleukin-1 receptor; HH, hypercapnia +
hypoxemia; ns, non‑significant. |
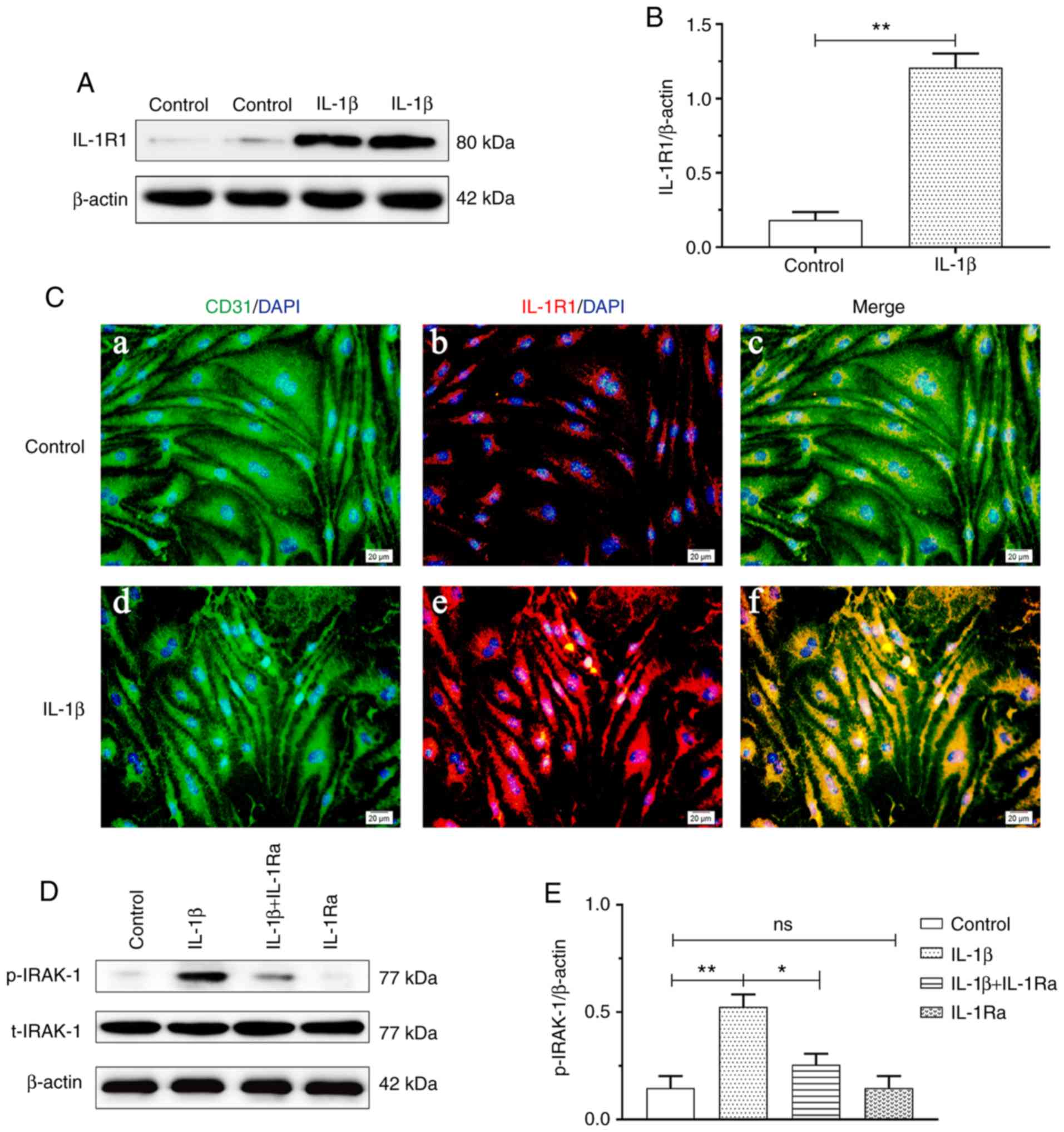
IL‑1β treatment increases IL‑1R1 and
p‑IRAK‑1 expression in RBECs
IL-1R1 expression was increased in the IL-1β group
compared with that in the control group (P<0.01; Fig. 4B). Double immunofluorescence was
used to examine IL-1R1 expression in RBECs. Enhanced IL‑1R1
immunofluorescence was observed in the IL-1β group compared with
that in the Sham group (Fig. 4C).
Increased p-IRAK-1 expression was observed in the IL-1β group
compared with that in the control group (P<0.01). The
protein expression of p‑IRAK‑1 was significantly suppressed with
IL-1Ra pretreatment (P<0.05; Fig. 4E).
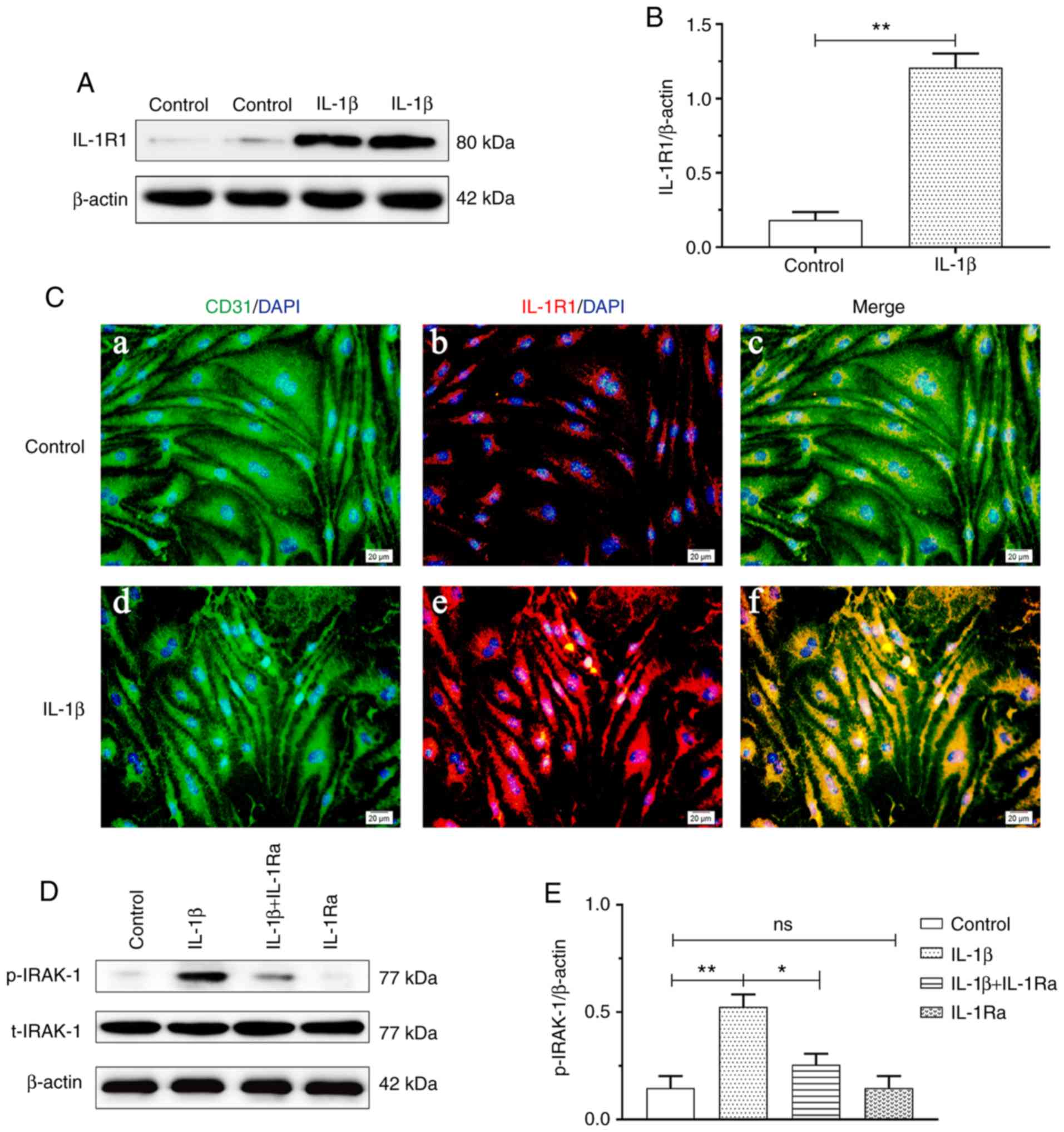 | Figure 4IL-1β treatment increased IL-1R1 and
p-IRAK-1 expression in RBECs (n=4). (A) Immunoreactive bands of
IL-1R1 (80 kDa) and β-actin (42 kDa). (B) The bar graph shows
increased IL-1R1 expression in the IL-1β group compared with that
in the control group (**P<0.01). (C)
Immunofluorescence images showing the expression of
CD31+ RBECs (a and d, green), IL-1R1 (b and e, red), and
the co-localization of IL-1R1 and RBECs (c and f). Enhanced IL-1R1
immunofluorescence was evident in the IL‑1β group compared with the
control group. Scale bars (a-f): 10 μm. (D) Immunoreactive
bands of p-RIAK-1 (77 kDa), t-IRAK-1 (77 kDa) and β-actin (42 kDa).
(E) The bar graph shows increased p-IRAK-1 expression in the IL-1β
group compared with the control group (**P<0.01). The
protein expression of p‑IRAK‑1 was significantly suppressed with
IL‑1Ra treatment (*P<0.05). RBECs, rat brain
capillary endothelial cells; IL-1β, interleukin-1β; IL‑1R,
interleukin‑1 receptor; IL‑1Ra, interleukin‑1 receptor antagonist;
HC, high concentration of carbon dioxide; ns, non‑significant. |
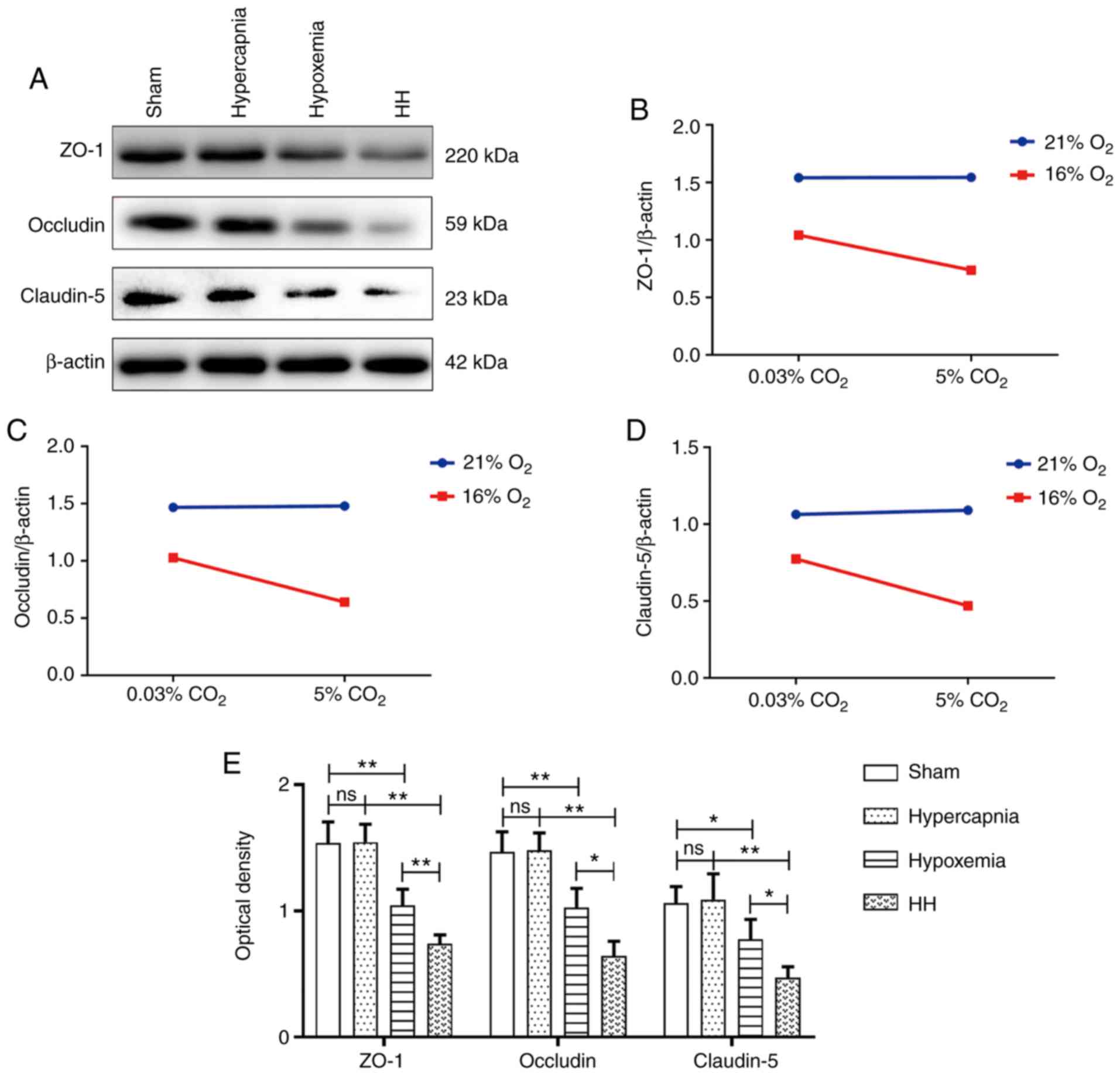
Hypercapnia decreases tight junctional
protein expression in the cerebrovascular endothelial cells of
hypoxemic rats
Significant interaction effects were observed
between hypoxia treatment and hypercapnia treatment (ZO-1:
P<0.05; occludin: P<0.05; and claudin-5: P<0.05; Fig. 5B-D). Simple effects analyses found
decreased expression of tight junctional proteins in the hypoxemia
group (ZO-1: P<0.01; occludin: P<0.01; and claudin-5:
P<0.05), but not in the hypercapnia group (ZO-1: P>0.05;
occludin: P>0.05; and claudin-5: P>0.05) compared with the
Sham group. The HH group exhibited the lowest expression levels of
tight junctional proteins in comparison with the hypoxemia group
(ZO-1: P<0.01; occludin: P<0.05; and claudin-5: P<0.05)
and the hypercapnia group (ZO-1: P<0.01; occludin: P<0.01;
and claudin-5: P<0.01; Fig.
5E). Double immunofluorescence was used to examine tight
junctional protein expression in cerebrovascular endothelial cells
(Figs. S1-S3). Reduced ZO-1,
occludin and claudin-5 immunofluorescence was observed in the
hypoxemia group, but not in the hypercapnia group, when compared
with the Sham group. The HH group exhibited the weakest ZO-1,
occludin and claudin‑5 fluorescence compared with the hypoxemia and
hypercapnia groups.
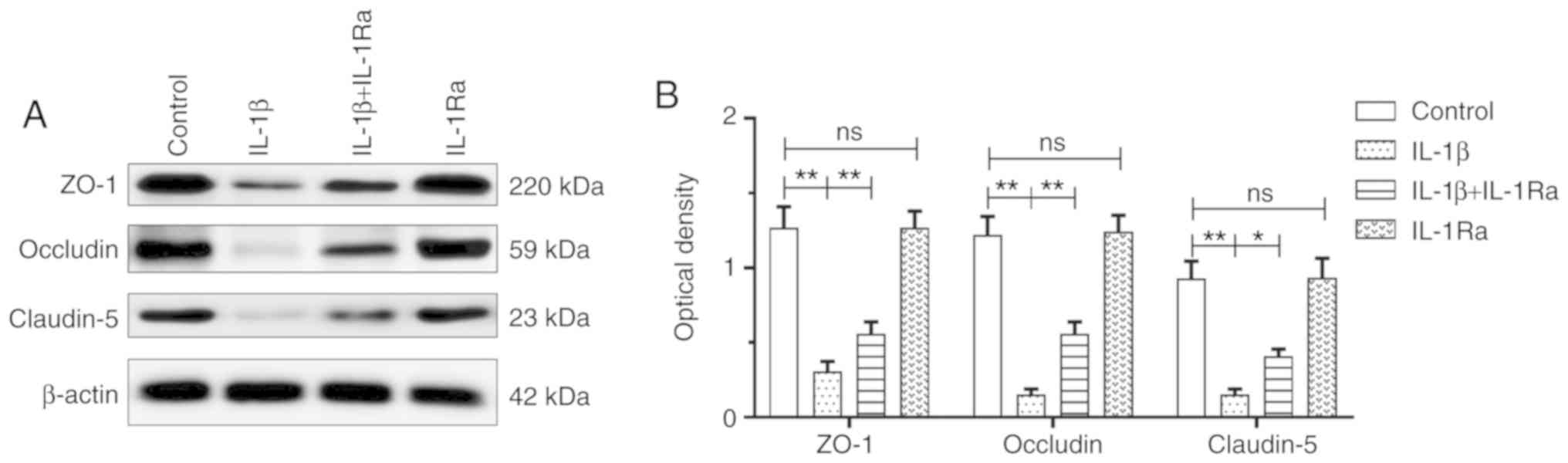
IL‑1β treatment decreases tight
junctional protein expression in RBECs
The IL-1β group exhibited decreased tight junctional
protein expression compared with the control group (ZO-1:
P<0.01; occludin: P<0.01; and claudin-5: P<0.01).
The tight junctional protein expression was significantly
upregulated with IL-1Ra pretreatment (ZO-1: P<0.01; occludin:
P<0.01; and claudin-5: P<0.05; Fig. 6). Double immunofluorescence was
used to examine tight junctional protein expression in RBECs
(Figs. S4-S6). Reduced ZO-1,
occludin and claudin‑5 immunofluorescence was observed in the IL-1β
group compared with that in the control group. Of note, ZO‑1,
occludin and claudin‑5 fluorescence was enhanced with IL-1Ra
pretreatment in RBECs.
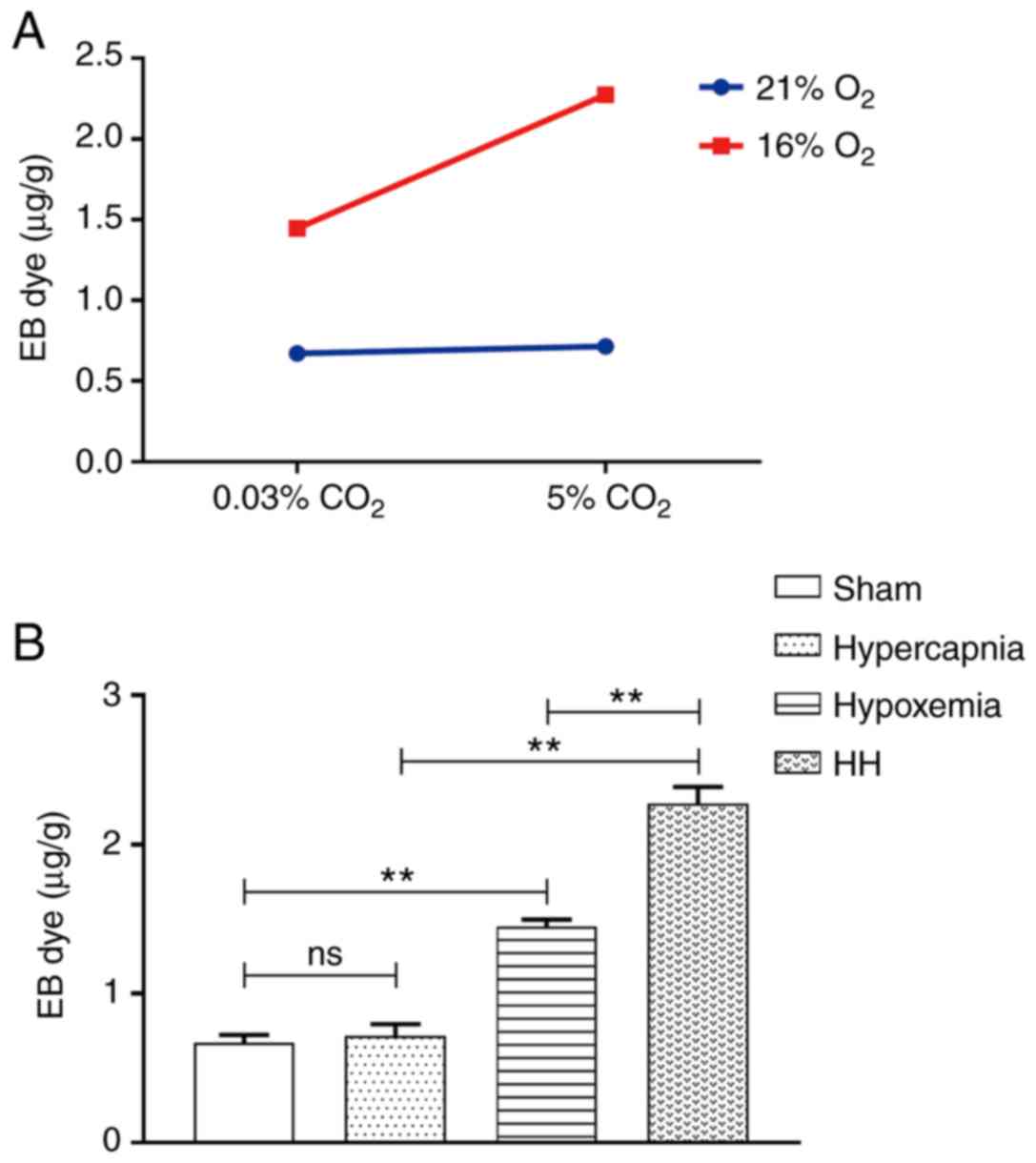
Hypercapnia increases BBB permeability to
EB in hypoxemic rats
An interaction effect was observed between hypoxia
treatment and hypercapnia treatment (P<0.01; Fig. 7A). Simple effects analyses found
increased extravasation of EB in the hypoxemia group (P<0.01),
but not in the hypercapnia group (P>0.05) compared with the Sham
group. The extravasation of EB was the most prominent in the HH
group compared with the hypoxemia group (P<0.01) and the
hypercapnia group (P<0.01; Fig.
7B).
Discussion
The present study demonstrated that hypercapnia
could increase BBB permeability through inducing IL-1β
overexpression in the blood of hypoxemic rats. Additionally, it was
demonstrated that hypercapnia decreased tight junctional protein
expression in hypoxic cerebrovascular endothelial cells via the
IL-1R1/p-IRAK-1 pathway. This was further verified by the increased
expression of tight junctional proteins in hypoxic cerebrovascular
endothelial cells when the effects of IL-1β were blocked by
IL-1Ra.
The present rat model of hypercapnia/hypoxemia was
established as described in our previous study (6). In the Sham group, the rats were
exposed to air when the ventilator settings were fixed. The
PaCO2 levels of the rats were maintained at 35-45 mmHg,
and the PaO2 levels were maintained at 90-100 mmHg. The
normal range of human PaCO2 and PaO2 is 35-45
and 80-100 mmHg, respectively, which are comparable between rats
and humans. Treatment with 16% O2 maintained the
PO2 levels of the arterial blood at ~60 mmHg, and 5%
CO2 treatment maintained the PCO2 levels of
the arterial blood at 60-70 mmHg, with the pH levels at 7.20-7.25.
In vitro, 0.02% O2 treatment maintained the
PO2 levels of whole-blood culture medium at ~60 mmHg.
The PCO2 was ~80 mmHg, with the pH at 7.20-7.25 when
treated with 10% CO2. The rats were treated with 5%
CO2 and 10% CO2 was used to treat human
whole-blood cultures. Although the CO2 concentrations
were different in vivo and in vitro, the pH levels
were consistent with the changes of permissive hypercapnia in ARDS
(26-29).
The results of the present study demonstrated that
hypercapnia enhanced the expression of IL-1β in hypoxic rats and
whole-blood cultures. It has been reported that hypercapnia
attenuated endotoxin‑induced inflammation through inhibiting
nuclear factor (NF)-κB activation (21,30). The earlier research results appear
to contradict those of the present study. However, the difference
may be due to the underlying mechanism, whereby hypercapnia would
exert its effects on IL-1β expression in the hypoxic blood.
Endotoxin may induce IL-1β expression through the Toll-like
receptor/NF-κB pathway (31-33). Hypoxia may also activate the NLRP3
inflammasome via inducing reactive oxygen species (ROS)
overproduction, which can promote the secretion of IL-1β (34-37). In the present study, it was
observed that hypercapnia alone may not be sufficient to increase
the expression of IL-1β, but hypercapnia may exert its effects in
the presence of hypoxia. It was suggested that hypercapnia can
induce ROS overproduction via intensifying hypoxia, may activate
the NLRP3 inflammasome and promote IL-1β release. In the central
nervous system, it was previously demonstrated that
hypercapnia-induced NLRP3 inflamma-some activation in
hypoxia-activated microglia upregulated the expression of IL-1β
(6). These findings are
consistent with the effects of hypercapnia on IL-1β expression in
the hypoxic blood in the present study.
To elucidate the mechanism through which hypercapnia
can increase BBB permeability in hypoxemic rats through
upregulating the expression of IL-1β, the expression levels of
IL-1R1, p-IRAK-1 and tight junctional proteins (ZO-1, occludin and
claudin-5) in cerebral vascular endothelial cells were examined. It
was demonstrated that hypercapnia increased the expression of
IL-1R1 and p-IRAK-1 and downregulated the expression of tight
junctional proteins in hypoxic cerebral vascular endothelial cells.
The expression of tight junctional proteins was markedly increased
following treatment with IL-1Ra, an IL-1 receptor antagonist.
IRAK-1 is critically involved in the regulation of intracellular
signaling networks. IRAK-1 may perform distinct functions,
including activation of NF-κB (38), which is closely associated with
the disruption of the BBB (39,40). Taken together, these findings
suggest that hypercapnia may aggravate BBB disruption in hypoxemic
rats via inducing IL-1β overproduction. However, a limitation of
the present study is that other cytokines (e.g., tumor necrosis
factor-α) were not investigated, which should be addressed in
future studies.
In summary, the present study demonstrated that
hypercapnia serves as a stimulus triggering inflammation in the
hypoxic blood. In this setting, hypercapnia may contribute to IL-1β
overproduction in the hypoxic blood, and then down-regulate the
expression of tight junctional proteins in the hypoxic cerebral
vascular endothelial cells, thereby further disrupting BBB
integrity in hypoxemic rats. The increased expression of tight
junctional proteins in hypoxic cerebro-vascular endothelial cells
when the effects of IL-1β are blocked by IL-1Ra further supports
this hypothesis. Thus, the cascade of hypercapnia-induced IL-1β
overproduction in hypoxic blood may be a potential target for
ameliorating BBB disruption.
Supplementary Data
Funding
This study was supported by the Natural Science
Foundation of Guangdong Province (grant nos. 2016A030311043 and
2017A030313691), the Medical Scientific Research Foundation of
Guangdong Province (grant nos. A2019135 and A2017284), the
Scientific Research Project of Guangdong Provincial Bureau of
Traditional Chinese Medicine (grant no. 20201045) and the Science
and Technology Program of Guangzhou (grant no. 202002030338).
Availability of data and materials
The datasets generated and/or analyzed during the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
HZ conceived the project and designed the
experiments. HD carried out the assessment of BBB permeability and
IL-1β evaluation by ELISA. XuL established the rat model of
hypercapnia/hypoxemia. XiL carried out human whole-blood cultures
and treatment. MW carried out cerebrovascular endothelial cell
cultures and treatment. YH, LH and YL performed western blotting
and immunofluorescence staining. HD and ML conducted the
statistical analysis. HD and XuL wrote the manuscript. All the
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The animal experimental protocols were approved by
the Experimental Animal Care and Use Committee at Jinan University
(approval no. 20171011001). The protocols involving human samples
were approved by the Research Ethics Committee of Guangdong
Provincial People's Hospital, Guangdong Academy of Medical
Sciences, Guangzhou, China [approval no. GDREC2018424H(R1)] and all
the participants provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
All the authors declare that they have no competing
interests.
Abbreviations:
|
ARDS
|
acute respiratory distress
syndrome;
|
|
BBB
|
blood-brain barrier;
|
|
IL-1β
|
interleukin-1β;
|
|
IL-1R1
|
IL-1 receptor 1;
|
|
IL-1Ra
|
IL-1 receptor antagonist;
|
|
NF-κB
|
nuclear factor-κB;
|
|
RBECs
|
rat brain capillary endothelial
cells
|
Acknowledgements
The authors would like to thank Zhengkang Ding and
Zixi Yang for the technical support.
References
|
1
|
Matthay MA, Zemans RL, Zimmerman GA, Arabi
YM, Beitler JR, Mercat A, Herridge M, Randolph AG and Calfee CS:
Acute respiratory distress syndrome. Nat Rev Dis Primers. 5:182019.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Papazian L, Aubron C, Brochard L, Chiche
JD, Combes A, Dreyfuss D, Forel JM, Guerin C, Jaber S, Mekontso-
Dessap A, et al: Formal guidelines: Management of acute respiratory
distress syndrome. Ann Intensive Care. 9:692019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Broccard AF, Hotchkiss JR, Vannay C,
Markert M, Sauty A, Feihl F and Schaller MD: Protective effects of
hypercapnic acidosis on ventilator-induced lung injury. Am J Respir
Crit Care Med. 164:802–806. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Laffey JG, Tanaka M, Engelberts D, Luo X,
Yuan S, Tanswell AK, Post M, Lindsay T and Kavanagh BP: Therapeutic
hypercapnia reduces pulmonary and systemic injury following in vivo
lung reperfusion. Am J Respir Crit Care Med. 162:2287–2294. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Peltekova V, Engelberts D, Otulakowski G,
Uematsu S, Post M and Kavanagh BP: Hypercapnic acidosis in
ventilator-induced lung injury. Intensive Care Med. 36:869–878.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ding HG, Deng YY, Yang RQ, Wang QS, Jiang
WQ, Han YL, Huang LQ, Wen MY, Zhong WH, Li XS, et al: Hypercapnia
induces IL-1β overproduction via activation of NLRP3 inflam-masome:
Implication in cognitive impairment in hypoxemic adult rats. J
Neuroinflammation. 15:42018. View Article : Google Scholar
|
|
7
|
Bowman GL, Dayon L, Kirkland R, Wojcik J,
Peyratout G, Severin IC, Henry H, Oikonomidi A, Migliavacca E
Bacher and Popp J: Blood‑brain barrier breakdown,
neuroinflammation, and cognitive decline in older adults.
Alzheimers Dement. 14:1640–1650. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nwafor DC, Brichacek AL, Mohammad AS,
Griffith J, Lucke-Wold BP, Benkovic SA, Geldenhuys WJ, Lockman PR
and Brown CM: Targeting the blood-brain barrier to prevent
sepsis-associated cognitive impairment. J Cent Nerv Syst Dis.
11:5933000842019. View Article : Google Scholar
|
|
9
|
Toyama K, Spin JM, Deng AC, Huang TT, Wei
K, Wagenhäuser MU, Yoshino T, Nguyen H, Mulorz J, Kundu S, et al:
MicroRNA-mediated therapy modulating blood-brain barrier disruption
improves vascular cognitive impairment. Arterioscler Thromb Vasc
Biol. 38:1392–1406. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ni P, Dong H, Wang Y, Zhou Q, Xu M, Qian Y
and Sun J: IL-17A contributes to perioperative neurocognitive
disorders through blood-brain barrier disruption in aged mice. J
Neuroinflammation. 15:3322018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Montagne A, Barnes SR, Sweeney MD,
Halliday MR, Sagare AP, Zhao Z, Toga AW, Jacobs RE, Liu CY, Amezcua
L, et al: Blood-brain barrier breakdown in the aging human
hippo-campus. Neuron. 85:296–302. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Iadecola C: Dangerous leaks: Blood-brain
barrier woes in the aging hippocampus. Neuron. 85:231–233. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nation DA, Sweeney MD, Montagne A, Sagare
AP, D'Orazio LM, Pachicano M, Sepehrband F, Nelson AR, Buennagel
DP, Harrington MG, et al: Blood-brain barrier breakdown is an early
biomarker of human cognitive dysfunction. Nat Med. 25:270–276.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang B, Li S, Cao X, Dou X, Li J, Wang L,
Wang M and Bi Y: Blood-brain barrier disruption leads to
postoperative cognitive dysfunction. Curr Neurovasc Res.
14:359–367. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ye ZY, Xing HY, Wang B, Liu M and Lv PY:
DL-3-n-butylphthalide protects the blood-brain barrier against
ischemia/hypoxia injury via upregulation of tight junction
proteins. Chin Med J (Engl). 132:1344–1353. 2019. View Article : Google Scholar
|
|
16
|
Jiao H, Wang Z, Liu Y, Wang P and Xue Y:
Specific role of tight junction proteins claudin-5, occludin, and
ZO-1 of the blood-brain barrier in a focal cerebral ischemic
insult. J Mol Neurosci. 44:130–139. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dhanda S and Sandhir R: Blood-brain
barrier permeability is exacerbated in experimental model of
hepatic encephalopathy via MMP-9 activation and downregulation of
tight junction proteins. Mol Neurobiol. 55:3642–3659. 2018.
|
|
18
|
Zenaro E, Piacentino G and Constantin G:
The blood-brain barrier in Alzheimer's disease. Neurobiol Dis.
107:41–56. 2017. View Article : Google Scholar :
|
|
19
|
Obermeier B, Daneman R and Ransohoff RM:
Development, maintenance and disruption of the blood-brain barrier.
Nat Med. 19:1584–1596. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang Y, Jin S, Sonobe Y, Cheng Y, Horiuchi
H, Parajuli B, Kawanokuchi J, Mizuno T, Takeuchi H and Suzumura A:
Interleukin-1β induces blood-brain barrier disruption by
down-regulating Sonic hedgehog in astrocytes. PLoS One.
9:e1100242014. View Article : Google Scholar
|
|
21
|
Kimura D, Totapally BR, Raszynski A,
Ramachandran C and Torbati D: The effects of CO2 on
cytokine concentrations in endotoxin-stimulated human whole blood.
Crit Care Med. 36:2823–2827. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nakagawa S, Deli MA, Nakao S, Honda M,
Hayashi K, Nakaoke R, Kataoka Y and Niwa M: Pericytes from brain
microvessels strengthen the barrier integrity in primary cultures
of rat brain endothelial cells. Cell Mol Neurobiol. 27:687–694.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takata F, Sumi N, Nishioku T, Harada E,
Wakigawa T, Shuto H, Yamauchi A and Kataoka Y: Oncostatin M induces
functional and structural impairment of blood-brain barriers
comprised of rat brain capillary endothelial cells. Neurosci Lett.
441:163–166. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Morofuji Y, Nakagawa S, So G, Hiu T, Horai
S, Hayashi K, Tanaka K, Suyama K, Deli MA, Nagata I and Niwa M:
Pitavastatin strengthens the barrier integrity in primary cultures
of rat brain endothelial cells. Cell Mol Neurobiol. 30:727–735.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Han Q, Lin Q, Huang P, Chen M, Hu X, Fu H,
He S, Shen F, Zeng H and Deng Y: Microglia-derived IL-1β
contributes to axon development disorders and synaptic deficit
through p38‑MAPK signal pathway in septic neonatal rats. J
Neuroinflammation. 14:522017. View Article : Google Scholar
|
|
26
|
Takeuchi M, Taki J, Hayashi K, Higashi M,
Tachibana K, Takauchi Y and Imanaka H: Early application of the
lung protective ventilation strategy at different stages in two
ARDS patients. Masui. 53:514–521. 2004.In Japanese. PubMed/NCBI
|
|
27
|
Thorens JB, Jolliet P, Ritz M and
Chevrolet JC: Effects of rapid permissive hypercapnia on
hemodynamics, gas exchange, and oxygen transport and consumption
during mechanical ventilation for the acute respiratory distress
syndrome. Intensive Care Med. 22:182–191. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hickling KG, Walsh J, Henderson S and
Jackson R: Low mortality rate in adult respiratory distress
syndrome using low-volume, pressure-limited ventilation with
permissive hyper-capnia: A prospective study. Crit Care Med.
22:1568–1578. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dushianthan A, Cusack R, Chee N, Dunn JO
and Grocott MP: Perceptions of diagnosis and management of patients
with acute respiratory distress syndrome: A survey of United
Kingdom intensive care physicians. BMC Anesthesiol. 14:872014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Takeshita K, Suzuki Y, Nishio K, Takeuchi
O, Toda K, Kudo H, Miyao N, Ishii M, Sato N, Naoki K, et al:
Hypercapnic acidosis attenuates endotoxin-induced nuclear
factor-[kappa]B activation. Am J Respir Cell Mol Biol. 29:124–132.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Gay NJ, Symmons MF, Gangloff M and Bryant
CE: Assembly and localization of Toll-like receptor signalling
complexes. Nat Rev Immunol. 14:546–558. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen Y, Liu T, Langford P, Hua K, Zhou S,
Zhai Y, Xiao H, Luo R, Bi D, Jin H and Zhou R: Haemophilus parasuis
induces activation of NF-κB and MAP kinase signaling pathways
mediated by toll-like receptors. Mol Immunol. 65:360–366. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhang Y, Lu Y, Ma L, Cao X, Xiao J, Chen
J, Jiao S, Gao Y, Liu C, Duan Z, et al: Activation of vascular
endothelial growth factor receptor-3 in macrophages restrains
TLR4-NF-κB signaling and protects against endotoxin shock.
Immunity. 40:501–514. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tschopp J and Schroder K: NLRP3
inflammasome activation: The convergence of multiple signalling
pathways on ROS production? Nat Rev Immunol. 10:210–215. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Dai Y, Zhang J, Xiang J, Li Y, Wu D and Xu
J: Calcitriol inhibits ROS-NLRP3-IL-1beta signaling axis via
activation of Nrf2-antioxidant signaling in hyperosmotic stress
stimulated human corneal epithelial cells. Redox Biol.
21:1010932019. View Article : Google Scholar
|
|
36
|
Hoyt LR, Randall MJ, Ather JL, DePuccio
DP, Landry CC, Qian X, Janssen-Heininger YM, van der Vliet A, Dixon
AE, Amiel E and Poynter ME: Mitochondrial ROS induced by chronic
ethanol exposure promote hyper-activation of the NLRP3
inflammasome. Redox Biol. 12:883–896. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Abais JM, Xia M, Zhang Y, Boini KM and Li
PL: Redox regulation of NLRP3 inflammasomes: ROS as trigger or
effector? Antioxid Redox Signal. 22:1111–1129. 2015. View Article : Google Scholar :
|
|
38
|
Song YJ, Jen KY, Soni V, Kieff E and
Cahir-McFarland E: IL-1 receptor-associated kinase 1 is critical
for latent membrane protein 1-induced p65/RelA serine 536
phosphorylation and NF-kappaB activation. Proc Natl Acad Sci USA.
103:2689–2694. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Dong L, Qiao H, Zhang X, Zhang X, Wang C,
Wang L, Cui L, Zhao J, Xing Y, Li Y, et al: Parthenolide is
neuro-protective in rat experimental stroke model: Downregulating
NF-κB, phospho-p38MAPK, and caspase-1 and ameliorating BBB
permeability. Mediators Inflamm. 2013:3708042013. View Article : Google Scholar
|
|
40
|
Zhao T, Zhang X, Zhao Y, Zhang L, Bai X,
Zhang J, Zhao X, Chen L, Wang L and Cui L: Pretreatment by
evodiamine is neuroprotective in cerebral ischemia: Up-regulated
pAkt, pGSK3β, down-regulated NF-κB expression, and ameliorated BBB
permeability. Neurochem Res. 39:1612–20. 2014. View Article : Google Scholar : PubMed/NCBI
|